INTERMEDIATE
Clinically, there are some commonly used pacemaker types. Each has its own strengths and weaknesses, making them ideally suited for certain conditions. In this text, we shall review the most popular types and show you some examples of each for your review. As is customary, we will present various clinical strips at the end of the chapter.
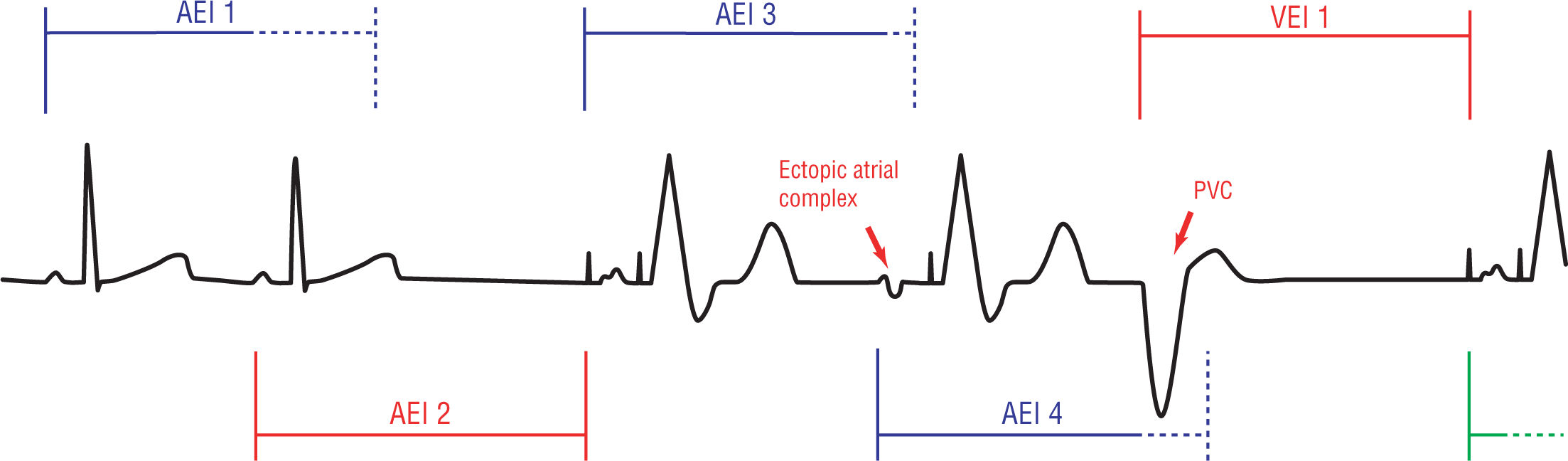
When a patient has problems with bradycardia-related symptoms but has a normally functioning AV node, the atrial demand pacemaker (AAI) may be the ideal solution. The AAI pacemaker senses the atria and paces the same atria in an inhibitory fashion. Basically, the pulse generator senses the atria for spontaneous activity. If no spontaneous atrial activity is detected during a specified period (the atrial escape interval), then the pacemaker fires an atrial depolarization wave. The wave then spreads normally through the rest of the atria, the AV nodes, and the ventricles. If spontaneous atrial activity is detected, the pacemaker is inhibited from firing, allowing the normal complex to proceed unimpeded (Figure 39-6).

Figure 39-6 An AAI pacemaker senses an atrial complex and begins to time out an atrial escape interval (AEI 1). The interval is broken by a normally occurring P wave, and the interval is reset (AEI 2). AEI 3 and 4 are not reset and so the pacemaker fires an atrial impulse.
© Jones & Bartlett Learning.
DescriptionThe ventricular demand pacemaker (VVI) is the ventricular counterpart of the AAI pacemaker discussed previously. This type of pacemaker senses and paces only the ventricles in an inhibitory manner. The pacemaker senses the ventricles for any type of spontaneous activity. When it senses activity, the pacemaker begins to time out a specified period (the VEI, discussed before). If no spontaneous ventricular activity is detected during the VEI, the pacemaker fires a ventricular depolarization wave. If spontaneous ventricular activity is detected, the pacemaker is inhibited from firing, allowing the normal complex to proceed unimpeded (Figure 39-7).

Figure 39-7 A VVI pacer senses the ventricles for spontaneous activity. If ventricular activity is sensed, no complex is fired by the pacer (see VEI 1). If ventricular activity is not sensed during the VEI (VEI 2 and 3), the pacer fires and causes a ventricular contraction.
© Jones & Bartlett Learning.
DescriptionAtrial activity will in no way interfere with the functioning of a VVI pacemaker. If a P wave occurs but does not conduct to the ventricles, the pacemaker will not be affected in any way and does not get reset. Only ventricular activity is sensed and only the ventricles are paced. These are the main functional characteristics of the VVI pacer.
The main functional characteristics mentioned earlier are also the cause of the major complications associated with this type of pacer, the so-called pacemaker syndrome. The lack of atrial contribution to ventricular filling and the inability of the heart rate to compensate for any form of exertion or exercise will give rise to various clinical symptoms related to decreased cardiac output and hypotension. These include fatigue, light-headedness, syncope, dyspnea, exercise intolerance, congestive heart failure, and anginal symptoms due to myocardial ischemia.
The AV sequential or DVI pacemaker was the first attempt to maintain AV synchrony. The DVI paces both the atria and the ventricle in a sequential manner when it does fire (Figure 39-8). The atria are depolarized first, and then a few milliseconds later, the ventricles are stimulated. This allows for ventricular filling and helps to maintain a more efficient and effective cardiac output. It does counter some of the events that lead to the pacemaker syndrome but is not as effective as the DDD pacemaker, which we will examine next.
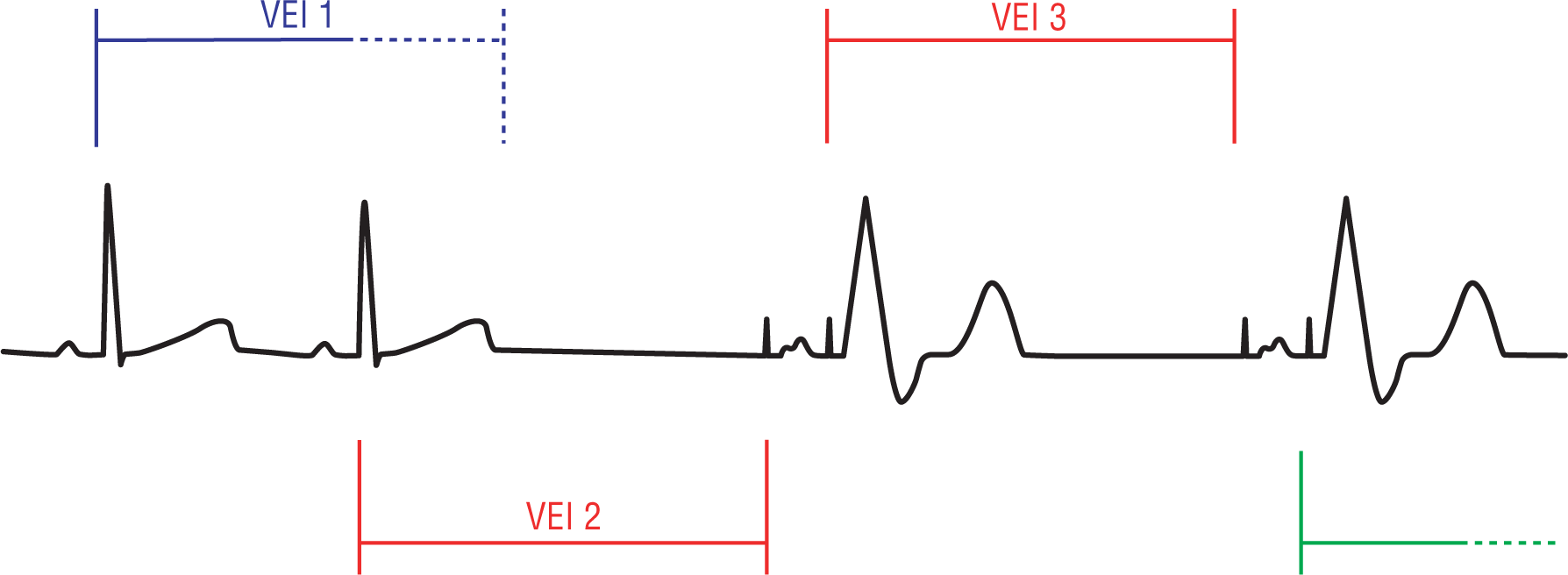
Figure 39-8 A DVI pacemaker is reset by a ventricular complex in VEI 1. During VEI 2, there is no spontaneous ventricular activity and the pacemaker fires a sequential atrial and then a ventricular complex. The same occurs in VEI 3.
© Jones & Bartlett Learning.
DescriptionThe DVI pacemaker senses the ventricle for any spontaneous ventricular activity and then paces in an inhibitory manner. If spontaneous ventricular activity is sensed by the pacemaker during the VEI that is set for that particular patient, then the pacemaker holds off and does not fire. If the pacemaker does not sense any ventricular activity during the VEI, then it fires a sequence of an atrial and then a ventricular depolarization.
The DVI pacemaker does not sense atrial activity in any way. As such, a supraventricular complex will be completely disregarded by the pacer unless it triggers a ventricular complex. This is the main drawback of the DVI pacer. By disregarding supraventricular complexes, the pacer will compete with the normal heart in some cases. PVCs and premature junctional contractions (PJCs) are sensed and will inhibit the pacer.