From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Final Test 1 Answers
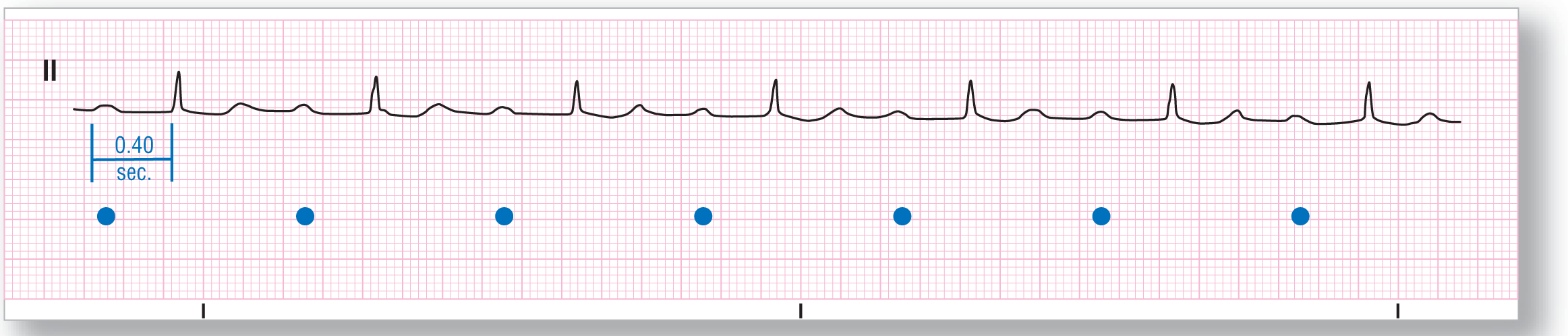
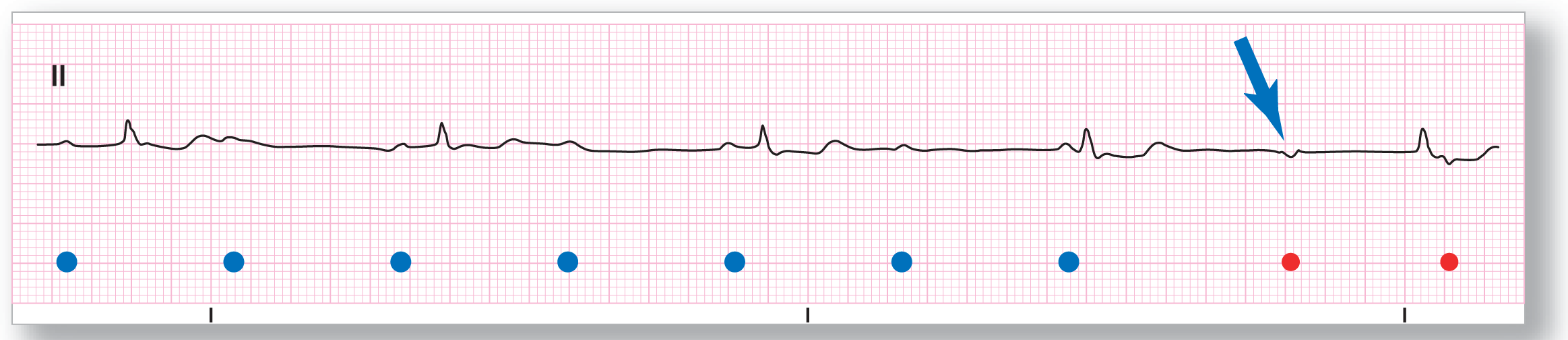
Final Test 1: ECG-1
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 60 BPM |
PR intervals: Wide |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus rhythm with a first-degree AV block |
Discussion:
The most important thing to do when approaching Final Test 1: ECG-1 is to clearly identify which are the P waves and which are the T waves because of their similar morphologies (P waves are labeled with the blue dots). This is not that difficult to do on this ECG, but if you were to have this problem in another strip, you could examine the morphologies in some different leads. The P waves are associated with very prolonged, consistent PR intervals at 0.40 seconds, making this is a first-degree AV block in a patient with an underlying sinus rhythm.
Since the P-wave and T-wave morphologies are so similar, mistaking them for each other could confuse some of you into thinking that there was a third P wave buried inside the QRS complex. The rhythm would then be an atrial tachycardia with block. This is a good thought, but it is not the case. If this were the case, the timing of the P wave would be such that you would see the beginning of the buried P wave appear as a slurring or slow upstroke of the R wave. In our strip, the R wave begins with a sharp take-off and there is no evidence of any buried P wave.
While we are on the topic of buried P waves, is there a buried P wave on the second QRS complex of the strip? The answer is no. Why? Well, if this morphology was also seen in some or all of the other complexes, you could definitely make a compelling argument for buried P waves. However, since it only occurs in that one complex, the cadence of the beat is not disrupted, and the QRS does not show any evidence of widening or fusion, we have to assume that this is underlying artifact.
Remember, in this book we are hoping to pass along the principles of the art of interpretation as it relates to arrhythmia recognition. Part of that art includes knowing both what is and what is not significant.
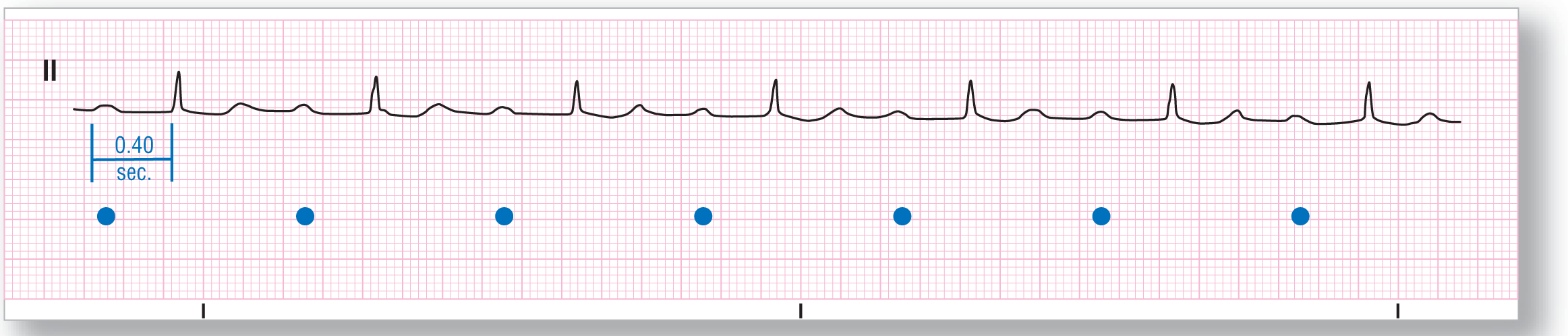
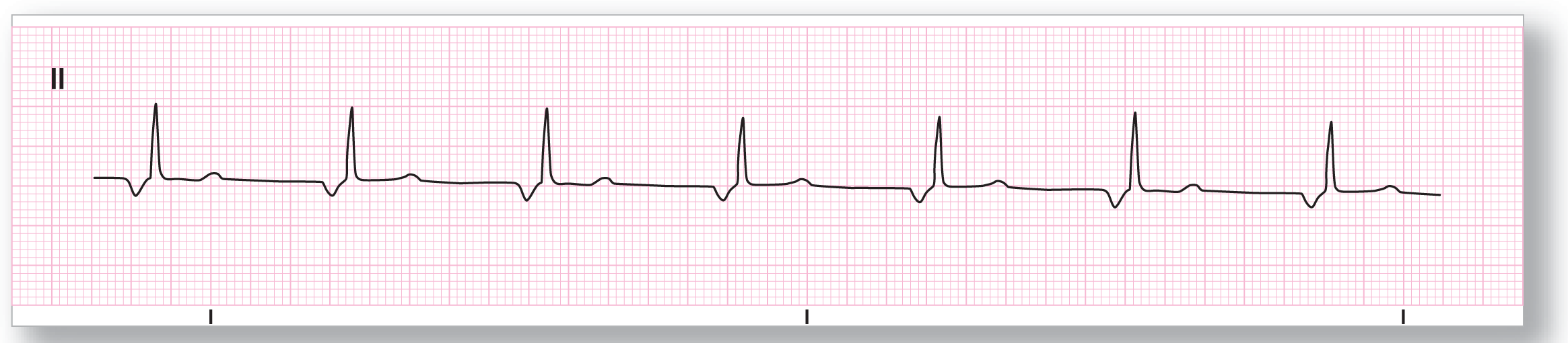
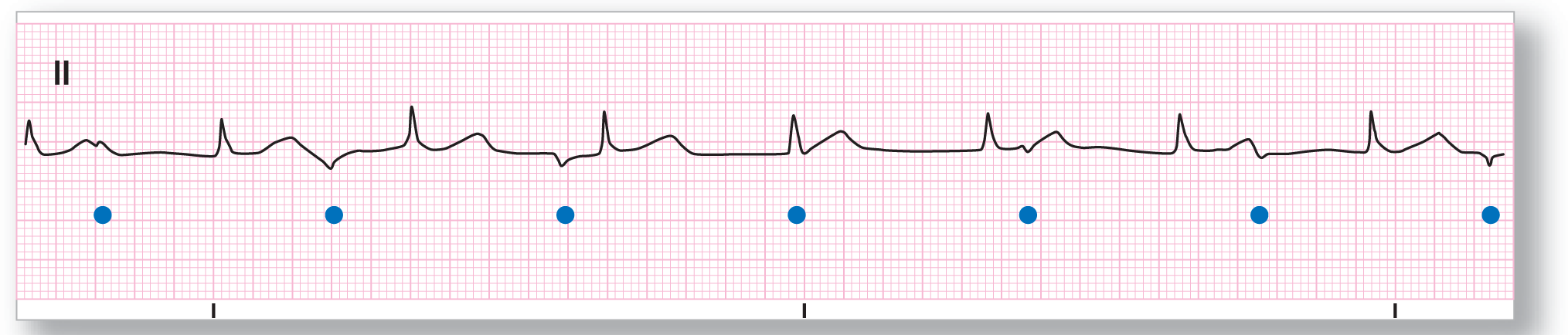
Final Test 1: ECG-2

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: Atrial: 50 BPM |
PR intervals: See discussion below |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: Third-degree AV block |
Discussion:
On Final Test 1: ECG-2, we can only see two P waves before any of the QRS complexes and they each are associated with different PR intervals (see blue arrows). On closer examination, we see that there are some morphologic changes in the QRS complexes that recur at regular intervals and are consistent with buried P waves (atrial rate of 50 BPM; see blue dots). The P waves are upright in lead II but they are completely dissociated from the QRS complexes. The lack of associated P waves and the narrow, regular ventricular response at a rate of about 64 BPM are consistent with an accelerated junctional ventricular response. Putting this all together, we have a complete or third-degree AV block with an underlying sinus bradycardia and an accelerated junctional escape rhythm.
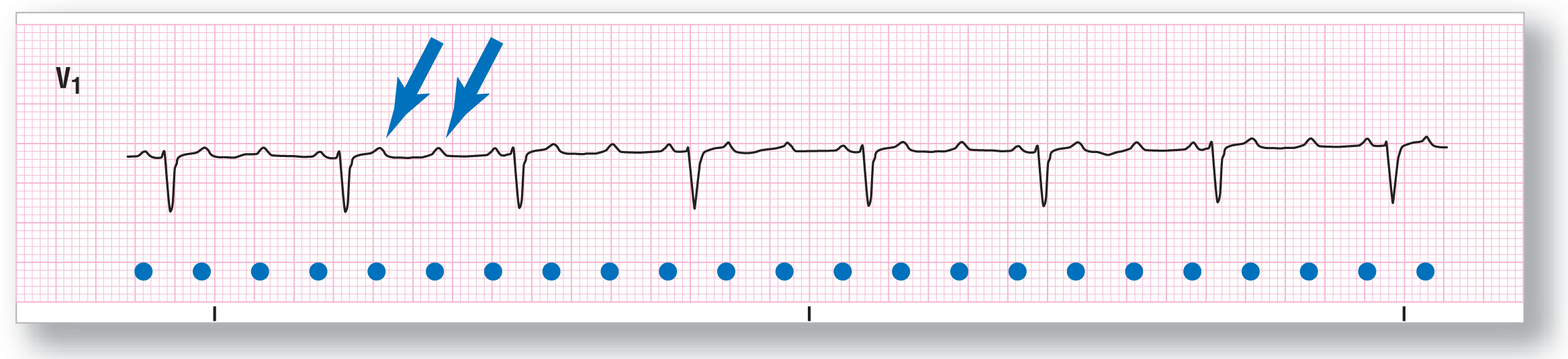
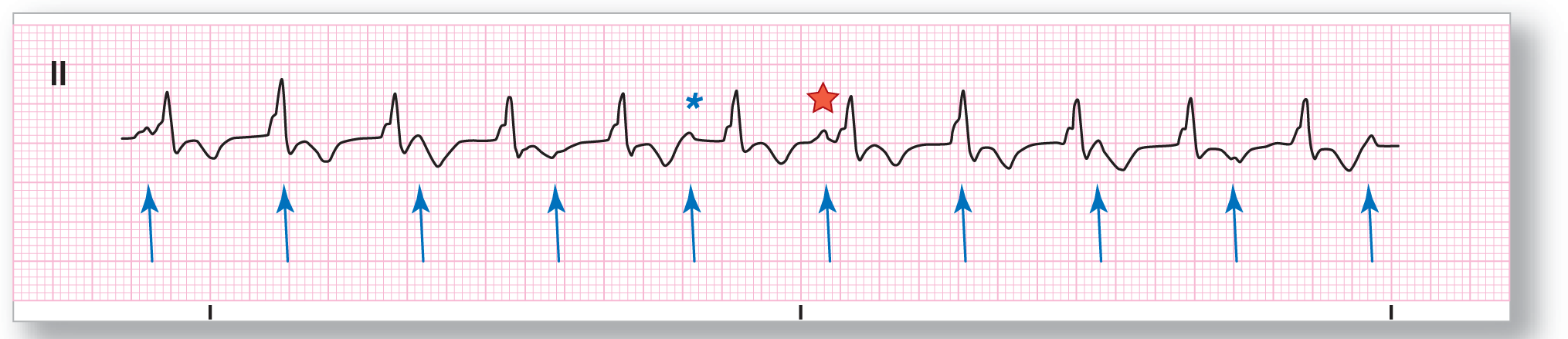
Final Test 1: ECG-3

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 150 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Inverted Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: AVNRT |
Discussion:
The first thing to ask yourself when you see a rate of about 150 BPM is: Could this be atrial flutter? In Final Test 1: ECG-3, the answer is no because there are neither flutter waves nor evidence of at least a 2:1 conduction ratio. The QRS complexes are narrow and very regular. There is an inverted area (see blue arrow) which is probably an inverted, retrograde P wave. The RP interval is short, making this consistent with an AVNRT at 150 BPM.
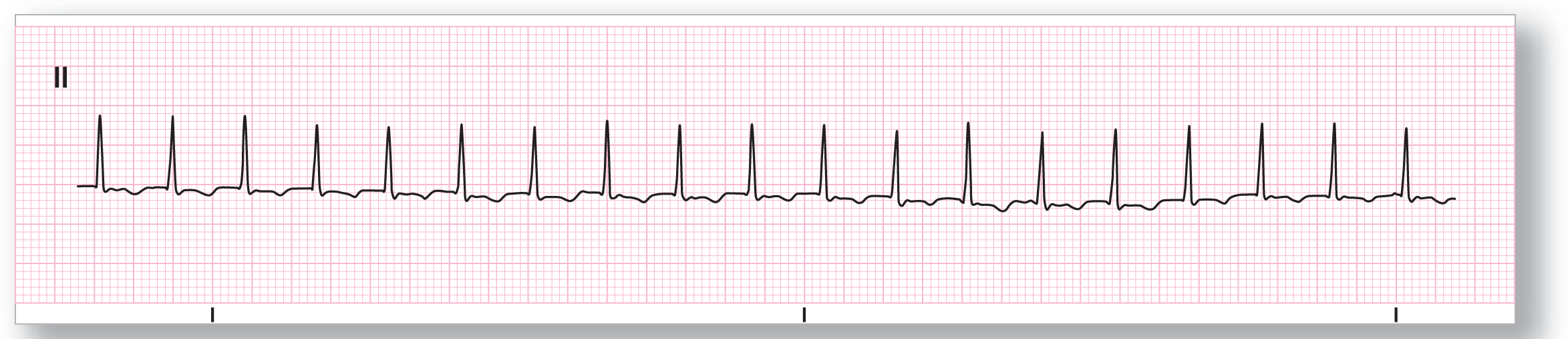
Final Test 1: ECG-4

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 62 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: Present Morphology: Inverted Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Accelerated idioventricular |
Discussion:
Final Test 1: ECG-4 shows a wide-complex rhythm with a morphology consistent with a ventricular origin. The rate is about 62 BPM, which is a little fast for a typical ventricular rhythm but is consistent with an accelerated idioventricular rhythm. The blue arrow is pointing to an inverted, retrogradely conducted P wave on the ST segment. The separation from the QRS complex to the retrogradely conducted, inverted P wave would be expected because of the long transit times needed by the depolarization wave to travel from the ectopic ventricular site of origin to the atria.
Final Test 1: ECG-5

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 150 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Monomorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-5 is a tough one. This is a wide-complex tachycardia at a rate of about 150 BPM. This could represent a ventricular tachycardia, an atrial flutter, an AVNRT, or an AVRT. It is almost impossible based on this strip to rule out any of these possibilities. Because of that reason, you should treat the patient as if she were in VTach. If she is unstable, shock her. If not, obtaining a full 12-lead ECG or looking at multiple leads would be extremely helpful. A full 12-lead ECG verified the diagnosis as VTach.
Remember, lead II can be quite deceptive in many patients because the QRS complexes tend to be small in that lead. A monomorphic VTach will, therefore, have small QRS complexes in those patients. You need to always have a high index of suspicion when you approach any wide-complex tachycardia and assume the worst.
Final Test 1: ECG-6

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 55 BPM |
PR intervals: See discussion below |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: See discussion below |
Rhythm: Mobitz I second-degree AV block |
Discussion:
Final Test 1: ECG-6 definitely shows grouping of the complexes. This should immediately make you think of the AV blocks. It doesn’t matter that the first group has a 4:3 conduction ratio and the second group has only a 3:2 conduction ratio. They are still grouped and variability in the conduction ratios is normal in AV blocks. Now, take a look at the P waves. Notice that all of the P waves have the same morphology, but their associated PR intervals are different. The PR intervals appear to lengthen until one of the P waves is eventually blocked from conducting. This is the hallmark of a Mobitz I second-degree AV block. The R-R intervals remain the same, which is atypical for a Wenckebach rhythm.
Final Test 1: ECG-7

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 95 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Atrial fibrillation |
Discussion:
Final Test 1: ECG-7 shows a wide-complex, irregularly irregular rhythm. The key words in that statement are irregularly irregular. There are three main irregularly irregular rhythms: atrial fibrillation, wandering atrial pacemaker, and multifocal atrial tachycardia. There are no obvious P waves visible on the strip, so WAP and MAT are immediately ruled out from your differential. This leaves you with atrial fibrillation. Could atrial fibrillation have wide complexes? Yes, if there were a preexisting bundle branch block, if there is aberrancy involved, or if there were significant electrolyte problems. Comparison with an old ECG showed that this patient had a preexisting left bundle branch block accounting for the wide complexes. Remember, monomorphic VTach is regular except for a few seconds at the onset of the strip or in the presence of fusion and capture beats.
Final Test 1: ECG-8

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 50 BPM |
PR intervals: Prolonged |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 1:1 |
Rhythm: Mobitz II, second-degree AV block |
Discussion:
Final Test 1: ECG-8 can be quite deceptive. At first glance the QRS complexes appear wide, but close measurement shows that they are within the normal range. Next, there is grouping with two dropped beats. The grouping makes you think of an AV block, and you would be correct. But, which one? On gross examination, the PR intervals appear to be progressively widening, but this is an optical illusion. Close measurement shows that all of the PR intervals are the same at 0.26 seconds. The optical illusion is caused by the slight fluctuations in the morphologies of the P and the QRS waves that are normally seen in almost every patient. This rhythm strip is just one of the reasons why we always suggest that you first form a quick original impression, but then use a set of ECG calipers and closely measure the intervals to verify your impressions. Rough observation can be deceptive, as it was in this case.
Final Test 1: ECG-9

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 115 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Junctional tachycardia |
Discussion:
Final Test 1: ECG-9 shows a regular narrow-complex tachycardia with no visible P waves at a rate of about 115 BPM. The only possible rhythm that fits these parameters is a junctional tachycardia.
Final Test 1: ECG-10

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 76 BPM |
PR intervals: See discussion below |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 2:1 |
Rhythm: 2:1 or untypable second-degree AV block |
Discussion:
Final Test 1: ECG-10 shows a patient who has a normally conducted P wave with a PR interval of 0.28 seconds. Then, there is another P wave that is blocked and nonconducted. Since the ratio of AV conduction is 2:1, you cannot tell which of the two kinds of type II block is involved, Mobitz I or Mobitz II. This, by definition, is an untypable or 2:1 second-degree AV block. Sometimes, longer strips in these patients will show some groupings that meet either Mobitz I or Mobitz II, allowing you to make a call as to the type involved.
Final Test 1: ECG-11

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 300 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: F waves are present Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: Variable |
Rhythm: Atrial flutter with variable block |
Discussion:
Final Test 1: ECG-11 shows a rapid atrial flutter at a rate of 300 BPM. Notice the lack of any isoelectric segment between the negative deflection, which is classic for atrial flutter. The ventricular rate in atrial flutter typically occurs at some multiple of the F-F interval, for example two, three, four, and so on times the F-F interval. However, in these uncommon cases, the R-R interval is not a direct multiple but comes at variable conduction rates. This creates a regularly irregular, or even an irregularly irregular ventricular response. Atrial flutter with variable block is one of those rare exceptions to the irregularly irregular rule we are constantly bringing up. (There are three main irregularly irregular rhythms: Afib, WAP, and MAT.)
Final Test 1: ECG-12

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: See discussion below |
PR intervals: Normal, consistent |
|
Regularity: Regularly irregular |
QRS width: See discussion below |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: Sinus rhythm with ventricular bigeminy |
Discussion:
Final Test 1: ECG-12 is a great example of ventricular bigeminy. There is one normally conducted beat and one PVC in a recurring pattern. The blue arrow points to an inverted, retrogradely conducted P wave, which is associated with a very prolonged RP interval. Remember to always check the pulse on these patients. If the PVC is causing a mechanical contraction, then the overall ventricular rate is about 80 BPM (8 beats in a 6-second strip multiplied by 10 = 80 BPM). If only the normally conducted complexes cause a mechanical contraction, then the effective ventricular rate is only 40 BPM, which could be a cause of significant hemodynamic compromise.
Final Test 1: ECG-13
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 200 BPM |
PR intervals: See discussion below |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 3:1 |
Rhythm: Focal atrial tachycardia with block |
Discussion:
The atrial complexes in Final Test 1: ECG-13 are fairly normal in appearance. There is a normal isoelectric segment between the P waves, so atrial flutter is not in the differential. This is a focal atrial tachycardia. The P waves conduct at a 3:1 ratio and the PR interval before the conducted beat is normal. The ventricular rate is about 68 BPM and the QRS complexes are narrow, which is consistent with a supraventricular origin to the complexes. The conduction ratio and the presence of the nonconducted P waves make the final diagnosis focal atrial tachycardia with block.
Final Test 1: ECG-14

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 160 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Ventricular tachycardia |
Discussion:
Final Test 1: ECG-14 is one of the toughest in this text. To begin with, you have a wide-complex tachycardia at about 160 BPM. The rhythm is regularly irregular rather than irregularly irregular because there are recurrent R-R intervals. The presence of this many recurrent R-R intervals essentially rules out atrial fibrillation as a possible cause. Ventricular tachycardia, however, is a big possibility. There are some morphologic changes in the appearance of the complexes due to fusion. (Fusion beats typically appear different from each other depending on the level of fusion between the normally conducted complex and the ventricular ectopic complex.) Could the fusion complexes account for the slight variations in regularity noted in the strip? Yes.
The third “F”-labeled complex is more consistent with a capture beat than a fusion beat. However, since we cannot tell what a native beat looks like in this patient, calling it a capture beat is a bit risky. However, saying that it is highly suggestive of one is perfectly appropriate. Remember, capture and fusion beats in a wide-complex tachycardia are basically diagnostic for VTach.
The two complexes at the end, labeled with the red stars, represent the last conundrum that we will need to address. The axis of the ventricular complexes seemed to have shifted. Morphologic shifts in appearance from LBBBs to RBBBs and axis shifts can be seen in ventricular tachycardia, although they are uncommon occurrences. To define this variant of VTach, the term bidirectional ventricular tachycardia is used. This is an advanced arrhythmia and beyond the scope of this book. For our purposes, we will just identify this rhythm as ventricular tachycardia. A full 12-lead ECG verified the diagnosis in this patient.
Final Test 1: ECG-15

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 90 BPM |
PR intervals: See discussion below |
|
Regularity: Regularly irregular |
QRS width: See discussion below |
|
P waves: See discussion below Morphology: See discussion below Axis: See discussion below |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: Sinus rhythm with intermittent PVCs and atrial pacing |
Discussion:
Final Test 1: ECG-15 is an example of a sinus rhythm that is complicated by some events. Two of those events (labeled with the blue arrows) are either PVCs or aberrantly conducted PJCs. It is impossible to determine if the pauses involved are compensatory or noncompensatory because the pauses are cut short by an atrial pacer spike (see red stars). That thin line under the red stars represents a pacemaker spike that is triggering an atrial depolarization. The atrial depolarization is then normally conducted to the ventricles, causing normal-looking, narrow QRS complexes. The type of pacemaker involved is not evident from this short strip but we do know that it senses the ventricles and paces the atria. The pacer does appears to be functioning normally.
Final Test 1: ECG-16
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 162 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Possible pseudo-S wave Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: AVNRT |
Discussion:
Final Test 1: ECG-16 shows a rapid narrow-complex tachycardia at about 162 BPM. There is a small deflection at the end of the QRS complex, which could be a part of the patient’s normally occurring QRS morphology or could represent a pseudo-S wave. Comparison with old strips or a reevaluation of the area after the tachycardia is broken will answer the question. This patient was having an episode of AVNRT at the time this strip was taken and the pseudo-S wave disappeared when the tachycardia was broken.
Final Test 1: ECG-17

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 300 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Atrial fibrillation in a patient with Wolff-Parkinson-White |
Discussion:
Final Test 1: ECG-17 brings up a commonly misdiagnosed rhythm. The initial impression of most clinicians when they look at this strip is that it is ventricular tachycardia or ventricular flutter. However, the rhythm is too irregular and too rapid to be either of these two possibilities. This rhythm is irregularly irregular even though the amount of variability between the complexes is very small. Normally, these small changes could be written off as being trivial but when the rate is this rapid, these very small distances represent a great overall change in these small R-R intervals. In other words, the smaller the R-R interval, the greater the chance that even a small variability in the interval is significant. A difference of even 0.04 seconds or less can be very significant at rates of 300 BPM.
Now, let’s discuss some issues about the rate itself. As the rate increases over 250 BPM for any rhythm, the chances that the complexes are being conducted through an accessory pathway increase. (Any rates over 200 BPM in atrial fibrillation should raise the same suspicion.) Normally, the AV node would never allow these rapid rates to be conducted but would interject some sort of AV block to slow the ventricles down. The rapid rates have to be going through some other pathway that does not have an intrinsic physiologic block. That other pathway is typically an accessory pathway. Rates over 250 BPM have been associated with the presence of an accessory pathway in about 85% of the cases. At rates of about 300 BPM, the chances of conduction through an accessory pathway are around 97%. To put this all together, Final Test 1: ECG-17 is an example of a very rapid atrial fibrillation being conducted through an accessory pathway at a rate of 300 BPM.
Final Test 1: ECG-18
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: Atrial: 70 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: Yes |
|
|
P:QRS ratio: See discussion below |
Rhythm: Third-degree AV block |
Discussion:
Final Test 1: ECG-18 shows a PR interval that is progressively getting shorter in front of each QRS complex. Wenckebach has progressively widening PR intervals, so that is not the answer. If you notice, there is another small positive deflection between the QRS complexes. Using your calipers, you see that these small deflections map out to be P waves. In addition, the P waves have no correlation or influence whatsoever over the QRS complexes. The QRS complexes are wider than 0.12 seconds and very slow, at about 37 BPM. This is an example of a third-degree AV block with both an underlying sinus rhythm controlling the atria and a ventricular escape rhythm controlling the ventricles.
The blue arrow represents a change in the morphology, and timing, of the P waves after this point. This morphologic and timing shift is due to another ectopic atrial pacemaker picking up the pacemaking function of the atria due to its faster intrinsic rate. This new and faster rate is represented by the red dots at the bottom of the strip.
Final Test 1: ECG-19

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 80 BPM |
PR intervals: Prolonged |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus rhythm with a first-degree AV block |
Discussion:
Final Test 1: ECG-19 shows a sinus rhythm with an obvious P wave occurring before each QRS complex. The P waves are tall, but otherwise normal, and the waves are positive in lead II. The PR intervals are constant but very prolonged at 0.34 seconds. Final diagnosis: Sinus rhythm with a first-degree AV block.
Final Test 1: ECG-20

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 332 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: See discussion below |
|
P waves: None, F waves are present Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 2:1 |
Rhythm: Atrial flutter |
Discussion:
Final Test 1: ECG-20 shows a rapid tachycardia with a ventricular response of 166 BPM. We have taken the liberty of graphically removing the QRS complexes from the strip, so that you can clearly see the underlying the saw-tooth pattern of the F or flutter waves (see pink strip). You should get into the habit of mentally “cleaning up” the strip whenever atrial flutter is suspected. It is a mental exercise that is easy to do, and you will be able to continuously do it during your clinical career.
Are the QRS complexes wide or narrow? It is really difficult to tell on this strip. Because the F:QRS ratio is 2:1, there is a fusion between the F waves from the atrial flutter and the small voltage QRS complexes, giving the appearance of deep and wide slurred S waves. Additional leads or a full 12-lead ECG will help you answer the question about the width of the ventricular complexes. These QRS complexes were indeed narrow in the other leads.
Final Test 1: ECG-21

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 175 BPM |
PR intervals: Small RP interval |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Pseudo-S wave present Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: AVNRT |
Discussion:
In Final Test 1: ECG-21, the presence of a rapid narrow-complex tachycardia with obvious pseudo-S waves in lead II should make you immediately think of AVNRT. Remember, both the pseudo-S and the pseudo-R’ waves are caused by the retrograde P wave occurring almost immediately after the QRS complex. (Pseudo-R’ waves would be visible in lead V1.)
Final Test 1: ECG-22
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 61 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Inverted Axis: Abnormal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Ectopic atrial rhythm |
Discussion:
Final Test 1: ECG-22 shows inverted P waves with normal PR intervals right before each QRS complex. In general, inverted P waves can be due to either ectopic atrial pacemakers from the lower part of the right atria or junctional pacemakers. Recall that the deciding factor between choosing from these two possibilities was the width of the PR interval. Normal or prolonged PR intervals are associated with ectopic atrial pacemakers. Short PR intervals are associated with junctional pacemakers. Since our patient has normal PR intervals, the rhythm is consistent with an ectopic atrial rhythm. The overall rate of the rhythm is 61 BPM, which makes the final diagnosis an ectopic atrial rhythm.
Final Test 1: ECG-23

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 260 to 280 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: Yes |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Polymorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-23 shows a wide-complex tachycardia with constantly changing morphology. The rhythm is irregularly irregular and has an undulating pattern with both amplitude and polarity changes. These are the classic attributes for polymorphic VTach and torsade de pointes. The final diagnosis depends on the presence of the QT interval when the patient is in sinus rhythm and/or the clinical correlation. Polymorphic VTach is associated with normal QT intervals and is strongly associated with myocardial infarctions. Torsade de pointes is associated with prolonged QT intervals and is caused by various clinical conditions (see page 539).
Final Test 1: ECG-24

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 50 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 4:3 then 3:2 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
Final Test 1: ECG-24 has all of the earmarks of a Mobitz I second-degree AV block. There is a progressive lengthening of the PR interval from 0.22 seconds to 0.31 seconds to 0.36 seconds, leading up to a dropped beat. The R-R interval decreases, as would be typically expected, from 0.88 seconds to 0.84 seconds. The conduction ratio of the two visible groups varies from 4:3 for the first group, to 3:2 for the second group. Note that the shortest PR interval is borderline prolonged at 0.20 seconds. (Yes, you can have both first-degree and either second-degree AV block occurring simultaneously in the same patient.)
Final Test 1: ECG-25

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 90 BPM |
PR intervals: Multiple |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Multiple Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Wandering atrial pacemaker |
Discussion:
In Final Test 1: ECG-25, there are nine complexes in a 6-second strip. This makes the overall rate of the rhythm around 90 BPM. The rhythm is irregularly irregular with at least three P-wave morphologies each with a different PR interval. This is a wandering atrial pacemaker. There are two buried P waves scattered throughout the strip (see blue asterisks). The blue arrows point to two QRS complexes that are aberrantly conducted. These two complexes are aberrantly conducted because the early occurring, buried P waves of these two complexes arrived at the right bundle branch before it was ready to receive it. This is an example of Ashman’s phenomenon (a long R-R interval followed by a short R-R interval; the QRS complex at the end of the short R-R interval tends to be aberrantly conducted). Ashman’s phenomenon is typically found in atrial fibrillation, MAT, and occasionally, rapid sections of WAP.
Final Test 1: ECG-26

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 110 BPM |
PR intervals: Normal, except in events |
|
Regularity: Regularly irregular |
QRS width: Normal, except in events |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus tachycardia with multiple PACs and a PJC |
Discussion:
Final Test 1: ECG-26 is full of small pathologic events that require a keen eye and a good set of calipers. There are two obviously different complexes in the strip: the fourth and ninth complexes. Are they PVCs? The answer is no—they are aberrantly conducted PACs. Notice the morphology of the T wave immediately before those two wide QRS complexes. They are taller and wider than the others on the strip because of prematurely occurring, buried P waves. The QRS complexes of these PACs are being aberrantly conducted because the early arrival of the PAC reached a right bundle that was not ready to normally conduct them. The pauses of these two PACs are noncompensatory pauses that reset the underlying sinus rate (see red dots and green dots).
If you were really observant, you would have noticed the complex to which the blue arrow is pointing. What is that complex? It is narrow, starts off in the same direction as the normally conducted QRS complexes, and is a bit premature. This is a PJC. Notice that the PJC arrives just a tiny bit before expected and gives the illusion that it is associated with a short PR interval. Why isn’t this a PAC with its own PR interval? Well, the P wave is not premature and has the same morphology as the surrounding normal P waves. Remember to always look at every part of the strip. Sometimes it is the most obscure change that provides a wealth of information.
Final Test 1: ECG-27

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: Atrial: 100 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: Yes |
|
|
P:QRS ratio: Not applicable |
Rhythm: Third-degree AV block |
Discussion:
Final Test 1: ECG-27 shows an obvious AV block. The atrial rate is 100 BPM, making the atrial rhythm either a sinus tachycardia or an atrial tachycardia. The ventricular rate of 20 BPM makes the ventricular response a ventricular escape rhythm. On first glance, the PR intervals right before the ventricular complexes appear to be the same. That, however, is not the case. The first PR interval measures 0.23 seconds, while the second one measures 0.18. This is not an advanced second-degree AV block, but a complete or third-degree AV block.
Final Test 1: ECG-28

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 200 BPM |
PR intervals: See discussion below |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present, intermittent Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: Monomorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-28 is a classic example of monomorphic ventricular tachycardia. First of all, it is a wide-complex tachycardia clipping along at about 200 BPM. There is one normally conducted capture beat (labeled “C”) and many fusion beats (labeled “F”), which are indirect evidence of AV dissociation. The P waves map out for a short time (see blue dots), but it is impossible to map them out any farther.
You have read many times during this text that monomorphic VTach is a regular rhythm. At first glance, this strip appears to have its cadence or timing disrupted by the capture and fusion beats, but take a look at the red stars above the strip. The timing of the red stars shows that the underlying ventricular reentry loop causing the tachycardia is not interrupted by the capture or fusion beats. In other words, the cadence of the rhythm is never reset. It remains as regular as clockwork.
Final Test 1: ECG-29

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 51 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Junctional rhythm |
Discussion:
In Final Test 1: ECG-29, the patient has a narrow-complex rhythm at a rate of 51 BPM. There are no visible P waves and the rhythm is regular. This is a junctional rhythm. Two things to mention: First of all, don’t let a wavy baseline fool you into thinking that the rhythm is an atrial fibrillation. Look at the regularity of the rhythm. The only time that atrial fibrillation can be regular is if there is complete AV block with a junctional or ventricular escape. The second thing to mention is that this person appears to have some serious ST-segment elevation. You should not use a rhythm strip to make any ST-segment evaluations, so get a full 12-lead ECG. This person is probably having a big MI.
Final Test 1: ECG-30

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 95 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Atrial fibrillation |
Discussion:
Final Test 1: ECG-30 shows an irregularly irregular rhythm with a very coarse baseline. This is an atrial fibrillation. It is important in these patients, however, to obtain multiple leads to make sure that P waves are not hidden by the coarseness of the baseline.
Final Test 1: ECG-31

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 300 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: F waves Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 2:1 |
Rhythm: Atrial flutter |
Discussion:
In Final Test 1: ECG-31, the patient has a ventricular rate of 150 BPM. This figure should trigger in your mind an instant search for the flutter waves of atrial flutter. If you remove the QRS complexes from the strip, you end up with an obvious saw-tooth pattern at a rate of 300 BPM consistent with atrial flutter (see pink strip).
Final Test 1: ECG-32

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 200 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Pseudo-S wave Morphology: Inverted Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: AVNRT |
Discussion:
Final Test 1: ECG-32 shows a narrow-complex tachycardia at a rate of about 200 BPM. There is a small negative deflection at the end of the QRS complexes which could represent a pseudo-S wave. The presumptive diagnosis is AVNRT. Electrical alternans, a common occurrence in tachycardias, is present. Clinical correlation and a full 12-lead ECG during and after the tachycardia will help confirm AVNRT as the final diagnosis.
Final Test 1: ECG-33

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 300 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 2:1 |
Rhythm: Atrial flutter |
Discussion:
First of all, notice that Final Test 1: ECG-33 was obtained from lead V1. There is an obvious P wave before each QRS complex, but there is another one right after the QRS complex that is not so obvious (see blue arrow). The atrial rate is 300 BPM and the conduction ratio is 2:1, making the ventricular rate 150 BPM. There’s that number again . . . Once again, when you see a rate of around 150 BPM, think atrial flutter. To confirm your diagnosis, you should obtain a full 12-lead ECG or multiple leads. Many times, however, you will not see anything in lead II, and the only lead where you can see any atrial activity is lead V1. As a reminder, typically, the best lead to see atrial activity is lead V1.
Final Test 1: ECG-34

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 128 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Pseudo-S Morphology: Inverted Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Junctional tachycardia |
Discussion:
Final Test 1: ECG-34 shows a rapid narrow-complex tachycardia with a pseudo-S wave (see blue arrow). The rate of 128 BPM is still within the range for a junctional tachycardia. Remember, by tradition, rates above 140 BPM are labeled AVNRT.
Final Test 1: ECG-35

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: See discussion below |
PR intervals: See discussion below |
|
Regularity: See discussion below |
QRS width: See discussion below |
|
P waves: See discussion below Morphology: See discussion below Axis: See discussion below |
Grouping: See discussion below |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
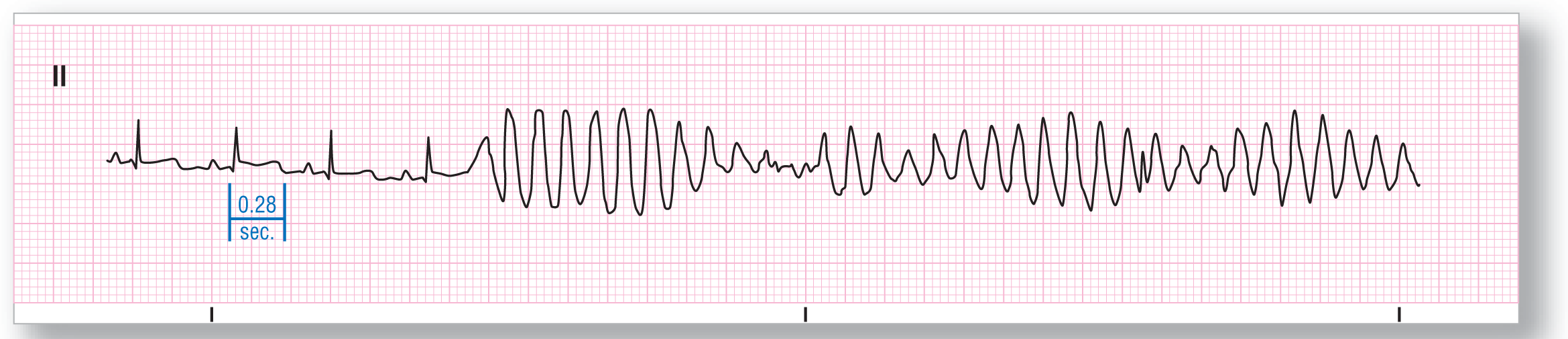
Rhythm: Sinus rhythm becoming torsade de pointes |
Discussion:
The start of Final Test 1: ECG-35 shows a sinus rhythm with a first-degree AV block and a QT interval at 0.46 seconds. The rate of the sinus rhythm is about 84 BPM, making the QT interval prolonged. The patient then has some event, most likely a PVC, which triggers off a run of torsade de pointes at a rate of between 240 and 280 BPM. The initial PVC is not clearly different morphologically from the subsequent ventricular complexes in this lead, but it did arrive during the relative refractory period of the ST-T wave area. The undulations and polarity shifts of the torsade de pointes are evident in the middle and latter parts of the strip.
Final Test 1: ECG-36

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 110 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 4:3 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
Final Test 1: ECG-36 shows a series of groupings that are conducted at a 4:3 ratio. The PR intervals are progressing between each complex in a group as the R-R intervals are decreasing. The final P wave in each group is not conducted. The longest PR interval in each group is the one before the dropped beat and the shortest is the one immediately after the pause. These are the hallmarks for a Wenckebach or Mobitz I second-degree AV block.
Final Test 1: ECG-37

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 280 BPM |
PR intervals: See discussion below |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 2:1 |
Rhythm: Focal atrial tachycardia with block |
Discussion:
Final Test 1: ECG-37 can be quite deceptive at first glance. The reason for this is that the height of the R waves is very short and they are almost the same size as the P waves that surround it (the blue arrow points to a low-amplitude QRS complex). There is 2:1 conduction throughout. The rates are consistent with atrial flutter but there is an isoelectric segment between the P waves. The presence of this isoelectric segment makes this rhythm a focal atrial tachycardia with block despite the rate inconsistency.
Final Test 1: ECG-38

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 300 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: F waves Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 5:1 |
Rhythm: Atrial flutter |
Discussion:
The underlying saw-tooth pattern of the F waves is evident on Final Test 1: ECG-38. The conduction ratio of this rhythm is 5:1. An easy way to figure out the ratio is to count the number of negative F waves clearly visible between the QRS complexes and then add one to that figure. You add one because there is always one F wave buried within the previous QRS complex. In this example, we have four easily identifiable F waves, so there has to be one more F wave buried in the previous QRS complex, giving you a 5:1 conduction ratio.
Final Test 1: ECG-39

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 60 BPM |
PR intervals: None |
|
Regularity: Regular with event |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Junctional rhythm with a PJC |
Discussion:
Final Test 1: ECG-39 shows a wide-complex rhythm at about 60 BPM. There are no visible P waves anywhere on the strip. The small positive deflections at the end of the T waves are U waves, not P waves. At this point, our list of possibilities includes an accelerated idioventricular rhythm or a junctional rhythm in a patient with aberrant conduction or a preexisting bundle branch block.
The blue arrow is pointing to a QRS complex that is narrow and arrives prematurely. Could this be a PJC? Yes, it could be. Actually, that PJC is the key to the diagnosis. Notice that the first deflection of the wide complexes and the PJC are identical. Both are positive and have a rapid ascent. You would not expect that similarity to occur if the wide rhythm originated from a ventricular origin. In a ventricular rhythm, you would expect to see a wider onset and a deflection opposite to one traveling down the His-Purkinje system. Those inconsistencies point us in the direction of a junctional rhythm.
So, if we have a junctional rhythm and then have a PJC occurring within it, shouldn’t the PJC be expected to have more aberrancy since it is premature? Yes, you would expect it to be wider and more bizarre. Why is this PJC narrower? We have no clue. Sometimes the depolarization wave just gets lucky and hits at just the right moment to transmit normally throughout the rest of the conduction system.
Final Test 1: ECG-40
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 102 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: Monomorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-40 is a wide-complex rhythm. In addition, it has a rate of 102 BPM, making it a tachycardia. With just those two bits of information, you should be thinking VTach initially. Now, let’s prove or disprove it. The first thing to look for is evidence of AV dissociation. Do you see anything that looks like a P wave? Take a look at the wave under the red star. This is an obvious P wave. Can you see any other deflections near that area that resembles another P wave? If you look at the area under the asterisk, there appears to be another P wave peeking out after the T wave of the previous complex. Now, take your calipers and measure out that distance. Map that distance back and forth across the strip and you will notice irregularities in the strip at those exact sites (see thin blue arrows). These are buried P waves, and this is direct proof of AV dissociation. This rhythm, therefore, is ventricular tachycardia.
Final Test 1: ECG-41

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 110 BPM |
PR intervals: Variable |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal, but variable Axis: Variable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Multifocal atrial tachycardia |
Discussion:
Final Test 1: ECG-41 shows an irregularly irregular rhythm with P waves. There are two main possibilities for this: multifocal atrial tachycardia and wandering atrial pacemaker. The rate on this strip is about 110 BPM, making multifocal atrial tachycardia the most probable diagnosis. Now, to confirm our diagnosis. Are there at least three different P-wave morphologies, each with their own distinctive PR interval? Yes. We have confirmed MAT as the final diagnosis.
Final Test 1: ECG-42
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Not applicable |
PR intervals: None |
|
Regularity: None |
QRS width: None |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
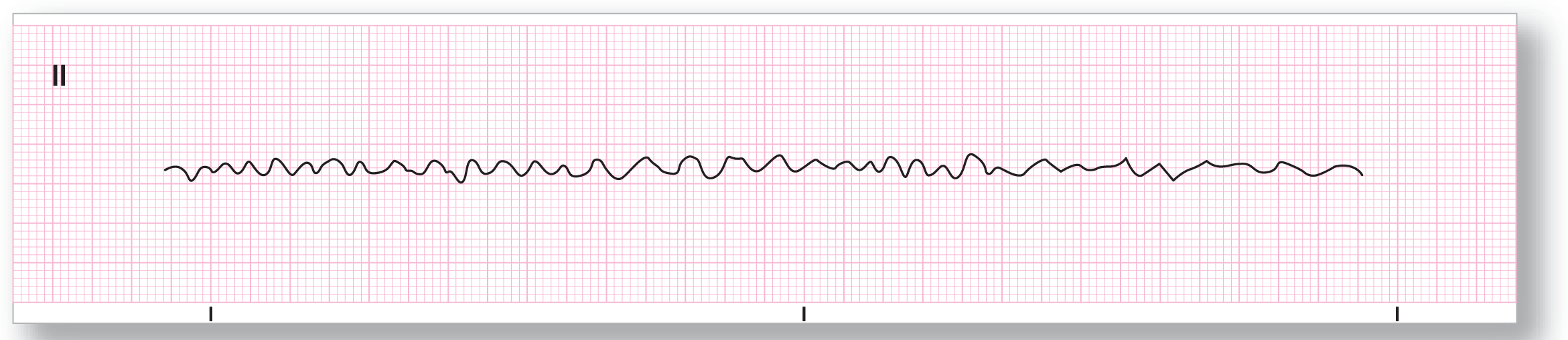
Rhythm: Ventricular fibrillation |
Discussion:
Final Test 1: ECG-42 shows a completely chaotic ventricular response. This is typical of only two possibilities: Ventricular fibrillation and artifact. Take a look at the patient. If he is unconscious or unresponsive, it is Vfib. If he is talking and having a good time, it is artifact. One more important clinical point: Make sure that you quickly change leads on the monitor anyway to make sure that artifact is not hiding some other potentially lethal arrhythmia.
Final Test 1: ECG-43

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 74 BPM |
PR intervals: Prolonged |
|
Regularity: Regular with frequent events |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus rhythm with a first-degree AV block with frequent PVCs |
Discussion:
Final Test 1: ECG-43 shows a patient with an underlying sinus rhythm with a first-degree AV block due to the prolonged PR interval. The patient has two PVCs (see complexes with the red stars) that are associated with fully compensatory pauses. The blue arrow is pointing to the normally occurring P wave that was starting when the second PVC fired. The result is that the P wave was buried at the start of the PVC, thereby altering its morphology slightly. The two PVCs are probably unifocal despite the different coupling intervals (the distance from the previous complex to the start of the PVC).
Final Test 1: ECG-44

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 215 BPM |
PR intervals: See discussion below |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: See discussion below Morphology: See discussion below Axis: See discussion below |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: See discussion below |
Rhythm: AVRT |
Discussion:
Final Test 1: ECG-44 is a diagnostic dilemma. It is a wide-complex tachycardia at about 215 BPM. The QRS complexes are a little narrower than you would expect to see for a ventricular origin, but VTach is still in the differential. There is a deflection at the bottom of the S wave, which either could be a morphologic feature of the aberrancy or could represent an inverted P wave with a long RP interval. Based on this one strip, you can’t narrow it down any further between VTach, AVNRT with aberrancy, or antidromic AVRT with any great degree of certainty. Remember to never gamble with a patient’s life; in other words, NEVER GUESS!
A full 12-lead ECG was able to move VTach down our list from number 1 to number 3. The possible inverted P wave was visible as a separate structure in almost every lead, making you lean toward an antidromic AVRT because of the longer RP interval. The clinical history, if available, could also be a major decision point.
The moral of this strip is that sometimes you can’t narrow down a rhythm completely. In those cases, you need to use all available means to arrive at a feasible conclusion. In this case, the patient needed to be treated as if he had VTach, with a strong suspicion that there may be an accessory tract involved and that it could actually be an AVRT. If the patient is unstable, direct cardioversion or defibrillation is indicated in either case. If the patient is stable, obtain a history and use drugs that work on both possibilities, like IV amiodarone (if there are no contraindications).
Final Test 1: ECG 45
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 110 BPM at onset |
PR intervals: Normal, at onset |
|
Regularity: See discussion below |
QRS width: Normal, at onset |
|
P waves: Present at onset Morphology: Normal at onset Axis: Normal at onset |
Grouping: Yes, at the end of the strip |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 at onset |
Rhythm: Sinus tachycardia becoming torsade de pointes |
Discussion:
Final Test 1: ECG-45 shows a sinus tachycardia that changes into a run of torsade de pointes. The torsade de pointes is triggered by an R-on-T PVC. The rhythm cannot be called polymorphic VTach because the sinus tachycardia has a QT interval of 0.28 seconds, which is prolonged for a rate of 110 BPM. Notice the grouping quality of the torsade de pointes and the constant fluctuation of the morphology and the polarity of the QRS complexes, giving the rhythm an undulating or wavelike quality.
Final Test 1: ECG-46

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 70 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 3:2 |
Rhythm: Mobitz I second-degree AV block |
Discussion:
Final Test 1: ECG-46 is a very deceptive strip. At first glance, the rhythm appears to be a simple third-degree AV block. However, close observation and some measurements quickly change this initial evaluation. To start off, is the rhythm regular? No, it is regularly irregular. That fact just about completely rules out third-degree AV block because all of the possible escape rhythms depolarizing the ventricles, either junctional or ventricular, are always regular. Is there any grouping? Yes, but it is difficult to spot. There are two different R-R intervals throughout the strip. One R-R interval is 0.84 seconds and the other is 1.08 seconds and they both alternate throughout the strip.
At this point, let’s turn our attention to the PR intervals. There are two measurable PR intervals; one is 0.27 seconds and the other is 0.42 seconds. Now, let’s go back and take a look at the groups we isolated in the previous paragraph. First there is a P wave with a PR interval of 0.27. Then, there is a PR interval of 0.42 seconds. Then, then there is a nonconducted P wave. This is a recurring pattern in each group, clinching the diagnosis of Wenckebach or Mobitz I second-degree AV block.
What makes this rhythm strip difficult to interpret is the small difference between the two R-R intervals. Usually, there is a larger difference between the groupings, reflecting the dropped beat. However, just because the groups are closer together than expected, it is still a Wenckebach. As mentioned earlier, a third-degree AV block would give you an escape rhythm of some sort that would have to be regular. When you are approaching a rhythm strip, it is essential to form an initial impression of the rhythm. However, you now have to go and confirm your diagnosis. Checking the regularity and the intervals is a critical step in this confirmation process. Initial impressions are right in most cases, but as this strip exemplifies, they can also be wrong.
Final Test 1: ECG-47

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 62 BPM |
PR intervals: See discussion below |
|
Regularity: See discussion below |
QRS width: Normal |
|
P waves: Present Morphology: See discussion below Axis: See discussion below |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Ectopic atrial rhythm (see discussion below for full details) |
Discussion:
Final Test 1: ECG-47 shows a transition between two different regular rhythms. The first is an ectopic atrial rhythm at about 62 BPM. Note the inverted P waves with normal PR intervals, which are consistent with an ectopic atrial pacemaker, which occur at the front end of the strip. The P wave highlighted by the blue arrow, however, comes after a longer pause than the previous R-R intervals. In addition, the P wave changes to upright and it has a different PR interval. This P wave either can be an atrial escape complex or it can signify a change to a sinus rhythm, or even a different ectopic atrial rhythm (caused by a different atrial pacemaker). Statistically, a new rhythm is more likely than an atrial escape complex, but a longer strip is needed to verify the change.
Final Test 1: ECG-48

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 220–260 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: See discussion below |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Polymorphic ventricular tachycardia or torsade de pointes |
Discussion:
Final Test 1: ECG-48 shows the typical undulating pattern either of polymorphic VTach or of torsade de pointes. Which one of these is the final diagnosis depends on the underlying QT interval of the patient when in a sinus rhythm. Note the continuous change in the size, morphology, and polarity of the QRS complexes in this strip. The undulating pattern caused by the changes gives the strip an appearance of having grouping.
Final Test 1: ECG-49

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Less than 10 BPM |
PR intervals: None |
|
Regularity: See discussion below |
QRS width: None |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Agonal rhythm |
Discussion:
Final Test 1: ECG-49 shows an agonal rhythm. Notice the width of the QRS complexes and the totally abnormal and bizarre appearance of the one complex. Agonal rhythms are terminal events and are a close precursor to complete asystole. Most of the time, the ventricular depolarizations are strictly an electrical event and there is no resultant mechanical contraction.
Final Test 1: ECG-50

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 50 BPM |
PR intervals: None (RP interval) |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: Present Morphology: Inverted Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Accelerated idioventricular rhythm |
Discussion:
Final Test 1: ECG-50 shows a wide, bizarre-looking rhythm, which is obviously ventricular in origin. There are no visible P waves before the QRS complexes, but there is an inverted P wave near the top of the T wave (see blue arrow). Note the very prolonged RP interval, which is commonly seen in ventricular rhythms due to the retrogradely conducted P waves.
Final Test 1: ECG-51

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 80 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Ventricular paced rhythm |
Discussion:
Final Test 1: ECG-51 shows a sharp deflection immediately before each ventricular complex that is caused by an artificial pacer. The pacer appears to be completely ignoring the underlying atrial rhythm (see blue dots). As there is no atrial sensing or pacing evident on this strip, the paced rhythm is consistent with a VVI pacer.
Final Test 1: ECG-52
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 51 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Inverted Axis: Abnormal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Third-degree AV block |
Discussion:
In Final Test 1: ECG-52, the ventricular response is regular and about 61 BPM. The atrial rhythm is actually slower at 51 BPM. There are some inverted P waves, but there is no association at all between the P waves and the QRS complexes. Notice the morphologic changes that develop when the inverted P waves fuse with the QRS complexes, ST segments, and T waves. This is a third-degree AV block with a sinus bradycardic atrial rhythm and an accelerated junctional escape rhythm.
Final Test 1: ECG-53

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: Atrial: 90 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Accelerated idioventricular rhythm |
Discussion:
Final Test 1: ECG-53 shows a wide-complex rhythm with a ventricular rate of about 90 BPM. The start of the strip shows some wide, bizarre complexes that are obviously of ventricular origin. Then there is a narrow capture beat with a P wave before it (see complex labeled “C”). Followed by several fusion complexes (see complex labeled “F”). These are indirect evidence for the presence of AV dissociation. The P waves map throughout the entire strip and cause some fusion with the ventricular complexes. For example, take a look at the area highlighted by the blue arrow. This area is slurred upward because of a fusion between the P wave and the ventricular complex. This is indirect evidence of AV dissociation.
Because the rate is less than 100 BPM, this is not a ventricular tachycardia. Instead, the slower rate makes this rhythm an accelerated idioventricular rhythm. Remember, idioventricular, accelerated idioventricular, and VTach can all have AV dissociation.
Final Test 1: ECG-54

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 59 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Biphasic Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Third-degree AV block |
Discussion:
Final Test 1: ECG-54 shows a complete or third-degree AV block with a sinus bradycardia and a very slow junctional escape rhythm. The blue arrows point to buried P waves inside of the QRS complex.
Final Test 1: ECG-55

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 66 BPM |
PR intervals: None |
|
Regularity: Regular with an event |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Accelerated junctional rhythm with a PVC |
Discussion:
Final Test 1: ECG-55 shows a narrow-complex rhythm at about 66 BPM. There are no visible P waves on the strip. There could be a pseudo-S wave pattern at the end of the QRS complex, but it could also represent part of the normal morphology for the QRS complex in that lead. There is one PVC (see blue arrow) near the start of the strip. A full 12-lead ECG will help you decide whether or not there is a pseudo-S wave. In either case, verification of the pseudo-S wave is not necessary for you to make the diagnosis of an accelerated junctional rhythm with a PVC.
Final Test 1: ECG-56

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 270 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: AVRT |
Discussion:
Final Test 1: ECG-56 shows a very, very rapid narrow-complex tachycardia with no visible P waves. The rhythm is very regular. There is some electrical alternans noted, which would be expected in many tachycardias, especially at this rate. The rhythm is too fast for an AVNRT. The only other logical possibility is an orthodromic AVRT. Clinical correlation and a full 12-lead ECG once the patient is stable would be highly recommended. Be careful treating this patient and keep in mind that there is a tremendously high probability that you are dealing with a patient who has an accessory pathway.
Final Test 1: ECG-57
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
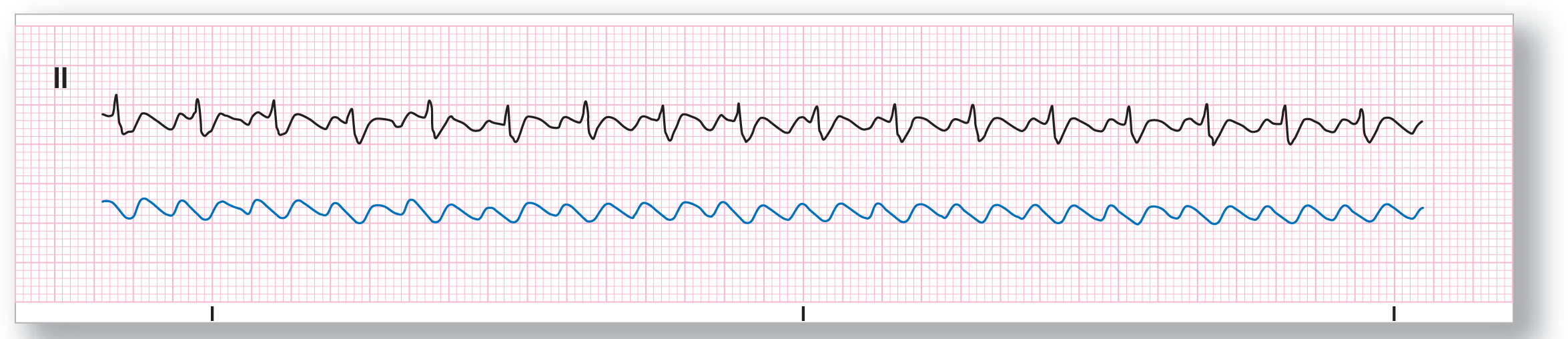
Rate: Atrial: 300 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: See discussion below |
|
P waves: F waves Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 2:1 |
Rhythm: Atrial flutter |
Discussion:
In Final Test 1: ECG-57, the ventricular rate of 150 BPM should immediately make you think of an atrial flutter. Can we rule this possibility in? Yes. Take a look at the strip and mentally remove the QRS complexes . . . the result is the strip in blue above. There is an obvious saw-tooth pattern on this modified strip. The saw-tooth pattern, however, is a bit more camouflaged in the original strip because the QRS complexes appear to be wide. We say appear to be wide, because we cannot be sure if this is an illusion caused by a fusion of the F wave with the overlying QRS in this lead. A full 12-lead ECG or looking at some other leads will help to clarify this issue. In this case, the 12-lead ECG showed very clear evidence that the QRS complexes were narrow, and the illusion we mentioned earlier was actually occurring.
Final Test 1: ECG-58

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 90 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Monomorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-58 is another tough one. The important thing is your initial logic. It is a wide-complex tachycardia; therefore VTach should be number 1 on your differential diagnosis list. The last two complexes hold the initial key to proving your original impression because they have obvious P waves right before the QRS complexes. Mapping this distance with your calipers, and then walking that distance over the rest of the strip, brings up irregularities in the strip, which are caused by buried P waves. This is direct evidence of AV dissociation. A wide-complex tachycardia with AV dissociation is VTach for all intents and purposes.
It is unclear whether the complexes marked by the red stars are capture complexes in a patient with an underlying bundle branch block or whether they are fusion complexes. Statistically, they should be fusion complexes because that is the most common possibility. However, you will need to obtain some old strips to be absolutely sure of this before making that call. The complex labeled with the “F” represents an obvious fusion complex.
Final Test 1: ECG-59

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: None |
PR intervals: None |
|
Regularity: None |
QRS width: None |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Ventricular fibrillation |
Discussion:
Final Test 1: ECG-59 shows a completely chaotic ventricular response. The only possibility is ventricular fibrillation. Once again, clinical correlation is required to rule out artifact.
Final Test 1: ECG-60
From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 80 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: Yes |
|
Dropped beats: Yes |
|
|
P:QRS ratio: 5:4 |
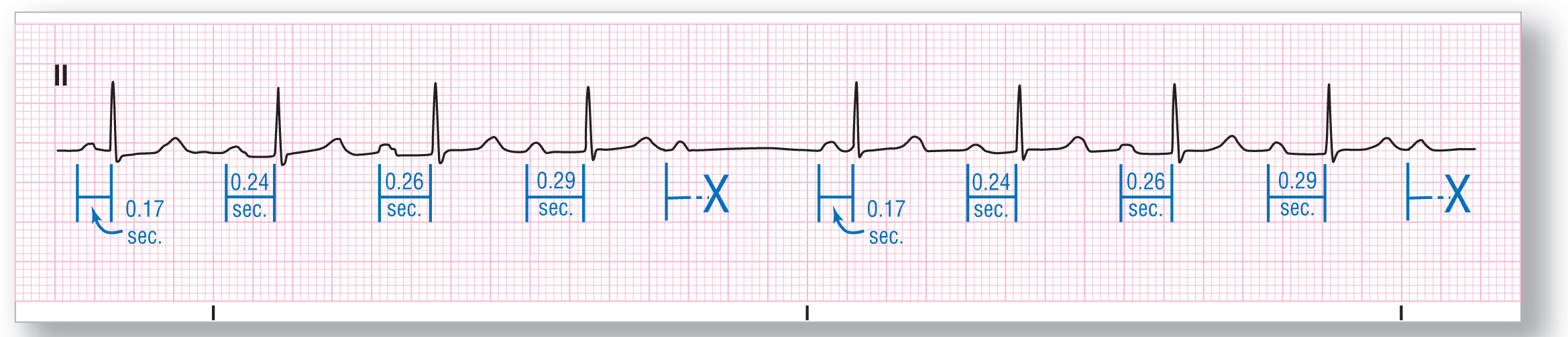
Rhythm: Mobitz I second-degree AV block |
Discussion:
Final Test 1: ECG-60 shows some obvious grouping of five atrial and four ventricular complexes and then a dropped beat. The P waves are all morphologically similar, but the PR intervals show the typical lengthening pattern seen in Wenckebach or Mobitz I second-degree AV block. Note that the widest incremental change in the PR intervals occurs between the first and second complexes. In addition, the PR interval immediately following the pause is the shortest, and the one before the pause is the longest. Finally, the R-R intervals shorten along the grouping, as would be expected. Final diagnosis is Mobitz I second-degree AV block.
Final Test 1: ECG-61

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 33 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Junctional rhythm |
Discussion:
Final Test 1: ECG-61 shows a very slow junctional rhythm. Junctional rhythm usually has rates between 40 and < 60 BPM, but can be slower at times. This is one of those times. It is important to try to figure out why this patient’s rate is so slow. Clinical correlation is needed to see if there is drug use or toxicity, a CNS event, ischemia, or an electrolyte problem, among other things, as the cause of the slower rate.
Final Test 1: ECG-62

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 44 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus bradycardia |
Discussion:
Final Test 1: ECG-62 shows your typical sinus bradycardia. Notice the P wave in front of each QRS. The P waves are the same morphology and have the same PR intervals. The QRS complexes are narrow, and there are no major abnormalities or irregularities noted anywhere else along the strip.
Final Test 1: ECG-63

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: Atrial: 90 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Ventriculophasic AV dissociation |
Discussion:
It is easy to spot the AV block in Final Test 1: ECG-63, but note that this is not a typical third-degree AV block. The ventricular rate is regular, narrow, and consistent with a junctional escape rhythm. The atrial rhythm is another matter. At the start of the strip there appear to be two different P-P intervals: One P-P interval occurs when there is a QRS complex falling between the two P waves. The other P-P interval occurs when there is no QRS complex falling between the two P waves. This part of the strip is a classic example of what is known as a ventriculophasic AV dissociation (see page 442 for further details).
The exact P-P intervals start to fall apart in the middle of the strip for some reason. The two P-P intervals labeled with the red stars are exactly even because the P wave falls right in the middle of the QRS complex (see first blue arrow). The green arrow also points to a buried P wave, but this time, the QRS complex does exert some influence on the underlying P-P interval, causing it to narrow slightly. Notice that the ventriculophasic influence remains throughout the strip, but is less classic toward the latter half of the strip.
Final Test 1: ECG-64

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 280 BPM |
PR intervals: Not applicable |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: F waves Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: 4:1 |
Rhythm: Atrial flutter |
Discussion:
Final Test 1: ECG-64 shows the very obvious saw-tooth pattern of atrial flutter along the baseline. The ratio of conduction is 4:1 with an atrial rate of 280 BPM and a ventricular response of 70 BPM.
Final Test 1: ECG-65

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 125 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: Not applicable |
Rhythm: Accelerated idioventricular rhythm |
Discussion:
Final Test 1: ECG-65 shows an underlying sinus rhythm that is broken up by a PVC and a PAC. The PVC and the PAC are both associated with compensatory pauses, which means that the underlying atrial cadence is not broken by the two events. In other words, the sinus node is not reset by either the PVC or the PAC. The PAC is associated with a buried P wave.
Final Test 1: ECG-66

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 85 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular with events |
QRS width: Wide |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus rhythm with a PVC and a PAC |
Discussion:
Final Test 1: ECG-66 shows a wide-complex rhythm that is broken up by one narrow complex (see red starred complex). This is a capture beat and indirect evidence of AV dissociation. When we look at the rest of the strip, we notice some P waves scattered throughout. These P waves map out at a tachycardic rate of 125 BPM (see blue dots). One of the P waves falls right after the QRS complex of the capture beat (see small blue arrow). Due to the ventricular rate of 74 BPM, this rhythm is an accelerated idioventricular rhythm.
Notice anything else unusual about the strip? The strip was recorded at half-standard (see calibration mark at the end of the strip). This means that all of the waves are actually twice as tall as they appear on this strip. These are some really big waves!
Final Test 1: ECG-67

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 135 BPM |
PR intervals: Variable |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Variable Axis: Variable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Multifocal atrial tachycardia |
Discussion:
Final Test 1: ECG-67 shows a rapid narrow-complex tachycardia that is irregularly irregular. Are there P waves? Yes. Then it is probably MAT. Are there at least three different P-wave morphologies each with their own PR interval? Yes. Then it is definitely MAT.
Final Test 1: ECG-68

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 220 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Atrial fibrillation |
Discussion:
Final Test 1: ECG-68 shows a wide-complex tachycardia. But, it is an irregularly irregular wide-complex tachycardia. This is atrial fibrillation. Because of the very fast rates and unusual morphology, you are dealing with antegrade conduction through an accessory pathway. (As a rule, you need to think about accessory pathways in atrial fibrillation when the rate is greater than 200 BPM.) Don’t be fooled into thinking that this is VTach or ventricular flutter! Those two rhythms are usually regular.
Final Test 1: ECG-69

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 135 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular |
QRS width: Normal |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Sinus tachycardia |
Discussion:
Don’t let the size of the QRS complexes in Final Test 1: ECG-69 fool you. This is a rapid, regular narrow-complex tachycardia with P waves before each of the QRS complexes. The P waves are all identical and so are the PR intervals. This is a sinus tachycardia.
Final Test 1: ECG-70

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: Atrial: 280 BPM |
PR intervals: Not applicable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: F waves Morphology: Not applicable Axis: Not applicable |
Grouping: None |
|
Dropped beats: None |
|
|
F:QRS ratio: Variable |
Rhythm: Atrial flutter with variable block |
Discussion:
Final Test 1: ECG-70 shows a narrow-complex tachycardia with a ventricular response of about 125 BPM. The rhythm is regularly irregular with one particular R-R interval recurring frequently throughout most of the strip. Once again, imagine mentally removing the QRS complexes from the rhythm strip. What you would be left with is the pink strip. The saw-tooth pattern of atrial flutter is evident on this strip. This is an atrial flutter with variable block.
Final Test 1: ECG-71

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
Description|
Rate: About 70 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Present Morphology: Variable Axis: Variable |
Grouping: Yes |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Supraventricular bigeminy |
Discussion:
Final Test 1: ECG-71 shows a rhythm that has one complex with a normal upright P wave followed by a complex with an inverted P wave. This causes a grouping pattern to develop, but this time, it is not due to an AV block. This is a rhythm known as a supraventricular bigeminy. It is a bigeminy because every other beat is premature; it is supraventricular because the premature beat is a PAC. If you cannot remember the term supraventricular bigeminy, it is OK to call it sinus rhythm with frequent PACs.
This is usually a stable rhythm as long as the PACs are causing a mechanical contraction. Checking the patient’s pulse for the same pattern as seen on the strip will answer that question. To treat it, find the underlying cause and treat that. It may be too much caffeine, drugs (legal and illegal), anxiety, hypoxemia, and many other causes. A good history, physical exam, and a full 12-lead ECG will usually help you spot the culprit.
Final Test 1: ECG-72

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 55 BPM |
PR intervals: Normal, consistent |
|
Regularity: Regular with an event |
QRS width: Normal, except in event |
|
P waves: Present Morphology: Normal Axis: Normal |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1, except in event |
Rhythm: Sinus bradycardia with a ventricular escape complex |
Discussion:
The event in question on Final Test 1: ECG-72 is obviously a ventricular complex. But, is it a PVC? No. It doesn’t arrive earlier than expected; it arrives later than expected. The ventricular pacemaker fired as a fail-safe mechanism because the sinus node took too long to fire. This is a ventricular escape complex. The underlying rhythm is a sinus bradycardia since the rate is 55 BPM.
Final Test 1: ECG-73

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 90 BPM |
PR intervals: None |
|
Regularity: Irregularly irregular |
QRS width: Normal |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Atrial fibrillation |
Discussion:
Final Test 1: ECG-73 shows an irregularly irregular rhythm with no obvious P waves. The rhythm is an atrial fibrillation. The QRS complexes are narrow and the rate is about 90 BPM.
Final Test 1: ECG-74

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 55 BPM |
PR intervals: Variable |
|
Regularity: Regularly irregular |
QRS width: Normal |
|
P waves: Variable Morphology: Variable Axis: Variable |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: 1:1 |
Rhythm: Wandering atrial pacemaker |
Discussion:
Final Test 1: ECG-74 shows a rhythm where the P waves are slowly transitioning from upright to inverted and then back again in a continuous pattern. This is the hallmark of a wandering atrial pacemaker.
Final Test 1: ECG-75

From Arrhythmia Recognition: The Art of Interpretation, courtesy of Tomas B. Garcia, MD.
|
Rate: About 155 BPM |
PR intervals: None |
|
Regularity: Regular |
QRS width: Wide |
|
P waves: None Morphology: None Axis: None |
Grouping: None |
|
Dropped beats: None |
|
|
P:QRS ratio: None |
Rhythm: Monomorphic ventricular tachycardia |
Discussion:
Final Test 1: ECG-75 shows a wide-complex tachycardia at a rate of 115 BPM. The complexes are regular and have the same morphologic presentation. There is no direct or indirect evidence of AV dissociation present. The differential diagnosis is short for this rhythm. It could either be a monomorphic ventricular tachycardia or a junctional tachycardia in a patient with a preexisting condition that widens the QRS complex. Statistically, the second possibility is less common. So, for all intents and purposes, you can make the call of a monomorphic ventricular tachycardia.
The width of the QRS complexes is also consistent with ventricular complexes. Usually, aberrancy does not present with QRS intervals above 0.14 seconds. A full 12-lead ECG could possibly help you confirm the diagnosis, if you have the time to get one.