
TWINS ARE MY thing! I started this journey specialising in baby sleep routines 20 years ago with newborn twins and, having mostly twins in my care for the first five years, I fast became a specialist in twin routines. Double trouble? No, double the joy! Of course, you do need to plan ahead, be organised and prepared, but with both babies on the same routine, doing everything together at the same time, it is not too different from having one baby; it’s just that everything takes half an hour longer.
Twins can be easier to establish on a routine as they are usually born on the small side so tend to need more sleeping time to grow, which means they will naturally sleep longer at night. Try to take advantage of this: if your babies are under 2.72kg (6lb), then wake them for a night feed, but allow longer stretches of sleep at night, between four and six hours, so that you are teaching them the difference between night and day straight away. Vary the time you wake them so you don’t set their body clocks to naturally wake at a certain time during the night. Once they are over 2.72kg (6lb), wake them only once in the night between 11pm and 2am until they are both gaining weight and are back to their birth weights; only then can you let them wake naturally for the night feed.
Despite being small and often premature, you can introduce a routine for twins from birth. Even premature babies, weighing only around 1.8kg (4lb), are put on to a three- to four-hourly feeding routine in hospital. If your babies are over 2.72kg (6lb) and putting on weight nicely, there is no reason why you cannot start my 7pm to 7am Sleeping Baby Routine with baby-led nights. If you do not feel comfortable with this and wish to wake your twins for a night feed in the first two weeks then, again, vary the waking time so as not to set a pattern of waking during the night.
The reason a routine for twins is a mixed feeding routine is that, when breastfeeding, you will eventually need 1½–2 ‘breasts-full’ per feed – a bit tricky when you only have the two breasts! Many mothers struggle to produce enough milk for one baby let alone two and, although it is possible to feed twins exclusively on the breast for a while, this may mean feeding every 2–3 hours day and night. Topping up with expressed breast milk or formula gives you the guarantee your babies are full at each feed, will make lighter work of implementing a routine and ensure your babies sleep at night.
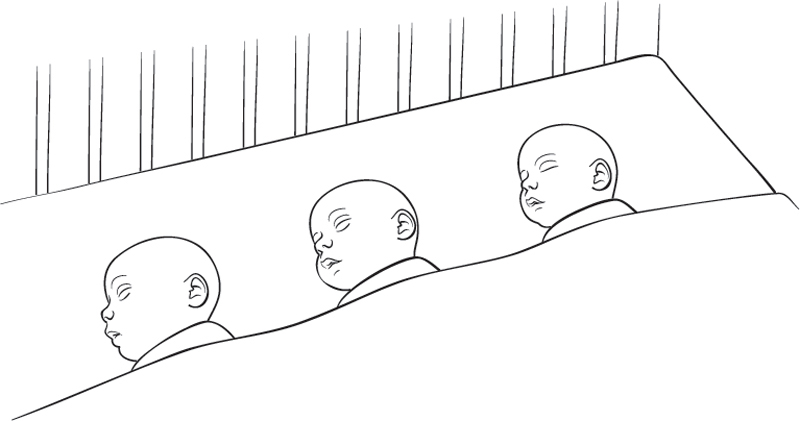
Tandem feeding (here) is key to the success of your routine, keeping your babies in sync and sleeping well at night. Start this as early on as you can. As your babies grow they will get heavier and move around so it is best to get used to tandem feeding while they are small and not yet on the move.
The twins’ routines are exactly the same in principle as a single baby routine, with the difference being your breastfeed is up to 30 minutes (rather than an hour) as it will take no longer than 30 minutes to drain one breast. Follow either the mixed feeding routine (here), also reading Chapter Two (here), or the bottle-feeding routine (see Part Two, here). Wake both babies up at the same time for feeds, put them down for their naps at the same time and do everything together as much as possible. The nights may be a bit tricky for a while, as twins often appear to take it in turns to wake for feeds. You may find that one twin will be the first to wake for a week, then the other will take over for a while. Regardless of which twin wakes in the night for feeds, get them both up to feed at the same time or you will exhaust yourself being awake all night, feeding them one at a time.
As with all my routines, the aim is to encourage your babies to sleep through the night and, with twins, it’s even more important not to ‘backtrack’ once you start to make progress. By this I mean that once the twins have started to fall into a pattern of waking at, say, 1am for a week, and then they start randomly waking earlier one night, try not to feed them but instead resettle them until after their usual waking time. The next day make sure the early waking twin has increased her milk intake and had enough awake time at each feed period. Your twins will most likely have growth spurts at different stages so their ability to stay awake for the duration of playtime and their appetites may differ. Work out what they are capable of individually in terms of milk intake and awake time, then build on and increase this until they can both stay awake for the full two-hour period. Also increase their milk intake during the day until they are sleeping through the night.
Once your babies are sleeping through the night and they have reached their maximum milk intake, you will need to be consistent with your routine to maintain results. By Week 8 your routine should now require less effort as feeds speed up as your babies’ guts start to mature and they now start to become self-winding, are able to stay awake with ease, settle themselves for naps and by Weeks 10–12 start to stay awake in motion, which takes all restrictions out of your previous daily routine. From Weeks 10–12 your babies’ rate of growth will have started to slow a little and their appetites will plateau. The longer your babies sleep through the night the more flexible feeds become as their appetites will go up and down slightly. So, once they are established and coming out of the newborn stage, allow your routine to become more flexible with milk intake and timings, but do keep to the bedtime routine to keep consistency with bedtime and sleeping through the night.
Although I do not recommend using dummies as they teach the wrong association with sucking, cause wind and digestive discomfort, and create a bad habit, I occasionally use them with twins as a temporary measure and only when they are both close to sleeping through the night; that is, when one twin is sleeping through and the other is still waking or they take it in turns to sleep through. For example, I would use a dummy if both babies were waking at 5am but their feed was not due until 6am, they had been waking at the same time for four or five nights and a habit of waking had been formed. This usually happens at around Weeks 6–8. Only use the dummy for a maximum of one week otherwise you will be stuck with it and then have the problem of your babies waking due to the dummy falling out, which could lead to you being awake in the night more often than ever before. The dummy trick will either work or it won’t, so, either way, stop using it. If it doesn’t work with settling or does work and waking issues are resolved, then throw it away! If you have a dummy around the house and have two whingeing babies at any point you may be tempted to use it which can create lots of problems within the routine. Only use the dummy when you have a consistent pattern – it should be the last resort in sleep training.
During the small wee hours of the night, a baby crying for two minutes can feel like 10 minutes because it is the only thing you can hear. As with a single baby, you should not jump to your babies’ every cry. This self-control can be harder with twins as you may worry that one crying baby will wake the other. I find that it’s not the crying that wakes the other twin but when they stop crying. You need to leave any crying for two minutes before reacting to see if your baby settles. Your twins may take it in turns to cry out, which can sound like they are awake for longer than they actually are when, in fact, they have only cried for a minute or so each and have resettled. You should be able to recognise the difference between each baby’s cry quite early on.
Tandem feeding allows you to feed both babies at the same time so they keep to the same schedule, which allows you to have the same amount of downtime as parents of a single baby. The routine is exactly the same as for a single baby, but may take a little longer when feeding and winding two babies, meaning day feeds – handling two babies to wind and feed – can take an extra 15 minutes at each feed.
When tandem feeding, each twin will have a whole breast each. Swap your starting breast for each baby at each feed, and then top up with expressed milk or formula until both babies are full. You should quickly get into a pattern of their milk intake. If your milk supply increases you will see a very slow increase in the milk your babies are taking at the top-up feed. If this doesn’t happen, or when your supply stops increasing, increase their top-up bottles by 30ml (1oz) per feed per week until they are sleeping through the night.
If you are using both expressed milk and formula for top-ups, use the expressed milk during the night firstly, then for the afternoon feed. Breast milk digests quicker and is a lighter feed than formula, and the aim is to encourage lighter feeds during the night and in the afternoon in order to build an appetite for the biggest feed of the day before bed. Formula should be given at the post-bath bedtime bottle as it is heavier and will sustain your babies for longer. It’s commonly thought that giving heavier feeds during the night will help your babies sleep longer at night, but this is simply not the case long-term. Instead, what this will do is encourage night waking for a big feed. Make sure you cap the night feeds at 120ml (4oz) maximum at any one feed or 20–30 minutes in total if you are breastfeeding. If you are finding you don’t have enough milk for a breastfeed alone, then give a 15–20-minute breastfeed and top up with a maximum of 30–60ml (1–2oz) to help settle your babies. The later they wake through the night, the more of a milk build-up you have and the more likely one breast will satisfy. If you have two night feeds, one could be a breastfeed and the other a 120ml (4oz) maximum bottle of expressed breast milk.
Breastfeeding, bottle-feeding and expressing with two babies is a lot of work for a mother so the second express (mid-morning) is optional. It’s still important to understand your milk supply so expressing after the morning feeds and in the evening will help you get to know your breasts, your milk flow and supply, while making sure your supply is tip-top. Expressing will also allow you a comfortable night as your babies sleep later through the night.
If you want to encourage a good milk supply and give your babies as much breast milk as possible, use the breast-feeding option during the night or for at least one of the night feeds if you have two night feeds. The bottle-feeding option for the nights is easier, but, as mentioned above, use breast milk here where possible to encourage lighter feeds during the night.
For tandem feeding you will need a sofa to feed your babies; one in the nursery for night feeds will make your life much easier. Tandem breastfeeding pillows only work if you have smaller, high breasts, but they are great if you can use them. Alternatively, two large, square pillows work well. Make sure the square pillows are firm and keep your babies raised, not sunken into the pillow. You may need a smaller pillow for support underneath. The pillows are slightly supported by your legs so your babies’ heads are higher than their bottoms either side of you.

Tandem feeding allows you to keep your babies on track and in sync with each other routine-wise. In the early weeks babies tend not to move, so tandem feeding is easy in that respect, but it means you don’t have the spare hand to prompt and keep your babies actively sucking. If you are bottle-feeding, hold the bottles lower down the bottle, closer to the teat so you can use your fingers to stroke their cheeks for encouragement. When one twin becomes inactive, take the bottle out and use your feeding hand to tickle her awake if the other twin is still actively drinking. This means you are not leaving the inactive twin to drift off to sleep, which will have an impact on playtime and naps. Leaving one twin sleeping while you are feeding the other encourages catnapping. Once the active twin starts to slow down, break them both for a wind break to help regain focus and encourage active feeding.
Once your babies start to move, with their arms and legs kicking and waving around out of control, their heads are able to turn away from the bottle and their stomach muscles start developing, you may be able to start the feed by tandem feeding for the first 90–150ml (3–5oz) and then need to feed one baby at a time, swapping them every 30–60ml (1–2oz). They will become increasingly harder to tandem feed as they get older. Moving forward with the bottle you can move to baby chairs to feed, sitting yourself between the two. Another option is to feed separately giving the most enthusiastic twin 30–60ml (1–2oz) to take the edge off her hunger and then swapping babies every 30–60ml (1–2oz). Tandem feeding where possible is your best option for keeping your babies on track for a successful routine.

Make up the bottles for top-ups before you start the breastfeed so they are ready to go. The milk will need to be warmed and the temperature tested on the inside of your wrist. If it stings it is too hot; it should feel warm or you should feel nothing. If the milk is too cold it can give your baby a stomach ache and be harder to digest, not to mention it is less appealing to drink. Leave both bottles in hot water, or a controlled temperature bottle warmer, to keep them at the perfect temperature for a quick change from breast to bottle. Wind your babies after every 5–10 minutes on the breast or every 15–30ml (½–1oz) on the bottle.
Your twin babies may vary dramatically in size but this doesn’t mean that the smaller twin will feed less. More often than not the smaller twin will have a bigger appetite in a race to catch up with her sibling. Your baby’s size doesn’t always determine the amount of milk you should give so try and keep both babies feeding around the same quantity of milk which will help keep them on the same routine. The intake only usually differs by 30ml (1oz) between babies. Wake them both at the same time, keep them awake for the same amount of time and put them to bed at the same time. Some days this might be tricky, much like keeping a single baby awake and on a routine, and they may have growth spurts at slightly different stages, but aim to encourage them both to feed, wind and have some awake time at each feed period.
| Weeks 3–5: Mixed Feeding Routine for Twins | |
| 7am | Tandem breastfeed for 25–30 minutes + 30–90ml (1–3oz) formula |
| 8/8.15am | Express Total awake and playtime (including feed): 2 hours |
| 9am | Nap |
| 10.30/11am | Tandem breastfeed for 25–30 minutes + 60–120ml (2–4oz) expressed breast milk/formula |
| 11.30am/12.15pm | Express Total awake and playtime (including feed): 1½–2 hours |
| 1/2.15pm | Nap |
| 2.30pm | Tandem breastfeed for 20–30 minutes + 90–120ml (3–4oz) expressed breast milk/formula Total awake and playtime (including feed): 1½–2 hours |
| 4/4.30pm | Nap |
| 6pm | Tandem breastfeed for 20–30 minutes |
| 6.30pm | Bath (34–35°C) |
| 6.45pm | 120–180ml (4–6oz) formula |
| 7.15/8pm | Bedtime (swaddled) |
| 9/9.30pm | Express |
| During the night | 11pm–3am: 90–120ml (3–4oz) bottle maximum or breastfeed for 30 minutes 3am–4am: 90ml (3oz) maximum or breastfeed for 20 minutes 4am–5am: 60–90ml (2–3oz) bottle maximum or breastfeed for 10–15 minutes, keep babies swaddled 5am–6am: No feed zone Wind every 30ml (1oz) or 5 minutes on the breast |
Jack and Samuel’s story
I arrived in the beautiful Peak District to help troubleshoot unsettled twin boys, Jack and Samuel, aged nine weeks old. The twins were already on a routine of structured feeding, being breastfed every three hours, but separately, and being topped up with a bottle of formula if and when they were not settling. They were not sleeping or settling well, they grunted, grizzled and were constantly passing wind, which gives the indication they were being fed too frequently, were not being winded frequently or may be sensitive to Mum’s diet. It was clear that wind and digestion were at least some of the reasons for their unsettled daytime naps – they were uncomfortable and needed to be winded more frequently during feeds. The boys were also waking three times a night. As soon as they cried out during the night, Mum was rushing in to feed, cuddle or rock them back to sleep, in the hope she could settle the crying twin quickly so he wouldn’t wake his brother. As a result the boys had not learned how to settle themselves. The twins were also being put to bed with their arms out and not tucked into their cot.
After assessing the situation for a few hours, we started putting my plan into action:
Putting this plan into action resulted in the boys waking once on my first night with them. By the second night they slept through the night, from 8pm to 7am, and they have kept on doing so ever since. Job done in just 48 hours!
MY ROUTINE IS based around 12 steps that can be used to introduce a simple structure into your baby’s life. The steps can be used as a tool to teach a better understanding of my method while following my routine, or they can assist you in creating your own. Maybe your end game isn’t a full night’s sleep but to help your baby’s digestion. Or you need help to encourage better feeding or settling habits. You will find that by following these simple steps they will have a positive effect on your baby’s well-being.
To encourage routine consistency, and for your day routine to have an effect on your nights, if your baby is not already awake from 6am, wake him up for a 7am feed every morning, regardless of feed timings in the night. This will help set your baby’s body clock and allow a flexible routine.
Newborns often find it hard to wake up after a nap and will easily fall asleep again once receiving the comfort of the breast or bottle. Waking your baby 10–15 minutes before each feed and having that time awake, even if it is fractious, will ensure he is wide awake and ready to feed effectively. When breastfeeding it is especially hard for a baby to stay awake while snuggled into Mum as the sucking action alone is soporific. Allowing enough time for your baby to wake properly will help in your quest for active and productive feeding. When your baby reaches 8–10 weeks and becomes interactive, this 10–15 minutes of wake-up time can be used to chat and say hello as, by this stage, your baby will want to communicate and engage with you. Interacting with your baby in this way before a feed means he will be able to focus better on feeding, otherwise you may find that he takes the edge off his hunger and then decides he wants to stop feeding before he is full to chat to you. The result is a reduced milk intake, which has a knock-on effect on your routine and night’s sleep.
When teaching your baby the difference between night and day, you need to encourage him to take the majority of his milk and awake time during the day. By waking your baby at specific times you are effectively setting his body clock to eat well at each feed, much like we do as adults, having breakfast, lunch and dinner usually at around the same time every day.
Making sure your baby is actively feeding, awake and well fed at each feed means you are giving him a ‘meal’, not a snack that would only sustain him for a short period – an hour or so, maybe less! Offering both breasts at each feed and encouraging active feeding not only stimulates the breasts to make more milk at each feed, but allows your baby to take enough milk to fill him up and sustain him for 3–4 hours. Making sure your baby is full at each feed also encourages longer sleep periods during the day and at night. By slowly and gradually increasing his milk intake during the day, your baby will naturally demand less milk at night, taking the majority of the milk he needs over a 24-hour period during daylight hours. The trick is to allow all feeds to increase but to cap the night feeds: if you are breastfeeding, by 10–15 minutes each side, including winding, and, if you are bottle-feeding, by 120ml (4oz). Over a period of weeks the quantity given at day feeds will become much more substantial than the night feeds, which are phased out naturally at your baby’s own pace.
Feeding meals not snacks will enable you to space out your baby’s day feeds long enough for his stomach to completely empty before the next feed. This helps aid digestion and overall stomach comfort. Feeding too frequently, every 1–2 hours say, and therefore topping up the stomach with milk before it has had a chance to digest the last feed and empty, causes wind and pain. Feeding too frequently will also inhibit long sleep periods. Once you have established breastfeeding, offer your baby both breasts at each feed for 30 minutes each side (which includes winding) every 3–4 hours during the day and for 15 minutes each side when he naturally wakes at night. When giving a bottle, increase your baby’s intake by 15–30ml (½–1oz) per bottle per week until night feeds are phased out and he is sleeping through the night.
As your baby grows, his appetite increases and you’ll find that the volume of milk he takes increases dramatically during the first six weeks. Obviously this is hard to gauge while breastfeeding, but expressing should help you understand your milk supply (see here). If bottle-feeding, you can easily track your baby’s progress.
Active sucking makes for efficient feeding and a well-fed baby. It’s so important to teach your baby to associate your breast or the bottle with food, and not with comfort or as an aid for sleep. If you are breastfeeding, this will ultimately increase your milk supply because your breasts are being properly stimulated. Comfort sucking and catnapping on the breast or bottle leads to less milk intake and disrupted sleep. Comfort sucking looks like a short up-and-down action, often with a shuddery jaw – nibble, nibble, pause, or long pause with the occasional suck. Active feeding looks like a wide circular motion with visible swallowing.
Your baby will naturally slow down as your milk flow slows, but try to encourage him to drain the breast and not slow down until his time is up or your breast is empty (see here for how to check your breasts for milk). Allow 30 minutes for each breast, including winding, until your flow of milk speeds up, your baby becomes an efficient feeder and he is sleeping through the night – this will happen at around Weeks 4–8. If you have a lower milk supply you may need to shorten the time on each breast to 20 minutes and top up if necessary in order to achieve longer periods of sleep at night. Help by massaging each breast while your baby is feeding for the last five minutes of the feed – it’s all about teamwork! That said, it is hard for a newborn baby to stay awake while feeding. In the first weeks of life, the sucking action alone is tiring and the cuddle-like position of breastfeeding is comforting. A build-up of wind, which gives a false sense of fullness, slowed milk flow and falling asleep all cause comfort sucking.
Bottle-fed babies tend to be more active when feeding than breastfed babies due to the constant flow of milk, but they can still start to doze off and lose focus. Drinking milk too quickly and finishing their bottle of milk in less than 30 minutes can result in a milk slump, vomiting and an inability to wake up. Wind regularly, at 15–30ml (½–1oz) intervals and use your spare hand to prompt him to keep your baby actively sucking. Don’t allow dozing and comfort sucking which is bad for digestion and leads to ineffective feeding.
Top tips for active feeding
Your baby’s digestive comfort will affect every part of your routine and is key to its success and a full night’s sleep. Newborns are unable to burp themselves and only become able to self-wind at around 8–12 weeks of age. It is hugely underestimated how much newborn babies need to be winded in order to be comfortable to feed, play and sleep well. Winding your baby frequently is very important as air in the tummy can swell up, giving a false sense of fullness, which makes a baby feel sleepy and can keep your baby asleep until the wind is relieved. This will not only lead to hunger (and therefore disrupted sleep) as your baby will not have fed enough, but it will also make him feel sleepy. The trapped wind can cause pain when the air travels through your baby’s digestive system, which, in turn, will also make for unsettled sleep. Trapped wind can also cause vomiting as the milk sits on top of a big air bubble in the stomach and, when you do eventually get the air out, it often brings the milk back up – this is known as ‘posseting’ (see here). I should say that a posset alone, which can happen often during and after a feed, does not mean your baby has wind, but babies will often posset milk when a burp pushes milk up on its way out.
I find that babies on my routine rarely pass wind. This is because my routine encourages you to expel most of the air caused by feeding throughout and after feeds through regular winding. In the first six weeks of life you will need to wind your baby every 5–10 minutes on the breast and every 15–30ml (½–1oz) on the bottle. Once you have finished feeding, your baby is still digesting milk, which creates gas, so you will need to wind him 10–15 minutes after feeding and then again 15–20 minutes after the last burp. This should come up easily, but if not check again in another 10–15 minutes. Don’t spend any length of time over this extra winding. Likewise, the winding process during feeds should take no longer than a few minutes – don’t spend most of the feed time winding. If you are breastfeeding and your milk is fast-flowing from around Week 4 then break to wind at two-minute intervals for the first two wind breaks on each breast.
To wind your baby make sure he is awake as you cannot wind a sleeping baby. Sit your baby on your knee with one of your hands supporting his stomach up to the chest so he has a nice straight back, with your forefinger and thumb supporting his chin and head. Pat his back with your other hand, cupping and moulding your hand around his back. By moulding your hand you are not directly patting his spine but either side of it. Rub his back using firm, circular, upward strokes.

It’s a myth that breastfed babies do not need winding; breastfed babies are as windy as bottle-fed babies! A baby drinks, therefore he has wind. Certain foods, such as the onion family and spices, can add fuel to the fire with wind issues so try and avoid these wind-forming foods in the first six weeks if you are breastfeeding.
You will find that effective winding makes all the difference to how long your baby sleeps. The less air in his tummy, the more milk he can take on and the happier playtime and better quality sleep he will have. Not winding frequently enough and effectively is the most common problem I come across with unsettled babies and sleep issues.
Contrary to popular belief, babies do much more than just feeding and sleeping in the first three months of life. Most babies in my care, aged 1–2 weeks old, are able to stay awake for 1¼–2 hours at each feed period, enjoying black-and-white pictures, looking around and working out their new environment. The aim is to keep your baby active and awake during and after feeds, while he digests the milk feed, though you will find that it is common for babies to become soporific during this period. Encouraging awake time helps with digestion by making sure your baby is wind-free before bed and nap time.

Having just been fed, this is also the most content time for your baby to be awake, which enables you to work out if he has had enough milk. A well-fed and winded baby will be able to play happily and engage. By encouraging awake time after feeds you are also teaching your baby the difference between night and day, which naturally has a positive effect on your nights.
Your baby’s awake time should be increased gradually over the first six weeks of life. With every baby in my care I first work out what each baby is capable of, by how long they regularly and naturally stay awake for after a feed, and build on that time. Of course, this may need to be helped along by a reviving nappy change after a feed to get your baby to wake if he has fallen asleep on the breast or bottle. Keep encouraging a longer awake time until each feed period is two hours. For some babies in my care this happens at Week 2, while for others it is at Weeks 4–6.
It’s important to recognise that your baby is not a robot and, during growth spurts, he may need more sleep and find it harder to stay awake. The aim is to encourage awake time at each feed period and, as sleep improves at night and your baby gets older, the easier he will find it to stay awake. Make sure you are starting your feeds and playtime somewhere you can remain still for the duration, such as at your house, or a friend or family member’s home. Newborns are unable to stay awake during motion and will quickly fall asleep while being pushed in the pram, driven in the car or worn in a sling. They will also struggle to stay awake if a room is too noisy or warm. It’s important for the routine that your baby falls asleep when he is truly tired, and not because of digestion, trapped wind or being coaxed into sleep with a cuddle, in a car seat or in the pram, which will make for unsettled sleep.
To help keep your little one awake:
Putting your baby down to sleep while he is still awake will teach self-settling. In the first few weeks this may be tricky as your baby may fall asleep while you are encouraging playtime or as soon as you start cuddling him. Once he is able to stay awake for two hours and is still awake just before his nap, then you can make sure he is put down to bed still awake but calmed and cuddled to encourage self-settling. Rocking or cuddling your baby to sleep is teaching him to associate falling asleep in this way. At some point, when he is a bit older, you will want him to settle himself and he won’t be able to. Teaching positive associations from the start is much kinder than having to break habits and cause confusion later on.
Having met all your baby’s needs – a full tummy, winded and sufficient awake time – he should settle easily without the aid of rocking, cuddling, a dummy or being pushed in the pram. If he does not settle you will need to work out why. Is he still hungry? Does he have wind? Has he not had enough awake time? Is he not swaddled and tucked into a pram or cot?
Despite the importance of teaching your baby to self-settle, you need to ensure you have a balance and allow plenty of cuddle and skin-on-skin time with your baby. This will ensure that you are getting the much-needed recovery rest which will help increase your milk supply and provide the all-important emotional bonding. Try to allocate one nap every day, or every other day, for skin-on-skin naps where your baby can sleep on you naked (but, of course, leave his nappy on!). See here for more on skin-on-skin naps. If you feel you need extra cuddles, pick your baby up from a nap and cuddle him 10–20 minutes earlier than your usual 10–15 minutes wake up, before feeds.
Naps should otherwise be in your baby’s bedroom in a cot, Moses basket or the pram, and he should be tucked in. Tucking your baby into bed will provide him with a feeling of comfort, being cuddled and security. (See Chapter Thirteen for more on sleep positions and tucking in.) Letting your baby fall asleep on a play mat or in a baby chair will not encourage good sleep habits.
Swaddling makes a baby feel secure and cuddled; it is the only prop I use to aid peaceful sleep. Babies go through much more light sleep periods than we do as adults and also have a startle (‘Moro’) reflex, which tends to kick in at around 3–6 weeks of age. The startle reflex means that a baby’s arms have no control and will startle and wave around, which can often wake a baby. Once woken, he will often find it hard to get back to sleep. Babies need to feel secure in order to sleep so swaddling at night and being tucked into their bed aids peaceful sleep.
If you find your baby’s day naps are unsettled then use the swaddle for day naps as well. I will usually swaddle a baby until they are sleeping through the night for a full two weeks, then wean them off by taking the swaddle away during the day for a week and then half-swaddling with one arm out at night for a few nights, before taking it awake completely by 4–5 months old. If it’s too soon for your baby and he is unsettled without the swaddle, keep swaddling for another two weeks and then try again. There is no need to rush the process.
Sleep positions are also important for enabling peaceful sleep (see here). I often see mothers pushing their wailing babies around in prams. Nine out of ten times the babies are flat on their backs with no covers on or with their arms flailing about. Babies need to feel secure in order to sleep. Tuck a blanket tightly over your baby’s shoulders and arms wherever he sleeps, as well as using the swaddle at night and if needed for day naps. Keep your baby’s blankets tucked in well to the sides of the pram, cot or Moses basket and at shoulder height so the material is not around your baby’s face. Loose blankets can be dangerous and can cause suffocation.
Though government advice is to sleep babies on their backs, and not on their stomachs or sides so they cannot roll on to their stomachs, I sleep babies slightly tilted on their sides using a roll pillow, which means they are unable to roll on to their stomachs. With the roll pillow, your baby’s back is leaning slightly raised on the pillow so any movement will result in back sleeping if used properly. If you wish to try side sleeping with your baby, discuss this with a healthcare professional first, and please see the video on my website for how to use roll pillows safely: www.thesleepingbabyroutine.co.uk. I change the direction the baby faces every 24 hours to form a perfectly round head and to eliminate the risk of flat head syndrome.
As the swaddling material and roll pillows (if using) can often raise your baby’s body slightly higher than his head, always raise the head of the cot, pram or Moses basket slightly higher than the feet. Use a rolled-up muslin under the Moses basket mattress or a small blanket under the cot mattress to ever so slightly raise the angle. Also ensure that you place your baby in the ‘feet to foot’ position, where his feet are at the end of the cot, Moses basket or pram. Please see the video on my website for how to safely swaddle your baby: www.thesleepingbabyroutine.co.uk.
Changing your baby’s nappy after each daytime feed has two benefits:
These days, quality disposable nappies work so well drawing moisture away from babies’ bottoms that nappy rash is not usually an issue. The key is to keep your baby’s bottom dry. Use plain, unbleached white kitchen roll to blot your baby’s bottom dry before putting on a fresh nappy. You shouldn’t need to use a barrier cream unless nappy rash occurs. Nappy rash is usually a result of poor hygiene, not drying a baby’s bottom properly after changing, the mother’s diet (too much acidity), teething or using low-grade, cheaper nappies which don’t absorb as well as the leading brands. If you are using lower-grade, eco-friendly nappies, you will need to change your baby before and after each daytime feed to keep him dry and prevent a sore, red bottom. If you need to change your baby’s nappy before a day feed then change it after the feed as well.
In terms of changing your baby at night-time, I recommend changing his nappy before a feed. Changing your baby before a night-time feed will avoid stimulation just before you want to settle him back to sleep. In fact, if your baby is only waking once in the night, you may not need to change his nappy at all, unless it is dirty of course.
Your baby’s body clock soon learns the difference between night and day and he will stop pooing at night usually when he starts sleeping through the night. I would highly recommend using a leading brand, such as Pampers Baby Dry, for night-time sleep; other nappies simply will not keep your baby’s bottom as dry. Some nappies now have a blue line indicator to let you know when your baby is wet. However, this does not mean that you need to change your baby’s nappy. Babies constantly wee and if you were to change his nappy every time a blue line showed you would be changing your baby three times more often than you need to. In my opinion, this wetness indicator is just a clever tactic by nappy companies to make you use and buy more nappies! You might want to try using a larger size nappy at night to absorb more and enable a longer time between nappy changes once your baby is sleeping through the night, but make sure the nappy is fitted securely around the legs to prevent any leaks.
If your baby has woken early or is unsettled during sleep for any reason, changing his nappy will only stimulate him! I have never known a baby to be upset and woken due to a wet or dirty nappy. It’s often thought that a nappy change will calm a baby and they will settle to sleep again once dry. However, in my experience, this will not work – your baby has woken or is crying for another reason and the nappy change will only stimulate and wake him fully, rather than soothe him back to sleep.
Staggering your baby’s last feed of the day and splitting it with a bath, whether you are breast- or bottle-feeding, will help to make this feed the largest and most important of all the daytime feeds, which will be key to helping your baby sleep for longer overnight. By staggering your baby’s milk intake and offering only a small amount of milk, including winding, before the bath helps for a calm bath without your baby screaming for milk. This really must be a small amount of milk: a maximum of 60ml (2oz) from the bottle or 10–15 minutes from each breast. Too much milk at this time may cause vomiting on the post-bath feed, from being sloshed around in the bath with a full tummy. Your baby may object to such a restricted feed at this time, but rest assured he will soon recognise it as part of the routine. Slow the 60ml (2oz) feed by breaking every 15ml (½oz), walk your baby around to distract him, or take him into the bathroom while you run the bath – the sound of running water has a white noise calming effect. Splitting the feed with the bath will enable your baby to take the majority of his milk after the bath, close to bedtime, and will mean he is ready to settle for a full night’s sleep or his longest stretch of sleep. Giving a bath as part of your bedtime routine also helps your baby to recognise that bedtime/night-time is coming. In the first six weeks while establishing the routine it’s a stimulating part of the day and your baby’s fourth awake period of the day.
Your baby’s bath temperature should be quite cool at the newborn stage – 34°C, or 32°C if we are in a heatwave and 35°C if it’s arctic weather! Use a bath thermometer, like the Philips AVENT bath and room thermometer, not your hand or elbow as we all have variations in skin sensitivity. As I mentioned earlier, babies are heat-sensitive, so a bath that is too warm will send your baby to sleep quickly and before he has had a chance to finish his bedtime feed. Only when your baby is out of the newborn stage, from three months old, will he be less heat-sensitive, so the temperature of the bath can increase. By this time you can also use the bath time routine as a calming, soothing tool to help settle your baby at bedtime and you can increase the duration of the bath as your baby finds the experience much more fun.
There is no need to actually wash your baby with soap every day – a sloshing of water for 5–10 minutes will do. For those newborns who are not yet used to the bath, make sure they are always covered in water by sloshing water over their tummies. I use a bath support, such as Angelcare, which goes into the bath and means you don’t have to break your back over the bath. These will usually last up until you use a seated position. Never step away from the bath – using a bath support may be hands-free, but you should never leave your baby unattended in water. A baby’s eye ducts are not working in the first 4–6 weeks of life – you may have noticed that your newborn does not cry tears – so any water or particles that get into the eyes are unable to drain away. For this reason, try not to get water into your baby’s eyes during bath time in the early days.
If you are breastfeeding, regardless of your milk supply, your milk will naturally deplete throughout the day. You can boost your supply with a lunchtime skin-on-skin nap, by resting, expressing or through your diet, but inevitably your supply will be lower in the late afternoon/evening than the morning. You may, in the first few weeks, have enough milk to satisfy your baby for the last and biggest feed of the day, but as your baby’s appetite grows to full capacity in 6–8 weeks, you will naturally have your lowest supply in the evenings. A poor design by Mother Nature indeed! If you are looking to get a full night’s sleep and phase out night waking, introducing a bottle of expressed breast milk, collected throughout the day, or formula at the last feed of the day will give your baby the boost and milk needed to sleep through the night. This bottle is key to the success of my routine. Babies at this time of day can be very sleepy and hard to feed so not only does the bottle-feed enable you to give a big feed but you won’t have the added issue of your baby drifting off to sleep as much as he would on the breast before he is full.
Another reason for introducing the bottle in the first weeks of life is that you won’t come up against bottle refusal. Rest assured, the bottle is your friend and this one bottle a day will not interfere with breastfeeding. Your baby will not reject your breast because of it or be confused, but instead will recognise it as part of his bedtime routine. This bottle-feed will result in a well-fed baby who sleeps for long periods at night. If you introduce a bottle at a later stage it may be, and often is, rejected. Introducing a bottle early on is also handy if, as a breastfeeding mother, you ever get sick, your supply dips or your baby is sick and throws up all his milk. If you don’t have enough breast milk collected giving formula at this stage is a win–win as your baby has all the night benefits of breast milk, and supplementing with formula at this time of day can often help babies sleep longer as it is heavier in composition and sustains for longer. This bottle-feed is a very small percentage of your baby’s overall milk intake and using formula at this time has no disadvantages. You should gradually increase the amount of this bottle-feed by 15–30ml (½–1oz) at a time until your baby has reached his own personal number of ounces needed to sleep through the night. I have found over the last 20 years that this number is generally between 200ml (7oz) and 260ml (9oz), which is usually reached between four and eight weeks of age. Bottle, teat shape and size do matter so head back to the bottle-feeding chapter to learn more (here).
Once you have established breastfeeding and your baby has regained his birth weight, is over 2.72kg (6lb) and is gaining weight, which should all happen by around Week 2, in contrast to your day routine you should let your baby wake of his own accord for feeds at night. This is where my technique differs from other baby experts who advise waking your baby on the dot for each feed day and night, or waking him for a ‘dream feed’ (a booster feed which is given before the parent would naturally go to bed). On my routine your nights are ‘baby-led’: if your baby is hungry, he will wake for a feed at night. By encouraging the majority of your baby’s milk intake during the day, combined with the staggered feed and bottle at bedtime, there is no need to wake your baby for a dream feed. As your baby’s day feeds and awake time increase over the weeks so will the length of time he sleeps at night, getting the much-needed rest to grow and thrive. As a result your baby will learn the difference between night and day very early on and night feeds will become efficient and short. You will also get the much-needed rest you need to recover and take care of your new baby.
When breastfeeding your baby will get into a routine much quicker than your breast, which can leave you feeling full, uncomfortable and unable to last until your baby naturally wakes. Your breasts will also need extra stimulation to make up for the loss of stimulation from your baby as he sleeps longer at night at this early stage. To combat this, express before you go to bed for the night at around 8–9pm. This will not only help keep your supply tip-top but keep you comfortable until your baby wakes naturally.
The ‘two-minute rule’ applies night and day, waiting two minutes to see if your baby resettles himself back to sleep. Babies wake often and go through many light periods of sleep. Most babies wake, shout and fall back to sleep until they are actually ready to be fed. You must allow your baby to do this to help encourage self-settling. This also means you are not jumping to his every whim, stimulating your baby awake unnecessarily or getting him up to feed when he is not ready. Babies who are picked up as soon as they shout, soon learn this is how to get picked up and you will end up with a baby who cries more, is insecure and is unable to be put down or settle himself.
The two-minute rule is not controlled crying but is instead simply a short pause to check and make sure your baby truly needs your attention. Babies cry! It’s their only way of verbal communication. It does not always mean they need feeding or attention. Babies cry to settle themselves, on waking, due to wind or when they are hungry. Giving your baby two minutes before you help him out will teach confidence in you and your baby’s ability to self-settle. The two-minute rule is for crying, not squeaking or grunting which most babies do in their sleep. Time it to make sure you are not jumping to attention too quickly.
The only time you would not wait for two minutes is after the bedtime feed. This is the only time of day your baby will go to bed on a full stomach. With the day feeds, he has playtime to digest his feeds and the night feeds are much lighter. If your baby cries out after you have settled him to bed, it is likely to be due to wind, overstimulation or because he is still hungry. Firstly, check for wind and then that the swaddle is secure. Give your baby a calming cuddle over the shoulder, in a dark or a very dimly-lit room, and if he still doesn’t settle, offer another 30–60ml (1–2oz) of milk. The last 30ml (1oz) should be slow moving, so if he finishes the bottle easily, offer a little more and increase it by another ounce the following evening.
The 7pm to 7am Sleeping Baby Routine allows your routine to be flexible. Your growing baby is not a robot and will often wake early or you may simply need to change the routine according to your day. Having said this, all my variations of the routine end the day with the same timings for the bath and bedtime routine. Ending each day at the same time encourages consistency which is important for your baby to recognise that bedtime is coming and to set his body clock to sleep at night.
Below are some alternative routine feed timings:
These 12 steps will help you to understand your baby’s needs and give you the flexibility if your routine goes a little off-piste. A routine needs to be flexible but consistent for it to work during the newborn stage, but once you are established everything becomes much less restrictive and automatic, and you will have a happy, sleeping baby.