 lift head briefly when on stomach on a flat surface
lift head briefly when on stomach on a flat surfaceYou’ve brought your baby home and you’re giving parenthood everything you’ve got. Yet you can’t help wondering: Is everything you’ve got enough? After all, your schedule (and life as you seem to recall knowing it) is upended; you’re holding your baby as if he or she were made of glass; and you can’t remember the last time you’ve showered or slept more than two hours in a row.
As your baby grows from a cute but largely unresponsive newborn to a full-fledged cuddly infant, your sleepless nights and hectic days will likely be filled not only with pure joy but also with exhaustion—not to mention new questions and concerns: Is my baby getting enough to eat? Why does he spit up so much? Are these crying spells considered colic? Will she (and we) ever sleep through the night? And how many times a day can I actually call the pediatrician? Not to worry. Believe it or not, by month’s end you’ll have settled into a comfortable routine with baby, one that’s still exhausting but much more manageable. You’ll also feel like a seasoned pro in the baby-care game (at least compared to what you feel like today)—feeding, burping, bathing, and handling baby with relative ease.
All babies reach milestones on their own developmental time line. If your baby seems not to have reached one or more of these milestones, rest assured, he or she probably will very soon. Your baby’s rate of development is almost certainly normal for your baby. Keep in mind, too, that skills babies perform from the tummy position can be mastered only if there’s an opportunity to practice. So make sure your baby spends supervised playtime on his or her belly. If you have concerns about your baby’s development, check with the doctor. Premature infants generally reach milestones later than others of the same birth age, often achieving them closer to their adjusted age (the age they would be if they had been born at term), and sometimes later.
All parents want to know if their babies are developing well. The problem is that when they compare their babies to the “average” baby of the same age, they find that their own child is usually ahead or behind—few are exactly average.
To help you determine whether your baby’s development fits within the wide range of normal rather than just into the limited range of “average,” we’ve developed a monthly span of achievements into which virtually all babies fall, based on the Denver Developmental Screening Tests and on the Clinical Linguistic and Auditory Milestone Scale (CLAMS). In any one month, a full 90 percent of all babies will have mastered the achievements in the first category, “What your baby should be able to do.” About 75 percent will have gained command of those in the second category, “What your baby will probably be able to do.” Roughly half will have accomplished the feats in the third category, “What your baby may possibly be able to do.” And about 25 percent will have pulled off the exploits in the last category, “What your baby may even be able to do.”
Most parents will find their babies achieving in several different categories at any one time. A few may find their offspring staying constantly in the same category. Some may find their baby’s development uneven—slow one month, making a big leap the next. All can relax in the knowledge that their babies are perfectly normal.
Only when a baby is not achieving what a child of the same age “should be able to do” on a consistent basis, need a parent be concerned and consult the doctor. Even then, no problem may exist—baby may just be marching (or rolling over, or pulling up) to a different drummer.
Use the What Your Baby May Be Doing sections of the book to check progress monthly, if you like. But don’t use them to make assessment of your baby’s abilities now or in the future. They are far from predictive. If checking your baby against such lists becomes anxiety-provoking rather than reassuring, by all means ignore them. Your baby will develop just as well if you never look at them—and you may be a lot happier.
By one month, your baby … should be able to:
 lift head briefly when on stomach on a flat surface
lift head briefly when on stomach on a flat surface
 focus on a face
focus on a face
… will probably be able to:
 respond to a bell in some way, such as startling, crying, quieting
respond to a bell in some way, such as startling, crying, quieting
… may possibly be able to:
 lift head 45 degrees when on stomach
lift head 45 degrees when on stomach
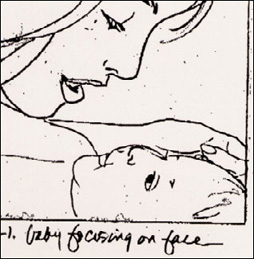
By the end of this month, a baby should be able to focus on a face.
 vocalize in ways other than crying (e.g. cooing)
vocalize in ways other than crying (e.g. cooing)
 smile in response to your smile
smile in response to your smile
… may even be able to:
 lift head 90 degrees when on stomach
lift head 90 degrees when on stomach
 hold head steady when upright
hold head steady when upright
 bring both hands together
bring both hands together
 smile spontaneously
smile spontaneously
Well-baby checkups will be events you’ll come to look forward to; not only as an opportunity to see how much your baby’s grown, but to ask the dozens of questions that have come up since the last visit with the practitioner but didn’t rate an immediate frantic phone call (there will be plenty of those, too). Make sure you keep a list of these questions and bring them along to appointments.
Each practitioner will have his or her own approach to well-baby checkups. The overall organization of the physical exam, as well as the number and type of assessment techniques used and procedures performed, will also vary with the individual needs of the child. But, in general, you can expect the following at a checkup when your baby is between one and four weeks old. (The first visit may take place earlier, or there may be more than one checkup in the first month, under special circumstances, such as when a newborn has had jaundice, was premature, or when there are any problems with breastfeeding.)
 Questions about how you and baby and the family are doing at home, and about baby’s eating, sleeping, bowel movements, and general progress.
Questions about how you and baby and the family are doing at home, and about baby’s eating, sleeping, bowel movements, and general progress.
 Measurement of baby’s weight, length, and head circumference, and plotting of progress since birth.
Measurement of baby’s weight, length, and head circumference, and plotting of progress since birth.
 Vision and hearing assessments.
Vision and hearing assessments.
 A report on results of neonatal screening tests (for PKU, hypothyroidism, and other inborn errors of metabolism), if not given previously. If the doctor doesn’t mention the tests, the results were very likely normal, but do ask for them for your own records. If your baby was released from the hospital before these tests were performed, or if they were done before he or she was seventy-two hours old, they will probably be performed or repeated now.
A report on results of neonatal screening tests (for PKU, hypothyroidism, and other inborn errors of metabolism), if not given previously. If the doctor doesn’t mention the tests, the results were very likely normal, but do ask for them for your own records. If your baby was released from the hospital before these tests were performed, or if they were done before he or she was seventy-two hours old, they will probably be performed or repeated now.
 A physical exam. The doctor or nurse practitioner will examine all or most of the following; some evaluations will be carried out by the experienced eye or hand, without comment:
A physical exam. The doctor or nurse practitioner will examine all or most of the following; some evaluations will be carried out by the experienced eye or hand, without comment:
 heart sounds with a stethoscope, and visual check of the heartbeat through the chest wall
heart sounds with a stethoscope, and visual check of the heartbeat through the chest wall
 abdomen, by palpation (feeling outside), for any abnormal masses
abdomen, by palpation (feeling outside), for any abnormal masses
 hips, checking for dislocation by rotating the legs
hips, checking for dislocation by rotating the legs
 hands and arms, feet and legs, for normal development and motion
hands and arms, feet and legs, for normal development and motion
 back and spine, for any abnormalities
back and spine, for any abnormalities
 eyes, with an ophthalmoscope and/or a penlight, for normal reflexes and focusing, and for tear duct functioning
eyes, with an ophthalmoscope and/or a penlight, for normal reflexes and focusing, and for tear duct functioning
 ears, with an otoscope, for color, fluid, movement
ears, with an otoscope, for color, fluid, movement
 nose, with otoscope, for color and condition of mucous membranes
nose, with otoscope, for color and condition of mucous membranes
 mouth and throat, using a wooden tongue depressor, for color, sores, bumps
mouth and throat, using a wooden tongue depressor, for color, sores, bumps
 neck, for normal motion, thyroid and lymph gland size (lymph glands are more easily felt in infants, and this is normal)
neck, for normal motion, thyroid and lymph gland size (lymph glands are more easily felt in infants, and this is normal)
 underarms, for swollen lymph glands
underarms, for swollen lymph glands
 the fontanels (the soft spots on the head), by feeling with the hands
the fontanels (the soft spots on the head), by feeling with the hands
 respiration and respiratory function, by observation, and sometimes with stethoscope and/or light tapping of chest and back
respiration and respiratory function, by observation, and sometimes with stethoscope and/or light tapping of chest and back
 the genitalia, for any abnormalities, such as hernias or undescended testicles; the anus for cracks or fissures; the femoral pulse in the groin, for a strong, steady beat
the genitalia, for any abnormalities, such as hernias or undescended testicles; the anus for cracks or fissures; the femoral pulse in the groin, for a strong, steady beat
 healing of the umbilical cord and circumcision (if applicable)
healing of the umbilical cord and circumcision (if applicable)
 the skin, for color, tone, rashes, and lesions, such as birthmarks
the skin, for color, tone, rashes, and lesions, such as birthmarks
 reflexes specific to baby’s age
reflexes specific to baby’s age
 overall movement and behavior, ability to relate to others
overall movement and behavior, ability to relate to others
 Guidance about what to expect in the next month in relation to feeding, sleeping, development, and infant safety.
Guidance about what to expect in the next month in relation to feeding, sleeping, development, and infant safety.
 Possibly hepatitis B vaccination, if baby did not receive it at birth and won’t be getting the combined DTaPhepB-IPV vaccine (Pediarix) starting at two months.
Possibly hepatitis B vaccination, if baby did not receive it at birth and won’t be getting the combined DTaPhepB-IPV vaccine (Pediarix) starting at two months.
Before the visit is over, be sure to:
 Ask for guidelines for calling when baby is sick. (What would necessitate a call in the middle of the night? How can the doctor be reached outside of regular calling times?)
Ask for guidelines for calling when baby is sick. (What would necessitate a call in the middle of the night? How can the doctor be reached outside of regular calling times?)
 Express any concerns that may have arisen over the past month—about baby’s health, behavior, sleep, feeding, and so on.
Express any concerns that may have arisen over the past month—about baby’s health, behavior, sleep, feeding, and so on.
 Jot down information and instructions from the doctor so you don’t forget.
Jot down information and instructions from the doctor so you don’t forget.
When you get home, record all pertinent information (baby’s weight, length, head circumference, blood type, test results, birthmarks) in a permanent health record.
Though this early in the parenting game you and your baby probably haven’t been apart for more than an hour or two (if that), there comes a time in every nursing mother’s life when she needs, or wants, more flexibility than round-the-clock breastfeeding can provide. When she can’t breastfeed her baby—because she’s working, traveling, or just out for the evening—but still wants her baby to be fed breast milk. Enter expressed milk.
It’s not so much a law of physics as it is a law of busy motherhood: You can’t always count on your baby and your breasts being at the same place at the same time. There is a way, however, to feed your baby breast milk (and keep your milk supply up) even if you and baby are miles apart: by expressing milk.
There are many situations (short- or long-term, on a regular schedule or just occasionally) when a mother might need or want to express breast milk, usually by pumping. The most common reasons why women pump are to:
 Relieve engorgement when the milk comes in
Relieve engorgement when the milk comes in
 Collect milk for feedings when working
Collect milk for feedings when working
 Provide relief bottles when away from home
Provide relief bottles when away from home
 Increase or maintain the milk supply
Increase or maintain the milk supply
 Store milk in the freezer for emergencies
Store milk in the freezer for emergencies
 Prevent engorgement and maintain milk supply when nursing is temporarily halted because of illness (mother’s or baby’s)
Prevent engorgement and maintain milk supply when nursing is temporarily halted because of illness (mother’s or baby’s)
 Maintain milk supply if nursing needs to be stopped temporarily because mother is taking medication that is incompatible with nursing
Maintain milk supply if nursing needs to be stopped temporarily because mother is taking medication that is incompatible with nursing
 Provide breast milk for a hospitalized sick or premature baby
Provide breast milk for a hospitalized sick or premature baby
 Provide milk for bottle or tube feeding when a baby (premature or otherwise) is too weak to nurse or has an oral defect that hinders nursing
Provide milk for bottle or tube feeding when a baby (premature or otherwise) is too weak to nurse or has an oral defect that hinders nursing
 Stimulate relactation, if a mother changes her mind about nursing or if a baby turns out to be allergic to cow’s milk after early weaning
Stimulate relactation, if a mother changes her mind about nursing or if a baby turns out to be allergic to cow’s milk after early weaning
 Induce lactation in an adopting mother, or in a biological mother whose milk is slow in coming in
Induce lactation in an adopting mother, or in a biological mother whose milk is slow in coming in
At one time, the only way to express milk was by hand, a long and tedious process that often failed to produce significant quantities of milk (and, frankly, hurt—a lot). Today, spurred by the resurgence of breastfeeding, manufacturers are marketing a variety of breast pumps—ranging from simple hand-operated models that cost a few dollars to pricey hospital-grade electric ones (that are now more affordable for home use)—to make pumping easier and more convenient. Though an occasional mother will still express by hand, at least to relieve engorgement, most will invest in either an electric, battery-operated, or manual pump.
Before deciding which type of pump is best for you, you’ll need to do a little homework:
 Consider your needs. Will you be pumping regularly because you’re going back to work or will be out of the house on a daily basis? Will you pump only once in a while to provide a relief bottle? Or will you be pumping full-time to provide nourishment for your sick or premature baby, who may be in the hospital for weeks or months?
Consider your needs. Will you be pumping regularly because you’re going back to work or will be out of the house on a daily basis? Will you pump only once in a while to provide a relief bottle? Or will you be pumping full-time to provide nourishment for your sick or premature baby, who may be in the hospital for weeks or months?
 Weigh your options. If you’ll be pumping several times a day for an extended period of time (such as when working or to feed a preterm infant), a double electric pump will probably be your best bet. If you need to pump only for occasional outings, a single electric, battery, or manual pump will fill your needs (and those few bottles). If you’re planning on expressing only when you’re engorged or for a rare bottle feeding, you can probably get away with expressing by hand (though an inexpensive manual pump may still make sense; it can take a lot of squeezing by hand to fill even one bottle).
Weigh your options. If you’ll be pumping several times a day for an extended period of time (such as when working or to feed a preterm infant), a double electric pump will probably be your best bet. If you need to pump only for occasional outings, a single electric, battery, or manual pump will fill your needs (and those few bottles). If you’re planning on expressing only when you’re engorged or for a rare bottle feeding, you can probably get away with expressing by hand (though an inexpensive manual pump may still make sense; it can take a lot of squeezing by hand to fill even one bottle).
 Investigate. Talk to friends who use pumps to see which they prefer. Not all pumps are created equal—not even among the electric ones. Some electric pumps can be uncomfortable to use, and some hand pumps painfully slow (and sometimes just plain painful) for expressing large quantities of milk. Also, discuss the options with a lactation consultant or your doctor. Research the types of pumps available (call up the manufacturers, check their Web sites), and consider your wallet as well as the models’ features before choosing one.
Investigate. Talk to friends who use pumps to see which they prefer. Not all pumps are created equal—not even among the electric ones. Some electric pumps can be uncomfortable to use, and some hand pumps painfully slow (and sometimes just plain painful) for expressing large quantities of milk. Also, discuss the options with a lactation consultant or your doctor. Research the types of pumps available (call up the manufacturers, check their Web sites), and consider your wallet as well as the models’ features before choosing one.
All pumps use a breast cup or shield that’s placed over your breast, centered over your nipple and areola. Whether you’re using an electric or manual pump, suction is created when the pumping action is begun, mimicking baby’s suckling. Depending on the pump you use (and how fast your let-down is), it can take anywhere from ten to forty-five minutes to pump both breasts. Pumping shouldn’t hurt; if it does, make sure you’re pumping correctly. If you are, and it still hurts, the fault might lie with the pump; consider making a switch.
It’s normal for human milk to be bluish or yellowish in color. Expressed milk will separate into milk and cream. This, too, is normal. Just shake gently to mix before feeding.
Electric pump. Powerful, fast, and easy to use (usually), a fully automatic electric pump closely imitates the rhythmic suckling action of a nursing baby. Many electric pumps allow for double pumping—a great feature if you’re pumping often. Not only does pumping both breasts simultaneously cut pumping time in half, it stimulates an increase in prolactin, which means you’ll actually produce more milk faster. Hospital-grade electric pumps are usually expensive, costing anywhere from a few hundred to a little more than a thousand dollars, but if time is an important consideration, one may be well worth the investment. (Also, when you weigh it against the cost of formula, you may break even or possibly come out ahead.)
Many women rent hospital-grade electric pumps from hospitals, pharmacies, or La Leche groups; some buy or rent jointly with other women, or buy them, use them, and then sell them (or lend them). Electric pumps also come in portable models that are inconspicuous (the black carrying cases are designed to look like backpacks or shoulder bags) and are also less expensive, smaller than and just as efficient as the hospital-grade ones. Some also come with a car adapter and/or battery pack so you don’t have to plug them in.
Battery-operated pump. Less powerful than the electric pumps, more expensive than the manual pumps, battery-operated pumps promise portability and efficient operation, but not all models deliver. They are usually moderately priced, but the speed at which some eat batteries makes them expensive to use and of questionable practicality.
Double pumping is quick, efficient, and comfortable.
Taking convenience to another level entirely are battery-operated pumps that are “wearable.” They come with soft breast cups about the size of a doughnut that are placed inside your bra and hooked up to small collection bags that lie flat against your body. Because the system is so discreet, you can wear it at the office, pumping while you work, without anyone being the wiser. And since it’s completely hands free, it’s the multitasker’s dream come true; you can pump while typing at the computer, talking on the phone, even cooking dinner. Check with your local La Leche League for the latest scoop on these.
Manual pump. These hand-operated pumps come in several styles; some are better than others:
 A syringe pump is composed of two cylinders, one inside the other. The inner cylinder is placed over the nipple and the outer, when pushed in and pulled out, creates suction that draws milk into it.
A syringe pump is composed of two cylinders, one inside the other. The inner cylinder is placed over the nipple and the outer, when pushed in and pulled out, creates suction that draws milk into it.
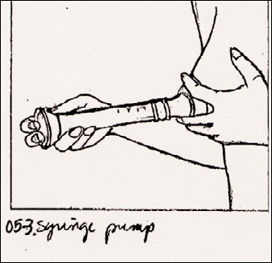
Though tough on the arm that’s doing the pumping, the syringe pump is a convenient way to express milk.
 A trigger-operated pump creates suction with each squeeze of the handle. One popular type includes petal massage cushions designed to simulate the infant’s compression on the areola, which stimulates let-down.
A trigger-operated pump creates suction with each squeeze of the handle. One popular type includes petal massage cushions designed to simulate the infant’s compression on the areola, which stimulates let-down.
 A bulb or “bicycle-horn” pump, which suctions milk from breasts with each squeeze of the bulb, is not recommended because it is very inefficient, uncomfortable, and extremely unsanitary (breeding bacteria that can contaminate the breast milk). It can also lead to sore nipples and damage breast tissue.
A bulb or “bicycle-horn” pump, which suctions milk from breasts with each squeeze of the bulb, is not recommended because it is very inefficient, uncomfortable, and extremely unsanitary (breeding bacteria that can contaminate the breast milk). It can also lead to sore nipples and damage breast tissue.
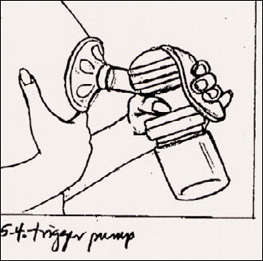
A trigger pump can efficiently stimulate let-down, making expressing milk an easy task.
No matter what method of expressing you choose, you may find it difficult to extract much milk the first few times. Consider those initial pumping sessions to be practice—your goal should be to figure out how to use the pump, not necessarily to score large quantities of milk. Milk probably won’t be flowing in copious amounts during early sessions anyway, for two reasons: First, you’re not producing that much milk yet (if your baby is still less than a month or two old); second, a pump (especially as wielded by a novice pumper) is much less effective in extracting milk than a baby is. But with perseverance (and practice, practice, practice), you’ll become an expert pumper in no time.
Both the syringe and trigger pumps are popular because they are fairly simple to use, moderate in price, easy to clean, portable, and can also double as feeding bottles.
Whenever you pump (and no matter what type of pump you’re using), there are basic preparation steps you’ll need to take to ensure a safe and easy pumping session:
 Time it right. Choose a time of day when your breasts are ordinarily full. If you’re pumping because you’re away from your baby and missing feedings, try to pump at the same times you would normally feed, about once every three hours. If you’re home and want to stock the freezer with breast milk for emergencies or relief bottles, pump one hour after baby’s first morning feeding, since most women have more milk earlier in the day. (Late afternoon or early evening, when women typically have the least milk, thanks to exhaustion and end-of-the-day stress, is usually a particularly unproductive time to pump.) Or pump from one breast while nursing your baby from the other one; the natural let-down action your body produces for your suckling baby will help stimulate milk flow in the pumped breast as well. (But don’t try this until you’re skilled at both nursing and expressing, since this can be a tricky maneuver for a beginner).
Time it right. Choose a time of day when your breasts are ordinarily full. If you’re pumping because you’re away from your baby and missing feedings, try to pump at the same times you would normally feed, about once every three hours. If you’re home and want to stock the freezer with breast milk for emergencies or relief bottles, pump one hour after baby’s first morning feeding, since most women have more milk earlier in the day. (Late afternoon or early evening, when women typically have the least milk, thanks to exhaustion and end-of-the-day stress, is usually a particularly unproductive time to pump.) Or pump from one breast while nursing your baby from the other one; the natural let-down action your body produces for your suckling baby will help stimulate milk flow in the pumped breast as well. (But don’t try this until you’re skilled at both nursing and expressing, since this can be a tricky maneuver for a beginner).
 Wash up. Wash your hands and make sure that all your pumping equipment is clean. Washing your pump immediately after each use in hot, soapy water will make the job of keeping it clean easier. If you use your pump away from home, carry along a bottle brush, detergent, and paper towels for washup.
Wash up. Wash your hands and make sure that all your pumping equipment is clean. Washing your pump immediately after each use in hot, soapy water will make the job of keeping it clean easier. If you use your pump away from home, carry along a bottle brush, detergent, and paper towels for washup.
 Keep it quiet. Choose a quiet, comfortably warm environment for pumping, where you won’t be interrupted by phones or doorbells, and where you will have some privacy. At work, a private office, an unoccupied meeting room, or the women’s lounge can serve as your pumping headquarters. If you’re at home, wait until baby’s naptime, or hand baby over to someone else so you can be free to concentrate on pumping (unless you’re pumping while nursing).
Keep it quiet. Choose a quiet, comfortably warm environment for pumping, where you won’t be interrupted by phones or doorbells, and where you will have some privacy. At work, a private office, an unoccupied meeting room, or the women’s lounge can serve as your pumping headquarters. If you’re at home, wait until baby’s naptime, or hand baby over to someone else so you can be free to concentrate on pumping (unless you’re pumping while nursing).
If you’re not double pumping, the breast not being pumped will start getting into the action ahead of time and will leak accordingly. To avoid a mess, make sure the breast that’s being ignored is well packed with breast pads (especially if you’ll be going back to your desk after pumping), or take advantage of every drop of milk and collect whatever leaks in a bottle, a clean cup, or a milk cup.
 Get comfy. Make yourself comfortable, with your feet up, if possible. Relax for several minutes before beginning. Use meditation or other relaxation techniques, music, TV, or whatever you find helps you unwind.
Get comfy. Make yourself comfortable, with your feet up, if possible. Relax for several minutes before beginning. Use meditation or other relaxation techniques, music, TV, or whatever you find helps you unwind.
 Hydrate. Drink some water, juice, milk, decaffeinated tea or coffee, or broth just before beginning.
Hydrate. Drink some water, juice, milk, decaffeinated tea or coffee, or broth just before beginning.
 Encourage let-down. Think about your baby, look at baby’s photo, and/or picture yourself nursing, to help stimulate let-down. If you’re home, giving baby a quick cuddle just before you start pumping could do the trick. If you’re using a “wearable” pump or an electric pump that leaves your hands free (by using a special “bra” devised to keep the pumps in place), you can even hold the baby—though many babies balk at being so near and yet so far from the source of their food (“Hey … why’s that machine having all the fun?”). Applying hot soaks to your nipples and breasts for five or ten minutes, taking a hot shower, doing breast massage, or leaning over and shaking your breasts are other ways of enhancing let-down.
Encourage let-down. Think about your baby, look at baby’s photo, and/or picture yourself nursing, to help stimulate let-down. If you’re home, giving baby a quick cuddle just before you start pumping could do the trick. If you’re using a “wearable” pump or an electric pump that leaves your hands free (by using a special “bra” devised to keep the pumps in place), you can even hold the baby—though many babies balk at being so near and yet so far from the source of their food (“Hey … why’s that machine having all the fun?”). Applying hot soaks to your nipples and breasts for five or ten minutes, taking a hot shower, doing breast massage, or leaning over and shaking your breasts are other ways of enhancing let-down.
Though the basic principle of expressing milk is the same whichever pump you use (stimulation and compression of the areola draws milk from the ducts out through the nipples), there are subtle differences in techniques depending on the type of pump (or, in the case of hand expression, nonpump) you’re using.
Expressing milk by hand. To begin, place your hand on one breast, with your thumb and forefingers opposite each other around the edge of the areola. Press your hand in toward your chest, gently pressing thumb and forefinger together while pulling forward slightly. (Don’t let your fingers slip onto the nipple.) Repeat rhythmically to start milk flowing, rotating your hand position to get to all milk ducts. Repeat with the other breast, massaging in between expressions, as needed. Repeat with the first breast, then do the second again.
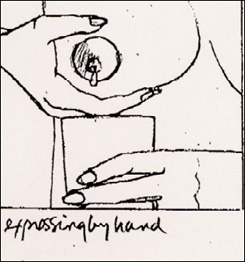
Expressing breast milk by hand is a slow process. This method is best for expressing only small amounts, as when the breast is too engorged for baby to get a comfortable mouthful.
To massage your breast, place one hand underneath your breast, the other on top. Slide the palm of one hand or both from the chest gently toward the nipple and apply mild pressure. Rotate your hands around the breast, and repeat in order to reach all the milk ducts.
If you want to collect the milk expressed, use a clean wide-topped cup under the breast you’re working on. You can collect whatever drips from the other breast by placing a breast shell2 over it inside your bra. Collected milk should be poured into bottles or storage bags and refrigerated as soon as possible (see page 162).
Expressing milk with a manual pump. Follow the directions for the pump you are using. You might find moistening the outer edge of the flange with water or breast milk will ensure a good suction, but it’s not a necessary step. The flange should surround the nipple and areola, with all of the nipple and part of the areola in it. Use quick, short pulses at the start of the pumping session to closely imitate baby’s sucking action. Once let-down occurs, you can switch to long, steady strokes. If you want to use a hand pump on one breast while nursing your baby on the other, prop the baby at your breast on a pillow (being sure he or she can’t tumble off your lap).
Expressing milk with an electric pump. Follow the directions for the pump you are using. Double pumping is ideal because it saves time and increases milk volume. You might want to moisten the outer edge of the flange with water or breast milk to ensure a good suction. Start out on the minimum suction and increase it as the milk begins to flow, if necessary. If your nipples are sore, keep the pump at the lower setting. You might find you get more milk from one breast than the other when you double pump—that’s normal, because each breast functions independently of the other.
Many pumps come with containers that can be used as storage and feeding bottles; others allow you to use a standard feeding bottle to collect the milk. Special breast milk storage bags are convenient for freezing milk. (Disposable bottle liners are made of thinner plastic than the milk storage bags and can break more easily.) Some pumps allow you to collect the expressed milk directly into the storage bags, so you don’t need the extra step of transferring the milk from bottle to bag before storing. Be sure to wash any containers or bottles used for milk collection in hot soapy water or a dishwasher after you’re done.
Fill breast milk storage containers or bags for the freezer only three-fourths full to allow for expansion, and label with the date (always use the oldest milk first).
Keep the milk that you expressed fresh and safe for baby by keeping these storage guidelines in mind:
 Refrigerate expressed milk as soon as you can; if that’s not possible, breast milk will stay fresh at room temperature (but away from radiators, sun, or other sources of heat) for as long as six hours.
Refrigerate expressed milk as soon as you can; if that’s not possible, breast milk will stay fresh at room temperature (but away from radiators, sun, or other sources of heat) for as long as six hours.
 Store breast milk for up to forty-eight hours in the refrigerator, or chill for thirty minutes, then freeze.
Store breast milk for up to forty-eight hours in the refrigerator, or chill for thirty minutes, then freeze.
 Breast milk will stay fresh in the freezer for anywhere from a week or two in a single-door refrigerator, to about three months in a two-door frost-free model that keeps foods frozen solid, to six months in a freezer that maintains a 0°F temperature.
Breast milk will stay fresh in the freezer for anywhere from a week or two in a single-door refrigerator, to about three months in a two-door frost-free model that keeps foods frozen solid, to six months in a freezer that maintains a 0°F temperature.
 Freeze milk in small quantities, 3 to 4 ounces at a time, to minimize waste and allow for easier thawing.
Freeze milk in small quantities, 3 to 4 ounces at a time, to minimize waste and allow for easier thawing.
 To thaw breast milk, shake the bottle or bag under lukewarm tap water; then use within thirty minutes. Or thaw in the refrigerator and use within twenty-four hours. Do not thaw in a microwave oven, on the top of the stove, or at room temperature; and do not refreeze.
To thaw breast milk, shake the bottle or bag under lukewarm tap water; then use within thirty minutes. Or thaw in the refrigerator and use within twenty-four hours. Do not thaw in a microwave oven, on the top of the stove, or at room temperature; and do not refreeze.
When your baby has finished feeding on a bottle, discard the remaining milk. Also discard any milk that has been stored for periods longer than those recommended above.
“I’m so afraid of handling the baby—he’s so tiny and fragile looking.”
Newborn babies may look as fragile as porcelain dolls, but they’re not. In fact, they’re really pretty sturdy. As long as their heads are well supported, they can’t be harmed by normal handling—even when it’s a little clumsy and tentative, as is often the case when the handling’s being done by a first-time parent. You’ll gradually learn what’s comfortable for your baby and for you, since handling styles vary greatly from parent to parent. Soon you’ll be toting your baby as casually as a bag of groceries—and often with a bag of groceries. For handling instructions, see pages 144–146.
“I’m so nervous when I handle my baby’s head—that soft spot seems so vulnerable. Sometimes it seems to pulsate, which really makes me nervous.”
That “soft spot”—actually there are two and they are called fontanels—is tougher than it looks. The sturdy membrane covering the fontanels is capable of protecting the newborn from the probing of even the most curious sibling fingers (though that’s definitely not something you’d want to encourage), and certainly from everyday handling.
These openings in the skull, where the bones haven’t yet grown together, aren’t there to make new parents nervous about handling baby (though that’s often the upshot) but, rather, for two very important reasons. During childbirth, they allow the fetal head to mold to fit through the birth canal, something a solidly fused skull couldn’t do. Later, they allow for the tremendous brain growth of the first year.
The larger of the two openings, the anterior fontanel, is on the top of the newborn’s head; it is diamond shaped and may be as wide as two inches. It starts to close when an infant is six months old and is usually totally closed by eighteen months.
The fontanel normally appears flat, though it may bulge a bit when baby cries, and if baby’s hair is sparse and fair, the cerebral pulse may be visible through it (which is completely normal, and nothing to worry about). An anterior fontanel that appears significantly sunken is usually a sign of dehydration, a warning that the baby needs to be given fluids promptly. (Call the baby’s doctor immediately to report this symptom.) A fontanel that bulges persistently (as opposed to a little bulging with crying) may indicate increased pressure inside the head and also requires immediate medical attention.
The posterior fontanel, a smaller triangular opening toward the back of the head less than half an inch in diameter, is much less noticeable, and may be difficult for you to locate. It generally is completely closed by the third month. Fontanels that close prematurely (they rarely do) can result in a misshapen head and require medical attention.
“At three weeks, my baby seems skinnier than when he was born. What could be wrong?”
Occasionally, an infant who had a lot of facial swelling at birth begins to look thinner as the swelling goes down. Most, however, have started to fill out by three weeks, looking less like scrawny chickens and more like rounded babies. In most cases, you can expect a breastfed baby to regain his birthweight by two weeks and then gain roughly 6 to 8 ounces a week for the next couple of months. But your eyes are not necessarily a reliable gauge of your baby’s weight gain (sometimes those who see a baby every day are less likely to notice his growth than those who see him less often). If you have some doubt about whether your baby’s making that kind of progress, call the doctor’s office and ask if you could bring him in for an impromptu weighing.
If baby’s tipping the scales just fine, then chances are he’s being fed just fine. If his weight isn’t up to speed, it’s possible that he’s not getting enough to eat (see page 164).
“When my milk came in, my breasts were overflowing. Now that the engorgement is gone, I’m not leaking anymore, and I’m worried I don’t have enough milk for my son.”
Since the human breast doesn’t come equipped with ounce calibrations, it’s virtually impossible to discern with the eye how adequate your milk supply is. Instead, you’ll have to use your baby as a guide. If he seems to be happy, healthy, and gaining weight well, you’re producing enough milk. You don’t have to spray like a fountain or leak like a faucet to nurse successfully; the only milk that counts is the milk that goes into your baby. If at any time your baby doesn’t seem to be thriving, more frequent nursing plus the other tips on the opposite page should help you produce more milk.
“My baby was nursing about every three hours and seemed to be doing very well. Now, suddenly, she seems to want to nurse every hour. Could something have happened to my milk supply?”
Unlike a well, a milk supply is unlikely to dry up if it’s used regularly. In fact, quite the opposite is true: The more your baby nurses, the more milk your breasts will produce. A much more plausible explanation for your baby’s frequent trips to the breast is a growth or appetite spurt. These occur most commonly at three weeks, six weeks, and three months, but can occur at any time during an infant’s development. Sometimes, much to parental dismay, even a baby who has been sleeping through the night begins to wake for a middle-of-the-night feeding during a growth spurt. In this case, a baby’s active appetite is merely nature’s way of ensuring that her mother’s body increases milk production to meet her growth needs.
Just relax and keep your breasts handy until the growth spurt passes. Don’t be tempted to give your baby formula (or even worse, solids) to appease her appetite, because a decrease in frequency of nursing would cut down your supply of milk, which is just the opposite of what the baby ordered. Such a pattern—started by baby wanting to nurse more, leading to mom becoming anxious about the adequacy of her milk supply and offering a supplement, followed by a decrease in milk production—is one of the major causes of breastfeeding being abandoned early on.
Sometimes a baby begins to demand more daytime feedings temporarily when she begins to sleep through the night, but this, too, shall pass with time. If, however, your baby continues to want to nurse hourly (or nearly so) for more than a week, check her weight gain (and see below). It could mean she’s not getting enough to eat.
“How can I be sure that my breastfed son is getting enough to eat?”
When it comes to bottle feeding, the proof that baby’s getting enough to eat is in the bottle—the empty bottle. When it comes to breastfeeding, determining whether baby’s well fed takes a little more digging. Luckily, there are several signs you can look for to reassure yourself that your breastfed baby is getting his fair share of food:
He’s having at least five large, seedy, mustardy bowel movements a day. Fewer than five movements a day in the early weeks could indicate inadequate food intake. (Though later on, around age six weeks to three months, the rate could slow down to one a day or even one every two to three days.)
His diaper is wet when he’s changed before each feeding. A baby who urinates more than eight to ten times a day is getting adequate fluid.
His urine is colorless. A baby who is not getting enough fluids passes urine that is yellow, possibly fishy smelling, and/or contains urate crystals (these look like powdered brick, give the wet diaper a pinkish red tinge, and are normal before the mother’s breast milk comes in but not later).
You hear a lot of gulping and swallowing as your baby nurses. If you don’t, he may not be getting much to swallow. Don’t worry, however, about relatively silent eating if baby is gaining well.
He seems happy and content after most feedings. A lot of crying and fussing or frantic finger sucking after a full nursing could mean a baby is still hungry. Not all fussing, of course, is related to hunger. After eating, it could also be related to gas, an attempt to push out a bowel movement or to settle down for a nap, or a craving for attention. Or your baby could be fussy because of colic (see pages 186–187).
You experienced breast engorgement when your milk came in. Engorgement is a good sign you can produce milk. And breasts that are fuller when you get up in the morning and after three or four hours without nursing than they are after nursing indicate they are filling with milk regularly—and also that your baby is draining them. If baby is gaining well, however, lack of noticeable engorgement shouldn’t concern you.
You notice the sensation of let-down and/or experience milk leakage. Different women experience let-down differently (see page 82), but feeling it when you start nursing indicates that milk is coming down from the storage ducts to the nipples ready to be enjoyed by your baby. Not every woman notices let-down when it occurs, but its absence (in combination with signs of baby’s failure to thrive) should raise a warning flag.
You don’t start menstruating during the first three months postpartum. The period usually doesn’t return in a woman who is exclusively breastfeeding, particularly in the first three months. Its premature return may be due to changing hormone levels, reflecting inadequate milk production.
“I thought my baby was getting enough to eat, but the doctor says the baby isn’t gaining weight quickly enough. What could be the problem?“
There are a number of possible reasons why your baby may not be thriving on breast milk. Many of them can be easily remedied, so that baby can continue nursing and start gaining weight faster:
Possible problem: You’re not feeding baby often enough.
Solution: Increase feedings to at least eight to ten times in twenty-four hours. Don’t go more than three hours during the day or four at night between feedings (four-hour daytime schedules were devised for bottle-fed babies). That means waking up a sleeping baby so that he won’t miss dinner or feeding a hungry one even if he just finished a meal an hour earlier. If your baby is “happy to starve” (some newborns are) and never demands feeding, it means taking the initiative yourself and setting a busy feeding schedule for him. Frequent nursings will not only help to fill baby’s tummy (and fill out his frame), they will also stimulate your milk production.
Possible problem: You’re not draining at least one breast at each feeding.
Solution: Nursing for at least ten minutes at the first breast should drain it sufficiently; if your baby accomplishes this task, let him nurse for as long (or as little) as he likes on the second. Remember to alternate the starting breast at each feeding.
Possible problem: You’re limiting the amount of time spent at the breast. Switching breasts after only five minutes (or before baby is ready to let go) can deprive baby of the rich, fatty hindmilk necessary for weight gain.
Solution: Watch your baby—and not the clock—to ensure that he gets not only the foremilk but also the hindmilk.
Possible problem: Your baby is a lazy or ineffective suckler. This may be because he was preterm, is ill, or has abnormal mouth development (such as a cleft palate or tied tongue).
Solution: The less effective the suckling, the less milk is produced, setting baby up for failure to thrive. Until he’s a strong suckler, he will need help stimulating your breasts to provide adequate milk. This can be done with a breast pump, which you can use to empty the breasts after each feeding (save any milk you collect for future use in bottles). Until milk production is adequate, your doctor will very likely recommend supplemental bottle feedings of formula (given after breastfeeding sessions) or the use of a supplemental system, or SNS (see illustration on facing page). The SNS has the advantage of not causing nipple confusion because it doesn’t introduce an artificial nipple.
If your baby tires easily, you may be advised to nurse for only a short time at each breast (you can pump the rest later to empty the breast), then follow with a supplement of expressed milk or formula given by bottle or the supplemental nutrition system, both of which require less effort by the baby.
Possible problem: Your baby hasn’t yet learned how to coordinate his jaw muscles for suckling.
Solution: An ineffective suckler will also need help from a breast pump to stimulate his mother’s breasts to begin producing larger quantities of milk. In addition, he will need lessons in improving his suckling technique; the doctor may recommend you get help from a lactation consultant and possibly even a speech/language pathologist. While your baby is learning, he may need supplemental feedings (see above). For further suggestions on improving suckling technique, call your local La Leche League.
Possible problem: Your nipples are sore or you have a breast infection. Not only can the pain interfere with your desire to nurse, reducing nursing frequency and milk production, it can actually inhibit milk let-down.
Solution: Take steps to heal sore nipples or cure mastitis (see pages 83 and 88). But do not use a nipple shield, as this can interfere with your baby’s ability to latch on to your nipples, compounding your problems.
Possible problem: Your nipples are flat or inverted. It’s sometimes difficult for a baby to get a firm hold on such nipples. This situation sets up the negative cycle of not enough suckling, leading to not enough milk, to even less suckling, and less milk.
Solution: Help baby get a better grip during nursing by taking the outer part of the areola between your thumb and forefinger and compressing the entire area for his sucking. Use breast shells between feedings to make your nipples easier to draw out, but avoid breast shields during nursing, which, though they can draw nipples out, can prevent baby from properly grasping your nipple and sets up a longer-term problem.
Possible problem: Some other factor is interfering with milk let-down. Let-down is a physical function that can be inhibited as well as stimulated by your state of mind. If you’re embarrassed or anxious about breastfeeding in general, or in a particular situation, not only can let-down be stifled, but the volume and calorie count of your milk can be affected.
Solution: Try to feed baby where you are most at ease—in private, if nursing around other people makes you tense. To help you relax, sit in a comfortable chair, play soft music, have something nonalcoholic to drink, try meditation or relaxation techniques. Massaging the breasts or applying warm soaks also encourages let-down, as does opening your shirt and cuddling baby skin to skin.
Supplemental Nutrition System: This apparatus can supply baby with supplementary feedings while stimulating mother’s milk production. A feeding bottle hangs around the mother’s neck; slim tubes leading from the bottle are taped down her breasts, extending slightly past the nipples. The bottle is filled with mother’s own milk, collected with a breast pump, with breast milk from a milk bank, or with the formula recommended by the baby’s doctor. As baby nurses at the breast, he takes the supplement through the tube. This system avoids the nipple confusion that arises when supplementary feedings are given in a bottle (a baby must learn to suck differently at bottle than at breast) and stimulates the mother to produce more milk even as she is supplementing artificially.
Possible problem: Your baby is getting sucking satisfaction elsewhere. If your baby is getting most of his sucking satisfaction from a pacifier or other nonnutritive source, he may have little interest in the breast.
Solution: Toss out the pacifier, and nurse baby when he seems to want to suck. And don’t give him supplementary bottles of water, which not only supply nonnutritive sucking but can dampen appetite and, in excess, alter blood sodium levels.
Possible problem: You’re not burping baby between breasts. A baby who’s swallowed air can stop eating before he’s had enough because he feels uncomfortably full.
Solution: Bringing up the air will give him room for more milk. Be sure to burp baby between breasts (or even mid-breast if nursing is taking a while) whether he seems to need it or not, more often if he fusses a lot while nursing.
Possible problem: Your baby is sleeping through the night. An uninterrupted night’s sleep is great for your looks but not necessarily for your milk supply. If baby is going seven or eight (or even ten) hours a night without nursing, your milk may be diminishing, and supplementation may eventually be needed.
Solution: To make sure this doesn’t happen, you may have to wake your little sleepyhead once in the middle of the night. He shouldn’t be going longer than four hours at night without a feeding during the first month.
Possible problem: You’ve returned to work. Returning to work—and going eight to ten hours without nursing during the day—can also decrease the milk supply.
Solution: One way to prevent this is to express milk at work at least once every four hours you’re away from baby (even if you’re not using the milk for feeding).
Possible problem: You’re doing too much too soon. Producing breast milk requires a lot of energy. If you’re expending yours in other ways and not getting adequate rest, your breast milk supply may diminish.
Solution: Try a day of almost complete bed rest, followed by three or four days of taking it easy, and see if your baby isn’t more satisfied.
Possible problem: You’re sleeping on your stomach. When you sleep on your stomach, something a lot of women are eager to do after the later months of pregnancy when they couldn’t, you also sleep on your breasts. And the pressure on your breasts could cut down on your milk production.
Solution: Turn over, at least partway, to take the pressure off those mammary glands.
Possible problem: You can use some help. Solution: Breastfeeding doesn’t come easily to every mother and every baby—and chances are some guidance from a knowledgeable source, such as a lactation consultant, can put you back on course (see page 69).
Possible problem: You’re harboring placental fragments in your uterus. Your body won’t accept the fact that you’ve actually delivered until all the products of pregnancy have been expelled, including the entire placenta. Until it’s thoroughly convinced that baby’s living on the outside now, your body may not produce adequate levels of prolactin, the hormone that stimulates milk production.
Solution: If you have any abnormal bleeding or other signs of retained placental fragments, contact your practitioner at once. A dilatation and curettage (D & C) could put you and your baby on the right track to successful breastfeeding, while avoiding the danger a retained placenta can pose to your own health.
Even with your best efforts, under the best conditions, with ample support from your doctor, a lactation consultant, your spouse, and your friends, it may turn out that you’re still unable to provide all the milk your baby needs. A small percentage of women are simply unable to breastfeed their babies without supplementation, and a very few can’t breastfeed at all. The reason may be physical, such as a prolactin deficiency, insufficient mammary glandular tissue, markedly asymmetrical breasts, or damage to the nerves to the nipple caused by breast surgery. Or it could be due to excessive stress, which can inhibit let-down. Or, occasionally, it may not be pinpointed at all. An early clue that your breasts may not be able to produce adequate milk is their failure to enlarge at all during pregnancy—though it’s not an infallible clue and is often less reliable in second and subsequent pregnancies than in first ones.
If your baby isn’t thriving, and unless the problem appears to be one that can be cleared up in just a few days, his doctor is almost certain to prescribe supplemental formula feedings. Don’t despair. What’s most important is adequately nourishing your baby, not whether you give breast or bottle. In most cases, when supplementing, you can have the benefits of the direct parent-baby contact that nursing affords by letting baby suckle at your breast for pleasure (his and yours) after he’s finished his bottle, or by using a supplemental nursing system.
Once a baby who is not doing well on the breast is put on formula, he almost invariably thrives. In the rare instance that he doesn’t, a return trip to the doctor is necessary to see what it is that is interfering with adequate weight gain.
“Why does my baby have a blister on her upper lip? Is she sucking too hard?”
For a baby with a hearty appetite, there’s no such thing as sucking too hard—although a new mother with tender nipples may disagree. And though “nursing blisters,” which develop on the center of the upper lips of many newborns, both breast and bottle fed, are caused by vigorous suckling, they have no medical significance, cause the infant no discomfort, and will disappear without treatment within a few weeks to months. Sometimes, they even seem to disappear between feedings.
“I seem to be nursing my new daughter all the time. Whatever happened to the four-hour schedules I’ve heard about?”
Apparently, your baby (like all the other nursing babies you’ll notice nipping at their mothers’ breasts almost continuously in the first few months of life) hasn’t heard about the four-hour schedule. Hunger calls and she wants to eat—a lot more often than most “schedules” would permit her to.
Let her—at least for now. Three- and four-hour schedules are based on the needs of bottle-fed newborns, who usually do very well on such regimens. But most breastfed babies need to eat more often than that. That’s because breast milk is digested more quickly than formula, making them feel hungry again sooner, and because frequent nursing helps establish a good milk supply—the foundation of a successful breastfeeding relationship.
Nurse as frequently as baby seems to want to during the early weeks. But if your baby is still demanding food every hour at three weeks of age or so, check with the doctor to see if her weight gain is normal. If it isn’t, seek advice from the doctor, and see Baby Getting Enough Breast Milk, page 166. If she seems to be thriving, however, it’s time to start making demands of your own. Hourly nursing is not only too much of an emotional strain for you, it’s a physical strain as well, making you exhausted, and may actually lead to decreased milk supply. Neither is it best for your baby, since she needs longer periods of sleep and longer periods of wakefulness when she should be looking at something other than a breast. Keep in mind, too, that crying doesn’t always signal hunger; babies also cry when they’re sleepy, bored, or just in the mood for attention (for help interpreting your baby’s cries, see page 123).
Assuming your milk supply is well established, you can start slightly stretching the periods between feedings (which may also help your baby sleep better at night). When baby wakes crying an hour after feeding, don’t rush to feed her. If she still seems sleepy, try to get her back to sleep without nursing her. Before picking her up, pat or rub her or turn on a musical toy, and see if she’ll drift back off. If not, pick her up, sing softly to her, walk with her, rock her, again with the goal of getting her back to sleep. If she seems alert, change her, talk to her, distract her in some other way, even take her for a stroll outdoors. She may become so interested in you and the rest of the world that she actually forgets about your breasts—at least for a few minutes.
When you finally do nurse, don’t accept the snack-bar approach some babies try to take; encourage her to nurse at least ten minutes on each side. If she falls off to sleep, try to waken her to continue the meal. If you can manage to stretch the periods between nursings a little more each day, eventually you and baby will be on a more reasonable schedule: two to three hours, and eventually four or so. But it should be a schedule based on her hunger, not the clock.
Today, most expectant parents of twins see double on the ultrasound screen early in pregnancy, making mad postpartum dashes to the store for a second set of everything rare. But even with seven or eight months’ notice, it may be impossible to prepare completely for the day when babies make four (or, if siblings are already on the scene, more). Knowing how to plan and what to expect can provide a greater sense of control over what may seem (at least initially) a fundamentally uncontrollable situation.
Be doubly prepared. Since double blessings often come early (full term for twins may be 37 weeks, rather than 40), it’s a good idea to start organizing for the babies’arrival well in advance. Try to have every childcare item in the house and ready for use before you go to the hospital. But while it makes sense to devote a lot of time to preparations, it doesn’t make sense to exhaust yourself (particularly if your practitioner has given you specific orders to take it easy). Get plenty of rest before the babies arrive—you can expect it to be a rare luxury once they do.
Double up. Do as much as possible for your babies in tandem. That means waking them at the same time so they can be fed together, putting them in the bath (once they’re able to sit) together, walking them in the stroller together. Double burp them together across your lap, or with one on your lap and the other your shoulder. When you can’t double up, alternate. At an early age, daily baths aren’t necessary, so bathe one one night, the other the next. Or bathe them every second or third night and sponge in between. Putting them foot to foot in the same crib during the early weeks may help them sleep better—but ask your doctor first. Some experts warn that tandem sleeping can increase the SIDS risk once the twins are able to roll over.
Split up. The work, that is. When both parents are around, divide the household chores (cooking, cleaning, laundry, shopping) and the babies (you take over one baby, your spouse the other). Be sure that you alternate babies so that both children get to know both parents well, and vice versa.
Try the double-breasted approach. Nursing twins can be physically challenging but eliminates fussing with dozens of bottles and endless ounces of formula. Nursing simultaneously will save time and avoid a daily breastfeeding marathon. You can hold the babies, propped on pillows, in the football position with their feet behind you (see page 72), or, with one at each breast, their bodies crossed in front of you. Alternate the breast each baby gets at every feeding to avoid creating favorites (and to avoid mismatched breasts, should one baby turn out to be a more proficient sucker than the other, or one baby getting less to eat if one breast turns out to be a less productive provider). If you find it too difficult to breastfeed your twins exclusively, you can nurse one while you bottle feed the other—again alternating from feeding to feeding. To keep up both your energy and your milk supply, be sure to get super nutrition (including 400 to 500 extra calories per baby) and adequate rest.
Plan to have some extra hands on hand, if you’re bottle feeding. Bottle feeding twins requires either an extra set of hands or great ingenuity. If you find yourself with two babies and just two hands at feeding time, you can sit on a sofa between the babies with their feet toward the back and hold a bottle for each. Or hold them both in your arms with the bottles in bottle proppers raised to a comfortable height by pillows. You can also occasionally prop the bottle for one in a baby seat (but never lying down), while you feed the other the traditional way. Feeding them one after the other is another possibility, but that will significantly cut into the already tiny amount of time you’ll have for other activities. This procedure will also put the babies on somewhat different napping schedules if they sleep after eating, which can be good if you’d like some time alone with each, or bad if you depend on that tandem sleeping time to rest or get things done around the house.
Double the help. All new parents need help—you need it twice as much. Accept all the help you can get, from any willing source.
Double up on equipment. When you don’t have another pair of hands around to help, utilize such conveniences as baby carriers (you can use a large sling for two babies, use two slings, or tote one baby in a carrier and one in your arms), baby swings (some models can’t be used until a baby is six weeks old), and infant seats. A play yard is a safe playground for your twins as they get older, and because they’ll have each other for company, they will be willing to be relegated to it more often and for longer periods than a singleton would. Select a twin stroller to meet your needs (if you will be traversing narrow grocery aisles, for example, a back-to-front model will be more practical than a side-by-side one); you will probably find a baby carriage a waste of money. And don’t forget that you will need two car seats. Put both in the backseat of the car.
Keep twice as many records. Who took what at which feeding, who was bathed yesterday, who’s scheduled for today? Unless you keep a log (in a notebook posted on the nursery wall, or on a blackboard), you’re sure to forget. Also make note in a permanent record book of immunizations, illnesses, and so on. Though most of the time, the babies will both get everything that’s going around, occasionally only one will—and you may not remember which one.
Don’t split zzz’s. Sleep will necessarily be scarce for the first few months, but it will be scarcer if you allow your babies to waken at random during the night. Instead, when the first cries, wake the second and feed them both. Any time that both your little darlings are napping during the day, catch a few winks yourself—or at least put your feet up.
Go one-on-one. Though it won’t be easy (at least in the beginning), there are ways to find that special one-on-one time with each child during the day. When you’re better rested yourself, stagger naptime—put one child down 15 minutes before the other—so you can shower some individualized attention on the one who’s awake. Or take only one child on an errand and leave the other one with a sitter or your spouse. Join a playgroup or parent-and-me class and alternate which child you bring along each week. Even everyday baby chores, such as diapering or dressing, can become special one-onone time for each child.
Double up on support. Other parents of twins will be your best source of advice and support; be sure to tap them. Find a parents-of-twins support group in your neighborhood or, if one is lacking, start one. But avoid becoming too clannish, socializing with only the parents of twins and having your babies participate in twins-only play groups. Though there’s something indisputably different about being a twin, excluding your children from relationships with singletons will discourage normal social development with peers—the majority of whom will not be twins.
Be doubly alert, once your twins are mobile. You’ll find, as your babies begin crawling and cruising, that what one of them doesn’t think of in the way of exploits, the other will. So they will need to be watched twice as carefully.
Expect things to get doubly better. The first four months with twins are the most challenging. Once you begin to work out the many logistics, you’ll find yourself falling into an easier rhythm. Keep in mind, too, that twins are often each other’s best company—many have a way of keeping each other busy that parents of demanding singletons find enviable, and which will free you up more and more in the months and years to come.
“I’ve been breastfeeding my son for three weeks, and I’m just not enjoying it. I’d like to switch to a bottle, but I feel so guilty.”
Beginning breastfeeding can be a frustrating series of trials and (plenty of) errors. As far as enjoyment goes, it can be elusive on both sides of the breast in this early adjustment period. It’s very possible that your dissatisfaction with Breastfeeding is just the result of a bumpy start (which almost always turns into a smooth ride by the middle of the second month). So it might make sense to hold off on your decision until your baby is six weeks old (or even two months), by which time he will have received many of the benefits of breastfeeding (though there are a lot of benefits to extended breastfeeding, see page 268), and breastfeeding generally will have become much easier and more satisfying for both participants. Then, if you’re still not enjoying nursing, feel free—and free of remorse—to wean. Remember, if it doesn’t feel right for you and your baby, it probably isn’t. Trust your feelings and your instincts.
“My baby loves his bottle. If it were up to him, he’d drink all day. How do I know when to give him more formula or when to stop?”
Because their intake is regulated both by their appetite and by an ingenious supply-and-demand system, breastfed babies rarely get too much—or too little—of a good thing. Bottle-fed babies, whose intake is regulated instead by their parents, can. As long as your baby is healthy, happy, and gaining adequate weight, you know he’s getting enough formula. But he can be taking in more than he needs—especially if his bottle becomes the liquid equivalent of an all-you-can eat buffet, continuously refilled by well meaning parents even after his appetite is satisfied.
Like labor contractions, intervals between feedings are timed from the beginning of one to the beginning of the next. So a baby who nurses for forty minutes starting at 10 A.M., then sleeps for an hour and twenty minutes before eating again, is on a two-hour schedule, not a one-hour-and-twenty-minute one.
Too much formula can lead to a too chubby baby (which, research shows, can lead to a too chubby child and a too chubby adult). But it can also lead to other problems. If your baby seems to be spitting up a lot (more than normal, see page 174), if he has abdominal pain (he draws his legs up onto a tense abdomen immediately after a feeding), and/or is gaining weight excessively, he might be taking too many ounces. Your baby’s pediatrician will be able to tell you what his rate of gain should be, and how much formula (approximately) he should be getting at each feeding (see page 108). If he does seem to be taking too much, try offering smaller-volume feedings, and stop when baby seems full instead of pushing him to take more; burp more often to relieve any abdominal discomfort he may have; and ask the doctor about whether you can give him an occasional small bottle of water (to quench his thirst without filling him up). Keep in mind, too, that it may just be the sucking (not the formula that comes with it) that he’s craving; some babies need to suck more than others. If that’s the case, consider using a pacifier during the next couple of months, while this need to suck is strongest (see page 194), or help him find his fingers or fist to suck on.
“I’m wondering if I should give our daughter bottles of water instead of nursing her so often.”
Sorry, but a bottle of water is no substitute—or supplement—for your breasts right now. A baby who is exclusively breastfed gets all the fluids she needs from breast milk, and that’s exactly where she should be getting them from. Not only doesn’t she need supplementary water under normal circumstances, she shouldn’t be offered any. First of all, bottles of water (particularly early on in breastfeeding) can satisfy her appetite and her need to suck, sabotaging nursing efforts. Second of all, too much water can dangerously dilute a baby’s blood, causing chemical imbalances. This second potential problem also holds true for bottle-fed babies who are fed too much water. Though it’s fine to give a little water to a bottle-fed baby in very hot weather, it’s not usually necessary. Giving an older infant (over age four months) small sips of water from a cup, however, is fine (they won’t be able to take too much from a cup, only from a bottle). Children on solids can handle more water, whether they’re breastfed or formula-fed.
“Everybody we talk to has a different opinion on vitamins for babies. We can’t decide whether or not to give them to our new son.”
The science of nutrition is still in its relative infancy—and that includes the study of vitamins (they weren’t even given that name until 1912). With lots more to learn, and with new information being uncovered each day, it’s not surprising that recommendations on giving vitamins seem to be ever-changing and ever-conflicting. And it’s not surprising that consumers—including new parents—are often left wondering how to proceed.
What’s clear is that babies who are formula-fed don’t need supplemental vitamins of any kind, because all the nutrients they need are already in the formula (just read the label and you’ll see). Plus, the double dose of vitamins can up their risk of developing food allergies, according to researchers. The picture’s less clear when it comes to babies who are exclusively breastfed. Current research indicates that healthy breastfeeding infants get most (though not all) of the vitamins and minerals they are believed to need from breast milk (if their mothers are eating a good diet and taking a pregnancy-lactation supplement daily). The vitamins that are missing from breast milk, most notably vitamin D, can be obtained from supplemental drops (see box on pages 174–175).
Some infants may need even more in the way of supplemental nutrients—for instance, babies who have health problems that compromise their nutritional status (those who are not able to absorb certain nutrients well from their foods and/or are on restricted diets) and babies of breastfeeding vegans who eat no animal products and take no supplements themselves. The latter should receive, at the very least, vitamin B½, which may be totally absent in their mother’s milk, and probably folic acid as well; but a complete vitamin-mineral supplement with iron is usually a good idea.
Healthy older children with adequate diets, on the other hand, probably do not need routine vitamins—even if one day the oatmeal ends up on the floor, most of the yogurt appears to be smeared on the high chair tray, and the evening offering of pureed chicken is tentatively tasted, then spit out. Some physicians nevertheless recommend giving vitamin drops daily, as health insurance, and probably will recommend an over-the-counter supplement that supplies no more than the recommended daily allowance of vitamins and minerals for your older baby. Don’t give your baby any additional vitamin, mineral, or herbal supplements unless recommended by the pediatrician.
Here’s a guide to the most common supplemental nutrients your baby’s pediatrician may prescribe:
Vitamin D. This vitamin, which is necessary for proper bone development and protects against diseases such as rickets, is naturally manufactured by the skin when it is exposed to sunlight. But because not all babies get enough sun to fill their vitamin D quota (about 15 minutes a week for fair-skinned babies, more for dark-skinned babies) due to protective clothing, sunscreen, and long winter months in certain instances, and because breast milk contains only a small amount of D, the AAP recommends vitamin D supplementation for infants who are breastfed—often in the form of ACD drops (which contain vitamins A, C, and D)—beginning within the first two months of life.
Since all the vitamins and minerals a baby needs (including D) are provided by commercial baby formula, bottle-fed infants who receive more than 16 ounces of formula a day do not need any additional supplementation. (Too much vitamin D can be toxic.)
Iron. Since iron deficiency during the first eighteen months of life can cause serious developmental and behavioral problems, it’s important that babies get enough iron. Your newborn, unless premature or low birth-weight, probably arrived with a considerable iron reserve, but this will be depleted somewhere between four and six months of age.
If you’re formula feeding, iron-fortified formula (the only kind recommended by the AAP) will fill baby’s needs. Breast milk contains sufficient iron during the first six months, so if you’re nursing, there’s no need for supplemental iron until the half-year mark is reached. Once solids are started, you can guarantee that your baby will continue to fill his or her requirement for this vital mineral by serving up foods that contain supplemental iron, such as enriched cereals, meats, and green vegetables. Adequate vitamin C intake will improve iron absorption, and once your baby begins taking a lot of solids, it’s a good idea to give a vitamin C food at each meal so that the benefits of any iron taken are maximized (see page 318). Supplemental iron drops are not a first choice for babies (though they may be recommended for preemies) because they are not well tolerated and can cause staining on the teeth. Also, the mineral can be toxic in large doses, so pediatricians use drops only when necessary.
Fluoride. According to the AAP, babies do not need fluoride supplementation during the first six months of life. After six months, a fluoride supplement should be given if there isn’t adequate fluoride in your water system. If you’re uncertain of the fluoride levels in your tap water, your baby’s doctor may be able to advise you. Or you can call your local water company or water authority. If your water is from a well or other private source, you can have its fluoride content checked by a lab (ask the health department how to have this done). Then check with your pediatrician to see if any additional fluoride is necessary.
With fluoride, as with most good things, too much can be bad. Excessive intake while the teeth are developing in the gums, such as might occur when a baby drinks fluoridated water (either plain or mixed with formula) and takes a supplement, can cause “fluorosis,” or mottling (white striations appearing on the teeth). Excessive intake can also occur if a baby or young child uses fluoridated toothpaste, which they tend to swallow. The lesser forms of mottling are not noticeable or aesthetically unattractive. More serious mottling, however, is not only disfiguring, but the pitting can predispose the teeth to decay, eliminating the good that fluoride is supposed to do.
Babies and young children, because of their small size and because their teeth are still developing, are particularly susceptible to fluorosis. So be wary of overdose. Once brushing is started, don’t use toothpaste unless your baby insists (and then use a tiny drop, or you can choose an unfluoridated baby toothpaste). Cap the paste whenever it’s not in use, and put it out of baby’s reach—some babies and toddlers love to eat the stuff.
“My baby spits up so much that I’m worried she’s not getting enough nourishment.”
Although it may seem all that’s going into your daughter is coming back up, that’s almost certainly not the case. What looks like a mealful of milk to you is probably no more than a tablespoon or two, mixed with saliva and mucus—certainly not enough to interfere with your baby’s nourishment. (To see how much a little bit of liquid can look like, spill a couple of tablespoons of milk on your kitchen counter.) Spitting up is extremely common in infancy, and although it’s messy and smelly, it’s not usually a cause for concern. (Doctors are fond of saying that spit-up is a laundry problem, not a health problem.)
Most babies spit up at least occasionally; some spit up with every feeding. The process in newborns may be related to an immature sphincter between the esophagus and the stomach and to excess mucus that needs to be cleared. In older babies, spitting up occurs when milk mixed with air comes back up with a burp. Sometimes a baby wisely spits up because she’s eaten too much.
The material your baby spits up will be relatively unchanged from the form in which it entered her mouth if it went only as far as the esophagus before coming back up. But if it traveled down to the stomach before its return trip, it will look curdled and smell like sour milk.
There are no sure cures for spitting up. But you can try to minimize the air gulping around mealtimes that can contribute to it: Don’t feed her when she’s crying (take a break in the action to calm her down); keep her as upright as possible while feeding and for a while afterward; if bottle feeding, be sure bottle nipples are neither too large nor too small and that bottles are tilted so that formula (not air) fills the nipple (or use an angled bottle or one with disposable liners). It may also be helpful to avoid bouncing her around while she’s eating or just afterward (when possible, strap her in a baby seat or stroller for a while after feedings). And don’t forget to burp her during a meal, instead of waiting until the end of the meal, when one big bubble may bring up the works.
Accept, however, that no matter what you do, if your baby’s a spitter, she’s going to spit—and you’re going to have to live with it for at least six months. (The living will be a little neater, however, if you keep a precautionary diaper on your shoulder or lap whenever you’re on baby duty.) Most babies ease up on their spitting when they start sitting upright, although a few will continue causing malodorous mayhem well up until their first birthdays.
Keep a small plastic bottle of water mixed with a little baking soda handy for spit-up spot cleaning. Rubbing a cloth moistened with the mixture on spots will keep them from setting and will eliminate most of the odor. Or use a diaper wipe.
While ordinary spitting is normal and no cause for concern, some kinds of spitting up do, however, signal possible problems. Call the doctor if your baby’s spitting up is associated with poor weight gain or prolonged gagging and coughing, if it seems severe (gastroesophageal reflux or GER), or if her vomit is brown or green in color or shoots out two or three feet (projectile vomiting). These could indicate a medical problem, such as an intestinal obstruction or pyloric stenosis (treatable by surgery). For more information on these conditions, see pages 556 and 646. Also call if the spitting seems to be causing baby discomfort. Most babies are “happy spitters”; if your baby is having pain with spitting, it may be because it’s causing an irritation in her esophagus.
“When my two-week-old spit up today after I nursed her, there were some reddish streaks in with the curdled milk. I’m really worried about her.”
Any blood that seems to be coming from a two-week-old baby, particularly when it’s found in her spit-up, is bound to be alarming. But before you panic, try to determine whose blood it actually is. If your nipples are cracked, even very slightly, it’s probably your blood, which baby could be sucking in (and then spitting up) along with the milk each time she nurses.
If your nipples aren’t obviously the cause (they may be, even if you can’t see the tiny cracks), or if you’re not Breastfeeding, call your pediatrician to help you figure out the source of the blood in your baby’s spit-up.
“My baby is crying a lot, and I’m wondering if he might be allergic to the milk in his formula. How can I tell?”
As eager as you might be to uncover a cause (and an easy cure) for your baby’s crying, milk is not a likely suspect. Milk allergy is the most common food allergy in infants, but it is less common than most people believe (only about one in a hundred babies will develop a true intolerance to milk). Most doctors believe it an unlikely possibility in a child whose parents don’t have allergies, and in one whose only symptom is crying. A baby who is having a severe allergic response to milk will usually vomit frequently and have loose, watery stools, possibly tinged with blood. Less severe reactions may include occasional vomiting and loose mucousy stools. Some babies who are allergic to milk may also have eczema, hives, wheezing, and/or a nasal discharge or stuffiness when exposed to milk protein.
Unfortunately, there’s no way to test for milk allergy, except through trial and error. If you suspect milk allergy, discuss the possibility with your baby’s doctor before taking any action. If there is no history of allergy in your family, and if there are no symptoms other than the crying, then it is likely the doctor will suggest you treat the crying spells as ordinary colic (see pages 186–187).
If there are family allergies or symptoms other than crying, a trial change of formula—to hydrolysate (in which the protein is partly broken down or predigested) or soy—may be recommended. A rapid improvement in the colicky behavior and the disappearance of other symptoms, if any, would suggest the possibility of an allergy to milk—or it could just be a coincidence. Reinstating the milk formula is one way of verifying the diagnosis; if the symptoms return with the milk, allergy is likely.
In many cases, there’s no change when a baby is switched to a soy formula. This may mean he’s also allergic to soy, has a medical condition that has nothing to do with milk and that needs to be diagnosed, or simply has an immature digestive system. A switch from soy to hydrolysate formula should help if the baby seems to be sensitive to both soy and milk.
Very rarely, the problem is an enzyme deficiency—an infant is born unable to produce lactase, the enzyme needed to digest the milk sugar lactose. Such a child has persistent diarrhea from the start, and fails to gain weight. A formula containing little or no lactose will usually resolve the problem. Unlike a temporary lactose intolerance that sometimes develops during a bout with an intestinal bug, a congenital lactase deficiency is usually permanent. The baby will probably never be able to tolerate ordinary milk products—though he is likely to be fine on those that are lactose reduced.
If the problem is not traced to milk allergy or intolerance, it’s probably best to stay with—or switch back to—a cow’s milk formula, since it is the better breast milk substitute.
Infant allergy to cow’s milk is usually outgrown by the end of the first year, and almost always by the end of the second. If your baby is taken off cow’s milk formula, his doctor may suggest trying it again after six months on a substitute formula, or may suggest waiting until the first birthday.
“I’m breastfeeding my son exclusively, and when I changed his diaper today, I noticed some streaks of blood in his bowel movement. What can that mean?”
Babies are virtually never allergic to their mother’s milk, but, very rarely, a baby can be allergic to something in his mother’s diet that ends up in her milk—often cow’s milk proteins. And it sounds as if this might be the case with your very sensitive infant.
Symptoms of such an allergy, known as allergic colitis, include blood in baby’s stool; fussiness or crankiness; lack of, or minimal (or no) weight gain; vomiting and/or diarrhea. Your baby could have one or all of these symptoms. Researchers suspect that some babies may become sensitized to certain foods mother eats while baby is still in utero, causing such allergies after birth.
While cow’s milk and other dairy products are a common culprit in these reactions, they’re not the only ones. Other possibilities include soy, nuts, wheat, and peanuts. A quick check with your baby’s doctor will probably lead you to this course of action: To determine what in your diet is causing your baby’s allergy, try eliminating all potentially offending foods for a week (or until your baby’s symptoms disappear), and then slowly reintroduce them into your diet while you monitor your baby’s reaction.
Usually, you’ll quickly see which of the foods you eat cause problems for your baby. Occasionally, no correlation between foods and allergic symptoms is found. In that case, your baby might just have had a gastrointestinal virus that caused the streaks of blood in his stool. Or there might be small cracks or fissures in his anus that caused the bleeding. Monitoring by your baby’s doctor should solve the mystery.
“I expected one, maybe two, bowel movements a day from my breastfed baby. But she seems to have one in every diaper—sometimes as many as ten a day. And they’re very loose. Could she have diarrhea?”
Your baby isn’t the first breastfed infant ever who seemed to be bent on beating the world record for dirtying diapers. Not only is such an active elimination pattern not a bad sign in a breastfed newborn, it’s a good one. Since the amount that’s coming out is related to the amount going in, any breastfeeding mother whose newborn has five or more movements daily can be assured that her baby is getting sufficient nourishment. (Mothers of nursing newborns who have fewer movements should see page 167.) The number of movements progressively decreases and may dwindle down to no more than one a day, or every other day, next month, though some babies continue to have several movements a day for the entire first year. It’s not necessary to continue keeping count—the number may vary from day to day, and that’s perfectly normal, too.
Normal, also, for breastfed infants is a very soft, sometimes even watery, stool. But diarrhea—frequent stools that are liquidy, smelly, and may contain mucus, often accompanied by fever and/or weight loss—is less common among children who dine on breast milk alone. If they do get it, they have fewer, smaller movements than bottle-fed babies with diarrhea and recover more quickly, probably because of the antibacterial properties of breast milk.
“My son’s bowel movements come with such force and such explosive sound, I’m worried that he has some digestive problem. Or maybe something’s wrong with my breast milk.”
Breastfed newborns are rarely discreet when it comes to making bowel movements. The noisy barrage that fills the room as they fill their diapers can often be heard in the next room, and can alarm first-time parents. Yet these movements and the surprising variety of sounds that punctuates their passing are normal, the result of gas being forcefully expelled from an immature digestive system. Things should quiet down in a month or two.
“My baby passes gas all day long—very loudly. Could she be having stomach troubles?”
The digestive exclamations that frequently explode from a newborn’s tiny bottom, at least as emphatically as the grownup variety, can be unsettling—and sometimes embarrassing—to parents. But, like explosive bowel movements, they are perfectly normal. Once your newborn’s digestive system works out the kinks, the gas will pass more quietly and less frequently. Until then, you can always blame the dog (that is, if you have one handy).
“I’m worried that my baby is constipated. He’s been averaging only one movement every two or three days. Could it be his formula?”
Childhood constipation has been flippantly defined as having movements less often than your parent. But that’s an unreliable gauge, since each individual has a personal pattern of elimination, and it’s not necessarily a case of “like parent, like child.” Some bottle-fed babies go three or four days between movements. But they’re not considered to be constipated unless those infrequent movements are firmly formed or come out in hard pellets, or if they cause pain or bleeding (from a fissure or crack in the anus as a result of pushing). If your baby’s movements are soft and cause no problems, don’t worry. But if you suspect constipation, consult his doctor. Giving baby a little water (only with the doctor’s okay) might help. (For babies older than four months, a small amount of prune juice may ease constipation; check with the doctor before offering it.) Rarely, a milk allergy can cause constipation, in which case a switch of formulas might do the trick (again, only with the doctor’s approval). And don’t take any other steps, such as giving laxatives (even mineral oil), enemas, or herbal teas without medical advice.
“I thought breastfed babies were never constipated—but my daughter grunts and groans and strains whenever she has a bowel movement.”
It’s true that breastfed babies are rarely constipated, because breast milk is just the right match for the human baby’s digestive tract. But it’s also true that some have to push and strain to get their movements out, even though the movement comes out soft and seems as though it should have been easy to pass.3 Why this is so isn’t certain. Some have theorized it’s because the soft stool of the breastfed baby doesn’t put adequate pressure on the anus. Others speculate that the muscles of the newborn anus are neither strong enough nor coordinated enough to eliminate any stool easily. Still others point to the fact that young babies, who usually have bowel movements lying down, get no help from gravity.
Whatever the reason, the difficulty should ease up when solids are added to your baby’s diet. But, in the meantime, don’t worry. And don’t use laxatives (even mineral oil), enemas, or any other home remedies for the problem—because it really isn’t one. When an adult is constipated, walking often helps alleviate the problem; you might try flexing and extending your baby’s legs in a bicycling motion while she’s on her back to assist her when she seems uncomfortable.
“My parents say they always put me to sleep on my tummy. But the doctor says our baby should sleep on her back. I’m confused.”
When your parents were putting you to sleep, tummy was indeed the position of choice. That’s because experts used to believe that being tummy down prevented babies from choking on their spit-up while they slept. But more recent research indicates that the back position is the safest position of all. Studies have shown that back sleepers have fewer fevers, fewer problems with nasal congestion, and fewer ear infections than tummy sleepers, and are no more likely to spit-up during the night (or choke on their spit-up). But by far the most important reason why back sleeping is safer: Placing babies to sleep on their backs sharply reduces the risk of crib death (SIDS). This compelling evidence has prompted the Back to Sleep campaign of the American Academy of Pediatrics, which recommends that all healthy infants be put to sleep on their backs.4
Start your baby sleeping on her back right away, so that she’ll get used to and feel comfortable in that position from the beginning (most babies naturally prefer being tummy down). Some babies fuss a lot on their back; because their flailing arms and legs don’t have the mattress to snuggle against, they may feel less cozy and secure. Because of that, you’ll probably find that your baby startles more often during sleep, which may lead to slightly more frequent wakings. (Swaddling baby early on may make her more comfy—and content—on her back; see page 199.) It’s also possible that she will develop a flat or bald spot from always facing in the same direction—usually because she is focusing on the same spot (often a window)—while lying on her back. To minimize this problem, alternate her position (head at one end of the crib one night, the other the next). If in spite of your efforts her head flattens or a bald spot develops, don’t worry. These problems will gradually correct themselves as she gets older. Severe cases can be corrected with a special headband or helmet.
Putting baby on her tummy to play when she’s awake (and watched) will minimize flattening while allowing her to develop muscles and practice gross motor skills (see page 210). Remember: Back to sleep, tummy to play.
“I thought newborns were supposed to sleep all the time. Our three-week-old daughter hardly seems to sleep at all.”
Newborns often seem not to know what they’re “supposed to do.” They nurse erratically when they’re “supposed to” be on a three- or four-hour schedule, or they sleep twelve hours a day (or twenty-two) when they’re “supposed to” sleep sixteen and a half hours. That’s because they know what we often forget—that there’s almost nothing a baby is supposed to do at any specific time. “Average” babies, who do everything by the book, do exist—but they’re in the minority. The sixteen and a half hours that reflects the average sleeping time for babies in their first month of life takes into account babies who sleep twelve hours a day and others who sleep twenty-three, as well as all those in between. The baby who falls at either end of the spectrum is no less normal than one who falls near the average. Some infants, like some adults, appear to need more sleep than others, some less.
So assuming your baby seems healthy and happy in every way, don’t worry about her wakefulness, but do get used to it. Infants who sleep very little tend to grow into children who sleep very little—with parents who, not coincidentally, also sleep very little.
“My baby gets up several times a night. My mother says if I don’t get her into a regular sleeping pattern now, she may never develop good sleep habits. She says I should let her cry it out instead of feeding her all night.”
Any experienced parent, particularly whose experience has included coping with a child who wouldn’t sleep through the night or who had trouble falling asleep, knows the importance of fostering good sleep habits in children at an early age. But the first month of life is way too early. Your baby is just beginning to learn about the world. The most important lesson she needs to learn now is that when she calls, you will be there—even at 3 A.M., and even when she’s up for the fourth time in six hours. There are many methods that can be used by parents who want to help their baby figure out how to fall asleep by herself, but not for several months yet—not until she begins to feel more secure and more in control of her environment.
If you’re breastfeeding, trying to institute a sleeping schedule now could also interfere with establishing a good milk supply—and with your baby’s growth. Breastfed newborns need to eat more frequently than bottle-fed babies, often every two or three hours, which generally prevents them from sleeping through the night until somewhere between the third and sixth month. Like the time-honored four-hour feeding schedule, the belief that babies should sleep through the night by two months is based on the developmental behavior of formula-fed infants, and it’s often unrealistic for those who are nursing.
So while there’s no harm in thinking ahead about fostering good sleep habits in your child, it’s too early to put those plans into action.
“Our baby, who shares our room, tosses and turns all night. Could our being near be keeping him from sleeping soundly?”
Although the phrase “sleeping like a baby” is often equated with enviably peaceful rest, particularly by the manufacturers of mattresses and sleep aids, babies’ sleep isn’t peaceful at all. Newborns do sleep a lot, but they also wake up a lot in the process. That’s because much of their sleep is REM (rapid eye movement) sleep, an active sleep with dreaming and a lot of movement. At the end of each REM sleep period, the sleeper usually awakens briefly. When you hear your baby fuss or whimper at night, it’s probably because he’s finishing a REM period, not because you share a room with him.
As he gets older, his sleeping patterns will mature. He will have less REM sleep and longer periods of the much sounder “quiet sleep,” from which it’s harder to rouse him. He will continue to stir and whimper periodically, but less frequently.
Though your being in the same room with baby probably isn’t disturbing his sleep at this stage, it certainly is disturbing yours. Not only do you waken at every moan, but you are also tempted to pick him up more often than necessary during the night. Try to ignore your baby’s midnight murmurings; pick him up only when he begins to cry steadily and seriously. You’ll both sleep better. If you find that difficult, then perhaps you should consider separate sleeping quarters—if you have the space and aren’t choosing to co-sleep for other reasons.
Do be alert, however, for sudden waking and crying, unusual restlessness, or other changes in sleeping patterns that don’t seem to be related to events in baby’s life (such as teething or an over-stimulating day). If you note them, check for signs of illness such as fever, appetite loss, or diarrhea (see chapter 18). Call your doctor if the symptoms persist.
“My three-week-old sleeps most of the day and wants to stay up all night. How can I get her to reverse her schedule so we all can get some rest?”
Babies who work (or play) the night shift, getting most of their sleep by day, can turn normally active, alert parents into barely functioning zombies. Happily, this blissful ignorance of the difference between day and night isn’t a permanent condition. The newborn who, before her arrival in the world of daytime light and nighttime darkness, was kept in the dark for nine months just needs a little time to adjust.
Chances are your baby will stop mixing up her days and nights within the next few weeks on her own. If you’d like to help speed the process, try limiting her daytime naps to no more than three or four hours each. Although waking a sleeping infant can be tricky, it’s usually possible. Try holding her upright, eliciting a burp, stripping off her clothes, rubbing under her chin, or massaging her feet. Once she’s somewhat alert, try to further stimulate her: Talk to her, sing lively songs, dangle a toy within her range of vision, which is about 8 to 14 inches. (For other tips on keeping baby awake, see page 122.) Don’t, however, try to keep her from napping at all during the day, with the hope that she’ll sleep at night. An overtired, and perhaps overstimulated, baby is not likely to sleep well at night.
Making a clear distinction between day and night may help. If she naps in her room, avoid darkening it or trying to keep the noise level down. When she wakens, ply her with stimulating activities. At night, do the opposite. When you put baby to bed, strive for darkness (use room-darkening shades), relative quiet, and inactivity. No matter how tempting it may be, don’t play with or talk to her when she wakens during the night; don’t turn on the lights or the TV while you’re feeding her; keep communications to a whisper or softly sung lullabies; and be certain when she’s back in her crib that sleeping conditions are ideal (see Better Sleep for Baby, page 184).
Although it may seem like a dubious blessing, consider yourself lucky that your baby sleeps for long stretches—even if it is during the day. It’s a good sign that she’s capable of sleeping well and that once she’s got her internal clock set correctly, she will sleep well at night.
“I have a friend who turns off the phone when her son is sleeping, has a note on the door asking people to knock instead of ring, and tiptoes around the apartment at naptime. Is this a good idea?”
By attempting to turn off all the sound in her baby’s life, your friend is programming him to be able to sleep only under controlled conditions. The problem is, this programming, though well intentioned, will probably make it difficult for her child to get a good night’s shut-eye later on in life when he has to sleep in the real world—a world where phones and doorbells ring.
And what’s more, her efforts will probably be counterproductive. Though a sudden loud sound may waken some babies, others can sleep through fireworks, wailing sirens, and barking dogs. For most, however, a steady hum of background noise—from a TV or stereo, a fan or air conditioner, a musical toy or one that imitates uterine sounds, or from a white-noise machine—appears to be more conducive to restful sleep than perfect silence, particularly if the baby has fallen asleep to the beat of such sounds.
Just how much noise, as well as what kinds of noise, a baby can sleep through depends partly on the sounds he became accustomed to before birth and partly on individual temperament (some babies are much more sensitive to stimulus than others). So parents have to take their cues from their babies in determining how far they must go to protect them from noise during naps and at night. If a baby turns out to be especially sound-sensitive during sleep, it’s probably wise to turn the phone down to low, to change the doorbell to a less abrasive ring, and to play the radio or TV more softly. Such tactics are unnecessary, however, if a baby sleeps through everything.
“Every time I watch my newborn sleep, her breathing seems irregular, her chest moves in a funny way, and frankly it frightens me. Is something wrong with my baby?”
No, your baby is perfectly normal—and you are, too, for worrying (and for standing over her crib watching her breathing—something most new parents do frequently in the first few weeks of their babies’ lives; see next question).
A newborn’s normal breathing rate is about forty times each minute during waking hours; when your baby sleeps, however, it may slow down to as few as twenty times per minute. But what’s alarming you—and what often alarms new parents—is how irregular an infant’s breathing pattern is while she’s sleeping. Your baby might breathe fast, with repeated rapid and shallow breaths, lasting 15 to 20 seconds, and then pause (that is, stop breathing—and this is where it gets really scary), usually for less than 10 seconds (though it might seem forever to you), and then, after that brief respiratory respite, breathe again (which is generally when her parents can start breathing again, too). This type of breathing pattern, called periodic breathing, is normal and is due to your baby’s immature (but, for her age, developmentally appropriate) breathing control center in the brain.
You may also notice your baby’s chest moving in and out while she is sleeping. Babies normally use their diaphragm (the large muscle below the lungs) for breathing. As long as your baby shows no blueness around the lips and resumes normal shallow breathing without any parental intervention, you have nothing to worry about.
Half of a newborn’s sleep is spent in REM (rapid eye movement) sleep, a time when she breathes irregularly, grunts and snorts and twitches a lot—you can even see her eyes moving under the lids. The rest of her slumber is spent in quiet sleep, when she breathes very deeply and quietly and seems very still, except for occasional sucking motions or startling. As she gets older, she will experience less REM sleep, and the quiet sleep will become more like the non-REM sleep of adults.
In other words, what you’re describing is normal baby breathing. If, however, your baby takes more than sixty breaths per minute, flares her nose, makes grunting noises, looks blue, or sucks in the muscles between the ribs with each breath so that her ribs stick out, call the doctor immediately.
“Everybody always jokes about sneaking into the baby’s room to hear if he’s breathing. Well, now I find myself doing just that—even in the middle of the night.”
Anew parent neurotically checking a baby’s breathing does seem like good comic material—until you become a new parent. And then it’s no laughing matter. You wake in a cold sweat to complete silence after putting baby to bed five hours earlier. Could something be wrong? Why didn’t he wake up? Or you pass his crib and he seems so silent and still that you have to poke him gingerly to be sure he’s okay. Or he’s grunting and snorting so hard you’re sure he’s having trouble breathing. You … and millions of other new parents.
Whether a good sleeper or a not so good one, your baby can be helped to sleep to potential with some or all of the following sleep enhancers, many of which help re-create some of the comforts of home in the womb:
Cozy sleeping space. A crib is a great modern invention—but in the early weeks many newborns somehow sense its vastness and balk when sentenced to solitude, smack in the center of its mattress, so clearly removed from its distant walls. If your baby seems uncomfortable in the crib, a cradle, a bassinet, or a baby carriage can be used for the first few months to provide a snugger fit that’s closer to the nine-month-long embrace in the uterus. For added security, swaddle your infant (but not once he or she becomes more active; see page 150), or use a baby sleeping bag.
Controlled temperature. Being too warm or too cold can disturb a baby’s sleep. For tips on keeping baby comfortable in warm and cold weather, see pages 508 and 517.
Soothing movement. In the uterus, babies are most active when their mothers are at rest; when their mothers are up and on the go, they slow down, lulled by the motion. Out of the womb, movement still has a soothing effect. Rocking, swaying, and patting will help get your baby to sleep.
Soothing sound. For many months, your heartbeat, the gurgling of your tummy, and your voice entertained and comforted your baby. Now sleeping may be difficult without some background noise. Try the hum of a fan, the soft strains of music from a radio or stereo, the tinkling of a music box or musical mobile, or one of those baby soothers that imitate uterine or heartbeat sounds.
A peaceful place. Babies sleep better when they are in a room of their own, not because they’re disturbed by your presence but because you’re more likely to pick them up at the least little whimper—breaking up their sleep unnecessarily. So unless you’re planning on co-sleeping and/or can stop yourself from picking up your baby at any toss or turn, keep baby in his or her own room, if possible. You should, however, be close enough to hear your baby’s cries before they turn into frantic ear-piercing wails—or use an intercom between baby’s room and yours.
Routine. Since your newborn will fall asleep most of the time while nursing or bottle feeding, a bedtime routine might seem unnecessary. But it’s never too early to begin such a routine, and certainly by the age of six months it should top off every evening. The ritual of a warm bath, followed by being dressed in nightclothes, a little quiet playtime on your bed, a singsong story or nursery rhyme from a picture book, can be soothing and soporific for even the youngest babies. The breast or bottle can be last on the agenda for babies who still fall asleep that way, but can come earlier for those who have already learned to doze off on their own.
Adequate daytime rest. Some parents try to solve nighttime sleeping problems by keeping their babies awake during the day, even if the baby wants to sleep. This is a big mistake (though it’s all right to limit the length of daytime naps a little to maintain the contrast between day and night), because an overtired baby sleeps more fitfully than a well rested one.
Seeing the light of day. Infants exposed to afternoon sunlight tend to have a much better night’s sleep, so try an after-lunch stroll.
Not only are your concerns normal, but your baby’s varied breathing patterns when he snoozes are, too. You will eventually become less panicky about whether he’s going to wake up in the morning, and more comfortable with both you and him sleeping eight hours at a stretch.
Still, you may never totally be able to abandon the habit of checking on your child’s breathing (at least once in a while) until he’s off to college and sleeping in a dorm—out of sight, though not out of mind.
“I’m a nervous wreck when I try to put my sleeping baby down in her crib. I’m always afraid she’ll wake up—and she usually does.”
She’s finally asleep—after what seems like hours of nursing on sore breasts, rocking in aching arms, lullabying in an increasingly hoarse voice. You rise ever so slowly from the glider and edge cautiously to the crib, holding your breath and moving only the muscles that are absolutely necessary. Then, with a silent but fervent prayer, you lift her over the edge of the crib and begin the perilous descent to the mattress below. Finally, you release her, but a split second too soon. She’s down—then she’s up. Turning her head from side to side, sniffing and whimpering softly, then sobbing loudly. Ready to cry yourself, you pick her up and start all over.
The scenario’s the same in almost every home with an infant. If you’re having trouble keeping a good baby down, wait ten minutes until she’s in deep sleep, then try:
A high mattress. If you were a gorilla, you might be able to set your baby down in a crib with a low mattress without having to scale the rail or, alternatively, drop her the last 6 inches. Since you’re only human, you will find it much easier if you set the mattress at the highest possible level (at least 4 inches from the top of the rail); just be sure to lower it by the time your baby is old enough to sit up. If your crib has the option, lower the side rail before putting baby down to avoid having to bend over a high railing. Or, for the first few weeks, use a crib substitute such as a carriage, bassinet, or cradle, all of which may be easier to lift a baby into and out of. Often these offer the important plus of being rockable, so the rocking motion that started in your arms can continue after you bed baby down.
A little light. Though it’s a good idea to get baby to sleep in a darkened room, be sure there’s enough light (a night-light will do) for you to see your way to the crib without bumping into a dresser or tripping over a toy—which is sure to jar you, and your baby.
Close quarters. The longer the distance between the place where baby falls asleep and the place where you are going to put her down, the more opportunity for her to awaken on the way. So feed or rock her as close to the cradle or crib as possible.
A seat you can get out of. Always feed or rock your baby in a chair or sofa that you can rise from smoothly, without disturbing her.
The right side. Or the left. Feed or rock baby in whichever arm will allow you to put her in the crib most easily. If she falls asleep prematurely on the wrong arm, gently switch sides and rock or feed some more before attempting to put her down.
Constant contact. When baby is comfortable and secure in your arms, suddenly being dropped into open space, even for an inch or two, startles—and awakens. Cradle baby all the way down, back first, easing your bottom hand out from under just before you reach the mattress. Maintain a hands-on pose for a few moments longer, gently patting if she starts to stir.
A lulling tune. Hypnotize your baby to sleep with a traditional lullaby (she won’t object if you’re off-key) or an improvised one with a monotonous beat (“aah-ah aah-ah ba-by, aah-ah aah-ah ba-by”). Continue as you carry her to her crib, while you’re putting her down, and for a few moments afterward. If she begins to toss, sing some more, until she’s fully quieted.
“We congratulated ourselves in the hospital on having such a good baby. We were home hardly a week when she started howling.”
If one- and two-day-old babies cried as much as they were destined to a couple of weeks later, new parents would doubtless think twice about checking out of the hospital with their newborns. Once they’re safely ensconced at home, babies don’t seem to hesitate to show their true colors, with all doing some crying, and many doing a considerable amount. Crying is, after all, the only way infants have of communicating their needs and feelings—their very first baby talk. Your baby can’t tell you that she’s lonely, hungry, wet, tired, uncomfortable, too warm, too cold, or frustrated any other way. And though it may seem impossible now, you will soon be able (at least part of the time) to decode your baby’s different cries and know what she’s asking for (see page 123).
Some newborn crying, however, seems entirely unrelated to basic needs. Eighty to 90 percent of all babies, in fact, have daily crying sessions of from fifteen minutes to an hour that are not easily explained. These periodic crying spells, like those associated with colic, a more severe and persistent form of unexplained crying, most often occur in the evening. It may be that this is the most hectic time of day in the home, with dinner being prepared, parents and siblings coming home from work and school, the family trying to eat, other children, if any, vying for attention; the hustle-bustle may be more than the baby can tolerate. Or it may be that after a busy day of taking in and processing all the sights, sounds, smells, and other stimuli in her environment, a baby just needs to unwind with a good cry.
Some perfectly happy babies seem to need to cry themselves to sleep, possibly because of fatigue. If your baby cries for a few minutes before nodding off, don’t be concerned. She will eventually outgrow this. What may help is a regular prebedtime ritual and enough rest during the day so she isn’t overtired at night.
Meanwhile, hang in there. Though you’ll be drying some tears for the next eighteen years or so, these probably tearless newborn crying spells are likely to be a thing of the past by the time your baby is three months old. As she becomes a more effective communicator and a more self-reliant individual, and as you become more proficient at understanding her, she will cry less often, for shorter periods, and will be more easily comforted when she does cry.
A sudden bout of crying, however, in a baby who hasn’t cried a lot before could signal illness or early teething. Check for fever and other signs that baby isn’t well or might be teething, and call the doctor if you note anything out of the ordinary.
“My spouse and I haven’t had dinner together since our baby was three weeks old. We have to take turns gulping our food and carrying him around while he cries for hours every evening.”
For the parents of a colicky baby, even a steak dinner becomes fast food, choked down to the accompaniment of indigestion-provoking screams. That the doctor promises baby will outgrow colic offers little consolation for their misery.
And if misery likes company, parents of colicky babies have plenty of it. It’s estimated that one in five babies have crying spells, usually beginning in late afternoon and sometimes lasting until bedtime, that are severe enough to be labeled colic. Colic differs from ordinary crying (see previous question) in that the baby seems inconsolable, crying turns to screaming, and the ordeal lasts for three hours, sometimes much longer, occasionally nearly round-the-clock. Most often colicky periods recur daily, though some babies take an occasional night off. Doctors usually diagnose colic based on the “rules of three”: at least three hours of crying, at least three days a week, lasting for at least three weeks.
The baby with a textbook case of colic pulls his knees up, clenches his fists, and generally increases his activity. He closes his eyes tightly or opens them wide, furrows his brow, even holds his breath briefly. Bowel activity increases and he passes gas. Eating and sleeping patterns are upset by the crying—the baby frantically seeks a nipple only to reject it once sucking is begun, or dozes for a few moments only to awaken screaming. But few infants follow the textbook description exactly. No two babies experience exactly the same pattern and intensity of crying and associated behavior, and no two parents respond in exactly the same way.
Colic generally begins during the second or third week of life (later in preterm infants), and usually gets as bad as it’s going to get by six weeks. For a while, colic seems as though it will stretch on interminably, but by twelve weeks, it usually begins to diminish, and at three months (again, later in preterm babies) most colicky infants appear miraculously cured—with just a few continuing their problem crying through the fourth or fifth month. The colic may abate suddenly or gradually, with some good and some bad days, until they are all good.
Though these daily screaming periods, whether marathon or of more manageable duration, are usually dubbed “colic,” there is not a clear definition of exactly what colic is or how it differs, if it does, from other types of problem crying. Definitions and differences, however, matter very little to parents who are desperately trying to calm their infant during these prolonged crying spells.
What causes colic remains a mystery. Theories, however, abound. Many of the following now have been totally or partially rejected: Colicky babies cry to exercise their lungs (there is no medical evidence of this); they cry because of gastric discomfort triggered by allergy or sensitivity to something in their mothers’diets if they are breastfeeding or in their formula if they are bottle-fed (this is only occasionally a cause of colic); they cry because of parental inexperience (colic is no less common in second or subsequent babies, though parents may handle the crying with more aplomb); colic is hereditary (it does not appear to run in families); colic is more common in babies whose mothers had complications in pregnancy or childbirth (statistics don’t bear this out); exposure to fresh air stirs up colic (in practice, many parents find that fresh air is the only way they can quiet their crying babies).
The latest research seems to point to a number of potential reasons why colic may occur in some babies:
 Overload. For the first few weeks of life, babies are able to block out the extraneous stimuli in their environment, probably so they can focus on sleeping and eating. Once they become more aware of the world around them, they sometimes take in more stimuli than they can handle. Bombarded all day long with sensations (new sounds, sights, and smells), they can reach the early evening hours at sensory overload—overstimulated and overwhelmed. The result in babies who are particularly sensitive to stimuli (in some cases because they’re extra alert): lots of crying, and sometimes colic. Fortunately, once babies acquire the ability to tune out the environment before overload occurs (usually by three months, occasionally not until five), bouts of colic end. In the meantime, if you think this might be the cause of your baby’s colic, the try-everything approach (rocking, bouncing, driving, swinging, singing) may actually make things worse. Instead, watch how your baby responds to certain stimuli and steer clear of the offending ones (if baby cries harder when you rub or massage him, limit that kind of touching during colic; instead, try swinging him in a swing once he’s old enough; see page 335).
Overload. For the first few weeks of life, babies are able to block out the extraneous stimuli in their environment, probably so they can focus on sleeping and eating. Once they become more aware of the world around them, they sometimes take in more stimuli than they can handle. Bombarded all day long with sensations (new sounds, sights, and smells), they can reach the early evening hours at sensory overload—overstimulated and overwhelmed. The result in babies who are particularly sensitive to stimuli (in some cases because they’re extra alert): lots of crying, and sometimes colic. Fortunately, once babies acquire the ability to tune out the environment before overload occurs (usually by three months, occasionally not until five), bouts of colic end. In the meantime, if you think this might be the cause of your baby’s colic, the try-everything approach (rocking, bouncing, driving, swinging, singing) may actually make things worse. Instead, watch how your baby responds to certain stimuli and steer clear of the offending ones (if baby cries harder when you rub or massage him, limit that kind of touching during colic; instead, try swinging him in a swing once he’s old enough; see page 335).
 Immature digestion. Another theory is that a baby’s immature digestive tract contracts violently when gas is passed, causing pain and, not surprisingly, lots of crying. When gas seems to be pulling the colic trigger, there are medications that may help (see page 190).
Immature digestion. Another theory is that a baby’s immature digestive tract contracts violently when gas is passed, causing pain and, not surprisingly, lots of crying. When gas seems to be pulling the colic trigger, there are medications that may help (see page 190).
 Reflux. Recent research has found that one common cause of colic is reflux. This form of reflux irritates the esophagus (much like heartburn in an adult), causing discomfort and crying. If reflux seems to be the cause of the colic in your baby, some of the treatment tips on page 558 may help.
Reflux. Recent research has found that one common cause of colic is reflux. This form of reflux irritates the esophagus (much like heartburn in an adult), causing discomfort and crying. If reflux seems to be the cause of the colic in your baby, some of the treatment tips on page 558 may help.
 Environment. One factor that does seem to contribute to an increase in colicky behavior, though the reason for it isn’t clear, is tobacco smoke in the home. And the more smokers in a household, the greater the likelihood of colic and the worse the colic will be.
Environment. One factor that does seem to contribute to an increase in colicky behavior, though the reason for it isn’t clear, is tobacco smoke in the home. And the more smokers in a household, the greater the likelihood of colic and the worse the colic will be.
 Milk supply problems. Insufficient milk or other breastfeeding problems is another possible cause of colic. Milk supply often diminishes in the early evening, just the time when the baby starts crying. If this is the cause of your baby’s colic, improved breastfeeding technique or supplementation with pumped milk usually corrects the problem.
Milk supply problems. Insufficient milk or other breastfeeding problems is another possible cause of colic. Milk supply often diminishes in the early evening, just the time when the baby starts crying. If this is the cause of your baby’s colic, improved breastfeeding technique or supplementation with pumped milk usually corrects the problem.
 Parental tension. The theory that babies are colicky because their parents are tense is a more controversial one. Though many experts believe it’s more likely that it’s the baby’s crying that makes a parent tense, some insist that a parent who is very anxious may unconsciously communicate this to the baby, making him cry. It may be that although parental anxiety doesn’t cause colic, it can make it worse.
Parental tension. The theory that babies are colicky because their parents are tense is a more controversial one. Though many experts believe it’s more likely that it’s the baby’s crying that makes a parent tense, some insist that a parent who is very anxious may unconsciously communicate this to the baby, making him cry. It may be that although parental anxiety doesn’t cause colic, it can make it worse.
What’s reassuring about colic is that babies who have these crying spells do not seem to be any the worse for the wear (though the same can’t always be said for their parents), either emotionally or physically—they thrive, usually gaining as well as or better than babies who cry very little, and display no more behavioral problems than other children later on. Children who cry vigorously as infants appear, in fact, more likely to be vigorous and active problem solvers as toddlers than those with limp cries. And most reassuring of all is the certainty that the condition won’t last forever. In the meantime, the tips on the following pages should help you deal with the problem. (See page 738 if you have an older child who’s having trouble coping with baby’s colic.)
“This is our first baby and she cries all the time. What are we doing wrong?”
Relax. You’re not guilty. The theory that a baby’s colic is somehow the fault of the parents just hasn’t held up. And, in fact, your baby would probably be doing just as much crying if you were doing everything right (which, of course, no human parent does, even with the benefit of experience). Colic, the latest research indicates, has to do with baby’s development and not yours.
The “rightest” thing you can do is to try to cope with your baby’s crying as calmly and rationally as possible, since your tenseness will only compound your baby’s. Keeping your cool in the face of colicky fire isn’t easy, but knowing that you’re not at fault can help. So can the tips you’ll find in the next answer.
“Sometimes when I’m rocking the baby through his third hour of colic, and he won’t stop screaming, I have this terrible urge to throw him out the window. Of course I don’t—but what kind of parent am I to even think such a thing?”
You’re a perfectly normal one. Even those otherwise qualified for sainthood couldn’t survive the agony and frustration of living with a baby who won’t stop crying without experiencing some feelings of anger—even fleeting animosity—toward him. And though few would admit it freely, many parents of chronic criers regularly have to fight off the same kinds of horrifying impulses you’ve been feeling. (If you find such feelings are more than momentary, and/or if you’re afraid that you might really hurt your baby, get help immediately.)
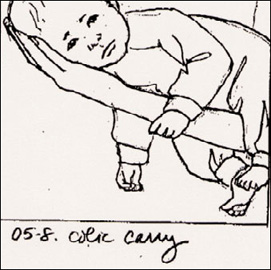
The colic carry. Some colicky babies are soothed by the pressure applied to their abdomen when they are carried in this position.
There’s no question that parents get the worst of colic. Though it can safely be said that the crying doesn’t seem to hurt baby, it certainly does leave its mark on mom and dad. Listening to a crying baby is irritating and anxiety-provoking. Objective studies show that everyone, even a child, responds to the constant crying of a young infant with a rise in blood pressure, a speeding up of the heartbeat, and changes in blood flow to the skin. If the baby was born prematurely, was poorly nourished in the uterus, or if the mother had toxemia (preeclampsia/eclampsia), the pitch of his cry may be unusually high and particularly hard to tolerate.5
In order to survive the two or three months of colicky behavior with some semblance of sanity, try the following:
Take a break. If you’re the one who’s been left holding the crying baby seven nights a week at colic time, the strain is going to take its toll not only on your parenting but on your health and your relationship with your spouse as well. So if there are two parents at home, make sure colic duty is divided up equally between the two of you (an hour on, an hour off, a night on, a night off; or whatever arrangement you find works best). A fresh set of arms (and a different rocking rhythm) sometimes even induces calm in a crying baby, which may make switching off frequently your best bet.
The desperate parent of a colicky baby often turns to the physician for a magic potion (or, failing that, a prescription) to stop the crying. Unfortunately, there is no medicine that is known to completely cure colic in all infants, and because all prescription medications have side effects, most doctors prefer not to pick up their prescription pad routinely when treating these chronic criers. There is, however, one medicine for infants, widely used to treat colic in Europe, that is sold over-the-counter here for gas and that may reduce or alleviate symptoms in some colicky babies. Its active ingredient is simethicone, the same antigas ingredient found in many adult preparations.
Though there is no clear scientific consensus that gas is the cause of infant colic, it is recognized that many colicky infants do seem gassy (whether this is a cause of the crying or an effect isn’t clear), and studies show that reducing the gas may reduce the discomfort (and the crying). Because the body doesn’t absorb the product, it is completely safe and has no side effects. If your colicky baby seems gassy, ask the doctor about simethicone drops. They are available under such brand names as Mylicon and Phazyme.
There are also herbal remedies such as “gripe waters” or fennel tea that have been touted as cures for colic. Some pediatricians say they are perfectly safe and effective, others caution that there is no way to know if the ingredients are safe for infants, because they are not regulated by the Food and Drug Administration. Do not give your baby any medication, herbal or otherwise, without talking to your baby’s doctor.
Then, make sure that you both take a break together occasionally—preferably at least once a week. Rely on paid help (but make sure you hire someone who is endlessly patient and experienced with crying babies), or impose on relatives or friends (but not relatives or friends who drop direct or indirect hints that the crying is your fault—it isn’t). Go out to dinner (even if you’re breastfeeding, you should be able to squeeze in a restful meal at a local restaurant), visit with friends, go to the gym, get a couple’s massage, or just take a long, quiet walk.
If you’re the only parent in the house (either all or some of the time), you’ll need to call on help even more often; coping with a crying infant for hours a day every day is more than anyone can handle alone. Again, look to a baby-sitter, if you can afford one, a willing relative or friend (grandparents sometimes have a magical touch with fussy babies; friends who’ve been there and done that with their own children can offer perspective and experience). Even a young teenager whom you wouldn’t consider leaving alone with your colicky infant can hold him or push him in the stroller while you take a break nearby.
Give baby a break. Sure, it’s important to respond to baby’s crying, which is an infant’s sole form of communication. But once you’ve met all his needs (feeding, burping, changing, comforting, and so on) without perceptibly altering his level of screaming, you can give him a break from you—by putting him down in his crib or bassinet (on his back) for a little while. It won’t hurt him to cry in his bed instead of your arms for ten or fifteen minutes while you do something relatively relaxing, such as lying down; checking e-mail; doing some yoga, visualization, or meditation; watching television; or reading a few pages of a book (see Tune Out, below). In fact, it will do him good if you’re a little less ragged and a little more refreshed when you pick him up again where you left off.
Tune out. To lessen the impact of your baby’s wails, use earplugs—they won’t block out the sound entirely, just dull it so it will be more tolerable. Tucked in your ears, they can help you relax during a break from baby, or even while you’re walking the floor with him. Or drown out the racket by listening to music on a portable CD player.
Get physical. Exercise is a great way to work off tension, something you’ve got plenty of. Work out at home with baby early in the day (see page 684), swim or exercise at a health club (wallop a punching bag if they have one) that has childcare services, or take the baby for a brisk walk outdoors in his carriage when he’s fussy (which may help calm him while it calms you).
Talk about it. Do a little crying yourself—on any willing shoulder: your spouse’s, the baby’s doctor’s, your own doctor’s, a family member’s, a friend’s, even a stranger in a parenting chat room. Talking about it may not cure the colic, but you may feel a little better after sharing your saga. Most beneficial may be discussing your situation with other parents of colicky babies, particularly those who have weathered the storm successfully and are now sailing on clear waters; you may find some who are—or have been—in the same boat as you in parenting chat rooms. Just knowing you’re not alone in the world of inconsolable babies can make a world of difference.
If you really feel violent, get help. Almost everyone is irritated by a constantly crying baby. But for some people, such crying finally becomes more than they can bear. The result is sometimes child abuse. You may be even more likely to cross that line if you’re suffering from untreated (and possibly undiagnosed) postpartum depression (see page 672). If your thoughts of hurting your baby are more than fleeting, if you feel about to give in to the urge to strike or shake your baby or harm him in any way, get help immediately. Go to a neighbor’s, if you can, and hand the baby over until you can collect yourself. Then call someone who can help you—your spouse, a relative, a close friend, the baby’s doctor or your own, or the local child-abuse hotline (the number should be listed inside the cover of your local classified directory). Even if your powerful feelings don’t lead to child abuse, they can start eroding your relationship with your baby and your confidence in yourself as a parent unless you get counseling (and if you’re suffering from postpartum depression or psychosis, appropriate treatment) quickly.
“We always pick our baby up when she cries. Are we spoiling her?”
Not sparing the comfort won’t spoil the baby. In fact, studies show pouring on the comfort now—by picking her up within a couple of minutes whenever she cries and catering to all her needs—not only won’t turn out a spoiled brat, it will turn out a happy, more self-reliant child who in the long run will cry less and demand less attention. She will also have a closer attachment to you (or to whoever it is who responds to her) and be more trusting. An additional plus: Since she’ll come calmly to breast or bottle, without a bellyful of air swallowed while screaming, she will have better feeding sessions.
No medication, pharmaceutical or herbal remedy, or treatment approach is a sure cure for a baby’s crying, and some may actually worsen it. To complicate matters more, what may be soothing to one baby may step up squalling in another. But there are a number of strategies that may work—at least some of the time. When trying out various methods of baby calming, stick to one at a time, being sure to give each a fair trial before switching to another—otherwise, you may find you are trying, trying, trying and baby is crying, crying, crying. Here are a few tricks you can pull out of your parental hat the next time the crying starts:
Respond. Crying is your baby’s only way of wielding any control over a vast and bewildering new environment, of communicating, of making things happen: “When I call, someone answers.” If you regularly fail to respond, the baby may feel not only powerless but also worthless (“I’m so unimportant that no one comes when I call”). Though it may sometimes seem that you’re responding in vain because no matter what you do, nothing helps, responding promptly to your baby’s calls will eventually reduce crying. And, in fact, studies show that babies whose parents responded to them regularly and promptly in infancy cry less as toddlers. In addition, crying that’s been left to intensify for more than a few minutes becomes harder to interpret—the baby becomes so upset, even he or she doesn’t remember what started all the fuss in the first place. And the longer baby cries, the longer it takes to stop the crying. Of course, you don’t always have to drop everything to answer baby’s call if you’re in the middle of taking a shower, draining the spaghetti, or answering the doorbell. Baby’s being left to cry for a couple of extra minutes now and then won’t prove harmful—as long as the infant can’t get into trouble while waiting for you. A ten- or fifteen-minute break taken from a colicky marathon of crying won’t hurt baby, either—again, as long as he or she is in a safe place. (For particularly difficult cases of inconsolable crying, some experts suggest setting up a routine in which you let baby cry for ten or fifteen minutes in a safe place like his crib, pick him up and try to soothe him for another fifteen minutes, then put him down and repeat. If you’re comfortable with this, it apparently won’t cause any problems.)
Don’t worry about spoiling your baby by responding promptly. You can’t spoil a young infant. And more attention doesn’t lead to increased dependency. In fact, quite the opposite is true: Babies whose needs are readily met are likely to grow into more secure and less demanding children.
Assess the situation. Before deciding your baby is crying just for crying’s sake, determine if there’s a simple and remediable underlying cause. If you think it may be hunger, try breast or bottle, but don’t make the mistake of invariably responding to tears with food. Even at this tender age, food should be a response to a need for food, not attention or comfort. If you suspect fatigue, try rocking baby to sleep—in your arms, a carriage, a cradle, or a baby carrier. If a wet diaper may be triggering the crying, change it. If baby seems too warm (perspiration is a clue), take off a layer or two of clothing, open the window, or turn on a fan or air conditioner. If cold may be the problem (neck or body feels cold to the touch), add a layer or turn up the heat. If baby began to cry when clothes were stripped off for a bath (most newborns dislike being naked), quickly cover him with a towel or blanket. If you think baby’s being in the same position for too long may be causing discomfort, try a new position. If he’s been staring at the same view for the last half hour, try changing it. If you’ve been inside all day, venture outside (weather permitting).
Get close. In societies where babies are carried papoose style, long periods of crying or fussiness in healthy children are unknown. This traditional wisdom seems to translate well in our culture, too; research has shown that babies who are carried in the arms or in a baby carrier for at least three hours every day cry less than babies who aren’t carried as often. Not only does carrying your baby give him or her the pleasure of physical closeness to you (and after nine months of constant closeness, that may be just what baby’s crying for), but it may help you tune in better to baby’s needs.
Swaddle. Being tightly wrapped is very comforting to some young infants, at least during times of colicky distress. A few, however, intensely dislike swaddling; the only way you’ll know which holds true for your baby is to give swaddling a try the next time colic begins (see page 150).
Give a cuddle. Like swaddling, cuddling gives many babies a sense of security; hold baby pressed close to your chest, encircled snugly by your arms. (And, as with swaddling, some babies prefer more freedom of movement and will balk at being held tightly.)
Try a little comfort. Comfort for a newborn comes in different packages. In addition to holding, wearing, and cuddling your baby, try any or all of the following:
 Rhythmic rocking, in your arms, a carriage, a cradle, a vibrating infant seat, automatic baby swing (when baby’s old enough; see page 135). Some babies respond better to fast rocking than to slow—but don’t rock or shake your baby vigorously, since this can cause serious whiplash injury. For some babies, rocking side to side tends to stimulate, rocking back and forth to calm. Test your baby’s response to different kinds of rocking.
Rhythmic rocking, in your arms, a carriage, a cradle, a vibrating infant seat, automatic baby swing (when baby’s old enough; see page 135). Some babies respond better to fast rocking than to slow—but don’t rock or shake your baby vigorously, since this can cause serious whiplash injury. For some babies, rocking side to side tends to stimulate, rocking back and forth to calm. Test your baby’s response to different kinds of rocking.
 Walking the floor with baby in a carrier or swing, or simply in your arms. Tried and true, it’s tiring but it often works.
Walking the floor with baby in a carrier or swing, or simply in your arms. Tried and true, it’s tiring but it often works.
 A warm-water bath. But only if your baby likes the bath; some babies only scream louder when they hit the water.
A warm-water bath. But only if your baby likes the bath; some babies only scream louder when they hit the water.
 Singing. Learn whether your baby is soothed by soft lullabies, sprightly rhymes, or pop tunes, and whether a light, high-pitched voice or a deep, strong one is more pleasing. If you hit on a tune your baby likes, don’t hesitate to sing it over and over—most babies love repetition.
Singing. Learn whether your baby is soothed by soft lullabies, sprightly rhymes, or pop tunes, and whether a light, high-pitched voice or a deep, strong one is more pleasing. If you hit on a tune your baby likes, don’t hesitate to sing it over and over—most babies love repetition.
 Rhythmic sounds. Many babies are calmed, for example, by the hum of a fan, vacuum cleaner, or clothes dryer, a tape recording of uterine gurglings, a parent’s repeated “sh” or a recording that plays soothing nature sounds, such as waves breaking on the beach or wind blowing through trees.
Rhythmic sounds. Many babies are calmed, for example, by the hum of a fan, vacuum cleaner, or clothes dryer, a tape recording of uterine gurglings, a parent’s repeated “sh” or a recording that plays soothing nature sounds, such as waves breaking on the beach or wind blowing through trees.
 Laying on the hands. For babies who like to be stroked, massage can be very calming (though it can cause increased screaming in those who don’t). You may find it relaxing to both of you to administer the massage lying on your back, baby facedown on your chest. (See page 304 for tips on baby massage.)
Laying on the hands. For babies who like to be stroked, massage can be very calming (though it can cause increased screaming in those who don’t). You may find it relaxing to both of you to administer the massage lying on your back, baby facedown on your chest. (See page 304 for tips on baby massage.)
Add a little pressure. On baby’s tummy, that is. The “colic carry” (see illustration, page 189) or any position that applies gentle pressure to baby’s abdomen (such as across an adult lap, with belly on one knee and head on the other), can relieve discomfort that might be contributing to the crying. Some babies prefer being upright on the shoulder, but again with pressure on their abdomens while their backs are being patted or rubbed. Or try this gas reliever: Gently push baby’s knees up to his or her tummy and hold for ten seconds, then release and gently straighten them; repeat several times.
Resort to ritualism. For babies who thrive on routine, having as regular a schedule as possible (feeding, bathing, changing, outing, and so on up to bedtime ritual) may reduce crying. If this seems to be the case with your baby (and you won’t know unless you check the theory out), be consistent even to the method you use for soothing baby or reducing crying—don’t go for a walk one day, ride around in the car the next, and use a baby swing the third. Once you find what works, stick with it most of the time.
Satisfy with sucking. Babies often need sucking for its own sake, rather than simply for nourishment. Some babies appreciate your help in getting their fingers (particularly their thumbs) to their mouths for their sucking enjoyment. Others prefer grownup pinkies. Still others find pleasure in a pacifier (as long as you give it only to calm baby after you’ve attended to other needs and once breastfeeding is well established).
Start fresh. A parent who’s been struggling for an hour to soothe a sobbing newborn will almost invariably start to show signs of stress and fatigue, which the infant is certain to sense and respond to with more crying. Hand baby over to another pair of arms for a fresh start—the other parent’s, a relative’s or friend’s, a sitter’s—and the crying may cease.
Seek fresh air. A change to an outdoor locale will often miraculously change a baby’s mood. Try a trip in the car, the baby carrier, or the stroller. Even if it’s dark out, baby’s sure to find distraction in the twinkling of street and car lights. The motion will also almost certainly prove soothing. (If crying doesn’t stop during a car ride, it can distract the driver—in that case, head home and try another trick.)
Control air. A lot of newborn discomfort is caused by swallowing air. Babies will swallow less of it if they’re properly latched on during breastfeeding or slightly upright during bottle feeding. The right-size nipple hole on a bottle will also reduce air intake; be sure it isn’t too large (which promotes gulping of air with formula) or too small (struggling for formula also promotes air swallowing). Hold the bottle so that no air enters the nipple (or use an angled bottle or one with disposable liners), and be sure the formula is neither too hot nor too cold (though most babies do fine with unheated formula, a few seem disturbed by it). Be sure to burp baby frequently during feedings to expel swallowed air. One suggested pattern for burping: every half-ounce or every ounce when bottle feeding, between breasts when breastfeeding (or more often if baby seems to be gulping a lot or seems in discomfort mid-breast), and, in both cases, after feeding.
Be entertaining. In the early months, some infants are content to sit and watch the world go by, while others cry out of frustration and boredom because there is, as yet, so little they are able to do on their own. Toting them around and explaining what you’re doing as you go about your business, and making an extra effort to find toys and other objects in the environment for them to look at and later swat at and play with, may help keep them busy. On the other hand, an overstimulated baby may be more prone to crying, so know when to stop sending in the clowns and start bringing on the quiet comfort.
Excise excitement. Having a new baby to show off can be fun—everyone wants to see the baby, and you want to take him or her everywhere to be seen. You also want to expose baby to new experiences, to stimulating environments. That’s fine for some babies, too stimulating for others (particularly young ones). If your baby is colicky, limit excitement, visitors, and stimulation, especially in the late afternoon and evening.
Do a diet check. Be sure your baby isn’t crying because of hunger. Lack of adequate weight gain or signs of failure to thrive (see page 167) can clue you in. Increasing baby’s intake may eliminate the crying. If baby is bottle fed, ask the doctor whether the crying might be due to an allergy to the formula (though this isn’t a likely scenario unless crying is accompanied by other signs of allergy). If you’re breastfeeding, you might consider doing a check of your own diet, since there’s the very slight possibility that the crying might be triggered by baby’s sensitivity to something you’re eating. See pages 176 and 177 if you suspect allergy.
Check with the doctor. While the odds are that your baby’s daily screaming sessions are due to normal crying or colic, it’s a good idea to discuss it with the doctor to make sure there’s no underlying medical problem. Describe to the pediatrician the crying, its duration, intensity, pattern, and any variation from the norm—all aspects that may provide clues to an illness.
Look for relief. This is one time it doesn’t make sense to say, “I’d rather do it myself.” Take advantage of any and every possibility for sharing the burden.
Wait it out. Sometimes nothing relieves colic but the passing of time. Living with it will be a struggle, but it may help to remind yourself (over and over and over again): This, too, shall pass—usually by the time baby’s three months old.
Realistically, you won’t always be able to pick up your baby the moment she starts crying (there will be times when you’re in the bathroom, on the phone, or taking dinner out of the oven). And there will be times when you’ll need to take a break during colicky crying. Again, no harm done—as long as you’re responding promptly most of the time.
“My baby has crying jags in the afternoon. Should I give him a pacifier to comfort him?”
It’s easy, it’s quick, and for many babies it turns on the comfort and turns off the tears more reliably than a dozen hoarse choruses of “Rockabye Baby.” Yet is the pacifier the perfect panacea for crying babies that weary parents like you are searching for?
Probably not. Though it may come in handy in the short term (and may be nothing short of indispensable for babies who have a strong sucking need but haven’t yet figured out how to get their fingers in their mouths), the benefits of the pacifier don’t come without some drawbacks. Consider the following before deciding whether or not to pop a pacifier, and, if you do, when to begin and how long to use it:
 Pacifier use can interfere with long-term breastfeeding. Though research has concluded that offering a pacifier early on doesn’t cause nipple confusion or interfere with breastfeeding success in the first three months, there is clear evidence that pacifier use does shorten the duration of breastfeeding. What’s not clear is whether the pacifier itself is actually the cause of early weaning, or whether pacifier use is a marker of breastfeeding difficulties to begin with, or whether moms who rely on pacifiers to calm their babies are less likely to nurse frequently in general. Pacifiers shouldn’t be offered even early on, however, when a baby isn’t gaining weight at an adequate clip or is a poor nurser, since it may give him so much sucking satisfaction that he loses interest in nutritive suckling at the breast.
Pacifier use can interfere with long-term breastfeeding. Though research has concluded that offering a pacifier early on doesn’t cause nipple confusion or interfere with breastfeeding success in the first three months, there is clear evidence that pacifier use does shorten the duration of breastfeeding. What’s not clear is whether the pacifier itself is actually the cause of early weaning, or whether pacifier use is a marker of breastfeeding difficulties to begin with, or whether moms who rely on pacifiers to calm their babies are less likely to nurse frequently in general. Pacifiers shouldn’t be offered even early on, however, when a baby isn’t gaining weight at an adequate clip or is a poor nurser, since it may give him so much sucking satisfaction that he loses interest in nutritive suckling at the breast.
 The pacifier is in the parent’s control. That can be a good thing—as when you’ve fed, rocked, sung, and pushed the stroller for hours, yet nothing but plunking that pacifier in your baby’s mouth will generate calm. Or it can become a bad thing—as when plunking that pacifier in your baby’s mouth becomes just a little too easy, and when what starts out as baby’s crutch quickly becomes yours. The well-meaning parent who offers the pacifier to make sure his or her baby has adequate opportunity to suck may soon be finding it convenient to pop the pacifier the moment the baby becomes fussy, instead of trying to determine the reason for the fussing or if there might be other ways of placating him. A parent may use it to get the baby off to sleep instead of spending time cuddling, to ensure quiet while on the phone instead of picking him up and consoling him, to buy his silence while grocery shopping instead of involving him in the interaction. The result may be a baby who can be happy only with something in his mouth, and who is unable to comfort himself any other way.
The pacifier is in the parent’s control. That can be a good thing—as when you’ve fed, rocked, sung, and pushed the stroller for hours, yet nothing but plunking that pacifier in your baby’s mouth will generate calm. Or it can become a bad thing—as when plunking that pacifier in your baby’s mouth becomes just a little too easy, and when what starts out as baby’s crutch quickly becomes yours. The well-meaning parent who offers the pacifier to make sure his or her baby has adequate opportunity to suck may soon be finding it convenient to pop the pacifier the moment the baby becomes fussy, instead of trying to determine the reason for the fussing or if there might be other ways of placating him. A parent may use it to get the baby off to sleep instead of spending time cuddling, to ensure quiet while on the phone instead of picking him up and consoling him, to buy his silence while grocery shopping instead of involving him in the interaction. The result may be a baby who can be happy only with something in his mouth, and who is unable to comfort himself any other way.
 Pacifiers at night can mean less sleep for everyone. Used at bedtime, a pacifier can interfere with a baby’s learning to fall asleep by himself—which ultimately can mean less sleep all around the house. It can also interrupt his sleep when he loses it in the middle of the night and can’t get back to dreamland without it—who do you think will have to rise to put it back in his mouth?
Pacifiers at night can mean less sleep for everyone. Used at bedtime, a pacifier can interfere with a baby’s learning to fall asleep by himself—which ultimately can mean less sleep all around the house. It can also interrupt his sleep when he loses it in the middle of the night and can’t get back to dreamland without it—who do you think will have to rise to put it back in his mouth?
 Pacifiers can be a hard habit to break. Used temporarily, to satisfy the need for sucking when it’s at its most intense, a pacifier’s harmless—and can help parents and baby over what would otherwise be a tough time. Used longer, it can become addictive for both—and a habit that can be increasingly tricky to kick as a malleable baby turns into a fiercely inflexible toddler.
Pacifiers can be a hard habit to break. Used temporarily, to satisfy the need for sucking when it’s at its most intense, a pacifier’s harmless—and can help parents and baby over what would otherwise be a tough time. Used longer, it can become addictive for both—and a habit that can be increasingly tricky to kick as a malleable baby turns into a fiercely inflexible toddler.
In the long run, it’s probably better for babies to learn—at least to some extent—to comfort themselves (or to be comforted by their parents) than to rely often on artificial aids such as a pacifier. A thumb (or a fist) can do the job of providing extra sucking for comfort as well as a pacifier, but it’s in the baby’s control, not the parents’ (which may make it a harder habit to break). It’s there whenever he needs it; can be plucked out when he wants to smile, coo, cry, or otherwise express himself; and it won’t cause nipple confusion.
Still, if you’re desperate for some relief from your son’s crying, and the pacifier seems to do the trick—don’t hesitate to use it. Give it a try, too, if your child has such a strong sucking need that you’re finding your nipples have become human pacifiers (or baby is taking too much formula because he won’t let go of the bottle nipple). But use it wisely. Never attach a pacifier to the crib, carriage, playpen, or stroller, or hang it around your baby’s neck or wrist with a ribbon, string, or cord of any kind—babies can be strangled this way. Use it in moderation and only when your baby really seems to need it (each time you consider plugging it in, you might ask yourself first whether it’s you or the pacifier baby wants). And to avoid development of a habit that’s hard to break, plan to begin pulling the plug by the time he’s three to six months old. Another reason to wean from the pacifier sooner than later: Long-term use of a pacifier into the toddler years has been linked to recurrent ear infections and a higher risk of misaligned teeth later on.
“The cord still hasn’t fallen off my baby’s belly button, and it looks really awful. Could it be infected?”
Healing belly buttons almost always look and smell worse than they actually are. What constitutes “perfectly normal” in medical terms can actually send the weak-of-knee to the floor as fast as the climactic scene in a horror film.
Infection of the cord stump is unlikely, especially if you’ve been taking care to keep it clean and dry. (Some doctors still recommend using alcohol swabs to promote healing and prevent infection, but studies show that the cord heals as well, and, in some cases, even faster, without the alcohol). If you note redness in the surrounding skin (which could be due to irritation from alcohol applications as well as infection) or a discharge from the navel or from the base of the umbilical cord, particularly a foul-smelling one, check with your baby’s doctor. If infection is present, antibiotics will probably be prescribed to clear it up.
The cord, which is shiny and moist at birth, usually dries up and falls off within a week or two, but the big event can occur earlier, or even much later—some babies don’t seem to want to give them up. Until it does drop off, keep the site dry (no tub baths), exposed to air (turn diaper down so it doesn’t rub), and cleaned with alcohol if recommended (but try to protect the surrounding skin, perhaps coating with a baby lotion prior to swabbing or applying alcohol just to the base of the cord—not to the skin—with a cotton swab). When it does fall off, you might notice a small raw spot, or see a small amount of blood-tinged fluid oozing out. This is normal, and unless it doesn’t dry up completely in a few days, there is no need for concern. If it is not completely closed and dry two weeks after the stump falls off, call the pediatrician. Occasionally, an umbilical granuloma (a small piece of scar tissue that looks bright red and moist) can develop after the cord has fallen off. It’s usually treated with silver nitrate (to dry it out), tied off with a suture, and allowed to wither and drop off. If it doesn’t, it can be removed (a very minor procedure).
“Every time she cries, my baby’s navel seems to stick out. What does that mean?”
It probably means that your baby has an umbilical hernia—which (before you start worrying) is absolutely nothing to worry about.
Prenatally, all babies have an opening in the abdominal wall through which blood vessels extend into the umbilical cord. In some cases (for black babies more often than white), the opening doesn’t close completely at birth. When these babies cry, cough, or strain, a small coil of intestine bulges through the opening, raising the umbilicus and often the area around it, in a lump that ranges from fingertip to lemon size. While the appearance of such a lump (especially when it’s tagged with the term hernia) might be alarming, it’s rarely cause for concern. The intestine almost never strangulates (resulting in the blood supply to the intestine being cut off) in the opening, and in most cases, the hernia eventually resolves without intervention. Small openings usually close or become inconspicuous within a few months, large ones by age two.
The best treatment for an umbilical hernia is usually no treatment at all. Home remedies that press the lump down (such as bellybands or binders) are ineffective and in some cases potentially harmful. Surgery to correct umbilical hernias is not recommended unless the opening in the abdomen is very large, is growing larger, or bothers baby. Often the pediatrician will suggest waiting until the child is six or seven before considering surgery, because most hernias will have closed by then. If, however, you see signs of strangulation—the lump does not recede after crying, can’t be pushed in, suddenly becomes larger, is tender, baby is vomiting—go to the ER. Immediate surgery may be needed.
“My son was circumcised yesterday and there seems to be oozing around the area today. Is this normal?”
Not only is a little oozing normal, it’s a sign that the body’s healing fluids are heading to the site to begin their important work. Soreness and, sometimes, a small amount of bleeding are also common after a circumcision and nothing to be concerned about.
Using double diapers for the first day will help to cushion the penis and also to keep the baby’s thighs from pressing against it; this isn’t usually necessary later. Usually, the penis will be wrapped in gauze by the doctor or mohel (a ritual circumciser of the Jewish faith). Some doctors recommend putting a fresh gauze pad, dabbed with petroleum jelly or other ointment, on the penis with each diaper change; others don’t think it’s necessary as long as you keep the area clean. You’ll also need to avoid getting the penis wet in a bath (you probably won’t be dunking your baby yet anyway, because the umbilical cord is not likely to have fallen off at this point) until healing is complete.
“Our son’s scrotum seems huge. Should we be concerned?”
Probably not. A boy’s testicles are encased in a protective pouch called the scrotum, which is filled with a bit of fluid to cushion them. Sometimes a child is born with an excessive amount of fluid in the scrotal sac, making it appear swollen. Called hydrocele, this condition is nothing to worry about since it gradually resolves during the first year, almost always without any treatment.
You should, however, point out the swelling to your son’s doctor to be sure what you see isn’t an inguinal hernia (more likely if there is also tenderness, redness, and discoloration; see page 235), which can either resemble a hydrocele or occur along with it. By examining your son, the doctor can determine if the scrotal swelling is due to excess fluid or if there is a hernia involved.
“We were just told that the outlet in our son’s penis is in the middle instead of the end. What will that mean?”
Every so often, something goes slightly awry during prenatal development of the urethra and the penis. In your son’s case, the urethra (the tube that carries both urine and semen, but not at the same time) doesn’t run all the way to the tip of the penis but opens elsewhere. This condition is called hypospadias and is found in an estimated one to three in one thousand boys born in the United States. First-degree hypospadias, in which the urethral opening is at the end of the penis but not in exactly the right place, is considered a minor defect and requires no treatment. Second-degree hypospadias, in which the opening is along the underside of the shaft of the penis, and third-degree hypospadias, in which the opening is near the scrotum, can be corrected with reconstructive surgery.
Because the foreskin may be used for the reconstruction, circumcision, even ritual circumcision, is not performed on a baby with hypospadias.
Occasionally, a girl is born with hypospadias, with the urethra opening into the vagina. This, too, is usually correctable with surgery.
“I’ve been trying to keep my baby swaddled, like they showed me in the hospital. But she keeps kicking at the blanket, and it gets undone. Should I stop trying?”
The first few days of life on the outside can be a little disorienting—and even a little unsettling. After spending nine months snugly enveloped in the uterine cocoon, a newborn must adjust to the suddenly wide-open spaces of her new environment. Many childcare experts feel the transition can be made more comfortable if the security and warmth of the newborn’s former home is simulated by swaddling, or wrapping, her in a receiving blanket. Swaddling also keeps the infant from being disturbed by her own jerky movements while she sleeps, keeps her more comfortable and content on her back, and keeps her warm in the early days when her thermostat is not at peak efficiency. (Though to avoid overheating, a baby should never be swaddled in a warm room.)
Just because all babies are swaddled in the hospital, however, doesn’t mean all babies need—or like—to be swaddled at home. Many babies will continue to derive comfort from swaddling (and hence will sleep better) for a few weeks, some even longer. It may also help calm some colicky infants. On the other hand, some babies seem perfectly content without swaddling or obviously disturbed by it right from the start. A good rule: If swaddling seems to feel good to your newborn, do it; if it doesn’t, don’t.
All babies eventually outgrow the need for swaddling once they become a little more active—and make this clear by trying to kick off the wrapping. At this point, swaddling during naps becomes potentially unsafe, since a kicked-off blanket poses a suffocation risk. For that reason, and because swaddling can interfere with a baby’s ability to practice motor skills, babies shouldn’t be swaddled once they become more active—unless they really seem to need that “wrapped up” feeling during colic spells, in which case swaddling should be limited to those hours only.
“It seems too hot out for a sweater and hat, but when I bring my baby out in just his T-shirt and diaper, everyone who sees us comments that he’s underdressed.”
As far as well-meaning strangers on buses, in stores, and on the street are concerned, new parents (even if they’re on their second or third child) can do no right. So get used to the criticism. But, for the most part, don’t let it affect how you take care of your baby. Grandmothers and grandmotherly types will go to their graves claiming otherwise, but once a baby’s natural thermostat is properly set (within the first few days of life), you don’t normally need to dress him any more warmly than you dress yourself. (And, in fact, prior to that, too much clothing, especially in mild weather, can be as taxing to the newborn’s heat-regulating mechanism as too little.)
So, in general, use your temperature comfort to gauge baby’s (unless you’re the kind of person who’s always warm when everybody else is cold, or always cold when everybody else is warm). If you’re unsure, don’t check his hands for confirmation (as those “well-meaners” will, with disapproving clucks of “See! His hands are cold!”). A baby’s hands and feet are usually cooler than the rest of his body, again because of an immature circulatory system. Don’t take the fact that your baby sneezes a few times to mean he’s cold either; he may sneeze in reaction to sunlight or because he needs to clear his nose.
But while you shouldn’t listen to strangers, do listen to your baby. Babies will usually tell you that they are too cold (as they tell you most everything else) by fussing or crying. When you get this message (or if you’re just not sure whether you’ve dressed him appropriately), check the nape of the neck, arms, or trunk (whichever is easiest to reach under baby’s clothing) with the back of your hand for a temperature reading. If baby feels comfortably warm, maybe it’s a hungry or tired cry you’re hearing. (And if he’s sweaty, he’s probably complaining that he’s overdressed; take a layer off.) If he’s cool, add clothing or covering, or turn up the thermostat. If a young baby seems extremely cold, get him to a warm place right away, because his body probably can’t produce enough heat to re-warm him even if he has a lot of covering. In the meantime, put him close to the warmth of your body, under your shirt if necessary.
The one part of a baby that needs extra protection in all kinds of weather is his head—partly because a lot of heat is lost from an uncovered head (especially a baby’s head, which is disproportionately large for his body), and partly because most babies have very little protection in the way of hair. On even marginally cool days, a hat is a good idea for a baby under a year old. In hot, sunny weather, a hat with a brim will protect baby’s head, face, and eyes—but even with this protection (plus sunscreen), exposure to full sun should be brief.
A young baby also needs extra protection from heat loss when he’s sleeping.
In deep sleep, his heat-producing mechanism slows down, so in cooler weather, bring along an extra blanket or covering for his daytime nap in the stroller. If he sleeps in a cool room at night, a blanket sleeper over his pajamas will help him stay warm (quilts and comforters are unsafe coverings for a sleeping baby). Don’t, however, put a hat on baby when you put him or her to sleep indoors—it could lead to overheating.
When it comes to dressing baby in cold weather, the layered look is not only fashionable, it’s sensible. Several light layers of clothing retain body heat more efficiently than one heavy layer, and the outer layers can be peeled off as needed when you walk into an overheated store or board a stuffy bus, or if the weather takes a sudden turn for the warmer.
An occasional baby falls outside the norm for body temperature control—just as the occasional adult does. If your baby seems cooler than you do, or warmer, all the time, then accept that fact. You may find in talking to your in-laws that your spouse was the same way as a baby. That means, for the cooler baby, more coverings and warmer clothes than you would usually need. For the warmer baby (you’ll probably discover this because of heat rash even in the winter), it means fewer coverings and lighter clothes.
“It’s been ten days since I brought my baby home from the hospital, and I’m starting to go stir-crazy cooped up in the house. When can I take her out?”
Unless your hospital and your home are connected by subterranean tunnel, you’ve taken your baby outside already. And barring a blizzard, a rainstorm, or significantly subfreezing temperatures, you could conceivably have continued to take her outside every day since. The old wives’ tales (which continue to be perpetuated by even not-so-old mothers and mothers-in-law) that have kept newborns and new parents captives in their own homes for two weeks postpartum and more aren’t valid. A healthy, full-term baby is hardy enough to weather a stroll through the park, a quick trip to the market, even a lengthy excursion to visit grandmother (though in flu season, you might want to limit baby’s exposure to indoor crowds, and the germs they carry, for the first six to eight weeks). Assuming you’re up to the exercise (you’re likely to need to spend a lot of time off your feet for at least the first postpartum week), feel free to plan that first escape from the confines of your home.
When you take baby out, dress her appropriately, protect her from weather extremes, and always take along an extra covering if there’s a possibility of a change for the cooler in the weather. If it’s windy or rainy, use a weather shield on the stroller or carriage; if it’s very chilly or extremely hot and humid, limit the amount of time your baby spends outdoors—if you’re freezing or sweltering, she is, too. Avoid more than brief exposure to direct sunlight, even in mild weather. And, most important, if your outing is in a car, be sure your baby is properly harnessed in her rear-facing infant safety seat.
“Everybody wants to touch our son. The doorman, the clerk in the supermarket, old women in stores, visitors we have in our home. I’m always worried about germs.”
There’s nothing that cries out to be squeezed more than a new baby. Baby cheeks, fingers, chins, toes—they’re all irresistible. And yet resist is just what most parents would like outsiders to do when it comes to their newborns.
Your fear that baby can pick up germs this way is a legitimate one. A very young infant is more susceptible to infection because his immune system is still relatively immature and he hasn’t had a chance to build up immunities. So, for now at least, politely ask strangers to look but not to touch—particularly baby’s hands, which usually end up in his mouth. You can always blame it on the doctor: “The pediatrician said not to let anyone outside the family handle him yet.” As for friends and family, ask them to wash their hands before picking up baby, at least for the first month. And skin-to-skin contact should obviously be avoided with anyone who has a rash or open sores.
No matter what you do or say, expect that every once in a while your baby will have some physical contact with strangers. So if a friendly bank clerk tests your child’s grasp on his finger before you can stop the transaction, just pull out a diaper wipe and discreetly wash off baby’s hands. And be sure to wash your own hands after spending time outdoors and before handling your baby. Germs from outsiders (and from door handles or shopping carts) can easily be spread from your hands to your baby.
As your baby gets older, however, he needn’t—and shouldn’t—be raised in an overly sterile environment. He needs to be exposed to a wide variety of “bugs” in order to start building up immunities to those common in your community. So loosen up a little and let the germs fall where they may after the first six to eight weeks.
“I thought babies were supposed to have beautiful skin. But my two-week-old seems to be breaking out in a terrible case of acne.”
It’s unfair, and usually inopportune (arriving just in time for a visit from the grandparents or the first formal portrait), but many babies go through bouts with “adolescent” skin before they’re a month old, let alone on the precipice of puberty. Infant acne, which affects around 40 percent of all newborns, usually begins at two to three weeks and can often last until baby is four to six months old. No one knows for sure the cause of baby acne, but it is believed that such complexion problems have the same cause as many of the complexion problems of teenagers: hormones.
In the case of newborns, however, it’s not their hormones that are causing the problems, but those of their mothers that are still circulating in their systems. These maternal hormones stimulate baby’s sluggish sweat glands, causing pimples to crop up. Another reason for infant acne is that the pores of newborns aren’t completely developed, making them easy targets for infiltration by dirt and the resultant blossoming of blemishes.
Don’t squeeze, scrub with soap, slather with lotions, or otherwise treat your newborn’s acne. Just wash it with water two or three times daily, pat it dry, and it will clear within a few months, leaving no lasting marks.
“My baby suddenly turned two colors—reddish blue from the waist down and pale from the waist up. What’s wrong with her?”
Watching your baby turn color before your eyes can be frightening. And yet there’s virtually nothing to fear when a newborn suddenly takes on a split-color appearance, either side to side or top to bottom. As a result of her immature circulatory system, blood has simply pooled on half of your baby’s body. Turn her gently upside down (or, if the color difference is side by side, over) momentarily, and normal color will be restored.
You may also notice that your baby’s hands and feet appear bluish, even though the rest of her body is pink. This, too, is due to immature circulation and usually disappears by the end of the first week.
“Sometimes when I’m changing my new baby I notice his skin seems to be mottled all over. Why?”
Purplish (sometimes more red, sometimes more blue) mottling of a tiny baby’s skin when he’s chilled or crying isn’t unusual. These transient changes are yet another sign of an immature circulatory system, visible through baby’s still very thin skin. He should outgrow this colorful phenomenon in a few months. In the meantime, when it occurs, check the nape of his neck or his midsection to see if he is too cool. If so, increase his clothing or covering. If not, just relax and wait for the mottling to disappear, as it probably will in a few minutes.
“My baby doesn’t seem to react much to noises. In fact, she sleeps right through the dog’s barking and my older daughter’s tantrums. Could her hearing be impaired?”
It’s probably not that your baby doesn’t hear the dog barking or her sister screaming, but that she’s used to these sounds. Although she saw the world for the first time when she exited your uterus, it wasn’t the first time she heard it. Many sounds—from the music you played on the stereo to the honking horns and screeching sirens on the street—penetrated the walls of her peaceful uterine home, and she became accustomed to them.
Most babies will react to loud noise—in early infancy by startling, at about three months by blinking, at about four months by turning toward the source of the sound. But those sounds that have already become a part of the background Muzak of a baby’s existence may elicit no response—or one so subtle the untrained eye misses it, such as a change in position or activity.
Most newborns are screened for hearing problems (see page 101). So it is likely that yours was screened and found to be fine. You can confirm this by asking your baby’s doctor if the test was performed and what the results were.
If you’re still concerned about your baby’s hearing, try this little test: Clap your hands behind her head and see if she startles. If she does, you know she can hear. If she doesn’t, try again later; children (even newborns) have a wonderful way of ignoring or blocking out their environment at will, and she may have been doing just that. A repeat test may elicit the response you want. If it doesn’t, try to observe other ways in which your baby may react to sound: Is she calmed or does she otherwise respond to the soothing sounds of your voice, even when she isn’t looking directly at you? Does she respond to singing or music in any way? Does she startle when exposed to an unfamiliar loud noise? If you baby seems never to respond to sound, discuss this with her doctor as soon as it’s practical. The earlier a child’s hearing deficit is diagnosed and treated, the better the long-range outcome.
Testing is particularly important for high-risk infants, including those who weighed under 5½ pounds or had complications during delivery, those exposed in the uterus to drugs or infections (such as rubella) that can cause hearing problems, those with a family history of deafness, and those with other serious abnormalities.
“My spouse likes to play loud rock music on the stereo. I’m afraid that it might damage our daughter’s ears.”
All ears, young and old, have a lot to lose when they’re exposed for long periods of time to loud music (whether rock, classical, or any other type), namely, a certain amount of their hearing capacity. Though some ears are more naturally sensitive and prone to damage than others, in general the hearing of babies and small children is most susceptible to the harmful effects of overly loud sound. Damage to the ears can be either temporary or permanent, depending on the noise level and the duration and frequency of exposure.
How loud is dangerously loud? While a baby’s crying might signal that music (or another noise) is too loud for her, don’t wait for her protests before turning the volume down; a baby’s ears don’t have to be “bothered” to be harmed. According to the workplace standards set by the Occupational Safety and Health Administration (OSHA), the maximum noise level that is safe for adults is 90 decibels—a level that can easily be exceeded by a stereo set. If you don’t have the equipment to measure the decibels your stereo is putting out when your spouse plays the stereo, you can set the volume safely by maintaining a level that can easily be talked over—if you have to shout, it’s too loud.
“I put a mobile over my baby’s crib, hoping the colors would be stimulating. But he doesn’t seem to notice it. Could something be wrong with his vision?”
It’s more likely there’s something wrong with your mobile—at least with where it’s hung. A newborn baby focuses best on objects that are between 8 and 14 inches away from his eyes, a range that seems to have been selected by nature not randomly, but by design—it being the distance at which a nursing infant sees his mother’s face. Objects closer to or farther away from a baby lying in his crib will be nothing but a blur to him, although he will fixate on something distant that is bright or in motion if there is nothing worth looking at within his range of vision.
Babies are, despite their fragile appearance, pretty hardy. They don’t “break” when you pick them up, their heads don’t snap off when you forget to support them, and they weather most falls without major injury. But they can be vulnerable. Even very young ones, who seem too tiny to get into trouble, do—sometimes the very first time they turn over or reach for something. To protect your baby from accidents that don’t have to happen, be sure to follow all of these safety tips all of the time:
 In the car, always buckle your baby into an infant safety seat—no matter how far you’re going or how fast or slow you’ll be driving. Wear a seat belt yourself, and make sure whoever’s doing the driving does, too; no one’s safe unless the driver is. And never drink and drive (or drive when you’re very tired or taking medication that makes you sleepy), or let baby ride with anyone who does. (See page 138 for more on safety for baby in the car.)
In the car, always buckle your baby into an infant safety seat—no matter how far you’re going or how fast or slow you’ll be driving. Wear a seat belt yourself, and make sure whoever’s doing the driving does, too; no one’s safe unless the driver is. And never drink and drive (or drive when you’re very tired or taking medication that makes you sleepy), or let baby ride with anyone who does. (See page 138 for more on safety for baby in the car.)
 If you bathe baby in a large tub, put a small towel or cloth at the bottom to prevent slipping. Always keep one hand on baby during the bath.
If you bathe baby in a large tub, put a small towel or cloth at the bottom to prevent slipping. Always keep one hand on baby during the bath.
 Never leave your baby unattended on a changing table, bed, chair, or couch—not even for a second. Even a newborn who can’t roll over can suddenly extend his or her body and fall off. If you don’t have safety straps on your changing table, you should always keep one hand on your baby.
Never leave your baby unattended on a changing table, bed, chair, or couch—not even for a second. Even a newborn who can’t roll over can suddenly extend his or her body and fall off. If you don’t have safety straps on your changing table, you should always keep one hand on your baby.
 Never put baby in an infant (or car) seat or carrier on a table, counter, or any elevated surface; never leave baby unattended in a seat on any surface, even the middle of a soft bed (where suffocation is a risk should baby tip over).
Never put baby in an infant (or car) seat or carrier on a table, counter, or any elevated surface; never leave baby unattended in a seat on any surface, even the middle of a soft bed (where suffocation is a risk should baby tip over).
 Never leave a baby alone with a pet, even a very well behaved one.
Never leave a baby alone with a pet, even a very well behaved one.
 Never leave baby alone in a room with a sibling who is under five years old. A game of peekaboo affectionately played by a preschooler could result in tragic suffocation for an infant. A loving but overly enthusiastic bear hug could crack a rib.
Never leave baby alone in a room with a sibling who is under five years old. A game of peekaboo affectionately played by a preschooler could result in tragic suffocation for an infant. A loving but overly enthusiastic bear hug could crack a rib.
 Don’t leave the baby alone with a sitter who is younger than fourteen, or whom you don’t know well, or whose references you haven’t checked. All sitters should be trained in infant safety and CPR.
Don’t leave the baby alone with a sitter who is younger than fourteen, or whom you don’t know well, or whose references you haven’t checked. All sitters should be trained in infant safety and CPR.
 Never jiggle or shake your baby vigorously (even in play) or throw him or her up into the air.
Never jiggle or shake your baby vigorously (even in play) or throw him or her up into the air.
 Never leave baby alone at home, even while you go for the mail, move the car, or check the laundry in the apartment building basement; it takes only seconds for an accident to happen.
Never leave baby alone at home, even while you go for the mail, move the car, or check the laundry in the apartment building basement; it takes only seconds for an accident to happen.
 Never leave a baby or child alone in an automobile. In hot (or mild) weather, even keeping the windows down might not prevent the baby from succumbing to heat stroke. In any weather, a child snatcher on the prowl could quickly make off with the car’s precious cargo.
Never leave a baby or child alone in an automobile. In hot (or mild) weather, even keeping the windows down might not prevent the baby from succumbing to heat stroke. In any weather, a child snatcher on the prowl could quickly make off with the car’s precious cargo.
 Never take your eyes off your baby when you’re shopping, going for a walk, or sitting at the playground. A stroller or carriage makes an easy target for abduction.
Never take your eyes off your baby when you’re shopping, going for a walk, or sitting at the playground. A stroller or carriage makes an easy target for abduction.
 Avoid using any kind of chain or string on baby or on any of baby’s toys or belongings—that means no necklaces, strings for pacifiers or rattles, no religious medals on chains, no ribbons longer than 6 inches on cribs or cradles. Make sure the ends of strings in hoods, gowns, and pants are knotted so they can’t slip through, and never leave cords, string, ropes, or chains of any kind around where baby might get to them. Be sure, too, that baby’s crib, play yard, and changing table are not within reach of electric cords (which present double danger), telephone cords, or venetian blind or drapery cords. All of these items can cause accidental strangulation.
Avoid using any kind of chain or string on baby or on any of baby’s toys or belongings—that means no necklaces, strings for pacifiers or rattles, no religious medals on chains, no ribbons longer than 6 inches on cribs or cradles. Make sure the ends of strings in hoods, gowns, and pants are knotted so they can’t slip through, and never leave cords, string, ropes, or chains of any kind around where baby might get to them. Be sure, too, that baby’s crib, play yard, and changing table are not within reach of electric cords (which present double danger), telephone cords, or venetian blind or drapery cords. All of these items can cause accidental strangulation.
 Don’t place filmy plastics, such as those used by dry cleaners, or plastic bags on mattresses or anywhere baby can get at them.
Don’t place filmy plastics, such as those used by dry cleaners, or plastic bags on mattresses or anywhere baby can get at them.
 Don’t leave an unattended infant (awake or asleep) within reach of pillows, stuffed toys, or other plush items, or let baby sleep on a sheepskin, plush-top mattress, beanbag, waterbed, or a bed wedged up against the wall. Always remove bibs and any hair ties or barrettes before putting baby down to sleep.
Don’t leave an unattended infant (awake or asleep) within reach of pillows, stuffed toys, or other plush items, or let baby sleep on a sheepskin, plush-top mattress, beanbag, waterbed, or a bed wedged up against the wall. Always remove bibs and any hair ties or barrettes before putting baby down to sleep.
 Remove crib gyms once baby can get up on hands and knees (around four to six months). Consider removing crib bumpers when baby can pull up (so that he or she can’t use them as a climbing step.)
Remove crib gyms once baby can get up on hands and knees (around four to six months). Consider removing crib bumpers when baby can pull up (so that he or she can’t use them as a climbing step.)
 Do not place a baby on any surface next to an unguarded window, even for a second, and even asleep.
Do not place a baby on any surface next to an unguarded window, even for a second, and even asleep.
 Use smoke detectors and carbon monoxide detectors in your home, and install them according to the recommendations of your local fire department. Keep them maintained.
Use smoke detectors and carbon monoxide detectors in your home, and install them according to the recommendations of your local fire department. Keep them maintained.
In addition, he will spend most of his time looking to his right or to his left, rarely focusing straight ahead in the early months. A mobile directly above his crib is not likely to catch his fancy, whereas one hung to one side or the other may. Few babies, however, show any interest at all in mobiles until they are three to four weeks old, and many not until even later. (For safety reasons, remember to remove mobiles and gyms from the crib by the time baby can get up on his hands and knees, usually around four to six months.)
So your newborn can see, but not the way he will in three or four months. If you want to evaluate your baby’s vision, hold a penlight to one side of his line of vision, about 10 to 12 inches from his face. During the first month, a baby will generally focus on the light for a brief period, long enough for you to know he’s seeing it. By the end of the first month, some babies will follow as you move the light slowly toward the center of their field of vision. Generally, not until three months will a baby begin to follow an object in a full 180-degree arc, from one side to the other.
Your baby’s eyes will continue maturing during the first year. He probably will be farsighted for several months and not be able to perceive depth well (which may be why he’s a perfect candidate for falling off changing tables and beds) until nine months. But though his vision isn’t perfect now, he does enjoy looking at things—and this pastime is one of his most important avenues to learning. So provide him with plenty of visual stimuli. But don’t overload his circuits—one or two eye-catchers at a time are about all he can handle. And because his attention span is short, change the scenery frequently.
Most young babies like to study faces—even crudely drawn ones, and even their own in a crib mirror (though, of course, they won’t recognize it as their own for many months to come). They prefer to gaze at things that are highly contrasted, such as black and white or red and yellow; complex objects to simple ones. They love looking at light: a chandelier, a lamp, a window (especially one through which light is filtered via the slats of vertical or horizontal blinds), will all attract their rapt scrutiny; and they are usually happier in a well-lighted room than in a dim one.
Vision screening will be part of your baby’s regular checkups. But if you feel that your baby doesn’t seem to be focusing on objects or faces or doesn’t turn toward light, mention this to his doctor at the next visit.
“I’ve noticed that our baby blinks when the flash from our camera goes off. Could it be hurting his eyes?”
Only the most sought-after celebrities are as hounded by the popping of a camera’s flash as a newborn baby whose paparazzi parents are determined to capture in pictures every detail of his first days of life. But, unlike celebrities, infants can’t hide behind dark glasses when the flashing starts. To protect your baby’s eyes against the possibility of injury from a flash that’s too near him and from too intense and too close exposure to the camera lights, it’s a good idea to take a few precautions during photo sessions. Try to keep the camera at least 40 inches from baby, and if your photographic equipment allows, bounce the light off a wall or ceiling instead of in baby’s face. If you failed to take such precautions during previous shoots, don’t worry. The risk of harm is exceedingly small.
“The swelling is down around my baby’s eyes. Now she seems cross-eyed.”
Babies are very obliging: They always give their parents something new to worry about. And most parents worry plenty when they notice their babies’eyes appear to be crossed. Actually, in most cases, it’s simply extra folds of skin at the inner corners of the eyes that make the babies look cross-eyed. When the folds retract as baby grows, the eyes begin to seem more evenly matched. For extra reassurance, mention your concern at baby’s next checkup.
During the early months, you may also notice that your baby’s eyes may not work in perfect unison all the time. These random eye movements mean she’s still learning to use her eyes and strengthening her eye muscles; by three months, coordination should be much improved. If it isn’t, or if your baby’s eyes always seem to be out of sync, then talk to her doctor about the problem. If there is a possibility of true crossed eyes (strabismus, in which the baby uses just one eye to focus on what she’s looking at, and the other seems aimed anywhere), consultation with a pediatric ophthalmologist is in order. Early treatment is important, because so much that a child learns she learns through her eyes, and because ignoring crossed eyes could lead to “lazy” eye, amblyopia (in which the eye that isn’t being used becomes lazy and consequently weaker, from disuse).
“At first, there were no tears when my baby cried. Now her eyes seem filled with tears even when she’s not crying. And sometimes they overflow.”
Tiny tears don’t start flowing out of the tiny eyes of newborns until close to the end of the first month. That’s when the fluid that bathes the eye (called tears) is produced in sufficient quantity by the glands over the eyeballs. The fluid normally drains through the small ducts located at the inner corner of each eye, and into the nose (which is why a lot of crying can make your nose run). The ducts are particularly minute in infants, and in about 1 percent of babies—yours included—one or both are blocked at birth.
Since a blocked tear duct doesn’t drain properly, tears fill the eyes and often spill over, producing the perpetually “teary-eyed” look even in happy babies. But the clogged ducts are nothing to worry about; most will clear up by themselves by the end of the first year without treatment, though your baby’s doctor may show you how to gently massage the ducts to hasten the clearing. (Always wash your hands thoroughly first before using massage; if baby’s eyes become puffy or red, stop massaging and inform the doctor.)
Sometimes, there is a small accumulation of yellowish white mucus in the inner corner of the eye with a tear duct blockage, and the lids may be stuck together when baby wakes up in the morning. Mucus and crust can be washed away with water and sterile absorbent cotton balls. A heavy, darker yellow discharge and/or reddening of the whites of the eye, however, may indicate infection or another condition that requires medical attention. The doctor may prescribe antibiotic ointments or drops, and if the duct becomes chronically infected, may refer your baby to an ophthalmologist. Call the doctor immediately if a tearing eye seems sensitive to light or if one tearing eye looks different in shape or size from the other.
“My baby sneezes all the time. He doesn’t seem sick, but I’m afraid he’s caught a cold.”
Hold off on the chicken soup. What your baby’s caught isn’t likely to be a cold but some amniotic fluid and excess mucus in his respiratory passages—a very common occurrence in young babies. And to clear it out, nature has provided him with a protective reflex: sneezing. Frequent sneezing (and coughing, another protective reflex) also helps the newborn to get rid of foreign particles from the environment that make their way to his nose—much as sniffing pepper makes many adults sneeze. Your baby may also sneeze when exposed to light, especially sunlight.
“Everybody says that my baby’s smiles are ‘just gas,’ but he looks so happy when he does it. Couldn’t they be real?”
They read it in books and magazines. They hear it from mothers-in-law, friends with children, their pediatricians, perfect strangers in the park. And, yet, no new parent wants to believe that baby’s first smiles are the work of a passing bubble of gas, rather than of a wave of love meant especially for mommy or daddy.
But, alas, it appears from scientific evidence so far to be true: Most babies don’t smile in the true social sense before four to six weeks of age. That doesn’t mean that a smile is always “just gas.” It may also be a sign of comfort and contentment—many babies smile as they are falling asleep, as they urinate, or as their cheeks are stroked.
When baby does display his first real smile, you’ll know it, and you’ll melt accordingly. In the meantime, enjoy those glimpses of smiles to come—undeniably adorable no matter what their cause.
“My baby gets the hiccups all the time—and for no apparent reason. Do they bother him as much as they do me?”
Some babies aren’t just born hiccupers, they’re hiccupers before they’re born. And chances are, if your baby hiccuped a lot inside of you, he’ll hiccup plenty in the first few months on the outside, too. But a newborn’s hiccups, unlike the adult variety, don’t have a known cause, though theories abound. One is that they are another of baby’s reflexes, though they’re frequently triggered by giggling later on. Another theory is that infants get hiccups when they gulp down formula or breast milk, filling their tummies with air. Unlike adult hiccups, they’re not bothersome, at least not to baby. If they are to you, try letting your baby nurse or (if he’s bottle fed) suck on a bottle, which may quell the attack.
“I’ve been using baby soap flakes to wash my daughter’s clothes. But nothing seems to come clean, and I’m also getting tired of doing her loads separately. When can I start using our usual detergent?”
Although manufacturers of special baby laundry soaps wouldn’t want it to get around, many babies probably don’t need their clothes washed separately from the rest of the family’s. Even the high-potency detergents that really get clothes clean, eliminating most stains and odors (the kind babies are very good at generating), aren’t irritating to most infants when they’re well rinsed. (Rinsing is most thorough, and stain-fighting powers are most effective, with liquid detergents.)
To test your baby’s sensitivity to your favorite laundry detergent, add one garment that will be worn close to baby’s skin (such as a T-shirt) to your next family load, being careful not to overdo the detergent or underdo the rinse. If baby’s skin shows no rash or irritation, go ahead and wash her clothes with yours. If a rash does appear, try another detergent, preferably one without colors and fragrances, before deciding you have to stick with baby soap flakes.
One extra laundry step you may want to consider is pre-spotting to avoid those telltale yellow spit-up stains. Better still, tackle spit-up while it’s still fresh.
From the day a baby’s born, the race is on—and it’s a sure bet that most parents, rooting their offspring on from the starting line, will be disappointed if their entry doesn’t make a good showing. If the child development chart shows that some babies start turning over at ten weeks, why hasn’t their baby accomplished it by twelve weeks? If the baby in the next stroller at the park grabbed an object at three and a half months, why hasn’t their baby done it by then? If grandma insists all of her children sat up by five months, why is theirs still slumping at six?
But in this race, the child who comes in first in mastering early developmental skills doesn’t necessarily finish in the money, while the one who moseys along developmentally doesn’t necessarily finish out of it. Though the very alert baby may indeed turn out to be a bright child and a successful adult, attempts to measure infant intelligence and correlate it with intelligence in later years have not been fruitful. The baby who seems to be a little slow, it appears, can also turn out to be bright and successful. Studies have shown, in fact, that one in seven children gains forty IQ points from the middle of the third year to the age of seventeen. That means an “average” toddler can become a “gifted” teenager.
Part of the difficulty, of course, is that we don’t know how intelligence manifests itself in infancy, or even if it does. And even if we did know, it would be difficult to test for it because infants are nonverbal. We can’t ask questions and expect answers, we can’t assign a passage for reading and then test for comprehension, we can’t present a problem to assess reasoning power. About all we can do is evaluate motor and social skills—and these just aren’t equitable with what we later think of as intelligence. Even when we evaluate early developmental skills, our results are often in question; we never know whether a baby is not performing because of inability, lack of opportunity, hunger, fatigue, or a momentary lapse in interest.
Anyone who’s spent any time at all around more than one baby knows that children develop at different rates. Many of these differences are due more to nature than to nurture. Each individual seems to be born programmed to smile, lift his or her head, sit up, and take first steps at a particular age. Studies show that there is little we can do to speed up the developmental timetable, though we can slow it down by not providing an adequate environment for development, by lack of stimulation or opportunity, by poor diet, by poor health care (certain medical or emotional problems can hamper development), and by simply not giving enough love and attention.
Infant development is usually divided into four areas:
Social. How readily your baby learns to smile, coo, and respond to the human face and voice tells you something about him or her as a social being. Though some babies are naturally more serious than others, and some more social, a major delay in this area could indicate a problem with vision or hearing, or with emotional or intellectual development.
Language. The child who has a large vocabulary at an early age or who speaks in phrases and sentences before the usual time is probably going to have a way with words. But the child who makes requests with grunts and gestures into the second year may catch up and do just as well or even better later on. Since receptive language development (how well baby understands what is said) is a better gauge of progress than expressive language development (how well baby actually speaks), the child who “understands everything” but says very little is not likely to be experiencing developmental delay. Again, very slow development in this area occasionally indicates a vision or hearing problem and should be evaluated.
Large motor development. Some babies seem physically active from the first kicks in the womb; once born, they hold their heads up early, sit, pull up, and walk early, and may turn out to be more athletic than most. But there are slow starters who end up excelling on the football field or tennis court, too. Very slow starters, however, should be evaluated to be certain there are no physical or health impediments to normal development.
Something you should definitely keep in mind when your compulsion to compare gets the best of you (and it will): Babies today are developing later in some major gross motor skill categories than they used to. Not because they’re less naturally precocious, but because they’re spending less time on their tummies. Putting babies to sleep on their backs dramatically reduces the risk of SIDS, but it also temporarily slows motor development. With little opportunity to practice those skills babies used to practice on their tummies (such as rolling over and crawling), more babies are accomplishing these skills later.
Many are even skipping the crawling stage entirely. Though this slowdown isn’t considered significant developmentally (and skipping the crawling phase is never a problem unless a baby is skipping other developmental milestones as well, such as rolling over, sitting up, and so on), parents can help their babies along by making sure they spend plenty of supervised playtime on their bellies from an early age. (Parents who wait too long to flip their babies at playtime will find that their babies balk at this unaccustomed position.) So remember: Back to sleep, tummy to play.
Small motor development. Early eyehand coordination, and reaching for, grasping, and manipulating objects before the average age may predict a person will be good with his or her hands. However, the baby who takes longer to become skilled in this area is not necessarily going to be “all thumbs” later on.
Most indicators of intellectual development—creativity, sense of humor, and problem-solving skills, for example—don’t usually become apparent until toward the end of the first year at the earliest. But, eventually, given plenty of opportunity, encouragement, and reinforcement, a child’s various inborn abilities will combine to create the adult who is a talented painter, a resourceful mechanic, an effective fund-raiser, a savvy stockbroker, a sensitive teacher, an all-star pitcher.
The rate of development in the various areas is usually uneven. One child may smile at six weeks but not reach for a toy until six months, while another may walk at eight months but not talk until a year and a half. When an occasional child does develop evenly in all areas, this may provide a clearer clue to future potential. A child who does everything early, for instance, is likely to be brighter than average; the child who seems extremely slow in every area may have a serious developmental or health problem, in which case professional assessment and intervention (which can make a tremendous difference) is necessary.
Though children develop at different rates, each child’s development—assuming no environmental or physical barriers exist—follows the same three basic patterns. First, the child develops from the top down, from head to toes. Babies lift their heads up before they can hold their backs up to sit, and hold their backs up to sit before they can stand on their legs. Second, they develop from the trunk outward to the limbs. Children use their arms before they use their hands, and their hands before they use their fingers. Development progresses not surprisingly, from the simple to the complex.
Another aspect of infant learning is the deep concentration directed toward learning a particular skill. A child may not be interested in beginning to babble while practicing to pull up. Once a skill is mastered, another moves to center stage, and the baby may seem to forget the old, at least for a while, so involved is he or she in the new. Eventually, your baby will be able to integrate all the various skills and use each spontaneously and appropriately. But, in the meantime, don’t worry when he or she seems to forget what was recently learned or looks at you blankly when called on to perform the most recently acquired skill.
No matter what your child’s rate of development, what is accomplished in the first year is remarkable—never again will so much be learned so quickly. Enjoy this time, and let your baby know you’re enjoying it. By accepting your baby’s timetable as okay, you will be letting your child know that he or she is okay, too. Avoid comparing your child with other babies (yours or anyone else’s) or with norms on developmental charts. The monthly development charts in this book are not meant to inspire such competition (or worry), in parents of babies who aren’t achieving at the highest level. Rather, they’re meant to give parents an idea of the wide range of normal, so they can be sure their babies don’t have any developmental lags that might need looking into.
Trying to figure out what month baby’s in—and which one you should be reading right now? Here’s how it works: The “First Month” chapter covers your baby’s progress from birth to the first-month birthday; the “Second Month” chapter gives you the low-down on your one-month-old (until he or she turns two months old), and so on—with the first year’s expectations ending as baby blows out those first birthday candles.

1. If you’re breastfeeding. Bottle-feeding issues are covered starting on page 106.
2. Breast shells (also called milk cups) are intended to correct inverted nipples. However, they can also be used during a feeding to catch and collect milk that leaks from one breast while the baby nurses from the other or while pumping. Place the milk cup inside your bra on the alternate breast.
3. If your breastfed baby has very infrequent bowel movements and is not gaining well, then see page 167 and check with your doctor. It’s possible she isn’t getting enough to eat and thus has not much to eliminate.
4. Some case-by-case exceptions might be made for infants with severe gastroesophageal reflux or those with airway malformations.
5. If a baby’s cry is inexplicably high-pitched, check with the doctor; such a cry could indicate illness.