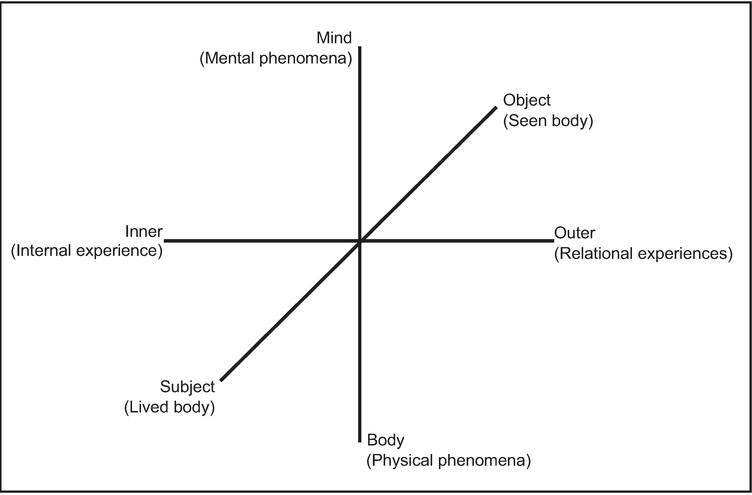
Figure 3.1 A clinical model of embodiment
A model for the conceptualization and treatment of mental illness
Jessica Acolin
Surrounded by increasingly sophisticated diagnostic tools and interventions, many clinicians have forgotten one crucial factor: the individual. While many agree that healing is dependent upon a patient’s motivation and behaviour (in adherence to medication or clinical homework), current diagnoses and medical language depersonalize the experience. A person is more than a list of symptoms; they are the lived experience of those symptoms, and their lived experience is what will determine their motivation and behaviour. In order to treat mental illness, clinical practitioners need tools and language for connecting with, assessing, and intervening at the level of a patient’s lived experience.
Thus far, such an approach has been relegated to the realm of ‘clinical judgment’; that is, a hazily defined realm of subjective evaluations that varies according to practitioner and patient. This is borne from necessity and efficacy: necessity, due to the dearth of research or tools to standardize such important judgments [for a notable exception, see Pallagrosi, Picardi, and Biondi (2013)]; and efficacy, as clinicians instinctually have access to sophisticated, fast, and at times unconscious evaluations of nonverbal cues and behaviour that may supersede the information accessible through existing standardized diagnostic tools.
Such unconscious evaluations are largely based on nonverbal cues such as movement, facial expressions, postural changes, or tone of voice. Such evaluations, rather than being subjective and unreliable, are increasingly being shown to be important, reliable, and measurable in the laboratory environment. Embodiment researchers from diverse academic backgrounds are beginning to illustrate this connection between the verbal and the nonverbal, the unconscious and the conscious, and the mind and the body. This body of work supports the clinical importance of ‘subjective’ clinical judgments and may, in time, show how such evaluations are as important as, if not more important than, existing symptom checklists.
Nevertheless, the development of standardized tools based on embodiment research would advance mental health practice and encourage additional research to understand and improve existing clinical judgment and interventions. Thus, it is beneficial for researchers, clinicians, and patients alike to integrate embodiment research gained in the labs with clinical expertise gained through practice. The formulation of such a model of health, illness, and change—in short, a clinical theory of embodiment—would guide future research, inform current clinical interventions, and ultimately move individuals more effectively from illness to health. This chapter outlines such a practical model for clinicians as a foundation for such a clinical theory of embodiment.
Embodiment research illustrates how embodiment and the mind-body connection are important in cognition, social interaction, emotional regulation, and self-expression. Here, embodiment is defined as the dynamic interaction between mental and physical states that comprise individual experience. This definition is raised in opposition to out-dated models of human behaviour based on Cartesian dualism, which treats the mind and its processes, such as cognition, logic, judgment, preference, and personality as both separate from and more important than the body and physical sensations. While Cartesian dualism continues to guide certain branches of research and practice, particularly the ‘hard’ sciences which encourage purely cognitive interventions, embodiment researchers are showing that the mind-body connection is central to a full understanding of human experience.
Cognition, for instance, long touted as the epitome of the human brain overcoming limitations of the physical body, is embodied. Language comprehension engages the sensorimotor cortex; comprehending a word such as ‘cinnamon’ automatically involves sensory processing (Pulvermüller, 1999, 2013).
Thinking about complex social concepts such as age can elicit unconscious bodily responses such as slower gait (Bargh, Chen, and Burrows, 1996). Abstract concepts of time elicit gentle sways forward for the future and backwards for the past (Miles, Nind, and Macrae, 2010). Thus, cognition, or what has been considered disembodied ‘thinking’, is not as separate from the body as previously believed.
Similarly, social judgments such as threat, friendliness, and intimacy are embodied. Individuals have been shown to judge a neutral stranger as more generous and caring when holding a warm versus cold beverage (Williams and Bargh, 2008). Individuals with positive evaluations of a demographic group (the elderly) unconsciously mimicked their movement patterns (slower gait) (Cesario, Plaks, and Higgins, 2006). Social psychology research increasingly illustrates the myriad ways in which social interactions and behaviour are embodied (Niedenthal, Barsalou, Winkielman, Krauth-Gruber, and Ric, 2005).
The advice to ‘take a step back’ when agitated is more than an expression; physically stepping backwards has been shown to improve cognitive control (Koch, Holland, Hengstler, and Knippenberg, 2009). Deep breathing, sometimes called ‘belly breathing’, has been shown to regulate emotional arousal without additional cognitive intervention (Benson and Klipper, 1992). Depression and sadness manifest in downward gaze and slower gait (Meier and Robinson, 2004, 2006; Michalak et al., 2009). In these and other ways, human experience is being increasingly understood as embodied.
A significant challenge is the search for a language to consistently describe the body-based variables being studied. Here, two systems of movement analysis and notation used by dance researchers and dance/movement therapists are valuable. Laban Movement Analysis (LMA), provides a vocabulary that describes movement behaviour based on body position, movement quality, and relationship to space (Dell, 1970). The Kestenberg Movement Profile (KMP) adds criteria for observing rhythms and patterns of motion (Kestenberg-Amighi, Loman, Lewis, and Sossin, 1999). When used by trained movement analysts, these two languages provide a comprehensive, objective, and efficient system of observing and categorizing nonverbal behaviour.
This movement vocabulary captures relationships between psychological phenomena and the mechanics of movement (such as pace, tension, or direction) as well as the quality of movement (Koch, 2014). Movement quality and patterns play an important role in connecting nonverbal behaviour to mental functions and may provide much-needed order to the overwhelming variety of variables currently studied by embodiment researchers.
Phenomenological theory reminds us to pay attention, not only to external observations, but also to the individual’s lived experience. The importance of embodied experience lies in the meaning it holds for the individual, regardless of whether it was observed via neuroimaging, lab measurements, or in the clinical session room. This phenomenological approach invites greater introspection on the part of the observer of personal biases and movement. Defining and standardizing such a clinical approach represents a new and exciting direction (Pallagrosi et al., 2014) and will contribute to a greater respect for the opinions, experiences, and interpretations of both patient and clinician.
Fuchs (2010) outlines a phenomenological account of psychopathology which categorizes mental illness by disturbances in the patient’s lived, embodied experiences. In this account, schizophrenia is defined by an overwhelming sense of disembodiment, or a broken connection between cognition and bodily self-awareness. Depression is characterized by an inescapable sense of confinement to the lived body, which Fuchs refers to as hyperembodiment and a falling back in or out of time. Fuchs categorizes the experience of mental illness based upon disturbances in balanced embodiment: the balance between the subject and the object body, the immediate and the narrative self, and the mental processes and physical sensations.
Advances in neuroscience support this understanding of mental illness as rooted in the individual lived experience. Trauma researchers increasingly show how the plethora of symptoms currently associated with attention deficit hyperactivity disorder, oppositional defiant disorder, obsessive compulsive disorder, panic disorder, generalized anxiety disorder, bipolar disorder, borderline personality disorder, and others can be traced to fundamental physical reactions associated with survival and body regulation (Soma, 2016). Anxiety, for instance, results from the body remaining in a hyper-aroused state in preparation to respond to threats; this bodily state is then interpreted by the individual as fear, even when no immediate threat is present. Anxious behaviour follows. The individual’s lived experience of their physical state, thus, is important in understanding how to clinically intervene.
Emphasizing balance, functional adaptability, and in-the-moment observation, rather than unilateral increase or decrease of symptoms, or analysis of past or future experiences, reflects ancient Eastern philosophies and underlies approaches such as dialectical behaviour therapy, dance/movement therapy, and trauma-informed yoga (Levy, 2005; Linehan, 1993; van der Kolk, 2014). In these models, health is not defined by a static maintenance of a desired state but rather by the ability of an individual to move and self-regulate as a situation requires. Acknowledging that life experiences and stressors are varied and require different solutions, such therapies focus on enhancing an individual’s access to many functional states and empowering the individual to access varied skills and strategies as needed. From this body of research, theory, and practice, a clinical theory of embodiment begins to emerge.
Several key conclusions can be drawn from the literature that provide the foundation for a clinical theory of embodiment. First, it becomes clear that humans are embodied beings who understand and interact with the world around them via the dynamic relationship between mind and body. In addition, this mind-body connection is complex and is involved in anything from language acquisition to abstract concept comprehension; in fact, in view of its complex nature and high inter-subject variability, the task of merely describing embodiment from an external observer’s perspective may seem daunting.
Nevertheless, humans are embodied. Their individual lived, embodied experiences are essential to understanding their distress and, in turn, to ameliorating it. Thus, a shift in focus from the external observation of symptoms and behaviours to the individual’s lived and embodied experiences provide an important direction forward for clinical intervention. It is the individual’s interpretation of symptoms, the interplay of their mind with their lived body, which is of key clinical significance.
This approach emphasizes the individual’s lived experience in the present, or what is called the ‘here and now’. It focuses on how past experiences (all simultaneously) manifest themselves in current body experiences, which acknowledges the importance of formative memories (Fuchs, 2012) while providing an immediate avenue for intervention. Thus, assessments and interventions are designed to be immediate and to be implemented in the present, in the session room, rather than as homework or as analysis of past memories.
Next, the theoretical emphasis on balance and flexibility in coping with the environment, rather than a static or unilateral focus on symptoms, offers a widely applicable clinical approach that empowers the patient in the long term and better meets the needs of individuals living in a dynamic world. A clinical theory founded on balance serves both clinicians and patients by acknowledging the multifaceted nature of individuals and normalizing temporary fluctuations in behaviour while allowing for varied capabilities.
Finally, a standardized tool for assessing and diagnosing an individual’s lived experience in order to best design interventions is both important and possible. Observation approaches of body movement such as LMA and the KMP, alongside phenomenological theories of psychopathology, provide the rudimentary structure for such a tool.
The model presented in this chapter identifies three axes of embodiment, each of which is important in its own right but can be maladaptive when taken too extremely or rigidly. Though an individual may, at different times, fall in different places on each axis, the clinical goal is for the individual to find balance in order to regularly adapt to changing needs and desires.
The first axis addresses how an individual experiences, understands, and makes decisions. Does the individual rely primarily on thoughts, logic, and reasoning (mental processes) or on intuition, sensory experience, and feeling (body processes)? For instance, two individuals both have the same experience of walking by the beach. One who relies primarily on mental processes may explain tides, measure temperature, and categorize marine biology. One who relies primarily on physical processes may focus on the warm sand, crashing waves, and the smell of saltwater. Neither approach is better than the other. Cognitive processes are necessary in problem solving, while physical sensations are important in intimate relationships. A well-balanced individual can access both forms of processing and is able to adjust according to environmental and situational demands. However, inflexibility or too strong a preference in one direction results in maladaptive behaviours. This axis is called the decision access, with Mind at one pole and Body at the other.
The second axis focuses on an individual’s identity, or how they see themselves. Are they defined by their own perceptions, judgments, and expectations—or those of others? The latter is called an objectified body, where the individual sees themselves (and their bodies) from an external point of view, sometimes even as objects to be manipulated or controlled. Such a body may feel contorted and confined by excessive demands and judgments (Fuchs, 2010; Serlin, 1996). The former is referred to as a subject or lived body, and it is one that is guided by internal sensations such as pleasure, pain, and instinct. Again, both the object and subject body are important for optimal functioning. Awareness of social expectations and exerting conscious control over our bodies and lives are the hallmark of civil society. Yet, access to internal experiences and desires are important for immediate threat detection, pleasurable enjoyment, and social attunement. Thus, a balance and flexibility of movement between the two poles is necessary. This axis is called the identity access with Object at one pole and Subject at the other.
The third axis brings attention to where an individual directs their focus. Is the individual turned inward, noticing only their own thoughts and feelings and ruminating on the past or future? Or is the individual turned outward, seeing and reacting to the world around them and living in present sensations? The former is crucial to successful problem solving and conscious decision-making. However, an individual stuck in internalized focus can become anxious, dissociated, or paralyzed by inactivity. Engagement with the outside world underlies initiation, action, and since humans are fundamentally social beings, emotional regulation (Homann, 2010). Again, balance and flexibility on this axis leads to a well-functioning and adjusted individual. This axis is called the focus access, with Inner at one pole and Outer at the other.
This model is graphically illustrated below and can be used to assess both an individual’s capacity and their current state. What an individual has access to determines the range within which they can move at the present time; one therapeutic goal can be to increase the individual’s capacities through skill-building and practice. An individual’s current state can be marked within the model; the therapeutic goal may then be to assist the individual in accessing greater balance. Such representation both of an individual’s capabilities and current state provides the practitioner with a practical tool for here-and-now assessment and intervention to help an individual achieve greater balance and flexibility.
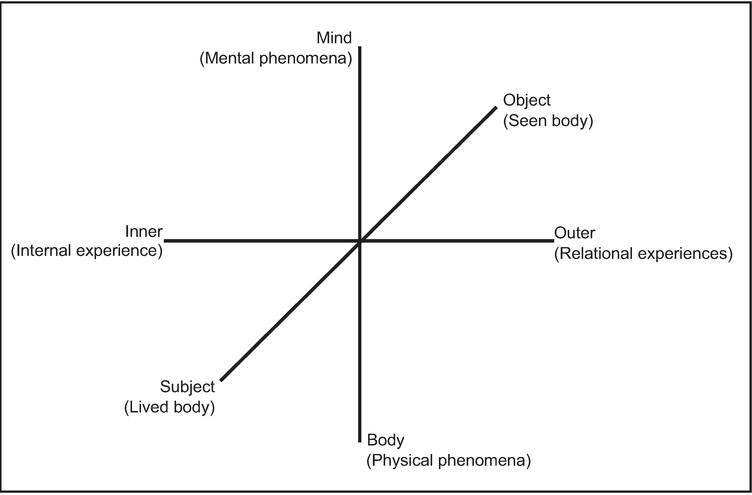
Figure 3.1 A clinical model of embodiment
This model of health, illness, and adaptive functioning prizes balanced access to both poles and flexibility. As stated above, no individual pole is sufficient in isolation; each is necessary in certain instances. Thus, balance on all three axes is important to healthy functioning. Flexibility is the ability to move between poles as needed. Environmental demands are varied and ever changing. The facility with which an individual has access to each pole contributes to their ease of interacting effectively with any challenges they may face. Thus, the therapeutic goal is to achieve greater balance and flexibility, rather than to unilaterally increase individual capacities. Figure 3.1 illustrates a clinical model of embodiment.
Currently, schizophrenia is characterized in the American Diagnostic and Statistical Manual of Mental Disorders (DSM) 5 by psychotic symptoms (hallucinations or delusions), disorganization, and negative symptoms such as flat affect and lack of motivation.
Imagine the experience of such an individual. Internal thoughts and feelings are so strong that they partly constitute reality, creating a tyranny of the mind. There is little connection to the outside world; reassurances from others feel threatening, less ‘real’ than the world their mind has trapped them in. Body sensations are foreign and dangerous, and touch feels alien or threatening. The body is held in rigid defence, muscles tensed in preparation for danger, pleasurable sensations ignored. The physical body is forced to succumb to the mind’s control. Such individuals often present with disorganized movement patterns (Davis, 1997), giving the observer the sense that their limbs are separate from their torso and their body parts have been cobbled together from incompatible sources.
This is a thought experiment, an attempt to imagine the lived experience of schizophrenia. However, in engaging in the exercise, it becomes clear how an individual with schizophrenia may be conceptualized through this clinical model of embodiment. Fuchs (2010) describes schizophrenia as a disorder of disembodiment, and this is consistent with the conceptualization provided by this model.
First, on the Decision axis, the individual with schizophrenia is guided primarily by the Mind. Delusions and hallucinations are faulty interpretations by the mind of thoughts, feelings, and body sensations. The individual does have access, at the extremes, to both mental and physical processes; what is lacking is any connection between the two. The result is a disorganized method of decision-making shaped simultaneously by body sensations and mental interpretations, while lacking a bridge, or any integration, of the two.
The individual is represented in Figure 3.2:
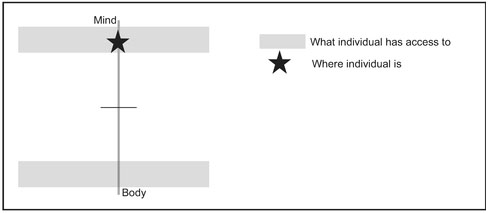
Figure 3.2 Decision axis in schizophrenia
On the second axis, Identity, the schizophrenic body is one that is controlled, confined, and fought. Muscles are held rigidly in defence against any subjective feelings, as if the individual is at war with their own body. The individual sees themselves as separate from their body, and the possibility of subjective experience can be threatening. The individual is thus represented as in Figure 3.3 below:
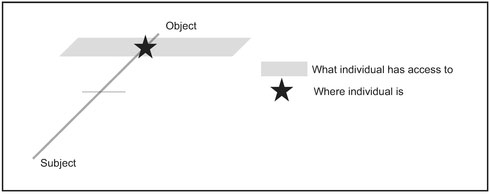
Figure 3.3 Identity axis in schizophrenia
Finally, the individual is trapped in an internal world; connection to or comprehension of others is limited as in Figure 3.4.
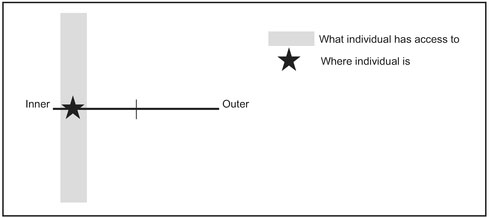
Figure 3.4 Focus axis in schizophrenia
The disembodiment referenced by Fuchs thus appears on all three axes, placing the individual in the top left quadrant of the model as in Figure 3.5.
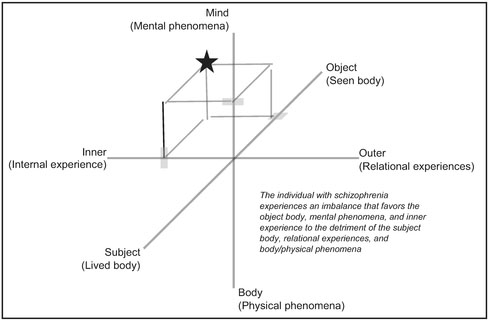
Figure 3.5 Schizophrenia conceptualization
When selecting clinical interventions, two kinds of information are important: what is the goal? And what options or resources are available? The proposed model provides direction on both questions.
First, the goal for any individual is to bring balance and improve flexibility. Thus, it is relevant to ask: What does the individual currently have access to, and what capacities need to be strengthened?
Individuals who have unipolar strength, such as having access to Mind but not Body or Subject but not Object, need to gain access to the opposite pole. Their current abilities provide the entry into treatment, while what they lack provides the direction. For instance, individuals high on the Mind (thinking) axis may benefit from body awareness and sensory interventions such as yoga, massage, somatic experiencing, progressive muscle relaxation, and guided body scans. However, these body-based interventions may best be introduced through cognitive reasoning, step-by-step explanations and rationales for effectiveness. Conversely, individuals high on the Body (feeling) axis may benefit from development of cognitive analyses as offered by cognitive therapies. Such individuals may respond best if these cognitive therapies are presented first in terms of body sensations, and therapists may teach such individuals cognitive strategies for examining body sensations.
In both cases, while the Mind or the Body provide the entry into treatment, the end goal is to increase capacity at both poles and to encourage flexible movement. As illustrated by embodiment research, a body-based intervention has ramifications for mental processes of cognition, judgment, and social interaction. Similarly, cognitive interventions can impact physical processes such as regulating heart rate and blood pressure. Again, mind and body are intimately connected, and each of the three axes exist in dynamic relationship with each other.
In selecting the intervention, it remains important for the clinician to consider the individual’s unique state and background. Is a lack of balance due, not to a lack of capacity, but rather to a recent traumatic event that has cut off access to it? Dissociation, for instance, is a common reaction to severe trauma and can translate into an avoidance of the Body/Physical Phenomena and Lived Body/Body as Subject poles of the model. However, the momentary loss of the capacity to access these poles is different from a case where the individual, for biological or early childhood trauma reasons, never gained it. Disability, developmental delay, and biological limitations may all influence the individual’s lived experience and must be taken into account.
An individual with schizophrenia may be conceptualized as follows in Figure 3.6.
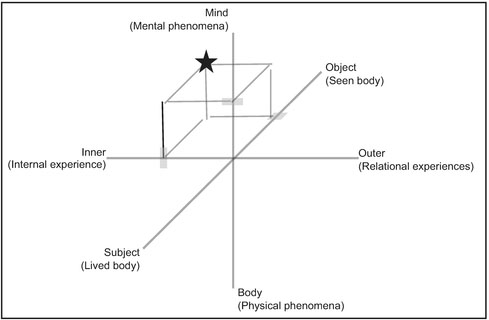
Figure 3.6 Schizophrenia conceptualization
This is an individual who is imbalanced, with limited access to the poles of Outer and Subject, and inflexible, with little ability to move between the extremes. The first step, then, would be to build the individual’s capacity to access a complete range of embodiment experiences. Interventions to increase access to the Outer world may include the dance/movement therapy technique of mirroring, where a therapist coaxes the individual into the intersubjective space through the matching of movements and movement quality, or dance/movement therapy groups, where the individual is placed in a space with others and encouraged to interact through the use of music, rhythm, props, and games. Interventions to increase awareness of the Subject body may include progressive muscle relaxation, focusing on the breath, and guided body scans.
It is possible that the individual’s limited capacities are related to chemical imbalances in the brain and body. A lack of proprioceptive ability, which may translate to a lack of ability to experience the Subject body, may be the result of biological abnormalities. In such cases, administration of pharmacological interventions may be necessary.
As the individual’s capacity to access a wider range increases, the focus of therapeutic interventions shifts to address their ability to flexibly move between poles as the environment requires. Structured and mindful movement styles such as yoga may encourage integration of Mind and Body. Social dances, such as ballroom or Latin dancing, encourage both Inner and Outer focus, as the individual learns to balance their own impulses with cues given by their partner. Finally, practicing movement in a mirrored studio space allows the individual to practice experiencing the Subject body while being simultaneously aware of the Object body, or the body the individual observes in the mirror.
In this manner, the proposed framework provides direction for designing therapeutic interventions to help an individual achieve better balance and increased capacity for interacting with the environment.
This chapter outlined the beginnings of a clinical theory of embodiment. The framework presented offers a method of understanding mental illness as existing on a multi-dimensional continuum and defines health in terms of balance and flexibility, rather than symptomology or traits. It provides a structure for categorizing a broad range of mental illness and for selecting clinical interventions based on the individual’s needs. It also brings attention to the lived experience of the individual, as opposed to diagnostic criteria identified by an outside observer and highlights the importance of the here-and-now in clinical work.
This approach carries a number of benefits. First, by drawing from advances in phenomenological theory and current embodiment research, it is positioned at the forefront of research. It questions the assumption that psychiatric illness is a purely ‘mental’ phenomenon, an assumption that has been challenged by empirical data illustrating the substantial connection between the mind and the body. In addition, building this bridge between psychology and embodiment provides a basis for explaining phenomena such as the effectiveness of psychiatric medication and the use of body-based methods in treating mental illness. In sum, a clinical theory grounded upon embodiment most accurately reflects the latest developments in the understanding and treatment of mental illness and incorporating current research into one clinical theory provides an invaluable tool for clinicians and researchers.
Second, an approach that values the lived experience of individuals and places the choice of intervention in the hands of the individual both normalizes the range of human experience and empowers individuals to take control of their own treatment. Current diagnostic trends and societal stereotypes stigmatize mental illness, leaving those suffering from mental illness feeling ashamed, broken, or fundamentally different from others. Distinguishing between those who are ‘normal’ and those with mental illness creates a sense of other-ness that may leave those with diagnoses feeling helpless, incapable of reaching normalcy, while discouraging those without diagnoses from seeking treatment. The clinical theory of embodiment presented in this chapter places both mental illness and mental health on one continuum, illustrating how one can move between illness and health due to imbalance or rigidity. It offers a way for understanding how mental illness may be caused and, consequently, how it may be cured.
Third, this approach provides a language to bridge the gap between clinical language and alternative treatment methods such as yoga, meditation, dance, and the creative arts. Thus far, these treatment methods have been shown to be effective in outcome studies (eg. Koch, Kunz, Lykou, and Cruz, 2013).
However, the mechanisms by which they are effective and how they relate to mental illness remain a mystery. The proposed clinical theory includes potential mechanisms that may explain effectiveness. For instance, a treatment such as dance/movement therapy groups may work by bridging Inner and Outer experiences, as the individual simultaneously experiences internal body sensations while being seen and interacting with other members. A treatment such as yoga encourages integration of Mind and Body, as individuals are encouraged simultaneously to be mindful of their movement and to concentrate on physical sensations to achieve various poses. Thus, the proposed clinical theory offers a language to begin to explain the relationship between alternative therapies and mental health.
Finally, embracing this new approach, one grounded on embodiment and lived experiences, organizes current research while highlighting a research agenda for future investigation. Existing research can be categorized according to which continuum of health and illness it addresses. In this way, previously unrelated research and methods can be compared and integrated. Results need no longer be isolated according to field (such as social psychology versus cognitive science) or diagnosis (such as depression, trauma, or attention deficit hyperactivity disorder) but can be analysed in relation to each other and to their connection to embodied understandings of health and illness. Applying this lens of analysis may, in turn, further elucidate these complex categories and point the way towards future research questions. Each category and continuum presented in this chapter is preliminary and, thus far, very broadly defined. Much can be done to further clarify what is meant by Body/Mind, Inner/Outer, and Subject/Object. A clinical theory of embodiment thus provides the foundation both for understanding current research and lighting the way for future investigation.
It must be noted that an embodied clinical theory, based on lived experiences and the connection between mind and body, differs fundamentally from other diagnostic tools such as the DSM 5. The theoretical orientations of phenomenology, which emphasizes subjectivity and lived experience, may not be compatible with post-positivism, which emphasizes objectivity and external observation (Mertens, 2010). These differences play out in fundamental issues such as the definition of health and illness, whether or not there is one ‘right’ diagnosis, what training or professional role is required for the ability to give a diagnosis, and how to measure the efficacy of an intervention. Thus far, the majority of mental health treatment has spawned from the theoretical orientation of post-positivism. Phenomenological approaches, as proposed in this chapter, are gaining support from clinical practitioners but remain on the sidelines. Acknowledging this fundamental difference and contributing to a body of knowledge grounded in phenomenology and embodiment can only strengthen the dialogue between these two theoretical orientations and, in turn, increase our understanding and ability to treat mental illness.
Embodiment research and phenomenological theory provide the foundation for a clinical theory based on the mind-body connection and individual lived experiences. The disconnection between current clinical practice, which is grounded primarily in a disembodied conceptualization of mental illness and in an external observation of symptoms, and growing research, theory, and clinical evidence on the importance of embodied approaches, highlights the need for the development of such a theory. The proposed theory includes a framework on which individuals may be conceptualized and on which interventions can be based. This framework envisions mental illness and health as falling on a continuum and values balance and flexibility over unilateral improvement of symptoms. It identifies three axes—Decision, Identity, and Focus—on which an individual may be situated. The proposed clinical theory and associated framework represent a significant departure from current post-positivist diagnostic language and provides a structure upon which current research may be organized, empirical data may be analysed, and future research may be guided.
Bargh, J. A., Chen, M., and Burrows, L. (1996). Automaticity of social behavior: Direct effects of trait construct and stereotype activation on action. Journal of Personality and Social Psychology, 71(2), 230–244.
Benson, H., and Klipper, M. Z. (1992). The relaxation response. New York, NY: HarperCollins.
Cesario, J., Plaks, J. E., and Higgins, E. T. (2006). Automatic social behavior as motivated preparation to interact. Journal of Personality and Social Psychology, 90(6), 893–910.
Davis, M. (1997). Guide to movement analysis methods. Part 2: Movement Psychodiagnostic Inventory (Unpublished manual). Available from Martha Davis.
Dell, C. (1970). Primer for movement description using effort/shape (2nd ed.). New York, NY: Dance Notation Bureau Press.
Fuchs, T. (2010). Phenomenology and psychopathology. In D. Schmicking and S. Gallagher (Eds.), Handbook of phenomenology and cognitive science (pp. 547–573). Dordrecht, Netherlands: Springer Science + Business Media B.V.
Fuchs, T. (2012). The phenomenology of body memory. In S. Koch, T. Fuchs, M. Summa, and C. Müller (Eds.), Body memory, metaphor, and movement (pp. 9–22). Philadelphia, PA: John Benjamins Publishing Company.
Homann, K. B. (2010). Embodied concepts of neurobiology in dance/movement therapy practice. American Journal of Dance Therapy, 32, 80–99.
Kestenberg-Amighi, J., Loman, S., Lewis, P., and Sossin, K. M. (1999). The meaning of movement: Developmental and clinical perspectives of the Kestenberg Movement Profile. New York, NY: Brunner-Routledge.
Koch, S., Holland, R. W., Hengstler, M., and van Knippenberg, A. (2009). Body locomation as regulatory process: Stepping backward enhances cognitive control. Psychological Science, 20(5), 549–550.
Koch, S., Kunz, T., Lykou, S., and Cruz, R. (2013). Effects of dance movement therapy and dance on health-related psychological outcomes: A meta-analysis. The Arts in Psychotherapy, 41(1), 46–64.
Koch, S. C. (2014). Rhythm is it: Effects of dynamic body feedback on affect, attitudes and cognition. Frontiers in Psychology, 5, 537.
Levy, F. (2005). Dance movement therapy: A healing art. Reston, VA: AHERF.
Linehan, M. M. (1993). Skills training manual for treating borderline personality disorder. New York, NY: Guilford.
Meier, B. P., and Robinson, M. D. (2004). Why the sunny side is up: Associations between affect and vertical position. Psychological Science, 15(4), 243–247.
Meier, B. P., and Robinson, M. D. (2006). Does “feeling down” mean seeing down? Depressive symptoms and vertical selective attention. Journal of Research in Personality, 40(4), 451–461.
Mertens, D. M. (2010). Research and evaluation in education and psychology: Integrating diversity with quantitative, qualitative, and mixed methods (3rd ed.). Thousand Oaks, CA: Sage Publications.
Michalak, J., Troje, N. J., Fischer, J., Vollmar, P., Heidenrech, T., and Schulte, D. (2009). Embodiment of sadness and depression: Gait patterns associated with dysphoric mood. Psychosomatic Medicine, 71, 580–587.
Miles, L. K., Nind, L. K., and Macrae, C. N. (2010). Moving through time. Psychological Science, 21(2), 222–223.
Niedenthal, P. M., Barsalou, L. W., Winkielman, P., Krauth-Gruber, S., and Ric, F. (2005). Embodiment in attitudes, social perception, and emotion. Personality and Social Psychology Review, 9(3), 184–211.
Pallagrosi, M. F. L., Picardi, A., and Biondi, M. (2014). Assessing clinician’s subjective experience during interaction with patients. Psychopathology, 47, 111–118.
Pulvermüller, F. (1999). Words in the brain’s language. Behavioral and Brain Sciences, 22(2), 253–279.
Pulvermüller, F. (2013). How neurons make meaning: Brain mechanisms for embodied and abstract-symbolic semantics. Trends in Cognitive Sciences, 17(9), 458–470.
Serlin, I. A. (1996). Kinesthetic imaging. Journal of Humanistic Psychology, 36(2), 25–33.
Soma, C. (2016). Advanced mind-body interventions. Harrisburg, PA: The National Institute of Trauma and Loss in Children.
van der Kolk, B. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. New York, NY: Penguin Books.
Williams, L. E., and Bargh, J. A. (2008). Experiencing physical warmth promotes interpersonal warmth. Science, 322(5901), 606–607.