Cardiologists and public health officials, responsible for the medical care of patients living in developing regions of the world, are faced with the unique challenge of a wide spectrum of cardiac diseases: valvular and heart muscle diseases of infectious aetiology and chronic degenerative diseases such as hypertensive and coronary heart diseases. Therefore, knowledge about cardiac diseases affecting developing countries should include epidemiological explanations for their heterogeneity as well as the distinctive characteristics of individual cardiac diseases.
According to the World Bank, countries with a gross national income per capita lower than US$9200 are considered low- and middle-income countries. These countries are located in six regions of the world: East Asia and the Pacific, Central Asia and Europe, South Asia, Middle East and North Africa, Sub-Saharan Africa and Latin America and the Caribbean.
Cardiovascular diseases and cardiovascular mortality have decreased progressively in the last decades in most high-income countries. However, low- and middle-income countries show just the opposite tendencies. More than two-thirds of the world cardiovascular deaths occur in these countries, the prevalence of risk factors is also increasing and cardiovascular diseases are the leading causes of death. Cardiovascular deaths affect the population at the peak of their working age and the benefits of secondary prevention are not readily available to all patients (Joshi et al. 2008). These obvious differences, with developed countries are probably due to the stage of epidemiological transition. Low- and middle-income countries are undergoing or have partially experienced the epidemiological transition from the ages of pestilence–famine and receding epidemics to the age of degenerative and man-made diseases (Gaziano 2007).
The prevalence of certain cardiac diseases is closely related to the degree of economic development and social organization. Thus, malnutrition and infectious diseases lead to rheumatic heart disease and its long-term effects on heart valves. These cardiac diseases are most prevalent in sub-Saharan Africa, rural areas of Latin America, South Asia, and in the indigenous populations of Australia and New Zealand. Chagas’ disease, which mainly affects heart muscle and is particularly related to housing conditions, is endemically present in Latin America. However, migration of infected individuals has now extended this endemic disease to high-income countries. Industrialization, improved nutrition, and control of infections have allowed for the transition to the next two stages: receding pandemics and degenerative and man-made diseases. Chronic diseases such as hypertension and its disabling consequence (i.e. ischaemic stroke) are now present. Risk factors for coronary artery disease (cigarette smoking, diabetes mellitus, and obesity) show a marked tendency to increase (Gaziano 2007; Bestetti et al. 2008).
• Deaths because of cardiovascular diseases were estimated worldwide, by the year 2005, at 17.5 million.
• Eighty per cent of all cardiovascular deaths occur in low-and middle-income countries.
• Cardiovascular diseases are the main causes of death in persons of all ages, in developing countries.
• One-half of all cardiovascular deaths affect the population under 70 years of age.
• Loss of economic production from heart disease, stroke and diabetes, by the year 2015, has been estimated in US$84 billion.
Twenty million people living in South America have Chagas’ disease due to infection by Trypanosoma cruzi. Recent surveys among blood donors indicate that in some regions up 3.4 percent of the population have positive serological tests. In the early stages of this disease, myocardial damage is localized and progresses to a diffuse form of a congestive cardiomyopathy, which is a common cause of hospitalization for congestive heart failure. Compared with congestive heart failure of other aetiologies, Chagas’ cardiomyopathy is considered to be the main prognostic factor of mortality. However, when chagasic patients with congestive heart failure are given the same non-specific treatment strategy, based on beta-adrenergic blockers, mortality is similar to that of patients with non-chagasic heart failure (Bestetti et al. 2008).
Rheumatic heart disease affects about 15.6 million people worldwide. It is estimated that every year about 300 000 individuals develop rheumatic heart disease. The incidence of acute rheumatic fever in children from developing countries is four to five times higher than in high-income countries. Indigenous populations of Australia and New Zealand have an incidence of 80% per 100 000 children, whereas the non-indigenous population of these two same countries is less than 10% per 100.000 children (Carapetis et al. 2005). The prevalence of rheumatic heart disease is also heterogeneous and related to the diagnostic strategies used for diagnosis (Marijon et al. 2007). Thus, in countries like Cambodia and Mozambique, systematic screening with echocardiography has shown a much higher prevalence than clinical screening (21.5 cases per 1000 children versus 2.2 cases per 1000 children. Different prevalences, notwithstanding the current controversy (changing virulence of group A streptococci versus changing living conditions), are now present in countries like China, where hospitalizations due to rheumatic heart disease have declined from 50% in 1948–57 to 2% in 2000–5 (Cheng 2009).
• Self-limited febrile illness, usually diagnosed in about 5% of infected individuals.
• Asymptomatic stage, with normal cardiac findings. Very low morbidity and good prognosis. Fifty per cent of the patients will progress to a chronic cardiac or digestive form (Brazil).
• Cardiac rhythm and conduction abnormalities. Symptoms and signs of congestive heart failure.
• Two positive serologic tests (indirect immunofluorescence, indirect haemagglutination, or enzyme-linked immunosorbent assay (ELISA)) and evidence of cardiomyopathy.
• Impaired left ventricular function, New York Heart Association functional classes III/IV, cardiomegaly, non-sustained ventricular tachycardia, and no treatment with beta-adrenergic blockers.
Specific treatment with benznidazol is currently indicated only in patients with unequivocal evidences of, or at high risk for, acute infection by Trypanosoma cruzi (organ transplant and immunosuppression). Cardiac arrhythmias and congestive symptoms should be treated as in non-chagasic heart diseases.
• 15 million cases of rheumatic heart disease are found in developing countries.
• Rheumatic heart disease is present in 1–2% of Latin American children.
• The prevalence of rheumatic heart disease increases with age, reaching its peak by age 25–34 years.
• Mitral regurgitation is the dominant lesion, but stenosis becomes more common with increasing age.
Risk factors for coronary artery disease and stroke are on the rise in most low- and middle-income countries. At the present time, diabetes affects more than 150 million people of the entire world population. By the year 2025, the rate of increase will be 170% in low- and middle-income countries compared to 42% in high-income countries. The population affected is between 45 and 65 years of age, and as in developed countries it is detected in subjects over 65. Concerning tobacco use, about 1 billion people are smokers and more than two-thirds of them reside in developing countries. The prevalence of smoking among adult men in Russia has increased from 57% to 62%. In contrast, Australia decreased its prevalence from 28% to 25%. Quit rates are very low and range from 5% to 2% in countries like China and India respectively (Gaziano 2007; Joshi et al. 2008).
Average blood pressure levels, for all ages, are highest in Eastern Europe, Russia, Middle East, North Africa and sub-Saharan Africa. Prospective studies carried out in white and Asian populations have demonstrated a direct continuous association of usual levels of systolic and diastolic blood pressure with the risk of coronary heart disease and stroke. The prevalence of these risk factors in Latin America has similar patterns (Cubillos-Garzón et al. 2004; Perkovic et al. 2007).
Myocardial damage induces, regardless of the underlying aetiology, maladaptative and compensatory mechanisms that ultimately lead to heart failure. Earlier investigations in low-income countries attributed heart failure to cardiomyopathy and valvular heart disease. However, more recent studies in Africa and Latin America clearly indicate that, in the developing world, the most common causes of congestive heart failure are hypertension and coronary artery disease (Cubillos-Garzón et al. 2004; Stewart et al. 2008). In other words, epidemiological transition is also modifying the spectrum of heart diseases responsible for heart failure.
• Stroke-related deaths in certain developing countries among people age 15–59 years is three to eight times than in high-income countries.
• Less than one-fifth of those patients with past medical history of cardiovascular disease have access to secondary prevention treatment.
• WHO budget: $7.50 is spent per communicable disease death, only $0.50 is spent per death from chronic disease.
• In Latin American countries, the ratio of deaths from cardiac diseases to deaths from infectious diseases will rise from 1.1 to 4.75.
• Prevalence of hypertension in urban populations of Latin American countries: 14.1 in Colombia to 32.0 in Mexico.
• Prevalence of obesity in urban populations of Latin American countries: 6.9 in Brazil to 25.7 in Paraguay.
• Prevalence of diabetes in urban populations of Latin American countries: 4.0 in Chile to 8.5 in Argentina.
The vast majority of scientific articles published between 1995 and 2002 originated from Western Europe (39.4%) and the USA (37.1%). The USA, Oceania, and Canada had the highest mean impact factor. The number of scientific articles from Eastern Europe, Latin America and the Caribbean, and Asia was much smaller. Although, the contribution of Africa was very low, the rate of increase in the number of published articles was higher than in developed countries. This promising trend will surely provide new knowledge and therapeutic strategies to reduce the growing burden of cardiovascular diseases on the developing world.
Bestetti RB, Tatiana AD, Theodoropoulos TAD, et al. Treatment of chronic systolic heart failure secondary to Chagas heart disease in the current era of heart failure therapy. Am Heart J 2008;156:422–30.
Carapetis JR, McDonald M, Wilson NJ. Acute rheumatic fever. Lancet 2005;366:155–168.
Cheng TO. Editorial How much of the recent decline in rheumatic heart disease in China can be explained by changes in cardiovascular risk factors?. Int J Cardiol 2009;132:300–2.
Cubillos-Garzón LA, Casas JP, Morillo CA, Bautista LE. Congestive heart failure in Latin America: The next epidemic. Am Heart J 2004;147:412–17.
Gaziano TA. Reducing the global burden of cardiovascular disease in the developing world. Health Affairs 2007;26:13–24.
Joshi R, Jan S, Wu Y, MacMahon S. Global inequalities in access to cardiovascular health care. J Am Coll Cardiol 2008;52:1877–25.
Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 2007;357:470–6.
Perkovic V, Huxley R, Wu Y, et al. The burden of blood pressure-related: A neglected priority for global health. Hypertension 2007;50:991–7.
Rosmarakis ES, Vergidis PI, Soteriades ES, et al. Estimates of global production in cardiovascular diseases research. Int J Cardiol 2005;100:443–9.
Stewart S, Wilkinson D, Hansen C. Predominance of Heart Failure in the Heart of Soweto Study Cohort: Emerging Challenges for Urban African Communities. Circulation 2008;118:2360–7.
Coronary artery disease remains the major cause of morbidity and mortality worldwide. Despite recent advances in reperfusion therapy for acute myocardial infarction (MI) and pharmacotherapy for post MI left ventricular (LV) remodelling, an increasing trend of incidence and mortality is observed. In this regard, stem cell and gene therapies have emerged as potential novel therapies for patients with acute MI, heart failure, and chronic myocardial ischaemia.
• Stem cell-based therapy relies on the belief that exogenous cells or mobilized endogenous cells can transdifferentiate into mature cardiomyocytes (CMs) and integrates both electrically and mechanically with host CMs to improvement of cardiac function.
• In addition, data have demonstrated that cellular mediated paracrine effects also played an important role for the improvement in LV function by secreting proangiogenic cytokines to enhance neovascularization.
• The paracrine factors secreted from the transplanted cells exert anti-apoptotic effects, alter the restoration of extracellular matrix and recruit endogenous stem cells.
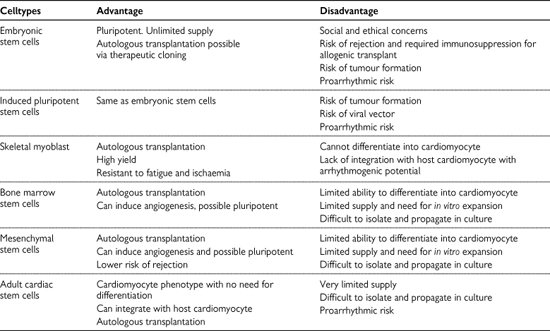
• Various types of stem or progenitor cells, including bone marrow (BM)-derived cells, placental/cord blood-derived cells, adipose tissue-derived cells, resident cardiac progenitor cells, embryonic stem cells and induced pluripotent stem cells, have been investigated for cardiac repair. Their advantages and disadvantages are shown in Table 12.14.1.
• One of the greatest challenges in stem cell therapy is optimal delivery, engraftment, and survival of transplanted cells.
• The homing and engraftment of stem or progenitor cells after administration relies on the method of cell delivery, the characteristics of transplanted cells, and the host environment.
• In addition to direct cell delivery, mobilization of endogenous stem cell can be achieved by administration of cytokines or growth factors.
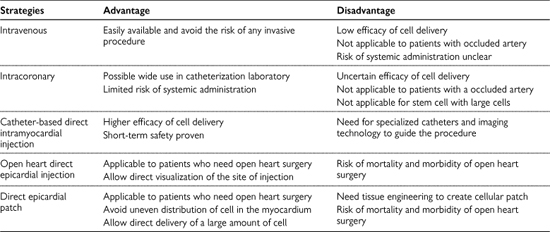
• Potential application of different methods of cell delivery is shown in Table 12.14.2.
• In the setting of acute MI, stem cells can be delivered by intravenous or intracoronary routes after coronary revascularization. The intravenous infusion is the simplest approach, but have a low efficacy for cellular engraftment (<1%) due to the cell trapping in the other organs. However, both intravenous and intracoronary routes are not suitable for patients with an occluded artery and for delivery of stem cells of larger size or limited migration ability, such as skeletal myoblasts due to risk of microembolization.
• For patients with chronic myocardial ischaemia, direct intramyocardial injection via either surgical epicardial or transcatheter endocardial approaches is needed for optimal cell delivery. These techniques allow direct cell delivery into the targeted regions even in patients with occluded artery and with the use of certain larger cell types.
• Finally, in patients with post-MI heart failure due to large area of infarcted and non-viable myocardium, direct injection of stem cells into myocardium scar will result in low graft survival and differentiation. Therefore, the use of bioengineering approaches, such as cardiac patches and injectable delivery matrices may be needed to improve cell retention, survival, and differentiation. Nevertheless, the safety and efficacy of this approach has not been tested in clinical trials due to the lack of optimal technique to create three-dimensional viable cellular patches.
Table 12.14.1 Different types of stem cells for cardiovascular diseases
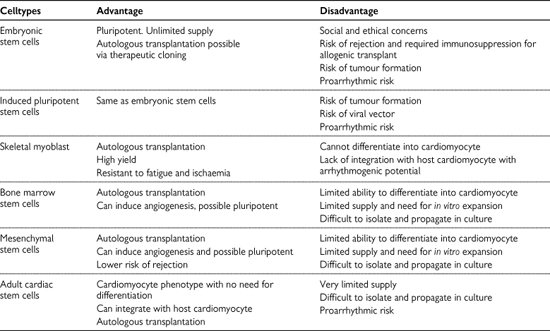
Table 12.14.2 Potential clinical strategies for stem cell delivery
• In patients with acute MI, the majority of randomized controlled clinical trials are focused on the use of intracoronary administration of autologous BM cells in patients who had undergone successful percutaneous coronary intervention of infarcted related artery.
• These studies yielded mixed results on the effect of intracoronary administration of BM cells due to relative small patients sample size (<200), differences in the study population, the dosage, preparation and types of cells, timing of cell transfer, and the methodology of functional assessment. Nevertheless, none of these studies showed major adverse effects.
• Trials have demonstrated a modest (~3–4%) but significant improvement in left ventricular ejection fraction and a small reduction in infarct scar size and left ventricular dimension (Siu et al. 2010).
• Clinical efficacy of intracoronary BM cells therapy, the optimal timing and dosage of cell administration required several larger ongoing trials to address.
• There are only two randomized controlled clinical trials on the use autologous BM or skeletal myoblast in patients with congestive heart failure after MI (Siu et al. 2010).
• Patients received intracoronary BM cell transplantation but not circulating progenitor cells showed a modest but significant improvement in LV ejection fraction (2.9%) at 3 months compared with controls. However, there was no difference in LV dimension after cell transplantation.
• The Myoblast Autologous Grafting in Ischemic Cardiomyopathy (MAGIC) trial investigated the safety and efficacy of low dose (400 × 106) or high-dose (800 × 106) autologous skeletal myoblasts versus placebo in patients with ischaemic cardiomyopathy and indication for coronary artery bypass grafting. Because of the safety concern of proarrhythmia in the early pilot studies, all patients were treated with implantable cardioverter-defibrillators before transplantation. At 6 months there were no significant differences in regional or global LV function as determined by echocardiogram and arrhythmia events among these three groups. However, patients receiving the highest dose of cells had a significant decrease in LV end-diastolic and end-systolic volume as compared with control, suggesting the possibility of reverse remodelling.
• In contrast to acute MI, there are only a few small randomized controlled clinical trials on stem cell therapy for treatment of refractory angina due to chronic myocardial ischaemia.
• These trials mainly focused on the use of intramyocardial injections of BM cells into chronic ischemic myocardium which are not amenable to conventional coronary revascularization (Siu et al. 2010).
• In these studies, cell transplantation was performed by three-dimensional electromechanical mapping guided catheter-based intramyocardial injection into the ischaemic myocardium as described previously. Use in chronic ischaemic myocardium not amendable to conventional coronary revascularization.
• An improvement in clinical status, angina frequency, exercise capacity, and left ventricular ejection fraction has been demonstrated in these trials.
• No significant adverse events including cardiac arrhythmias have been reported.
Gene therapy is a potential new treatment of cardiovascular disease and may provide a novel approach to treat patients with both genetic disorders and acquired pathophysiologies such as arteriosclerosis, heart failure, and arrhythmias. Recombinant DNA technology and the sequencing of the human genome have identified many candidate therapeutic genes available for cardiovascular diseases. However, the major challenge in the field of gene therapy for cardiovascular disease is to develop effective and safe gene delivery systems for localizing gene therapy to specific sites to optimize transgene expression and efficacy.
• Several pathological alterations that occur during heart failure have been targets for gene therapy, but main focus has been emphasized on restoring Ca2+ transport using gene therapy, including SERCA2a, phospholamban (PLB), ryanodine receptor (RyR2), and the sodium–calcium exchanger (NCX).
• Among them, SERCA has proven a very promising candidate for gene transfer because its expression and activity are decreased in a wide variety of pathologic conditions in heart failure.
• One phase I clinical trial (CUPID trial: Calcium Up-Regulation by Percutaneous Administration of Gene Therapy in Cardiac Disease) using SERCA2 gene transfer (AAV1-SERCA2a, Mydicar; Celladon Corporation, La Jolla, CA) in patients with congestive heart failure has been completed. Seven of nine patients treated showed improvements over 6 months in several areas: symptomatic (five patients), functional (four patients), biomarker (two patients) and left ventricular function/remodelling (six patients). Two patients with pre-existing antibodies to the viral vector delivery system did not show improvements. Importantly, the approach was shown to have an acceptable safety profile. Currently, Phase II CUPID trial is ongoing.
• Furthermore, another phase I study using AAV6-SERCA2a to evaluate efficacy and safety in ischemic patients undergoing left ventricular assist placement is also planned.
Gnecchi M, Zhang Z, Ni A, et al. Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res 2008;103:1204–19.
Habib M, Caspi O, Gepstein L. Human embryonic stem cells for cardiomyogenesis. J Mol Cell Cardiol 2008;45:462–74.
Menasche P. Stem cells for clinical use in cardiovascular medicine: current limitations and future perspectives. Thromb Haemost 2005;94:697–701.
Siu CW, Liao SY, Liu Y, et al. Stem cells for myocardial repair. Thromb Haemost 2010;104:6–12.