CASE 4
A healthy 25-year-old man is undergoing a brief surgical procedure (inguinal hernia repair) requiring general anesthesia. Intubation and induction of anesthesia using IV succinylcholine and inhaled halothane proceed unremarkably. During surgery the patient develops muscle rigidity and tachycardia, and his temperature rapidly rises.
 What is the mechanism of action of succinylcholine?
What is the mechanism of action of succinylcholine?
 What reaction is occurring in the patient?
What reaction is occurring in the patient?
 What drug should immediately be given to the patient, and what is its mechanism of action?
What drug should immediately be given to the patient, and what is its mechanism of action?
ANSWERS TO CASE 4:
Skeletal Muscle Relaxants
Summary: A 25-year-old man develops muscle rigidity, tachycardia, and high fever during surgery.
 Mechanism of action of succinylcholine: Nicotinic receptor agonist at the motor endplate of the neuromuscular junction, which causes persistent stimulation and depolarization of muscle cells.
Mechanism of action of succinylcholine: Nicotinic receptor agonist at the motor endplate of the neuromuscular junction, which causes persistent stimulation and depolarization of muscle cells.
 Reaction that is occurring: Malignant hyperthermia.
Reaction that is occurring: Malignant hyperthermia.
 Drug given for treatment and its mechanism of action: Dantrolene, which acts by interfering with calcium release from the sarcoplasmic reticulum.
Drug given for treatment and its mechanism of action: Dantrolene, which acts by interfering with calcium release from the sarcoplasmic reticulum.
CLINICAL CORRELATION
Succinylcholine is the only depolarizing neuromuscular agent in wide clinical use. It is used for the rapid induction of a brief flaccid paralysis. It works as an agonist of the nicotinic receptor at the motor endplate of the neuromuscular junction. This causes a persistent stimulation and depolarization of the muscle, preventing stimulation of contraction by ACh. It has a rapid onset and short duration of action because it is quickly hydrolyzed by plasma and liver cholinesterase.
Malignant hyperthermia, a rare but significant cause of anesthetic morbidity and mortality, is an inherited autosomal dominant disorder that results in tachycardia, muscle rigidity, and high body temperatures in response to the use of certain inhaled anesthetics in combination with muscle relaxants, usually succinylcholine. It is caused by a release of calcium ions from the sarcoplasmic reticulum in muscle cells. Dantrolene interferes with this release and is therefore the treatment of choice for this condition.
APPROACH TO:
Pharmacology of Skeletal Muscle Relaxants
OBJECTIVES
1. Contrast the mechanism of action of depolarizing and nondepolarizing neuromuscular junction-blocking agents.
2. List the therapeutic uses and adverse effects of skeletal muscle relaxants.
DEFINITIONS
Hyperkalemia: Elevated levels of the electrolyte potassium in the serum.
Myalgia: Pain originating in skeletal muscle.
Depolarizing neuromuscular agent: A drug that acts at the neuromuscular junction to prevent the initiation of an action potential by ACh.
DISCUSSION
Class
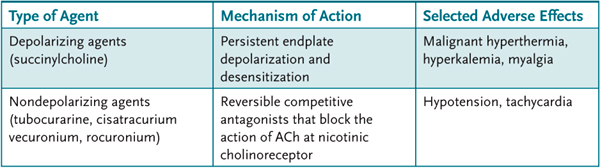
Neuromuscular blocking agents are classified as either depolarizing or nondepolarizing (Table 4–1) and are used mostly as adjuncts with general anesthetics to block activity of ACh at the neuromuscular junction.
Table 4–1 • SELECTED SKELETAL MUSCLE RELAXANTS
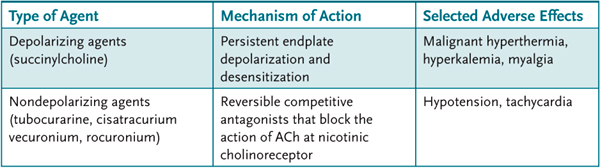
Succinylcholine is the prototype for depolarizing agents and used for brief paralysis for surgery and for intubation. Tubocurarine, the prototype, and other nondepolarizing agents (eg, cisatracurium, vecuronium, rocuronium) are used for longer term paralysis for surgery.
In addition to malignant hyperthermia, succinylcholine administration may result in hyperkalemia, particularly in patients with burn and trauma, which could result in cardiac arrest. Myalgia is also commonly reported. It is contraindicated in patients with neuromuscular disease, such as myasthenia gravis and muscular dystrophy, as well as in stroke. Bradycardia may also occur, but can be prevented by pretreatment with atropine.
Certain nondepolarizing agents may produce hypotension, as a result of histamine release and some ganglionic blocking activity, and tachycardia as a result of vagolytic activity. The effects of nondepolarizing agents may be reversed by the acetylcholinesterase inhibitor, neostigmine.
Numerous drug interactions between neuromuscular blocking agents and other drugs have been reported that lead to increased neuromuscular blockade, particularly with certain antibiotics and inhaled anesthetics.
Structure
The neuromuscular blocking agents resemble ACh (succinylcholine contains two linked ACh molecules) and contain one or two quaternary nitrogens that limit entry into the CNS.
Mechanism of Action
After a single dose, succinylcholine occupies the nicotinic receptor to produce a persistent endplate depolarization (phase I block) that results in flaccid paralysis because the muscles become unresponsive to endogenously released ACh. The initial depolarization is accompanied by muscle fasciculations. Continued exposure of endplates to succinylcholine results in their repolarization. However, through an unclear mechanism, they become relatively insensitive to subsequent depolarization (so-called desensitization, or phase II block).
Nondepolarizing blocking agents act as reversible competitive antagonists that block the action of ACh at nicotinic cholinoreceptors in muscle endplates and autonomic ganglia. In contrast to succinylcholine, which has a duration of action of about 6–10 min, the nondepolarizing agents have a longer duration of action (up to an hour).
Cholinesterase inhibitors (eg, neostigmine, pyridostigmine) can effectively antagonize and reverse the neuromuscular blocking action of nondepolarizing agents and succinylcholine during phase II. However, they will augment the action of succinylcholine during phase I.
Administration
The neuromuscular blocking agents are highly polar and therefore must be administered parenterally. Most nondepolarizing agents are eliminated through the kidney. Succinylcholine is eliminated by the hydrolytic action of plasma butyrylcholinesterase (pseudocholinesterase).
Pharmacokinetics
Neuromuscular blocking agents are highly ionized and therefore have limited volume of distribution and limited access to the CNS.
COMPREHENSION QUESTIONS
4.1 The use of succinylcholine as an adjunct to general anesthetics during surgery is based on its ability to:
A. Block the action of ACh at the motor endplate
B. Increase release of ACh from autonomic ganglia
C. Increase release of histamine from mast cells
D. Inhibit cholinesterase
4.2 Continued exposure of muscle endplates to succinylcholine results in their:
A. Conversion to ion channels
B. Enhanced sensitivity to ACh
C. Regeneration of ACh receptors
D. Repolarization
4.3 Cholinesterase inhibitors can reverse the action of which of the following?
A. Cisatracurium
B. Succinylcholine
C. Both A and B
D. Neither A nor B
4.4 A 35-year-old man undergoes surgery for a hernia repair. After the surgery, he complains of diffuse muscle aches, which the anesthesiologist states is likely caused by the skeletal muscle relaxant. He has a temperature of 37.8°C (100°F). Which of the following is the most accurate statement?
A. The agent also commonly causes hypokalemia.
B. The agent blocks ACh at the nicotinic receptor.
C. The agent causes persistent endplate depolarization and desensitization.
D. The patient likely has malignant hyperthermia.
ANSWERS
4.1 A. Succinylcholine acts like ACh to cause depolarization of the muscle endplate. However, unlike ACh, succinylcholine is not metabolized at the synapse. Therefore, the endplate remains depolarized and unresponsive to endogenous ACh, resulting in muscle paralysis.
4.2 D. Continued exposure of the muscle endplate to succinylcholine results in desensitization (phase II block) where the endplate repolarizes but cannot readily be depolarized.
4.3 C. Cholinesterase inhibitors like neostigmine can effectively antagonize and reverse the neuromuscular blocking action of nondepolarizing agents and succinylcholine during phase II. However, they will augment the action of succinylcholine during phase I.
4.4 C. Myalgia (muscle aches) is a common adverse reaction of depolarizing agents such as succinylcholine; these agents also may induce hyperkalemia and malignant hyperthermia.
PHARMACOLOGY PEARLS
 Malignant hyperthermia is a rare autosomal dominant disorder characterized by tachycardia, muscle rigidity, and high body temperatures, which occurs when the patient is exposed to inhaled anesthetics in combination with muscle relaxants, usually succinylcholine.
Malignant hyperthermia is a rare autosomal dominant disorder characterized by tachycardia, muscle rigidity, and high body temperatures, which occurs when the patient is exposed to inhaled anesthetics in combination with muscle relaxants, usually succinylcholine.
 Dantrolene interferes with the release of intracellular calcium and is therefore used to treat the muscle rigidity and hyperthermia associated with malignant hyperthermia.
Dantrolene interferes with the release of intracellular calcium and is therefore used to treat the muscle rigidity and hyperthermia associated with malignant hyperthermia.
 The neuromuscular blocking agents are highly polar and highly ionized and, therefore, must be administered parenterally and have limited volume of distribution and limited access to the CNS.
The neuromuscular blocking agents are highly polar and highly ionized and, therefore, must be administered parenterally and have limited volume of distribution and limited access to the CNS.
 A small number of patients (1:10,000) with atypical cholinesterase experience long-lasting apnea of 1–4 hours following succinylcholine (or the nondepolarizing neuromuscular blocking drug mivacurium that is also eliminated by the action of butyrylcholinesterase). Mechanical ventilation is used to manage the apnea even though prescreening could detect this rare condition.
A small number of patients (1:10,000) with atypical cholinesterase experience long-lasting apnea of 1–4 hours following succinylcholine (or the nondepolarizing neuromuscular blocking drug mivacurium that is also eliminated by the action of butyrylcholinesterase). Mechanical ventilation is used to manage the apnea even though prescreening could detect this rare condition.
REFERENCES
Bowman WC. Neuromuscular block. Br J Pharmacol. 2006;147(Suppl 1):S277–86.
Hopkin PM. Malignant hyperthermia: pharmacology of triggering. Br J Anaesth. 2011;107:48–56.
Larach MG, Gronert GA, Allen GC, et al. Clinical presentation, treatment and complications of malignant hyperthermia from 1987 to 2006. Anesth Analg. 2010;110:498.
Levitan R. Safety of succinylcholine in myasthenia gravis. Ann Emerg Med. 2005;45:225.
Sparr HJ, Beaufort TM, Fuchs-Buder T. Newer neuromuscular blocking agents. How do they compare with established drugs? Drugs. 2001;61(7):919–42.
 What is the mechanism of action of succinylcholine?
What is the mechanism of action of succinylcholine? What reaction is occurring in the patient?
What reaction is occurring in the patient? What drug should immediately be given to the patient, and what is its mechanism of action?
What drug should immediately be given to the patient, and what is its mechanism of action? Mechanism of action of succinylcholine: Nicotinic receptor agonist at the motor endplate of the neuromuscular junction, which causes persistent stimulation and depolarization of muscle cells.
Mechanism of action of succinylcholine: Nicotinic receptor agonist at the motor endplate of the neuromuscular junction, which causes persistent stimulation and depolarization of muscle cells.