CASE 6
A 70-year-old man is seen in follow-up at your office after he has been hospitalized for a myocardial infarction (MI). He underwent successful angioplasty and is currently asymptomatic. In the hospital, his blood pressure was consistently elevated. The patient’s discharge medications include an ACE inhibitor, a statin, aspirin, and metoprolol.
 Metoprolol is selective for which adrenoceptor?
Metoprolol is selective for which adrenoceptor?
 What effects do agents such as metoprolol have on the cardiovascular system?
What effects do agents such as metoprolol have on the cardiovascular system?
 In which organ is metoprolol primarily metabolized?
In which organ is metoprolol primarily metabolized?
ANSWERS TO CASE 6:
Adrenoceptor Antagonists
Summary: A 70-year-old hypertensive man had a recent MI and is prescribed metoprolol.
 Adrenoceptor selectively antagonized by metoprolol: β1.
Adrenoceptor selectively antagonized by metoprolol: β1.
 Effect of β-adrenoceptor antagonists on the cardiovascular system: Reduction of sympathetic-stimulated increases in heart rate, contractility, and cardiac output; lower blood pressure as a result of effects on the heart, renin-angiotensin system, and CNS; increased atrioventricular (AV) conduction time and refractoriness.
Effect of β-adrenoceptor antagonists on the cardiovascular system: Reduction of sympathetic-stimulated increases in heart rate, contractility, and cardiac output; lower blood pressure as a result of effects on the heart, renin-angiotensin system, and CNS; increased atrioventricular (AV) conduction time and refractoriness.
 Organ in which metoprolol is metabolized: Liver.
Organ in which metoprolol is metabolized: Liver.
CLINICAL CORRELATION
β-Adrenergic receptor antagonists are widely used in medicine, primarily for their beneficial effects on the cardiovascular system and for lowering intraocular pressure in patients with glaucoma. Both the nonselective β-adrenoreceptor antagonists and the β1-adrenoceptor selective antagonists are used to treat hypertension. The mechanism of their action is multifactorial, probably including reduction in cardiac output, reduction in renin release, and effects in the CNS. They are also beneficial for treating coronary artery disease. β-Blockers are part of the standard treatment after myocardial infarction as they reduce sympathetic-stimulated increases in heart rate and contractility. This helps to reduce myocardial oxygen demand, providing prophylaxis for angina. β-Adrenoceptor antagonists have a proven benefit in prolonging survival after heart attacks. They lengthen AV conduction time and refractoriness and suppress automaticity. This helps to prevent both supraventricular and ventricular arrhythmias.
APPROACH TO:
Pharmacology of Adrenoceptor Antagonists
OBJECTIVES
1. Describe the therapeutic uses and adverse effects of α-adrenoceptor antagonists.
2. Describe the therapeutic uses and adverse effects of β-adrenoceptor antagonists.
3. Contrast the differences between the nonselective and relatively β1-selective adrenoceptor antagonists.
DEFINITIONS
Pheochromocytoma: A tumor of the adrenal medulla that releases excess levels of epinephrine and norepinephrine that can result in hypertension, cardiac anomalies, and severe headache.
Myocardial infarction: Death of cardiac muscle as a result of ischemia.
DISCUSSION
Class
There are two classes of clinically important α-adrenoceptor antagonists: nonselective antagonists and selective α1-antagonists. Phentolamine, a nonselective, competitive α-adrenoceptor antagonist, and phenoxybenzamine, a nonselective, noncompetitive α-adrenoceptor antagonist, are used for the preoperative management of the marked catecholamine-induced vasoconstriction associated with pheochromocytoma. Prazosin and other α β1-adrenoceptor selective antagonists (doxazosin, terazosin) are used to manage chronic mild-to-moderate hypertension and benign prostatic hypertrophy.
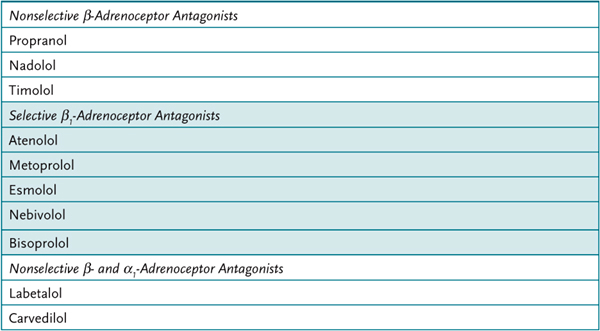
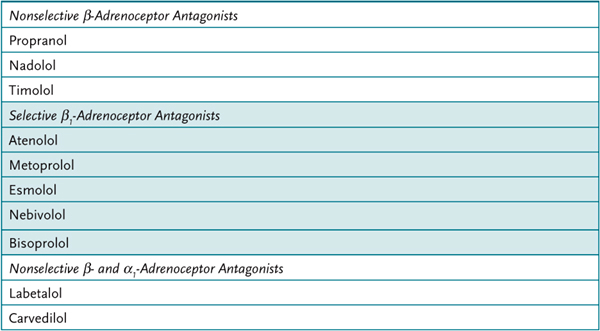
In addition to the nonselective β-adrenoceptor antagonists, there are two classes of clinically important selective β-adrenoceptor antagonists, β1 and β2 (Table 6–1). The major clinical uses for β-adrenoceptor antagonists include ischemic heart disease, cardiac arrhythmias, hypertension, hyperthyroidism, and glaucoma. Ischemic heart disease is managed with nonselective β-adrenoceptor antagonists, propranolol, timolol, and nadolol, as well as β1-adrenoceptor selective antagonists, metoprolol, atenolol, bisoprolol, nebivolol, and esmolol. Cardiac arrhythmias are managed, depending on the arrhythmia, with propranolol and esmolol.
Table 6–1 • β-ADRENOCEPTOR ANTAGONIST SELECTIVITY
Although hypertension can be managed with a wide variety of nonselective and β1-adrenoceptor selective antagonists, except esmolol, they are no longer considered the first-line drug for this indication. ACE inhibitors, Ca2+ channels blockers and thiazide diurectics are now considered the best drugs for treatment of hypertension. Timolol and other β-adrenoceptor antagonists are used to manage glaucoma by decreasing aqueous humor production and thereby reducing intraocular pressure.
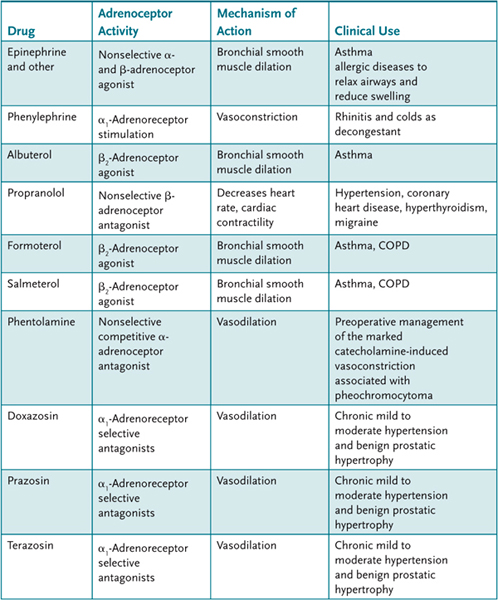
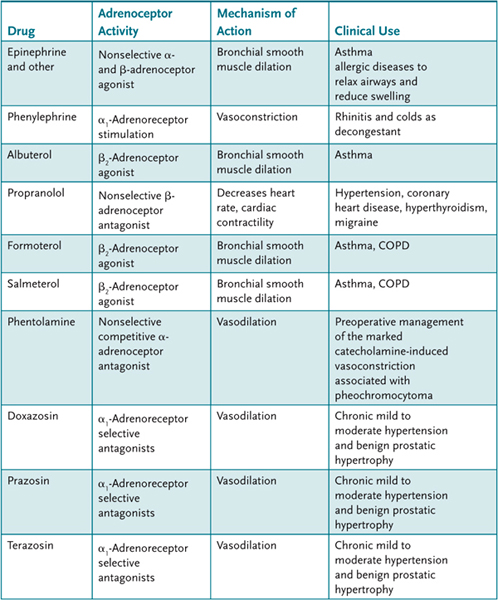
Labetalol (and several other agents, including carvedilol), in formulations used clinically, blocks both β- and α1-adrenoceptors in a 3:1 ratio. It also has some β2-adrenoceptor agonist activity. Labetalol lowers blood pressure by decreasing systemic vascular resistance without any major effect on heart rate or cardiac output. It is used to treat hypertensive emergencies and hypertension from pheochromocytoma. Table 6–2 has a listing of selected drugs that affect autonomic function.
Table 6–2 • SELECTED DRUGS AND THEIR EFFECTS ON THE AUTONOMIC NERVOUS SYSTEM
The major adverse effects of nonselective α-adrenoceptor antagonists are cardiac stimulation, primarily tachycardia because of baroreflex-mediated sympathetic discharge, and postural hypotension. Additional cardiac stimulation by phentolamine may be caused by antagonist activity at presynaptic α2-adrenoceptors that result in increased norepinephrine release. (Prazosin and other selective α1-adrenoceptor selective antagonists are less likely to cause reflex tachycardia.) A β-adrenoceptor antagonist may be required to counter the cardiac effects. α-Antagonists are rarely used as first-line agents for hypertension, as they are associated with a higher rate of congestive heart failure than other agents.
The major adverse effects of nonselective β-adrenoceptor antagonists are related to their effects on smooth muscle, carbohydrate metabolism. The use of a selective β-adrenoreceptor antagonists is recommended in patients with asthma or COPD. In patients, with insulin-dependent diabetes, nonselective β-adrenoceptor antagonists increase the incidence and severity of hypoglycemic episodes. The use of selective β1-adrenoceptor antagonists in patients with this condition offers some potential benefits. β-Adrenoceptor antagonists can also cause erectile dysfunction. The β-adrenoreceptor antagonists can reduce HDL cholesterol and significantly raise serum triglercerides. The latter effect is particularly prevalent with the non-selective β-adrenoreceptor antagonists. Combined α- and β-adrenoreceptor antagonist (labetolol) or β-adrenoreceptor antagonists with sympathomimetic activity (acebutolol or pindolol) have no effect on serum tricglycerides.
Mechanism of Action
α-Adrenoceptor antagonists and β-adrenoceptor antagonists interact directly, and either competitively or irreversibly with, respectively, α-adrenoceptors and β-adrenoceptors to block actions of the endogenous catecholamines (norepinephrine and epinephrine), and exogenously administered sympathomimetic agents.
The α1-adrenoreceptor is a Gi-coupled receptor whose activation leads to production of inositol triphosphate (IP3) and diacylglycerol (DAG) to promote increased intracellular Ca2+ and ultimately smooth muscle contraction. Antagonists of this receptor will therefore promote smooth muscle relaxation; in blood vessels, where these receptors are largely expressed, this leads to dilation.
β-Adrenergic receptors are Gs-coupled receptors that activate adenylyl cyclase leading to elevation of cAMP and activation of protein kinase A. β1-Adrenorecptors are located primarily in the heart and kidney. In the heart, activation of β1-receptors causes an increase in the force of contraction of cardiac muscle and an increase in heart rate. β2-Adrenoreceptors are located in the bronchial, where their activation promotes relaxation. β1-Antagonists, therefore, are effective in decreasing heart rate, contractility, and conduction velocity.
Administration
α- and β-adrenoceptor antagonists are administered orally or parenterally. β-Adrenoceptor antagonists are also available for ophthalmic application.
Pharmacokinetics
Metoprolol and propranolol undergo extensive and variable interindividual first-pass hepatic metabolism resulting in relatively low bioavailability. Oral sustained-release preparations of these agents are available. Drugs that inhibit cytochrome P450 2D6 may decrease the metabolism of carvedilol. Esmolol is ultra-short-acting as a result of its ester linkage that is rapidly metabolized by plasma esterases.
COMPREHENSION QUESTIONS
6.1 Which of the following actions of epinephrine are blocked by prazosin?
A. Bronchial dilation
B. Increased cardiac stroke volume
C. Increased heart rate
D. Mydriasis
6.2 A 34-year-old man is prescribed labetalol for hypertension. The effect on the cardiovascular system is a result of its action as an antagonist at which of the following?
A. α-Adrenoceptors
B. β-Adrenoceptors
C. Both α- and β-adrenoceptors
D. Muscarinic cholinoreceptors
6.3 Which of the following is the least likely clinical use for β-adrenoceptor antagonists?
A. Benign prostatic hypertrophy
B. Cardiac arrhythmias
C. Hypertension
D. Ischemic heart disease
6.4 Which of the following patients would not benefit from beta blockers?
A. 64-year-old female with daily migraines
B. 35-year-old female with hyperthyroidism and symptomatic tachycardia and tremors
C. 56-year-old male with erectile dysfunction
D. 74-year-old male with history of systolic heart failure that is stable
E. 57–year-old male with past history of coronary artery disease
ANSWERS
6.1 D. Prazosin is an α-adrenoceptor antagonist that will block epinephrine-mediated contraction of the radial smooth muscle of the eye that results in mydriasis. All the other actions listed are mediated by β-adrenoceptors, which would be blocked by β-adrenoceptor antagonists like propranolol.
6.2 C. Labetalol blocks both β- and α-adrenoceptors. It lowers blood pressure by decreasing systemic vascular resistance (α-adrenoceptor antagonist activity), without any major effect on heart rate or cardiac output (β-adrenoceptor antagonist activity).
6.3 A. β-Adrenoceptor antagonists are used therapeutically to manage ischemic heart disease, cardiac arrhythmias, and hypertension. α1-Adrenoceptor selective antagonists are used to manage benign prostatic hypertrophy.
6.4 C. Beta blockers, especially at higher doses, will cause erectile dysfunction and hence it would not be ideal in this patient. Beta blockers have proven to reduce morbidity and mortality in patients with systolic, diastolic, and mixed dysfunction heart failure as well as in those with coronary artery disease. Propanalol is a first-line agent in migraine prophylaxis. It also is very effective in controlling the symptoms of tachycardia and tremors in Grave disease.
PHARMACOLOGY PEARLS
 α1-Adrenoceptor selective antagonists, such as doxazosin and terazosin, are used for mild chronic hypertension and benign prostatic hypertrophy.
α1-Adrenoceptor selective antagonists, such as doxazosin and terazosin, are used for mild chronic hypertension and benign prostatic hypertrophy.
 The major clinical uses for β-adrenoceptor antagonists include ischemic heart disease, cardiac arrhythmias, hypertension, hyperthyroidism, and glaucoma.
The major clinical uses for β-adrenoceptor antagonists include ischemic heart disease, cardiac arrhythmias, hypertension, hyperthyroidism, and glaucoma.
 The major adverse effects of nonselective β-adrenoceptor antagonists are related to their effects on bronchial smooth muscle (increased airway resistance in asthmatics) and on carbohydrate metabolism (hypoglycemia in insulin-dependent diabetics).
The major adverse effects of nonselective β-adrenoceptor antagonists are related to their effects on bronchial smooth muscle (increased airway resistance in asthmatics) and on carbohydrate metabolism (hypoglycemia in insulin-dependent diabetics).
 β-Adrenoceptor antagonists are no longer the first-line drug for the treatment of hypertension. ACE inhibitors, thiazide diurectics, and Ca2+ channels blockers are recommended.
β-Adrenoceptor antagonists are no longer the first-line drug for the treatment of hypertension. ACE inhibitors, thiazide diurectics, and Ca2+ channels blockers are recommended.
REFERENCES
Firnhaber, JM. Clinical inquiries: what are the best prophylactic drugs for migraine? J Fam Pract. 2009 Nov;58(11):608–10.
Shin J, Johnson JA. Pharmacogenetics of beta-blockers. Pharmacotherapy. 2007;27(6):874–87.
Piascik MT, Perez DM. Alpha 1-adrenergic receptors: new insights and directions. J Pharmacol Exp Ther. 2001;293(2):403–10.
 Metoprolol is selective for which adrenoceptor?
Metoprolol is selective for which adrenoceptor? What effects do agents such as metoprolol have on the cardiovascular system?
What effects do agents such as metoprolol have on the cardiovascular system? In which organ is metoprolol primarily metabolized?
In which organ is metoprolol primarily metabolized? Adrenoceptor selectively antagonized by metoprolol: β1.
Adrenoceptor selectively antagonized by metoprolol: β1.