CASE 7
A 64-year-old female with a past medical history of coronary artery disease, hypertension, and congestive heart failure (CHF) presents with dyspnea at rest and with exertion, orthopnea, and lower extremity pitting edema. Her symptoms have worsened over the last 2 weeks and also include orthopnea, worsening exercise tolerance, and tachypnea. On examination, she is notably dyspneic and tachypneic, and also has jugular venous distension, 2+ pitting edema, and rales on lung examination. Patient is also found to have an audible S3. Her chest x-ray, pro-Brain Natriuretic Peptide (BNP) level, and echocardiogram confirm the clinical suspicion of CHF exacerbation with pulmonary edema. She is already on maximal medical therapy with an ACE inhibitor, beta blocker, statin, and aspirin. She is appropriately placed on oxygen and given intravenous furosemide.
 What is the mechanism of action of furosemide?
What is the mechanism of action of furosemide?
 What electrolyte abnormalities can be caused by furosemide?
What electrolyte abnormalities can be caused by furosemide?
ANSWERS TO CASE 7:
Diuretics
Summary: A 64-year-old woman with pulmonary edema is prescribed furosemide.
 Mechanism of action of furosemide: Inhibit active NaCl reabsorption in the ascending limb of the loop of Henle, increasing water and electrolyte excretion.
Mechanism of action of furosemide: Inhibit active NaCl reabsorption in the ascending limb of the loop of Henle, increasing water and electrolyte excretion.
 Potential electrolyte abnormalities: Hypokalemia, hypomagnesemia, and metabolic alkalosis because of enhanced H+ excretion.
Potential electrolyte abnormalities: Hypokalemia, hypomagnesemia, and metabolic alkalosis because of enhanced H+ excretion.
CLINICAL CORRELATION
Loop diuretics given intravenously promote diuresis within minutes, making them ideal for the treatment of acute pulmonary edema. Furosemide is the prototype and most widely used drug in this class. Loop diuretics inhibit NaCl reabsorption in the ascending limb of the loop of Henle. This causes a marked increase in the excretion of both water and electrolytes. The excretion of potassium, magnesium, and calcium ions are all increased, which may cause clinically significant adverse effects. A metabolic alkalosis may also occur as a result of the excretion of hydrogen ions. However, the ability to cause excretion of these electrolytes may also provide a clinical benefit in certain situations. Forced diuresis by giving IV saline and furosemide is a primary method of treatment of hypercalcemia.
APPROACH TO:
Pharmacology of the Loop Diuretics
OBJECTIVES
1. Know the site and mechanism of action of diuretic agents.
2. Know the electrolyte effects of the various diuretic agents.
3. Know the therapeutic uses, adverse effects, and contraindications to diuretic use.
DEFINITIONS
Diuretic: An agent that increases the production of urine. The most common are natriuretic diuretics, agents that increase urine production by interfering with sodium reabsorption in the kidney.
Edema: Accumulation of water in interstitial spaces. Causes include elevated blood pressure, a decrease in plasma oncotic pressure caused by a reduction in hepatic protein synthesis, or an increase in the oncotic pressure within the interstitial space.
DISCUSSION
Class
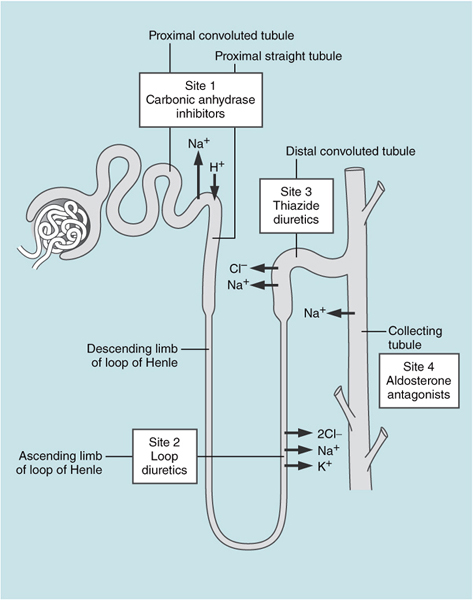
Natriuretic diuretics all act within the kidney to reduce the reabsorption of Na+ and Cl-. There are four sites within the kidney where various diuretics act; these correspond to four anatomic regions of the nephron. The proximal tubule (site 1) is the site of approximately 60 percent Na+ reabsorption, but diuretics acting here are relatively ineffective because of the sodium-reabsorbing capacity in more distal regions of the nephron. The ascending loop of Henle (site 2) has active reabsorption of approximately 35 percent of the filtered Na+. This is mediated by a cotransporter termed NKCC2 that transports 1 Na+, 1 K+, and 2 Cl-. This is the molecular target of furosemide and other loop or “high-ceiling” diuretics. The distal convoluted tubule (site 3) is responsible for transport of approximately 15 percent of filtered sodium. Thiazide diuretics act in this segment of the nephron by interfering with a different cotransporter, NCC, which cotransports Na+ and Cl-. Site 4 diuretics act in the collecting tubule by interfering with Na+ reabsorption through a specific channel, the epithelial sodium channel (ENaC), also called the amiloride-sensitive sodium channel (Figure 7–1).
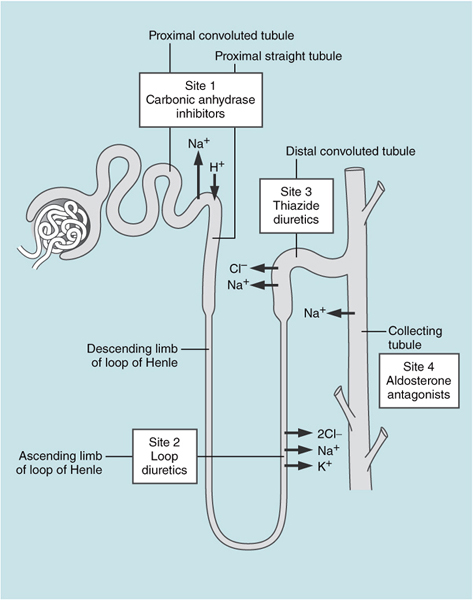
Figure 7–1. Sites of action of the nephron and diuretic agents.
Loop diuretics—furosemide, ethacrynic acid, bumetanide, and torsemide—are highly acidic drugs that act on the luminal side of the tubule. They reach this site by being secreted into the tubule by anion secretion in the proximal tubule. Compared with other diuretics, loop diuretics cause the greatest diuresis because the Na+ K- 2Cl- transporter is responsible for a large fraction of Na+ reabsorption, and regions distal to the ascending limb have more limited capacity for sodium transport. Loop diuretics are useful for the treatment of peripheral and pulmonary edema, which may occur secondarily as a consequence of cardiac failure, liver failure, or renal failure. Loop diuretics increase the excretion of Na+, Cl-, K+, Mg2+, Ca2+ and decrease the excretion of Li+. The increased excretion of Ca2+ is clinically relevant, and loop diuretics can be used to treat hypercalcemia. Some of the diuretic actions of furosemide are mediated via prostaglandins, which have diuretic activity. Inhibitors of prostaglandin biosynthesis diminish the increase in diuresis produced by loop diuretics. In addition, furosemide has actions on the vascular system that occur prior to diuresis and this action may be mediated by prostaglandins. Other effects include changes in renal blood flow and a reduction in left-ventricular filling pressure. Loop diuretics increase urine production and decrease plasma K+ in patients with acute renal failure.
The major adverse effects of loop diuretics are electrolyte imbalances. Increased delivery of Na+ to the collecting duct increases K+ and H+ excretion. Loop diuretics therefore cause hypokalemia, hypochloridemia, and metabolic alkalosis. Hyperuricemia may be caused by the volume contraction and enhanced uric acid reabsorption by the proximal tubule. Loop diuretics can produce dose-dependent ototoxicity and this adverse effect is exacerbated in the presence of other ototoxic drugs such as the aminoglycosides.
Structure
Most loop diuretics are sulfonamide derivatives; the exceptions are ethacrynic acid, which is a phenoxyacetic acid derivative, and torsemide, which is a sulfonylurea. Due to the lack of a sulfur atom, ethacrynic acid causes fewer hypersensitivity reactions.
Mechanism of Action
The molecular target of furosemide and other loop or high-ceiling diuretics is the sodium-potassium-2 chloride cotransporter (NKCC2), which transports 1 Na+, 1 K+, and 2 Cl-. The activity of this transporter is blocked by loop diuretics.
Administration
All loop diuretics can be administered orally, and their onset of action is approximately 1 hour (torsemide) to 2 hours (furosemide). Loop diuretics can also be administered IV, and for furosemide, this produces vasodilation in as little as 5 minutes and diuresis in 20 minutes.
Pharmacokinetics
All loop diuretics are extensively bound to plasma proteins. Half-lives vary from 45 minutes (bumetanide) to 3.5 hours (torsemide). Approximately 65 percent of a dose of furosemide is eliminated by the kidney, and the remainder is metabolized. Only 20 percent of torsemide is eliminated by the kidney, and 80 percent is metabolized.
COMPREHENSION QUESTIONS
7.1 Furosemide acts to inhibit Na+ reabsorption in which of the following locations?
A. Ascending limb of the loop of Henle
B. Collecting duct
C. Descending limb of the loop of Henle
D. Distal convoluted tubule
7.2 A patient arrives in the emergency room in a coma and has a serum Ca2+ of 4.5 mM. You start a saline infusion of which of the following drugs?
A. Calcitonin
B. Ethacrynic acid
C. Hydrochlorothiazide
D. Spironolactone
7.3 A 55-year-old man with congestive heart failure is noted to be taking furosemide each day. Which of the following is most likely to be found in the serum?
A. Decreased potassium level
B. Decreased uric acid level
C. Elevated magnesium level
D. Low bicarbonate level
7.4 A 65-year-old male with CHF exacerbation is given IV furosemide. Which of the following adverse events are not associated with this medication?
A. Transient neurotoxicity from high dose
B. Hypotension
C. Worsening renal function
D. Hyperkalemia
ANSWERS
7.1 A. Furosemide acts specifically on a Na+ K+ 2Cl- transporter in the ascending limb of the loop of Henle.
7.2 B. Loop diuretics such as ethacrynic acid increase the excretion of Ca2+.
7.3 A. Furosemide leads to hypokalemia, hypomagnesemia, and metabolic alkylosis (elevated bicarbonate level).
7.4 D. Furosemide infusion may cause transient ototoxity with higher doses. Hypotension, hypokalemia, and azotemia with possible worsening renal failure are all possible adverse events with furosemide.
PHARMACOLOGY PEARLS
 Furosemide, which acts on the loop of Henle, is the most efficacious diuretic.
Furosemide, which acts on the loop of Henle, is the most efficacious diuretic.
 Hypokalemia is a frequent adverse effect encountered with loop diuretics, and this can be managed with the concomitant use of potassium-sparing diuretics such as triamterene or spironolactone.
Hypokalemia is a frequent adverse effect encountered with loop diuretics, and this can be managed with the concomitant use of potassium-sparing diuretics such as triamterene or spironolactone.
 Loop diuretics can produce dose-dependent ototoxicity; this is reduced with the non-sulfur containing ethacrynic acid.
Loop diuretics can produce dose-dependent ototoxicity; this is reduced with the non-sulfur containing ethacrynic acid.
REFERENCES
Wargo KA, Banta WM. A comprehensive review of the loop diuretics: should furosemide be first line? Ann Pharmacother. 2009;43:1836–47.
Masuyama T, Tsujino T, Origasa H, Yamamoto K, Akasaka T, Hirano Y, Ohte N, Daimon T, Nakatani S, Ito H. Superiority of long-acting to short-acting loop diuretics in the treatment of congestive heart failure. Circ J. 2012;76:833–42.
Wile D. Diuretics: a review. Ann Clin Biochem. 2012;49(Pt 5):419–31.
 What is the mechanism of action of furosemide?
What is the mechanism of action of furosemide? What electrolyte abnormalities can be caused by furosemide?
What electrolyte abnormalities can be caused by furosemide? Mechanism of action of furosemide: Inhibit active NaCl reabsorption in the ascending limb of the loop of Henle, increasing water and electrolyte excretion.
Mechanism of action of furosemide: Inhibit active NaCl reabsorption in the ascending limb of the loop of Henle, increasing water and electrolyte excretion.