CASE 9
A 72-year-old man presents to the office for routine follow-up. He is under treatment for hypertension and congestive heart failure with enalapril and a diuretic. His blood pressure is under acceptable control, and he has no symptoms of heart failure at present. He does complain that he has been coughing frequently in the past few months. History and examination reveal no other cause of a chronic cough, so you decide to discontinue his enalapril and start him on losartan.
 What is the mechanism of action of enalapril?
What is the mechanism of action of enalapril?
 By what mechanism does enalapril convert to its active form enalaprilat?
By what mechanism does enalapril convert to its active form enalaprilat?
 What is the likely cause of the cough?
What is the likely cause of the cough?
 What is the mechanism of action of losartan?
What is the mechanism of action of losartan?
ANSWERS TO CASE 9:
Drugs Active on the Renin-Angiotensin System
Summary: A 72-year-old man with hypertension and congestive heart failure presents with an ACE inhibitor-induced cough, and is switched to losartan.
 Mechanism of action of enalapril: Inhibits the conversion of angiotensin I to angiotensin II; this also inhibits the angiotensin II-stimulated release of aldosterone. Angiotensin-converting enzyme (ACE) inhibitors also reduce the inactivation of bradykinin.
Mechanism of action of enalapril: Inhibits the conversion of angiotensin I to angiotensin II; this also inhibits the angiotensin II-stimulated release of aldosterone. Angiotensin-converting enzyme (ACE) inhibitors also reduce the inactivation of bradykinin.
 Mechanism of converting enalapril to enalaprilat: Deesterification in the liver.
Mechanism of converting enalapril to enalaprilat: Deesterification in the liver.
 Mechanism of ACE inhibitor-induced cough: Secondary to the increased bradykinin levels, which is caused by reduction in the inactivation of bradykinin.
Mechanism of ACE inhibitor-induced cough: Secondary to the increased bradykinin levels, which is caused by reduction in the inactivation of bradykinin.
 Mechanism of action of angiotensin receptor blockers (ARBs): Antagonists of angiotensin-1 (AT-1) receptors, which mediate the pressor effects of angiotensin II.
Mechanism of action of angiotensin receptor blockers (ARBs): Antagonists of angiotensin-1 (AT-1) receptors, which mediate the pressor effects of angiotensin II.
CLINICAL CORRELATION
ACE inhibitors have gained wide-scale use in medicine for their effectiveness in hypertension, congestive heart failure, coronary artery disease, and renal protection in diabetics. They inhibit the conversion of angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor and also stimulates the release of aldosterone, which promotes sodium and water retention. Angiotensin II also increases catecholamine release by the adrenal medulla and at sympathetic nerves. Inhibition of the production of angiotensin II reduces vascular resistance and sodium and water retention. Another effect of ACE inhibitors is to reduce the inactivation of bradykinin. Active bradykinin is a vasodilator, and inhibiting its degradation provides an additive mechanism to lower blood pressure. However, raising bradykinin levels contributes to one of the ACE inhibitors’ most bothersome side effects, chronic dry cough. Elevated bradykinin can also cause angioedema. In general the drugs are well tolerated, but along with cough, can cause hyperkalemia and should be used with caution with potassium-sparing diuretics or in persons with impaired renal function. ARBs are antagonists of the angiotensin I receptor, which mediates the direct vasoconstrictor effect of angiotensin II. This also blocks the release of aldosterone. ARBs have a much reduced effect on the bradykinin system and have a much lower incidence of cough and angioedema. ARBs rarely cause chronic cough. They are also well tolerated but, like ACE inhibitors, can cause hyperkalemia. Aliskiren (Tekturna) is a small-molecule direct renin inhibitor. It appears to be as efficacious as ACE inhibitors or ARBs, but clinical experience is more limited.
APPROACH TO:
Pharmacology Of The Renin-Angiotensin System
OBJECTIVES
1. Know the mechanism of action of ACE inhibitors.
2. Know the therapeutic uses, side effects, and contraindications to ACE inhibitor use.
3. Know the mechanism of action of ARBs.
4. Know the therapeutic uses, side effects, and contraindications to ARB use.
DEFINITIONS
Hypertension: From the Seventh Report, Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure, normal blood pressure is 120/80 mm Hg. Progressive disease may be staged as prehypertensive (120–139/80–89), Stage 1 (140–159/90–99), and Stage2 (>160/>100).
Bradykinin: A member of a class of peptides, the kinins, that have a variety of effects on the cardiovascular system, including vasodilatation and inflammation.
ARB: Angiotensin receptor blocker, more precisely angiotensin AT-1 receptor blockers.
DISCUSSION
Class
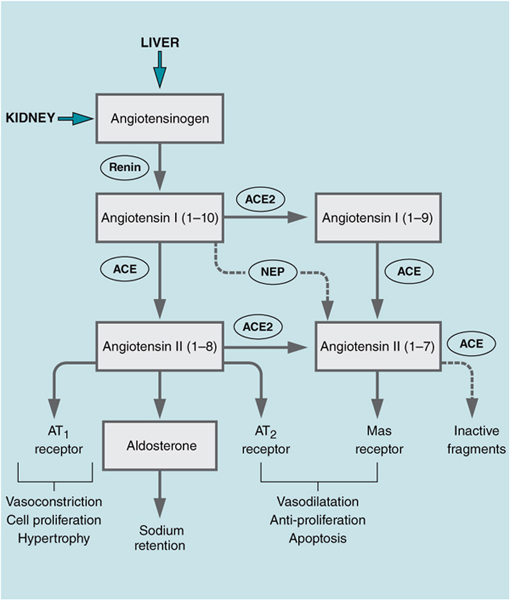
The renin-angiotensin-aldosterone system provides a humoral system for controlling blood pressure and electrolyte levels. The “sensors” in this system monitor Na+, K+, vascular volume, and blood pressure. A reduction in blood pressure, detected by intrarenal stretch receptors, or a fall in the delivery of Na+ to the distal portions of the nephron results in release of renin from the juxtaglomerular apparatus (JGA). Renin secretion can also be increased through the baroreceptor reflex mediated by increased central nervous system (CNS) outflow and β1-adrenergic receptors on the JGA. Renin is an aspartyl protease that cleaves angiotensinogen, a 56-kD polypeptide produced in the liver, to the decapeptide angiotensin I (Figure 9–1, “classic” pathway).
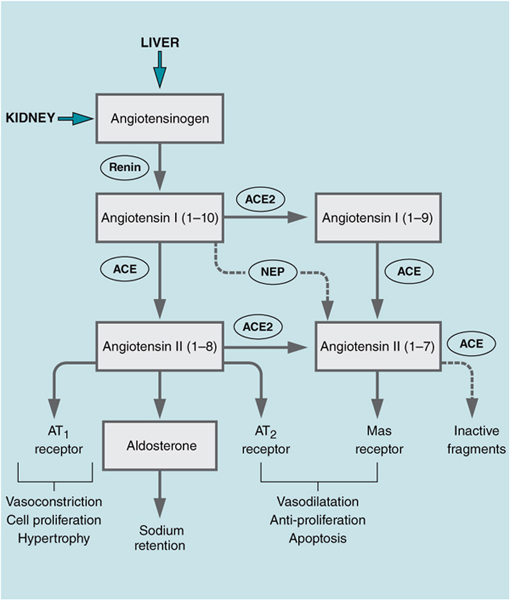
Figure 9–1. Schematic of angiotensin pathway.
Angiotensin I is biologically inactive and is rapidly converted to the octapeptide angiotensin II by the action of ACE, a dipeptidyl peptidase. ACE is also responsible for degradation of bradykinin. ACE2 is a unique gene product that is 41 percent identical to ACE. It cleaves angiotensin II (Ang 1–8) into angiotensin 1–7.
Metabolism of Angiotensinogen
The “classic” pathway consists of angiotensinogen, which is cleaved by renin to AgI, which in turn is cleaved by ACE to AgII. AgII binds to AT-1 and AT-2 receptors. AgI or AgII can be cleaved by the carboxypeptidase ACE2 to AgI-7. AgI-7 binds to the Mas receptor whose actions oppose those of AT-1 receptors. AgI-7 can also be formed by neprilysin (NEP), an endopeptidase that cleaves a number of physiologically important substrates. AgI-7 has physiologic actions that oppose those of AgII, including vasodilatation and antiproliferative effects.
Angiotensin II has multiple actions that act in concert to increase blood pressure and alter electrolyte levels. Angiotensin II is a potent vasoconstrictor, 10–40 times more potent than epinephrine, an effect mediated by receptor-coupled Ca2+ channels in vascular smooth muscle cells, as described below. Angiotensin II enhances the release of catecholamines both from the adrenal medulla and at peripheral nerve endings. Within the adrenal cortex, angiotensin II increases the biosynthesis of aldosterone, which leads to an increase in Na+ and water reabsorption in the kidneys and volume expansion. Angiotensin II has several actions within the CNS, including altering vagal tone to increase blood pressure, increasing thirst, and increasing the release of antidiuretic hormone.
Angiotensin II also has effects on the heart and the vasculature that do not directly affect blood pressure. Angiotensin II induces cardiac hypertrophy, is proproliferative, and enhances matrix remodeling and the deposition of matrix proteins, which leads to increased myocardial stiffness. Within vessel walls, angiotensin II is proinflammatory and can stimulate the release of several chemokines.
Three angiotensin receptors mediate these actions. The AT-1 and angiotensin-2 (AT-2) receptors have been described in various tissues. Both are seven-transmembrane receptors that appear to couple to various signaling pathways. AT-1 receptors bind angiotensin II, angiotensin III, and angiotensin IV. This receptor mediates most of the cardiovascular and central responses to angiotensin II, including vasoconstriction of vascular smooth muscle and aldosterone biosynthesis in the adrenal medulla. AT-1 receptors also mediate the cardiac hypertrophic and proproliferative responses to angiotensin II. AT-2 receptors also bind angiotensin II and play a role in the development of the cardiovascular system. In general, activation of AT-2 receptors is physiologically antagonistic to the action of AT-1 receptors. Activation of AT-2 receptors is hypotensive and antiproliferative and is coupled to distinctly different signaling pathways compared to AT-1 receptors. Angiotensin-4 (AT-4) receptors appear to be identical to transmembrane aminopeptidase insulin-regulated aminopeptidase (IRAP) and have a single transmembrane domain. AT-4 receptors are expressed in the numerous tissues and bind angiotensin IV. Activation of these receptors has been reported to regulate cerebral blood flow, and to stimulate endothelial cell expression of plasminogen activator inhibitor, and has effects on both memory and learning.
AgI-7 is produced by the action of ACE2. AgI-7 binds to the Mas receptor, another G-protein-coupled receptor. AgI-7 has numerous beneficial cardiovascular actions, including antihypertensive, antifibrotic, antioxidant, anti-inflammatory, and antiatherosclerotic effects.
Inhibition of the renin-angiotension system (RAS) is accomplished pharmacologically in three ways: inhibition of the production of angiotensin II, blockade of AT-1 receptors, or inhibition of renin activity. ACE inhibitors, or peptidyl dipeptidase (PDP) inhibitors, include enalapril, lisinopril, fosinopril, captopril, and nine others. These drugs differ in their chemistry and pharmacokinetic properties, but all are orally active, have the same range of activities, and are equally effective clinically. ACE is the enzyme responsible for both activation of angiotensin I (metabolism to angiotensin II) and inactivation of bradykinin. The decreased metabolism of bradykinin is partly responsible for the hypotensive action of ACE inhibitors, and is also responsible for enhancing the irritability of airways that leads to the dry cough associated with ACE inhibitors and seen in 10–33 percent of patients taking the drugs. Elevated bradykinin is also associated with angioedema (0.1–0.5% incidence).
ARBs block the action of angiotensin II by acting as antagonists at AT-1 receptors. These nonpeptide antagonists include losartan, valsartan, candesartan, and five others. ARBs bind with high affinity to AT-1 receptors without interfering with AT-2 or AT-4 receptors.
The ACE inhibitors and ARBs are equally effective in reducing blood pressure. More clinical experience exists with the ACE inhibitors, and it has been well established that this class of drugs reduces the risk of second events in patients who have had an MI and renal damage in patients with diabetic nephropathy. Hypotension and hyperkalemia are adverse effects seen with both classes of RAS inhibitors. Cough and angioedema, caused by increased bradykinin levels, are more frequently seen with the ACE inhibitors. ARBs have been shown to have anti-inflammatory activity and can decrease the production of several cytokines. This activity appears to be independent of AT-1 receptor blockade.
Aliskiren is a small molecule inhibitor of renin and is approved for use as an antihypertensive. Several clinical trials have shown aliskiren as effective in 24-hour blood pressure control as ARBs with a similar safety and tolerability profile. Aliskiren was shown to be more effective than hydrochlorothiazide in hypertensive obese patients.
Structure
Although the various ACE inhibitors have different chemical structures, they are mostly based on extensive modifications of L-proline. The ARBs are also quite distinct chemically: Valsartan is an L-valine derivative, and losartan is an imidazole derivative. Aliskiren was designed based on the crystal structure of renin and is a nonpeptide, small molecule, transition-state mimetic that binds to the active site of the enzyme and is effective in the nM range.
Mechanism of Action
ACE inhibitors are all competitive inhibitors of angiotensin-converting enzyme. ARBs are competitive antagonists of the angiotensin II type 1 receptor (AT-1), while aliskiren is a direct renin inhibitor.
Administration
All ACE inhibitors are available for oral administration. Enalaprilat, the active metabolite of enalapril, is available for intravenous infusion. Aliskiren is an oral agent. Coadministration of ARBs and ACE inhibitors, while demonstrating additive reductions in blood pressure, may be associated with increased frequency of renal dysfunction. Combinations of aliskiren with an ARB, a thiazide, a calcium channel blocker, or atenolol have all shown a greater reduction in blood pressure compared to monotherapy.
Pharmacokinetics
Many of the current ACE inhibitors are prodrugs and require conversion to the active metabolite in the liver. For example, enalapril is converted to enalaprilat, and fosinopril is converted into fosinoprilat. Captopril and lisinopril are active drugs that do not require metabolism. The onset of action of ACE inhibitors is 0.5–2 hours, and the duration of action is typically 24 hours (captopril is 6 hours). Most are eliminated in the urine. Aliskiren is poorly absorbed (2–3%) and is eliminated unchanged by the hepatobiliary system.
COMPREHENSION QUESTIONS
9.1 Losartan acts to decrease which of the following?
A. AT-1 receptor activity
B. Bradykinin production
C. Production of angiotensin II
D. Renin production
9.2 Which of the following is a limiting adverse effect of ACE inhibitors?
A. Acidosis
B. Hyperkalemia
C. Hypernatremia
D. Hypokalemia
E. Hyponatremia
9.3 Which of the following is an advantage of losartan over enalapril?
A. Better efficacy in lower blood pressure
B. Better prevention of secondary myocardial events
C. Less cost
D. Less incidence of angioedema
9.4 A 74-year-old male with PMH CHF, prior MI, CKD Stage 3, diabetes is being treated with an ACE inhibitor (among other medications). Which of the following conditions does the ACE inhibitor offer proven benefit?
A. CHF
B. CAD
C. CKD
D. DMII
E. All of the above
ANSWERS
9.1 A. Losartan is a prototypical angiotensin AT-1 receptor antagonist.
9.2 B. By reducing aldosterone levels, ACE inhibitors decrease K+ excretion in the distal nephron.
9.3 D. Losartan does not lead to elevated bradykinin levels; thus, there is less of an incidence of angioedema and dry cough. The effects on blood pressure are equal. The track record for prevention of secondary cardiovascular events is well established for ACE inhibitors, although the same is speculated for ARBs.
9.4 E. ACE inhibitors and ARBs have been shown in numerous trials to improve outcomes in cardiovascular disease such as CAD/CHF by optimizing preload, reducing afterload, decreasing remodeling, and controlling blood pressure. They have also been proven in reducing proteinuria and being renoprotective in CKD and diabetic patients.
PHARMACOLOGY PEARLS
 Elevation of the bradykinin levels is thought to be the etiology of the dry cough and angioedema of ACE inhibitors.
Elevation of the bradykinin levels is thought to be the etiology of the dry cough and angioedema of ACE inhibitors.
 ACE inhibitors improve outcome in patients with cardiovascular disease and have been recommended as therapy in several guidelines.
ACE inhibitors improve outcome in patients with cardiovascular disease and have been recommended as therapy in several guidelines.
 Clinical experience suggests that inhibitors of the renin-angiotensin system are somewhat less effective in African Americans.
Clinical experience suggests that inhibitors of the renin-angiotensin system are somewhat less effective in African Americans.
 ARBs block the action of angiotensin II by acting as antagonists at AT-1 receptors.
ARBs block the action of angiotensin II by acting as antagonists at AT-1 receptors.
REFERENCES
Miura S, Karnik SS, Saku K. Review: angiotensin II type 1 receptor blockers: class effects versus molecular effects. J Renin Angiotensin Aldosterone Syst. 2011;12:1–7.
Lazich I, Bakris GL. Newer renin-angiotensin-aldosterone system blocker combinations: is there an advantage? Curr Opin Nephrol Hypertens. 2011;20:471–5.
Jagadeesh G, Balakumar P, Stockbridge N. How well do aliskiren’s purported mechanisms track its effects on cardiovascular and renal disorders? Cell Signal. 2012;24:1583–91.
 What is the mechanism of action of enalapril?
What is the mechanism of action of enalapril? By what mechanism does enalapril convert to its active form enalaprilat?
By what mechanism does enalapril convert to its active form enalaprilat? What is the likely cause of the cough?
What is the likely cause of the cough? What is the mechanism of action of losartan?
What is the mechanism of action of losartan? Mechanism of action of enalapril: Inhibits the conversion of angiotensin I to angiotensin II; this also inhibits the angiotensin II-stimulated release of aldosterone. Angiotensin-converting enzyme (ACE) inhibitors also reduce the inactivation of bradykinin.
Mechanism of action of enalapril: Inhibits the conversion of angiotensin I to angiotensin II; this also inhibits the angiotensin II-stimulated release of aldosterone. Angiotensin-converting enzyme (ACE) inhibitors also reduce the inactivation of bradykinin.