CASE 14
A 19-year-old man is brought to the physician’s office by his very concerned mother. He has been kicked out of the dormitory at college for his “bizarre” behavior. He has accused several fellow students and professors of spying on him for the CIA. He stopped attending his classes and spends all of his time watching TV because the announcers are sending him secret messages on how to save the world. He has stopped bathing and will only change his clothes once a week. In your office you find him to be disheveled, quiet, and unemotional. The only spontaneous statement he makes is when he asks why his mother brought him to the office of “another government spy.” His physical examination and blood tests are normal. A drug screen is negative. You diagnose him with acute psychosis likely secondary to schizophrenia, admit him to the psychiatric unit of the hospital, and start him on haloperidol.
 What is the mechanism of therapeutic action of haloperidol?
What is the mechanism of therapeutic action of haloperidol?
 What mediates the extrapyramidal side effects (EPSs) of the antipsychotic agents?
What mediates the extrapyramidal side effects (EPSs) of the antipsychotic agents?
 Which autonomic nervous system receptors are antagonized by antipsychotic agents?
Which autonomic nervous system receptors are antagonized by antipsychotic agents?
ANSWERS TO CASE 14:
Antipsychotic Drugs
Summary: A 19-year-old man with acute psychosis likely from schizophrenia is prescribed haloperidol.
 Mechanism of therapeutic action of haloperidol: Antagonist activity at postsynaptic dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain.
Mechanism of therapeutic action of haloperidol: Antagonist activity at postsynaptic dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain.
 Mechanism of EPSs: Antagonist activity at dopamine receptors in the basal ganglia and other dopamine receptor sites in the central nervous system (CNS).
Mechanism of EPSs: Antagonist activity at dopamine receptors in the basal ganglia and other dopamine receptor sites in the central nervous system (CNS).
 Autonomic nervous system receptors blocked by antipsychotic agents: α-Adrenoceptors and muscarinic cholinoreceptors.
Autonomic nervous system receptors blocked by antipsychotic agents: α-Adrenoceptors and muscarinic cholinoreceptors.
CLINICAL CORRELATION
Schizophrenia is a chronic thought disorder that often presents in adolescence or early adulthood. It is characterized by the presence of “positive symptoms,” which include delusions, hallucinations, and paranoia, and “negative symptoms,” which include blunt effect, withdrawal, and apathy. The therapeutic effects of the antipsychotic agents result from their antagonist actions on postsynaptic dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain, although their benefits may also be related to their antagonist activity at dopamine receptors in other areas of the CNS; additionally, atypical antipsychotic agents have efficacy at serotonin receptors. The dopamine receptor antagonist activity of antipsychotic agents at multiple sites in the CNS, and their antagonist activity at various other receptors in the CNS and throughout the body, contributes to the presence of numerous adverse effects. The presence of so many, and frequently severe, side effects makes patient compliance with long-term antipsychotic therapy an important clinical issue. However, newer, “atypical” agents are now available with greater specificity for the receptors that mediate antipsychotic actions than for the receptors that mediate adverse effects.
APPROACH TO:
Pharmacology of Antipsychotic Drugs
OBJECTIVES
1. List the classes and specific drugs that have antipsychotic activity.
2. Describe the mechanism of therapeutic action of antipsychotic agents.
3. Describe the common side effects of antipsychotic agents and indicate the receptors that mediate them.
DEFINITIONS
Acute dystonia: Sustained painful muscle spasms producing twisting abnormal posture usually occurring shortly after taking an antipsychotic medication.
Akathisia: Characterized by feelings of intense muscle restlessness or strong desire to move about, usually during the first 2 weeks of treatment with an antipsychotic medication.
Parkinson syndrome: Characterized by flat affect, shuffling gait, joint rigidity, and tremor that occurs weeks to months after treatment.
Neuroleptic malignant syndrome: Characterized by the acute onset of hyperthermia, muscle rigidity, tremor, tachycardia, mental status changes, diaphoresis, labile blood pressure, and exposure to a neuroleptic. This syndrome is associated with a significant mortality rate and usually occurs within the first few weeks of therapy.
DISCUSSION
Class
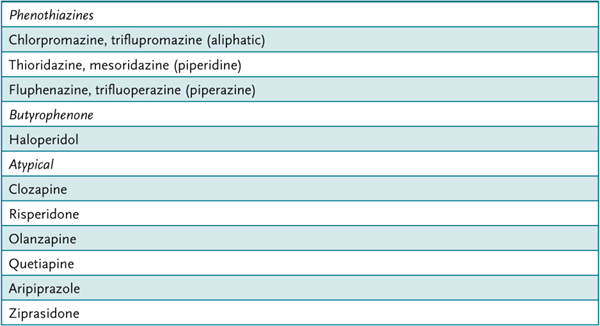
Antipsychotic drugs can be classified according to chemical structure as phenothiazines, butyrophenones, and an important group with diverse atypical structures. The phenothiazines are further subdivided according to side-chain constituents: aliphatic, piperidine, and piperazine (Table 14–1).
Table 14–1 • REPRESENTATIVE ANTIPSYCHOTIC DRUGS (SIDE CHAINS)
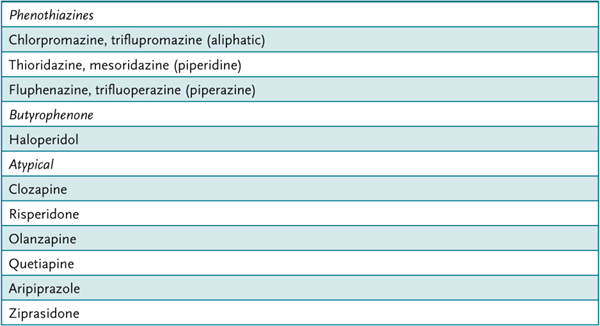
Although very similar in their therapeutic efficacy, the “low– (oral-) potency” aliphatic and piperidine phenothiazines have a somewhat different adverse effect profile than the “high-potency” agents that include the piperazine phenothiazines, and also thiothixene, and haloperidol.
The newer, atypical agents have generally unique structures; some studies have suggested that they may have greater therapeutic efficacy with regard to the negative symptoms of schizophrenia. They also have been documented to have superior adverse effect profiles. Recent clinical trials have called into question the safety of several of the newer agents. In summary, individual patient response to antipsychotic agents varies widely and often dictates drug selection.
Administration of the low-potency antipsychotic agents is more likely to result in autonomic adverse effects that include orthostatic hypotension caused by α-adrenoceptor blockade, and dry mouth, urinary retention, and tachycardia resulting from blockade of muscarinic cholinoreceptors. Their blockade of histamine H1 receptors in the CNS results in sedation. The still widely used high-potency agents, for example, haloperidol, are more likely to result in adverse neurologic effects. Among these are the EPSs, acute dystonia, akathisia, and Parkinson syndrome, which occur relatively early in therapy and are thought to be primarily mediated by blockade of dopamine D2 receptors in the nigrostriatal dopamine pathway of the basal ganglia. A late-occurring tardive dyskinesia that is often irreversible and that may be a result of the slow development of dopamine receptor supersensitivity also in the basal ganglia is more or less likely to occur with all antipsychotic agents except clozapine. A potentially fatal neuroleptic malignant syndrome is another serious adverse effect of antipsychotic agents in sensitive patients (1%). Also, hyperprolactinemia in women may occur as a result of enhanced prolactin release from the posterior pituitary, because of antipsychotic drug blockade (phenothiazines, butyrophenones, risperidone) of dopamine D2 receptors of the tuberoinfundibular dopaminergic pathway, which may lead to amenorrhea, galactorrhea, gynecomastia, decreased libido, and impotence. Weight gain is also a likely effect of many of these antipsychotic agents.
The atypical agents are less likely than the conventional agents to result in adverse EPSs. Like the conventional agents these can also cause potentially fatal neuroleptic malignant syndrome. Although most atypical agents do not cause hyperprolactinemia, risperodone, specifically, similar to conventional agents, can elevate prolactin. However, weight gain (clozapine, olanzapine, quetiapine), hypotension, and sedation are not uncommon events. Atypical antipsychotics (except aripiprazole and ziprasidone) can exacerbate diabetes and hyperlipidemia, as well as precipitate the onset of these illnesses. Routine lipid and diabetic screening is advised for patients taking these medications. Seizures (2–5%) and agranulocytosis (2% risk, 10% fatality) limit the use of clozapine to patients unresponsive to other agents. Both conventional and atypical agents may also cause QTc prolongation in the ECG, which predisposes the patient to a potentially fatal arrhythmia (torsades de pointes).
Mechanism of Action
The clinically useful antipsychotic drugs block postsynaptic dopamine D2 receptors, although the degree of blockade among the drugs varies greatly in relation to their action on other neuroreceptors, particularly serotonin 5-hydroxytryptamine 2A (5-HT2A) receptors and certain other dopamine receptor subtypes. Aripiprazole has a unique mechanism of action in that it is a partial D2 agonist.
Antipsychotic drugs appear to exert their therapeutic effect, at least in part, by inhibition of dopamine’s action in the mesocortical and mesolimbic dopaminergic pathways of the CNS.
Administration
All antipsychotic agents can be administered by either the oral or the parenteral route or both. Long-acting depot forms of antipsychotics improve patient compliance. The typical antipsychotics, fluphenazine decanoate and haloperidol decanoate, are available as parenteral depot preparations. Risperidone microspheres, olanzapine pamoate, and paliperidone palmitate are atypical depot formulations available.
Pharmacokinetics
Most antipsychotic agents are readily but incompletely absorbed. They are highly lipid soluble and have longer clinical duration of action than would be expected from their plasma half-life, probably as a consequence of their deposition in fat tissue.
Thioridazine, which is metabolized to mesoridazine, is the exception to the rule that hepatic metabolism of the antipsychotic agents results in less active metabolites.
Concurrent use of certain antipsychotic agents with other drugs that also block cholinoreceptors may result in additive peripheral and CNS dysfunction.
COMPREHENSION QUESTIONS
14.1 A 37-year-old man with psychosis has been treated with haloperidol. He has been developing Parkinson-like symptoms. Haloperidol-induced Parkinson syndrome is a result of haloperidol’s action in which of the following tracts?
A. Mesocortical tract
B. Mesolimbic tract
C. Nigrostriatal tract
D. Tuberoinfundibular tract
14.2 The therapeutic effect of haloperidol is mediated, at least in part, by its blockade of which of the following receptors?
A. α-Adrenoceptors
B. Dopamine D2 receptors
C. Histamine H1 receptors
D. Muscarinic receptors
14.3 Compared to the low-potency phenothiazine antipsychotic agents, haloperidol is more like to cause which of the following adverse effects?
A. Akathisia
B. Orthostatic hypotension
C. Sedation
D. Urinary retention
14.4 A 30-year-old woman is diagnosed with schizophrenia. Treatment is being weighed between typical and conventional antipsychotic agents. An advantage of atypical antipsychotic agents over conventional antipsychotics is:
A. Cheaper cost
B. Less tardive dyskinesia
C. Specificity for antagonism on D2 receptors
D. Less likely to cause diabetes
14.5 A 59-year-old male with schizophrenia and obesity presents for routine monitoring. He is currently on olanzapine as he developed tardive dyskinesia on haloperidol. This patient should be screening for which of these conditions due to his medication?
A. Hemachromatosis
B. Diabetes
C. Hemolysis
D. Malignancy
ANSWERS
14.1 C. Haloperidol-induced Parkinson syndrome is a result of inhibition of dopamine D2 receptors in the nigrostriatal tract of the CNS.
14.2 B. Antipsychotic drugs like haloperidol exert their therapeutic effect, at least in part, by inhibition of dopamine’s action at dopamine D2 receptors in the mesocortical and mesolimbic dopaminergic pathways of the CNS. A number of adverse effects of these drugs are caused by inhibition of dopamine action in the nigrostriatal and tuberoinfundibular dopaminergic pathways of the CNS; blockade of histamine, muscarinic, cholinergic, and α-adrenergic receptors in the CNS and the peripheral nervous system are also contributory.
14.3 A. Haloperidol is most likely to cause dystonia, akathisia, and Parkinson syndrome, whereas the low-potency phenothiazines are more likely to cause autonomic adverse effects that include orthostatic hypotension, sedation, and urinary retention.
14.4 B. Although tardive dyskinesia can occur with atypical agents, the frequency of this adverse effect is less frequent than with conventional agents. Because most of the atypical agents are still under patent protection, they are more expensive than the older, conventional agents. Atypical antipsychotics have divers actions on neuroreceptors, including antagonism of D2 receptors and action on serotonin receptors. Exacerbation or new onset of diabetes is more frequent with the atypical antipsychotics, except for aripiprazole and ziprasidone.
14.5 B. Atypical antipsychotics such as in this case have reduced motor side effects compared to the typical agents such as haloperidol. However, they have been associated with worsening metabolic parameters with respect to blood sugar and serum lipids.
PHARMACOLOGY PEARLS
 The low-potency antipsychotic agents are more likely to result in autonomic adverse effects that include orthostatic hypotension as a consequence of α-adrenoceptor blockade, dry mouth, urinary retention, and tachycardia resulting from blockade of muscarinic cholinoreceptors, and sedation (histamine H1-receptor blockade).
The low-potency antipsychotic agents are more likely to result in autonomic adverse effects that include orthostatic hypotension as a consequence of α-adrenoceptor blockade, dry mouth, urinary retention, and tachycardia resulting from blockade of muscarinic cholinoreceptors, and sedation (histamine H1-receptor blockade).
 High-potency agents, for example, haloperidol, are more likely to result in EPSs, acute dystonia, akathisia, and Parkinson syndrome, mediated by blockade of dopamine D2 receptors in the nigrostriatal pathway of the basal ganglia.
High-potency agents, for example, haloperidol, are more likely to result in EPSs, acute dystonia, akathisia, and Parkinson syndrome, mediated by blockade of dopamine D2 receptors in the nigrostriatal pathway of the basal ganglia.
 A late-occurring tardive dyskinesia is often irreversible and is a serious effect of many antipsychotic agents.
A late-occurring tardive dyskinesia is often irreversible and is a serious effect of many antipsychotic agents.
 A potentially fatal neuroleptic malignant syndrome is another serious adverse effect of antipsychotic agents in sensitive patients.
A potentially fatal neuroleptic malignant syndrome is another serious adverse effect of antipsychotic agents in sensitive patients.
 Hyperprolactinemia may occur as a result of enhanced prolactin release from the posterior pituitary, as a result of antipsychotic drug blockade of dopamine D2 receptors in the tuberoinfundibular tract.
Hyperprolactinemia may occur as a result of enhanced prolactin release from the posterior pituitary, as a result of antipsychotic drug blockade of dopamine D2 receptors in the tuberoinfundibular tract.
 Agranulocytosis may occur in patients treated with clozapine.
Agranulocytosis may occur in patients treated with clozapine.
 Atypical antipsychotics can cause metabolic syndrome.
Atypical antipsychotics can cause metabolic syndrome.
REFERENCES
Ananth J, Burgoyne KS, Gadasalli R, et al. How do atypical antipsychotics work? J Psychiatry Neurosci. 2001;26(5):385–94.
Freedman R. Schizophrenia. N Engl J Med. 2003;349(13):1738–49.
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353:1209–23.
Newcomber JW, Haupt DW. The metabolic effects of antipsychotic medications. Can J Psychiatry. 2006; 51(8):480.
Thacker GK, Carpenter WT. Advances in schizophrenia. Nature Med. 2001;7(6):667–71.
 What is the mechanism of therapeutic action of haloperidol?
What is the mechanism of therapeutic action of haloperidol? What mediates the extrapyramidal side effects (EPSs) of the antipsychotic agents?
What mediates the extrapyramidal side effects (EPSs) of the antipsychotic agents? Which autonomic nervous system receptors are antagonized by antipsychotic agents?
Which autonomic nervous system receptors are antagonized by antipsychotic agents? Mechanism of therapeutic action of haloperidol: Antagonist activity at postsynaptic dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain.
Mechanism of therapeutic action of haloperidol: Antagonist activity at postsynaptic dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain.