CASE 46
A 48-year-old man comes to your office with a 6-day history of worsening cough productive of green sputum. He has had fever and chills. He complains of pain in the right midback with deep breathing or coughing. Further history reveals that he has smoked one pack of cigarettes a day for 30 years. He has no other significant medical history. On examination, his temperature is 38.1°C (100.5°F); his respiratory rate is 24 breaths per minute; pulse, 98 beats per minute; blood pressure, 120/75 mm Hg; and saturation of oxygen, 96 percent on room air by pulse oximetry. Auscultation of his lungs reveals rales in the right lower-posterior lung field. The remainder of his examination is within normal limits. A posterior-to-anterior (PA) and lateral chest x-ray show a right lower-lobe infiltrate. A sputum Gram stain reveals gram-positive cocci, and subsequent sputum and blood culture results confirm the diagnosis of pneumonia caused by Streptococcus pneumoniae (pneumococcus). You treat him with a combination of amoxicillin and clavulanic acid.
 What is the mechanism of action of amoxicillin?
What is the mechanism of action of amoxicillin?
 What is the mechanism of action of clavulanic acid?
What is the mechanism of action of clavulanic acid?
ANSWERS TO CASE 46:
Antibacterial Agents
Summary: A 48-year-old man with pneumococcal pneumonia is being treated with amoxicillin and clavulanic acid.
 Mechanism of action of amoxicillin: Inactivation of bacterial transpeptidases and prevention of cross-linking of peptidoglycan polymers necessary for cell-wall integrity, resulting in loss of cell-wall rigidity and cell rupture; also inhibition of cell-wall synthesis.
Mechanism of action of amoxicillin: Inactivation of bacterial transpeptidases and prevention of cross-linking of peptidoglycan polymers necessary for cell-wall integrity, resulting in loss of cell-wall rigidity and cell rupture; also inhibition of cell-wall synthesis.
 Mechanism of action of clavulanic acid: Irreversible inhibition of β-lactamase.
Mechanism of action of clavulanic acid: Irreversible inhibition of β-lactamase.
CLINICAL CORRELATION
Penicillin is the prototype antibiotic in the β-lactam class. β-Lactam antibiotics interfere with bacterial transpeptidases and thereby prevent the cross-linking of peptidoglycan polymers essential for cell-wall integrity. They do this by binding to the active site of the penicillin-binding protein (an enzyme) that is involved in maintaining cell-wall stability. β-Lactam antibiotics are bactericidal in growing cells, with gram-positive bacteria being particularly susceptible. Penicillin has activity against many gram-positive aerobic organisms, some gram-negative aerobes and anaerobic organisms. It does not have significant activity against gram-negative rods. Amoxicillin is an extended-spectrum penicillin with better activity against gram-negative rods and similar activity against other organisms. Both penicillin and amoxicillin are susceptible to β-lactamases, which cleave the β-lactam ring required for antibacterial action. Clavulanic acid (and sulbactam and tazobactam) is structurally similar to penicillin. It has no antimicrobial activity of its own but it irreversibly inhibits certain β-lactamases. It frequently is given in fixed combination with amoxicillin, thus allowing it to be used to treat β-lactamase-producing organisms. Penicillins can cause hypersensitivity reactions in susceptible persons. Approximately 5 to 10 percent of penicillin-allergic persons will have a cross-sensitivity to cephalosporin drugs as well. Penicillins also have gastrointestinal (GI) side effects, and the addition of clavulanic acid significantly increases the incidence of diarrhea. Although antibiotic resistance should be considered in the choice of antibiotic therapy in streptococcal pneumonia, the incidence of resistance is declining due to the availability of a vaccine routinely given to children.
APPROACH TO:
Pharmacology of Antibacterial Agents
OBJECTIVES
1. Describe the factors in choosing appropriate antibiotic agents.
2. List the classes of antibiotics, and describe their mechanisms of action, therapeutic uses, and adverse effects.
3. Outline mechanism of development of bacterial drug resistance.
DEFINITIONS
Plasmids: Extrachromosomal genetic elements that may be transferred between bacteria.
Bactericidal antibiotics: Kill bacteria.
Bacteriostatic antibiotics: Prevent the growth of bacteria.
DISCUSSION
Class
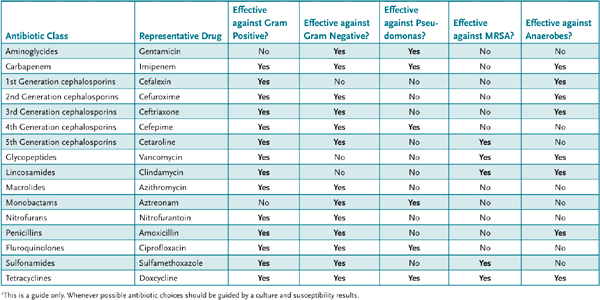
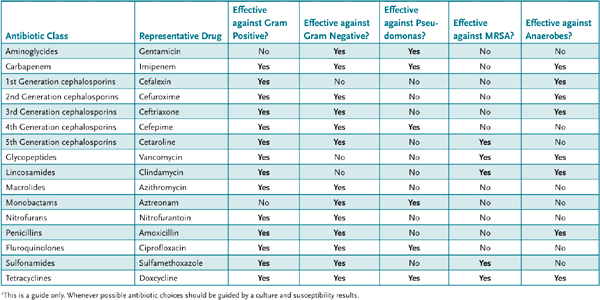
The basic principles for the selection of antibacterial therapy include consideration of factors such as the likelihood that the infection is bacterial and the identification of the likely infecting organism to support a rational selection of an antibiotic (Table 46–1). Consideration of host and drug factors that could influence antibiotic selection include identification of the site of infection, which will influence the selection of the antibiotic and its route of administration; recognition of concomitant diseases such as AIDS; recognition of the likelihood of drug allergies; recognition of hepatic or renal dysfunction that could alter antibiotic clearance; and recognition of drug toxicity, drug-drug interactions, drug resistance, the patient’s age or pregnancy or maternal status; and drug cost.
Table 46–1 • ANTIBIOTIC DRUG TARGETS*
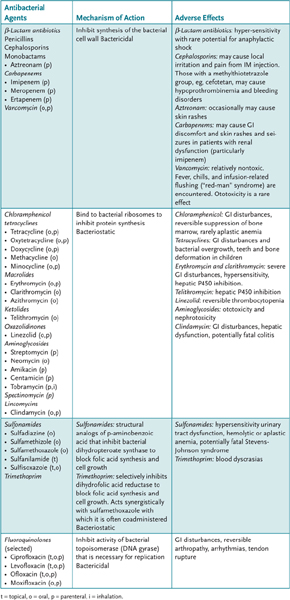
Antibacterial agents, which target specific components of microorganisms that are unique or more essential to their function than they are to humans, are classified according to their mechanisms of action. The component targets include enzymes necessary for bacterial cell-wall synthesis, the bacterial ribosome, and enzymes necessary for nucleotide synthesis and deoxyribonucleic acid (DNA) replication.
Resistance of pathogens to antibacterial and other chemotherapeutic agents may be the result of a natural resistance or may be acquired. In either case, it occurs through mutation, adaptation, or gene transfer. The mechanism of resistance for any antibacterial agent varies, but is a result of either changes in uptake of drug into, or its removal from, the bacterial cell, or to changes in the bacterial cell target site of the drug from a gene mutation. Multiple drug resistance is also a major impediment to antibacterial therapy and may be chromosomal or plasmid mediated, where genetic elements from resistant bacteria that code for enzymes that inactivate antibacterial agents are transferred to nonresistant bacteria. The emergence of drug resistance is to a large degree the result of the widespread and often unnecessary or inappropriate use of antibiotics in humans.
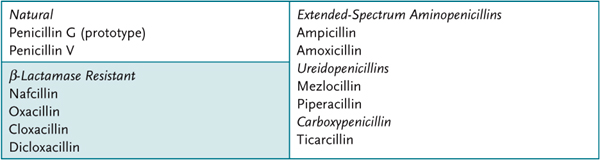
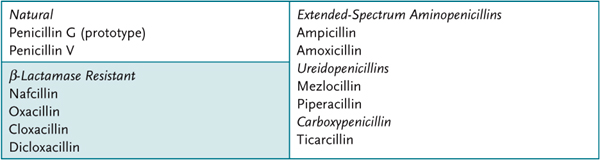
The penicillins (see above) include natural penicillins, penicillins that are resistant to staphylococcal β-lactamase, and extended-spectrum penicillins (Table 46–2).
Table 46–2 • PARTIAL LISTING OF PENICILLINS
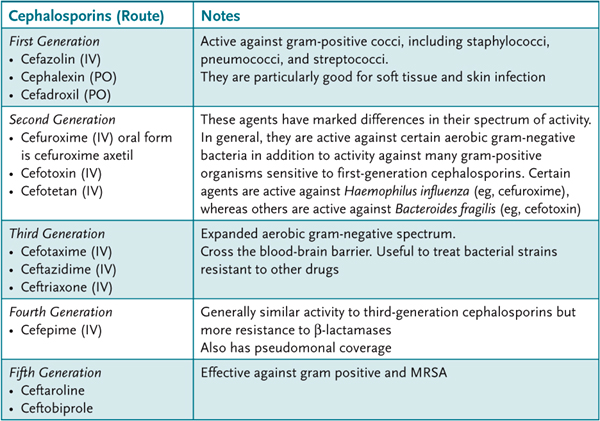
The cephalosporins are classified as first to fifth generation, according to their antibacterial spectrum (Table 46–3).
Table 46–3 • SELECTED LISTING OF CEPHALOSPORINS REPRESENTATIVE
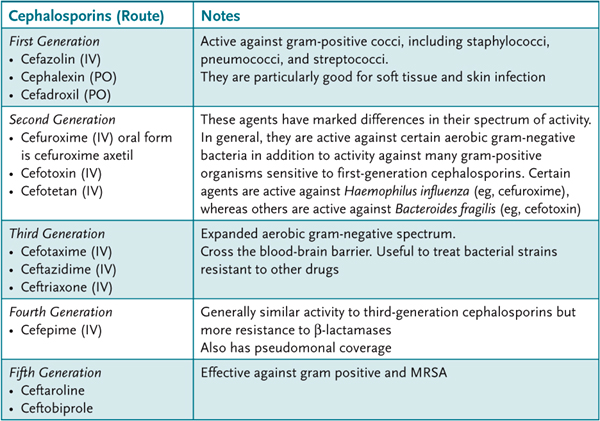
Table 46–4 lists these and other selected antimicrobial agents. Aztreonam, which is relatively β-lactamase resistant, is the only available monobactam. It is nonallergenic and is active only against aerobic gram-negative bacilli (eg, pseudomonas, serratia). The carbapenems (imipenem, meropenem, and ertapenem), which are resistant to most β-lactamases, have a wide spectrum of activity against gram-positive and gram-negative rods and anaerobes. To prevent its metabolism, imipenem is administered with an inhibitor of renal tubule dehydropeptidase, cilastatin.
Table 46–4 • PARTIAL LISTING OF ANTIMICROBIAL AGENTS
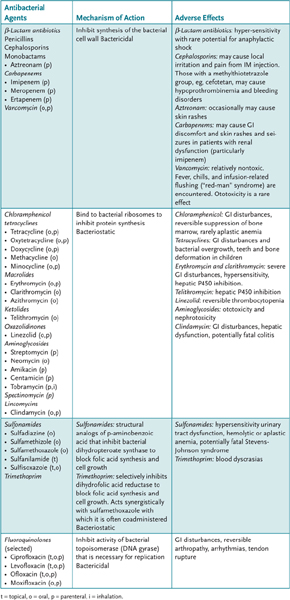
Vancomycin, which is unaffected by β-lactamases, inhibits bacterial cell-wall synthesis by covalent binding to the terminal two D-alanine residues of nascent peptidoglycan pentapeptide to prevent their elongation and cross-linking, thus increasing the susceptibility of the cell to lysis. It is active against gram-positive bacteria.
COMPREHENSION QUESTIONS
46.1 Which of the following is the most likely explanation for multiple drug resistance to antibiotics that spreads from one type of bacteria to another?
A. Adaptation
B. Decreased bioavailability
C. Gene transfer
D. Mutation
46.2 Penicillins inhibit which of the following bacterial processes/compounds?
A. Protein synthesis
B. Topoisomerase
C. Dihydropteroate synthase
D. Cell-wall synthesis
46.3 Ototoxicity and nephrotoxicity are characteristic adverse effects of which of the following?
A. Aminoglycosides
B. β-Lactam antibiotics
C. Chloramphenicol
D. Fluoroquinolones
ANSWERS
46.1 C. Antibiotic drug resistance can occur through bacterial cell mutation, adaptation, or gene transfer. The best route for multiple drug resistance that spreads from one type of bacteria to another is via plasmid or chromosomal gene transfer.
46.2 D. Penicillins inhibit synthesis of the bacterial cell wall. Chloramphenicol, tetracyclines, macrolides, ketolides, oxazolidinones, aminoglycosides, spectinomycin, and the lincomycin bind to bacterial ribosomes to inhibit protein synthesis. The fluoroquinolones inhibit activity of bacterial topoisomerase to inhibit protein synthesis, and the sulfonamides inhibit bacterial dihydropteroate synthase to block folic acid synthesis and cell growth.
46.3 A. Ototoxicity and nephrotoxicity are characteristic adverse effects of aminoglycosides. Chloramphenicol can cause GI disturbances, reversible suppression of bone marrow, and rarely aplastic anemia. As a group, the β-lactam antibiotics can cause hypersensitivity and have the potential to cause anaphylactic shock. The fluoroquinolones can cause GI disturbances, reversible arthropathy, and arrhythmias.
PHARMACOLOGY PEARLS
 β-Lactam antibiotics inactivate bacterial transpeptidases and prevent the cross-linking of peptidoglycan polymers essential for cell-wall integrity.
β-Lactam antibiotics inactivate bacterial transpeptidases and prevent the cross-linking of peptidoglycan polymers essential for cell-wall integrity.
 Both penicillin and amoxicillin are susceptible to β-lactamases.
Both penicillin and amoxicillin are susceptible to β-lactamases.
 To prevent its metabolism, imipenem is administered with an inhibitor of renal tubule dehydropeptidase, cilastatin.
To prevent its metabolism, imipenem is administered with an inhibitor of renal tubule dehydropeptidase, cilastatin.
 Vancomycin, which is unaffected by β-lactamases, is active against gram-positive bacteria.
Vancomycin, which is unaffected by β-lactamases, is active against gram-positive bacteria.
 Aminoglycosides may cause ototoxicity or nephrotoxicity and should be used with caution in those patients who have renal insufficiency or who are elderly.
Aminoglycosides may cause ototoxicity or nephrotoxicity and should be used with caution in those patients who have renal insufficiency or who are elderly.
REFERENCES
Conte JE. Manual of antibiotics and infectious diseases. Philadelphia (PA): Lippincott Williams & Wilkins, 2001.
Khardori N. Antibiotics – past, present and future. Med Clin North Am. 2006;90(6);1049–75.
Mehlhorn AJ, Brown DA. Afety concerns with fluoroquinolones. Ann Pharmacother. 2007;41:1859.
Robicsek A, Jacoby GA, Hooper DC. The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis. 2006;6:629.
Tenover FC. Mechanisms of antimicrobial resistance in bacteria. Am J Med. 2006;119(6 suppl 1):S3–10; discussion S62–70.
Wright AJ. The penicillins. Mayo Clin Proc 1999;74(3):290–307.
 What is the mechanism of action of amoxicillin?
What is the mechanism of action of amoxicillin? What is the mechanism of action of clavulanic acid?
What is the mechanism of action of clavulanic acid? Mechanism of action of amoxicillin: Inactivation of bacterial transpeptidases and prevention of cross-linking of peptidoglycan polymers necessary for cell-wall integrity, resulting in loss of cell-wall rigidity and cell rupture; also inhibition of cell-wall synthesis.
Mechanism of action of amoxicillin: Inactivation of bacterial transpeptidases and prevention of cross-linking of peptidoglycan polymers necessary for cell-wall integrity, resulting in loss of cell-wall rigidity and cell rupture; also inhibition of cell-wall synthesis.