
Now that you have read the first two chapters, you should feel comfortable in your understanding about what FODMAPs are, the foods they are found in, and how they can trigger symptoms of IBS. The low-FODMAP diet has been embraced around the world and it is likely you will meet more and more people following the diet as time passes. This chapter will teach you how you, too, can follow the diet.
Interestingly, the low-FODMAP diet differs from other diets used to manage adverse reactions to food, such as celiac disease and allergies. For example, a gluten-free diet for celiac disease involves the strict restriction of all gluten (even crumbs!) for life – no “breaking” the diet! For those with an anaphylactic allergy to nuts, it is important not to break the diet either, as there can be dire life-threatening consequences. These are examples of diets that require strict avoidance – eating a little bit of problematic foods is not OK.
There’s simply no point restricting more foods than you need to in order to feel well.
By contrast, the low-FODMAP diet has a lot of flexibility. This is a dietary management plan that is tailored just for you! People following the low-FODMAP diet will all have different needs. To help determine your needs, undertake the two-step process described. You will typically find that a small amount of foods containing FODMAPs is indeed alright, and you may find that you can tolerate more than just a little (it is a low-FODMAP diet, not a NO-FODMAP diet!). You may also find you don’t have a problem with every type of FODMAP – in fact many people find that while some types of FODMAPs are definite triggers for their symptoms, other types of FODMAPs can be well tolerated. Everyone is different.
Here are some suggestions on how to embark on your two-step low-FODMAP diet journey. It is recommended to undertake both Step One and Step Two in consultation with an experienced dietitian.
“ After many years of various tests, several dietitians, sleepless nights and not least intolerable pain, my boyfriend finally discovered the low-FODMAP diet. He has only been on it for one to two weeks so far but we are both noticing a huge difference. He is not in as much pain, he can sleep without waking up in the middle of the night due to a painful stomach and I have got my boyfriend back! ”
The aim of Step One is to investigate if FODMAPs are triggers for your IBS symptoms. This is usually done by restricting foods known to be high in all FODMAPs for six to eight weeks. This broad approach is suggested since many people don’t have their symptoms triggered by every type of FODMAP, and it can be hard to know which ones are your triggers as you commence this first step of your low-FODMAP journey.
If you’re like many people and eat a variety of foods, then the culprits could be dispersed throughout your diet and it won’t necessarily be clear which one is the trigger. In such instances, it’s often most practical to cut out all FODMAPs from your diet for six to eight weeks, as that can be the fastest pathway to symptom relief.
You may be able to work out which FODMAPs are the most likely triggers for your symptoms, especially with the help of an experienced dietitian. This is best done by keeping a seven-day food and symptom diary.
You may be able to work out which FODMAPs are the most likely triggers for your symptoms, especially with the help of an experienced dietitian. This is best done by keeping a seven-day food and symptom diary and looking out for a relationship between the frequency and severity of your symptoms and the foods you ate anytime earlier in the day. Consume and record your usual diet – the food and drink you usually consume when you experience your IBS symptoms. By asking you some specific questions and looking at a completed seven-day food and symptom diary, your dietitian may establish that you seem to tolerate one or more types of FODMAPs. For example, the information that your dietitian gathers may indicate you can tolerate milk. If you can, then lactose may not be a problem for you. It is wise to look at the list of foods high in lactose and be sure that none of these trigger symptoms in you. If you and your dietitian are confident lactose is not your problem, then it may be decided that lactose does not need to be restricted in Step One.
Although some individualization in the first step is possible (such as the lactose example just described), the more common approach is to restrict foods in all types of FODMAPs. Try the Step One menu plans to help guide you to delicious eating while restricting all FODMAPs.
This first step highlights the role FODMAPs play in triggering your symptoms. The goal of this step is for you to attain relief with your IBS symptoms by restricting high-FODMAP foods from your diet. It’s then important to have a review appointment with your dietitian to assess your symptom response and begin Step Two.
“ I’m twenty-two years old. I have suffered from horrible IBS symptoms my entire life, and over my entire life I’ve been through many tests for celiac disease, lactose and fructose intolerance. Up until Christmas Day, nobody had been able to tell me anything or help me manage my symptoms. My cousin showed me your low-FODMAP diet in your book, The Complete Low-FODMAP Diet, and it has been a godsend to me. I want to thank you for your work. I’ve suffered badly from my IBS and now I can live normally and enjoy life more. ”

Please record all food and drinks consumed. Brand names can be helpful. Please also indicate any gastrointestinal symptoms and the time you experience them.
Note: You can download a printable PDF of the charts in this ebook from this webpage: theexperimentpublishing.com/?isbn=9781615193158
It is now time to assess how well your symptoms have improved after the first six to eight weeks doing Step One. You (and your dietitian at your review appointment) can now evaluate how symptoms have changed since you commenced the diet. For help finding a dietitian, see the resources in Part 3. If your symptoms have had a noticeable, satisfactory improvement, then it is time to follow a plan to reintroduce foods slowly, in a structured, individualized way, to determine types and amounts of FODMAPs you can tolerate.
There’s simply no point restricting more foods than you need to in order to feel well. Although Step One is important to determine if FODMAPs are triggers for your symptoms, it’s usually more restrictive than necessary for you to achieve symptom relief. It’s much better to eat a greater variety of foods and feel just as well as when you were eating less variety in Step One. Additionally, FODMAPs are like prebiotics; restricting all FODMAPs may change the amount and type of bacteria in your large intestine. Any FODMAPs you can tolerate are good for other aspects of your bowel health.
First, a reminder of some key FODMAP facts:
The aim of Step Two is to liberalize your food intake so that your diet is not unnecessarily restricted. It is recommended to work with your dietitian so they can show how to include a greater variety of foods in your diet while maintaining the symptom control you achieved in Step One.
It’s not desirable to completely restrict all high-FODMAP foods forever. It’s preferable that you work out:
This is done via a plan to reintroduce foods slowly, in a structured way, one FODMAP at a time, so you can establish your own individualized FODMAP-modified dietary needs.
Reintroduce FODMAPs in a controlled way to determine the types and amounts of FODMAPs you can tolerate while still enjoying symptom relief.
Each week, test a new FODMAP. The foods suggested contain only one FODMAP. Consume that food three times in the test week in the amount specified. You don’t need to eat it every day. The purpose is to see if you can handle the food in the suggested quantity, at a “normal” frequency in the diet, without pushing yourself. (Too much of anything can potentially cause symptoms in anyone!)
In summary:
The Step Two menu plans will help you with reintroducing lactose, sorbitol, mannitol, excess fructose, fructans and GOS (with some fructan tolerance, too, as most foods with GOS in them also have fructans).
Now that you have completed all of the reintroductions for the FODMAP groups you restricted in Step One, you are aware of the types and amounts of FODMAPs that are your symptom triggers.
You can now include other foods containing the FODMAPs that you tolerated in your reintroduction trial into your diet again. See the other foods that contain the FODMAPs you now tolerate, and enjoy them as tolerated. Note that if your symptoms return, it may be due to the accumulation of different FODMAPs (e.g., having an additive effect), as well as large doses of individual FODMAPs. Also be aware that your sensitivity to FODMAPs may change over time, so it is recommended you try reintroducing any failed FODMAP again in the future.
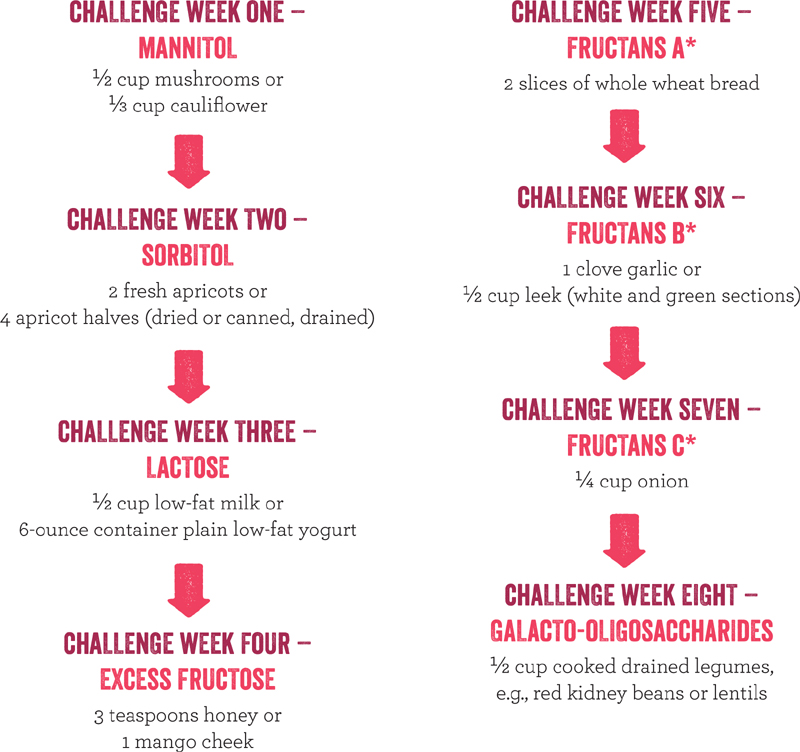
* A wide range of foods contain fructans in varying amounts. So the fructan challenge is staggered over three levels, increasing in the amount of fructans at each level from A to C. This is helpful to show that in someone who passes fructan challenges A and B but doesn’t tolerate challenge C, it doesn’t have to mean all fructan-containing foods need to be restricted – foods that are the equivalent of levels A and B should be tolerated.
Fructan Level A equivalents: crackers, rye bread, barley bread, spelt pasta
Fructan Level B equivalents:
Remember, several foods contain more than one FODMAP. For example, apples contain both excess fructose and sorbitol. If you found during the reintroduction process that you can tolerate more than one FODMAP, you can trial your tolerance to foods that contain the FODMAPs that you tolerated. So if you can tolerate excess fructose and sorbitol, then you may now like to trial your tolerance to apples.

The low-FODMAP diet doesn’t cure IBS; rather, it is an effective treatment to minimize symptoms. It works to make IBS symptoms manageable in the majority of people who try it. Around 75 to 80 percent of those who go on the low-FODMAP diet are happy with their symptom response, as shown through many of the real-life testimonials in this book. However, if you try the low-FODMAP diet and it does not adequately manage your symptoms, you may be wondering what to do next. Your symptoms could be triggered by other foods or food components, including alcohol, fat, caffeine, gluten, or natural food chemicals, including salicylates, amines and glutamates. If you are confident that what you eat triggers your symptoms, consult with a gastrointestinal specialist dietitian to explore further the relationship between your food intake and your symptoms.
Although food seems to be the logical trigger for IBS symptoms (after all, food goes into the digestive tract, which is where the symptoms occur), it is sometimes incorrectly blamed. In many people, food isn’t the main trigger for IBS symptoms, but rather psychological factors such as stress, worry, anxiety and depression. Some exciting research findings have come about from gut-focused hypnotherapy, cognitive behavioral therapy, mindfulness and other strategies to help manage these psychological influences. If you feel that these may be affecting your symptoms, or if you haven’t improved after dietary changes, then I recommend speaking with your dietitian regarding a recommendation for a gut-focused clinical hypnotherapist or other IBS-focused psychologist who may be able to assist. You should also discuss this with your doctor.
BEING VEGETARIAN ON A LOW-FODMAP DIET
Eating vegetarian may be a religious, lifestyle or other choice, and people who follow a vegetarian diet can indeed eat flavorful and exciting foods. It’s important to ensure that any vegetarian diet provides all the nutrients required daily for good health. A vegetarian meal is not simply a plate of meat and three vegetables with the meat taken off. Such a meal would be lacking in protein, vitamin B12, and other essential nutrients such as iron and zinc.
In a vegetarian diet, legumes (e.g., chickpeas, various dried beans, lentils, lupins and soybeans) are often major sources of protein. While on the low-FODMAP diet, particularly in the first step, these foods are restricted. Alternative low-FODMAP vegetarian sources of protein are listed below, and may be sufficiently varied for you in the first step. Also see sample vegetarian and vegan low-FODMAP diet menu plans.
Protein-rich vegetarian foods and beverages:
In the second step, you can continue to enjoy the high-protein foods listed above and also try to include small amounts of legumes and lentils in your diet (because of their nutritional importance), up to your symptom threshold. Lentils contain fewer FODMAPs than legume beans and chickpeas; a half cup of cooked, drained lentils contains fewer amounts of GOS and fructans compared with other legumes. You might find that you can manage your symptoms by being stricter in cutting out other FODMAP food sources so that you can “fit” these nutritious foods within your threshold.
Vegetarians should also ensure they have adequate intake of iron and zinc. Good vegetarian sources of iron and zinc include eggs, quinoa, brown rice, leafy green vegetables and nuts. Iron from plant sources is called non-heme iron, and is not absorbed as well by the body. Try to have a food containing vitamin C with your non-heme-iron foods to optimize iron absorption. A special note for vegans on a low-FODMAP diet:
These menu plans will provide you with balanced meals during either one week of the strict phase (Step One) or one week of the reintroduction phase (Step Two). I haven’t provided exact quantities because we all have different energy needs and this isn’t a weight-loss diet.
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Obviously, the foods listed in Step One menu plans are the low-FODMAP varieties, so “fruit” will mean balanced fruit and you’ll need to check suggested quantities of other foods.
Notes: The following low-FODMAP menu plans have some gluten-containing suggestions. Please choose only gluten-free foods if you also follow a gluten-free diet. When a meal calls for sandwich bread, use a maximum of two slices in the meal. Also note LF means lactose-free (not low-fat).
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|
|
Day |
Breakfast |
Lunch |
Dinner |
|---|---|---|---|
|
Monday |
|
|
|
|
Tuesday |
|
|
|
|
Wednesday |
|
|
|
|
Thursday |
|
|
|
|
Friday |
|
|
|
|
Saturday |
|
|
|
|
Sunday |
|
|
|