Until recent decades, few seriously ill people got a second chance at life. It wasn’t until the twentieth century that effective treatments were developed for many diseases. Now, antibiotics and other medical interventions routinely preserve life for many who might otherwise die. Like people with serious infections and people with cancer, people with kidney failure are now having much longer life expectancies than they would have had in the past. In the past, the kidneys of people with kidney failure deteriorated to the point where uremia, an excessive buildup of toxins in the blood, resulted in death.
Today, however, there are treatments for kidney failure, including dialysis. Although tested as early as the nineteenth century, dialyzing blood to reduce uremia only became a useful treatment for chronic kidney failure in the 1960s. Now dialysis is in use all over the United States and is available to anyone who needs it. According to the latest statistics from the National Institutes of Health, more than 381,000 people were on some form of dialysis at the end of 2008.1
There are two forms of dialysis to treat kidney failure: peritoneal dialysis and hemodialysis. Both forms of dialysis move toxins across a barrier through which only some substances can pass. The following section explains the basic concepts of dialysis.
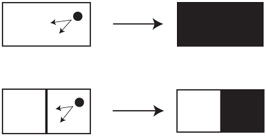
Dialysis involves filtration. Start with a basic concept: imagine a tank of water into which you carefully place a drop of ink in one corner of the tank. The concentrated ink tends to diffuse over time throughout the entire container of water until it reaches the same concentration in all parts of the tank (figure 6.1, top).
Now insert a barrier, through which nothing can pass, in the middle of the tank. The ink diffuses throughout only half the container, as shown in figure 6.1 (bottom). If, however, you punch tiny holes into the barrier, ink will flow through them—as long as the ink molecules are smaller than the holes. If the molecules are smaller, they disperse throughout the entire container of water (just like in figure 6.1, top). If the holes are too small for the ink molecules to pass through, the ink remains on one side of the barrier (figure 6.1, bottom).
Increasing the volume of the left side of the tank causes the ink to diffuse faster through the barrier until the concentration of ink is equal on both sides, while the amount of ink is reduced on the right side (see figure 6.2). For example, if you place 3 grams of ink in the right side of the tank with 1 liter of water and the ink moves through the barrier to the other side with 2 liters of water, the concentration of ink will eventually be equal on both sides of the barrier. This means only 1 gram remains on the original side of the barrier, and the remaining 2 grams have crossed the barrier. Thus, on the original side, the concentration of ink declined from 3 g/l to 1 g/l, while on the other side the concentration rose from 0 g/2 l to 2 g/2 l, or 1 g/l. (Figure 6.2 shows the amount of ink on each side of the barrier rather than the concentration of ink. Because the concentration would be equal on each side, if concentrations were illustrated, both sides would be the same shade, as in the top part of figure 6.1.)
Figure 6.1. Dialysis as Filtration I. With no barriers, a substance will diffuse uniformly (top). If a barrier is added, diffusion will only occur in half the container (bottom).
Figure 6.2. Dialysis as Filtration II. This figure shows the amount of ink on each side of the barrier rather than the concentration of ink.
Since the concentration would be equal on each side, if concentrations (rather than amounts) of ink were illustrated, both sides would be the same color, as in the top part of figure 6.1.
This concept, called dialysis, has been used for years by biochemists to purify chemicals. Similar to the ink analogy, dialysis involves a semi-permeable membrane (a barrier with holes) that allows some substances to pass through and not others, depending on the size of the molecules involved. To accomplish this, the chemical needing purification is placed into a small sac made of the membranous material (the barrier from above) through which the substance to be purified cannot pass. Next, the sac is placed in a volume of appropriate solution much larger than the volume of solution in the sac. The impurities that can pass through the membrane will flow until the concentration is equal on both sides of the membrane, but reducing their amount inside the sac. For maximum efficiency, the solution is changed frequently to allow for the greatest removal of the contaminants in the sac. When successively repeating the exchanges, nearly all of the impurities will eventually be removed.
This is the same basic approach to filtering the blood of people with kidney failure. Early studies in the 1940s, using this principle of dialysis to clean human blood, used pig intestines as the semi-permeable membrane, with the blood passing through the interior part. The intestines were placed in big wooden vats of solution composed of salts and buffers compatible with blood. Other laboratories tried using cellophane. The idea was to remove the toxins without removing cells and important proteins from the blood. This approach proved more difficult than simple biochemical dialysis, but over time, with further refinements and miniaturizing the process, the modern forms of dialysis were born.
Today, peritoneal dialysis and hemodialysis are the most common forms of dialysis. Hemodialysis is more routinely used, but increasing numbers of patients are choosing peritoneal dialysis because of its advantages. There are disadvantages to both forms of dialysis, however; these are covered in depth later in this chapter.
The principles of peritoneal dialysis remain the same as described above, but the application is a bit more complicated. Like the biochemical approach to dialysis, peritoneal dialysis takes advantage of the semi-permeable membrane that lines the peritoneal cavity of the abdomen. Some substances can pass through it, others cannot. Tiny blood vessels are embedded in this peritoneal membrane. The blood from the body is analogous to the contents of the membranous sac described above. A solution, called the dialysate, is placed in the abdomen, allowing the toxins in the blood to flow through the peritoneal membrane into the solution (see figure 6.3). This occurs because the concentration of toxins in the blood is higher than it is in the dialysate (as in figure 6.2). To avoid loss of needed substances in the blood, the dialysate contains salts and buffers in concentrations equivalent to those normally found in the blood, creating equal concentrations of these substances on both sides of the membrane.
Because fluid balance is compromised in people with kidney failure, dialysis must also remove excess water from the body. In peritoneal dialysis, the dialysate contains glucose (sugar) to help remove the excess water. Because the concentration of glucose exceeds the concentration in the blood and does not appreciably pass into the body, excess fluid in the blood flows through the peritoneal membrane into the dialysate to dilute the glucose. To remove more fluid, higher concentrations of glucose are needed. The rate of diffusion of toxins into the dialysate declines with time, so the dialysate must be exchanged up to five times a day in order to maximize the removal of the toxins.
Before peritoneal dialysis can be performed, a surgeon must place a special catheter inside the abdominal wall (see figure 6.4). The part of the catheter that is inside the abdominal wall is either straight or curled like a pig’s tail, and has holes in it, whereas on the outside the catheter is straight, solid, and flexible and has a hole only at the outside tip. The hole in the abdomen through which the catheter exits is known as the exit site. The subcutaneous and peritoneal cuffs hold the catheter in place, and are sewn into the abdominal wall. With peritoneal dialysis it is crucial to avoid infections, which can occur because either the catheter or the exit site becomes contaminated. After the catheter has been in place for about two weeks, dialysis can begin. Once an exchange has been completed, a sterile cap with an antiseptic (like Betadyne) on the inside is screwed onto the outside end of the catheter (on the left ends of the catheters in figure 6.4) until the next exchange.
Figure 6.3. Dialysate Flowing into the Abdomen
Figure 6.4. Straight Catheter (top) and Curled Catheter (bottom) Used for Peritoneal Dialysis
A surgeon has flexibility on where to place the catheter. Unfortunately, I did not talk with my surgeon about placement because I did not know that I could. As a result, when I received a peritoneal catheter, it was placed at my waistline. Wearing pants, with the subcutaneous and peritoneal cuffs directly under my belt, was very uncomfortable. Talk with your surgeon about what options he or she can provide for catheter placement that will minimize discomfort.
To perform exchanges, you need good manual dexterity, but there are devices to help people with physical limitations. There are even devices that help blind people with exchanges.
Peritoneal dialysis is typically begun using a procedure known as continuous ambulatory peritoneal dialysis (CAPD), in which dialysis occurs throughout the day between changes of the dialysis solutions (called exchanges). Exchanging solutions is relatively simple—it is a process that takes about twenty minutes, once you are used to it. What follows is the description of a typical procedure for performing exchanges to give you an idea of what is involved.2 (Note: The following description is not a substitute for appropriate training by a qualified dialysis health care provider. Talk to your doctor about the best way to perform your exchanges.) The exchange process must be sterile, so you must make every effort to avoid contamination. Hand washing with antibacterial soap or other suitable decontaminant is required at critical steps in the process. You may also want to dry your hands with a fresh paper towel rather than a cloth towel, to reduce possible contamination from the soiled cloth. Your dialysis center may provide you with an ultraviolet lamp to sterilize the connections between the tubing and your catheter.
Dialysis bags contain sterile solutions and come in sealed outer bags. After washing your hands, you will open the outer bag and remove its contents. Bags of dialysis solution include an attached drain bag, collectively known as a Y-set (see figure 6.5). Before starting, warm the dialysis solution to body temperature (easily done in a microwave oven). Warm solution will help prevent abdominal cramping. Attach the fluid-filled bag to a bag pole, and start your exchange.
Figure 6.5. Y-Set Used in Dialysis
After washing your hands and drying them with a paper towel, remove and discard the cap on the catheter. Then, attach the catheter to the system, which has a tube to the drain bag and one to the bag containing fresh dialysate. Before flow can occur, break two seals—one on the dialysis bag and one attached to the catheter. After allowing some dialysate to pass through the lines to prime the system (see the upper left side of figure 6.6), clamp the line to the dialysate bag and open the catheter line to allow drainage of your peritoneal fluid (see the upper right side of figure 6.6).
Once drainage is complete, unclamp the line to the dialysate bag to allow flow of some fresh solution into the drain bag to remove bubbles (see the lower left side of figure 6.6), clamp the tube to the drain bag, and then allow flow of fresh dialysate into your abdomen (see the lower right side of figure 6.6). Because the force of gravity helps the dialysate to flow more easily, hang the bag above your head. When the bag is empty, clamp the tube from the dialysate bag and wash your hands again. Then, detach the catheter from the exchange system and immediately screw a fresh cap containing Betadyne on the catheter. Finally, empty the drain bag and then discard the whole system. At this point, your exchange is complete.
Dialysis exchanges can be done almost anywhere you can find privacy. Avoid doing exchanges in public bathrooms or other places where there might be contamination. It is also best not to have people in the same room while you are exchanging—again, because of the risk of contamination.
If you work while on peritoneal dialysis, you will have to find a way to do exchanges in an office or comparable room. If there is a drop ceiling, you can attach the dialysate bags to the ceiling grid with an S-hook, like a plant holder. Otherwise, you may use a bag pole. During exchanges, you can continue working as long as you have privacy. To minimize the number of exchanges at work, do the first one as soon as you get up in the morning at home, one just before lunch at the office, one just before leaving for home at the end of the workday or when you first get home, and the last one just before going to bed.
Figure 6.6. Dialysis Exchange with Peritoneal Dialysis
This scenario may not work for everyone. For example, if you do not have your own office or another suitable place to perform exchanges, you may not be a candidate for CAPD. Continuous cyclic peritoneal dialysis may be a better alternative.
Like CAPD, continuous cyclic peritoneal dialysis (CCPD) can be a useful option. CCPD uses a machine, called a cycler, which performs exchanges during the night while you are asleep (see figure 6.7). The machine (manufactured by Baxter International, Inc., in Deer-field, Illinois) consists of several parts: (1) a dialysis bag heater; (2) a peristaltic pump inside the machine; (3) a place for a cassette (behind the door in figure 6.8); and (4) a computer (behind the control panel in figure 6.8) to run everything. The cassette controls the flow of fluid from dialysate bags to the abdomen and channels used dialysate to waste. All of the tubing attached to the cassette is needed for dialysis (see the disposable dialysis set in figure 6.9). The cassette works with the peristaltic pump to roll the fluids through the tubing. The computer is programmed to direct the flow either to waste or from one of the dialysis bags.
The rules for use of a cycler are similar to the rules for CAPD, especially when it comes to cleanliness. With practice and training on how the machine works and how to avoid contamination, you can set up the cycler for use in about ten minutes. First, place a 5-liter dialysis bag on top of the cycler where the heater is located. Next, put the cassette in its receptacle and attach the drain line, routing it to a drain, like a toilet, sink, or bathtub. Before attaching the appropriate tubes to the dialysis bags, wash your hands to avoid contaminating the bags when you insert the tubes. When the cycler has filled the tubing with fluid, wash your hands again, remove and discard the cap on your catheter, and then attach it to the tube at the far left of the organizer (see figure 6.9).
Figure 6.7. Cycler Used in Continuous Cyclic Peritoneal Dialysis
Figure 6.8. Parts of the Cycler
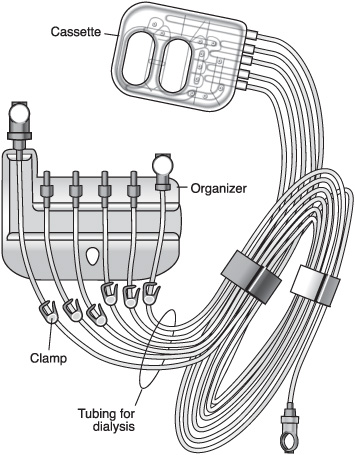
Figure 6.9. Organizer and Tubing of the Cycler
Once the cycler is activated, you can go to sleep. While sleeping, if you turn more than once in succession in the same direction, you might become entangled in the tubing or crimp the tube. If this happens, an alarm will sound to awaken you, and the cycler will stop itself, as a safety measure. Train yourself to roll only back and forth when you want to change your sleeping position.
While you are asleep, the cycler does several exchanges as programmed on the computer, based on your nephrologist’s prescription. As the amount of dialysate in the bag on the heater declines, the computer begins pumping dialysate from the other bags, so that the heater can warm the solution from those bags before use. After washing your hands the next morning, detach your catheter from the cycler and screw on a fresh cap containing Betadyne. To complete the process, discard all the plastic tubing and the cassette. This process at first seems complicated but it becomes less so with practice. The biggest advantage of CCPD is that fewer exchanges are needed during the day, especially if you still have some residual kidney function.
Dialysis is a prescribed treatment and, just like with other prescriptions, its effectiveness needs to be monitored. Nephrologists use two methods to determine how efficiently your treatment removes wastes from your blood. One test is the creatinine and urea clearance. This test is similar to the test your doctor requested to determine your kidney function before your kidneys failed (see chapter 4). To have the test now, you will collect all of the dialysis bags over a twenty-four-hour period as well as any urine you still produce in a large container. When you take the specimens in for analysis, you will be asked to provide a blood sample to determine how much creatinine and urea were removed from your blood.
Another way to measure the efficacy of your dialysis treatment is through a peritoneal equilibrium test (PET). In this test, you will be asked to provide a sample of dialysate at hourly intervals for up to four hours. The dialysate will be tested. The rate at which dialysis removes urea and creatinine from your blood and the extent to which your body absorbs sugar from the dialysate will tell your nephrologist how many exchanges you need to maximize the effectiveness of treatment. From this test your nephrologist can determine if your peritoneal membrane is a rapid transporter or a slow transporter. If it is a rapid transporter, your blood can more easily absorb glucose from the dialysate. This feature can make it difficult to maintain your blood sugar if you have diabetes; as a result, a person with diabetes needs more frequent exchanges. If your membrane is a slow transporter, however, you would benefit from fewer exchanges, with the dialysate remaining in your abdomen for a longer period.

Both CAPD and CCPD offer a great deal of freedom compared to hemodialysis. However, peritoneal dialysis may not be for everyone. Many nephrologists do not offer peritoneal dialysis as an option because some of their patients have developed peritonitis (an inflammation of the lining of the abdomen) from it. But peritoneal dialysis is worth considering if you have the discipline to keep up with all of the exchanges and observe the routines necessary to maintain the required cleanliness. Your nephrologist will help you weigh the pros and cons of peritoneal dialysis (including peritonitis, covered later in this chapter) and will help you decide if peritoneal dialysis is right for you.
Hemodialysis works on a principle similar to that of peritoneal dialysis, except the blood is cycled outside the body through a special filter, called a dialyzer, by a machine that is usually located in a dialysis center (see figure 6.10). Unlike peritoneal dialysis, which is a continuous form of dialysis, hemodialysis is intermittent. Thus, fluid, toxins, and electrolyte imbalances build up between sessions of hemodialysis, which means that the patient must restrict fluid intake and limit some foods. Most patients go to a center three times a week, with each dialysis session typically lasting three to four hours.
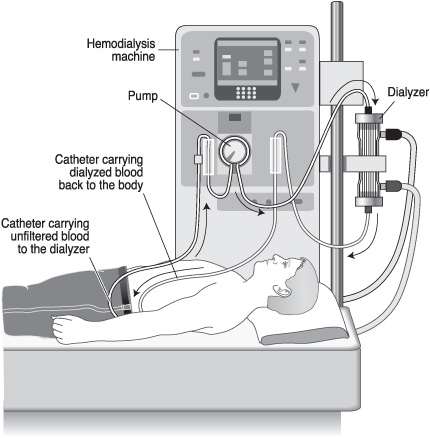
Figure 6.10. Dialyzer Used in Hemodialysis
Some dialysis centers offer home hemodialysis. If you have someone who can help you set up the machine, insert the needles into your fistula or graft, and monitor your session, home hemodialysis may be an attractive option, especially if you cannot schedule dialysis around work or if your center is not open late in the day. In addition to regular four-hour, three-day-a-week sessions, you may be a candidate for daily dialysis, which would reduce the accumulation of fluid and toxins between sessions. Home hemodialysis sessions last two hours each day, or they can be performed during the night while you sleep. Research suggests that daily hemodialysis may provide a better outcome than three-day-a-week, in-center sessions, since it is a more continuous form of hemodialysis. An increasing number of patients dialyze at home, as long as their dialysis center can provide adequate oversight. To dialyze at home, you must have a person assisting you each time you dialyze, to monitor the treatment in case you experience bleeding or a drop in blood pressure. If your center offers home hemodialysis, consult your nephrologist to see if it is a good choice for you.
The core of hemodialysis is the dialyzer, also known as an artificial kidney. The filter is composed of tiny filaments (semi-permeable membranes) through which the blood passes (see figure 6.11). These filaments are bathed in a continuously flowing dialysate containing salts and buffers in concentrations to avoid excessive loss of these substances from the blood. This process in hemodialysis is analogous to the presence of dialysate in the abdomen when using peritoneal dialysis. The blood cells and large molecules pass through the dialyzer and return to the body, while the toxins flow freely through the pores in the filaments and wash away.
Figure 6.11. Filaments Comprising the Filter of the Dialyzer
If you are to receive hemodialysis on a regular basis, your nephrologist or a surgeon must perform a surgical procedure to access your blood supply; blood will be drawn, pumped through the dialysis machine and dialyzer, and then returned to your body. Typically, an access is placed when the estimated GFR is below 30. With sufficient advance notice, most people can have a permanent access placed (see below). Initially, however, you may need a simple, temporary catheter placed in a large vein in your upper chest or groin. There are two types of dialysis catheter: the untunneled (above the skin) and the tunneled (below the skin) cuffed catheter.
Figure 6.12. Tunneled, Cuffed Hemodialysis Catheter
If you need dialysis immediately, you may get an untunneled catheter placed through the right internal jugular vein in your neck into the right atrium of your heart or through the femoral vein in your groin. Your nephrologist, interventional radiologist, or surgeon will perform the procedure while you are under local anesthesia. You may experience a brief, temporary fluttering in your heart if the tip of the catheter contacts heart muscle in the atrium. Untunneled catheters can be used only for a few days to a few weeks, because they tend to come loose, fall out, or become infected.
Tunneled, cuffed catheters may be used for a few weeks to a few months (see figure 6.12). Buried under the skin, the tunneled catheter is larger and longer than an untunneled catheter and is less likely to be dislodged. Moreover, sealed against bacteria, it is less likely to become infected.
Neither of these temporary catheters will serve you for the long term, however. A more permanent and stable access is needed. Two types of access are used: the fistula and the graft. For both of these, the dialysis technician will insert two needles, one to draw blood into the dialysis tubing, and one to return the blood. Both of them will provide a more efficient dialysis treatment than catheters, because the blood can be cleaned more quickly. Planning for a fistula or graft should be done early, to prepare for the time when dialysis will be needed.
To create a fistula, a surgeon joins an artery in an arm or groin directly to a vein (see figure 6.13). This procedure is done while you are under anesthesia. Over six to eight weeks, the pressure on the vessel increases, thickening the wall, and then enlarging the vein, making it easier for a dialysis nurse or technician to place the large needles for dialysis. The fistula is the most desirable access to have. Because the fistula is created from your own tissues, it is more resistant to infection, lasts the longest, and has the least number of complications, compared to the other accesses.
The graft is a Gore-Tex tube that a surgeon places under the skin, attaching one end of the tube to an artery in your arm or groin and the other end to a vein (see figure 6.14). In this way the procedure is like the fistula procedure, and it, too, is done while you are under anesthesia. The graft may be used sooner than the fistula—generally you can use it after a two-week recovery period. Grafts are not as good as fistulas for dialysis and are more likely to become infected than fistulas. They are a good substitute if the veins are too small for creating a fistula, however.
Figure 6.13. Fistula Joining an Artery and a Vein
Fistulas and grafts use needles with larger internal diameters than catheters, which allows the blood to move faster through the dialyzer. Dialysis is more efficient when blood can pass many times through the dialyzer during a session. However, inserting these larger needles can be painful. To help ease the pain, a dialysis nurse or technician can numb the injection site using a local anesthetic prior to insertion. In order to avoid clotting of the access, the tubing, and the dialyzer, heparin (a blood thinner) is injected into the access tubing. As a result, you may experience some bleeding from your access after dialysis. The staff in your center can minimize blood loss by applying pressure to the site using clamps. Some dialysis centers have special bandages containing a substance that helps clot blood.
Figure 6.14. Graft Joining an Artery and a Vein
As with peritoneal dialysis, nephrologists must determine how effective hemodialysis treatments are. Nephrologists use two measures for this purpose: the urea reduction rate (URR) and the Kt/V. For the URR, the dialysis technician draws a blood sample from a port on the dialysis machine at the beginning and at the end of dialysis treatment, and sends the blood samples to a lab to determine how much urea is in each sample. The URR is then calculated. A good URR is at least 0.65, which means that the treatment is removing at least 65 percent of urea from the blood.
Kt/V provides the best estimate of the effectiveness of your dialysis treatment. “K” stands for urea clearance during dialysis, “t” for time, and “V” for volume. The calculation of Kt/V is too technical to discuss here. Suffice it to say that, unlike the URR, Kt/V accounts for wide variations in weight among patients by determining the volume of water in the body and the nutritional status. Thus, the Kt/V provides a more accurate measure of effectiveness of a treatment. Good Kt/V values are at least 1.2 to 1.4, but higher values are not more beneficial. Using the Kt/V, a nephrologist can modify a prescription to maximize the efficiency of a dialysis session and help you feel better.
Your nephrologist has several ways to improve the quality of your treatment. For example, he can control the flow rate of your blood through the dialyzer. If you have a fistula or graft, he can increase your flow rate to obtain more dialysis for your time at the center. Another way to improve your treatment is to increase the time on dialysis. Finally, your nephrologist can order a larger dialyzer to allow more purification of blood each time it cycles through.
Whether using peritoneal dialysis or hemodialysis, your health must be monitored closely. Your nephrologist will assess whether your dialysis prescription is optimal, and she will also help you stay as healthy as possible, so you can feel your best and participate in many of your regular activities. Your laboratory measures provide an open window into your health that will help your nephrologist treat you appropriately.
As we learned before, some of these measures still must be monitored. For example, urea (the BUN number on a lab report) and creatinine levels reveal how well dialysis is cleaning your blood. If these levels are too high, you may need to adjust your diet, or your nephrologist may need to change your medications. Potassium levels are important in regulating heartbeat. If your potassium becomes too high, you could experience an irregular heartbeat or, in extreme cases, a heart block, resulting from a profound slowing of the heart rate. Calcium, phosphorus, and parathyroid hormone levels reflect your bone health. If phosphorous and parathyroid hormone levels are too high, you may have to limit further your phosphorus-rich foods or take higher doses of phosphate binders. Your nephrologist will also monitor your red blood cell count and iron levels. If you become anemic, you may require iron supplementation or erythropoietin injections.
There are other measures of your health. Albumin is a protein that can be a measure of your nutritional status. If albumin levels in the blood are too low, you will need to eat more calories and protein. Even if you are eating the recommended amounts of protein, you must consume sufficient calories from other sources, or your body will begin to burn protein for fuel. In addition, your nephrologist will assess your liver function as a general health measure and to look for toxicity from any of the medications that you take.
I recommend that you monitor and understand all of your laboratory results. Your nephrologist or dialysis nurse can teach you the meaning of excessively higher or lower values and tell you about any treatment changes that might be required if the laboratory results change. Learn how to manage your diet, lifestyle, and compliance to your dialysis regimen. You may want to keep copies of the results to help you get a sense of what is optimal for you. All of these steps will give you more control over your health and well-being.
Each type of dialysis has advantages and disadvantages. Talk to your nephrologist about these pros and cons to decide which type is best for you.
Only 8.2 percent of patients choose or are able to use peritoneal dialysis. The main advantage of peritoneal dialysis is independence, because it does not require trips to a dialysis unit. Peritoneal dialysis works best if you are a self-starter, disciplined, and physically able to perform the necessary steps involved. Peritoneal dialysis is a better treatment than hemodialysis for people with low or unstable blood pressure (which can make hemodialysis difficult or even hazardous), a bad heart, or poor vascular access to the blood supply. Peritoneal dialysis gives you more control over when, where, and how exchanges are performed. Depending on your work situation, you may be able to dialyze in your office without interruption. Having a private space during exchanges can make peritoneal dialysis the more attractive option. You can even dialyze in the car if you have a long drive ahead of you. Avoid exchanges in public bathrooms or other places where contamination is a greater possibility.
Peritoneal dialysis also requires fewer dietary restrictions than hemodialysis. However, the body loses a lot of protein during peritoneal dialysis. You may need to take a protein supplement. One drawback of protein supplements is that many of them contain high levels of phosphorus, especially if they come from dairy products. One excellent option is powdered egg whites, sold by Optimum Nutrition at www.optimumnutrition.com, which taste good and mix well with water, milk, or juices. Your local GNC store may carry this product or can order it for you. If you have diabetes, you may have trouble controlling your blood sugar with peritoneal dialysis, since the dialysate contains glucose. Talk to your nephrologist about the potential nutritional side effects of peritoneal dialysis.
If you like to travel or must travel often for your job, peritoneal dialysis may be preferable to hemodialysis. Dialysis bags and other treatment tools can be sent directly to your hotel. (Contact your equipment supplier in advance to make arrangements for delivery.) When traveling by plane, people who use CCPD can place the cycler in the overhead bins, as long as they are physically capable of handling a 30-pound machine. Because checked luggage can be lost, it is a good idea to carry extra caps and tubing in your carry-on luggage. For travel within the United States, the Americans with Disabilities Act protections should allow a traveler to take a dialysis machine onboard the plane, but with today’s strict airport security procedures, you should always check with the Transportation Services Administration before traveling with your dialysis equipment. For international travel, contact the airlines.
There are some disadvantages that may dampen enthusiasm for peritoneal dialysis. Peritoneal dialysis can be time-consuming and disruptive (although CCPD is less so). You must perform dialysis every day, regardless of your activities. Generally, you should be able to integrate exchanges into your life. However, depending on your work or travel schedule, you may have to arrange to do dialysis in the company of strangers, which you may find embarrassing. Occasionally, you can skip an exchange, which is not a disaster as long as you rarely do so. Remember, you will feel your best if you perform all of the exchanges that your nephrologist prescribes.
Although not as common as in the past, infections like peritonitis are still possible. If you live in an area where the water supply comes from an unchlorinated well, or if you have any concerns about recurring infections and showers, whether using city or well water, you should consult your doctor for advice. Also, be diligent about cleaning your exit site using a sterile cotton swab dipped in a special bleach solution your dialysis nurse will provide. These precautions should minimize your chances of getting peritonitis. If you do get peritonitis, you might need to spend one or more days in the hospital getting treatment. Peritonitis is treatable, but if you have recurrent episodes, you may need to have your catheter removed.
Peritoneal dialysis also causes weight gain and an increased waistline, which are mostly caused by fluid retention. It may be difficult to find clothes that fit properly, because your abdomen may become quite large. Moreover, you may feel uncomfortable with the dialysate pressing against your abdomen, especially if you have polycystic kidney disease (PKD) and large kidneys. If you have PKD, your nephrologist will help you to determine if peritoneal dialysis is a good choice for you.
If your home has limited storage space, you may have trouble storing your boxes of dialysate and paraphernalia. In addition, carrying heavy bags of solutions can be difficult, especially if you are weak from the disease and have no one to help you on a daily basis. If you are single and live alone, peritoneal dialysis may not be for you.
Peritoneal dialysis also requires dealing with a considerable amount of waste. The empty boxes, some of which do not collapse, can create a special challenge if you do not have municipal curbside trash removal. Some people must transport their trash to a local disposal site. If you have to haul your own trash, you will need to transport it more often, especially if you do not have a large vehicle. If you cannot remove your trash regularly, the amount of discarded material can become overwhelming. You may need help from your family or friends to manage the trash problem.
Peritoneal dialysis offers many advantages if you prefer to be responsible for and manage your own treatment. Although it can be very time consuming, peritoneal dialysis offers enough benefits that it may work well for you. Talk to your nephrologist and share your interests and concerns. She will be able to help you make a decision that will be best for you.
Hemodialysis has some advantages. For example, it is a good choice for people who like to spend time around other people. In addition, hemodialysis treatments provide structure and a consistent schedule to follow, with technicians at a center taking care of you. All you have to do is show up, and the nurses and technicians do the rest.
At hemodialysis centers, patients often develop a sense of camaraderie with other patients and the technicians. Because you will be spending so much time with these people, it helps if everyone is on good terms. You may even develop some close relationships at the dialysis center and they help pass the time. Some patients like talking, whereas others just prefer to sleep and be left alone. Or they watch television, read, or work on a laptop. In some dialysis centers, the social worker organizes activities and exercise programs.
The disadvantages of hemodialysis are related to the advantages. Although people may prefer having a flexible schedule for their dialysis treatments, people with full-time jobs may not be able easily to schedule treatments. The stress of commuting, especially in a large metropolitan area, just adds to the difficulty of traveling to a dialysis center. For those living in rural communities, travel distances to a dialysis center may be long. Getting to and from a dialysis center can be a problem if you do not drive. Public transportation and taxicabs are options, and many people have relatives and friends who are happy to help with transportation. But care-givers run the risk of burning out while they try to help a loved one and find their own schedules becoming overburdened. The social worker at the dialysis center can assist you with finding suitable transportation if you need it.
Medically, too, hemodialysis has a disadvantage that peritoneal dialysis does not have. As we saw previously, hemodialysis is an intermittent form of dialysis. Unlike peritoneal dialysis, which continuously dialyzes patients, hemodialysis allows waste products and imbalances in blood chemistries to accumulate between sessions. As a result, you will have to monitor your fluid, potassium, and phosphorous levels carefully. As with the peritoneal catheter, the access for hemodialysis may become infected.
Other disadvantages of hemodialysis involve the procedure itself. Because your vascular access, whether a fistula or graft, is penetrated with needles, you may experience discomfort or pain. If you need it, ask the technician to use a local anesthetic, like lidocaine.
During or after hemodialysis, you may develop cramps in your legs or feet, or you may feel lightheaded when you try to stand up. These symptoms are due to excess fluid removal during sessions, which is needed because you consumed too much fluid between sessions. The best solution is to restrict your fluid intake. Some dialysis centers will give you a salty solution to drink after a session. Although that helps at the time, you may feel thirstier and drink more fluid later. If you have difficulties restricting your fluid intake, talk to your dietician about strategies to help you. You might try avoiding having drinks close by or sucking on ice chips when you are thirsty. I found not having drinks nearby to be a particularly useful strategy in restricting fluid intake. When working and keeping my mind otherwise engaged, I successfully kept my intake to 1 liter per day.
Complications related to the access may also develop over time, including clotting, infections, and bleeding. Your nephrologist can manage most of these side effects. If a fistula or graft develops a blockage, then an interventional radiologist will be called in to remove the blockage. She will insert a catheter into a major vein in the groin, snake it into the fistula or graft, and attempt to dislodge the obstruction. If the blockage is a blood clot, the radiologist may use an enzyme called thrombin plasminogen activator (TPA) to dissolve it. Or she may insert a balloon, which can be inflated to enlarge the interior of the access site. Sometimes radiologists cannot repair the fistula or graft, and the patient will need a new access.
Fluid and dietary restrictions are more difficult to manage with hemodialysis than they are with peritoneal dialysis. This is especially true for controlling sodium, potassium, and phosphorus.
Excess salt (sodium) retention (and therefore fluid retention) is often the most difficult to manage. Salt is in almost everything we eat, and sodium levels are especially high in processed foods and restaurant foods. Thus, knowing how much sodium you are consuming becomes critical. Here is what happens if you ingest too much salt.
The body uses salt (sodium chloride) to keep a balance between the volume of blood and the volume of fluid in the tissues. The proper balance is essential for healthy hydration. Ingesting too much salt has several consequences. The sodium draws water from cells in the bloodstream and into the tissues outside of cells. This can raise the volume of blood and can contribute to hypertension. The overfilled tissues swell, causing fluid retention in the legs and feet. In addition, excess fluid in and around the lungs can cause shortness of breath. Excess salt ingestion also stimulates thirst, which can lead a person to drink too much fluid, causing fluid overload in the body. You can minimize fluid retention by strictly controlling both your salt intake and your fluid intake. For some people the nephrologist will establish a limit of 1 liter (approximately 1 quart) of fluids a day.
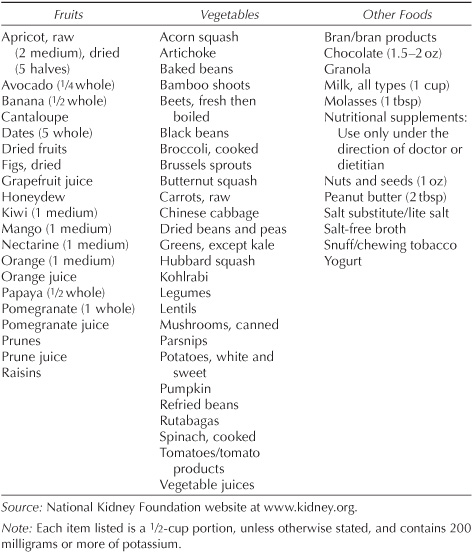
Potassium levels in the blood must be prevented from rising too high. The best way to control potassium levels is by restricting potassium in your diet. High potassium concentrations in the blood can lead to heart spasms and potentially death. Therefore, limit high-potassium foods, like orange juice, bananas, tomato paste, potatoes, and colas. See table 6.1 for a complete list of foods to avoid. Table 6.2 lists foods with low amounts of potassium.
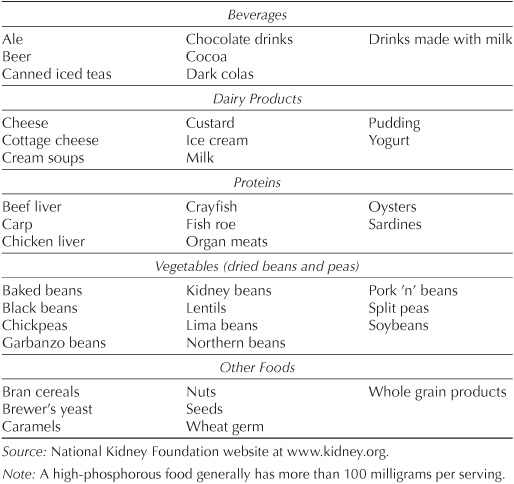
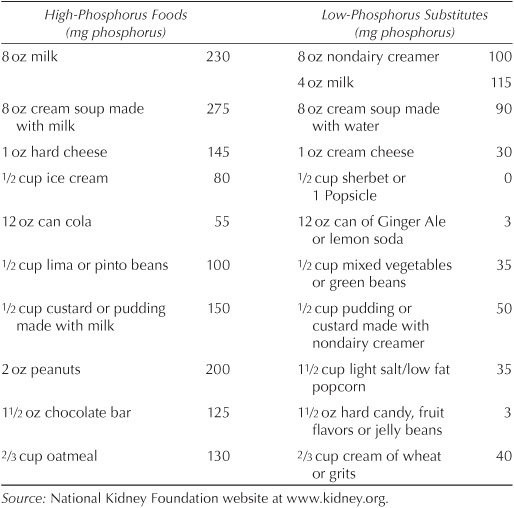
High phosphorus levels have long-term implications—unlike high sodium and potassium levels, which pose more immediate concerns. As we learned in chapter 4, high phosphorus can lead to weakened bones and to the formation of plaques in various organs. Avoid foods that are high in phosphorus (see table 6.3). Take phosphate binders if your nephrologist prescribes them. Table 6.4 suggests how to substitute food with low phosphorus levels for foods with high levels.
Read food labels to identify potentially harmful ingredients. Consider getting a nutritional guide to some of the foods you commonly eat. The American Association of Kidney Patients offers a free guide on their website, which includes sodium, potassium, phosphorus, protein, and caloric values (see www.aakp.org).
You may feel overwhelmed at first by the list of dietary dos and don’ts. A dietitian can help you avoid the wrong foods, while showing you how to continue eating some of the foods you love. Restricting your diet may be difficult at first, but when you begin to feel so much better, you will decide it is worth it. Over time, tracking food values becomes second nature.
Table 6.1
Foods with High Levels of Potassium
The healthier your diet is, the fewer complications you are likely to have. Eating right requires self-discipline and understanding from your family and friends, who must be sensitive to your dietary needs, since you may not be able to eat what they serve. At times, you may have cravings for foods that you should not eat. You may find that you can occasionally eat these foods, but do so sparingly and in small quantities. You may find that you need only the taste of these foods to feel satisfied. Stick to your basic diet (see chapter 5) and avoid forbidden foods and you will probably be okay. Be honest with your dietitian and nephrologist about what you are eating, especially if your blood chemistries are abnormal. They will be able to help you modify your diet to keep you healthy and allow you to eat some of the foods you like.
Table 6.2
Foods with Low Levels of Potassium
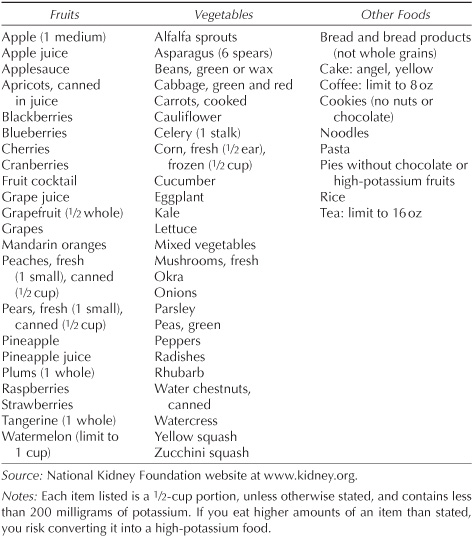
Table 6.3
Foods with High Levels of Phosphorus
People undergoing hemodialysis may experience restless legs syndrome. Estimates of the percentage of people affected range from 6 to 60 percent of people having hemodialysis. Restless legs syndrome, a neurological disease with an unknown cause, is a strong urge to move the legs that is difficult to resist. Patients describe restless legs syndrome as creepy-crawly, itching, pulling, tugging, or gnawing sensations. These sensations begin when the person is at rest, not moving, and especially when going to sleep. The symptoms of restless legs syndrome can be extremely unpleasant. You may have an uncontrollable urge to move and jerk your legs. If you resist it, the negative feelings may be overwhelming, almost painful. Moving may be the only way for the sensations to stop. Ultimately, you may get little sleep and feel exhausted during the day.
Table 6.4
Low-Phosphorus Substitutions for High-Phosphorus Foods
Treatments are available to relieve the symptoms of restless legs syndrome. To determine whether these treatments are right for you, your nephrologist will first examine your nutritional status. Deficiencies in iron and certain vitamins, like B-12 and folate, can contribute to restless legs syndrome. However, since most people on dialysis take iron and vitamin supplements, nutrition is usually not the cause of restless legs syndrome for them.
Various medications can help relieve the symptoms of restless legs syndrome. For people with chronic kidney failure, low doses of a drug like clonazepam (Klonopin), which is a benzodiazepine derivative with anticonvulsant, muscle relaxant, and anxiety-relieving properties, may provide relief. Other drugs in this same class may give you a hangover, however. Clonazepam works very well, even using the lowest dose needed to alleviate the symptoms. If you have restless legs syndrome, treatment with clonazepam may help you get a good night’s sleep and feel rested during the day.
Anticonvulsants are another class of drugs your nephrologist may prescribe. Originally developed to treat Parkinson’s disease, anticonvulsants like pramipexole (Mirapex) and ropinirole (Requip) may be helpful in treating restless legs syndrome. The downside is that anticonvulsant drugs have caused nausea, lightheadedness, and, in rare cases, hallucinations in some people taking these medications to treat Parkinson’s disease. Since treating restless legs syndrome requires lower doses of these drugs than for Parkinson’s disease, the side effects may not be as severe.
If you have restless legs syndrome, talk to your nephrologist. You do not have to suffer from this disorder.

No one likes dialysis, and it is neither risk free nor complication free. However, it is possible to make dialysis tolerable and to limit how much it interferes with your activities. Talk about your options with your nephrologist, and understand your own temperament and lifestyle. If you cannot obtain a transplant from a living donor before going on dialysis, the waiting time for kidney transplants can be long. Help yourself during this time by complying with your treatment, following your prescribed diet, restricting your fluid intake, and taking your medications. Taking care of yourself will make dialysis tolerable and will keep you in the best health possible.
A successful kidney transplant may be your best chance at living a long and healthy life. That’s the topic of the following chapter.