9 The Role of Technology in Dementia Care
Learning objectives
By the end of this chapter, the reader will be able to:
- Explore current debates about the ethics of technology in dementia care.
- Examine the use of technology in dementia care.
- Consider how technology may be used to promote relationship-based approaches to care.
- Develop a user involvement plan to engage the person with dementia and their families in the use of technology.
Introduction
Technology is ubiquitous in the twenty-first century with young adults who cannot remember life before the internet. Indeed, telling my students that I remember a time before Google places me in the same sphere as the older people I nursed in the 1980s as a young adult, who would tell me about their experiences in the first ever aeroplane and driving the very first car. As an even younger person, I remember my grandmother telling me about her life as a housewife before the labour saving technologies of refrigeration and washing machines. Technology or the concept of technology is not new; the scale, the speed and sophistication of technology, however, is markedly different in this century compared to the last. Marc Prensky (2001) speaks about ‘Digital natives’ as compared to ‘Digital immigrants’. Those children born into the digital age (Digital natives) interact with the world and learn in a very different way from those of us described as ‘Digital immigrants’ who tend to learn in a step-by-step fashion (Prensky, 2001). This doesn’t mean ‘Digital immigrants’ do not embrace technology but they will use technology differently (Prensky, 2001). This is a critical point in understanding how technology may be embraced and accepted (or not) by older people with dementia.
Once a technology is developed, is intuitive to use and makes our lives easier, it soon becomes an integral part of our lives – such as the mobile phone. Wearable technology is now becoming the norm as many people use tracking devices, for example to monitor exercise and activity. Digitalisation and miniaturisation are also opening up whole new fields of development. ‘Smart’ technologies such as Artificial Intelligence (AI) are becoming increasingly commonplace where a machine is able to create new knowledge and so ‘learn’ by processing a series of algorithms much more quickly than a human brain. AI as an example has real potential for saving time in healthcare processes such as Emergency Triage. The rapid development of technology is creating new frontiers with which to support people with dementia. However, with development also comes potential dilemma particularly if we are considering how to implement relationship-based approaches to care.
Technologies are developed regularly but not all technologies will be adopted by those for whom they have been developed. Indeed those developing the technology may not fully understand the work processes, the environment, or the needs of the end user. When considering the development of technology in dementia care, involving the person with dementia, the family member and staff is vital to ensure the end product meets the needs of everyone who will be using the technology. There are a number of often overlapping reasons why technology is used in dementia care and in this chapter we will explore the overriding concern of safety and surveillance and whether this can equal independence for the person with dementia. The rights of people with dementia to take risks within their capabilities will also be explored in relation to the available technology.
Activity 9.1 Reflection
Who is technology serving?
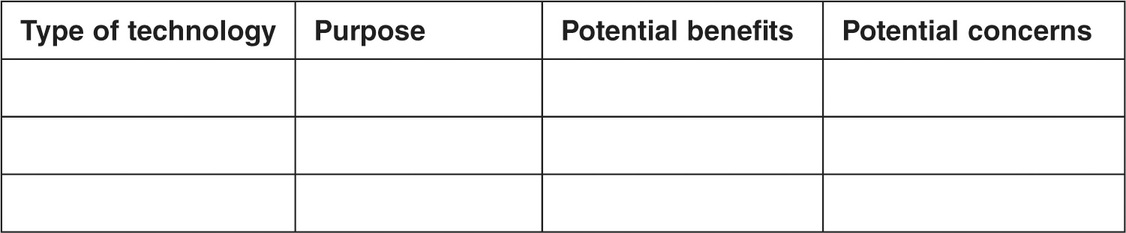
Identify the technology currently in use in the organisation in which you practise and identify the benefits and concerns from each stakeholder’s perspective:

What issues are raised by using Assistive Technology in dementia care?
Technology is becoming a common feature of healthcare provision to monitor variables such as patient safety, activity patterns, sleeping characteristics, cognitive ability and changes in patient behaviour (Bharucha et al., 2009). Systems using Radio-Frequency IDentification (RFID) composed of tags, readers and servers, use radio waves to transfer data from a tag attached to people and are increasingly being used for real-time tracking of a person’s movement (Bharucha et al., 2009). RFID tags are divided into two classes: active and passive, depending on how they are powered. Active tags have an integrated or replaceable battery which continuously powers the tag and its RF communication circuitry, thus allowing communication over a longer range and the incorporation of additional functionality such as memory and sensor devices. Passive tags have no internal power supply; the reader is responsible for powering and communicating with the tag. Passive tags are limited in their functionality but are smaller in size, cheaper and have a longer life span than active tags (Want, 2006). When used in dementia care, the passive RFID tags can be worn by the person with dementia (Hanser et al., 2008), embedded in clothing (Miura et al., 2009) or incorporated into jewellery (Nomura and Yamaji, 2008) and the readers inserted into floor mats or located on the walls of the rooms and corridors of interest. Camera surveillance may also be used, for example in remote monitoring to reduce falling, panicking and wandering, particularly at night (Schikhof and Mulder, 2008; Schikhof et al., 2010). The increasing use of remote monitoring in people’s homes is now enabling access to healthcare that might not otherwise have been possible. This may include the use of everyday technologies such as televisions and phones to maintain contact with both health services and their social network.
In dementias where there is progressive neurological reduction, mobility may be one of the last functions to be lost. Continued mobility may be the vehicle by which people with dementia retain a key feature of their independence and thus their ability to make decisions that influence their wellbeing. Cognitive loss in dementia precipitates issues with recognition of familiar environments and wayfinding that are a major risk factor in residential admissions due to safety concerns, particularly when family caregivers feel unable to cope with this pattern of behaviour (van Hoof et al., 2007). The risk of a person with dementia becoming lost has given rise to the development of surveillance technologies to maintain safety and enable people with dementia to remain living in the community (Godwin, 2012; Zwijsen et al., 2012). Maintaining independence and improving quality of life for the person with dementia are suggested benefits of employing surveillance technology although few studies have been able to demonstrate such benefits (Niemeijer et al., 2010). The main concern regarding surveillance technologies in the literature is the autonomy of the person with dementia versus the duty of care that staff need to exercise to ensure safety (Niemeijer et al., 2010). This overrriding concern for safety may result in staff using sensor technology as a restraint rather than enabling the person with dementia to move freely (Godwin, 2012; Zwijsen et al., 2012). Concerns have also been raised that Assistive Technology may reduce contact between staff members and the person with dementia which promotes positive relationships, with such technology possibly impeding the implementation of person-centred care (Savenstedt et al., 2006; Niemeijer et al., 2010; Zwijsen et al., 2012). Ethical issues are not well addressed within the literature (Niemeijer et al., 2010; Zwijsen et al., 2012) and older people themselves may potentially accept AT in an effort to avoid admission to a nursing home (Zwijsen et al., 2012). However, not all technology may prevent people with dementia from being admitted to residential care (Godwin, 2012) and concerns over safety continue to be a feature in the residential environment (Van Hoof et al., 2007).
Technology for surveillance and safety
A common focus of technology in residential environments for people living with dementia is the prevention of falls and subsequent injury. The concern about the risk of falls may result in enforced restrictions on the person with dementia with subsequent accelerated loss of function, so increasing disability (van Hoof et al., 2007).
Holmes et al. (2007) evaluated an integrated RFID system that comprised a bed exit sensor positioned under each resident’s bed sheet in conjunction with bathroom and bedroom exit monitors that alerted caregivers via a silent pager when a high-risk resident exited his or her bed, bedroom or bathroom. Only one outcome (improved mood related to sleep quality) was found to be improved with no change being found in falls, behaviour or staff outcomes. This may be due to concerns staff had in trusting the technology, which resulted in them continuing to check on people rather than wait until the technology alerted them (Holmes et al., 2007). Also, staff considered a limitation of Assistive Technology was its inability to prevent falls or adverse events and that it did not always guarantee someone receiving timely assistance due to multiple alarms going off simultaneously (Zwijsen et al., 2012). Engstrom et al. (2009) interviewed staff to identify their perception of the implementation of similar technology (passage alarms, sensor activated night time illumination, and fall detectors). Staff identified how the system enabled people with dementia to make decisions about their location without staff being concerned about the person with dementia’s safety. This was echoed in a study that considered how access technology influenced the wellbeing of the person with dementia where it was suggested that access control technology promoted autonomy of movement for the person with dementia as well as providing a sense of security for staff (Margot-Cattin and Nygard, 2006). This technology involved a RFID card on the person with dementia that opened the door to their room but then locked the doors to the external environment. Staff considered that this system supported the capability of the person with dementia in their integration into the environment (Margot-Cattin and Nygard, 2006).
Part of the concerns with safety in residential environments is ensuring people with dementia remain in the care environment. Technology is commonly used to alert staff when a person begins to leave a care environment. Aud (2004) conducted a retrospective review of 62 elopement incidents using case records, where 32% of cases resulted in injury to the resident. The technology included alarms on doorways that alerted staff when the door was opened, or when residents wearing a sensor approached or exited through a door. Subsequently the study identified key areas of concern in how staff used this technology; particularly regarding the active ignoring of alarms or difficulty in hearing them (Aud, 2004). In an ethnographic study, Wigg (2010) considered the impact of locked doors compared with motion sensors which detected when a person had left the premises, alerting staff to join them and guide them back to the home. In Wigg’s (2010) study, locked doors created a sense of frustration with people with dementia trying the door or milling around looking for ways to exit the premises. This study suggested that motion detection promoted a person’s autonomy in where they chose to walk with staff being alerted if there was the risk of harm. Chen et al. (2007) used video to detect behaviour around doorways that may lead to elopement and this prompted alerts to staff. RFID tags are also used to detect elopement and their use in a day care centre in Taiwan provided the people with dementia with more freedom to move around the building without staff becoming anxious (Lin et al., 2008). These studies demonstrate the potential for AT to facilitate interaction with the physical environment by removing potential barriers to activity due to locked doors (Margot-Cattin and Nygard, 2006; Chen et al., 2007; Lin et al., 2008; Engstrom et al., 2009; Wigg, 2010) resulting in less agitation (Wigg, 2010). Enabling people with dementia to choose where they go within an environment was considered to facilitate independence (Engstrom et al., 2009; Wigg, 2010) thus providing residents with feelings of security and achievement (Margot-Cattin and Nygard, 2006). Residential care staff also described how people with dementia who were walking to different areas within the home appeared happier with this freedom (Margot-Cattin and Nygard, 2006; Engstrom et al., 2009).
Motion patterns using RFID tags (sewn into the resident’s collar) with readers (Greiner et al., 2007) demonstrated to staff that the patterns of movement of people with dementia were purposeful, rather than aimless wandering. This was achieved by creating a graphic display of residents’ movement pattern that was then sent to a computer at the nurses’ station. The study concluded that patterns of movement can be understood in respect to a person’s previous behaviours. Similarly, a longitudinal study of resident data (30 months) using a system of under flooring pressure sensors and tags in residents’ slippers (Miura et al., 2009) suggested that mobility patterns may be linked to seasonal variations or changes in condition (Fujinami et al., 2011). Whilst technology provides us with this critical information, graphic displays are meaningless unless something is done with the information provided by the technology that improves the quality of life for the person with dementia. A group of researchers in Austria used a technological system to improve the quality of life for people living in a dementia unit. Using a combination of tags, accelerometers and microphones, information was gathered on social interaction, aggressive behaviour, the quality of sleep and where residents liked to spend their day (Hanser et al., 2008; Grünerbl et al., 2011). This information was used to identify motion patterns that represented positive, negative and neutral states of the person with dementia when compared with the medical notes. Grünerbl et al. (2011) suggest that this system may enable people with dementia to live their lives comfortably in small group homes without constant staff interaction, thus improving quality of life.
Schikhof and Mulder (2008) used Value Sensitive Design and a human-centred approach to design a technological solution that would meet the needs of all stakeholders in a dementia care unit. A central focus of this study was the mapping of values for all stakeholders and an iterative process of returning to stakeholders as the technology was developed and piloted to ensure that everyone’s needs were being met in the final system. Video camera and infra-red technology were installed in resident bedrooms for use solely at night time, which was considered acceptable by both staff and family members. Following the implementation of this technology, staff and managers reported that the video camera technology provided more freedom by enabling the people with dementia to take acceptable risks (Schikhof et al., 2010).
Video cameras were also used to improve the quality of life for people with dementia in group homes in Japan by supporting staff in understanding the person with dementia (Takatsuka and Fujinami, 2005; Sugihara et al., 2008). Caregivers described improved decision-making and communication with the person with dementia, which changed the working patterns of staff, enabling the person with dementia to live more independently (Sugihara et al., 2008, Sugihara and Fujinami, 2011).
Does surveillance + safety = independence for the person with dementia?
The discussion in the previous section suggests that technology may facilitate the promotion of wellbeing for people with dementia in residential care environments by reducing barriers within the environment that impact on a person’s functioning (Schneidert et al., 2003). There is some evidence for enhanced participation of people with dementia in the social context using surveillance technologies with two studies that demonstrated an enhanced capacity for the person with dementia to make choices as to where they wish to spend their time and who they wish to interact with (Hanser et al., 2008; Grünerbl et al., 2011). There was also some evidence that enabling staff to recognise problems remotely provides the person with dementia with greater freedom in their daily living (Grünerbl et al., 2008; Sugihara and Fujinami, 2011). However, in order to promote this level of independence using AT, privacy was often infringed through the use of video technologies (Bharucha et al., 2009). Privacy and autonomy are regular concerns in the AT literature with both family caregivers and staff often resistive to using video technology (Zwijsen et al., 2011).
Activity 9.2 Critical Thinking
Identify a person with dementia from your practice:
- What type of technology is being used to enhance their care?
- What additional technology might be used to increase their independence?
- What are the potential benefits and concerns that might emerge?
Now consider:
- How would you measure the potential benefits?
- How would you monitor the potential concerns?
Technology to promote independence in the community
Technology embedded into a person’s living environment that enables the interaction between technology and healthcare professionals is becoming widely accepted as a mechanism for improving health outcomes in Chronic Disease Management (Department of Health, 2011). For example, the Whole Systems Demonstrator (WSD) project in the UK demonstrated that using a range of embedded technology via tele-health substantially reduces mortality and hospital admissions for people living with chronic conditions (Department of Health, 2011). The term often used for these systems is Ambient Assisted Living (AAL) which refers to an ecosystem of sensors, computers, wireless networks, software applications and actuator networks (WSANs) which are interconnected to exchange data, which is then sent via a gateway to provide healthcare services. AAL is an integrated system of systems (Memon et al., 2014). AAL systems should be developed with the end user having a focus on usability and dependability. In particular, technological solutions should be non-invasive, embedded into the environment and adaptive to the end user’s needs (Cavallo et al., 2015). In a review of the AAL literature, Memon et al. (2014) found that few studies fully explored the end-user experience and there was a dearth of participatory approaches to the development process. Pol et al. (2016) report that community dwelling seniors use sensor technology in their homes to feel a sense of safety and to continue living independently. The older people in this sample felt that capturing movement did not infringe their privacy and enabled the healthcare professional to provide advice on how to keep active (Pol et al., 2016).
Cavallo et al. (2015) suggest there needs to be a user-centred design approach including a multidisciplinary team involving the older person. We saw this approach earlier in the design of a system for a residential dementia unit (Schikhof and Mulder, 2008). Working with people living with dementia in the community, Roger Orpwood and colleagues at the Bath Institute of Medical Engineering use a participatory design approach that enables the person with dementia to lead the research process by identifying the issues they find challenging and for which a technological solution might be found (Orpwood et al., 2010). A participatory approach involving people living with dementia needs to be an integral feature of developing relevant and usable systems that will have meaning for people living with dementia and their caregivers. Similarly, Evans et al. (2011) evaluated a range of sensors that was designed to improve the independence and quality of life for a person with dementia. A system of automatic lighting, motion sensors and voice reminders alerted staff when there was a problem, enabling the person with dementia to live more independently. Cavallo et al. (2015) developed a system for people living with dementia that included iterative development with extensive involvement of professional and family caregivers in the design and piloting phases to ensure the system could be integrated into the life of the person with dementia as well as the services being delivered. The purpose of this project was to integrate technology in such a way as to maintain and enhance functional health, security, safety, and quality of life for people living with dementia. This was achieved using a range of wearable devices alongside smart environments that continuously monitor the person’s activities and physical status, adapting the environment and providing proactive supportive measures (Cavallo et al., 2015). Whilst the level of independence achieved is high in this project, the loss of privacy is also high. Herein lies the dilemma as to whether the infringement on privacy will lead to a loss of autonomy or the ability of the person with dementia to make their own decisions.
In a number of studies that have explored caregiver perceptions of technology, each study reports that family caregivers are more likely to suggest the infringement of the person with dementia’s privacy and autonomy when compared to issues of safety (Robinson et al., 2007; Olsson et al., 2012; Mao et al., 2015). This is because family caregivers find it immensely challenging to maintain a sense of safety and security in their daily lives when faced with the unpredictability of how dementia influences the behaviour of the person they are caring for (Robinson et al., 2007; Olsson et al., 2012). Professional caregivers tend to give more weight to autonomy over security suggesting a person-centred approach should be adopted before implementing tracking devices (Robinson et al., 2007). People with dementia refer to the value of being able to go out of doors independently but suggest they find mobile devices confusing and difficult to use (Robinson et al., 2007). The use of GPS technology remains a common debate when supporting people with dementia (Landau et al., 2010; Magnusson et al., 2014). Whilst a predominant benefit of GPS technology is the family caregivers’ peace of mind, professional caregivers’ views change according to the locus of responsibility with patient safety overshadowing autonomy when the professional caregiver has primary responsibility for the person with dementia (Landau et al., 2010). A Swedish Demonstration Project for people living with dementia across twelve municipalities reveals mixed reports between the professional and family caregivers and the person with dementia using GPS technology (Magnusson et al., 2014). Lennart Magnusson and colleagues (2014) developed an Extended Safety and Support (ESS) system using a participatory approach involving people with dementia, family caregivers and the staff supporting them. The ESS system was not considered to be an intrusion of privacy for the majority of people with dementia involved in the study. Although the amount of times the person with dementia accessed the outdoors decreased over the length of the study, possibly due to disease progression, family caregivers reported the person with dementia was able to be more independent when they did engage in outdoor activities (Magnusson et al., 2014). Professional caregivers believed the ESS system enabled the person with dementia to remain in their home for longer. However, professional caregivers also had greater concerns for privacy issues when compared to the person with dementia or their family caregiver, which may impact on whether AT is recommended or supported by professional caregivers. The discrepancy between the views of professional and family caregivers is well documented in the literature (Robinson et al., 2007). The ESS study (Magnusson et al., 2014) suggests the value of undertaking individual and person-centred assessments to ensure the views of the person with dementia as well as the family caregiver are taken into account when making decisions about the use of AT. The following activity supports you in thinking about the potential technology may have to promote relationship-based approaches to care.
Activity 9.3 Critical Thinking
Use of technology to enhance the opportunity for person-centred practice
Consider how technology might be used to facilitate the following aspects of person-centred care:
- Getting to know the person – using the information from informal care interactions to support the ongoing development of care planning.
- Attention to significant details – with attention to the biography of the person.
- Anticipating needs – with attention to the social environment.
How might the person with dementia and their family contribute to this process using technology?
Consider how technology might be used to facilitate relationship-centred care:
- How might the information from person-centred care be shared across the team and between shifts to develop shared understandings?
- How might information be shared informally and frequently using technology to enable responsive care:
- How might the contribution of the person with dementia and families to the community be facilitated using technology?
Return to Activity 9.2 – consider the types of technology in that list and compare their function to what is needed in the current list. Are there other technologies that need to be explored?
The next section of this chapter will explore how AAL environments have been developed to improve health outcomes in Assisted Living (AL) environments. AL environments enable older people to live independently within individual units providing access to shared social spaces and healthcare. In the US, the University of Missouri have created ‘Tiger Place’, an AL environment that provides state-of-the-science care alongside the opportunity for residents to be involved in cutting-edge research.
Practice Scenario 9.1
Tiger Place is an Assisted Living environment jointly managed by a private healthcare provider and the University of Missouri. The aim of Tiger Place is to promote the health and independence of older people for as long as possible. The objective is to enable older people to ‘Age in Place’. To fully provide the best research-informed practice, Tiger Place also provides a research environment where technology and care interventions can be developed and evaluated whilst ensuring the residents have access to cutting-edge care. In this context, research is undertaken in collaboration with residents and only residents who provide informed consent are involved in the research. Over the past 10 years, within Tiger Place, there has been the development and implementation of a range of sensor technology that passively and unobtrusively collects information about patterns of movement, activity and sleeping patterns through motion sensors, bed sensors and Microsoft Kinect. Video sensors only extract silhouettes or other graphical representation to maintain privacy. This information is analysed via a behaviour reasoning component that can generate alerts. Information is sent to a database through a wireless internet connection with a secure web-based interface available for viewing by residents, families and healthcare professionals. This system is used in conjunction with a system of electronic health records and Registered Nurse Care co-ordination to improve health outcomes of the residents. All residents receive a comprehensive health assessment on admission and thereafter every six months from a Registered Nurse who is available 24 hours a day/7 days per week. In addition residents have access to health promotion activities and a social worker to support life transitions.
Source: based on Rantz et al. (2005).
Residents in Tiger Place were invited to focus groups to identify their preferences for the use of AT and opted not to wear devices but accepted installed unobtrusive devices. Cameras were also considered acceptable as long as they only captured the silhouette of the person. Data are collected from an apartment and displayed in a map of activity, the density of which can be captured across a 24-hour period. In this way, the activity of a person can be compared over time with any changes being sent automatically as an alert to the Registered Nurse Care Coordinator (Rantz et al., 2005, 2013a 2015b; Popescu and Mahnot, 2012).
The sensor technology at Tiger Place has been used to detect subtle changes in older people that might not be immediately apparent (Rantz et al., 2011) alerting caregivers earlier in the trajectory of illness thus enabling them to provide timely treatment, preventing potential decline in mobility and independence (Alexander et al., 2011; Rantz et al., 2012, 2015b). A series of case studies from Tiger Place demonstrate how sensor technology can collate patterns of activity, documenting changes in behavioural patterns indicating urinary tract infections (Rantz et al., 2011) and mental health, including dementia (Galambos et al., 2013) with subsequent work in detecting risk of falls (Rantz et al., 2015a).
As changes in a person’s cognitive status may present in diverse ways, the key aspect of this system is to be able to identify a person’s usual pattern before the onset of decline (Rantz et al., 2015b). Retrospective data for residents with a diagnosis of dementia demonstrated a pattern of changing activity both within the apartment and in taking opportunities to leave their apartment (Galambos et al., 2013). Once additional care was implemented, the data can then be analysed to chart improvement in the person with dementia’s activity patterns, demonstrating the effectiveness of the treatment. Density maps provide a visual display that could act as prompts for healthcare professionals to undertake mental health assessment and implement treatment earlier in the trajectory of illness (Galambos et al., 2013).
Companion technology is another emerging field where the system adapts to the user’s needs thus creating a smart human–technology interaction (Biundo et al., 2016). Companion systems may focus on conversational interaction or provide support for activities of daily living (Bemelmans et al., 2012). Kerssens et al. (2015) developed an in-house system to deliver personalised support in the management of Neuropsychiatric symptoms (NPS) within the home environment. The ‘Companion’ is a touch screen computer based on reminiscence of a person’s life story, customised to activities and memories that provide pleasure. The purpose was for the person with dementia to use this independently and so provide meaningful activity. Caregivers and the people with dementia using this technology were overwhelmingly positive although it did not increase the person with dementia’s independence from the caregiver’s perspective (Kerssens et al., 2015).
Other types of companion technology include animal robots. Libin and Cohen-Mansfield (2004) provided a group of people living with dementia in nursing homes with either a toy plush cat or a robotic cat and found that both reduced agitation and increased pleasure when the person with dementia interacted with either cat. A well known companion robot in dementia care is the Paro seal (Wada et al., 2007, 2008). Paro is designed as a baby harp seal to avoid preconceptions that may come with other animals and is designed with a behaviour generation system. This means that the seal can respond to interactions via inbuilt sensors (sight, auditory, balance and tactile) (Wada et al., 2008). Paro was given to a day centre where people with dementia engaged regularly with the seal. Urine tests suggested the people with dementia were less stressed and the staff also reported less stress using a burnout scale (Wada et al., 2004). Although no structured tests were undertaken, Paro’s use in one institution for five years suggested residents interacted regularly with Paro, reporting it made them feel happier (Wada et al., 2009). There have been few structured studies in assessing the effectiveness of Paro, with the majority being observational studies focusing on increased social interaction between residents (Kidd et al., 2006; Wada et al., 2007). Professor Wendy Moyle undertook a pilot randomised controlled trial (RCT) in Australia in 2013, comparing the effects of Paro to a structured reading group (Moyle et al., 2013a). The group receiving Paro improved in their quality of life and pleasure scores and there is a larger trial underway (Moyle et al., 2015).
A recurrent theme throughout this chapter has been user-centred design, involving the person with dementia and their caregivers at all points in the design process, from conception through to user interface to ensure the technology meets the needs of those for whom it is intended (Schikhof and Mulder, 2008; Bharucha et al., 2009). User-centred design also enables people with dementia to have a voice in what matters to them (Magnusson et al., 2014). Returning to our lens of Complex Adaptive Systems, utilising multidisciplinary groups including the end user provides for greater cognitive diversity, resulting in novel and creative solutions ensuring the end product remains usable and feasible (Bangar et al., 2015; Cavallo et al., 2015).
Practice Scenario 9.2
Developing technology using partnerships
This project started with a watermelon and a can of Coke to demonstrate the potential for a collection of polymer optic fibres to capture the weight of objects and transfer these into images using tomographic imaging principles.
I was involved in convening a multi-professional group including people with dementia, family caregivers, care managers, researchers and health professionals to identify the potential use for this technology in dementia care. The potential for this technology to record changes in pressure distribution of foot balance, step sequence and position in real time suggested it could be developed into a ‘SMART’ carpet, which the engineers then built with input from health professionals and a person with dementia who was an engineer. Data were then collected to identify how the system communicates changes in gait pattern leading to a fall.
These findings were presented to focus groups comprised of people with dementia, family caregivers and professionals from the NHS and private care sector. The objective of these focus groups was to evaluate the utility of this system for clinical practice including the acceptability of this technology for people with dementia and family caregivers.
People with dementia, family caregivers and staff identify the relevance of technology that can alert them prior to an incident such as a fall occurring. Embedded optical fibres in a mat or underlay can be used to non-intrusively collect data over time without infringement on privacy. Clinical staff can use a sequence of images that identify changes in walking patterns to identify risk factors that may precipitate a fall. However, further development of predictive capacity would be needed for utility in the clinical environment. Involving people with dementia, family caregivers and clinical staff in the development of technology at an early stage, significantly enhances the likelihood of such developed technology meeting the needs of the end users in healthcare.
Activity 9.4
Using technology with people living with dementia
Develop a plan that enables the perspective of the person with dementia and the family caregiver to be included in the decision-making process for use of technology:
- What is the purpose of using the technology?
- What are the ethical implications of using this technology? How might these be addressed?
- What are the risks in not using the technology being considered?
- How did the person with dementia interact with technology before they were diagnosed with dementia?
- Has the technology been discussed with the person with dementia and their family caregivers?
- Will the technology enhance the person with dementia’s life? If so, how?
Conclusion
Assistive technology is becoming increasingly sophisticated as we move through the twenty-first century. Older people and those living with dementia may be digital immigrants but this does not mean they do not engage with technology. Technology has the potential to promote independence but in doing this it might also infringe the privacy and autonomy of the person with dementia. Whilst surveillance technologies can be used to collect a range of data to improve health outcomes, there remain issues around privacy and autonomy. Whilst different stakeholders will view the balance of risk differently it is vital that all perspectives are included when making the decision whether to use technology.
Final reflections
Technology is a ubiquitous feature of modern living. With advances in technology come ethical and moral debates about the inclusion of the person with dementia in being able to make decisions that affect their right to autonomy within their decision-making capacity. We have seen in this chapter the potential for technology to contribute to relationship-based approaches to care by enabling the transfer of information for responsive care decisions to be made. Equally, there is a role for technology in promoting the contribution of the person with dementia and their family caregivers by capturing the stories they share. The potential for technology to improve health outcomes is compelling for healthcare professionals, yet this must never overshadow the risks to privacy and autonomy. The Registered Nurse is in a unique position in this debate to enable the involvement of the person with dementia in the decision-making process. The following chapter will take you through how this might be achieved.
Further reading
Assistive technology for people with dementia
This website contains a range of information including a directory of services, access to research and development, as well as information on the ethical use of technology and how to obtain Assistive Technology. Available at: www.atdementia.org.uk (accessed 27/01/17).
Centre for Eldercare and Rehabilitation Technology, University of Missouri
An interdisciplinary group of faculty, staff and students who are focused on investigating, developing and evaluating technology to serve the needs of older adults and others with physical and cognitive challenges. Research results are disseminated and effective technologies are translated to commercialisation to serve those in need. New healthcare technologies, driven by actual clinical needs, are developed and evaluated in real world settings. Available at: www.eldertech.missouri.edu/ (accessed 27/01/17).
Bath Institute of Medical Engineering (BIME)
BIME is a design and development charity working alongside various partners to promote and establish the potential of using new technology in the field of dementia care. Available at: www.bath.ac.uk/health/about/partner-organisations/designability/ (accessed 27/01/17).
Paro seal
This website explains the design of Paro with access to a range of research papers. Available at: www.parorobots.com/ (accessed 27/01/17).
Companion robots
Professor Wendy Moyle from Griffith University, Australia speaks about her work with robot therapy and people with dementia. The video also demonstrates the different robots involved in the programme of research. Available at: www.youtube.com/watch?v=UklgDdcf02Q (accessed 27/01/17).