One day we hear that a high-fat diet causes cancer, and the next day a study shows that those on low-fat diets do not have
lower cancer rates. The public is so confused and fed up that they just eat anything, and the number of overweight people
continues to grow.
The China Project
Fortunately, evidence from a massive series of scientific investigations has shed some light on the confusion. The China-Cornell-Oxford
Project (also known as the China Project) is the most comprehensive study on the connection between diet and disease in medical history. The New York Times called this investigation the “Grand Prix of all epidemiological studies” and “the most comprehensive large study ever undertaken
of the relationship between diet and the risk of developing disease.”1
Spearheaded by T. Colin Campbell, Ph.D., of Cornell University, this study has made discoveries that have turned the nutritional
community upside down. To the surprise of many, the China Project has revealed many so-called nutritional facts as demonstrably
false. For example, the answer to all the nutrition quiz questions above is false.
China was an ideal testing ground for this comprehensive project because the people in one area of China ate a certain diet
and the people just a few hundred miles away may have eaten a completely different diet. Unlike in the West, where we all
eat very similarly, rural China was a “living laboratory” for studying the complex relationship between diet and disease.2
The China Project was valid because it studied populations with a full range of dietary possibilities, from a completely plant-food diet to diets that included a significant amount of animal foods. Adding small quantities of
a variable is how scientists can best detect the risk or value of a dietary practice. It’s the same principle as comparing
nonsmokers with those who smoke half a pack a day to best observe the dangers of smoking. Comparing a fifty-cigarette-per-day
habit with a sixty-cigarette-per-day habit may not reveal much more additional damage from those last ten cigarettes.
In China, people lived their entire lives in the towns they were born in and rarely migrated, so the dietary effects that
researchers looked at were present for the subjects’ entire lives. Furthermore, as a result of significant regional differences
in the way people ate, there were dramatic differences in the prevalence of disease from region to region. Cardiovascular
disease rates varied twentyfold from one place to another, and certain cancer rates varied by several hundredfold. In America,
there is little difference in the way we eat; therefore, we do not see a hundredfold difference in cancer rates between one
town and another.
Fascinating findings were made in this study. The data showed huge differences in disease rates based on the amount of plant
foods eaten and the availability of animal products. Researchers found that as the amount of animal foods increased in the
diet, even in relatively small increments, so did the emergence of the cancers that are common in the West. Most cancers occurred
in direct proportion to the quantity of animal foods consumed.
In other words, as animal-food consumption approached zero, cancer rates fell. Areas of the country with an extremely low
consumption of animal foods were virtually free of heart attacks and cancer. An analysis of the mortality data from 65 counties
and 130 villages showed a significant association with animal protein intake (even at relatively low levels) and heart attacks,
with a strong protective effect from the consumption of green vegetables.3
All animal products are low (or completely lacking) in the nutrients that protect us against cancer and heart attacks—fiber,
antioxidants, phytochemicals, folate, vitamin E, and plant proteins. They are rich in substances that scientific investigations
have shown to be associated with cancer and heart disease incidence: saturated fat, cholesterol, and arachidonic acid.4 Diets rich in animal protein are also associated with high blood levels of the hormone IGF-1, which is a known risk factor
for several types of cancer.5
The China Project showed a strong correlation between cancer and the amount of animal protein, not just animal fat, consumed.6 Consumption of lean meats and poultry still showed a strong correlation with higher cancer incidence. These findings indicate
that even low-fat animal foods such as skinless white-meat chicken are implicated in certain cancers.
Heart Health—It’s Not Just Fat and Cholesterol
There was also a relationship between animal protein and heart disease. For example, plasma apolipoprotein B is positively
associated with animal-protein intake and inversely associated (lowered) with vegetable-protein intake (e.g., legumes and greens). Apolipoprotein B levels correlate strongly with coronary
heart disease.7 Unknown to many is that animal protein has a significant effect on raising cholesterol levels as well, while plant protein
lowers it.8
Scientific studies provide evidence that animal protein’s effect on blood cholesterol may be significant. This is one of the
reasons those switching to a low-fat diet do not experience the cholesterol lowering they expect unless they also remove the
low-fat animal products as well. Surprising to most people is that yes, even low-fat dairy and skinless white-meat chicken
raise cholesterol. I see this regularly in my practice. Many individuals do not see the dramatic drop in cholesterol levels
unless they go all the way by cutting all animal protein from their diet.
Red meat is not the only problem. The consumption of chicken and fish is also linked to colon cancer. A large study examined
the eating habits of 32,000 adults for six years and then watched the incidence of cancer for these subjects over the next
six years. Those who avoided red meat but ate white meat regularly had a more than 300 percent increase over those who ate
no white meat in colon cancer incidence.9 The same study showed that eating beans, peas, or lentils at least twice a week was associated with a 50 percent lower risk
than never eating these foods.
| CHOLESTEROL CONTENT IN |
BEEF, TOP SIRLOIN |
CHICKEN BREAST, NO SKIN10 |
| 100 grams |
90 mg |
85 mg |
| 100 calories |
33 mg |
51 mg |
Chicken has about the same amount of cholesterol as beef, and the production of those potent cancer-causing compounds called
heterocyclic amines (HCAs) is even more concentrated in grilled chicken than in beef.11 Another study from New Zealand that investigated heterocyclic amines in meat, fish, and chicken found the greatest contributor
of HCAs to cancer risk was chicken.12 Likewise, studies indicate that chicken is almost as dangerous as red meat for the heart. Regarding cholesterol, there is no advantage to eating lean white instead of lean red
meat.13
The best bet for overall health is to significantly limit or eliminate all types of meat—red and white. Dr. Campbell further
explains his view that animal protein (in addition to animal fats) is implicated in disease causation:
I really believe that dietary protein—both the kind and the amount—is more significant, as far as cholesterol levels are concerned,
than is saturated fat. Certainly it is more significant than dietary cholesterol. We do know that animal protein has a quick
and major impact on enzymes involved in the metabolism of cholesterol. Whether it is the immune system, various enzyme systems,
the uptake of carcinogens into the cells, or hormonal activities, animal protein generally only causes mischief.14
It may be impossible to extricate which component of animal food causes the most mischief. However, it is clear that while
Americans struggle in vain to even marginally reduce the amount of fat in their diet, they still consume high levels of animal
products and very little unrefined produce.
Remember, those countries and areas of China with extremely low rates of Western diseases did not achieve them merely because
their diets were low in fat. It was because their diets were rich in unrefined plant products—they were not eating fat-free
cheesecake and potato chips.
Never forget that coronary artery disease and its end result—heart attacks, the number one killer of all American men and
women—are almost 100 percent avoidable. Poring over nation-by-nation mortality data collected by the World Health Organization,
I found that most of the poorer countries, which invariably consume small amounts of animal products, have less than 5 percent
of the adult population dying of heart attacks.15 The China Project confirmed that there were virtually no heart attacks in populations that consume a lifelong near-vegetarian
diet and almost no heart attacks in populations consuming a diet that is rich in natural plant foods and receives less than
10 percent of its calories from animal foods.
My observation of the worldwide data is supported by studies of American vegetarians and nonvegetarians.16 These studies show that the major risk factors associated with heart disease—smoking, physical inactivity, eating processed
food, and animal-product consumption—are avoidable. Every heart attack death is even more of a tragedy because it likely could
have been prevented.
Understanding the Conflicting and Confusing Cancer Studies
The China Project data also helps explain findings from the Nurses’ Health Study in Boston, which showed that American women
who reduced their fat intake surprisingly did not have a decreased risk of breast cancer.17 First of all, those on the lower-fat diet consumed 29 percent of their calories from fat. This is still a high-fat diet (by
my standards) and even higher than the group with the highest fat intake in China. It’s like cutting back on smoking from
three packs a day to two and expecting to get a significant decrease in lung cancer risk. By the way, the lowest-fat group
in China, whose diet was almost entirely composed of plants, was getting 6 percent of their calories from fat, and the high-fat
group in China consumed about 24 percent of their calories from fat.
Second, these women who reported eating less fat in the Nurses’ Health Study actually consumed just as much as or more calories
from animal protein than those on the higher-fat diet, and the amount of unrefined plant produce did not increase. The low-fat group in China was not eating anywhere near the quantity of processed foods that we do in America. Their cancer rates
were so low not solely because the diet was low in fat and animal protein but also because, unlike Americans, they actually
ate lots of vegetables.
Generally speaking, the reason the evidence from the China Project is so compelling is that results from population studies
in the West are not very accurate. They generally study adults who have made some moderate dietary change later in life, and
all subjects are past the age when dietary influence has the most effect. Certain cancers, such as breast and prostate cancer,
are strongly influenced by how we eat earlier in life, especially right before and after puberty.
After studying multiple diseases, not just one type of cancer, the researchers involved in the China Project concluded: “There
appears to be no threshold of plant-food enrichment or minimization of animal product intake beyond which further disease
prevention does not occur. These findings suggest that even moderate intakes of foods of animal origin are associated with
significant increases in plasma cholesterol concentration, which are associated, in turn, with significant increases in chronic
degenerative disease mortality rates.”18 In other words, populations with very low cholesterol levels have not only low heart disease rates but low cancer rates as
well.
The insight provided by the research is simple: As long as Americans continue to practice nutritional indifference, they will
suffer the consequences. Don’t expect any significant protection from marginal changes.
Cancer Is a Fruit-and Vegetable-Deficiency Disease
Fruits and vegetables are the two foods with the best correlation with longevity in humans. Not whole wheat bread, not bran,
not even a vegetarian diet shows as powerful a correlation as a high level of fresh fruit and raw green salad consumption.19 The National Cancer Institute recently reported on 337 different studies that all showed the same basic information:20
-
Vegetables and fruits protect against all types of cancers if consumed in large enough quantities. Hundreds of scientific
studies document this. The most prevalent cancers in our country are mostly plant-food-deficiency diseases.
-
Raw vegetables have the most powerful anti-cancer properties of all foods.
-
Studies on the cancer-reducing effects of vitamin pills containing various nutrients (such as folate, vitamin C, and vitamin
E) give mixed reviews; sometimes they show a slight benefit, but most show no benefit. Occasionally studies show that taking
isolated nutrients is harmful, as was discussed in chapter three regarding beta-carotene.
-
Beans in general, not just soy, have additional anti-cancer benefits against reproductive cancers, such as breast and prostate
cancer.21
Most Americans would prefer to take a pill so they could continue eating what they are accustomed to. Can you imagine a pill
made by a pharmaceutical company that could reduce cancer rates by 80 percent or more? Wouldn’t that be the most financially
successful pharmaceutical product of all time? You would be crazy not to take this life-extending gift.
The anti-cancer and disease-protective qualities of food demonstrate the crux of the failure of modern medicine. After billions
and billions of dollars allocated and donated to cancer research, we have nothing to show for it. We are losing the war on
cancer because we are on an incessant search for the impossible-to-find cure, when in fact removing the causes is the only
way to win.
You can close this book and put it away right now as long as you can incorporate this crucial dietary change into your life:
consume high levels of fruits, green vegetables, and beans. This is the key to both weight loss and better health. Exactly
how much veggies and beans you need to eat and how to incorporate them into your diet and make them taste great are covered in chapter
eight.
A Vegetarian Diet Is No Guarantee of Good Health
People who omit meat, fowl, and dairy but fill up on bread, pasta, pretzels, bagels, rice cakes, and crackers may be on a
low-fat diet, but because their diet is also low in vitamins, minerals, phytochemicals, important essential fatty acids, and
fiber, it is conspicuously inadequate and should not be expected to protect against cancer. Additionally, because these refined
grains are low in fiber, they do not make you feel full until after you have taken in too many calories from them. In other
words, both their nutrient-to-calorie and nutrient-to-fiber ratios are extremely low.
Let me repeat this again to be clear: Following a strict vegetarian diet is not as important as eating a diet rich in fruits
and vegetables. A vegetarian whose diet is mainly refined grains, cold breakfast cereals, processed health-food-store products,
vegetarian fast foods, white rice, and pasta will be worse off than a person who eats a little chicken or eggs, for example,
but consumes a large amount of fruits, vegetables, and beans.
Studies have confirmed this. Multiple studies have shown that vegetarians live quite a bit longer than nonvegetarians do.22 But when we take a close look at the data, it appears that those who weren’t as strict had longevity statistics that were
equally impressive as long as they consumed a high volume of a variety of unrefined plant foods.
Remember, long-term vegans (strict vegetarians who consume no dairy or other foods of animal origin) almost never get heart
attacks. If you have heart disease or a strong family history of heart disease, you should consider avoiding all animal-based
products. To quote a respected authority, William Castelli, M.D., director of the famed Framingham Heart Study in Massachusetts:
We tend to scoff at vegetarians, but they’re doing much better than we are. Vegans have cholesterol levels so low, they almost
never get heart attacks. Their average blood cholesterol is about 125 and we’ve never seen anyone in the Framingham study
have a heart attack with a level below 150.
The research shows that those who avoid meat and dairy have lower rates of heart disease, cancer, high blood pressure, diabetes,
and obesity.23 The data is conclusive: vegetarians live longer in America, probably a lot longer.
How Much Longer Do Vegetarians Live?
This is a difficult question to answer accurately, as there are few studies on lifelong vegetarians in countries with electricity,
refrigeration, good sanitation, and adequate nutrition. American studies conducted in 1984 on Seventh-Day Adventists, a religious
group that provides dietary and lifestyle advice to its members, sheds some light on this issue. Adventist leadership discourages
the consumption of meat, fowl, and eggs; pork is prohibited. Because eating animal products is only discouraged and not necessarily
prohibited, there is a large range in animal-product consumption. Some Adventists never eat meat and eggs, whereas others
consume them daily. When we take a careful look at the Seventh-Day Adventist data, those who lived the longest were those
following the vegetarian diet the longest, and when we look at the subset who had followed a vegetarian diet for at least
half their life, it appears they lived about thirteen years longer than their average, nonsmoking Californian counterparts.24 Most of the participants in this study were converted to the religion, not born into it. There was no data on those following
such a diet since childhood. However, the data from this carefully constructed study was compelling; and what is of considerable
interest to me is the association of green salad consumption and longer life.25 Leafy greens, the most nutrient-rich foods on the planet, were the best predictor of extreme longevity.
Some nutritional experts would argue that a strict vegetarian who follows a diet rich in natural vegetation, not refined grains,
has the longest longevity potential, as indicated by evaluating the China Project data together with hundreds of the smaller
food-consumption studies—but, of course, this is still educated speculation. Let’s not argue whether it is all right to eat
a little bit of animal foods or not, and thereby miss the point that cannot be contradicted or disagreed with:
The Breast and Prostate Cancer Mystery Unraveled
So much has been written about the causes of breast cancer (there are entire books devoted to the subject), yet women are
still confused. This section should not be skipped over by men. Men have mothers, daughters, sisters, and wives they must
help protect, and the same factors that cause breast cancer cause prostate cancer. Men with a family history of breast cancer
have an increased risk of prostate cancer, and women with a family history of prostate cancer have an increased risk of breast
cancer.26 So there is a strong link between these two hormonally sensitive cancers.
American women are now twice as likely to develop breast cancer as they were a century ago, and most of this increase has
occurred in the past fifty years. In spite of all the fear and publicity, American women are still in the dark about what
they can do to protect themselves, and researchers looking for a simple cause have met with frustration. The reason is that
breast cancer, like most cancers, is multicausal. Considering a number of contributing factors simultaneously is essential
to understand the rapid climb in the incidence of breast cancer in recent decades. We know much today about the causes of breast cancer, and the good
news is that genetics plays a minor role and the disease does not strike at random. The war against breast cancer can be won.
Understanding the Factors Involved in the Development of Cancer
Carcinogenesis, the process that leads to cancer, is believed to occur in a series of steps. It is a multistage process that
begins with precancerous cellular damage that gradually proceeds to more malignant changes. The first step is the development
of cellular abnormalities, which eventually leads to cancer. This usually occurs during adolescence, and soon after puberty.27 Remember that unhealthy childhood nutritional practices cause excessive sex hormone production and early pathologic changes
in the breast tissue that set the stage for cancer many years later.
We know that puberty at an earlier age is a significant marker of increased risk, and we know that there is overwhelming evidence
that ovarian hormones play a crucial role, at all stages, in the development of breast cancer.28 It is common knowledge among physicians that the earlier a woman matures, as measured by the age of her first menstrual period,
the higher her risk for breast cancer.29 Both early menarche (the onset of menstruation) and greater body weight are markers of increased risk of breast cancer.30
Women are not the only sex affected; the same increased risk as a result of early maturation is seen with both prostate cancer
and testicular cancer.31 If we grow and mature more rapidly, we increase our cancer risk and age faster. We see the same thing in lab animals; if
we feed them so they grow faster, they die younger.32
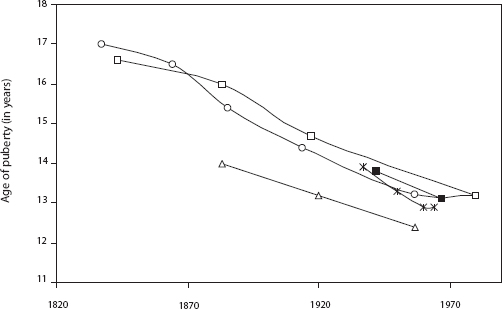
Ominously, the onset of menstruation has been occurring at a younger and younger age in Western societies during the past
century.33 The average age in the United States is now about twelve years. According to the World Health Organization, the average age
at which puberty began in 1840 was seventeen.34
During the time period that the age of menarche has decreased from seventeen to about twelve in western Europe and the United
States, there has been a concomitant change in Western eating habits. There has been an increased consumption of fat, refined
carbohydrates, cheese, and meat and a huge decrease in the consumption of complex carbohydrates such as starchy plants. Modern
studies of girls on vegetarian diets characterized by more complex carbohydrates and no meat show a later age of menarche
and, as one would expect, a significant reduction of acne as well.35 A greater consumption of animal foods leads to a higher level of hormones related to early reproductive function and growth.36 These hormonal abnormalities persist into adulthood.37 Uterine fibroids also develop from a diet deficient in fruits and vegetables and heavy in meat. As the consumption of meat
increases and vegetation decreases, one’s risk of fibroids increases proportionately.38 In other words, the stage is set by our poor dietary habits early in life. Breast and prostate cancer are strongly affected
by our dietary practices when we are young.
AGE OF PUBERTY OVER TIME
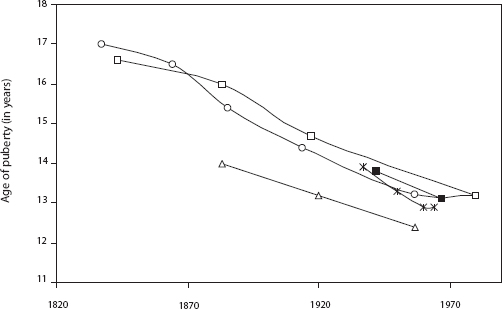
Source: Tanner, J. M. 1973. Trend toward earlier menarche in London, Oslo, Copenhagen, the Netherlands and Hungary. Nature 243: 75–76.
First European and then American studies have indicated that the protein richness of one’s diet is a more sensitive marker
of early menarche than increased body weight.39 This conclusion is consistent with the data relating earlier menarche with increased animal protein use in South African
girls.40 Then in the 1990s, when the data from the massive China-Cornell-Oxford Project was dissected, we again saw the high correlation
between breast cancer incidence and the consumption of animal products.41
In China, animal-food consumption correlated well with early menarche and increasing levels of sex hormones. Serum testosterone
levels had the best correlation with breast cancer, even better than estrogen. Of note is that increasing levels of testosterone
significantly increases the risk of both breast cancer and prostate cancer. Testosterone rises as well with increasing levels
of obesity, and being overweight is another consistent risk factor.42
What makes the data from the China Project so intriguing is that breast cancer incidence is so low in China compared with
Western countries and that animal-food consumption is so much lower than in America. Even those consuming the most animal
products in China consume less than half the amount Americans do. As animal-food intake increased from about once a week in
the lowest third to about four times a week in the highest third, breast cancer rates increased by 70 percent. Of note is
that the only difference among the diets was the addition of meat in varying amounts. Consumption of fresh vegetables in all
groups was about the same, offering little chance of confounding variables. There was a strong increase in the occurrence
of breast cancer mortality with increasing animal-product consumption.
In this country, we consume an enormous amount of cheese. Our record-high increase in cheese consumption is alarming: a 182
percent increase in the past thirty years.43 Cheese has more saturated fat and more hormone-containing and promoting substances than any other food, and the incidence
of our hormonally sensitive cancers has skyrocketed.
In spite of studies that do not show an impressive association with small differences in fat consumption later in life, large
changes early in life have huge repercussions.44 When we consider the diet consumed throughout our life, meat and dairy continue to be implicated as a strong causal factor
in breast cancer.45 There is almost no breast cancer at all in populations that consume less than 10 percent of their calories from animal products.46 After reviewing many studies on this issue for the Journal of the National Cancer Institute, a group of prominent scientists concluded that the studies that failed to show the relationship between animal-product consumption
and breast cancer suffered from methodological problems.47
Unraveling the Protein Myth
We have been indoctrinated since early childhood to believe that animal protein is a nutrient to be held in high esteem. We
have been brought up with the idea that foods are good for us if they help us grow bigger and faster. Nothing could be further
from the truth.
The public as well as the media are confused about this issue. They continue to associate the term better nutrition with earlier maturity and larger stature resulting from our greater consumption of animal protein and animal fats. These
unfavorable trends are repeatedly reported as positive events. Earlier writers and nutritionists have mistakenly equated rapid
growth with health. I believe an increased rate of growth is not a good thing. The slower a child grows, the slower he or
she is aging. Slower growth, taking longer to reach maturity, is predictive of a longer life in animal studies.48 We are finding the same thing in humans: an unnaturally rapid growth and premature puberty are risk factors for cancers and
other diseases later in life. Evidence continues to mount that these same factors leading to early maturity and excessive
growth in childhood increase the occurrence of cancer in general, not just breast and prostate cancer.49 Excluding malnutrition or serious disease, the slower we grow and mature, the longer we live.
The other side of the story is that it is not just the fat in animal foods that causes cancer and heart disease. Animal protein
is also getting a bad rap by legitimate nutritional researchers and scientists in studies. Scientists have discovered a link
between animal protein and cancer in both laboratory and human epidemiological studies, and reducing one’s consumption of
animal protein slows the aging process.50
Animal-product consumption in general is proportionally associated with multiple types of cancer. A massive international
study that amassed data from fifty-nine different countries showed that men who ate the most meat, poultry, and dairy products
were the most likely to die from prostate cancer, while those who ate the most unrefined plant foods and nuts were the least
likely to succumb to this disease.51
Another study from Germany found colon cancer and rectal cancer decreased by about 50 percent in adult vegetarians. However,
a significantly greater reduction of cancer and all-cause mortality (about a 75 percent reduction) was related to being on
a vegetarian diet for more than twenty years.52 The degree of protection correlated well with number of years on a vegetarian diet. Other studies on vegetarian diet in different
countries show almost the same thing.53 The causes start accumulating early.
There is considerable evidence that exposure to certain outlawed chemicals, especially PCBs and DDT, may promote further pathologic
changes. Women who have breast cancer have a higher concentration of these chemicals in their breast tissue than do women
who do not have cancer.54 This has also been noted in Long Island, New York, where there is a particularly high rate of breast cancer. Researchers
hypothesize that the increased exposure to these chemicals, still in our environment, is the result of eating coastal fish.
Added to all of this is the exposure to trans fats and cancer-causing compounds that are released when meat, fish, or fowl
is grilled, fried, or barbecued.55 Clearly, cancer causation is a complicated, multifactorial issue.
Exercise Powerfully Reduces Cancer Risk
Researchers at the University of Tromsø in Norway report that women who exercise regularly reduce their risk of developing
breast cancer substantially. Their study involved more than 25,000 women ages twenty to fifty-four at the time of their entry
into the study. The researchers found that younger, premenopausal women (under forty-five years old) who exercised regularly
had 62 percent less risk than sedentary women. The risk reduction was highest for lean women who exercised more than four
hours per week; these women had a 72 percent reduction in risk.
Diet and exercise have a much more important role to play in cancer prevention than mammograms and other detection methods.
Keep in mind that mammograms merely detect, not prevent, cancer; they show disease only after the cancerous cells have been
proliferating for many years.57 By that time the majority of cancers have already spread from their local site and surgically removing the tumor is not curative.
Only a minority of women who have their breast cancers detected by a mammogram have their survival increased because of the
earlier detection.58 The majority would have done just as well to find it later. I am not aiming to discourage women ages fifty to sixty-five
from having mammograms; rather, my message is that this alone is insufficient. Mammograms, which do nothing to prevent breast cancer, are heavily publicized, while women hear nothing else about what they
can do to prevent and protect themselves against breast cancer in the first place.
Do not underestimate the effect of a superior diet on gradually removing and repairing damage caused by years of self-abuse.
Do not be discouraged just because you cannot bring your risk down to zero because of your mistakes in the past. The same
thing could be said for cigarette smokers. Should they not quit smoking, merely because their risk of lung cancer can’t be
brought down to zero when they quit? Actually, lung cancer rates are considerably lower (about one-fifth) in countries that
have a high vegetable consumption, even though they may smoke like crazy.59 Raw fruits and vegetables offer powerful protection; leafy greens are the most protective.60
My main point is that our population has been ignoring those interventions that can most effectively save lives. We search
for more answers because the ones we have found are not to our liking. Our most powerful artillery on the war against breast
cancer, and cancer in general, is to follow the overall advice presented in this book and begin at as young an age as possible.
Increasing the Survival of Cancer Patients
It would be difficult for anyone to disagree that superior nutrition has a protective effect against cancer. The question
that remains is this: Can optimal nutrition or nutritional intervention be an effective therapeutic approach for patients
who already have cancer? Can the diet you eat make a difference if you have cancer? Scientific data indicates that the answer
is yes.
Researchers looking for answers to these questions studied women with cancer and found that saturated fat in the diet promoted
a more rapid spread of the cancer.61 Other researchers found similar results. For a woman who already has cancer, her risk of dying increased 40 percent for every
1,000 grams of fat consumed monthly.62 Studies also indicate that high fruit and vegetable intake improved survival, and fat on the body increases the risk of a
premature death.63
Similar findings are found in the scientific literature regarding prostate cancer and diet, indicating that diet has a powerful
effect on survival for those with prostate cancer.64 For humans, too much processed food and too many animal products are toxic.
| ANIMAL PROTEIN |
PLANT PROTEIN |
| Raises cholesterol |
Lowers cholesterol |
| Cancer promoter |
Cancer protector |
| Promotes bone loss |
Promotes bone strength |
| Promotes kidney disease |
No effect |
| Accelerates aging |
No effect |
| |
|
| Packaged with |
Packaged with |
| Saturated fat |
Fiber |
| Cholesterol |
Phytochemicals |
| Arachidonic acid |
Antioxidants |
When it is consumed in significant volume, animal protein, not only animal fat, is earning a reputation as a toxic nutrient
to humans. More books are touting the benefits of high-protein diets for weight loss and are getting much publicity. Many
Americans wish to protect their addiction to high-fat, nutrient-inadequate animal foods. These consumers form a huge market
for such topsy-turvy scientific-sounding quackery.
Today the link between animal products and many different diseases is as strongly supported in the scientific literature as
the link between cigarette smoking and lung cancer. For example, subjects who ate meat, including poultry and fish, were found
to be twice as likely to develop dementia (loss of intellectual function with aging) as their vegetarian counterparts in a
carefully designed study.65 The discrepancy was further widened when past meat consumption was taken into account. The same diet, loaded with animal products, that causes heart disease and cancer
also causes most every other disease prevalent in America, including kidney stones, renal insufficiency and renal failure,
osteoporosis, uterine fibroids, hypertension, appendicitis, diverticulosis, and thrombosis.66
Are Dairy Foods Protecting Us from Osteoporosis?
Dairy products are held in high esteem in America. Most people consider a diet without dairy unhealthy. Without dairy foods,
how could we obtain sufficient calcium for our bones? Let’s examine this accepted wisdom: is it true, or have we been brainwashed
by years and years of misinformation and advertising?
Hip fractures and osteoporosis are more frequent in populations in which dairy products are commonly consumed and calcium
intakes are commonly high. For example, American women drink thirty to thirty-two times as much cow’s milk as the New Guineans,
yet suffer forty-seven times as many broken hips. A multicountry analysis of hip-fracture incidence and dairy-product consumption
found that milk consumption has a high statistical association with higher rates of hip fractures.67
Does this suggest that drinking cow’s milk causes osteoporosis? Certainly, it brings into question the continual advertising
message from the National Dairy Council that drinking cow’s milk prevents osteoporosis. The major finding from the Nurses’
Health Study, which included 121,701 women ages thirty to fifty-five at enrollment in 1976, was that the data does not support
the hypothesis that the consumption of milk protects against hip or forearm fractures.68 In fact, those who drank three or more servings of milk a day had a slightly higher rate of fractures than women who drank
little or no milk.
This does not mean that dairy causes osteoporosis. However, it does suggest that dairy products are not protecting us from
osteoporosis as we have been indoctrinated to believe since childhood. On the contrary, studies show fruits and vegetables are protective against osteoporosis.69
Osteoporosis has a complex etiology that involves other factors such as dietary acid-alkaline balance, trace minerals, phytochemicals
in plants, exercise, exposure to sunlight, and more. Dr. Campbell, head of nutritional research for the China Project, reported,
“Ironically, osteoporosis tends to occur in countries where calcium intake is highest and most of it comes from protein-rich
dairy products. The Chinese data indicate that people need less calcium than we think and can get adequate amounts from vegetable
source plant food.” He told the New York Times that there was basically no osteoporosis in China, yet the calcium intake ranged from 241 to 943 mg per day (average, 544).
The comparable U.S. calcium intake is 841 to 1,435 mg per day (average, 1,143), mostly from dairy sources, and, of course,
osteoporosis is a major public health problem here.
To understand the causes of osteoporosis, one must comprehend the concept of negative calcium balance. Let’s say you consume
about 1,000 mg of calcium a day. About a third of the calcium ingested gets absorbed. So if you absorb about 300 mg, the remaining
700 mg remains in the digestive tract and passes out with your stool. If, in this same twenty-four-hour period, you excreted
350 mg of calcium in your urine, would you be in a negative or positive calcium balance?
| |
NEGATIVE BALANCE |
POSITIVE BALANCE |
| Ingested |
1,000 mg |
500 mg |
| Absorbed |
300 mg |
200 mg |
| Excreted |
350 mg |
100 mg |
| Retained |
− 50 mg |
+ 100 mg |
A negative calcium balance means more calcium is excreted in the urine than is absorbed through digestion. A positive calcium
balance means more calcium is absorbed than is excreted. A negative balance over time results in bone loss, as the additional
calcium must come from our primary calcium storehouse, our bones.
Epidemiologic studies have linked osteoporosis not to low calcium intake but to various nutritional factors that cause excessive
calcium loss in the urine. The continual depletion of our calcium reserves over time, from excessive calcium excretion in
the urine, is the primary cause of osteoporosis. Now, let us consider the factors that contribute to this excessive urinary
calcium excretion.
Published data clearly links increased urinary excretion of calcium with animal-protein intake but not with vegetable-protein
intake.71 Plant foods, though some may be high in protein, are not acid-forming. Animal-protein ingestion results in a heavy acid load
in the blood. This sets off a series of reactions whereby calcium is released from the bones to help neutralize the acid.
The sulfur-based amino acids in animal products contribute significantly to urinary acid production and the resulting calcium
loss.72 The Nurses’ Health Study found that women who consumed 95 grams of protein a day had a 22 percent greater risk of forearm
fracture than those who consumed less than 68 grams.73
The most comprehensive epidemiological survey involving hip fractures and food was done in 1992.74 The authors sought out every peer-reviewed geographical report ever done on hip-fracture incidence. They located thirty-four published studies
of women in sixteen countries. Their analysis showed that diets high in animal protein had the highest correlation with hip-fracture
rates, with an 81 percent correlation between eating animal protein and fractures.
The extra calcium contained in dairy foods simply cannot counteract the powerful effect of all the factors listed in the table
above. The average American diet is not only high in protein but high in salt, sugar, and caffeine and low in fruits and vegetables.
Fruits and vegetables can help buffer the acid load from all the animal protein and reduce calcium loss.75 So we need to consume a lot more calcium to make up for the powerful combination of factors that induce calcium loss in the
urine.
| COUNTRY |
ANIMAL PROTEIN INTAKE (APPROXIMATE G/DAY) |
HIP FRACTURE RATE (PER 100,000 PEOPLE) |
| South Africa (blacks) |
10.4 |
6.8 |
| New Guinea |
16.4 |
3.1 |
| Singapore |
24.7 |
21.6 |
| Yugoslavia |
27.3 |
27.6 |
| Hong Kong |
34.6 |
45.6 |
| Israel |
42.5 |
93.2 |
| Spain |
47.6 |
42.4 |
| Netherlands |
54.3 |
87.7 |
| United Kingdom |
56.6 |
118.2 |
| Denmark |
58 |
165.3 |
| Sweden |
59.4 |
187.8 |
| Finland |
60.5 |
111.2 |
| Ireland |
61.4 |
76 |
| Norway |
66.6 |
190.4 |
| United States |
72 |
144.9 |
| New Zealand |
77.8 |
119 |
Some researchers believe it is possible to compensate for our high protein intake just by consuming more calcium.76 This might be the case if the only thing we did to excess was consume a little too much animal protein, but in the context of everything
else we do wrong in the American diet and lifestyle, it just doesn’t fly.
Drinking more milk is simply not protective. Taking extra calcium supplements may help trim the calcium loss a little and
slow the rate of bone loss, but not enough. We need to reduce the other causes, too. We even add vitamin A to milk, and many
women take vitamin A supplements, which contributes to more calcium loss.77
All these factors help explain why calcium intake does not correlate well with reduced hip-fracture rates around the globe.
The Eskimos are a perfect example. They consume a huge amount of calcium, over 2,000 mg a day, from all the soft fish bones
they eat, yet they have the highest hip-fracture rate in the world because they consume so much animal protein from fish.78
The Best Foods for Bones: Fruits and Vegetables
Green vegetables, beans, tofu, sesame seeds, and even oranges contain lots of usable calcium, without the problems associated
with dairy. Keep in mind that you retain the calcium better and just do not need as much when you don’t consume a diet heavy
in animal products and sodium, sugar, and caffeine.
Many green vegetables have calcium-absorption rates of over 50 percent, compared with about 32 percent for milk.79 Additionally, since animal protein induces calcium excretion in the urine, the calcium retention from vegetables is higher.
All green vegetables are high in calcium.
The American “chicken and pasta” diet style is significantly low in calcium, so adding dairy as a calcium source to this mineral-poor
diet makes superficial sense—it is certainly better than no calcium in the diet. However, much more than just calcium is missing.
The only reason cow’s milk is considered such an important source of calcium is that the American diet is centered on animal
foods, refined grains, and sugar, all of which are devoid of calcium. Any healthy diet containing a reasonable amount of unrefined plant foods will have sufficient calcium without milk. Fruits and vegetables strengthen bones. Researchers have
found that those who eat the most fruits and vegetables have denser bones.80 These researchers concluded that not only are fruits and vegetables rich in potassium, magnesium, calcium, and other nutrients
essential for bone health, but, because they are alkaline, not acid-producing, they do not induce urinary calcium loss. Green
vegetables in particular have a powerful effect on reducing hip fractures, for they are rich not only in calcium but in other
nutrients, such as vitamin K, which is crucial for bone health.81
Deadly Vitamin D Levels
Numerous studies have shown that most Americans are severely vitamin D–deficient, a condition that causes osteoporosis as
well as increased heart disease, cancer, and autoimmune disease.
Vitamin D helps maintain healthy levels of calcium in the blood, ensuring that calcium is always available to the body’s tissues.
It increases calcium absorption in the small intestine, decreases calcium excretion in the urine, and facilitates the release
of calcium from bones. A deficiency of vitamin D can cause increased demineralization of bone, leading to weak and soft bones.
Strong evidence indicates that three out of four Americans would benefit from vitamin D supplementation with respect to fracture
and fall prevention, and possibly other public health targets, such as cardiovascular health, diabetes, and cancer.82
The optimal range for vitamin D seems to be between 35 and 50 ng/mL.83 Almost 80 percent of Americans are below this level. Approximately 50 percent of Americans have a vitamin D level below 20
ng/mL, which is dangerously low. For the past fifteen years, I have been telling people to track their blood levels of vitamin
D and to take vitamin D supplements. These recommendations have recently been corroborated by the Food and Nutrition Board
of the Institute of Medicine and the American Academy of Pediatrics.
Medical research studies that demonstrate the effectiveness of vitamin D supplements on reducing the risk of bone fractures and cancers depend on doses significantly higher than the
standard recommended daily dose of 400 IU.84 Most people need to take more than 1,000 IU of supplemental vitamin D to achieve adequate blood levels and to get substantial
protection against osteoporosis, as well as life-threatening diseases such as cancer and heart disease. Some may need to take
even higher doses initially to reestablish optimal blood levels.
Vitamin D is found naturally in very few foods; the primary sources are the sun, fortified dairy products, mushrooms, and
supplements. I do not recommend consumption of dairy products, and sun exposure places you at unnecessary risk of skin cancer
and wrinkling and aging of your skin. Regardless of the increased risk of skin damage, adequate sunshine is simply not available
to our population of indoor workers living in northern latitudes. Taking a daily supplement is your best choice for establishing
and maintaining optimal levels of vitamin D.
Got Milk—Or Leave It?
Dairy is best kept to a minimum. There are many good reasons not to consume dairy. For example, there is a strong association
between dairy lactose and ischemic heart disease.85 There is also a clear association between high-growth-promoting foods such as dairy products and cancer. There is a clear
association between milk consumption and bladder, prostate, colorectal, and testicular cancers.86 Dairy fat is also loaded with various toxins and is the primary source of our nation’s high exposure to dioxin.87 Dioxin is a highly toxic chemical compound that even the U.S. Environmental Protection Agency admits is a prominent cause
of many types of cancer in those consuming dairy fat, such as butter and cheese.88 Cheese is also a powerful inducer of acid load, which increases calcium loss further.89 Considering that cheese and butter are the foods with the highest saturated-fat content and the major source of our dioxin
exposure, cheese is a particularly foolish choice for obtaining calcium.
Cow’s milk is “designed” to be the perfect food for the rapidly growing calf, but as mentioned above, foods that promote rapid
growth promote cancer. There is ample evidence implicating dairy consumption as a causative factor in both prostate and ovarian
cancer.90 In April 2000 the Physicians’ Health Study reported that having 2.5 servings of dairy each day boosted prostate cancer risk
by more than 30 percent.91 Another controlled study conducted in Greece has shown a strong association between dairy products and prostate cancer.92 By analyzing the data, the authors calculated that if the population of Greece were to increase its consumption of tomatoes
and decrease its consumption of dairy products, prostate cancer incidence could be reduced by 41 percent, and an even greater
reduction would be possible in America, where the dietary risk is even higher. Other studies have found that prostate cancer
risk was elevated with increased consumption of low-fat milk, suggesting that the potential threat to prostate health may
be correlated more to dairy protein than dairy fat.93
Dairy protein boosts the amount of IGF-1 in the blood. IGF-1 is found in cow’s milk and has been shown to occur in increased
levels in the blood of individuals consuming dairy products on a regular basis.94 IGF-1 is known to stimulate the growth of both normal and cancer cells. Case-control studies in diverse populations have
shown a strong and consistent association between serum IGF-1 concentrations and prostate cancer risk.95 One study showed that men who had the highest levels of IGF-1 had more than four times the risk of prostate cancer compared
with those who had the lowest levels.96
Investigating the link between lactose (milk sugar) and ovarian cancer among the 80,326 women enrolled in the Nurses’ Health
Study, Dr. Kathleen Fairfield and her associates reported that women who consumed the highest amount of lactose (one or more
servings of dairy per day) had a 44 percent greater risk for all types of invasive ovarian cancer than those who ate the lowest
amount (three or fewer servings monthly). Skim and low-fat milk were the largest contributors to lactose consumption.97 Dairy products are just not the healthiest source of calcium.
Perhaps the strongest argument against dairy products in our diet: lots of us are lactose-intolerant. Those lactose-intolerant
folks, who don’t digest dairy well, are continually barraged with information that makes them believe they will lose their
bones if they don’t consume dairy products in some way. They may be better off without it.
If you choose to consume dairy, minimize your intake to small amounts. Remember the 90 percent rule: eat 90 percent health-giving
whole-plant foods. Dairy may be a part of that 10 percent; however, it is not essential for good health and carries potential
health risks.
You do not need dairy products to get sufficient calcium if you eat a healthy diet. All unprocessed natural foods are calcium-rich;
even a whole orange (not orange juice) has about 60 mg of calcium.
CALCIUM IN 100 CALORIES OF:
| bok choy |
775 |
| turnip greens |
685 |
| collard greens |
539 |
| tofu |
287 |
| kale |
257 |
| romaine lettuce |
194 |
| milk |
189 |
| sesame seeds, unhulled |
170 |
| broccoli |
114 |
| cucumber |
107 |
| carrots |
81 |
| cauliflower |
70 |
| soybeans |
59 |
| flaxseeds |
48 |
| fish |
33 |
| eggs |
32 |
| pork chop |
4 |
| T-bone steak |
3 |
Government health authorities advise us to consume 1,500 mg of calcium daily. This is a tremendous amount of calcium. So much
is recommended because of all the factors mentioned above. Even this high level of calcium will not prevent osteoporosis,
but in a population with so many factors that cause osteoporosis, the extra calcium will make the negative balance less negative
and partially slow the rate of osteoporosis. However, the only way to prevent osteoporosis and have strong bones is to exercise
and to stop the causes of high urinary calcium excretion. Eat to Live describes a diet that protects against osteoporosis.