Chapter 7
Nicotine Seduction and Stem Cells
As the site of gas exchange for the entire body, the lungs must maximize air flow. However, when we hijack this efficient system for other purposes—such as inhaling substances that bring us pleasure—bad things can happen. We’ve been exploiting our gas-exchange system for thousands of years, but only in the last few hundred have we taken it to such an extreme, and to our own detriment. Specifically, through the widespread use of tobacco, some have learned to stimulate their brains in a unique way that has changed the entire field of pulmonary medicine.
For millennia we have used the lungs, through smoking, to transport substances. This should not be surprising, since the lungs provide one of the fastest routes to deliver drugs to our brain. There is something calming and relaxing about smoking as it is part aromatherapy and part calming medicine, and its role in our cultural history has been enormous.
Smoke has been utilized throughout history by almost every culture and religion. Egyptians, Babylonians, and Hindus all burned incense as an offering to their gods. Historical evidence of direct inhalation of smoke is also abundant, starting in ancient China with the use of cannabis, which spread to India, the Middle East, and Africa. In the fifth century BCE, the Roman historian Herodotus documented how Scythians, an ancient nomadic people of what is now southern Siberia, placed hemp seeds on hot stones, “and immediately a more agreeable vapor is emitted than from the incense burnt in Greece. The Company, extremely transported with the scent, howl aloud.”128
Just as the Scythians did several thousand years ago, our culture has taken advantage of the efficiency of the lungs to transport drugs. We have unfortunately taken the utility of smoking completely out of balance. Respiratory illnesses in this country have exploded over the past fifty years, increasing 163 percent from 1965 to 1998. The increase has continued more recently, though at a somewhat slower rate, with a 30 percent increase in the death rate from respiratory illnesses between 1980 and 2014.129 Mortality rates associated with lung disease have stabilized since 2014, but the continued burden of respiratory illnesses is undermining the narrative in this country that we are continually getting healthier and living longer than the generation before. Widespread use of tobacco is a huge part of the problem.
Lung physicians know these diseases well and see firsthand every day what they can do to people’s lives. To combat the tobacco scourge, most lung doctors take time at each office visit to counsel patients on quitting smoking. A few have focused their careers on the problem, and from them lessons are available that will help us bring this scourge under control.
Mr. Johnson was frustrated the first time I saw him in my hospital’s pulmonary clinic. At rest he was fine, but whenever he tried to do something that demanded the slightest increase in his metabolic rate, he became short of breath and had to stop. Mr. Johnson could not take in enough air to do what he wanted to do in life.
He was only in his late forties, but he told me he had already been smoking for some thirty years, often more than a pack per day. This was more than enough time to make him part of the unlucky 5 percent who develop very serious lung disease from smoking. I sent him for a breathing test, and fifteen minutes later had the answer to the question of what was causing his breathing problems—when he exhaled, he could not get the air out of his chest because his airways had lost the needed elastic tissue and had been rendered floppy from the years of smoking.
“You have COPD,” I told him. “Chronic obstructive pulmonary disease.”
“Is that like emphysema?” he asked. I replied yes, it was the same disease.
He looked at me and asked earnestly how we were going to fix this, proclaiming that he was here and ready, that I was the doctor and he trusted me. I didn’t say anything right away, trying to let some of the expectation dissipate. I then asked him if he had any other medical problems. He told me that when he was in his teens, he had had a bad case of pneumonia, but it had been cured effectively with antibiotics. I wondered if now he expected me to pull out my prescription pad and write him a script for a few tablets, much as the doctor had done for his pneumonia, curing his lungs of COPD after a few weeks of therapy. Except there were no tablets to give him, no medications beyond inhalers, which would only help him feel a little better.
I asked him if he still smoked, and he replied yes. Still a pack a day. After another pause, he continued, stating he was discouraged with his breathing and his life, and he was here to get better. I kept quiet, trying to think of the best way through this. When Mr. Johnson finished, I stayed silent for a moment more, and then started talking slowly and carefully. “You’re frustrated because your world is small right now,” I said to him, making a small box with my hands. I was pushing him emotionally to acknowledge what was going on. “You can’t do the things you want to do because of your very difficult breathing, and you’re angry at yourself, and you’re angry that your world is small.”
After a long silence he replied. “Yes, yes.” He shook his head. “I’m frustrated and angry. I can’t do what I want to do.”
We went over his breathing tests with brutal honesty. At almost fifty, he had horrible lung function. Many eighty-year-olds who have smoked for a lifetime had better lung function than he did. I prescribed an inhaler to help provide a measure of relief and to hopefully take the edge off his frustration. At the end, I told him what he already knew. “You need to quit smoking.”
“I know,” he replied, and left.
When a smoker like Mr. Johnson lights a cigarette and inhales, the smoke rushes past the vocal cords, through the trachea, into the bronchi and bronchioles, and finally into the alveoli. At that point, the smoker pauses, allowing the nicotine a moment to pass through the barrier of the lung tissue and into the capillaries, where it is then carried to the brain. The remaining smoke gets exhaled, the cloud expelled into the atmosphere.
The years of toxic inhalation does different things in different parts of the lung. One of the first effects it produces is inflammation at the level of the bronchi and bronchioles, where normal mucus-secreting cells, called goblet cells, begin producing copious amounts of mucus in reaction to the irritation. This is why many smokers carry a diagnosis of chronic bronchitis (inflammation of the bronchi) and have a hacking cough that produces yellow and green sputum.
With ongoing smoking, the next change that begins to happen is cell death. Cellular death is normal for all organs of the body, and the lungs are no different: every day, hundreds of lung cells die and are replaced. The problem with smoking is that the death of cells is accelerated, while the replacement of cells slows down. In the bronchi and bronchioles, it is believed that the unchecked death of the airway basal cells is particularly problematic. The airway basal cell is a short, squat, cuboidal cell that lies deep within the tissue of the airway. Although it is not present in overwhelming numbers, its job is critical as it functions as the stem cell for other airway cells—differentiating and then multiplying into the other workhorse cells of the airway, like the squamous cell.
As squamous cells and others die off and fail to get replenished, the airway loses its tone and gets floppy. This is not such a big problem for when we inhale, but during exhalation these floppy airways collapse, and air gets trapped in the lung along with carbon dioxide. This is why some COPD patients have a barrel-shaped chest from trapped air. Others tend to develop thin lips as they constantly try to slow down the flow of air to avoid collapse of the bronchioles and bronchi. Ventilation becomes a challenge, and carbon dioxide, and subsequently acid, begins building up in the blood.
While the damage in the airways progresses from inflammation to destruction, deeper down in the alveoli it is usually simply destruction that occurs. The cells that comprise the gas exchange units of our lungs, type I alveolar cells, begin dying off. The source of replenishment for these cells, the type II alveolar cells, also begin to die off. Vast holes develop in the lung, empty spaces of air where no gas exchange is occurring, like a sponge whose holes have tripled in size. Now, getting oxygen into the blood becomes a problem as well.
When I saw Mr. Johnson back in the office a few months after the first visit, I immediately noticed something different about him. His eyes appeared clearer, his skin more radiant, his hair softer and neater. He appeared more alert, more alive, and the stale smell about him was gone. I had seen this transformation several times before and asked him right away the question I thought I knew the answer to: “Did you quit smoking?”
He answered without hesitation: “Yes, Doc, I got rid of those cigarettes. I haven’t had a cigarette in over a month.”
We took another look at his lung function. The typical total amount of air in the chest for a man his size is a little more than four liters. With the years of smoking and the damaged airways, Mr. Johnson had over five liters in his lungs—the absence of tissue meant more air was filling his chest cavity, and with floppy airways he couldn’t inhale and exhale at the normal speed. Rather than being able to exhale all of his air in two seconds, a typical amount of time for healthy lungs, he needed eight seconds. Given that our ability to move depends on energy that comes from the flow of air through our lungs, this reduced air flow slowed Mr. Johnson’s world down by a factor of four.
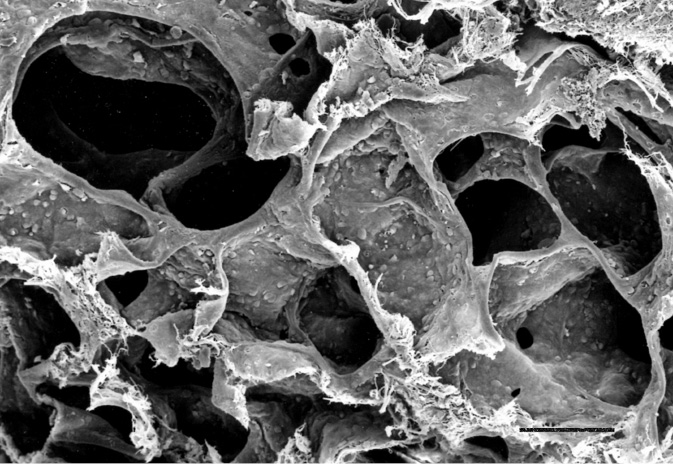
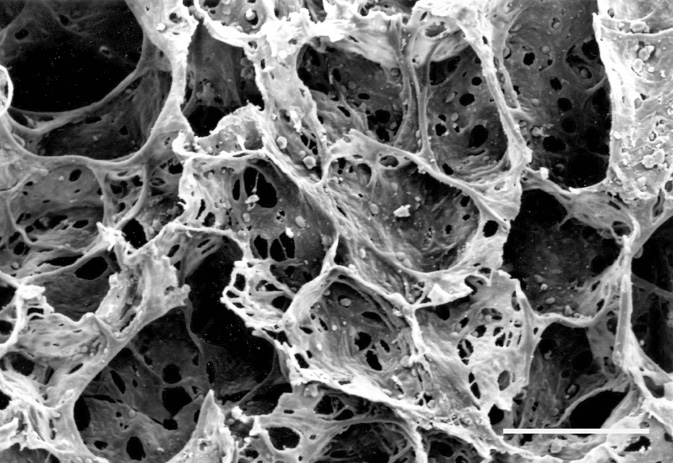
Figure 10: On top, the normal lung cut in cross section. On the bottom, the lung of a COPD patient with prominent holes.
We did what we could, and over the months and years we worked together to get the most out of what remained of his lungs. I stressed to him, as I stress to all patients with COPD, that he didn’t get sick in a day, and he would not feel better in a day. The same time and effort and money he put into cigarettes and smoking he now needed to put into getting his body back in shape. He promised me he would, and true to his word, he stayed off cigarettes, used his inhalers, and went to physical therapy to get stronger. With the additive effect of a few small things, his life improved tremendously, and even with severely diseased lungs he is getting vastly more out of life today than when I first met him.
The tobacco plant is indigenous to the Americas and wasn’t known in Europe, Africa, or Asia until explorers returned with it in the sixteenth century. Before then, Native American civilizations had used tobacco ceremoniously and as a gesture of good will at the end of bartering to seal a transaction.
One of the first descriptions of tobacco in Western literature came from the Spanish historian Bartolomé de las Casas, who in 1527 noted that the indigenous people in Cuba used “certain herbs to take their smokes, which are some dry herbs put in a certain leaf. [They] receive that smoke inside with the breath, by which they become benumbed and almost drunk, and so it is said they do not feel fatigue.” De las Casas also was aware of the addictive power of tobacco, observing: “I knew Spaniards on this island of Española who were accustomed to take it, and being reprimanded for it, by telling them it was a vice, they replied they were unable to cease using it. I do not know what relish or benefit they found in it.”130
A few decades later, tobacco as a cash crop took off with the establishment of the Virginia colony, where it was mass-produced and exported by English settlers. Sir Walter Raleigh is credited with first bringing Virginia tobacco to Europe in 1578, where its health effects were lauded. In 1595, the Englishman Anthony Chute published the pamphlet Tabaco, outlining how the plant had therapeutic potential if rubbed on the skin or inhaled, and how it relieved any sense of fatigue at the end of the day. His printer, Adam Islip, added that it “cured a gentleman that long languished of a consumption,” and also wrote somewhat ironically that tobacco “hath many strange vertues which are yet unknowne.”131
Not everybody was receptive to the tobacco plant. The British king James I, in 1607, wrote one of the first treatises against tobacco, the use of which he described as “a custome lothsome to the eye, hatefull to the Nose, harmefull to the braine, dangerous to the Lungs, and in the blacke stinking fume thereof, neerest resembling the horrible Stigian smoke of the pit that is bottomelesse.”132
Whatever the feelings of the king may have been, the economic reality was that tobacco drove the early economies of the Virginia and Carolina colonies. The English settler John Rolfe was one of the first to benefit financially from its mass production, introducing the plant Nicotiana tabacum, a native of Bermuda, into Virginia. In 1620, forty thousand pounds of tobacco were exported to England. Its use and economic importance grew, and during the first one hundred years of American colonialism, excise taxes from tobacco made up a third of the revenue collected by the British government.
Early use of tobacco centered on pipes, chewing tobacco, snuff, and cigars. In the American South, it was a ubiquitous drug, as journalist Sidney Andrews observed in 1866 during a tour of North Carolina: “The amount of tobacco consumed by the people is beyond all calculation. At least seven-tenths of all persons above the age of twelve years use it in some form. Nearly every man and boy smokes or chews, and very many of them do both, while the country women chew and smoke to some extent, and women of most classes ‘dip.’”133 But even with this level of consumption, profits stagnated after the Civil War. The tobacco industry searched for something new to boost revenue, and one person found it in the mass-produced rolled cigarette.
James Buchanan Duke, known as Buck Duke, was born in 1856 near Durham, North Carolina, and at age twenty-four was managing a factory making hand-rolled cigarettes. At the time, the rolled cigarette was a niche product, with most Americans preferring pipes, chewing tobacco, or cigars. His factory was modest, with each worker able to produce about two hundred rolled cigarettes per day. Not happy with this output, Buck Duke thought a new invention, by James Bonsack, could improve it.134
Others had also looked to increase the efficiency of producing the rolled cigarette, and in 1875 the tobacco company Allen & Ginter, of Richmond, Virginia, offered a reward of $75,000 to anyone who could invent a machine that could roll cigarettes. Eighteen-year-old college student James Bonsack decided to drop out of school and dedicate himself to winning the prize. After several years of work, by 1880 he finally had his invention, his patent, and the reward. His machine was a major upgrade from the hand-rolled factory method and was capable of producing a remarkable 120,000 cigarettes per day.
Although impressive in its promise to mass-produce cigarettes, the machine suffered from mechanical breakdowns. Also, the now-open ends of the cigarette tended to dry out, whereas the traditional hand-rolled cigarette had twirled paper at either end. All the major tobacco companies declined to invest in the new machine, but Buck Duke struck a deal to work with Bonsack to improve his device. Duke labored with his own engineers to iron out the mechanical issues, and they applied additives to the ends of the cigarette—glycerin, sugar, molasses, and a few chemicals—to prevent them from drying out.
Their efforts paid off, and Buck Duke’s machine started successfully cranking out more than one hundred thousand cigarettes per day. Since he had no market for these cigarettes, Duke created one, giving away his cigarettes at beauty pageants and other events. He took out ads in the new “glossies,” the first magazines in the United States. He put baseball cards in the packages to capitalize on the rising popularity of the sport. In 1889 alone, Duke spent the equivalent of $25 million on advertising. His new cigarette also fit the changing lifestyle of Americans: rolled cigarettes were suited to the increasing urban crowd, with no messy spit to dispose of or dirty pipe to carry around. They were very portable, had a modern look, and lit quickly, making them easier to use during coffee breaks and in restaurants.
Buck Duke’s aggressive advertising paid off. Acquiring money and market share, he bought out four of his competitors and in 1890 merged them into the American Tobacco Company. He also saw potential overseas and formed the British American Tobacco Company to expand into the European market, taking advantage of his one-size-fits-all product, easily recognized and branded as Duke Cigarettes.
Duke became extraordinarily rich and in 1924 gave away some of his money to the then-small Trinity College in Durham, North Carolina. In return for his gift of $100 million, the leaders of the college honored Duke by renaming the institution after him. Ironically, his donation amounted to $1 for each of the estimated one hundred million lives lost to cigarette smoking during the twentieth century.135
Though certainly a master businessman, advertiser, and human psychologist, Buck Duke had something else on his side that made his job easy. He had one of the most addictive drugs known to humankind, and he gave it a delivery system that transported it to the brain in seconds. The rest was just Madison Avenue spin.
At the beginning of the twentieth century, Buck Duke used all his energy to get people to start smoking. Some hundred years later, Frank Leone is trying just as hard to get people to quit smoking. And because smoking has such a deleterious effect on people’s lives—it affects lung health, heart health, and brain health, increases the risk of many lethal cancers, negatively affects mood, exacerbates depression, impairs sleep quality, and puts children’s lives at risk—Leone is actually doing much more than helping people quit smoking. Through a deep understanding of neurobiology, he is giving people back their free will, their ability to choose, and thus their entire lives.
Leone talks to smokers looking to quit with the passion of a preacher. He grew up in New York City and later attended the University of Pittsburgh and its medical school. He moved to Philadelphia in 1990 and did his residency at Thomas Jefferson University Hospital, where he saw that Philadelphia had a serious tobacco problem, with a smoking rate of 28 percent of the population, more than ten percentage points above the national average.
But what motivated Frank Leone to dedicate his life to getting people off cigarettes wasn’t the statistics. Lung doctors know the majority of diseases they see are somehow linked to cigarettes. As a young lung doctor, Leone would frequently try to get patients to stop smoking, and like most physicians, he didn’t have much luck. Nonetheless, he considered his patients’ inability to stop smoking as their problem, their weakness, their inadequacy. Eventually, however, he realized he had to own his patients’ conditions and addictions and come up with a plan for improvement, just as he did with any other pulmonary disease.
Frank Leone also recognized that in order to solve the mystery of cigarette addiction, he needed to understand the neuroscience and the psychology of tobacco addiction. He needed this knowledge because he has one of the most difficult jobs in the world. Quit rates are abysmal; if a tobacco cessation product has a quit rate of 20 percent, that’s considered a huge success.
One question Leone asks his smoking cessation classes regularly is, “Why does a bright, intelligent, motivated adult, with a million reasons to stop smoking, who has tried a million times, still find it so difficult to quit?” And he goes on to empathize: “Who hasn’t had a friend look at them and say, ‘Why don’t you just stop?’ To the smoker, this sounds like the friend is telling them to grow a third eye.”
This is the power of the cigarette, the grip of nicotine. Yet, the addictive nature of smoking is hard to explain. It is unlike that of other drugs. We are aware that when one snorts cocaine, injects heroin, takes a shot of whiskey, or smokes methamphetamine, a high comes along with it. Nicotine offers no such high, no effect of being “stoned,” no significant change in sensory input or experience. It is not euphoric or reality-altering in any respect. One doesn’t escape the world or drown one’s sorrows with cigarettes, which begs the question of where the addictiveness of this drug is coming from.
The answer is found deep in our brainstem, the ancient part of the brain that lies near the base of our skull. Within it lies the ventral tegmental area (VTA), which can be thought of as a relay station for all the danger and survival signals that come into our head.136 These signals get processed in the VTA and screened for threat level. If a barking dog with bared teeth is coming at us, that signal is sent to the VTA and gets prioritized as something important. The VTA then sends out a signal to another part of the midbrain, the nucleus accumbens, which amplifies the signal and creates motivation to do something, in this case probably to run away from the dog, and fast.
If one can get away from the dog to a safe place, the brain then needs a signal to turn off the VTA, to calm it down so it stops sending out danger signals to the nucleus accumbens. This function is performed by the neurotransmitter acetylcholine, which latches onto the VTA to cool things down. Many of the receptors in the VTA are, not surprisingly, acetylcholine receptors, and there are several different types, some called nicotinic acetylcholine receptors because nicotine can also bind there, creating an imposter safety signal.
So rather than a high, nicotine creates a sense of well-being that all is good and safe in the world. It is a powerful emotion, so powerful that it easily overrides the rational understanding that cigarettes are unhealthy. The drug nicotine is an “invisible hand,” guiding smokers to a feeling of calm and well-being. Cigarettes manipulate the mind at a deep neurobiological level, taking away not only our health, but our ability to choose. And it all starts with the lungs as the gateway.
When you light a cigarette, the paper and tobacco explode into a bright orange of combustion and heat. The temperature at the burning end of a smoldering cigarette is an astonishing 900 degrees Fahrenheit, and with a deep drag, oxygen feeds the fire, causing a burst of orange that reaches about 1,200 degrees Fahrenheit.137 The air that the smoker inhales is a toxic mixture of nanoparticles floating in nitrogen, oxygen, and carbon dioxide, mixed with the deadly gases carbon monoxide and hydrogen cyanide.
The particles in the smoke itself contain nicotine, which has been used as an insecticide, but also approximately seven thousand other ingredients. The gas of tobacco smoke also contains benzene, which is found in rubber cement; cadmium, an ingredient in battery acid; and arsenic, as in rat poison. The list of known toxins and carcinogens includes acetone, toluene, DDT, butane, and naphthalene.138 So-called natural cigarettes, without some of the additives, are thought to be no safer, as the dried tobacco leaf stands on its own as a toxic product.
This mixture of toxic gas and poisonous nanoparticles makes its way down into the deepest part of the lungs, where it quickly spreads out into the vast network of alveoli. Here, it crosses easily into the blood, flows to the heart, and within ten seconds of inhalation is attaching itself onto acetylcholine receptors in the brain’s VTA. There is no more efficient drug delivery system than cigarette smoke via the lungs. Light, inhale, wait a few seconds, and then feel the rush of calm descend.
Nicotine binds very strongly to the VTA, and once acclimated to nicotine, the brain likes to keep its levels constant. The half-life of nicotine is about two hours, so over the course of a day, smokers are in a constant battle to maintain steady levels. In the morning the brain is more desperate, after eight hours without its fix. Heavy smokers often wake up, grab a pack of cigarettes strategically placed next to the bed, and get a quick inhalation before doing anything else.
In addition to creating a short-term sense of well-being, smoking causes other, more permanent changes in the brain, including turning off certain genes. Some of these don’t turn back on for years after a smoker has quit. So when smokers try to quit, they are fighting short-term changes in receptor sensitivity and a constant need to maintain nicotine levels, as well as longer-term rewiring and genetic changes. We like to think that quitting tobacco is a one-time event, and once you quit, you’re cured. But with these long-term changes, quitting is much more like fighting a chronic disease, one that needs constant attention throughout the rest of one’s life.
Considering the neurobiology of nicotine addiction, it’s a wonder that anybody can quit smoking. But Frank Leone is convinced it can be done effectively and painlessly, and he helps people do it in a way that is the exact opposite of what most doctors tell them to try. Leone, quite purposely, does not focus on the smoking, but rather on the dependence, the reason people feel they need to use nicotine to create a constant sense of well-being.
He also knows that all smokers who come to him have a conflict within: the thinking part of their brain that wants to quit, while the instinctual part of their brain is not letting them. They have, as he describes it, extreme ambivalence, a deep conflict that is both psychological and biological.
Leone knows that he must be careful with this ambivalence. If he pulls too hard on the part that wants to quit smoking, the boomerang effect of the midbrain—the VTA—pulling back will take effect. His main weapon for fighting this ambivalence is aggressive nicotine replacement, since to him there is no such thing as toughing it out with the brain. A smoker’s brain chemistry will win every time. The system that is controlling them, the central portion of which is the ventral tegmental area, is evolutionarily millions of years old, hardwired into one’s survival circuitry. A common joke in tobacco cessation classes speaks to the challenge: “Quitting smoking’s easy. I’ve done it a hundred times.”
Of the total smokers in the United States, about 70 percent say they want to stop smoking entirely. Of those, about half tried to quit in the past year, but success rates are abysmal. For those who don’t use nicotine replacement, only about 7 percent remain tobacco free at six months, while those who use various types of nicotine replacement average quit rates of 15 to 20 percent.139 Varenicline is a newer medicine that works in the brain to mimic the effects of nicotine. With sales of $755 million per year worldwide, it is a blockbuster drug, but it, too, has low quit rates, also in the 15 to 20 percent range.
Frank Leone knows these statistics by heart. He counsels patients to use multiple options for treatment, all at once if necessary and tolerated. He feels fears of nicotine toxicity in replacement products are overblown, since many people who smoke two packs a day for decades are fine, so extra short-term nicotine is worth it in the service of quitting. The key is to trick the brain into thinking it’s still getting its fix, and then slowly wean off the need for the replacement.
The lungs have a remarkable ability to repair themselves, but after smoking goes on for years and COPD develops, much of the lung is destroyed and cannot regenerate. Stem-cell therapy holds enormous promise to fill the holes that have formed and return the lung to a healthy state. And stem cells are just part of a larger plan of organ regeneration that could one day change the field of medicine, and change how we approach injury and repair not just in the lungs but throughout the body.
One of the scientists at the forefront of lung regeneration efforts is Darrell Kotton, head of the Center for Regenerative Medicine at Boston University School of Medicine. Since completing his fellowship in 1997, he has devoted himself to the single question of how to rebuild the lung after an injury. When he began, Dr. Kotton noticed that almost all of the therapies available for lung diseases, including COPD, could at best be said to abide by the time-honored Latin phrase primum non nocere, first do no harm. With his work in regenerative medicine, Dr. Kotton wants to shift the paradigm to primum succurrere, or first hasten to help. It is a simple but profound change in expectations.
After the egg and the sperm connect, for a moment they exist as a single cell. This quickly begins to divide, and then divide again, until at about day five we have what is called a blastocyst—a tiny circular structure, less than one millimeter in size, that is made up of about two hundred cells. It has a ring of outer cells, called the trophoblast, and a mass of inner cells, aptly called the inner cell mass.
This inner cell mass is extremely important; it is made up of stem cells that are functionally pluripotent—any one of these cells has the potential to develop into any other cell in the body, whether in the lung, the brain, the heart, or the skin. They are completely undifferentiated—it is not yet determined what type of cell they will be.
In the course of development, this inner cell mass of undifferentiated cells lasts only a fleeting few hours. It quickly begins to differentiate into cell lines destined to become different organs, making stem cells in this state almost impossible to study. But a breakthrough occurred in 1981, when Dr. Gail Martin at the University of California, San Francisco, and Drs. Martin Evans and Matthew Kaufman at University College London were able to isolate and maintain the undifferentiated cells for study.140,141 This breakthrough offered the prospect of being able to reproduce what the human body knows how to do instinctively, namely to assign a pluripotent cell to differentiate into a cell of the organ of our choice.
The key to success in regenerative medicine lies in what scientists in the field call directed differentiation. Investigators must decipher the different and complex chemical signals produced within the inner cell mass that guide each cell to its final destination. This daunting task got easier in 2006, when Dr. Shinya Yamanaka of Kyoto University in Japan managed to reprogram skin cells from an adult and turn them into pluripotent cells similar to those in the blastocyst.142 This earned Dr. Yamanaka the Nobel Prize in medicine and also eliminated the ethical considerations of working with embryos, the original source of stem cells used in research. Just as important, this new process allowed scientists to work with a patient’s own cells, making it much easier to introduce them later without fear of rejection. Since 2006, various other cells have also been taken back to a pluripotent state.
Back at Boston University, Dr. Kotton has begun to guide these pluripotent cells toward final differentiation of a lung cell. In 2017 he published a paper in which he specifies the exact factors needed to take somebody’s own blood cells, engineer them back to a pluripotent state, and then bring them forward to one of the most common lung cells, the alveolar type 2 epithelial cell (the cell that secretes surfactant and is also the stem cell for the rest of the alveolar cells).143
Dr. Kotton also described the process of successfully retooling the cells from the blood of patients with a genetic disease that causes their type 2 epithelial cells to produce defective surfactant. He began by engineering pluripotent cells from the patients’ own blood cells. Then, using a cutting-edge technology called CRISPR, he genetically corrected the surfactant defect. Finally, he brought these re-engineered blood cells forward to mature type 2 cells without the genetic defect these patients had lived with their whole lives—an amazing accomplishment.
The next big step in this journey of regenerative medicine will be to devise a procedure for getting these cells back into the patient, a process called engraftment. This may be very difficult in the lung, which, over the course of its evolution, has built up immense immunological defenses. If successful, though, this procedure would complete the circle of regeneration: extracting a blood cell, bringing it to a pluripotent state, modifying its defect, moving it forward to a lung cell, and then placing it back. The range of lung and other diseases that could be improved, even cured, is vast.
Darrell Kotton cautions that efficacious lung regeneration is still many years off. Other organs, such as the eye, will likely see results much sooner than the lung, as engraftment will be more easily accomplished there. Dr. Kotton also feels strongly that his research should be available to all—he has made pluripotent cell lines engineered from different lung diseases available to any researcher in the world, and when he publishes his results, it is almost always in open-access research journals, available to all without cost. He advocates that reciprocity and exchange of ideas among researchers is the best way we can shift from primum non nocere— doing no harm—to primum succurrere—hastening to help.
The lessons we have learned from a century of widespread tobacco addiction are many, and there are numerous positive signs today, especially in this country, where smoking rates have dropped to a remarkable low of 13.7 percent in 2018.144 Considering the rate was above 40 percent in the 1960s, this is a huge step forward.
Frank Leone, however, is guarded in his optimism. In the 1950s, addiction to drugs and alcohol was thought to be primarily a question of moral character; then we decided a biological dependence was driving this behavior. In the 1970s and 1980s, addiction came to be seen as a problem involving neurotransmitters and receptors, with the solution being to block these receptors with drugs like methadone in the case of opiate addiction or nicotine replacement for tobacco.
Today, Dr. Leone does employ receptor biology, using nicotine replacement to help people quit smoking. But deep down, with his focus on why people have a dependence on tobacco, he firmly believes that tobacco addiction, and all addictions, have a component of disordered learning. He also believes there is simply too much disordered learning in our society for us to make significant inroads into our multiple addictive behaviors.
There is a lot of evidence to support Dr. Leone’s position that there is no end in sight to our addictive behaviors. One of the most obvious signs is the epidemic of electronic cigarette use, especially among teenagers. A 2019 survey published by the CDC showed that 31.2 percent of high school students (4.7 million) and 12.5 percent of middle school students (1.2 million) currently use tobacco, the vast majority using electronic cigarettes.145 Many of these teens have reported trying to quit, but many others have reported seeing no harm in intermittent use. Prevalence of tobacco use among young adults aged eighteen to twenty-four is also increasing, with the rate of 5.1 percent in 2014 increasing to 7.6 percent in 2018.146 These numbers show that the recently improved smoking rates among our youth have been wiped out.
Not unexpectedly, a crisis of the lungs has emerged because of this new and completely unregulated industry of e-cigarettes and vaping. Beginning in March 2019, the CDC received reports of a few cases of lung injury requiring hospitalization suspected to have resulted from e-cigarettes or vaping. The number of cases skyrocketed in July 2019, with cases reported from every single state, and hundreds in total. The new disease has been termed EVALI (E-cigarette or Vaping Associated Lung Injury), and 77 percent of the cases reported are in people under thirty-five. As of December 2019, forty-eight deaths have been recorded, likely an underestimate.147 The additive vitamin E may be to blame, but the only way to assure safety is total avoidance of these products.
Beyond nicotine, we are all aware of the eruption of drug overdose deaths in the United States. This crisis has been fueled by the increased potency of available opiate drugs, most notably fentanyl, but these new drugs are only part of the problem. Overall, there has been an increased use of illicit drugs in the United States, from 8.3 percent of adults in 2002 to 11.2 percent in 2017.148,149 And with the easy availability of all types of drugs today, both legal and illegal, Frank Leone is not sanguine about any end to addiction in our society. The mass legalization of cannabis for recreational use will certainly not help, as this drug, too, can teach our brain to crave inappropriate rewards, just like any other drug.
The solutions may be obvious, to focus on the personal and societal causes of our addictions, but until those issues are addressed, the opiate crisis, the tobacco crisis, and the electronic cigarette crisis will be with us in one form or another, and these addictions will continue as one of the greatest threats to the health of our lungs.
128. Robert Evans, A Brief History of Vice: How Bad Behavior Built Civilization (New York: Plume, 2016), 152.
129. Laura Dwyer-Lindgren, Amelia Bertozzi-Villa, Rebecca W. Stubbs, et al., “Trends and Patterns of Differences in Chronic Respiratory Disease Mortality Among US Counties, 1980–2014,” JAMA 318, no. 12 (September 26, 2017): 1136–1149.
130. Frederick Webb Hodge. Handbook of American Indians North of Mexico Part 2 (Washington: United States Government Printing Office, 1910), 767.
131. Anthony Chute, Tabaco (London, 1595), https://archive.org/details/tabacco00chutgoog/page/n7/mode/2up?q=consumption.
132. Iain Milne, “A counterblaste to tobacco: King James’s anti-smoking tract of 1616,” The Journal of the Royal College of Physicians of Edinburgh 41 (2011): 89.
133. Sidney Andrews, The South since the War: As Shown by Fourteen Weeks of Travel and Observation in Georgia and the Carolinas, abr. ed. (Baton Rouge, LA: Louisiana State University Press, 2004), 87.
134. William Kremer, “James Buchanan Duke: Father of the Modern Cigarette,” BBC News Magazine, November 13, 2012, https://www.bbc.com/news/magazine-20042217.
135. Rafael Laniado-Laborin, “Smoking and Chronic Obstructive Pulmonary Disease (COPD). Parallel Epidemics of the 21st Century,” International Journal of Environmental Research and Public Health 6 (2009): 209–224.
136. Mariella De Biasi and John A. Dani, “Reward, Addiction, Withdrawal to Nicotine,” Annual Review of Neuroscience 34 (2011): 105–130.
137. R. R. Baker, “Temperature Distribution Inside a Burning Cigarette, Nature 247 (1974): 405–406.
138. US Department of Health and Human Services, A Report of the Surgeon General: How Tobacco Smoke Causes Disease: What It Means to You (consumer booklet) (Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010), 30–44.
139. Stephen Babb, Ann Malarcher, Gillian Schauer, et al., “Quitting Smoking Among Adults—United States, 2000–2015,” Morbidity and Mortality Weekly Report 65 (2017): 1457–1464.
140. G. R. Martin, “Isolation of a Pluripotent Cell Line from Early Mouse Embryos Cultured in Medium Conditioned by Teratocarcinoma Stem Cells,” Proceedings of the National Academy of Sciences of the United States of America 78 (1981): 7634–7638.
141. M. J. Evans and M. H. Kaufman, “Establishment in Culture of Pluripotential Cells from Mouse Embryos, Nature 292 (1981): 154–156.
142. Kazutoshi Takahashi and Shinya Yamanaka, “Induction of Pluripotent Stem Cells from Mouse Embryonic and Adult Fibroblast Cultures by Defined Factors,” Cell 126, no. 4 (August 25, 2006): 663–676.
143. Anjali Jacob, Michael Morley, Finn Hawkins, et al., “Differentiation of Human Pluripotent Stem Cells into Functional Lung Alveolar Epithelial Cells,” Cell Stem Cell 21, no. 5 (October 5, 2017): 472–488.
144. Centers for Disease Control and Prevention, “Current Cigarette Smoking Among Adults in the United States,” CDC website, November 18, 2019, https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm.
145. Teresa W. Wang, Andrea S. Gentzke, MeLisa R. Creamer, et al., “Tobacco Product Use and Associated Factors Among Middle and High School Students—United States, 2019,” Morbidity and Mortality Weekly Report 68, no. 12 (December 6, 2019): 1–22, https://www.cdc.gov/mmwr/volumes/68/ss/ss6812a1.htm?s_cid=ss6812a1_w#T7_down.
146. Hongying Dai and Adam M. Leventhal, “Prevalence of e-Cigarette Use Among Adults in the United States, 2014-2018,” JAMA 322, no. 18 (2019): 1824–1827, https://jamanetwork.com/journals/jama/article-abstract/2751687.
147. Centers for Disease Control and Prevention, “Outbreak of Lung Injury Associated with Use of E-Cigarette, or Vaping, Products,” CDC website, Smoking and Tobacco Use, February 25, 2020, https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html#map-cases.
148. National Institutes of Health, “Nationwide Trends,” National Institute on Drug Abuse website, June 2015, https://www.drugabuse.gov/publications/drugfacts/nationwide-trends.
149. Centers for Disease Control and Prevention, “Table 20: Use of Selected Substances in the Past Month Among Person Aged 12 Years and Over, by Age, Sex, Race, and Hispanic Origin, United States, Selected Years 2002–2017,” pdf file, https://www.cdc.gov/nchs/data/hus/2018/020.pdf.