
4
Getting Uncle Sam to Play Fair with Medicare
Health care is the prime concern for most Americans in their prime of life. An illness or injury requiring medical attention can easily wipe out a life’s savings. Health insurance is an absolute must. But the cost of basic private coverage is out of reach for most older Americans. The Government’s answer is Medicare—federal health insurance available at age 65, which offers truly invaluable Golden Opportunities.
Unfortunately, your “friends” in Washington don’t play fair; they have transformed your Medicare program into a complex game and have stacked the deck against you. The rules are so confusing that even Uncle Sam doesn’t always understand them. And if that weren’t bad enough, the politicians keep reshuffling the playing cards to create “new and improved” versions of the game. Then they bury the rules you need to successfully compete.
Enough is enough. In the pages that follow we explain why the Medicare Monopoly Game was created; what the real Golden Rules are; and how you can WIN! The secrecy and mystery surrounding Medicare is about to come to an end!
THE TRUTH (ALMOST) BEHIND WHY MEDICARE DOESN’T CARE ABOUT YOU
One of the best-kept secrets of all time is the “real” reason why our Government created Medicare. In 1965, when President Lyndon B. Johnson signed the legislation for this program, Americans were told that the purpose of Medicare was to provide basic national health insurance for seniors. Phooey. That story was simply a cover-up. What you are about to read has never before been revealed to the public: the secret goal of the Medicare program. Be forewarned, the truth might shock you.
In the late 1950s, census studies showed that the American population was rapidly graying. The implications were grave. Too many seniors with too much leisure time spelled trouble. What if all these competent retirees decided to become political activists? Congress panicked. The prospect of being monitored by thousands of seniors was frightening.
A solution was needed that would keep America’s seniors so busy they wouldn’t have any energy left to pester Congress. In a flash of skin-saving genius, our legislators found the perfect answer: Congress gave America Medicare. We were told the program was designed with our best interests at heart. But Congress never intended to create a workable health-care safety net. What our legislators wanted was a time-consuming national “hobby” for seniors. Now you know the “truth.”
When President Johnson signed on the dotted line, what our citizens actually received was the rule book for the largest group activity ever created—the great Medicare Monopoly Game. (If you doubt the credibility of this theory, consider the following: Had Medicare truly been intended to provide you with health-care protection, don’t you think it would work just a little better?)
The concept behind Medicare Monopoly is brilliant. Here are some of the game’s key features:
1. Portable components—No matter where you travel in the United States, you will always be able to find playing pieces (stop in at any friendly Social Security office).
2. Socialization benefits—Swap Medicare war stories with others in any doctor’s waiting room. A common rapport is immediate.
3. All-season use—So, outside it’s too cold? Too hot? No sweat. You will never be at a loss for something to do. Interpreting and sorting denied claims is good for hours of activity.
4. Promotes family ties—If you are at a loss for ideas that will bring your relatives together, you can always invite them to Medicare Monopoly parties to develop new strategies for getting claims paid.
And you thought Medicare was a health insurance program!
WHEEL OF MISFORTUNE: LEARNING HOW TO PLAY MEDICARE MONOPOLY
Now that you know the “why” behind Medicare, you need to develop a fresh strategy for dealing with the system. You must learn how to play the game.
To win any game of chance, a player needs a combination of luck, nerve, and timing. Playing Medicare Monopoly is no different in this regard. Some aspects of the game you will have control over, like making sure information on a claim is accurate; some you won’t, like choosing the date and severity of an illness. But the key is knowledge. You would never think of going to Las Vegas, plunking down hundreds of dollars at the blackjack table, and playing, without ever bothering to learn the rules of the game. Yet when it comes to Medicare, that’s exactly what most people do. They toss the dice, shut their eyes, and hope the right numbers come up so the medical bills can get paid. People keep playing until their pockets are empty and there is nothing left to lose.
This is a tragedy, but it doesn’t have to happen to you. When you play Medicare Monopoly, don’t just keep picking the “Take a Chance” cards. There are rules of the game; if you know them, and turn them to your favor, you can improve your odds of opening the Community Chest of valuable benefits.
As you prepare to play, keep two important principles in mind:
• Medicare is not charity. You have earned your right to Medicare through the Social Security taxes that were deducted from your or your spouse’s salary. Remember when you looked at your paycheck and saw that big gap between gross and net income? Well, some of that hard-earned money should finally reappear in the form of Medicare benefits. When you play Medicare Monopoly, you’re playing to win your own funds.
• Medicare is confusing. No, you are not senile or stupid because you can’t understand all the ins and outs of the program. Medicare is a red-tape nightmare. (What did you expect when politicians, government bureaucrats, hospitals, doctors, and insurance companies all have a say in spending over $100 billion in taxpayer money!) Take heart—there is nothing wrong with your mind. To ask for help in battling the bureaucracy is not an admission of stupidity. Whether you have a high school diploma or three Ph.D.s, you will find dealing with Medicare exasperating because it often defies logic. Perseverance (not brains) is key for a successful game of Medicare Monopoly.
Preparing to Play
The official rules for playing Medicare Monopoly can be found in The Medicare Handbook, published annually by the U.S. Department of Health and Human Services. But as anyone who has used this guide knows, the instructions for playing are unclear at best. (Let’s face it, Uncle Sam wants to win the game, so he’s not anxious to reveal where the aces are hidden.) Don’t despair, this chapter will help even the odds.
The Medicare Handbook, despite its flaws, is still an essential game piece. Since the Handbook is updated every year to reflect changes in the program, make sure you have the latest edition. Medicare automatically provides the first copy when you enroll, but after that, staying current is up to you. If you have misplaced your Handbook, or if it’s outdated, get another. Call or visit your Social Security Office or local Office on Aging.
The Medicare Handbook should always be your starting point for explanations about Medicare coverage. Before wasting any time on the phone with Medicare personnel, refer to this guide. Uncle Sam just might have something to say on the subject. Scan the Table of Contents and the Medicare Ready Reference Chart at the very beginning of the guide. If you have a simple question, such as “What is the phone number to call when reporting Medicare fraud?” chances are you will find the answer.
It’s dealing with any issue beyond the realm of the most simple that can cause problems. The fine print of Medicare coverage, supposedly provided in the Handbook, can be so fine that it’s nonexistent. If you want to find out the Government’s “secret rules,” this chapter is just what the doctor ordered.
Armed with the newest Medicare Handbook in one hand and this book in the other, you will be ready to play Medicare Monopoly, set to pass go, and collect the treasure you are entitled to receive under Medicare law.
Begin at the Beginning
“Begin at the beginning … and go on till you come to the end” is the wise advice the King of Hearts offers Alice during her journey through Wonderland. Since we are not ones to tamper with sound suggestions, that’s exactly where we will begin our discussion of the Medicare Monopoly Game: at the beginning.
When we talk about Medicare, we’re referring to the federal health insurance program for people 65 or older and certain disabled people. It is run by the Health Care Financing Administration of the U.S. Department of Health and Human Services. Your local Social Security Administration office has the job of taking applications and answering questions about eligibility and basic benefits of the program. (Medicare carriers and intermediaries are responsible for handling your specific questions about claims.)
Health Insurance Card
Uncle Sam will give you a card identifying you as an official Medicare Monopoly player. Everyone calls this card the “Medicare Card.” It makes sense. The name is clear and simple. Even The Medicare Handbook refers to this document as the “Medicare Card.” Nevertheless, Uncle Sam actually has chosen another name as the official title: the “Health Insurance Card.” So don’t be surprised when the card you receive has “Health Insurance,” not “Medicare,” written in bold letters.
Your Medicare card is as unique as your fingerprint. You are assigned a health insurance claim number (Medicare number) that has nine digits (your Social Security number) and one letter (sometimes two letters), and it belongs to you alone. The only way the bureaucracy recognizes your existence as legitimate is by the identification information on the card. For this reason, always:
• Carry your Medicare card with you.
• Write your health insurance claim number on any documents or forms you send to Medicare.
• Replace a lost card immediately (call Social Security).
• Use your own card. Never use anyone else’s claim number, even your spouse’s. You are asking for a paperwork nightmare if you do.
The Medicare program has two parts: Hospital Insurance (Part A) and Medical Insurance (Part B). The highlights of both are summarized in Table 4.1. Table 4.2 shows the costs of health care services that will be shared between you and Medicare.
Medicare hospital (Part A) and medical (Part B) insurance are wonderful benefits—the rich rewards for winning Medicare Monopoly. But as we’ve said, Uncle Sam doesn’t want to make it too easy for you. So he’s written the rule book in Medicarese.
Medicarese
Medicarese is the mode of communication used by the folks at Medicare. It looks like English, but it’s not. The unique feature of this language is that it was created for the sole purpose of promoting secrecy and misunderstanding. (You’ve heard of legalese—well this is worse!)
Obviously, you can’t play a winning game of anything when the rules are not written in plain English. You’ve got to learn at least the basics of Medicarese vocabulary. The Government’s Medicare Handbook provides a Glossary of Medicare Related Terms (written, of course, in Medicarese). You will find it buried at the back of the Handbook. We have taken the liberty of translating the key Medicarese terms from this list into people-friendly language. Mr. Webster might not approve of our style, but he probably never had to read a Medicare document, either!
Defined here are certain words and phrases central to understanding both Parts A and B of the Medicare program. These VIPs (Very Important Phrases) deserve VIP attention because you can’t play Medicare Monopoly without them.
Medicare VIP Glossary
Approved Charge. This is the dollar amount that Medicare has decided is an appropriate fee for a provider’s service. Medicare uses a complex formula to arrive at this figure. The approved charge is like a price ceiling. Medicare generally won’t pay more than 80 percent of its approved charge for a service, no matter what the provider bills you. Don’t be confused—just because Medicare “approves a charge” does not mean Uncle Sam will pay 100 percent of the bill.
TABLE 4.1
Basics of the Medicare Program
Hospital Insurance—Part A
What Is Covered?
As you will see, Medicare’s use of the term “covered” is a gross overstatement. There are lots of limitations, but here is the basic list:
1. Inpatient hospital care
2. Inpatient Skilled Nursing Facility (SNF) Care
3. Home health care
4. Hospice care
Who Is Eligible?
At 65, you are entitled to receive Part A benefits based on your (or your spouse’s) employment record. Most people are covered.
What Are the Costs?
Part A is “free” (no premiums are required), but you must pay all deductibles ($652 in 1992) and co-insurance (a percentage of the bill for the care or service received—no small potatoes).
Medical Insurance—Part B
What Is Covered?
The following kinds of care and services fall under the Medicare Part B umbrella of coverage:
1. Doctor care
2. Outpatient hospital care
3. Diagnostic testing
4. Durable Medical Equipment (DME)
5. Ambulance travel
6. Various other services and supplies not included under Part A
See the Medicare Handbook under Medicare Medical Insurance (Part B) for an official summary.
At first glance, the range of care and services covered looks impressive. Don’t be fooled. When your first rainy day arrives, you will discover many leaks in your Part B umbrella of coverage.
Who Is Eligible?
Basically, anyone (65 or older) who wants to pay.
What Are the Costs?
You pay a monthly premium, plus deductibles and co-insurance. In 1992, the Part B premium is $31.80 a month and the annual deductible is $100.
TABLE 4.2
Health Care Payments Under Medicare

Assignment. This is perhaps the most misunderstood term in the Medicare VIP Glossary; it applies to Part B medical insurance. Understanding assignment is essential for playing the Medicare Monopoly game.
Assignment is a three-way agreement among you, Medicare, and a service provider (e.g., a doctor) to share the costs of your medical treatment. Here’s how the deal works:
• The provider agrees to accept the Medicare approved charge as total payment for a service.
• Medicare then pays its share (usually 80%) of that approved amount (less any unmet deductible) directly to the provider.
• To complete the triangle, you must pay your share (20% co-insurance for most services) of the approved charge to the provider (plus any unmet deductible).

A provider who accepts assignment accepts as payment in full the amount Medicare has approved as a reasonable charge for this service, even if his normal fee would be higher. The provider is not agreeing to accept Medicare’s check for 80 percent of the bill as payment in full. When a doctor accepts assignment you still must pay your 20 percent co-insurance; you don’t get off the hook. Unfortunately, a sign in a doctor’s office that reads “I accept assignment” is not a ticket to free medical care!
Benefit Period. This is Medicare’s way of measuring your use of Part A covered services. It is the period of time during a spell of illness when the care you receive is eligible for Medicare reimbursement. Maximum benefit periods are listed in Table 4.2; a spell of illness is defined below.
Co-insurance (or Co-payment). This is the amount you must pay after Medicare pays its share of the bill for Medicare approved services and supplies. Both Parts A and B can require you to pay co-insurance.
Under Part A, you get 60 days in a hospital or 20 days in a skilled nursing home absolutely free (after paying your deductible). Once you have exceeded the free day limit, you and Medicare will share the costs. Your portion is called co-insurance.
Under Part B, if the provider accepts assignment, Medicare pays 80 percent of the cost and you (or your private supplemental insurance) pay 20 percent (your co-insurance). Remember, assignment means you will not have to pay more than the Medicare approved charge for a service; it does not mean Medicare picks up the entire bill.
When a provider does not accept assignment, expect to pay more. Since the provider is not agreeing to use Medicare’s price lid on his fee, you will owe the 20 percent co-insurance (based on Medicare’s approved charge) plus all of the “unreasonable” charges for a service (any amount the doctor bills above Medicare’s approved charge) up to 120 percent of the Medicare approved amount. (Some states limit fees charged by providers even more.)
Deductible. This is a fee you must pay before Medicare will begin to pay for any of your hospital or medical expenses. In 1992, the Part A deductible (for each benefit period) is $652 and the Part B annual deductible is the first $100 in approved charges (see Table 4.2) and can be met by any Medicare-covered expenses over the course of a year. You must meet your Part A deductible each time you are admitted to the hospital or skilled nursing facility (SNF) if more than 60 days has passed since your last hospital or SNF stay. Medicare will keep a running tally and will deny payment until you hit the mark. It’s a good idea for you to keep track of your expenses too, so you can make sure you aren’t wrongfully denied benefits once the deductible is satisfied.
Reasonable and medically necessary. Medicare pays for “covered” services, but only if the services are also “reasonable and medically necessary.” Unfortunately, this vague language allows the Government to unfairly deny all sorts of claims.
It’s probably safe to say that no one really knows for sure what this term means, and Medicare likes it that way. What appears perfectly “reasonable” to you or us may not look that way to the Medicare claim processor who just happened to wake up on the wrong side of the bed the day your claim passed through. However, here’s a “reasonable” way of applying this slippery standard: Had a panel of doctors been convened to review your case, would the majority agree that your doctor’s plan for care:
• Was based on sound medical practice?
• Was a safe and effective choice of treatment?
• Gave consideration to your entire physical and mental condition?
If so, the service in question should be considered “reasonable and medically necessary.”
GEM: When You Choose, You Lose
In the vague world of “reasonable and necessary,” there is a very important, clear-cut no-no. When you exercise your freedom of choice and opt for nonessential care, Uncle Sam will exercise his veto power.
GEM: Be an Exception to the Rule
Your claim may be unfairly denied because the treatment you received is usually considered unreasonable and unnecessary. But the circumstances of your case might make you “exceptional” and, by law, Medicare must evaluate your claim based on the unique aspects of your total condition. If your claim is denied and you believe it’s unfair because Medicare didn’t notice that you were special, ask for a review. Have your doctor write and explain why the service was reasonable and necessary, and refile the claim. There’s a good chance Medicare will see it your way this time. (For details on how to file an appeal, see Chapter 5.)
EXAMPLE 1
Your doctor tells you that a cyst must be removed. He says he can fix you up in the office. But you’d feel better if the treatment is done in a hospital, so you ask to have it done there.
Get out your checkbook. If necessary treatment can be done on an outpatient basis but you opt to check into the hospital, you’ll have to pay yourself.
EXAMPLE 2
You might think a face-lift is essential to your well-being, but don’t expect Uncle Sam to agree. You will pay the price for beauty, as well as for any other procedure that is not essential for preserving your health.
* * *
Spell of Illness. You may receive Medicare benefits only during a spell of illness. A spell of illness begins when a patient is admitted to a hospital or skilled nursing facility and ends when the patient has not received hospital or skilled care for 60 consecutive days.
The Medicare Timer
When you play Medicare Monopoly, you’ll play Part A against a Medicare timer. Uncle Sam sets the timer when you go into the hospital or skilled nursing facility, and when your timer runs out—buzzzz, you lose. You can start the timer again for each new spell of illness.
The Medicare timer starts running when you start a benefit period, which is the time during which you can get Medicare Part A coverage. For example, for each Medicare hospital insurance benefit period, after meeting your deductible, you are eligible for 60 “free days” of coverage (you actually pay the deductible on the first day and then you pay no co-insurance for the next 59 days) plus 30 “shared” cost days (you must pay co-insurance—see Table 4.2 for amounts). These 90 days (free and shared) are “renewable”; when you begin a new spell of illness, the timer is reset for 90 days. You also have 60 “reserve days” you can draw on over your life, but these are not renewable. You still must pay co-insurance for each day, and once lifetime reserve days are used up, they are gone forever. Example 3 shows how this works:
EXAMPLE 3
Your husband first enters a hospital on April 15. He is there three days, and pays his deductible. When he reenters on May 1, all costs are paid by Medicare right from the start. The Medicare timer began running from the day he paid his deductible.
After 60 days in the hospital (combining both visits), you start sharing the costs. The sharing continues for 30 days. Then the timer runs out. Now you have a choice: you start using your 60 reserve days or you pay out of your own pocket.
EXAMPLE 4
Same facts as Example 3, except your husband’s prior hospitalization was February 15 to 18. When he reenters on May 1, he must pay his deductible ($652) again, even though he paid the deductible once already this year, because he is in a new spell of illness—he has been out of the hospital for more than 60 consecutive days. But the good news is he gets a new benefit period—60 new free days and 30 new shared-cost days.
How Does Medicare Calculate a Benefit Period?
The Medicare payment timer starts ticking on the first day you enter a hospital. Each free day is like one second on a stopwatch, and when the hands on the Medicare stopwatch reach 60, your full coverage days are over. You must begin paying co-insurance for the next 30 days of care.
How Do You Get a New Benefit Period?
Again, the stopwatch analogy applies. You can begin a new benefit period with each new spell of illness, after you have been out of the hospital (or SNF) for 60 days in a row. The day of discharge will count as your first day out.
There is no limit to the total number of benefit periods you can have, either in a year or in your life. If you are out of the hospital for 60 consecutive days, the timer goes back to zero and you are given a new benefit period (60 free days followed by 30 shared cost days). At the start of each new benefit period, you pay a deductible.
GEM: Play the Numbers
As you can see, you are playing a “60s” number game: You want to stay out of a hospital for 60 consecutive days, and because Medicare limits the number of free hospital days to 60 for each benefit period, your other goal is to avoid exceeding that magic number. Obviously, you don’t always have a choice, but sometimes you do. See Examples 5 and 6.
EXAMPLE 5
You require two complex nonemergency surgical procedures and extended hospitalization will be needed. Speak to your doctor about separating the treatments. By reentering the hospital after 60 days back home, you will be entitled to reset the Medicare timer for 60 more free days. Although you must pay a deductible again, it will still cost you less than the daily co-payments that you would have paid beginning on Day 61 of your long hospitalization. You and your doctor will need to consider all the medical and financial circumstances.
EXAMPLE 6
You are being treated for a chronic illness. You are hospitalized for 10 days, home for 20, then rehospitalized for 3 days and home for 15. If you keep this up, you will soon deplete your free days. So do whatever you can, without jeopardizing your health, to stay home for 60 days (e.g., arrange for home health care services). Then you can enter a new benefit period and gain new free days.
* * *
How Does Medicare Calculate a Day?
Sounds like a dumb question. A day is a day, right? Wrong. Medicare views a day in a different way from how you or we would. Since your coverage is based on calculating inpatient service days, it’s essential that you know how Uncle Sam defines a day. A Medicare day begins at midnight. (Not surprisingly, those bureaucrats chose the darkest hour as the starting point for a Medicare day!)
Any part of a day you are in a hospital or skilled nursing facility (including the day of admission) counts as one inpatient day. Your day of discharge does not count as an inpatient service day and will not be counted against you. To remember which days count, a quote from Shakespeare comes in handy (is it possible he had trouble with Medicare too?), “Life’s but a walking shadow, a poor [emphasis added] player that struts and frets his hour upon the stage, and then is heard no more; it is a tale told by an idiot, full of sound and fury, signifying nothing.” (Macbeth, Act V).
The day you depart does not count—it “signifies nothing.”
GEM: Avoid Late Charges
If you choose to stay in your room after normal checkout time for reasons of comfort or convenience, you will be responsible for any late charges, and the day will count even if you depart later that day. But if the delay is due to circumstances beyond your control (e.g., a morning treatment you were scheduled for was delayed, or the ambulance service does not to pick you up on time), then Medicare should cover any late charges, and your late departure should not be counted against you as another inpatient day.
GEM: Count Medicare Days
Double-check the dates of your admission and release on the hospital bill to make sure they are correct. When you are mistakenly billed for extra days, not only does it cost big bucks but it will also cause your Medicare game timer to run out early!
Also, keep watch on your Medicare timer to avoid unpleasant billing surprises later. You can’t count on Medicare or the hospital to watch out for you.
GEM: Watch Out for Unpaid Deductibles
Uncle Sam doesn’t play fair in starting the Medicare timer. Let’s say you are admitted to the hospital and this is your first illness. You have not yet met your Part A deductible. Even though you will be footing the bill until you have paid off your deductible, the Medicare timer does not go on hold. It will still begin ticking on the day you entered and will count toward your 60 free days.
* * *
When Should You Use Reserve Days?
You, or someone acting for you, can decide at any time during a hospital stay whether or not to dip into your 60 nonrenewable reserve days. You can use these only once, and when they’re gone—that’s it! So use them wisely.
A hospital should notify you, at least five days before you have used up your 90 days of coverage, that you have the option to begin drawing on reserve days for the remainder of your stay. You will receive a form to sign to start taking reserve days. The reserve-day withdrawals will begin the day after your signed notice is filed and will remain in effect unless it is revoked.
GEM: Recapture Lost Reserve Days
Your decision to use reserve days is not cut in stone—at least not immediately. If you change your mind after leaving the hospital, you can recapture reserve days if both:
• You notify the hospital within 90 days of discharge that you will pay back all costs for services not covered by insurance.
• The hospital agrees.
You can even recapture lost reserve days after 90 days if your expenses will be paid by a third party (insurance company) and the hospital agrees. See Example 7.
EXAMPLE 7
More than three months after leaving the hospital, you decide that you’ve made a mistake by using reserve days. You’ve discovered that your supplemental insurance will cover your hospital care after the first 90 days. Now you would like to recapture your reserve days.
Even though it’s been longer than 90 days since your discharge, don’t give up. Contact the hospital’s billing department and ask if you can file a retroactive request not to use reserve days. If the hospital agrees, Medicare will be reimbursed and your private health insurance company will be billed for the additional care.
GEM: Deal Yourself into the Game
Uncle Sam stacks the cards against you. Thanks to a “Joker” in the deck, the Medicare Monopoly Game may prevent you from getting necessary treatment. Why? Providers can only find out whether a service is covered by Medicare after they’ve given you the care. So if it’s not a sure bet that Medicare will foot the bill, then chances are they won’t take a gamble on treating you.
The trick is to convince the hospital, skilled nursing facility, or home health agency to provide service. How? If you can afford to pay in case Medicare denies the claim, say so. If you can’t afford the cost, become a squeaky wheel: badger the provider to take a chance. A provider who hasn’t filed many wrong claims may still get paid by Medicare even if it turns out that the service isn’t really eligible for coverage.
MEDICARE HOSPITAL INSURANCE (PART A)
Now that you know the general rules of Medicare Monopoly, you’re almost ready to play. We first look at Hospital Coverage (Part A), and then discuss Medical Coverage (Part B). By the time you’re through, you should be able to give Uncle Sam a good run for your money.
Medicare Part A is the hospital, skilled nursing facility, and home health insurance that Uncle Sam provides when you turn 65. You can get Medicare Part A premium-free if you are eligible to receive Social Security retirement or survivor benefits (Chapters 1 and 2) or Railroad Retirement benefits (Chapter 13).
GEM: Take Medicare Even If You Delay Other Benefits
If you are eligible but choose not to file for retirement or survivor benefits yet, you are still entitled to receive Medicare at age 65. Don’t pass up this freebie—delaying Medicare serves no purpose.
GEM: Get Medicare Even If You Are Not Eligible for Free Coverage
At age 65, if you are a U.S. citizen or have been a permanent resident for five years, you can still enroll in Part A, even if you are not eligible for Medicare based on Social Security or Railroad eligibility. You will pay a monthly premium ($192 a month in 1992), but it is often worth the price. Contact your local Social Security office for enrollment information and an application.
GEM: Get Medicare Before Age 65!
You can start taking Part A Medicare if you have received Social Security or Railroad disability benefits for at least 24 months (see here, here). Don’t miss out on this valuable gem!
GEM: Government Employees Can Now Cash In
Until recently, federal, state, and local government employees were not eligible to receive Medicare benefits. State and local government employees hired before April 1, 1986, are probably still not Medicare qualified. But the rules have been broadened, and if you are now paying for Medicare hospital insurance (Part A) as part of your FICA tax, you should be considered Medicare qualified at age 65.
The rules covering government employees are very confusing. Have the folks at Social Security check your and your spouse’s employment record to determine if you are eligible. If you are told you are not qualified, request a specific explanation so you can double-check with a Medicare lawyer or someone familiar with the employee benefits where you work. Don’t take one person’s word as gospel. Mistakes are made.
* * *
Enrollment
Application for Medicare Part A can be a hassle. Thankfully, most people don’t have to apply. If you are 65 and will be receiving Social Security or Railroad Retirement benefits, you can escape the filing process. You are automatically enrolled as soon as you start taking these other government benefits.
EXAMPLE 8
You are turning 65 and starting to collect Social Security. Don’t worry about Medicare application forms—you are automatically enrolled in Part A (you will also get Part B unless you choose to decline the opportunity and opt out).
EXAMPLE 9
At age 65, you were still working and didn’t apply for Social Security at that time. Now, at age 67, you are retiring. Your Social Security application automatically triggers your Medicare enrollment.
Individuals who take early Social Security retirement benefits will be enrolled automatically at age 65. If you opt to continue working after age 65, and delay receiving Social Security benefits, you can still start Medicare at 65, but you’ll have to apply—it won’t come automatically. You’ll also have to apply (at any age) to get Medicare benefits after receiving Social Security disability benefits for 24 months. Table 4.3 shows how this works.
If you qualify for automatic enrollment, your Medicare card should arrive in the mail. (If a card doesn’t appear in your mailbox by two weeks before your birthday, contact Social Security.) When you are Medicare eligible because of disability, your card will also come automatically. If you qualify at age 65, your card will be good for both Parts A and B. If you don’t want Part B, you will need to follow the instructions and notify Uncle Sam.
TABLE 4.3
Work Status and Enrollment

If you do not meet the automatic enrollment requirements, paperwork unfortunately will be necessary. Call or visit your local Social Security office to obtain an application. Be prepared to provide the following information:
1. Age. Don’t try fooling Uncle Sam; you need to submit proof—a birth certificate, hospital records, or some other documentation.
2. Social Security Number. If it’s lost, Uncle Sam has ways to track it down.
3. Income for the Previous Year. A W-2 form or copy of income tax return. Don’t worry, you won’t be audited.
4. Government Benefits. A list of any benefits you are entitled to receive (e.g., Federal Civil Service, Railroad Retirement).
GEM: Timing Is Everything
If you don’t qualify for automatic enrollment, sign up for Medicare Part A three months before your 65th birthday. Don’t procrastinate; delays could cost you. If you become ill and incur expenses before obtaining coverage, you may get stuck for all the medical bills. In addition, if you don’t apply promptly for Part B, you will pay a higher premium as a penalty for late enrollment, and your Part B coverage may be delayed a year or longer. Table 4.4 shows when to apply for Medicare.
TABLE 4.4
When to Apply for Medicare
If Your Birthday Is |
|
Apply for Medicare in |
|
||
January 2*–February 1 |
|
October |
February 2–March 1 |
|
November |
March 2–April 1 |
|
December |
April 2–May 1 |
|
January |
May 2–June 1 |
|
February |
June 2–July 1 |
|
March |
July 2–August 1 |
|
April |
August 2–September 1 |
|
May |
September 2–October 1 |
|
June |
October 2–November 1 |
|
July |
November 2–December 1 |
|
August |
December 2–January 1 |
|
September |
|
||
*Note: We will explain why we start with the second day of each month on here.
EXAMPLE 10
You have just turned 65. Although you are eligible to retire and to receive Social Security retirement payments, you have decided to continue working. You will wait to start Social Security, but you still expect to pick up Medicare now.
Your birthday came and went. You received cards from all your friends, but not the health insurance card from Uncle Sam. Should you be irate at the government bureaucracy for messing up again?
No. Here is one case where you can’t blame Uncle Sam. You don’t have to retire to receive Medicare Part A, but if you choose not to receive Social Security benefits at 65, your enrollment in Medicare Part A will not be automatic at that age. You must apply (contact your local Social Security office for an application).
EXAMPLE 11
You are retired and will begin receiving your Social Security benefits when you turn age 65 next month. You assume you don’t have to do anything to get Medicare.
Right! You are automatically enrolled in Medicare Part A when you receive Social Security benefits.
GEM: Get Medicare Part A Retroactively
You can change your mind and get Part A benefits retroactively! This is an extremely important tip to know when fate deals you an unlucky blow.
Let’s say you were eligible for Social Security but chose to postpone receiving those benefits. You forgot to apply for Medicare. Unfortunately, two months after your 65th birthday, you have a bad fall and fracture your hip. You are hospitalized and upon your release will require skilled physical therapy. If you sign up to receive Social Security (as soon as you can get back on your feet, so to speak), the Medicare Part A benefits you will receive can pay for any covered hospital and health care expenses even though they occurred before you applied.
However, there are time limits to Medicare’s patience. Here are the Golden Rules: You can pick up coverage dating back to the first day of your 65th birthday month, but not more than six months before the month you filed your application. (The deadline is 12 months if you are receiving Social Security survivor benefits.) You’ll be stuck paying any expenses incurred more than six months before you applied.
* * *
The date of your birthday can put money in your pocket. Our next three gems are Happy Birthday presents from your Uncle Sam.
GEM: Get Coverage for Your Full Birthday Month
You turn 65 on September 27. Surprise! Uncle Sam will give you Medicare coverage starting on September 1—the first day of your birthday month. Those extra days of coverage can mean a lot of dough to you.
GEM: Get an Extra Month Free If Your Birthday Falls on the First of the Month
Growing old is no laughing matter. Or is it? Consider this riddle: When is your birthday not your birthday? Answer: When you are dealing with Medicare!
Hard as it is to believe, Uncle Sam even had to stick his nose into this basic fact of life. For 65 years, you might have thought you knew your date of birth, but guess what? You were wrong. According to the folks at Social Security (who know better), you officially turn one year older on the day before your actual date of birth. Why do they do this? Who knows. Why does it matter? Because you can get an extra month of benefits, as Example 12 shows.
EXAMPLE 12
You turned 65 on February 1. Medicare says your birthday is really January 31. That means you can get Medicare benefits for the whole month of January!
Don’t forget that this crazy birthday rule will also affect the month in which you should enroll for Medicare. We’ve taken this into account when setting up Table 4.4.
MEDICARE PART A: INPATIENT HOSPITAL CARE
As we mentioned earlier, Medicare Hospital Insurance Part A is not exactly the most fitting title Uncle Sam could have picked to describe this entire program, because Part A actually covers more than just hospital-based services. Also included are inpatient skilled nursing facility care, home health care, and hospice care.1
We’ll first tell you about inpatient hospital care, giving you a treasure chest of gems to help you extend your coverage. Then we’ll uncover the secrets of the other Part A benefits.
How Do You Get in the Hospital Door?
Before the gates of Medicare Part A coverage are even opened to you, you need to meet Medicare’s four Hospital Entry Conditions, as stated in The Medicare Handbook (page 12).
• Has a doctor (not you) decided that your medical condition requires inpatient care?
• Is the type of care you need only available in a hospital?
• Is the hospital participating in Medicare?
• Has the hospital’s Utilization Review Committee (URC) or Uncle Sam’s Peer Review Organization (PRO) not disapproved your stay?
If you answered yes to all four questions, then go knock on the hospital’s doors. You should be allowed in, as Medicare’s guest.
What Medical Services Does Part A Inpatient Hospital Care Actually Include?
A good understanding of the inpatient hospital services you are entitled to under Medicare Part A should help assure you get what you deserve and avoid wrongful charges (which often occur). We have listed the most important covered services in Table 4.5.
TABLE 4.5
Covered Hospital Services
• Use of hospital facilities ordinarily provided to treat inpatients (isn’t that generous; there’s no extra charge for walls and floors).
• Semiprivate hospital room (2–4 beds).
• All your meals, special diets too (of course, we know they should be paying you to eat the food).
• Special care units, such as coronary care and intensive care, are thrown in at no extra charge.
• Medical social services, which can include:
1. Assessments of your social and emotional status to determine their impact on treatment and recovery
2. Evaluations of your medical and nursing needs to determine what community and personal resources will be needed upon discharge
3. Any social services ordinarily provided by the hospital that can contribute to the treatment of your illness
• Drugs ordinarily provided to hospital patients. Drug must be FDA approved as safe and effective for treating your illness. Experimental drugs or drugs that have not received final FDA marketing approval are not covered, unless specific permission has been given by Medicare.
• Blood transfusions. Although blood processing fees, starting with the first pint of blood, are covered, you are expected to either pay for, or find donors willing to replace, the first three pints you used. Don’t worry—Medicare does not intend to “bleed you dry.” During a calendar year, if you satisfy the blood deductible under Part B, you won’t be required to give another three pints for your Part A deductible. Isn’t that comforting?
• X-rays and other radiology services, including radiation therapy. These services must be billed by the hospital. Medicare bureaucrats with “x-rated” vision can see through any claims submitted from unapproved facilities and will deny coverage.
• Operating and recovery room costs, including hospital fees for anesthesia services. You can put your mind at rest. You won’t “go under” paying the hospital’s fees for surgery. The surgeon’s and anesthesiologist’s fees, though not covered by Part A, should be covered by Part B (here).
• Lab tests and diagnostic services performed by the hospital.
• Medical supplies and equipment. Medicare will pay for items a hospital ordinarily provides for the care and treatment of its inpatients—casts, splints, wheelchairs. However, you generally can’t take these items with you and expect Medicare Part A to pay (although Part B can cover these items; see here).
• Routine nursing care. You’re in luck: the nurse who wakes you at 6:00 A.M. to take your temperature is included at no extra charge!
• Specialists (e.g., nurses, anesthetists, psychologists). When the specialist works for the hospital, Medicare will pay.
• Rehabilitation services, such as speech therapy, occupational therapy, and speech pathology.
• Hospitalization due to dental-related disorders. Getting Medicare to pay for dental costs is, pardon the expression, like pulling teeth. But under certain circumstances, you will be covered for the hospital’s charges. For example, Medicare should pay hospital expenses for a noncovered dental service if your stay is required because of either the severity of the procedure or your physical condition (e.g., you have a history of heart trouble, and the dental surgery you’re having requires anesthesia). Your dental surgeon or physician must certify that hospitalization is necessary.
• Alcoholism treatment. Inpatient hospital care for alcoholism and detoxification should be covered (usually two to three days), if medical complications are likely to occur. A stay for rehabilitation will not be covered unless specific reasons can be given for a hospital setting rather than using a less costly outpatient treatment program.
• Inpatient psychiatric hospital care. You generally are entitled to a lifetime total of 190 days of coverage at a Medicare-approved psychiatric hospital.
Source: The Medicare Handbook, page 13.
The following gems can help you cash in on the covered services listed in Table 4.5.
GEM: Get Special Drug Coverage
If you can get the hospital to agree to specially order a drug for you because it is not routinely stocked, Medicare should cover the cost, even though it is not ordinarily provided to hospital patients. In addition, for a limited period of time, Medicare will pay the costs of drugs after you leave a hospital, if using that medication on an outpatient basis will speed your departure. Why? By treating you at home, Medicare saves money.
GEM: Get Special Coverage for Off-site Lab or Diagnostic Tests
If an off-site location must be used to perform diagnostic procedures because the hospital is unable to provide this care, Medicare should cover the cost.
EXAMPLE 13
In order to diagnose your hearing disorder, complex testing is necessary. The hospital does not have an audiologist on staff so you are sent to a hearing and speech center. This off-site service should be covered.
Part A should pay for any off-site lab and diagnostic service if the hospital has an agreement with a Medicare-approved provider and the services will be billed directly to the hospital. Ask your doctor or the hospital to make sure Medicare is covering. If you receive a bill for the service, DO NOT PAY! Call the service provider and explain why.
GEM: You Can Take It with You: Keep Your Pacemaker!
As Table 4.5 shows, Medicare generally won’t pay for supplies and equipment you take with you. But when it would be medically unreasonable to demand their return, you should be allowed to “carry out” items you are “wearing,” such as cardiac valves, pacemakers, drainage tubes, replaced body organs, and so on—at Medicare’s cost! Although equipment provided to use outside the hospital will not be paid under Inpatient Hospital coverage, you might be eligible for additional benefits under Medicare’s Part A Home Health Care Insurance (here) or under Medicare Part B (here).
GEM: Get Special Coverage for Nonstaff Members
While Medicare says it only pays for services by persons on the hospital staff, you should also be covered if hospital service is provided by a nonstaff member (such as a psychologist or therapist) under a contract with the hospital. (Any private agreements you work out don’t count!)
GEM: Pass the Rehabilitation Services Coverage Test
Although The Medicare Handbook states that rehabilitation services are covered, getting coverage is not as easy as it sounds. Medicare will pay only when you can prove the rehabilitation is “reasonable and necessary” for treating your illness. To meet these requirements, make sure the therapy is:
• Prescribed in writing by your doctor or physical therapist.
• Performed by a qualified therapist or done under his supervision. (Even health maintenance and routine services performed by nurses’ aides or other support staff to promote fitness or flexibility can sometimes be covered; check with your doctor or hospital’s representative who handles Medicare services.)
• Restorative. No matter who provides the service, Medicare won’t pay a penny for therapy if you are not going to improve “significantly” after a “reasonable” period of time. When you and the Government don’t see eye-to-eye on your progress, have your doctor or therapist write a letter explaining why the therapy is still justifiable to maintain or restore your health.
GEM: A Hospital Can’t Stick You Twice
If a service you receive at a hospital is eligible for Medicare coverage, the hospital is not allowed to charge you at all for that service, even if its actual cost for providing you with the care is more than the Medicare reimbursement. The hospital must pay any additional cost—so don’t let them “needle” you for the money.
* * *
What Hospital Services Will You Pay for?
Medicare will not pay for your “comfort and convenience” in the hospital. It is best to operate on the assumption that any care or service used to make your hospital visit more pleasant will not be paid for by Medicare. Therefore, according to The Medicare Handbook (page 13), you will be billed for:
1. Telephone, television (and any other personal conveniences).
2. Private-duty nurses. Even if this care was ordered by your doctor because the hospital was unable to provide the needed service, you must still pay.
3. Any extra charges for a private room, unless your condition required isolation or no semiprivate rooms were available.
What If You Go to a Non-Medicare Hospital?
Although most do, not every hospital participates in the Medicare program. If the hospital you go to has not signed a participation agreement with Medicare, Medicare will not pay even for covered services. Medicare does not pay for services performed at a nonparticipating hospital.
There’s an important exception to this rule: Medical services provided by a nonparticipating hospital in life threatening situations can be covered.
EXAMPLE 14
You are involved in a car accident and are very seriously injured. The emergency medical squad takes you to the closest hospital that is qualified to handle such emergencies. The bad news is that you were unconscious and couldn’t ask if it was a Medicare participating facility, and it isn’t. The good news is that Medicare may still pay.
To qualify for emergency Medicare coverage, you must meet all of the following requirements.
1. Your medical condition, if not treated immediately, would have resulted in death or serious impairment.
2. The hospital chosen was significantly easier to reach or closer than the nearest participating facility. (Caution: Medicare has denied claims when a participating hospital was available 15 miles away.)
3. The hospital meets Medicare’s standards for providing the needed emergency services.
The regional Health Care Financing Administration (HCFA) office is responsible for deciding if all criteria for coverage have been met. A physician’s statement supporting the claim of a medical emergency will also be required.
GEM: Get Out When the Emergency Is Over
Medicare will pay for your care at a non-Medicare facility for only as long as the emergency condition exists. When Medicare decides you are well enough to be transferred or released, coverage will stop.
* * *
Will you be covered if a medical emergency arises while you are vacationing in a foreign country? Non, Nein, Lo—the answer in any language is no, with one exception: If you were in Canada or Mexico and you can prove that the foreign (non-Medicare) hospital was closer than the nearest participating U.S. hospital, Medicare might pay.
MEDICARE PART A: SKILLED NURSING FACILITY (SNF) CARE
Nursing-home costs can be catastrophic. In limited cases, your Part A insurance can continue to pay for care at an SNF after you leave the hospital. But, as you probably have guessed, Medicare does not make it easy to qualify; very specific conditions must be met. You are eligible for this type of extended care coverage if you can check yes to all of these statements, according to The Medicare Handbook (page 15).

Medicare does not like paying for skilled nursing care. Nationally, only about 2 percent of all nursing-home costs are paid by Medicare. That is far too little. By understanding Medicarese and vigorously pursuing your rights, however, you should be able to get better results from Medicare. (If you can’t cash in on Medicare, Medicaid may provide a Golden Opportunity for funding; see Chapter 11).
What Is a Skilled Nursing Facility?
According to The Medicare Handbook, an SNF is “a specially qualified facility with the staff and equipment to provide skilled nursing care or rehabilitation services and other related services.” Some nursing homes provide only skilled care and participate entirely in Medicare. In others, only certain portions of the facility might participate in Medicare as an SNF, and some SNFs don’t participate in Medicare at all. Make sure you are in a Medicare-qualified bed in a Medicare-qualified facility.
The key question is, Is this facility a Medicare-qualified SNF for the services I need? Have your doctor give you a complete list of the services you need. That way you will have an accurate record to work with when you are playing caregiver matchmaker.
How do you find out if the facility qualifies for Medicare coverage for your service? Here is a list of likely sources for help:
• Hospital Discharge Planners. These folks are familiar with the services available at local SNFs and can usually provide an answer, or they can call and inquire for you.
• Nursing Home Admissions Offices and their Utilization Review Committee (URC). Every facility that participates in Medicare has a URC, and it is their job to decide whether the services you need will be covered by Medicare.
• The Medicare Intermediary for Your Area. Each state chooses which insurance company will act as an intermediary and process its Medicare Part A claims. The toll-free numbers of the Medicare Intermediaries for every state can be found in Appendix 17.
• Social Security. If you are lucky enough to get through on the toll-free number, tell the representative that it is printed in The Medicare Handbook that Social Security can “check with the HCFA” to determine whether your specific needs will be covered. (See the Handbook section titled Skilled Nursing Facility Care.) Then read the list of services you require.
GEM: Get Help to Help You Get Help
When we say “you,” you don’t need to take us literally. If you are not feeling up to taking action (and obviously if you were feeling terrific, you wouldn’t be needing SNF care services), don’t make yourself sicker trying to do all this alone. Get some help.
Whom should you ask? Consider all sources for assistance:
• Family
• Friends
• Hospital social worker or discharge planner
• Office on Aging (check the blue pages of your phone book under County Government)
• Senior citizen centers in your community
• State or county nursing home ombudsman (these individuals are paid by the state or county to act as advocates for nursing home residents)
GEM: Don’t Let the SNF’s Goof Cost You
You shouldn’t have to pay for someone else’s mistake. If you are incorrectly placed in the nonparticipating section of an SNF, Medicare will deny coverage. But since it is the facility’s fault, not yours, you shouldn’t be liable. Hold on to your wallet; let the facility fight it out with Uncle Sam.
* * *
What Is the Difference Between Routine (Custodial) and Skilled Care?
When it comes to extended care coverage, Medicare makes it perfectly clear that there is a major distinction between routine (custodial) and skilled care. You’d better know the difference too, because how your care is defined will determine who is paying—Uncle Sam or you. Medicare pays for skilled nursing-home care provided on a daily basis; you pay for routine or custodial care (unless you have purchased private nursing-home insurance or can qualify for Medicaid—see Chapter 11).
Custodial Care. Could any Tom, Dick or Harry perform the job safely? A service that does not require the medical expertise of a skilled professional is considered routine or custodial (e.g., help with bathing, feeding, dressing, eating, or walking). In practical terms, if Medicare defines your care as custodial care, you will pay the bill.
Table 4.6 provides a sampling of services which are “routinely” considered routine and custodial.
TABLE 4.6
Sampling of Custodial and Personal Care Services
• Assistance with routine application of eye drops, ointments, and other medications
• Maintenance of colostomy, ileostomy, bladder catheters
• Changes of dressings for noninfected postoperative or chronic conditions
• Baths or care for minor skin problems
• Routine care of incontinence (e.g., diaper and linen changes)
• Routine help with braces, casts
• Heat treatments for comfort (e.g., whirlpool)
• Assistance with medical gases, once a regimen has been established
• Help with dressing, eating, personal hygiene
• Supervision and assistance with exercise programs that have already been taught (e.g., repetitive exercises to maintain or improve strength and endurance) and do not require skilled supervision
Source: 42 C.F.R. §409.33(d).
Skilled Care. As you probably can guess, skilled care is just the opposite of routine care. A service is skilled when only someone with special training can perform safely and effectively the tasks of care, observation, or assessment. At least on paper, the difference between routine and skilled care seems clear. But as you will see, determining what care requires skilled services is not at all clear. Shades of gray appear because each person’s psychological, physical, and environmental circumstances are unique, and by law, Medicare is supposed to base its care decisions on your total situation [42 C.F.R. §409.33 (a) (1)].
Medicare can barely handle black and white, so do you actually believe some bureaucrat buried in paperwork has the time to examine the “gray”? You can expect “differences of opinion” (read that denial of claims). In fact, the Government unfairly avoids paying claims by strictly interpreting “skilled” care. We have had clients who were connected to so many tubes they looked like something out of a science fiction movie, and yet Uncle Sam refused to pay, claiming their care was not skilled! The Government will trample your rights unless you (or a loved one) insist on coverage.
Here is an example that illustrates the gray variations that can arise over routine and skilled care.
EXAMPLE 15
After a complex surgery, you were admitted to an SNF for care. Why was an SNF appropriate? In addition to needing physical therapy three times a week, a nurse had to take your temperature hourly each day. When the claim for your care is submitted, the Medicare bureaucrat who reviews it says, “Aha—do they take us for fools? Obviously, SNF level care isn’t needed for this person because reading a thermometer is an unskilled duty. The claim must be denied,” she says with glee.
Now here comes the gray. What she failed to notice (or could not know because the claim form was not specific enough in its explanation) was this key fact: You had recently been placed on a potent, potentially lethal medication, and the first sign of toxicity is a slight fever. The services of a skilled nurse to read a thermometer were truly medically justified to evaluate and manage your condition. In this situation, although the care itself is unskilled, only an LPN had the level of expertise to interpret symptoms and make recommendations for adjusting the treatment. Your care should be considered skilled—and covered!
The best way to get an idea of which type of care is skilled is to look at actual situations. In Table 4.7, we list some real-life circumstances that should qualify for skilled nursing service coverage.
TABLE 4.7
Sampling of Skilled Nursing Services
• Tube feedings and other related services. Gastrostomy feedings, and nasopharyngeal and tracheostomy maintenance and replacement, are complex activities requiring skilled nursing and should be covered when needed to treat your illness.
• Catheters. Insertion, cleaning, and replacement of catheters should be covered skilled services.
• Wound care. Don’t expect Medicare to pay for a skilled nurse to bandage your little nicks and scratches. But when the size and nature of a wound, burn, tube site, sore or tumor require application of medicated dressings or other special care and monitoring, the care should be considered skilled. Your doctor will need to document the reasons and provide specific instructions in your plan for care (your doctor’s written prescription for the services and treatment you will need to stabilize or cure your condition); otherwise, you might be denied coverage.
• Ostomy care. Immediately following surgery, or where complications occur, care for an ostomy can be covered.
• Heat treatments (e.g., hot packs, whirlpool baths, infrared treatments). You’ll take the heat for this care unless the treatments have been ordered by a physician and require observation by nurses to evaluate your progress.
• Intravenous, intramuscular, or subcutaneous injections. Diabetics take note: insulin injections fall into this category and so can be covered as a skilled service. This has often been a bone of contention for SNF eligibility.
• Medical gases. Administration of medical gases can be covered in an SNF. Teaching you or your caregivers how to administer treatment and also monitoring your response to the gases until your condition stabilizes also can be qualified as skilled service.
• Treatment of serious skin disorders. Serious skin problems, such as decubitus ulcers, often require skilled care.
• Bowel and bladder training. Helping a patient regain bowel and bladder control can qualify for coverage as skilled care.
Source: 42 C.F.R. §409.33(b).
What Are Skilled Rehabilitation Services?
You are entitled to coverage under Part A for skilled rehabilitation services—such as physical, speech, and occupational therapy—at an SNF. Speech therapy includes procedures necessary to diagnose and treat speech and language disorders. Occupational therapy includes treatment to improve or restore a patient’s ability to handle daily activities.
EXAMPLE 16
You had a hip replacement, and after the operation you have difficulty regaining your balance. Your doctor prescribes physical therapy. Working with a qualified therapist at an SNF, you learn standing and walking techniques to improve your balance. The cost for these services should be covered by Uncle Sam.
EXAMPLE 17
You suffer a stroke and lose partial use of your right arm. An occupational therapist teaches you new ways to hold eating utensils so that you can feed yourself and regain independence. The SNF costs should be covered.
Table 4.8 lists some examples of rehabilitation services that should qualify as skilled care in an SNF.
TABLE 4.8
Sampling of Skilled Rehabilitation Services
• Assessment of rehabilitation needs. These include tests and measurements of range of motion, strength, balance, coordination, endurance and functional abilities.
• Therapeutic exercises or activities. If the type of exercises or your condition requires supervision to ensure your safety or the effectiveness of the treatment, it should be covered.
• Walking evaluation and training. If your ability to walk has been impaired, evaluation and training should be covered.
• Exercises in response to loss or restriction of range of motion.
• Maintenance therapy. Let’s say you have Parkinson’s disease. Exercises to maintain your present level of functioning, under the supervision of a qualified therapist, should be covered.
• Ultrasound, short-wave, and microwave therapy.
• Hot pack, hydrocollator, infrared treatments, paraffin baths, and whirlpool. These should be covered if warranted to treat your specific condition and the skills, knowledge and judgement of a qualified therapist are required.
• Services of a speech pathologist or audiologist.
Source: 42 C.F.R. §409.33 (c).
The Government often catches you in one of two traps: your claim for SNF coverage will be denied if you can’t show that the treatment or therapy is essential to improve or maintain your physical condition; and coverage will be denied if skilled care is not required on a daily basis.
Uncle Sam generally expects improvement over a “reasonable” and “predictable” time period.
EXAMPLE 18
As a result of a stroke, your speech is impaired. A skilled speech pathologist assesses your rehabilitation potential and determines that, with therapy, a measurable improvement in your communicative skills can be achieved. A plan of care is devised with specific goals for speech production. Medicare will pay for the skilled speech therapy because you have “rehabilitation potential” and it is hoped significant improvement can be achieved in a predictable time. Keep in mind that coverage will last only as long as you can continue to “pass” the tests. Once the benefit of therapy stops, Medicare coverage will, too.
GEM: Maintenance Is Enough to Get Coverage
The Government has a tendency to overlook the fact that rehabilitation service should be covered as long as the treatment is necessary to maintain your condition. Don’t let them!
EXAMPLE 19
Your father suffered a stroke and is having trouble walking. A therapist in the SNF has been helping him learn to walk with a walker, but now the Government says he’s not making further progress.
Although he may not be making further progress, he is likely to regress if therapy is stopped. Without continued therapy, he will go back to the wheelchair. In this case, you can fight the Government’s decision to cut off benefits.
To qualify for coverage in an SNF, the skilled care must be provided on a daily basis. This means that the skilled nursing or rehabilitation service you receive must be needed seven days a week. Uncle Sam does allow one important exception: if skilled rehabilitation services are not available every day, you can still qualify for coverage if you receive the service at least five days a week.
* * *
GEM: A Short Break in Rehabilitation Should Not End Coverage
Let’s say your doctor suspends your rehabilitation program for a couple of days because you are exhausted and need a rest. Or maybe you get sick and miss three days. The short break should not cause you to lose Medicare coverage, but a break in skilled nursing care can terminate your benefits.
GEM: Try Part B Coverage
Therapy at an SNF can also be covered under Medicare Part B insurance. If you have used up, or aren’t eligible for, Part A coverage, check out this option with the SNF. Note: under Part B, the services of an independent therapist are limited to $750 a year and you must pay co-insurance, too.
GEM: Make Sure the Provider Uses the Right Claim Form
We have seen rehabilitation claims unfairly denied simply because the wrong claim form was used. You can’t use a Part B claim form to get Part A services, and vice versa. If you are denied, check to see if the right form was used and ask the provider to refile. Your denial may have just been from incorrect paper work.
GEM: Make Sure Doctor Certifies Need for Skilled Care
Your doctor must certify in writing that skilled-level care is required as an inpatient or on a daily basis (at least five days a week). If your doctor doesn’t routinely attend to Medicare patients, make sure he works with the hospital’s discharge planner to assure all the certification paperwork is done.
* * *
What Are the Time Requirements?
To get Medicare to cover SNF services, you must have been hospitalized at least three consecutive days before entering an SNF. That three-day requirement is a hidden trap that can cost you plenty.
EXAMPLE 20
Dan entered the hospital on January 1 and was transferred to a Medicare-approved SNF on January 3. Will Medicare pay? No. Even though Dan went to an approved facility and was receiving skilled nursing care, he did not meet the three-consecutive-day hospitalization requirement. Medicare counts the day of admission as one day, but does not count the day of discharge. If Dan had stayed in the hospital one more day and transferred on January 4, he would have been eligible for Medicare coverage. Instead, he will be paying thousands of dollars to the nursing home out of his own pocket.
EXAMPLE 21
Dan spent three days in a psychiatric hospital before being transferred to an SNF. Will he be covered? Yes. Treatment in a psychiatric hospital should be considered equivalent to a “general hospital,” so the three-day inpatient care requirement is met.
What if the three days prior to SNF admission were spent at a Christian Science Sanitorium? No. Medicare doesn’t consider these facilities hospitals, so time spent there is not counted.
Medicare applies the three-day requirement strictly. It won’t waive the three-day requirement even if you are forced out of a hospital because of a lack of beds.
EXAMPLE 22
You were treated in the hospital emergency room and required immediate hospitalization. Unfortunately no beds were available, so you were admitted to the SNF unit of the hospital. Medicare will not pay even though the unit was a participating SNF. Why? To receive benefits at an SNF, you must first be hospitalized for three days.
GEM: Beat the Three-Day Requirement!
Don’t let the hospital or doctor discharge you or a loved one to an SNF before you’ve spent three days in a hospital. Talk to your hospital discharge planner or doctor to see if an extra day can somehow be justified. That extra day can save you thousands of dollars in nursing costs.
If the hospital (through its Utilization Review Committee) or Peer Review Organization (PRO) tells you to leave, challenge their decision—don’t go! Insist on staying another day. If the PRO told you to leave, and you lose the appeal, you will have to pay the extra day of hospital care, but the cost will be worth it if the extra day helps you meet the three-day hospitalization requirement for SNF coverage! And if the notice to leave came from the hospital, you won’t have to pay while the PRO reviews your case (even if the PRO agrees with the hospital).
* * *
In addition to the three-day requirement, Medicare imposes another time requirement: You must enter the SNF within 30 days after leaving the hospital, and your care at the SNF must be necessitated by the same condition that first sent you to the hospital. Continuity of care is the key phrase here.
EXAMPLE 23
Dan was hospitalized for a severe foot infection; he stabilized and four days later was discharged. Twenty-two days later his doctor admitted him to a Medicare-approved nursing home, where he received skilled nursing care for a different condition. Will Medicare pay? No.
But Dan met the 30-day limit and 3-day hospitalization requirements, right? Yes and no. Remember, for the stay to be covered, the need for extended care services must either be due to the condition that necessitated hospitalization or be an ailment that arose during that stay.
GEM: Get Proof of Continuity of Care
Make sure your doctor’s statement certifying your need for care clearly establishes a link between your hospital stay and the skilled nursing care you will need.
* * *
Medicare expects you to enter an SNF within 30 days after the day you left the hospital. For example, if your date of discharge from the hospital is July 1, and you enter an SNF on July 31, you will be covered because the Medicare meter starts ticking on July 2, the day after discharge. But if you enter the SNF one day later on August 1, you will be out of luck. You will have exceeded the 30-day limit.
Will Medicare Pay?
Will Medicare pay if you:
• Enter an SNF for custodial care within 30 days after leaving the hospital but after 30 days you then need skilled care? NO. You must start skilled services within 30 days.
• Require skilled care for the first 10 days, only custodial care for the next twenty days, then on Day 31 skilled care again? NO. Medicare will pay for those first 10 days, but will not resume payment for the subsequent skilled care because 30 days have elapsed since your hospital discharge.
• Leave an SNF and are readmitted (to the same or a different SNF) within 30 days of your hospital discharge owing to the same illness? YES. You can go home again, so to speak, as long as it’s within Medicare’s time limits.
• Leave an SNF, then suffer a relapse within 30 days after discharge that requires a hospitalization? YES. If the hospitalization occurs within 30 days after your discharge from the SNF, Medicare will treat your hospital stay as if it’s a return to an SNF.
GEM: Extend the 30-Day Limit
Medicare—in its great wisdom—recognizes that, with certain health conditions, transfer to an SNF within 30 days to continue treatment is not always “medically appropriate.” In that case, you may be able to get an extension. To qualify, at the time you leave the hospital, your doctor must have a specific timetable for continuing skilled treatment at an SNF, and you must really follow through.
Medicare won’t accept any vague promises; Uncle Sam wants predictability. To illustrate this point, Examples 24 and 25 show two very different outcomes.
EXAMPLE 24
You fall and break a hip. After leaving the hospital you will still need physical therapy. Appropriate medical procedure requires a four- to six-week wait before treatment can begin. Your doctor prepares a written plan of care that states you will enter an SNF five weeks after hospitalization to begin rehabilitation therapy. Under Medicare rules, you shall be able to get an extension because the delay was “medically appropriate” and predictable.
EXAMPLE 25
You were hospitalized to treat a severe stomach disorder. It is very likely that you will require treatment again in the near future, but your doctor can’t give an exact time frame or estimate the level of care that will be needed. After 30 days, if you do need skilled care, tough luck! Although the delay in care might be medically appropriate, it is not predictable. That means no money.
GEM: If You Can’t Get in Within 30 Days, Try to Delay to 60
If you don’t need an SNF for 30 days, and you can’t get an extension, try to stay at home for 60 days, so that you can enter a new benefit period. If you then return as a hospital inpatient for three days, you will be entitled to a new chance to qualify for SNF benefits. Example 26 shows how this happens.
EXAMPLE 26
Let’s start with the same situation as Example 25. Just 59 days after your discharge from the hospital your stomach problems start to reappear. You immediately rush to the hospital, where you are treated for four days. You are then discharged to an SNF.
Unfortunately, since 60 days had not passed from the prior hospitalization, no new benefit period starts, so you don’t get coverage for the SNF. Had you been able to wait one more day at home before entering the hospital, your SNF bills would have been covered.
* * *
What Will Medicare Pay?
Once you qualify for SNF coverage, the questions are what Medicare will pay for, and what services are covered. Table 4.9 shows what Medicare pays.
TABLE 4.9
Who Pays for Skilled Nursing Facility Care Coverage?

As Table 4.9 shows, Medicare pays for all or part of your covered services for up to 100 days each benefit period. Keep in mind that once you are out of an SNF for 60 days in a row, the Medicare timer goes back to zero, and you are entitled to a new 100 days of SNF coverage. Of course, you must still meet all the same conditions (three-day hospital stay, etc.) before Medicare will pay.
What Services Do You Get?
Assuming you are in a participating SNF, you need skilled care, and you meet the time requirements, Medicare will pay for the services listed in Table 4.10. Table 4.11 lists services that Medicare will not pay for.
TABLE 4.10
SNF Services Paid by Medicare Part A
• Skilled nursing care.
• Semiprivate room (two to four beds in a room). If one isn’t available at time of admission, Medicare will pay for a private room, but when a semiprivate is ready, you must switch or pay.
• All meals and special diets (unfortunately, pizza doesn’t count as a special dietary need, so delivery charges for a pie aren’t covered!).
• Regular nursing services provided by SNF staff (e.g., taking your temperature or blood pressure).
• Rehabilitation services, including physical, speech, and occupational therapy.
• Drugs, medical supplies and therapeutic equipment (e.g., splints and wheelchairs).
• Blood transfusions (after meeting your three-pint deductible).
• Medical social services and diagnostic services, including a social worker’s assessment of your adjustment to treatment and help in responding to emotional issues resulting from the illness.
• Other services necessary to maintain your health that can only be provided by an SNF.
Source: The Medicare Handbook, pages 15–16.
TABLE 4.11
SNF Costs You Pay
• TVs, telephones, and any other personal luxuries
• Private-duty nurses
• Additional charges for a private room, unless medically necessary
• Custodial nursing home-care services (e.g., haircuts), other than daily personal care needs like bathing, feeding, and dressing
• Doctors’ bills (Medicare Part B insurance will help pay these fees—see here)
Source: The Medicare Handbook, page 16.
When Medicare is paying, don’t expect a room with a view and privacy, too. You are entitled to a semiprivate room (two to four beds in a room). That is it, period. This rule applies to both hospitals and SNFs.
GEM: Get a Private Room, at Uncle Sam’s Expense
Here are two ways you might get a private room.
First, if your condition requires isolation to protect your health or others, a private room should be considered “medically necessary.” Get Medicare to pay.
Second, if at the time you are admitted no semiprivate or ward rooms are available, you should be entitled to “fly first class for the price of coach.” You can have a private room at no extra charge. But don’t get too comfortable; as soon as a semiprivate room opens up, out you go (unless you’re willing to pay the difference).
If your admission could have been delayed until a semiprivate room was available, but you still chose to enter the facility, you will foot the bill for the price difference between the two types of accommodation.
GEM: Don’t Get a Private Room by Mistake—at Your Cost
State your room preference to your doctor; otherwise, if he has first-class taste, you could end up paying for his decision.
* * *
Extended care services that are custodial and not skilled are covered only if they are routinely provided by an SNF. Items and services that wouldn’t be covered if you were a hospital inpatient won’t be covered when you’re at an SNF, either. For example, expect to pay for personal laundry (does it strike you as odd that although you are sick enough to require skilled care, the folks at Medicare expect you to wash clothes?). When it comes to personal services, Medicare will hang you out to dry.
Plan Now to Avoid Pain Later
As much as we don’t like to think about needing nursing-home care, we should. Before a crisis arises, it makes sense for you (or a family member) to visit a few SNF facilities.
Where to Look. Ask friends who might have experience; call a local hospital’s discharge planning department for names; check the yellow pages and look for nursing-home listings that say “Medicare Certified.”
What to Look for. Call the chosen SNFs and request a tour and time to meet with the admissions director, then do some homework. There are many good books that deal with how to select an SNF. Checklists of questions to ask and what to look for are usually included. Take one with you when you visit.
How to Plan. After making the rounds, prepare a list of the facilities, noting any reasons why a particular SNF would not be acceptable to you.
When to Act. If you are hospitalized, begin your discharge planning ASAP! Don’t wait to be told. Ask your doctor what kind of posthospital care you might need. If he feels an SNF is appropriate, pull out your list.
By taking the initiative, you will feel less like a helpless victim. Your decisions can be based on information you obtained rather than relying solely on someone else’s advice (who might be under pressure to get you out of that hospital bed!). Of course, timing and luck are helpful because bed availability is an unknown variable. But by preplanning you can improve the odds of arriving at an acceptable SNF choice. And since seeking SNF care is far from fun, by making an informed choice at least you can transform a situation from nightmarish to tolerable. You and your family will sleep better knowing you have tried to do your best.
WARNING
When the hospital is ready to discharge you, you generally will have to accept the first SNF bed available, or pay for your extended hospital stay until a bed opens up in a facility of your choice. If you go home to wait for that bed to open, it may never become available because SNFs usually give preference to hospital patients.
GEM: Don’t Go to a Poor or Inconvenient SNF
You don’t have to accept the first available bed if the SNF is unsuitable—either not up to quality standards or not in a location reasonably close to your family. In these cases, Medicare should pay for the extended hospital stay while you wait. Unfortunately, Medicare often mistakenly denies coverage in these cases, and you might have to battle with a Medicare appeal. When you can justify your disapproval of an SNF, hang on to your hospital bed—you are right to stay and fight.
MEDICARE PART A: HOME HEALTH CARE
Rather than enter a nursing home, wouldn’t you prefer to be cared for in the warmth and comfort of your own home? Of course you would! In some circumstances, Uncle Sam may give you that option.
When it comes to home health care, there is good news and bad news. The good news is that Medicare does provide a wide range of benefits for this type of care. The bad news is that Uncle Sam does not make it very easy to qualify for the coverage. Even when you are entitled to home health care, unfair denials are common. To keep Uncle Sam honest, you must stay on your toes. (Now that’s good incentive to stick with physical therapy!) Here are the rules for playing—and winning—this part of the Medicare Monopoly Game.
Medicare will pay for home health visits only when you can answer yes to these four eligibility statements:
• I need skilled nursing care provided on a part-time or intermittent basis or physical therapy, speech therapy, or medical social services in order to remain at home.
• I am receiving care from a doctor, and he or she set up a specific home health plan for care that will be reviewed periodically (every two months).
• I am confined to my home (an occasional walk around the block, if you are able, will not be held against you).
• The home health agency I use participates in Medicare.
If you meet these four requirements, Medicare should cover all medically necessary home health services for as long as you need skilled care, therapy (physical, speech, or occupational), or medical social services. There are no deductibles, no co-insurance (except for medical equipment), and no limits on how long the services may continue.
As you can see, Medicare coverage for home care does not carry all of the same requirements as does SNF coverage. The care must still be “skilled,” but no prior three-day hospitalization is required, and no connection to hospital care need be shown.
Home health care carries some additional requirements, though. Most important, the care must be provided by a Medicare-approved home-health-care agency, skilled nursing care you receive must be provided only on an intermittent or part-time basis, and you must be confined to home.
What Is a Certified Home-Health-Care Agency?
To qualify for Medicare coverage, the home care you receive must be from a Medicare-approved home-health-care agency. The agency will make an initial evaluation visit to determine whether your medical needs can be satisfied in the home environment. Factors considered are your overall health, your surroundings, and the family support system.
GEM: Don’t Pay for the Initial Visit
Who pays for an initial evaluation visit? You don’t! Medicare considers the cost of this first evaluation an operating expense for a home health agency. But don’t let anyone provide skilled services for you at this first visit, unless you first have an agreement with the home-health-care agency in your hands! Otherwise, you could be stuck with a bill no one wants to pay.
GEM: Shop Around for a Home-Health-Care Agency
Not all home-health-care agencies are alike. Some agencies bury a clause in their agreements stating you must foot the bill if Medicare disallows. Some offer more care than others, too. Read the fine print!
* * *
There are many agencies out there, but not all participate in Medicare. You will need to do some detective work. Possible sources for help are:
• Your Doctor. Chances are he/she has been asked before and has referrals.
• Friends. Perhaps you know people who have had to research home-health-care agencies. If you can benefit from someone else’s experience, that’s great.
• Hospital Discharge Planners. It’s their job to know the appropriate community resources and they probably have a list. (Oftentimes, hospitals are affiliated with home-health-care agencies and an assessment can be made without even leaving the comfort of your hospital bed!)
• Yellow Pages. The Home Health Service section will list numerous agencies. Some ads will state “Medicare/Medicaid Certified.” Obviously, call those first.
If you do call a nonparticipating agency, chances are they, too, can offer names of agencies that are Medicare qualified.
GEM: Plan Ahead
Don’t wait until you are ready to leave the hospital before starting to plan for posthospital care. Formulate a plan of action before an emergency arises. Ask your doctor “what if?” Line up a family friend willing to be “on call” just in case you need help with organizing posthospital care plans. And have someone start exploring home health care as early as possible.
* * *
What Is Intermittent or Part-time Skilled Care?
Uncle Sam expects you to know just what he means when he talks about “intermittent” or “part-time” skilled care. His insurance intermediaries obviously have no difficulty with the term, because they routinely deny claims that don’t meet his standards. But guess what? Until 1988, no published federal regulations existed that clearly defined intermittent or part-time care! It was only when a brave soul sued HCFA over the unfairness of this “minor” omission, and the courts agreed, that Medicare rewrote the guidelines more specifically. If Medicare won’t put the rules for Medicare Monopoly on paper, how can we be expected to follow them? Yet we are.
Meeting the requirement for part-time or intermittent skilled nursing care can be as easy as building a house in quicksand—the ground keeps shifting! But that won’t stop us from providing some cement for building a solid case to receive benefits.
Part-time or intermittent care is care that is not required indefinitely on a full-time basis, seven days a week. For example, if you only need care at home for a few hours a day for several days a week, you should have no problem.
Part-time care means care provided less than eight hours per day. It can be any number of days per week, but no more than 35 hours total in a week. For example, Medicare should pay for three hours a day, seven days a week. This can go on indefinitely.
Intermittent care means care provided on a regular basis that is needed less than seven days per week. It can be any number of hours per day, up to 35 hours total in a week. For example, Medicare should pay for six hours a day, five days a week. This care also can go on indefinitely.
EXAMPLE 27
Your dad just had surgery, and the incision became infected. He needs a skilled nurse to come in for a short time every day to clean and monitor the skin. Because she will only be there a couple of hours each day, the care should be covered.
GEM: Get Full-time Daily Care
Uncle Sam offers a bonus: you can get care seven days per week, eight hours per day (56 hours in a week) if the care is finite and predictable, meaning it won’t last for more than about 21 days. In certain cases, this full-time daily care can be extended for up to six months. Don’t assume you are the exception to the rule; make sure you get official approval for an extension. See Example 28.
EXAMPLE 28
Your mother has just had a severe heart attack. Although she was released from the hospital, she needs daily full-time skilled observation. She needs the skilled care for two weeks. Since it’s only for a limited and predictable time, these services should be covered.
GEM: Get Coverage for Services Required Only Once Every Three Months
Let’s look at the other extreme. Generally Uncle Sam wants you to get home care on a regular, predictable schedule, which means at least once every 60 days. But if you need skilled care only once in 90 days, can that qualify as part-time or intermittent care? If your doctor shows that you have a medically predictable need for skilled services, we “predict” you should get coverage. See Example 29.
EXAMPLE 29
Mr. Roth, age 88, is a diabetic with limited vision. He self-injects insulin. Medicare will pay for skilled nursing visits once every 90 days because a professional is needed to assess any changes in his health and to assure that he’s receiving the proper level of care. The care is medically predictable.
GEM: Long-term Conditions Can Qualify
Part-time or intermittent care does not have to mean short term. Care for long-term conditions can still be covered if the care required is part time or intermittent, as we’ve explained. But don’t expect Medicare to tell you that. As a matter of fact, Uncle Sam’s insurance intermediaries want you to believe that “exceeding limitations on duration” is a valid reason for denial. They don’t want to be shelling out thousands of dollars for long-term care. Yet the fact is, you are entitled to an unlimited number of visits as long as the care is medically necessary!
* * *
When Are You Considered “Confined to Home”?
You are considered “confined to home” if you can leave on your own only with the help of a wheelchair, a walker, or another person, and only for limited periods of time. This should not be too tough a standard to meet; if you can’t get around on your own, you should pass.
What Will You Pay for?
Before focusing on what Medicare will pay for, it’s helpful to look at what Medicare won’t pay for. In general, any care that is not skilled will be your responsibility, not the Government’s. Everyday tasks that can be done by anyone are not covered. The “comfort and convenience” rule applies to home health care, too: services provided solely for your comfort, but which are not medically necessary, are not covered.
An important exception is home health aides. If you are receiving skilled care, you may get coverage for home health aides providing personal unskilled services (here).
Here is a list of services not covered by Medicare when you are at home. According to The Medicare Handbook (page 16), you will pay for these:
1. Meals delivered to your house (e.g., meals-on-wheels).
2. Housekeeping and any other homemaker services not related to your illness.
3. Transportation services, even if necessary to enable you to receive medical services at an outpatient facility!
4. Drugs and the administration of drugs. (In certain cases, drugs that can only be administered by your doctor can be covered under Part B.)
5. 20 percent co-payment for durable medical equipment purchases.
6. Blood transfusions. (Dracula will be disappointed, but for most of us, this exclusion is no great loss.)
7. 24-hour-a-day nursing care on a permanent basis.
GEM: Don’t Let Medicare Just Say No to Drugs
Medicare specifically excludes the administration of drugs from coverage. But here is one small dose of good news. If a drug necessary for your treatment can only be administered safely by a licensed nurse, Medicare should pay for the service (e.g., intravenous, intramuscular, or subcutaneous injections should be covered).
This fact might be hard to swallow, but Medicare does not think giving you oral medicine requires a skilled nurse’s expertise, and so Uncle Sam won’t generally pay for administering oral medicine. How can you get around this? If you can show that an unstable condition, or the quantity of drugs you must take, requires careful observation for side effects, a skilled nurse can be justified.
Uncle Sam really rubs it in when it comes to body ointments or eyedrops. Medicare generally won’t agree to the need for a skilled nurse to deposit a few eyedrops or to apply a cream on your back, even when you can’t do it yourself. But again, if observation by a skilled nurse is needed to monitor your condition, Medicare should pay. See Example 30.
EXAMPLE 30
Mr. Cotten is diabetic and needs an insulin shot once a day. He also has muscular dystrophy. Poor muscle control prevents him from filling the syringes and injecting the insulin he needs. Medicare should pay for a skilled nurse to perform the service for him.
If Mr. Cotten only needed help with prefilling the syringes, Medicare would not pay. Why? This service is routine and supposedly does not require skilled nursing. Anyone can do the job, according to the decision makers at Medicare.
Note: By law, some states require a licensed nurse to prefill syringes. In this situation, Medicare will pay (but only if you are also receiving some other skilled nursing care or therapy).
* * *
What Will Medicare Actually Pay for?
You must understand the golden rules for home-health-care coverage. Otherwise you are sure to lose out on valuable benefits that are rightfully yours.
Skilled Nursing Care. Medicare covers skilled care provided by a nurse in your home, if the care is reasonable and necessary to treat an illness or injury. Our discussion of skilled care here generally applies here, too. A nurse who is providing unskilled service must be paid by you.
EXAMPLE 31
Mr. Jones has a colostomy and needs help changing the colostomy bag. Although he has no one to assist him, Medicare won’t pay for a nurse to help because the care is considered routine and could be performed by anyone.
But services that may not be skilled in one situation may be skilled in another.
EXAMPLE 32
Let’s continue Example 31. Because Mr. Jones couldn’t maintain the colostomy adequately on his own, he developed an infection. Now he requires special skilled treatment to clean and monitor the colostomy. Guess what? Medicare should now pay for these services.
Services that generally would be considered unskilled should be covered by Medicare when the nature of your condition requires a skilled professional to monitor or perform the task. Medicare should pick up the tab for the periodic visits of a skilled nurse, when ordered by your doctor, to assess your progress and to determine if changes in treatment are needed.
EXAMPLE 33
Bess Tyler, age 83, broke her leg. She is now wearing a cast. Normally, a leg cast involves no skilled supervision. But because she suffers from circulatory problems, her condition must be monitored by skilled rehabilitation personnel who can teach her correct movement techniques. The unique aspects of Ms. Tyler’s situation make this level of care appropriate. Medicare should pay.
But don’t expect Medicare bureaucrats to take the time to look closely at each case. Chances are, claims for care that look routine will be routinely denied. Your doctor’s job is to prove why this care is reasonable for you (e.g., supplying a detailed plan of care or letters of explanation from the home health agency), and your job is to make sure the doctor does his.
GEM: Get Compensation for a Supervisor
Medicare may pay a skilled professional to manage and oversee unskilled help when the nature or complexity of your condition requires it. If your doctor can prove medical necessity, Medicare should accept the claim that necessary unskilled services you are receiving need skilled supervision. Example 34 shows how.
EXAMPLE 34
Mr. Carlisle is a 72-year-old diabetic who also suffers with angina. He has been hospitalized for a severe leg infection. His home-care plan will require several nonskilled treatments: exercise to restore muscle tone, careful skin-care treatments, and administration of oral medications.
Although these services normally could be performed by an unskilled health-care aide without supervision, the patient’s condition creates a serious risk of complications. Until Mr. Carlisle’s condition stabilizes, a skilled professional’s expertise is necessary to assure the treatment plan is correctly coordinated—and that should be covered by Medicare.
GEM: Get Medicare to Pay for Teaching Old Dogs New Tricks
If you or family members will be providing unskilled care, you generally can’t get compensated by Medicare. But if you need a skilled professional to provide training, the education services of a skilled nurse to teach you or your caregivers how to manage your care program can be covered.
For example, according to the federal regulations (42 C.F.R. §409.33(a) (3)), Medicare should consider it reasonable to hire a skilled licensed nurse to teach:
1. Self-administration of injections or medical gases
2. New diabetics all facets of health management (e.g., diet, foot care, etc.)
3. Wound care when severity or patient’s overall condition requires
4. Care for an ostomy
5. Self-catheterization
6. Prosthesis care; use of braces and splints
7. Care and application of dressings to treat severe skin disorders
8. Correct administration of oral medications when side effects and interactions with other drugs and foods might occur
EXAMPLE 35
Sixty-eight-year-old Mr. Block has just been placed on insulin to treat his diabetic condition. His doctor has ordered a skilled nurse to teach him how to manage self-injection, recognize signs of insulin shock, and take emergency procedures. Medicare should pay because these skilled services are reasonable and necessary for his treatment.
EXAMPLE 36
Let’s say Mr. Block has been self-injecting insulin for five years. He recently changed doctors. His new physician orders skilled nursing visits every two weeks to monitor his self-injection procedures. Since there’s been no deterioration in Mr. Block’s physical and mental status, skilled care is not reasonable or medically necessary, and Medicare won’t pay.
EXAMPLE 37
Now, let’s say Mr. Block suffers a mild stroke. As a result, the use of his right hand is limited. His doctor orders a skilled nurse to retrain him in the self-administration of insulin. Because there has been a change in Mr. Block’s health status, reteaching is reasonable and necessary, and Medicare should pay.
* * *
When it comes to skilled teaching, the Golden Rule for coverage is: Medicare will do unto others for only as long as they can’t do for themselves. When Medicare decides you have learned your lesson and your condition is stable, coverage will end. If you disagree, be prepared to appeal and prove your point. You may have to agree to pay for the home-health-care agency privately to continue the service while you are fighting with Medicare.
Additional Therapies and Services. We have said that Medicare will cover skilled nursing care, physical therapy, or speech therapy at home. But that’s not all you can get. You know the old song about love and marriage going “together like a horse and carriage … you can’t have one without the other”? Well, it’s true for Medicare home-health-care coverage, too.
If you are receiving part-time or intermittent skilled nursing care, physical therapy, or speech therapy at home, Medicare will also pay for:
• Occupational therapy
• Home health aides
• Medical social services
• Medical supplies
• Durable medical equipment (80% of approved amount)
We have already talked about occupational therapy in our discussion of SNF coverage; the same rules for coverage apply for home health care too. Durable medical equipment is discussed here. Home health aides and medical social services deserve special attention here, because these resources offer a true Golden Opportunity for important care.
Home Health Aides. A home health aide can provide any service, even unskilled service, but the aide must be from a Medicare-certified home-health-care agency. Medicare will cover personal-care services that are a “reasonable and necessary” part of your treatment, and the doctor must say so. The care provided by the aide need not be skilled, although you must also be receiving skilled care.
“Hands-on” care needed to recover or maintain your health can be covered. The doctor’s written plan of care must specify how often the home health services are needed. For a better feel for Medicare’s “rules of the game” for home health aides, here is a list of five common services that are covered.
PERSONAL CARE SERVICES. For example, bathing, dressing, feeding.
EXAMPLE 38
Mrs. Sax has a colostomy. Owing to complications, an LPN visits twice a month to monitor her condition. Because of arthritis, Mrs. Sax also has difficulty changing the colostomy bag. Her doctor orders home-health-aide services to perform this task. Because the care is reasonable and necessary to maintain Mrs. Sax’s health, and she is also receiving skilled care, Medicare should pay for the home health aides.
SKIN TREATMENTS. These are treatments not requiring skilled care (e.g., applications of ointments, simple bandaging tasks).
EXAMPLE 39
Mr. George recently had surgery. The incision is healing, but requires regular cleaning and rebandaging. Because of the location he can’t do the job himself. If he also needs skilled services, Medicare should cover a home health aide to care for the incision.
ASSISTANCE WITH MEDICATIONS. These are usually self-administered, or are medications that don’t require a skilled nurse to be given safely.
EXAMPLE 40
Mr. Fried is diabetic, and his vision is also impaired. A home health aide is needed to prefill his insulin syringes. (Note: Some state laws require a skilled nurse for this task.) This service should be covered.
ASSISTANCE WITH ROUTINE THERAPEUTIC EXERCISES. These exercises must enhance skilled therapy services.
EXAMPLE 41
As a result of a stroke, Mrs. Southers has suffered a loss of speech and arm mobility. Although she receives skilled therapy, she also needs to practice routine, repetitive exercises twice a day. Assistance is necessary, but she lives alone. A home health aide is called in to help. Guess what? It should be covered!
OTHER INCIDENTAL NONHEALTH-RELATED SERVICES. So far we’ve been talking about a home health aide providing health-related services. But can you get coverage if the aide also helps with nonhealth-related activities (e.g., meal preparation, light cleaning, etc.)? The answer is yes! Incidental nonhealth services can be provided and covered as long as this type of assistance is not the sole reason for the visit—the aide must also have a health-related task.
WARNING: DON’T GET GREEDY
The need for a home health aide must be linked in some way to your medical treatment, and the frequency of visits must be reasonable. If you are using a qualified home health aide, Medicare will not pay for more than 35 hours of total home-health-care services (skilled and unskilled) per week. We all would like household help seven days a week, but unless you can prove it’s essential for your condition don’t expect Medicare to clean up after you!
Medical Social Services. Medicare should cover services needed to help you respond to the social and emotional problems that arise from an illness. A medical social service professional will assess your situation and develop a plan of care to address your specific needs. If the professionals you deal with are Medicare-certified, your care should be covered.
EXAMPLE 42
Seventy-eight-year-old Mr. Epton has heart disease and hypertension. His doctor is concerned because Mr. Epton is not eating properly. He also can’t afford the medications needed to maintain his health. A medical social service worker is called; she assesses Mr. Epton’s situation and develops a plan of action that links him with available community resources for food and medical assistance. Medicare will pay because the doctor could document that the medical social services provided were “reasonable and necessary.”
GEM: Get the Care Provider to Confirm That Social Services Are Medically Appropriate for You
Medical social services are a prime target for denials. It’s not enough to know that a service generally is “covered.” Try to get the care provider to verify that the specific services that you are or will be receiving are “medically appropriate” for you. It’s always better to know ahead of time whether Medicare will pay for the service; you may decide that a particular social service isn’t worth the cost if it will be coming out of your pocket!
MEDICARE PART A: HOSPICE CARE
Thankfully, Uncle Sam comes through by subsidizing hospice care, which involves specialized services for terminally ill patients and their families. The focus of this care is pain relief, symptom management, and supportive services. Hospice programs can be operated by public or private agencies.
Uncle Sam has recognized that standard Medicare benefits are not adequate for the special types of care needed for a terminal illness. In this situation—comfort and convenience must also be considered. Costs for pain medications and a variety of support services not usually paid for by Medicare will be covered if, according to The Medicare Handbook (page 17):
• A doctor certifies that the person is terminally ill.
• The person chooses to receive hospice coverage instead of regular Medicare coverage.
• The care is being provided by a Medicare-participating hospice program.
• An oral plan of care is developed within two days of entering the hospice and a written care plan is signed within eight days of entering the hospice. The plan will need to be created by an interdisciplinary group that includes a doctor and other health professionals (nurses, social workers, counselors). The care will be based on this plan and reviewed regularly.
When you choose hospice care, Medicare requires that you waive your rights to services other than hospice care. What does this mean for you? It sounds worse than it really is. While generally you would be denied medical care when receiving hospice benefits, you may switch from hospice to standard Medicare coverage if you require treatment for another ailment (unrelated to your terminal illness). The intent of this distinction in coverage is to limit the treatments you receive under hospice benefits to those appropriate to hospice care—pain and symptom management. Invasive, cure-oriented treatments are not included under hospice coverage, but will still be paid under your standard Medicare coverage.
Why Choose Hospice Coverage?
As you will see, when you elect hospice coverage a broader range of services for your terminal illness are paid for by Medicare than under standard Part A benefits. Table 4.12 lists hospice benefits.
TABLE 4.12
Hospice Services Covered by Medicare
• Nursing services (care does not have to be skilled).
• Doctors’ services (related to the terminal illness).
• Drugs (when used mainly for pain relief and symptom management).
• Medical appliances and supplies needed to promote self-help or comfort when specified in the care plan.
• Therapies (physical, occupational, and speech pathology) when needed to help maintain basic functions or daily living activities.
• Home health aide and homemaker services to provide personal care (e.g., bathing, grooming) and other services needed to keep a patient’s environment safe and clean (e.g., light cleaning, linen changing, laundering).
• Around the clock care by nurses or aides during a medical crisis when needed to keep the patient at home.
• Respite care and short-term inpatient care. To provide time off for a caregiver, the patient can be admitted for up to five consecutive days (day of discharge does not count as a day) to a participating hospital, hospice, inpatient unit, or SNF that meets Medicare’s hospice requirements.
• Counseling for the patient, his or her family or other caregivers for a variety of purposes, including psychological counseling (to help with the emotional and physical issues related to terminal illness) and nutritional counseling (to provide dietary guidance and training). Although bereavement counseling after a patient’s death is not covered by Medicare, many hospices do offer this help.
Source: The Medicare Handbook, page 17.
GEM: Get More Than One Respite Stay
Table 4.12 shows that Medicare will pay up to five days in a hospital, hospice, or nursing home in order to give a caregiver a break. Five days isn’t much time, but there’s a loophole. Although the Medicare law states that you can only receive Medicare respite benefits for up to five days, the law does not specifically limit how many five-day respite visits you can have. The question of whether you get one or 10 respite breaks is left to the Medicare Intermediary. Check this out, and challenge anyone who tells you that you don’t “deserve a break today.”
* * *
What Will Medicare Pay for?
You are entitled to receive hospice benefits for 210 days (two 90-day periods followed by a 30-day period), but you can be “recertified” for an unlimited extension. In other words, you should be able to continue hospice coverage as long as necessary. You don’t need three days of hospitalization, and you don’t have to meet a 60-day waiting period in order to be eligible.
Unlike the standard Medicare program, you won’t need to pay any deductibles before hospice coverage begins. You will only have to pay:
• Drugs—5 percent of the cost of each outpatient drug or $5 (whichever is less).
• Inpatient respite care—5 percent of the Medicare allowed rate (about $4.53 a day in 1992).
How Do You Enroll?
To begin receiving hospice care, you (or a representative) must file an election form. Each hospice has its own form, so you will need to obtain and return it to the hospice you have chosen.
You can decide what date you want your coverage to start on (the first day you enter or any date after), but once you turn the meter on, it will run continuously from one benefit period to the next (and you won’t get Medicare coverage for any services unrelated to your terminal illness) unless you say stop.
How Do You Revoke Coverage?
You can change your mind at any time, stop hospice benefits, and return to regular Medicare Part A coverage. Again, you will need to file a form (ask the hospice) that states the date you want your coverage to end. You can reenroll at a later time.
EXAMPLE 43
Mr. Thompson had received hospice care for 60 days when he was hospitalized for treatment of a condition unrelated to his terminal illness. Because of the level of care needed, his family decided to return to his standard Part A coverage. Upon discharge from the hospital, he resumed hospice care.
MEDICARE MEDICAL INSURANCE (PART B)
Just in case Medicare Part A didn’t totally confuse you, Uncle Sam created Medicare Part B to have a second chance at completing the job.
Medicare Part B is a voluntary supplemental medical insurance program. Unlike Part A, which you get for free at age 65 when you start receiving Social Security benefits, you must pay for Part B coverage. If you have trouble remembering which is which, think “B is for BUCKS”!
The basic design of Medicare Part B is like any private health insurance policy. You, the beneficiary, must share the costs for the services you receive by paying premiums, deductibles, and co-insurance. The difference is that your partner is the Government. And with Uncle Sam, rest assured there is no free lunch. Medicare will buy you the basic no-frills sandwich (hold the lettuce and mayonnaise), and any extras will come out of your own pocket.
In a nutshell, Part B covers the “leftovers” from Part A. The three main categories of Part B coverage are:
• Doctors’ care
• Outpatient hospital care
• Other medically necessary services and supplies
Table 4.13 lists the common Part B covered services. To simplify the chart’s use, we have divided it into three coverage categories: persons, places, or things.
Eligibility
The eligibility requirements are very basic. You can buy Part B coverage if you are a 65-year-old American citizen. You do not have to be healthy to be accepted. Uncle Sam is an “equal opportunity insurer.”
GEM: Get Part B Even Without Part A
You can and should enroll in Part B even if you are not eligible to receive Social Security or Part A benefits. Although there are many gaps in the coverage, for the price you pay Part B is still a wise investment. (Of course, you won’t need Part B if you are already covered under other insurance—for example, through your employer.)
GEM: Get Part B to Get Medigap Coverage
Medigap or Medifil policies, as the names imply, are private insurance policies created to fill the many gaps in your Medicare coverage. If you haven’t signed up for Medicare Parts A and B, you aren’t eligible to purchase a Medicare supplement policy because you have a giant hole in your basic health insurance that can’t be filled by a Medigap policy.
* * *
Enrollment
Enrollment in Part B is similar to enrollment in Part A. If you will be receiving Social Security or Railroad benefits starting at age 65, you will automatically be enrolled in Medicare Parts A and B. Your Medicare card will come and will show that you have Part A benefits and you will be billed for Part B premiums. Your coverage will begin on the first day of your birthday month (e.g., if your birthday is February 27, coverage will begin February 1). If for some reason you don’t want Part B benefits, follow the instructions that come with the card.
TABLE 4.13
Medicare Part B Covered Services*

If you take early retirement Social Security or Railroad benefits, you won’t be entitled to Medicare until age 65. But again you don’t have to worry about applying; you should be enrolled automatically in both Parts A and B at age 65.
If you start receiving Social Security or Railroad benefits after age 65, and you elect to delay Medicare until that same time, your Social Security or Railroad benefits application will automatically trigger your application for Medicare Parts A and B at that later date.
If you delay Social Security or Railroad Retirement, but want to start taking Medicare at age 65, you must apply for both Medicare Parts A and B. And whenever you apply on your own, you must act early; delay will increase your premiums and leave you without coverage.
EXAMPLE 44
You are turning 65 and don’t plan to retire until 70, but you want to begin Medicare Parts A and B as soon as possible. Don’t assume that you automatically get Medicare at 65; that would be a costly mistake. When you delay Social Security past age 65, you must apply for Medicare if you want coverage to start at 65.
You can enroll for Medicare as early as three months before your birthday month (e.g., if you were born on July 20, April 1 will be the first day you will be eligible to apply). Don’t include your birthday month when counting back three months. Refer to Table 4.4 to see the earliest date you can apply.
GEM: Enroll at the Earliest Possible Time So That You Don’t Lose Coverage
If you apply for Medicare three months before your birthday month, your benefits will start promptly on the first day of your birthday month. In fact, if you apply one or two months before your birthday month—or even in your birthday month—Medicare benefits should start in your birthday month. But that’s not guaranteed; processing delays might cause your benefits to start one to three months late. See Example 45.
EXAMPLE 45
Your birthday is June 15, so you could apply for Medicare as early as March 1. When you apply then, Medicare (Parts A and B) can start promptly on June 1. But “if you snooze, you may lose.”
Let’s say, you wait until May 15 to apply. Owing to processing delays, your Medicare Part B coverage may not go into effect until July 1. Oh well, can a few weeks really matter? You bet! On June 10 you become very ill and incur medical bills of thousands of dollars. Your delay will cost you a bundle!
* * *
If you wait until your birthday month or after to apply, you will definitely lose coverage. Your Part B insurance will not start at the earliest date you became eligible. Table 4.14 shows the delays based on the date you apply, and Example 46 shows how to use the table.
TABLE 4.14
Starting Dates for Medicare Part B Coverage
If You Apply |
|
Medicare Part B Coverage Will Begin* |
|
||
3 months before your Month of Birth (MOB) |
|
1st day of MOB |
MOB |
|
1 month after MOB |
1 month after MOB |
|
3 months after MOB |
2 months after MOB |
|
5 months after MOB |
3 months after MOB |
|
6 months after MOB |
4 or more months after MOB |
|
Much later |
|
||
*Part A coverage works on a different, “no penalty,” time schedule and coverage will not be delayed.
EXAMPLE 46
Your birthday is April 15, so your MOB is April.
If You Apply in: |
|
Coverage Will Begin: |
|
||
January, February, or March |
|
April 1 (unless delayed by Medicare bureaucracy) |
April |
|
May 1 |
May |
|
July 1 |
June |
|
September 1 |
July |
|
October 1 |
After July |
|
Much later |
If you apply late, you are asking for disaster.
EXAMPLE 47
Your 65th birthday is April 29, but you don’t apply for Medicare Part B until May 15. Why sweat over a few weeks? Unfortunately, you become ill on April 20. Your medical bills, totaling hundreds of dollars, are not covered. Start sweating—because your Medicare Part B coverage doesn’t start until May 1.
The period starting three months before your birthday month, and ending three months after your birthday month, is called your “initial enrollment period”; that’s the best time to apply. By missing this initial enrollment period, you will not be allowed to enroll in Part B until the next “general enrollment period,” which runs from January 1 through March 31 each year. General enrollment is for people who either never applied or for those who dropped out and want to reenroll. (You can reenroll an unlimited number of times.)
When you apply in a general enrollment period, your Part B coverage will not begin immediately; you must wait until the following July 1. As you can see, by delaying you are risking financial disaster.
EXAMPLE 48
Your 65th birthday is April 29, but you don’t apply for Social Security, and you forget to apply separately for Medicare until September. Since you missed your initial enrollment period, you can’t enroll in Part B until the following January, when the next general enrollment period begins. You’ll need to make a second visit or call to Social Security then. And your Part B coverage won’t start until the following July. Better stay healthy!
We previously told you that if you wait until after age 65 to retire, your Social Security application at that time will automatically sign you up for both Medicare Parts A and B. Your Part A coverage begins promptly (as soon as your papers are processed). But because you missed your initial enrollment period (3 months before and after your 65th birthday month), your Part B enrollment will be considered to occur on the following January 1, during the next general enrollment period. And that will delay your coverage.
EXAMPLE 49
Alice Green became entitled to Social Security when she turned 65 in April. But because she was still working in a small family business and had medical insurance through her job, she didn’t apply for Social Security until the following September, when she left her job.
Ms. Green’s Social Security application enrolled her in Medicare Parts A and B. But because she missed her 7-month initial enrollment period (which ended on July 31, three months after her birthday month), her application now falls under the general enrollment rules, and her Part B coverage won’t begin until the following July 1.
She’d better not need expensive medical treatment before July. If she does, she may kiss her retirement nest egg goodbye.
GEM: Make Medicare Work for You: Apply for Medicare at 65, Even When You Don’t Retire
You can avoid disasters due to Medicare coverage gaps by applying for Medicare at the time or before you reach 65, even if you plan to keep working and you’ve got medical insurance at work. Otherwise, you could wind up without Medicare Part B for months after you retire.
GEM: Avoid Late Enrollment Disasters With Special Enrollment Protection
Take a look back at Example 49. If Alice Green had worked for an employer with at least 25 employees, and she had been covered by the company’s group plan, she should get “special enrollment protection” to avoid late filing disasters. This special protection allows a retiree to pick up Medicare Part B coverage immediately after leaving a job. Check with the company benefits supervisor about how and when to file for this special benefit.
GEM: Enroll at the Earliest Possible Time to Save on Premium Costs
Loss of coverage isn’t the only price you’ll pay for late enrollment in Medicare Part B. In addition, after age 65, for each full year (from your birthday month) you could have enrolled but didn’t, your monthly premium will be increased by 10 percent. For example, if you turned 65 in April 1991 but waited until June 1992 to enroll, your premium will be $34.98. Medicare math calculates as follows: $31.80 (1992 premium) + $3.18 (10% penalty for one-year delay) = $34.98. To put it simply, time is money—don’t wait!
* * *
Application Process
Three months before your 65th birthday, visit or call any Social Security office. (Look in the blue pages of your phone book. You will find the number listed under the U.S. Government heading.) If you are phoning, state that you want to apply for Medicare Part B. You might be able to complete most of the process over the phone. Whichever way you choose to apply, be prepared to provide the following information:
1. What is your age? Now is definitely not the time for coyness! You will need to submit proof; find a birth certificate or hospital birth record. Other documents are also okay, but ask.
2. What is your Social Security number? Don’t panic if you’ve lost your card or can’t remember the number. A replacement can be obtained from Social Security, and there are also ways to track down a number (e.g., old income tax or payroll forms).
3. What was your income for the past year? Dig out your W-2 form or copy of income tax return.
4. What other benefits are you entitled to? (e.g., Military, Railroad Retirement, Federal Civil Service). This information is used in order to coordinate coverage.
The Application for Hospital Insurance is Form SSA-18F5, which you can get from your local Social Security office. Look it over and if you have any questions, call your community’s Office on Aging or a local senior citizen center. It might be faster than trying to reach someone at Social Security. (To locate, look in the blue pages of your phone book under City or County Government.)
End of Coverage
Your Part B coverage will continue uninterrupted unless one of the following happens:
• You file a form with Medicare stating you no longer want to participate. This can be done at any time. Your coverage will be cancelled on the last day of the month after the month you filed. This means if you notified Medicare in May, the last day of your coverage will be June 30.
• You don’t pay your premium. If your payment isn’t received on time, you are out of luck and insurance. (This is a good reason to have premium payments deducted from your SSA check.)
• You die. (If you really want to terminate coverage, the first option is a less drastic choice!)
GEM: Try Not to Miss a Premium
Failing to pay premiums within the grace period can be very costly. After your Medicare Part B is cancelled, you can reenroll. But you’ll have to wait until a new general enrollment period. Your coverage won’t begin again until July 1. And you’ll have to pay a higher premium. If there’s any way to get the funds to pay the premium (e.g., borrowing from a child, taking a loan against a retirement fund), do it. Try not to let your insurance lapse.
* * *
What You Pay When You Have Part B Coverage
Part B “ain’t” free. Your basic Part B costs will always be:
• Monthly premium. In 1992, the monthly charge was $31.80.
• Annual deductible. At the start of each year, you must pay the first $100 in approved charges before Medicare Part B coverage will begin.
• Co-insurance. Medicare usually requires that you pay 20 percent of the approved cost of any covered service.
• If the doctor does not accept assignment, you can be required to pay the difference between your doctor’s actual charge and Medicare’s approved charge, up to 20 percent of the Medicare-approved amount.
GEM: Deduct the Costs
Just like other purchased medical insurance, costs of Part B are tax deductible.
* * *
Under Part B, it’s not enough to know the price of the supply or service. To determine your expenses, you must also know whether or not the provider accepts assignment. Not understanding the difference could cost you big bucks!
What Is Assignment?
When a doctor or supplier “takes assignment,” it means he has agreed to accept Medicare’s approved charge as full payment, even if his usual fee for that service or supply is higher. (See here for a more detailed explanation.)
How Does Assignment Work?
Accepting assignment is voluntary:
• Some providers always accept assignment
• Some providers don’t usually accept assignment but will make exceptions
• Some providers never accept assignment
Doctors and suppliers who always accept assignment are called participating providers. Participating providers have signed an agreement in advance with Medicare that requires them to accept assignment on all claims for Medicare-approved services. If a doctor says he’s a participating provider, that’s good financial news for you.
GEM: Get “A Directory of Participating Doctors in Your Area”
This free annual directory lists all participating Medicare providers. For a copy call the Medicare carrier in your state. (To find the phone number of the carrier, see Appendix 17.)
* * *
Some providers have not signed a contract with Medicare, but will accept assignment on a case-by-case basis. Since providers are not required by any law to work with Medicare, the decision is solely up to them. However, there is nothing illegal about trying to influence their choice. In this situation, your job is to take time out from Medicare Monopoly to play “Let’s Make a Deal.” If you like your doctor and have had a good working relationship, it is well worth your time to discuss assignment with him or her.
GEM: Negotiate Before the Bills Pile Up
You will be in the best position to ask the doctor or supplier to accept assignment before you incur some big bills. Don’t wait.
Successful negotiating requires:
• Knowing what you want.
• Stating these needs clearly.
• Leaving room for discussion to avoid creating a “win-lose” situation.
Ideally, your first choice is to have the physician agree to accept assignment for all Medicare-covered services provided. If the doctor turns down this opportunity, move on to your second choice: request that he accept assignment for specific treatments, especially high-cost procedures.
If this, too, is unacceptable, you must decide whether you want to continue as a patient or find a doctor who is a Medicare participating provider. Only you can decide what is best. Stay calm and shift to your third option: requesting his advice. Perhaps your doctor can recommend someone who does accept assignment. Bring along a copy of “A Directory of Participating Doctors in Your Area” and show it to your physician. He or she might recognize some peers—and maybe even feel guilty! At the very least, once you have found a new physician, it would be nice to have your doctor’s support in paving the way for a smooth transition (e.g., sending your records promptly, discussing your case history with the new provider) before an emergency arises. Ask.
* * *
There are very good reasons why you want the doctor to accept assignment, but what’s in it for him? Would you call being given the opportunity to deal with Medicare an “offer too good to refuse?” So, what enticements can you offer a doctor to get him or her to accept less money? The advantage of direct and electronic payment from Medicare might be appealing since it reduces paperwork and billing costs. But there are no pat answers. The following five strategies should help.
Game Strategies for Negotiating with Your Doctor
1. Be positive. Now is the perfect time to become a “stroke patient”—let your doctor know how much you have appreciated his or her care and service. Doctors enjoy having their egos stroked as much as the next guy.
2. Offer to be a responsible patient. Acknowledge that you understand the assignment process. Let the doctor know he can count on you to keep your part of the bargain. In exchange for his agreement, you promise to:
• Pay your Part B 20 percent co-insurance promptly for all services.
• Show flexibility. Perhaps the doctor has suggestions to cut costs, or ways you can work more efficiently together.
3. Choose the right time to talk. Timing can be everything. Catching your doctor at the end of a long day probably reduces the odds of having a receptive audience. If your physician has an office manager, try soliciting his or her support. Explain the purpose of your meeting and ask what time would be most convenient and what suggestions the person might have—perhaps she or he even knows what reasoning would be most persuasive. Try to arrange a personal meeting rather than a phone call.
4. Be a good listener. The bottom line is, the final decision rests with the doctor. You need to use common sense. If it is clear that your doctor is unmoved and unwilling to cooperate, there’s no point in creating ill will by pushing the issue. Thank him, ask for his suggestions, and leave. If, however, he seems to be against the idea but “swayable,” hang in there. Many doctors have a knee-jerk negative reaction; they automatically assume Medicare reimbursement is far too low. Perhaps he may conclude that accepting assignment for some services will not lead to financial ruin. (After all, the doctors who do accept assignment are maintaining practices.) Use the fine art of gentle persuasion to help him feel good about “doing the right thing” by accepting assignment.
5. Take the informed patient’s pledge. To help you scout out the important answers you need from your doctor, we offer an “informed patient’s pledge for action.” By following the guidelines listed below, you will improve the odds for success (at the very least, you’ll earn a merit badge from us!).
I promise to:
• Be prepared.
• Be polite.
• Be brief.
• Believe in the rightness of my request.
This means that you must do your homework. If you are discussing a specific treatment, find out beforehand what Medicare’s “approved charge” is and what your doctor’s fee will be. Perhaps the doctor is just not aware of the difference it can mean to you in out-of-pocket expenses.
* * *
You have the right to strive for the best quality care at the best price. Seeking a health care partnership with your doctor is not unreasonable. You don’t need to apologize for being a good consumer.
If you are a female with a male physician, this last point is especially important to keep in mind. Many women feel uncomfortable being assertive. If you are widowed, and your late husband used to take care of all the “big” decisions, it can be especially difficult, because speaking up for yourself is a new role. But if you expect your doctor to step in and play the part of “Doctor Knows Best,” you gain a false sense of security. In exchange for being “taken care of,” you will be treated like a “good little girl” who should be seen and not heard. You lose control over your health care because you have a parent-child relationship and not a partnership.
If the idea of speaking up makes you nervous, it will help if you practice your presentation before you visit the doctor. Ask a friend to role-play with you: she gets to “play doctor” and raise possible responses to your request. When you are comfortable with the “script” before “opening night,” it is easier to focus on the issues rather than your anxiety. It’s perfectly okay to admit to your doctor that this is new for you, but extremely important. You are likely to gain a physician’s respect, not disdain. The more often you take “the lead,” the easier this type of discussion will become.
GEM: There’s a Good Chance Your Doctor Is Overcharging You!
Lots has been said about excessive health-care costs and the need for cost containment. Yet there’s already a law on the books limiting health care costs, and the Government has kept it a secret.
Even if your doctor does not accept assignment, he or she cannot bill you (assuming you are a Medicare beneficiary) more than 20 percent over the approved Medicare fee. In 1993, the limit drops to 15 percent, reducing doctors’ charges even more.
The Explanation of Medicare Benefits (EOMB) you receive shows the Medicare-approved amount for the service. Then add 20 percent (15% in 1993) to figure the maximum allowable charge.
EXAMPLE 50
The doctor bills you $200, but the EOMB shows the approved fee is only $100. The doctor legally can only charge $120—20 percent above the Medicare approved fee. Medicare will pay $80 (80% of its approved fee), and you pay $40 ($120 minus $80). If you have Medigap or Medifil insurance, the insurance should pay $20 (20% of the approved amount), leaving you a bill of only $20 to pay.
Many doctors are charging too much, often because they don’t understand the law. To make matters worse, the Government has not been enforcing the law vigorously or educating the public. In many cases, in fact, personnel in the federal Health Care Financing Administration (HCFA), which oversees the Medicare program, have mistakenly told Medicare recipients to pay their entire bills—even when the fees charged exceed legal limits!
But this is beginning to change. Thanks to publicity by various public interest groups, including the American Association of Retired Persons (AARP), HCFA is starting to clamp down. If you are overcharged, contact the carrier. If you don’t get your bill reduced, try the state attorney general next.
GEM: Collect for Past Overcharges
Medicare recipients have been charged millions of dollars over the legal limits we’ve just described. Are you entitled to a refund if you’ve overpaid your doctor?
This question has not yet been answered. As we read the law, Medicare beneficiaries should have a right to reimbursement. But so far the Government has not taken any steps to make sure prior overcharges are repaid to patients.
Until the Government does something, you will only be able to collect through private action. Contact an attorney experienced in Medicare claims for assistance.
* * *
Now it’s time to look at services covered under Medicare Part B. These services—offered at a reasonable premium (at least as far as insurance goes)—provide a Golden Opportunity to secure basic health care for older Americans.
MEDICARE PART B: COVERED DOCTORS’ SERVICES
What Services Does Part B Cover?
The Medicare Handbook provides a summary of the major covered doctors’ services under Part B. For convenience, we have reproduced the list in Table 4.15. However, don’t assume that just because the service you receive is listed in the table it is automatically covered. Remember, before Medicare will pay a penny, Uncle Sam will also look to see if, given the circumstances of your case, the service was all of the following:
• A covered service (it’s on Medicare list as an acceptable treatment for your condition)
• Medically reasonable and necessary for you
• Provided by a medical professional who was the “right man for the job” (someone qualified to perform that treatment)
Whenever a provider files a claim for Part B insurance, Medicare will send you a notice called the Explanation of Medicare Benefits (EOMB). The EOMB will tell you a number of things, including whether the claim meets Medicare’s rules for coverage and how much Uncle Sam plans to pay.
TABLE 4.15
Services Covered by Medicare Part B
• Medical and surgical services, including anesthesia
• Diagnostic tests and procedures that are part of your treatment
• Radiology and pathology services by doctors while you are a hospital inpatient or outpatient
• Treatment for mental illness (Medicare payments for outpatient treatment are limited)
• Other services which are ordinarily furnished in the doctor’s office and included in his or her bill, such as:
1. X-rays
2. Services of your doctor’s office nurse
3. Drugs and biologicals that cannot be self-administered
4. Transfusions of blood and blood components
5. Medical supplies
6. Physical and occupational therapy and speech pathology services
Source: The Medicare Handbook, page 20.
Table 4.16 lists services Medicare Part B will not cover.
TABLE 4.16
Services Not Covered by Medicare Part B
• Routine physical examinations and tests directly related to such examinations (except some pap smears)
• Most routine foot care
• Examinations for prescribing or fitting eyeglasses (except after cataract surgery) or hearing aids
• Immunizations (except pneumococcal vaccinations or immunizations required because of an injury or immediate risk of infection, and hepatitis B for certain persons at risk)
• Cosmetic surgery, unless it is needed because of accidental injury or to improve the function of a malformed part of the body
Source: The Medicare Handbook, page 20.
GEM: Playing the Name Game, or an Illness by Any Other Name Could Cost You Money
Although Tables 4.15 and 4.16 seem fairly straightforward, nothing is easy in the game of Medicare Monopoly. The way a doctor describes your illness and treatment to Medicare can mean the difference between reimbursement or denial of your claim.
Why? Medicare reviews your claim based on a complex coding system. Every illness and treatment in the book has been assigned a corresponding code. The codes are made up of three- to five-digit number combinations. Your doctor must play the name game and select the code that most closely matches your condition and the service provided. If he makes a careless mistake or doesn’t choose the most specific code available, you end up being penalized. Your claim might be denied because the illness doesn’t match the treatment. At the very least, reimbursement can be less than you are entitled to because Medicare will pay less for a less serious procedure.
Talk to your doctor about the name game—don’t be shy. Make sure he or she describes your care in the best way to maximize your coverage.
EXAMPLE 51
You have been experiencing stomach pains and your doctor determines that you have an ulcer. The general code for a gastric ulcer is 531; when writing up the diagnosis, your doctor must use those three numbers. But that’s not enough. Is there a hemorrhage or perforation? The answer must be represented by a fourth digit. Was there an obstruction? “Inquiring minds want to know” and so does Medicare; a fifth digit will tell all.
If your doctor ignores these details, Medicare will ignore you, too. Your claim can be denied simply because an inaccurate code was used. But don’t assume Medicare is going to inform you about the source of the trouble. Keep this in mind when you are denied payment for a service that should be covered. Check with your doctor’s office to make sure an accurate diagnosis code was used. A claim can always be refiled, and a wrongful denial can be appealed.
GEM: Diagnostic Procedures Must Be Provided Directly to You
To be reimbursed for diagnostic procedures, your doctor must provide the service directly to you, the patient. That means he or she must examine your warm body or be looking at a direct visualization of you (e.g., X-rays, tissue samples, electrocardiogram). A doctor can’t take credit for a service if anyone else does the work for him.
EXAMPLE 52
A hospital cardiologist interprets your X-ray, bills Medicare, and sends your doctor a report. Your doctor then reads the information, scans the X-ray, and bills you for his review. Sound familiar? Unfortunately, Medicare won’t pay. Medicare thinks that analysis should be included as part of the doctor’s service fee and will not allow a separate charge.
GEM: Before Surgery, Get a Second Opinion
When your doctor is recommending surgery, Medicare will pay for a second look. And in certain nonemergency cases, Medicare requires a second opinion. If you don’t obtain this and go ahead with the surgery, you can’t cut a deal with Medicare; you pay. Check with your doctor or hospital to see if the procedure in question requires a second look.
Your doctor can give you the name of another physician who is “second opinionated.” Or if you prefer, you can call your Medicare Part B carrier for names. Toll-free numbers are listed in Appendix 17. If you get a second opinion and the recommendations of the two doctors differ, and if Medicare thinks it’s essential, the costs for a third look will be covered. Any services necessary to make an informed evaluation are included. You won’t have to pay a deductible or co-insurance, either.
GEM: Watch Out for Concurrent Care Coverage (Otherwise Known as Multiple Doctor Disorder)
A complex medical condition often requires the expertise of several different specialists. There is no limit to the number of doctors you can use. But Medicare will only pay if your doctors can document that the extra care given was necessary and not duplicative. Claims for the same services provided by different doctors will be denied.
GEM: Who Cares Where You Get the Care?
Surprise! Medicare isn’t worried. If the service meets the coverage requirements, it doesn’t matter to Uncle Sam where the care is provided—the doctor’s office, your home, a mountain top—any location in the nation is fine. (Under very specific circumstances, care in Canada and Mexico also are covered—see your Medicare Handbook for the rules on care in a foreign country.)
* * *
What Doctors Does Part B Cover?
Not only must the type of service provided be acceptable to Medicare, but the type of doctor providing the service must also be okay. Doctors of medicine (M.D.) and doctors of osteopathy (D.O.) are acceptable; others may not be.
Dentists, optometrists, podiatrists, and chiropractors are sometimes acceptable; we’ll talk about these below. Christian Science practitioners and naturopaths may provide services to you, but they don’t pass for Medicare coverage.
GEM: A Doctor Must Only Perform Authorized Service
Even if the doctor is acceptable and the service is acceptable, there must be a match. Medicare will only pay if the doctor is performing a service he or she is legally authorized to offer. If you let your chiropractor operate on your knee, your friends will question your sanity and Medicare will question the bill.
* * *
Chiropractors’ Services. Don’t get “bent out of shape” when you read this. Medicare covers only one service provided by a licensed chiropractor: “manual manipulation of the spine to correct a proven subluxation” (misalignment or abnormal spacing of vertebrae). How can you prove you have this condition? An X-ray is required, but Medicare won’t pay for that. Medicare will only pay if the X-ray is by a “real” doctor (doctor of medicine or osteopathy).
Podiatrists’ Services. Treatment for injuries and diseases of your foot by a licensed podiatrist should be covered (e.g., hammer toes, bunions, in-grown toenails). But here’s a “rule of toe”: Medicare will not pay for any care it classifies as routine. If your podiatrist bills you for basic hygienic services—trimming your toenails, corns—you will foot the bill.
GEM: Get Coverage for Podiatric Service Related to Another Medical Condition
If you have a medical condition that affects your legs or feet (such as diabetes or circulatory disorders), the podiatric costs are considered necessary and should be covered. However, treatment for putting your foot in your mouth on a routine basis is not eligible!
Dentists’ Services. Medicare offers you very little when it comes to dental coverage. Even if this strikes a raw nerve, Medicare will still not pay for: cleanings, fillings, removal or replacement of teeth, root canals, or any surgical procedures related to your teeth or gums.
Medicare should pay for:
• Dental services provided in cases where your medical problem is more extensive than the teeth or the structures supporting them (e.g., you require surgery on your gums to remove a tumor).
• Hospital care if the severity of a dental procedure requires hospitalization. Your stay should be covered under Part A benefits even though the dental services are not eligible for reimbursement.
In summary, Medicare dental coverage is pretty toothless, and you will be too if you wait for Uncle Sam to pick up your dental bills.
Optometrists’ Services. You and Medicare probably won’t see eye to eye on coverage for eye care. Routine services such as eye exams, fittings for eyeglasses or contact lenses, and the eyewear itself are not covered. Medicare will only pay for:
• Prosthetic lenses that are needed to replace the natural lens of your eye.
• Eyeglasses required after cataract surgery.
• An optometrist to provide a service that is already covered by Medicare. The optometrist must also be licensed by the state to perform the service.
What Other Health Care Providers Are Covered?
Medicare should also lend a hand for certain services provided by other Medicare-approved practitioners, such as certified registered nurses, physician assistants, nurse practitioners, and clinical psychologists. Of course, there are specific requirements. The service generally must be:
• A Medicare-covered service.
• Supervised by a physician.
• Provided in a hospital, intermediate care facility, or SNF. (Nurse practitioner services are only covered when provided in an SNF.)
• An integral part of your prescribed plan for care.
Golden Rule: Generally, Medicare should contribute to the cost when the service would have been covered if a physician had provided the care.
Treatment and diagnostic services by Medicare-certified psychologists may be covered. You can receive psychological services as an outpatient at a hospital, rural health clinic, community mental health center, or HMO. However, Medicare does “shrink” from its responsibility when it comes to reimbursement. Only 50 percent (not the usual 80%) of approved charges are covered; you pay the rest. But talk can still be cheap (at least cheaper) because your Medicare-certified psychologist must accept assignment.
Services by Medicare-certified clinical social workers may also be covered, but the reimbursement is even less. Services provided to diagnose and treat psychiatric problems are covered when a doctor would have been covered for doing the same job. Medicare will pay a social worker up to 75 percent of the fee a qualified psychologist would have received, or the actual service charge (whichever is less). In all cases, accepting assignment is a must.
What Supplies and Drugs Are Covered?
Supplies, drugs, vaccinations, and biologicals (such as blood) may be covered by Medicare Part B. Table 4.17 shows when you can and can’t cash in. As the table shows, Medicare will pay for an inoculation against a specific, immediate harm. It’s nice to know that Uncle Sam will give you a shot in the arm when there is a clear-cut injury or health risk.
TABLE 4.17
Supplies, Drugs, Biologicals, and Vaccinations Covered/Not Covered by Medicare Part B

EXAMPLE 53
You step on a rusty nail and get a tetanus shot or you are bitten by a mad dog and receive anti-rabies treatment. Since these treatments are a response to a particular injury or risk, Medicare should cover.
But what if you know you will end up in an elevator filled with sneezing, coughing passengers at the height of flu season? Shouldn’t a flu shot count as an immediate risk? Tough luck! Medicare does not consider it a threat worth paying for, no matter how susceptible you are to the virus.
MEDICARE PART B: OUTPATIENT HOSPITAL SERVICES
Medicare Part B will help pay for outpatient care, at a Medicare-approved hospital, when ordered by your doctor. Charges for the use of the facility, nurses, and other aides, as well as any supplies necessary for treatment, should all be included. Tables 4.18 and 4.19 list the major outpatient hospital services covered and not covered by Medicare.
TABLE 4.18
Major Outpatient Hospital Services Covered by Medicare Part B
• Services in an emergency room or outpatient clinic, including ambulatory surgical procedures
• Laboratory tests billed by the hospital
• Mental health care in a partial hospitalization psychiatric program, if a physician certifies that inpatient treatment would be required without it
• X-rays and other radiology services billed by the hospital
• Medical supplies, such as splints and casts
• Drugs and biologicals that cannot be self-administered
• Blood transfusions furnished to you as an outpatient
Source: The Medicare Handbook, page 21.
TABLE 4.19
Sample of Outpatient Hospital Services Not Covered by Medicare Part B
• Routine physical examinations and tests directly related to such examinations (except some pap smears)
• Eye or ear examinations to prescribe or fit eyeglasses or hearing aids
• Immunizations (except pneumococcal and Hepatitis B vaccinations, or immunizations required because of an injury or immediate risk of infection)
• Most routine foot care
Source: The Medicare Handbook, page 21.
GEM: Bring Your Most Recent Explanation of Benefits
The outpatient facility will want to know if you have already met your $100 annual deductible before services are provided. They’ll want this information because if you haven’t met it yet, and the fee for treatment is less than $100, chances are you will be asked to pay the entire bill. So avoid delays and problems by bringing along your most recent Explanation of Medicare Benefits (EOMB) notice, which shows your deductible balance.
EXAMPLE 54
You have already paid $25 toward your Medicare deductible. This means you must pay for $75 in approved services before Medicare will even begin sharing your bills. If the charge for your outpatient care is going to be $100, you must pay $75 out of your own pocket ($75 + $25 = $100) to meet your deductible. Now that leaves $25 of service fees that you and Uncle Sam must divide: Medicare’s share will be $20 (80% of $25) and you must pay your $5 co-insurance (20% of $25 = $5).
This brings your total costs for the outpatient service to $80. By bringing along your EOMB (which shows how much you have left on your deductible), you will reduce your out-of-pocket expenses by $20 ($100 – $80) because the hospital can’t make you pay the full amount.
If you don’t have the EOMB and the hospital requests payment in full to cover the deductible you really don’t owe, the hospital should eventually refund the amount you overpaid. But who needs the added nuisance of keeping track of the I.O.U.? Wouldn’t you rather have that money sitting in your bank account instead of the hospital’s?
MEDICARE PART B: OTHER COVERED SERVICES AND SUPPLIES
This category of Medicare Part B coverage is a real potpourri; there are quite an assortment of services and supplies eligible for reimbursement. Read on and you are bound to uncover a gem or two.
Comprehensive Outpatient Rehabilitation Facility Services (CORF)
Medicare will help pay for services provided at a CORF when your doctor has certified that you need this type of care. You will still need to pay the $100 annual deductible and 20 percent of all Medicare-approved charges. Covered services include doctors; physical, speech, occupational, and respiratory therapies; and counseling. Mental health care provided by doctors, physicians’ assistants, or psychologists at a CORF are also covered, but Medicare will only pay 50 percent of the approved charges (not the usual 80%).
Ambulatory Surgical Center (ASC) Services
These centers can be independent facilities or affiliated with a hospital. Their sole purpose is to perform outpatient surgical procedures. Before going under the knife, you will want to make sure: (1) the facility is participating in the Medicare program; and (2) the surgery you are having is on Medicare’s list of approved outpatient procedures. If the answer to both of these questions is yes, Medicare’s answer to your bill should be “yes,” too.
Table 4.20 lists ASC services that should be covered by Medicare Part B.
TABLE 4.20
Ambulatory Surgical Center Services
Covered
• Physicians, nurses, and other technical personnel services
• Use of the facilities (e.g., operating and recovery room)
• Drugs, surgical dressings, splints, or other supplies necessary for the surgical procedure and aftercare
Not Covered
• Diagnostic tests; with the exception of simple urinalysis and blood work (which are usually included in the base price of your surgery), Medicare will not pay for any testing done at an ASC.
• Items such as ace bandages, support hose, and surgical leggings are not classified as surgical dressings. They are considered secondary coverings and Medicare does not pay for this layer of care.
Note: The services must be provided at a Medicare-participating center in order to be eligible for coverage.
Rural Health Clinic Services
These clinics are located in areas defined by the Census Bureau as rural and by the Secretary of Health and Human Services as being medically under-served. If you receive care from a rural health clinic, Medicare should help pay for:
• Physician’s services
• Nurse practitioners, physician assistants, clinical psychologists, and clinical social workers
• Services and supplies “incident to” the care provided by your doctor or any of the professionals listed above
• Visiting nurses when care by a home-health-care agency is not available
GEM: Get Coverage for Rural Services
Essentially, any services Medicare would cover in a doctor’s office or hospital should be covered when furnished at a rural health clinic. Clinics submit claims directly to Medicare. You pay any unmet annual deductible and the 20 percent co-insurance on Medicare’s approved charges.
* * *
Independent Clinical Laboratory Services
First, the good news: Medicare will pay the entire approved fee for diagnostic tests. Now, the better news: the lab must accept assignment and can’t bill you; the same goes for your doctor if he’s the one furnishing the test. Unfortunately, good news is always tempered by bad news when it comes to Medicare. The bad news is that the laboratory you use must be Medicare approved. Note that some laboratories are Medicare approved only for certain kinds of tests.
GEM: Check Out an Independent Lab for Medicare Coverage
You or your doctor must find out if the lab is covered for the test(s) your doctor is ordering. If you make the mistake of assuming that a Medicare-approved lab will cover all your lab tests, you could end up being stuck with more than a needle.
* * *
Warning: Government studies show that doctors who own their own labs tend to recommend more lab services than necessary. Before going for lab services, ask the doctor who advised you to go whether he or she has a financial interest in the lab.
Portable Diagnostic X-Ray Services
When your doctor orders X-rays “to go,” they should be covered when provided by a Medicare-approved supplier.
Other Diagnostic Tests and X-Rays
When your doctor orders medically necessary diagnostic tests to evaluate your condition, Medicare should help pay.
Radiation Therapy
Medicare should cover these costs when treatment is performed under your doctor’s supervision.
Kidney Dialysis and Transplants
Medicare has extensive rules and regulations concerning coverage. Refer to the Medicare Coverage of Kidney Dialysis and Kidney Transplant Services Guide, available from Social Security.
Ambulance Transportation
What are Medicare’s “rules of the road” for ambulance reimbursement? The path to coverage is bumpy; here’s a road map to follow:
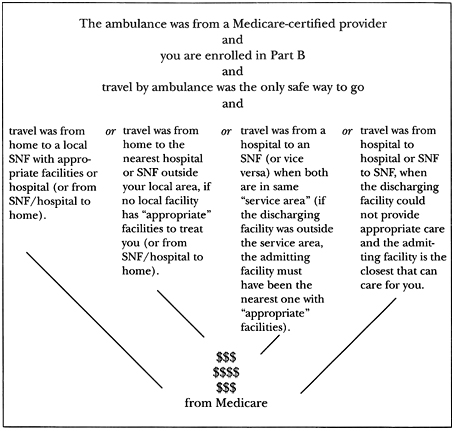
You will probably have to pay for a trip to the doctor’s office by ambulance. The only exception to this rule is if you can show that the service provided by the doctor was medically necessary and unavailable at the hospital or SNF where you were receiving inpatient care.
If the ambulance service was not a Medicare-certified provider, you are out of luck. There are no exceptions to this rule for coverage. If the company you used doesn’t fit the bill, you will pay the bill.
GEM: Find a Certified Ambulance Company Before You Need It
Now is the time to do your research—before you have an emergency. Check the yellow pages under the heading Ambulance Service—Emergency and Medical; find two or three companies serving your area with ads that include the words “Medicare Approved.” Call and confirm that they are, and that they service the medical facilities in your area. Write the phone numbers down and post with your other emergency information so that you’ll have it when needed.
* * *
Durable Medical Equipment (DME)
Medicare should help pay for durable (nondisposable) medical equipment like walkers and wheelchairs, but you’d better first read Medicare’s fine print because there’s a lot of it! Before Medicare will contribute to the costs, according to the Center for Medicare Advocacy, you must show that the equipment:
• Is prescribed by your doctor because it is a “necessary and reasonable” part of your home treatment program
• Can be used over and over
• Is no fun or comfort for healthy people
• Is appropriate for home use
• Is from a Medicare-certified provider
The DME must have a medical purpose. Medicare will not pay for any equipment designed particularly to make a healthy person’s life more pleasant, no matter how helpful it might be to you or your caregiver. This means that items such as room heaters, humidifiers, air conditioners, elevators, and seat boosters generally are no-go.
GEM: Bend the “No Fun Allowed” Rule
You may be able to get Medicare to show some flexibility and grant coverage for DME that is not primarily medical. But your doctor had better be able to clearly show that, in your case, the equipment is therapeutic and not purely for comfort.
EXAMPLE 55
A water mattress can be used by anyone to enhance a night’s sleep, but if your doctor prescribes one to help alleviate your severe case of bedsores, Medicare should consider its therapeutic value. The same goes for heat lamps, if (and only if) your need for heat therapy can clearly be proved as a necessary part of your home-treatment plan.
On the other hand, Medicare is completely cool to the idea of air conditioning as humidity and breathing therapy. No matter how helpful a lower room temperature would be for your overall health status, Medicare won’t pay because an air conditioner’s main use is nonmedical.
* * *
For the DME to be covered, those good old standards of “necessary and reasonable” must be satisfied, too. Medicare bureaucrats will ask questions like:
• Is the item really necessary for treatment or therapy to improve your functioning?
• Will the equipment make a significant difference in your health status?
• Are the therapeutic benefits worth the price, or is this the least expensive way to meet your needs? (Why buy a Cadillac when a Chevy will get you there?) Uncle Sam will do a cost-benefit analysis.
EXAMPLE 56
If you install a whirlpool to help your arthritis, enjoy it but don’t count on Medicare to help. The expense will probably be called unreasonable because a warm bath would work, too.
GEM: Chair Lifts—Raise Expectations but Buyer Beware!
Before renting or purchasing a chair lift, know the rules or you could lose your pants on the deal! In spite of what the ads say, Medicare won’t automatically pay.
The fact that one of these chairs would make your life more convenient isn’t enough incentive for Medicare to foot the bill. The same standards for DME coverage apply—the seat lift must be prescribed by your doctor as a reasonable and necessary part of your treatment. Its use must either improve or stabilize your condition so that you can avoid confinement to a bed or chair.
Also, in Uncle Sam’s eyes not all chairs are created equal. Don’t catapult yourself into debt by purchasing the wrong type of seat. Medicare will pay for a chair that enables you to safely stand or sit without help. Medicare will never pay for a chair lift that uses a spring release mechanism because the catapult-like motion can be dangerous. In any event, Medicare pays only for the lift mechanism, not the chair itself.
* * *
Once you and Medicare agree that the DME meets all the requirements for coverage, the next question is: “To buy or not to buy.” The folks at Medicare, not you, decide whether you rent or purchase the DME.
Medicare has divided all DME into six categories, which helps Medicare determine whether to pay for rental or purchase. The categories are described in Table 4.21. The amount of time you will need the DME should be a key factor in Medicare’s decision. When the doctor predicts that your needs will be short term, Uncle Sam is more likely to opt for rental.
In addition, Medicare has set a reimbursement price ceiling on fees for each category. When items are approved for rental, Uncle Sam will want to know the DME’s purchase price. He then checks his books to see if that exceeds his price ceiling for that category. The cheaper of the two prices (the supplier’s or Medicare’s) will become the base price; Medicare will then pay 10 percent of this base price directly to the supplier each month for rental costs.
TABLE 4.21
Medicare Payment Options for DME
Category of DME |
|
Form of Payment |
|
||
Inexpensive or routinely purchased rental equipment—items less than $150 (noncustomized power-driven wheelchairs are now included here) |
|
Lump-sum purchase or monthly |
Items requiring frequent servicing (any item that needs frequent care to assure safe operation, such as aspirators) |
|
Monthly rental |
Customized items (DME that must be adapted to meet your specific health needs) |
|
Lump-sum purchase |
Prosthetic and orthotic devices (items needed to substitute for a body part or internal body organ) |
|
Lump-sum purchase |
Capped rental items (“capped” means Medicare has put a limit on the length of time and amount of money to be paid: 15 months at 10 percent of the base price) |
|
Monthly rental (after 15 months, only maintenance and servicing fees reimbursable) |
Oxygen and oxygen equipment |
|
Monthly rental (rate of reimbursement based on local rates) |
If Medicare opts to pay a lump-sum payment for purchase, Medicare will calculate what it believes should be the “average reasonable charge” for the item in your neighborhood. It’s too bad if the actual price of the item is more; you will not get a higher level of reimbursement.
GEM: Don’t Buy Until Uncle Sam Says Yes
If you have jumped the gun and purchased an item, and then Uncle Sam decides it should be rented, too bad for you. Medicare will only contribute the approved monthly rental fee, and only for as long as the DME is needed or until Medicare’s approved purchase price is reached (whichever comes first). You will have to pay any additional money owed. Another downside to buying is that if you then die, Medicare will stop payments, no matter how much you still owe on the purchase. (Try to stick around just to break even!)
Before shelling out your money, call your Part B Medicare Carrier (Appendix 17) to find out how Uncle Sam wants to pay.
* * *
If Medicare decides that the DME should be purchased and you disagree, you can still opt to rent the item and Medicare will contribute to the fees, but only up to the equivalent of its “reasonable purchase price.” Find out what that amount is before making a final decision, because if you later change your mind and decide to buy, you will be penalized for not listening. Uncle Sam will not credit the entire amount of the money he’s been shelling out for rental to help purchase the item. You end up paying more.
GEM: Watch Out for DME “House Rules”
Medicare has “residency requirements” you must meet. If you’re not home enough, Uncle Sam will decide it’s not worth his money to rent supplies for you, and you will lose coverage.
EXAMPLE 57
You have rented an aspirator (with Medicare’s blessing). After three weeks of home use, complications arise and you enter a nursing home for a week. In this situation, because you were at your residence for part of the month, Medicare will contribute to the full month’s DME rental. But if you are out of the home for an entire month, Medicare will take a “use it or lose it” stand and won’t pay a penny.
* * *
Because DME falls under Part B, you are still responsible for paying a 20 percent share of the costs (co-insurance) and any unmet deductible. When this involves expensive equipment, your share could run into hundreds—even thousands—of dollars.
GEM: Negotiate If You Can’t Afford to Buy
What if Medicare says buy, but you can’t afford to? When a lump-sum payment is required and you can’t come up with your share of the lump, you can negotiate. Write to your Medicare carrier and explain why the money required would cause you “undue financial burden” (fancy Medicare language for saying you’ll go broke!). If no monthly installment plan can be worked out with the supplier, then the carrier must let you rent the equipment for up to three months while you figure out how to come up with the purchase money. The rental fees paid will then be subtracted from the purchase price.
What if you still can’t afford to pay your share? Medicare will tell you to prove it! You must show that:
• no other financial arrangements (e.g., charging or monthly installment plans) could be negotiated
• no cheaper sources were available
• no Medicare assignment was acceptable to the supplier(s)
If Medicare agrees, you will not be required to purchase the DME and your share will be based on a monthly rental plan instead.
GEM: Find an Accepting Supplier
Some suppliers accept assignment, others don’t. Cut your costs by finding a supplier that does.
GEM: A Better Bet—Buy It Used
When you buy any new DME, you are required to pay your 20 percent coinsurance. But if you get the carrier’s okay to purchase an item used, Medicare should let you off the hook, and you just pay any unmet deductible.
GEM: Don’t Forget Part A
The cost of doctor-prescribed DME may be paid entirely by Medicare under Part A. Check with your doctor about getting the necessary DME under Part A. Why? Under Part A, you pay no co-insurance. For example, let’s say you need a wheelchair. During your stay in an SNF, it is included. But what should you do when it’s time to go home? If the SNF is also a DME supplier, arrange to get the chair before you leave and you won’t have to pay any extra!
* * *
Nondurable items (items that cannot be used over and over) related to DME may sometimes be covered, too. Here are two gems to help you collect for items needed for the operation, maintenance, and repair of DME.
GEM: Get Repaid for Supplies and Accessories for DME
Nondurable items that are essential for the operation of your DME should be reimbursed by Medicare when obtained from a Medicare-approved supplier. You might be able to get coverage for oxygen or therapeutic drugs that are put into the equipment as part of your treatment (e.g., drugs used for chemotherapy and kidney dialysis). Your costs to replace essential nondurable parts, like mouthpieces or hoses, can also be shared with Medicare if you purchase or own the DME.
GEM: Collect for Repairs, Maintenance, and Related Costs
Nondurable items that are necessary to the upkeep and use of the DME may also be covered. Table 4.22 shows how.
TABLE 4.22
Repairs, Maintenance, and Related Costs for DME
Repairs |
|
|
• Covered |
|
Loaner costs—While your DME is in the shop, Medicare should pay for a substitute. |
• Not Covered |
|
Excessive costs—When it would be cheaper to rent or buy another one, Medicare won’t pay the repair bill. Abuse—If DME needs repair because you have purposely damaged or neglected to maintain it, you pay. |
|
||
Maintenance |
|
|
• Covered |
|
Complex tasks—When the instruction manual tells you a skilled technician is needed for the job, take their word for it because Medicare will pay. |
• Not Covered |
|
Routine tasks—Whatever owner maintenance tasks are listed in the instruction manual, Medicare figures you can manage. If you want someone else to do the work, that’s fine too, but you pay the bill. |
|
||
Replacement |
|
|
• Covered |
|
When DME wears out, is damaged beyond repair, lost, or no longer useful because of a change in your condition, a doctor can authorize replacement, at Medicare’s cost. |
• Not Covered |
|
If Medicare suspects you’ve abused or purposely lost the DME, sorry Charlie. |
|
||
Delivery and Service Charges |
|
|
• Covered |
|
Delivery charges on leased and purchased items should be covered if it’s the common practice to have a separate charge for this service. |
• Not Covered |
|
When Medicare thinks the supplier has already calculated the cost of delivering and servicing a DME in its price, you pay. For example, separate delivery charges for oxygen are usually denied unless the supplier has to travel outside his usual service area to deliver the oxygen to you and there is no other supplier available. |
GEM: Maintenance of Rental Items Used Beyond 15 Months
If you continue to require the DME beyond the 15-month rental time limit (see Table 4.21), Medicare will help pay for any service and maintenance not covered by a warranty once every six months. But you must have the work done during the first month of eligibility.
EXAMPLE 58
You start renting the DME on April 1, 1991. To be reimbursed for service and maintenance after 15 months, you must have the work done by September 1992 (six months after the 15-month rental cap, and every six months thereafter). If you procrastinate, you lose.
* * *
Prosthetic Devices
The bionic man would have been pleased to know that Medicare Part B covers the costs of a wide range of body repair and replacement parts. (Depending on the circumstances, coverage may also be provided under Part A.) Certain supplies, repairs, and replacements that enable you to use the prosthetic device effectively, and are integral to the operation of the prosthetic device, can be included too (e.g., batteries used in an artificial larynx). Tables 4.23 and 4.24 list some of the more commonly required “parts” that Medicare will and will not lend a helping hand to you with payment. Example 59 illustrates how this works.
TABLE 4.23
Covered Prosthetic Devices
• Artificial limbs.
• Body braces—e.g., arm, back, leg, neck.
• Internal body organs (e.g., corrective eye lenses needed after cataract surgery). Note: even if your own lens was removed before your entitlement to Part B benefits, a prosthetic lens received afterwards is covered. Also, prosthetic eyeglasses and contact lenses can be covered when your doctor states that they are medically necessary. But keep your choice of frames simple; Medicare sees no reason to pay the high price of “designer label” lenses.
• Breast prosthesis and surgical bras after mastectomies.
• Cardiac pacemakers. Medicare does have a heart and will cover the installation costs of an approved pacemaker. Uncle Sam will also pay for the followup visits to monitor you, but limits are set on how often. In most cases, “reasonable monitoring” is once a week for the first month; then every two months until 80 percent of the pacemaker’s life expectancy is reached (your doctor and Medicare decide this); and then monthly. Unless you can show “good cause” for more frequent monitoring (like your heart is skipping beats), Medicare will be skipping payments.
• Colostomy, ileostomy bags.
TABLE 4.24
Uncovered Prosthetic Devices
“See no evil, hear no evil, speak no evil—walk the path of truth,” but Medicare still won’t pay for these:
Vision |
|
Prescription lenses. Although these costs might be out of sight, glasses and sunglasses used to correct routine vision problems (e.g., nearsighted and farsightedness) are not covered. Cataract sunglasses. Medicare figures you can squint. Optician’s services. These are on your bill even if the visit was to fit or service prosthetic glasses (opticians are never covered by Medicare anyway). |
|
||
Hearing |
|
Hearing aids. What did you mumble? You think hearing is essential and should be covered? So far, Medicare has turned a deaf ear to requests for reimbursement. |
|
||
Speech |
|
Dentures. Bite your tongue, because no matter what you say, Medicare won’t pay (unless the dentures are an essential part of a medically necessary mouth reconstruction). |
|
||
Walking |
|
Orthopedic shoes. You will foot the bill. The sole exception is when shoes are an integral part of leg braces and their cost is included in the fee for the brace. (Medicare is currently paying for orthopedic shoes needed by diabetics with foot disease in a few states with demonstration projects.) |
EXAMPLE 59
As a result of permanent urinary incontinence, Mr. Walters needs a urinary collection and retention system. Medicare should pay for the Foley catheter (a nondurable component) as a prosthetic device because it is an essential supply to enable the urinary collection system to take over the bladder’s job. On the other hand, the rubber sheets, diapers, and antiseptic wipes Mr. Walters needs are helpful but not covered as prosthetic supplies because they aren’t integral to the urinary collection system’s operation.
Are prosthetic devices considered DME? As Table 4.23 showed, Uncle Sam sometimes says yes. But sometimes Medicare classifies prosthetic devices separately under Part B. Why does this matter? Because Uncle Sam might deny your perfectly legitimate claim simply because it was filed under the “wrong” code. To avoid frustration, check to make sure your doctor uses the correct Medicare vocabulary for coverage.
* * *
Navigating around the Medicare Monopoly board is like walking through a mine field. The tips we’ve provided should signal the mines and enable you to turn the Medicare mine field into a gold mine.