CHAPTER 8
Respiratory Monitoring
Operating Room Monitoring of Respiratory Function
One of the greatest risks of sedation and general anesthesia is respiratory compromise. Prior to any discussion of respiratory monitoring, it is important to define the terms ventilation and oxygenation. Ventilation refers to the bulk movement of gas in and out of the lungs, which in turn facilitates the elimination of carbon dioxide from the body. The anesthesia provider generally can control ventilation by changing the anesthetized patient’s respiratory rate or tidal volume. Oxygenation refers to the delivery of oxygen to the lungs and in turn to the blood and ultimately end organs. This is manipulated by changing the inspired fraction of oxygen (FiO2) and positive end-expiratory pressure (PEEP). Table 8.1 displays the normal values for monitors measuring ventilation and oxygenation.
Table 8.1. Normal Values for Monitors Measuring Ventilation and Oxygenation
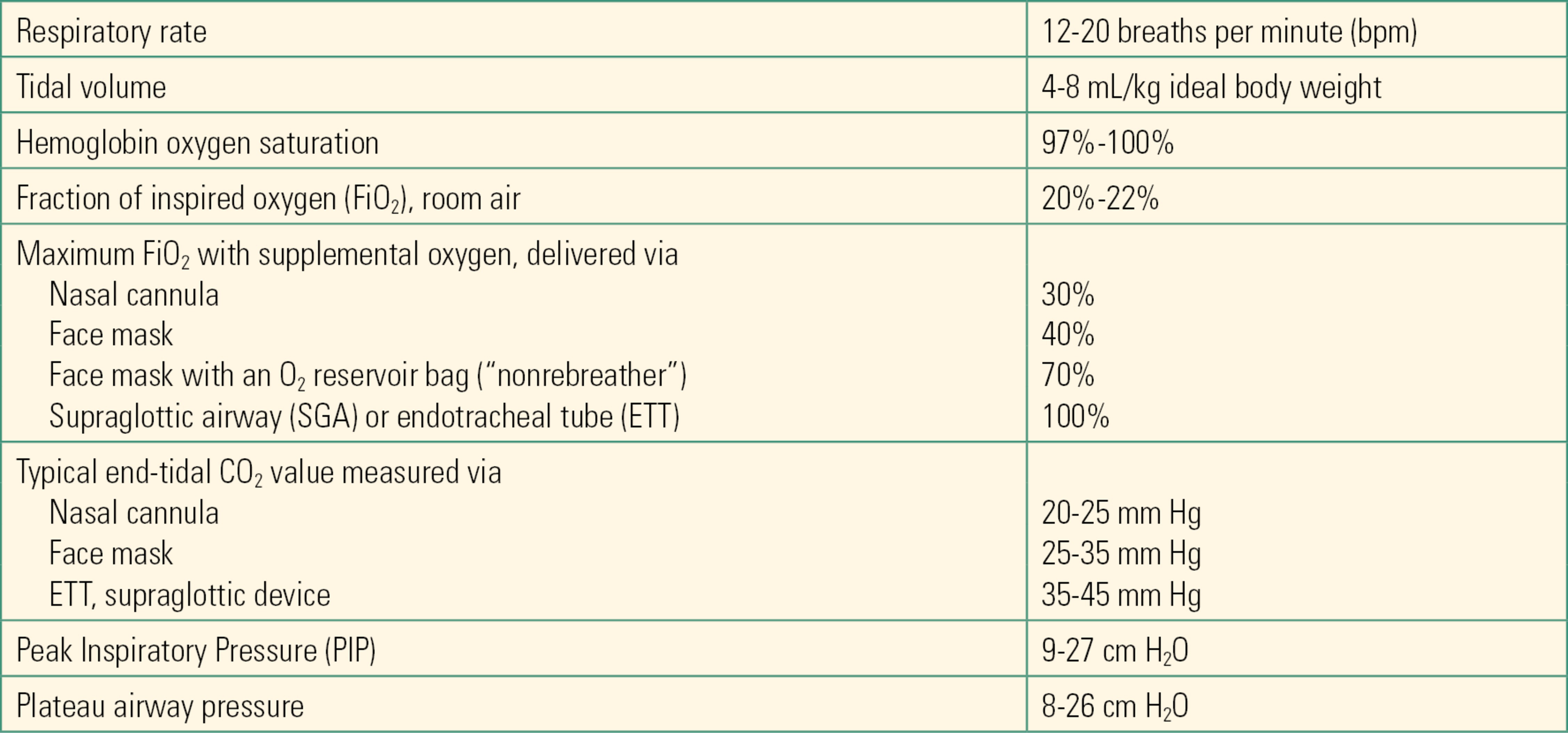
Monitors to track patient ventilation are needed in any anesthetized patient, particularly when the anesthesia provider is controlling ventilation with a mechanical ventilator. In this chapter, principles of assessing gas exchange will be discussed. Monitoring technology is covered in Chapter 31 (ASA Standard Monitors). Monitors of ventilation measure respiratory rate, tidal volume, and carbon dioxide movement out of the lungs, as well as respiratory mechanics, such as pressure, flow, and volume during mechanical ventilation. Monitors of oxygenation, such as pulse oximetry and arterial blood gas measurement, will also be briefly discussed. These topics are covered in depth in Chapters 31, ASA Standard Monitors, and 35, Point of Care Testing.
The Respiratory System and Acid-base Balance
The lungs participate in acid-base regulation of the blood by modulating carbon dioxide, that is, acid concentrations in the blood. Carbon dioxide is partially converted to carbonic acid in the blood and tissues and is an important contributor to the acid-base status of the body. Acid-base homeostasis may be determined in a patient by drawing an arterial blood sample from which pO2, pCO2, and pH can be measured. Chapter 10 presents a more detailed discussion of acid-base physiology. The lungs help to regulate pH through their connection to the brainstem. If the carbon dioxide level or blood acidity increases, the brainstem increases minute ventilation in an attempt to restore the pH to a normal physiologic value. As minute ventilation increases, additional carbon dioxide is eliminated from the body, lowering the amount of acid (increasing pH).
Normal values for arterial blood gases include
- pH: 7.35-7.45
- PaCO2: 35-45 mm Hg
- PaO2: (room air) 100 mm Hg
- HCO3−: 20-28 mEq/L
Ventilation
Breathing may be monitored utilizing many techniques including physical exam, visual inspection of a patient’s respiratory rate and chest excursion, or more objective measures such as impedance plethysmography, precordial and esophageal stethoscopes, flow meters, airway pressures, capnometry (the measurement of exhaled carbon dioxide), and measurement of arterial carbon dioxide tension. The respiratory rate may be monitored by watching the chest rise and fall. Chest movement indicates respiratory effort and rate, but it does not confirm gas movement into and out of the lungs. A patient may have the drive to breathe and his or her chest wall may be moving; however, there may be no gas flow into the lungs due to an obstruction of the upper airway. Obstruction or partial obstruction to gas flow through the upper airway occurs frequently during anesthesia without a controlled airway, particularly in patients with obstructive sleep apnea. Therefore, attention to the signs of obstruction or partial obstruction is crucial for anesthesia providers.
The respiratory rate may also be measured by impedance plethysmography, which measures small changes in resistance to the flow of electricity between electrocardiogram (ECG) leads placed on the patient’s chest. When a patient inhales, the thoracic volume increases, which increases the distance between the ECG electrodes. This changes the conduction of electrical currents to the electrodes. When the patient exhales, the distance between leads decreases, and conduction is restored to the original state. Impedance plethysmography can detect these changes and compute a respiratory rate. Impedance plethysmography is much less reliable than other methods of measuring respiratory rate, and it does not detect airway obstruction. It is, however, easy to implement in any patient with ECG monitoring and is occasionally used as an adjunct to clinical observation where capnometry is not available, for example, in the postanesthesia care unit (PACU).
Respiratory rate, airflow, and breath sounds may be measured by a precordial stethoscope. A precordial stethoscope may also be used to monitor heart sounds. It is placed on the chest near the neck and connected to a long tube attached to an earpiece worn by the anesthesia provider. The anesthesia provider can hear the patient inhale and exhale. In addition to monitoring the respiratory rate, the precordial stethoscope can be used to evaluate the quality of breath sounds. Breathing will be absent with a complete obstruction and sound different with a partial obstruction (e.g., snoring). This capability makes a precordial stethoscope superior to visual inspection of chest rise and impedance plethysmography. The precordial stethoscope is commonly used in pediatric anesthesia.
If a patient is intubated, then an esophageal stethoscope may be used to monitor respiratory rate and airflow. The esophageal stethoscope is a long, thin, soft tube placed through the mouth or nose and into the esophagus. The advantage of an esophageal stethoscope over a precordial stethoscope is that heart and lung sounds are more easily heard due to the proximity of the esophageal stethoscope to these organs. Many esophageal temperature monitors have a stethoscope function, though it may be rarely used.
Capnometry
Capnometry is the measurement of carbon dioxide (CO2) concentration in the exhaled gas. Ventilation is accurately measured through the use of capnometry. The detection of carbon dioxide during exhalation confirms the movement of gas into and out of the lungs. Measuring exhaled carbon dioxide may occur qualitatively or quantitatively. In environments where a gas analyzer is not easily available (e.g., during resuscitation on the hospital ward), having a portable, reliable qualitative method to detect carbon dioxide in the exhaled gas allows the practitioner to know that ventilation is in fact occurring, whether this is via an endotracheal tube, supraglottic airway, or bag-mask ventilation. A colorimetric capnometer contains a pH sensitive indicator that changes color when exposed to CO2. The color varies with inspiration and expiration as the level of CO2 in gas flow varies. Typically, the color changes from purple, when exposed to room air, to yellow, when exposed to carbon dioxide. The colorimetric capnometer can be attached to an endotracheal tube, supraglottic device, or face mask so that when exhaled CO2 passes through the capnometer it changes the color of an indicator. Color change confirms the presence of CO2 in the exhaled gas.
It is important to note that the stomach may contain carbon dioxide due to gastric contents, after difficult mask ventilation (gas gets pumped into the stomach during mask ventilation) or after ingestion of carbonated beverages. An endotracheal tube placed in the esophagus may return carbon dioxide from the stomach for one or two breaths; however, after a few breaths the carbon dioxide level will fall precipitously to zero. Thus, it is important to measure exhaled carbon dioxide over several breaths to confirm endotracheal tube placement in the trachea. In addition, other methods should be used to evaluate endotracheal tube placement including auscultation over both lung fields and the stomach (listening for gurgling as the esophageal intubation insufflates the stomach).
A capnogram is a graphic display of the CO2 waveform during the respiratory cycle. This information is useful in assessing the position of the endotracheal tube, patency of the airway and adequacy of the ventilation, as well as the estimation of the cardiac output and CO2 production. This may be accomplished when a patient breathes into a nasal cannula or face mask with a port connected to a capnometer to measure CO2. Similarly, in mechanically ventilated patients, the breathing circuit can be connected to a capnometer. During inhalation, the measured CO2 level drops to zero and during exhalation, the CO2 level rises. Counting the “peaks” per minute yields the respiratory rate. Capnography is also an excellent monitor for detecting apnea or airway obstruction. In both cases, the capnometer will not detect CO2 and alarms can help alert the anesthesia provider to the potential absence of air movement. The anesthesia provider must, however, be aware of false alarms. For example, in the spontaneously ventilating patient in whom CO2 is being measured via nasal cannula, the patient may be mouth breathing and the nasal cannula will not detect CO2 movement.
Lastly, the peak exhaled CO2 level, as measured by the capnogram, is also an important value to estimate arterial CO2 levels. During inhalation, fresh gas enters the lungs with some of it reaching the alveoli, delivering oxygen and picking up CO2. The last portion of inhaled gas is left in the conducting airway. That is, this gas does not reach the alveoli and does not participate in gas exchange—it does not lose any oxygen and does not pick up any CO2. During exhalation, the initial exhaled gas that is detected comes from the mouth, nose, and pharynx and then the conducting airways in the lungs. This gas is the same as the fresh gas that was inhaled as it did not reach the alveoli. As exhalation continues, the gas from the alveoli begins to reach the mouth and nose (or endotracheal tube). This gas contains CO2, which is detected by the capnometer and causes the graphed CO2 values to rise. At the end of exhalation, all of the gas being exhaled is gas that has come purely from the alveoli and will contain larger amounts of CO2. The CO2 level measured at the end of exhalation is called the end-tidal CO 2 (Fig. 8.1). Since the gas in the alveoli has equilibrated with the pulmonary blood, the end-tidal CO2 level is used to estimate the CO2 level in the blood leaving the lungs and entering the systemic circulation. The true end-tidal CO2 concentration is not possible to measure when carbon dioxide is sampled from a nasal cannula or face mask because the port draws in room air that dilutes the CO2 present in an exhaled breath.
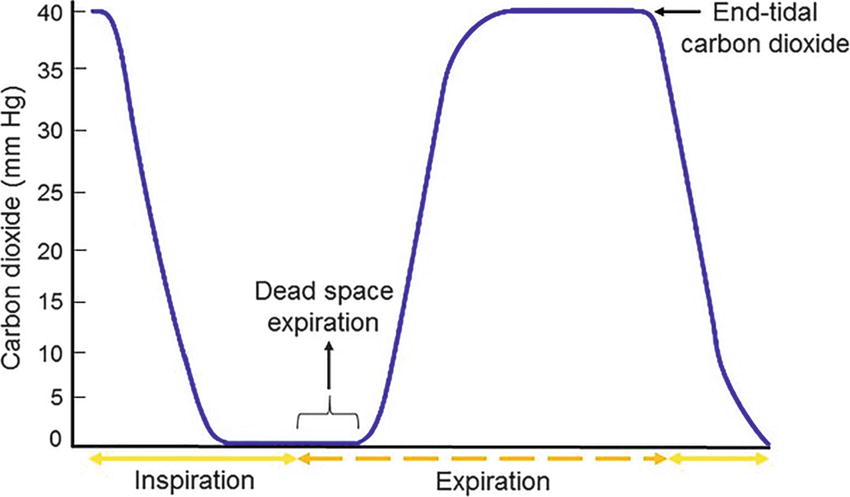
FIGURE 8.1. End-Tidal Wave Form. Original Artwork by Mark Kendall, Northwestern Memorial Hospital, Department of Anesthesiology.
Cardiac output, the amount of blood pumped by the heart every minute, also has an effect on exhaled CO2. In order for the lungs to eliminate CO2, deoxygenated blood must be delivered to the lungs from the heart. If the heart is stopped, blood with CO2 will not be delivered to the lungs. Even if an endotracheal tube was properly placed in the trachea, ventilating the lungs would not produce any exhaled CO2. If the heart is pumping but cardiac output is very low, blood flow to the lungs or pulmonary perfusion, will also be low. Low pulmonary perfusion creates profound dead-space ventilation, thus reducing the exhaled carbon dioxide values to levels that may be too low to measure with a colorimetric capnometer but can be measured with a quantitative capnometer. Thus, quantitative measurement of exhaled CO2 levels can be used as a crude indicator of cardiac output.
The gold standard for direct CO2 measurement is via arterial blood gas analysis. Blood gas analyzers are extremely accurate and can also be used to measure blood oxygen, hemoglobin levels, glucose, and electrolytes. It is important to note that arterial CO2 measurements will be different from end-tidal CO2 measurements. This is because the end-tidal CO2 level is altered by dead-space ventilation. As discussed in Chapter 7, not all regions of the lungs are equally ventilated and perfused. Alveoli that are ventilated but poorly perfused (dead space) will have low CO2 levels. During exhalation, exhaled gas from all the alveoli is mixed together. The dead-space alveoli will dilute the CO2 coming from the perfused and ventilated alveoli, effectively lowering the end-tidal carbon dioxide value as compared to arterial carbon dioxide levels. Alveoli that are perfused but not ventilated also cause arterial and alveolar CO2 measurements to differ. Only ventilated alveoli connect with the airways and send their carbon dioxide to be measured by the capnograph. Alveoli behind bronchi that are blocked by mucus, or closed by bronchoconstriction, will have high CO2 levels that are not reflected in the end-tidal CO2, but contribute to a high arterial CO2: thus, patients with obstructive pulmonary disease will have an alveolar-arterial CO2 gradient and may benefit from blood gas sampling to measure this.
Oxygenation
Oxygenation is the process through which oxygen is transferred from the alveoli to the pulmonary capillary blood. This process takes place continuously, throughout the respiratory cycle. Indicators of oxygenation are hemoglobin saturation and the arterial partial pressure of oxygen. Pulse oximeters measure the percentage of hemoglobin that is saturated with oxygen (see Chapter 31). Pulse oximetry is less sensitive than capnometry in monitoring adequacy of patient ventilation. This is because oxygenation may remain adequate despite increased or decreased carbon dioxide levels in the blood or even absent ventilation. It takes substantial time for saturation to fall after ventilation ceases, particularly if a patient has been breathing supplemental oxygen. A patient may be apneic for even a few minutes before a pulse oximeter alerts the provider that something is wrong. At that point, it may not be easy to re-establish gas exchange right away, and the hypoxemia may become critical. Thus, ventilation should be monitored separately from pulse oximetry. Although there are other reasons for oxygen saturation to decrease, hypoventilation is a very common cause of a decreased oxygen saturation in the perioperative patient. Pulse oximeters are required for all patients receiving any anesthetic.
As mentioned above, oxygenation may also be measured by obtaining an arterial blood sample. The amount of oxygen dissolved in the blood and bound to hemoglobin is related to the partial pressure of oxygen (pO2). Blood gas analyzers are very accurate in measuring pO2. Because they are point-of-care devices, they can provide rapid results. Arterial blood gas analysis is an important tool in the arsenal of the anesthesia provider and provides much information on which clinical decisions may be based. Obtaining this data, however, involves either placement of an invasive arterial catheter or drawing an arterial blood sample via arterial puncture, which can be painful in an awake patient. See Chapter 10 for an in-depth discussion of blood gas analysis.
Anesthesia Machine Monitors of Ventilation
When a patient has an endotracheal tube, supraglottic device, or tight-fitting face mask, additional data may be collected to ensure effective and safe respiratory function. The anesthesia machine can monitor flows, volumes, and pressures within the breathing circuit during both mechanical and spontaneous ventilation. Common respiratory mechanics parameters that can be monitored include:
- Tidal volume—this is a useful measure of ventilatory function in spontaneously breathing patients (indicator of the effects of opioids, anesthetic agents, or paralytics). In mechanically ventilated patients, the anesthesia machine allows the provider to monitor both the set and delivered tidal volume. Care should be taken to ensure that the patient is receiving an adequate tidal volume and minute ventilation. Tidal volumes vary between individuals based on gender and predicted body weight.
- Respiratory rate—Tachypnea, or rapid breathing, is a sensitive sign of impending respiratory failure. Most commonly it is due to hypoxemia. On the other hand, a decreased respiratory rate might be a consequence of sedating or pain medication and will result in both hypoxemia and hypercarbia.
- Minute ventilation—is the product of tidal volume and respiratory rate, reported in liters per minute.
- Airway pressure waveforms—high pressure is a consequence of tidal volumes that are too high, high airway resistance, machine malfunction, obstruction in the breathing circuit or endotracheal tube, mainstem intubation, bronchospasm or blockage within the airways, and restriction to lung expansion (body weight, patient position, external compression on the chest, decreased lung compliance). Low pressure might be caused by apnea, circuit disconnection or leak, fresh gas flow too low, or machine malfunction. Subatmospheric pressure is the result of machine malfunction or a spontaneously breathing patient. Peak inspiratory pressure (PIP) in mechanical ventilation is monitored to avoid “barotrauma”—injury to the lung from pressure that is too high. Tidal volumes are set to avoid generating high pressure or large volumes that can be harmful to the lungs. In addition, increased PIP can indicate obstruction in the breathing circuit, tube, or patient or may indicate a change in lung or chest wall compliance.
- Inspiratory and expiratory flows
- Flow volume loops
- Inspired oxygen concentration
In addition to the above, most anesthesia machines come equipped with a gas analyzer (see Chapter 30). A sample line is connected to the breathing circuit and the analyzer. These devices are capable of measuring inspired and expired concentrations of oxygen, nitrogen, carbon dioxide, nitrous oxide, and volatile anesthetic agents. The oxygen and carbon dioxide information is useful for managing oxygenation and ventilation.
Summary
Monitoring is at the core of anesthesiology practice. The anesthesia provider is constantly vigilant and must be able to respond quickly to changes in physiologic status. As an anesthesia technician, understanding the principles behind respiratory monitoring, most importantly the distinction between ventilation and oxygenation, and being able to anticipate and provide the necessary tools to make the delivery of anesthesia safer is of paramount importance.
The authors have retained several portions of the first edition’s chapter, written by Mark Burno, Casey A. Harper, Matthew Chao-Ben Chia, and M. Christine Stock with permission of the authors we were able to contact.
Review Questions
1. How does the brainstem react to increasing levels of carbon dioxide in the blood?
A) Increasing minute ventilation
B) Decreasing minute ventilation
C) Decreasing respiratory rate
D) Lowering tidal volume
E) Increasing total body acid
Answer: A
Carbon dioxide is partially converted to carbonic acid in the blood and tissues and is an important contributor to the acid-base status of the body. As carbon dioxide levels rise, acid levels rise, and the body’s goal is to decrease acid levels. This is accomplished by the brainstem, which increases minute ventilation in an attempt to restore the pH to a normal physiologic value. Minute ventilation is the product of respiratory rate and tidal volume.
2. Which of the following is the BEST method by which to measure ventilation in an intubated patient in real time?
A) Precordial stethoscope
B) Esophageal stethoscope
C) Capnometry
D) Arterial blood gas analysis
E) Impedance plethysmography
Answer: C
Capnometry is the measurement of carbon dioxide (CO2) concentration in the exhaled gas. Measuring exhaled carbon dioxide may occur qualitatively or quantitatively. This measurement may occur in real time. While esophageal and precordial stethoscope provide information regarding air movement, they can be cumbersome and placement may be precluded by the surgery. Impedance plethysmography does not provide information regarding air flow.
3. What is the maximum inspired oxygen concentration that can be delivered via nasal cannula?
A) 20%
B) 30%
C) 40%
D) 50%
E) 60%
Answer: B
Given the design of the nasal cannula, entrainment of room air, and lower gas flow rates, the maximum inspired oxygen concentration that can be delivered is approximately 30%. A face mask can deliver up to 40% oxygen concentration, while an endotracheal tube can deliver 100%.
4. Which of the following parameters cannot be monitored using the anesthesia machine in a patient who is mechanically ventilated?
A) Tidal volume
B) Respiratory rate
C) Inspiratory flow
D) Minute ventilation
E) Dead space
Answer: E
The anesthesia machine can measure tidal volume, respiratory rate, minute ventilation (which is tidal volume × respiratory rate). Flow sensors measure the inspiratory and expiratory flow rates. However, dead space (the subset of the tidal volume, which does not participate in gas exchange and is ventilated but not perfused) is a physiologic volume that is not easily measured directly by the anesthesia machine.
5. Which of the following would increase your suspicion of airway obstruction in a patient with obstructive sleep apnea?
A) End-tidal CO2 45 mm Hg
B) Positive breath sounds
C) Respiratory rate 20 breaths/min
D) End-tidal CO2 0 mm Hg
E) None of the above
Answer: D
Simply watching the chest rise and fall may indicate the respiratory rate, but it does not confirm gas movement into and out of the lungs. For example, a patient may have the drive to breathe and his or her chest wall may be moving; however, there may be no gas flow into the lungs due to an obstruction of the upper airway. With no gas flow, your end-tidal CO2 would be expected to be zero.
SUGGESTED READINGS
Barash PG, Cullen BF, Stoelting RK, et al. Clinical Anesthesia. 8th ed. Philadelphia, PA: Wolters Kluwer Health; 2016: Chapter 26: Commonly Used Monitoring Techniques.
Butterworth J, Mackey D, Wasnick J, eds. Respiratory physiology and anesthesia. In: Clinical Anesthesiology. 5th ed. New York, NY: McGraw-Hill Medical; 2013: Chapter 6: Noncardiovascular Monitoring.
D’Mello J, Butani M. Capnography. Indian J Anaesth. 2002;46(4):269-278.
Enright A, Merry A, Walker I, Wilson I. Lifebox: a global patient safety initiative. AA Case Rep. 2016;6(12): 366-369.
Kamant V. Pulse oximetry. Indian J Anaesth. 2002;46(4): 261-268.