Chapter 1

Chapter 1

Pilates fundamentals
How pregnancy, birth and motherhood challenge the body
Welcome to Motherland! After having a baby, society seems preoccupied with getting you back into your pre-pregnancy jeans looking fantastic, rather than back home into your body feeling well and functioning normally again. As long as you’ve ‘bounced back’, society doesn’t seem to mind if you’re weeing yourself when you sneeze. This chapter gives you an overview of the changes that birth and motherhood bring to your body and introduces the basic fundamentals of Pilates to show how this amazing body-conditioning programme can help rebuild our strength and counterbalance the effects of birth on the body. The exercises in this chapter form your foundation of Pilates and are appropriate for all postnatal stages. The following chapters then present a progressive Pilates programme for specific needs of each postnatal stage of recovery over the first year (and beyond).
The ‘bounce back’ culture is disrespectful to the vast changes that have happened within your body, emotions and brain over the course of pregnancy and from your childbirth experience. Moving into motherhood is a whole-body and mind transformation: a matrescence. This is a term that was coined in the 1970s by the anthropologist Dana Raphael to describe the period of transition – in mind, body and spirit – that women enter when they have a baby. Birthing a baby also births the mother. It’s akin to adolescence in the scale of hormonal intensity and body changes, and yet culturally we don’t view it with the same understanding of it being a huge metamorphosis. Look at reproductive psychiatrist Dr Alexandra Sacks’ wonderful TED talk on this time of change (details in the Resources). Just as adolescence brings with it an earthquake of physical and emotional changes, so does matrescence.
Motherhood presents a time where there is more change to brain activity than at any other stage in a woman’s life. Our brain shrinks slightly in later pregnancy, and these changes are thought to last for around two years after pregnancy. Our brains literally become restructured, fine-tuned to the skills needed once the baby is born. Emotional intelligence areas grow to ensure we can be empathetic and respond to our baby’s needs. Your amygdala, the ‘lizard’, ancient brain, is one of the greatest beneficiaries of these changes, but this also means that your fight-or-flight (anxiety) response is heightened. It makes perfect sense: you are now the protector of your young, but it can be an unexpected – and uncomfortable – change, particularly if you’ve never particularly experienced anxiety before. Consider it a brain upgrade, new software to deal with the greater demands being placed on it.
For a detailed outline of the brain and other physiological changes, see Dr Oscar Serrallach’s 2018 book The Postnatal Depletion Cure. The changes that we experience are profound and potentially long lasting. These are perfectly legitimate reasons to feel a bit low or weak, and yet we don’t prioritise our healing recovery. Kimberly Ann Johnson, author of the wonderful book The Fourth Trimester, likens modern postnatal recovery to the mentality we have if we fall over in the street: we get up immediately, eyes down, and speed off quickly to avoid embarrassment or attention, and like a cat, lick our wounds alone in private. Actually, we need to sit and breathe for a moment to assess the damage – or even better, be vulnerable and reach for help to get back up.
CASE STUDY

Julie, mum of three
I was really cynical about Pilates initially as I’ve previously enjoyed high-impact workouts and running as my exercise. I felt that if I didn’t have trouble breathing and wasn’t dripping in sweat, then how could I really be exercising! But I found that very quickly my back pain eased. I felt my core strengthening and noticed improvements in my breathing when I did other forms of exercise. The results were noticeable almost immediately. Also, I felt challenged, but at an attainable level.
What’s going on in my body?
Here’s a timeline of what to expect in the first year post birth, from the early days.
DAYS 1 TO 10
What to expect:
•Night sweats – loss of extra fluids, particularly if you had lots of swelling in late pregnancy. Expect to soak through your nightclothes in bodily fluids.
•Heavy bleeding.
•Discomfort/pain from pelvic floor trauma or Caesarean scar.
•Your blood pressure, heart rate, body temperature and breathing gradually return to normal over this time.
•Your boobs will go through huge changes as your milk comes in, whether you breastfeed or not. They may grow to an alarming size and become painfully rock hard. This will pass, but make sure you massage your boobs if you feel they are uncomfortably hard and full, and put baby on your breast as often as you can (even overnight) to establish breastfeeding and relieve the milk build-up to regulate your supply.
•Your nipples may be very sore and tender. This is normal even if breastfeeding is going well. Breathe deeply and slowly while feeding. The pain will settle soon. Be aware of the symptoms of thrush and mastitis (I’ve provided a link to the relevant NHS webpage in the Resources), and seek medical attention as soon as you can if necessary.
•Mood swings, heightened anxiety: often called the ‘baby blues’. There is a huge hormonal watershed now that you no longer have the placenta creating hormones for you, and you begin to return to pre-pregnancy hormone levels within the body. You may feel euphoric one moment and tearful the next. You may feel elated, or defeated by your birth experience. You may feel chaotic due to hormonal fluctuation and emotional intensity/sleep deprivation. All of these feelings are common and normal, but worth tracking in case they linger for longer than a short period of time.
•Urinary incontinence, especially when sneezing or coughing.
•If you had a C-section, flatulence and painful trapped wind are to be expected.
Safe exercises for this stage:
•Pelvic floor awareness exercises.
•Breathing: deep, long, full breaths.
•Ankle circles, pointing and flexing your feet, foot exercises (see here), Legs Up the Wall, neck and shoulder stretches: gentle, restorative, soothing movement.
•If you had a C-section: gentle coughs to stimulate the area around the stitches.
DAYS 10 TO 21
What to expect:
•Lighter bleeding.
•Healing around C-section and episiotomy should be progressing well but may still be painful, swollen and bruised.
•If C-section, the scar site will probably be numb and tender. It will hurt to cough, sneeze, laugh. Remember to take your pain medication.
•Your nipples will probably still be very sore if you are breastfeeding. Keep nipple cream in the fridge and apply liberally in between feeds. Allow your nipples to ‘air dry’ where possible. Breastmilk has magic powers for healing so squeeze some on your own nipples if they are really sore.
•Pregnant tummy will still be prominent.
•Healing still going on at deep level: organs are reassembling within your abdomen.
Safe exercises for this stage:
•Stay low intensity. When lifting your baby/carrying toddlers and when getting up off the floor, consciously breathe out and lift up your pelvic floor to support your effort.
•Avoid strenuous aerobic exercise for the first six weeks, even if you feel raring to go. Walking is fine.
•Your pelvic floor may still be sore and you may still be leaking when you sneeze/cough. Practise finding the pelvic floor muscles on an exhalation: and try to remember to lift your pelvic floor just before you cough or sneeze.
WEEKS FOUR TO SIX
What to expect:
•There may still be some wound healing/scar pain and discomfort.
•Pain from establishing breastfeeding should have settled by now – if it hasn’t, seek some advice and help about checking your baby’s latch. Details in the Resources.
•Bleeding should have completely stopped by now.
•By the end of this period your uterus has contracted back to its pre-pregnancy size, which can feel very painful; it is often more painful and happens more quickly with second and subsequent births.
•Your tummy may still look quite pregnant due to the stretching of your abdominal muscles and skin.
Safe exercises for this stage:
•Gentle, low-impact movement, Pilates, stretching, yoga – but be cautious of intense held stretches and avoid hot yoga, as ligaments will still be vulnerable due to pregnancy hormone levels still levelling off: the hormone relaxin increases the laxity of your joints.
•Moderate-intensity low-impact exercise: longer walks, cycling.
WEEKS SIX TO EIGHT
What to expect:
•Sleep deprivation accumulation may affect energy levels.
•Back, neck and shoulder aches and wrist pains are common due to repetitive movements in early motherhood.
•Hair may begin to fall out due to hormonal levels returning to pre-pregnancy levels (dependent on breastfeeding – if you’re breastfeeding your hormones may take a bit longer to recalibrate to pre-pregnancy levels).
•Pelvic pain may still be present if experienced during pregnancy, particularly if breastfeeding. Beware of starting HIIT or running in an effort to ‘bounce back’ at this stage as pelvic floor weakness will still be present and pelvic joints are vulnerable to injury.
•You may have your GP check – ask to be referred to a women’s health physio for a full physical check. All women should ideally be seen by a physio postnatally. This model of postnatal care is in the workings for the standard pathway of care in the next 10 years, but isn’t standard as yet so you’ll need to ask.
Safe exercises for this stage:
•Pelvic floor and stability exercises, Pelvic Tilts.
•Lots of stretching and opening shoulders. Lying on the floor, palms facing up, can be very beneficial.
•Low-impact cardio: walking, gentle cycling, swimming – although avoid breaststroke if experiencing pelvic pain or discomfort.
•Build in enough rest, deep breathing and stretching to release tension.
•Begin gentle abdominal massage.
MONTHS TWO TO THREE
What to expect:
•Chronic tiredness and fatigue may begin to affect your mental health and resilience.
•If you’re chronically tired and have low energy even though your baby has started sleeping a bit more then it may not purely be due to sleep deprivation, so go to your GP and request an iron and other mineral levels check. Now’s a good time to check in with your diet, if you haven’t already. Are you optimising your nutrient intake?
•If you have access to one, now is the ideal time to go to a women’s health physio to have a whole-body check: pelvic floor, abdominals, breathing, posture.
•Diastasis recti (DR): the greatest time of natural healing of abdominal separation occurs in the first eight weeks. After eight weeks the process of automatic healing slows down. See here for more about DR.
Safe exercises for this stage:
•Pelvic floor, pelvic floor, pelvic floor.
•Have your diastasis recti checked by a professional – and begin targeted deep abdominal recovery exercises.
•Avoid planks and sit-ups in favour of gentle but targeted core restore Pilates – standing, bending, squatting, side lying, all fours.
•Avoid running until cleared by a women’s health physio. Do NOT run at all yet if you are leaking urine. It doesn’t mean never again, it just means not now.
•The postnatal GP check is not, and never has been, a ‘clearance for exercise’. There is growing awareness of the fact that all women need to be seen for a physical check-up by a women’s health physio, but particularly if they desire to get back into high-impact exercise such as HIIT or running. For the latest (2018) physio-led guidelines about returning to high-impact exercise postnatally, see the publication listed in the Resources. Pelvic organ prolapse risk is high at this stage (see here).
•Stretch and release tension in neck, shoulders.
FOUR TO SIX MONTHS
What to expect:
•Tendency to gain weight, particularly if breastfeeding/energy levels are very low, or if still suffering from incontinence and scared to exercise.
•You should hopefully be feeling physically a bit ‘more normal’.
•Aches and pains are common: neck, back, shoulder, hips, due to the repetitive movements of motherhood and lack of stretching.
•Your periods may have returned by now, even if you’re exclusively breastfeeding (unfair, right?). It’s important to be aware that you can still get pregnant while breastfeeding, so if returning to sexual activity you need to consider contraception.
•Your uterus stretches during pregnancy, so it’s common for periods to be much heavier after pregnancy due to the extra surface area of the uterus. See your GP if you’re concerned about particularly heavy bleeding.
Safe exercises for this stage:
•Pelvic floor – important even if you had a C-section.
•Aerobic exercise. Bear in mind the fragile energy-balance equation: tiredness can be counterbalanced with exercise, and sleep/anxiety symptoms may be improved by exercise. But if you are exhausted and depleted, proper rest is more beneficial (meditation/reading/breathing and stretching, instead of scrolling on your phone when baby naps, etc).
•If you are still experiencing urinary incontinence, please don’t delay seeing a physio. Ask to be referred by your GP. Weeing yourself is common but not normal. Do not do high-impact exercise while still leaking: it won’t get better if you ‘push through’ it.
•Be mindful of potential ligament laxity and avoid wide-legged unstable HIIT moves such as Skaters if they feel uncomfortable in the pelvis.
•Focus on glute strengthening alongside pelvic floor/deep abdominal activation work.
SIX MONTHS TO ONE YEAR
What to expect:
•You may feel your mojo returning, depending on how much sleep you’re getting. It may take longer – everyone is on a different healing journey so don’t compare.
•Keep an eye on your mental health. Depression and anxiety can begin to take hold once the intensity of the newborn phase is over and as a result of the cumulative effects of sleep deprivation. Don’t be scared to reach out for support.
•Focus on your posture, breathing and how you feel inside rather than on weight loss or gain.
•It is also normal NOT to feel as strong as you were pre baby yet. Aches and pains from baby duties are common, your baby is getting heavier by the day and more challenging. You are still very newly postnatal in the grand scheme of things.
Safe exercises for this stage:
•Walking, swimming and low-impact cardio are very valuable for your physical and mental health.
•Returning to your pre-pregnancy levels of activity is safe so long as there are no pelvic floor and diastasis recti issues. However…
•You’re more vulnerable to injury right now, so literally don’t run before you can walk.
•Stretching, conscious resting, such as meditation, and deep breathing cannot be underestimated in value.
ONE YEAR TO FOREVER
•You are still postnatal.
•Be gentle with yourself. If you’re frustrated with ‘how far you’ve come’, remember postnatal strength and recovery is often not linear. It’s common to experience setbacks.

Your birthing body – what happens in your body during birth?
Your pelvis
The pelvis is a pretty amazing design. It’s made up of four bones, arranged like a fused bony ring at the bottom of your spine. You can locate certain parts of your pelvis by palpating your skin: at the front you can find the ilium bone; the iliac crest is the bony parts of your hips; at the front is your anterior-superior iliac spine (or ASIS); and at the back, your posterior-superior iliac spine (PSIS).

Your ischia are your sit bones – the oft forgotten bones that we tend to curl underneath us rather than actually sitting on. At the back, you can feel the triangular-shaped bony pattern of the sacrum, which ends in the coccyx, the remains of our tail. In the front is the pubic bone, which is in fact two bones, one from the left side of the pelvis and one from the right, fused together by thick fibrous cartilage.
Take some time to orientate yourself with your own pelvis. Get a sense of the width of your pelvis, the height, its relation to your ribcage. The pelvis is the seat of your power, and postnatally is the key to unlocking a lot of imbalances that flow through the body.
What happens to the pelvic bones during birth?
When not affected by hormones, the pelvic ligaments connecting the pelvic bones are fixed almost like grouting, allowing for minimal movement between the joints. Like the engineering of a bridge, some movement is necessary to react adequately to pressures of temperature, wind and load, but too much would compromise the strength of the bridge. Pregnancy hormonal changes ensure that these ligaments become more lax, which means the bones have a movement potential previously not allowed. If you suffered from pelvic girdle pain (PGP) you may be painfully aware of this.
The laxity is one of the miracles of the human body: during a vaginal birth this is how your baby is able to wriggle their way out of the birth canal. The pubic symphysis makes very small sliding and opening movements. The sacroiliac joints allow for a greater opening for the head to enter into the pelvis. The base of the sacrum moves backwards and the coccyx forwards. The iliac crests (hip bones) spread, which opens the top of the pelvis. Then, as your baby descends, the sit bones open, which triggers all of the preceding movements to reverse, like doors closing after baby exits. Imagine a time-lapse video of a flower opening and expanding, then closing – this is exactly what happens to your amazing, brilliant pelvis to allow your baby into the world. No wonder you may feel like you’ve been hit by a bus afterwards.
Your pelvic floor
The pelvic floor isn’t just one muscle. It’s a group of muscles: interlinked, overlapping and webbed together in a figure-of-eight shape around your anus, vagina and urethra, ensuring your bladder, uterus and bowel have a strict turnstile to get through before they can empty. The pelvic floor works in delicate balance with your abdominals, diaphragm, back muscles and glute (buttock) muscles that stabilise the pelvis – in other words, your pelvic floor influences and is influenced by the whole of your body. Men also have a pelvic floor, but they have only two orifices (the anus and urethra), and no baby exit route to consider – and therefore they don’t tend to suffer the pelvic floor trauma early on in their lives that women do.
Our pelvic floors go through a lot. Nine months (maybe slightly more) of pregnancy strains the muscles’ resilience. Any sickness you experienced places great additional pressure on the muscles, so if you suffered severe sickness throughout your pregnancy, such as hyperemesis gravidarum (HG), you may well have weakened your pelvic floor significantly before you had your baby.
Your pelvic floor, diaphragm and abdominal muscles together use huge strength during contractions to push your baby down through the pelvic cavity. The pressure your baby presents on the pelvic floor brings about a reflex contraction of the uterus, the expulsive reflex. This pressure, alongside these expulsive contractions cause the perineum to stretch, at first at the back because the head places most pressure at the coccyx to push out, and then at the front. Even for a Caesarean birth without labouring first, your pelvic floor has been your baby’s trampoline for nine months.
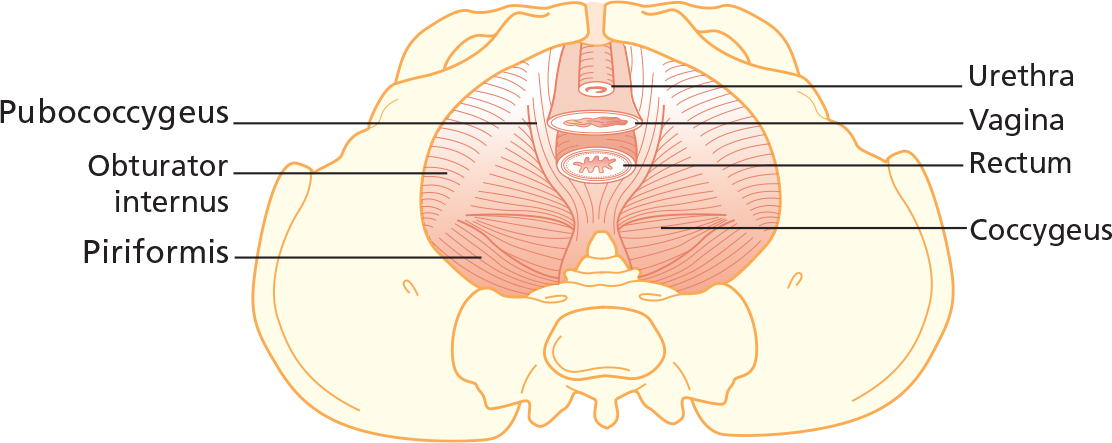
The pelvic floor muscles (female).
In an ideal world, every new mum would see a women’s health physio as a matter of course in a normal postnatal pathway of care, to make sure we’re firing on all cylinders before we take on the world again post birth. This isn’t yet part of our standard postnatal care, so we have to make sure we take responsibility for our own healing. The main thing to remember about your pelvic floor after birth is that you shouldn’t suffer in silence. Pelvic floor issues simply do not get better if they are ignored. If you are struggling with pain, discomfort, lack of sensation, a feeling of ‘bearing down’/‘falling out’, or simply if things don’t feel ‘normal’ – not asking for help means that the problem will only get worse over time.
One of the most common pelvic floor issues is incontinence. The 2019 National Institute for Health and Care Excellence (NICE) guidelines for treating stress urinary incontinence, and pelvic floor dysfunction such as pelvic organ prolapse advise that women should be offered ‘a trial of supervised pelvic floor muscle training of at least 3 months’ duration as first-line treatment’. In a trial study conducted in 2018 by BMC Women’s Health, women suffering from incontinence were offered pelvic physiotherapy alongside tailored Pilates classes for 12 weeks, and the results showed, ‘a range of benefits for women who attended Pilates classes … had lower symptom severity … improved self-esteem, decreased social embarrassment and lower impact on normal daily activities… Women with higher symptom severity showed improvement in their personal relationships.’ The data also indicated that Pilates classes, ‘could positively influence attitudes to exercise, diet and wellbeing.’ So you’re absolutely in the right place here.
Pelvic floor exercises
So Pilates can help with your pelvic floor. What does that actually mean? You’ve probably been told you need to ‘strengthen your pelvic floor’. You might have been squeezing hopefully, eyebrows raised, clenching everything – your bum, your thighs, your jaw? To retrain your pelvic floor for life after birth, pelvic floor awareness – learning to isolate only your pelvic floor and not grip the muscles that surround it, and knowing how to fully release as well as squeeze – is vital. And this awareness takes time to tune into.
Your pelvic floor strength is affected by how you move and carry yourself (and carry your children) every day. Movement stimulates your pelvic floor – so in this respect, every exercise in this book, and everything you do every day, is a pelvic floor exercise: stretching, toning, stimulating the floor through movement and breathing. That’s also why sitting a lot isn’t great for the pelvic floor: it deprives it of movement and circulation; a sedentary lifestyle isn’t good news for pelvic floor health.
Pelvic floor ‘exercises’ – where you rhythmically lift and release your pelvic floor muscles – are really important for postnatal healing and are profoundly effective, when done correctly. But we tend to think they’re boring, aren’t quite sure if we’re doing it right and so we skip them, which makes us feel guilty. Guilt and boredom – not really a magical combination, right? But actually, these exercises are the secret seasoning in the recipe for a vibrant life. You need them now more than you’ve ever needed them. Don’t see them as boring. Or, if they are boring for you, it’s the same boring that brushing your teeth is – something that you wouldn’t dream of forgoing or not making time for. They are part of essential life upkeep. Imagine if from now on you didn’t brush your teeth every day, twice a day. What would your teeth look and feel like, aged 75? Exactly the same principle applies to your pelvic floor health. Since you always remember to do one, why not try doing the other at the same time?
The way the human body was designed means that we shouldn’t need to ‘exercise’ our pelvic floor – we should be utilising its strength naturally through daily effort and movement. However, modern humans have a very convenient comfortable captive life where we now really don’t need to move that much (hello, sitting at a desk for 8 hours) or go that far under our own steam. We use a tiny fraction of the physical strength that our prehistoric ancestors needed on a daily basis to survive. We don’t climb, swing, jump, run or walk the way our bodies were meant to (and, indeed, the way children’s playgrounds encourage our children to). Once we’re adults, we generally sit on our bums quite a lot and eat biscuits.

Yet all movement, all of the power we need for the lifting, pushing, pulling etc in our daily lives stems from healthy pelvic floor function and its related synchronicities within the body. What’s more, the pelvic floor is the last line of defence to ensure our organs (and fluids) are safely held inside. So you can see that when you add the hormonal and physical demands of childbirth and motherhood that without a fully effective pelvic floor this defence will be poor. Luckily, becoming more aware of your breathing and of your alignment will quite quickly have a positive effect on your natural pelvic floor function, improve your daily movement patterns and lessen the general strain on your joints.
Pelvic organ prolapse (POP)
There is a real risk of pelvic organ prolapse postnatally. A prolapse is when the uterus, bowel or bladder descends into the vagina. Some studies have found that 50 per cent of women will suffer from a prolapse post birth (Hagen et al 2004) – and often it happens in the three-month period when people are keen to jump back into exercising to lose baby weight. It is so important to strengthen your pelvic floor to help you avoid this. If you feel any sensation of your insides ‘falling out’, do not ignore this. Go to your GP and ask to be referred to a women’s health physio. Pelvic organ prolapse can’t always be prevented, but it can be managed.
Pelvic floor health declines as we age, particularly if we do nothing to maintain awareness and strength – this is one of those inevitable facts of life, like death and taxes. Staggeringly, only 25 per cent of women aged 18–83 have ‘normal’ pelvic floor support (Swift et al 2003). Much of this is arguably to do with lifestyle, postural habits and suffering in silence. So make sure you proactively do all you can to ensure that you strengthen your pelvic floor post birth, particularly if you know you want to have more children. It’s not acceptable to be told that you should wait until you have completed your family before you can get proper help or be referred for surgery to ‘fix’ the problem. Statistics show that surgery without physiotherapy to help find the root cause of issues is rarely 100 per cent successful, with a significant chance of prolapse reoccurring. You need to strengthen as much as you can between babies otherwise you simply build more load on to an increasingly weaker foundation.

Pelvic floor dysfunction
Pelvic floor dysfunction makes itself apparent in a few ways. You may have lack of bladder control or lack of bowel control. You might wee a bit when you cough, sneeze laugh or run. You may have a desperate sudden need to run to the loo as soon as you turn your key in your lock when you get home. You may suffer from involuntarily breaking wind, which can feel excruciatingly embarrassing. Or constipation – and then straining on the loo causes even more pelvic floor and emotional issues. You may have pain, or a feeling of ‘bearing down’ during exercise or sex. All of these are symptoms of pelvic floor dysfunction. We shouldn’t laugh it off. It shouldn’t be something you’re just expected to put up with after having a baby. We deserve better ladies. Pelvic floor health is not something we should accept will inevitably decline after having babies.
Hypertonicity
Hypertonicity is something that isn’t widely understood as we’re generally so obsessed with ‘strengthening the pelvic floor’. When pelvic floor exercises are usually discussed, we only hear about ‘squeezing’, ‘strengthening’ and Kegels. But this misses out the full spectrum of recruitment for your pelvic floor muscles and can cause over-tightness. Consider your bicep muscles – they bend your arm in, but they can also release to straighten your arm out. You’d be a bit stuck if you could only hold your arm in a slightly bent ‘strong’ position, with neither of the two ends of the movement spectrum available to you. Sometimes strength is only half the story. We need softness, release, too: flexibility. This flexible strength is what we need in our pelvic floor.
Hypertonicity means excessive tone, tension or activity in the muscles – in other words, muscles held permanently in a ‘tight’ clenched position. Imagine walking around with a clenched fist all day. After a while, those muscles won’t function as efficiently, and they’ll fatigue and work incorrectly, causing you aches and pains. If this over-recruitment tightness happens to your pelvic floor, the muscles won’t be able to function well.
Possible signs and symptoms of hypertonicity are: pain during sex; general soreness in the pelvic floor; pelvic pain; downward pressure in the vagina; pain when sitting; tightness, throbbing, aching, stabbing, spasm; bladder frequency; difficulty emptying the bladder and bowels; constipation. If you recognise any of these symptoms, visit a specialist pelvic health physiotherapist so you can start to remedy the situation.
In order to avoid hypertonicity, then, we need to learn to fully release the pelvic floor, as well as strengthen it. This is where breathing patterns are essential, as by breathing properly you learn to train the pelvic floor to release down as you inhale and to lift and work correctly with the abdominals as you exhale.
Pelvic floor restoration
To heal the pelvic floor we need to:
•Realign: Notice your posture, patterns of movement, incorrect muscle recruitment and correct them.
•Release: Let got of any tension you’re holding on to in your pelvic area: abdominals/hips/glutes/pelvic floor.
•Awareness: Build your awareness of your pelvic floor and connect to it every day.
•Strengthen: Only after you have found your connection.
Remember: Stage 1 = Awareness
Stage 2 = Foundations
Stage 3 = Build on it
Your abdominals: diastasis recti
Around the second trimester, depending on the size of your bump, you will have experienced some degree of abdominal separation: diastasis recti. The rectus abdominis muscle is your ‘six-pack’ muscle. It runs down your front, from your breastbone to your pubic bone: two segments running vertically parallel and intersected by a fibrous band, the linea alba.

In a brilliant design feature that showcases the human body’s adaptability, as your bump grew, the linea alba stretched to allow your baby more space; the two bands of muscle stretched away from the centre. Normally, the linea alba has a non-stretchy consistency without much ‘give’, almost like cotton. During pregnancy, however, hormonal activity ensures that it becomes more like Lycra, and responds to your bump’s demand that it relaxes and stretches.
This is a normal structural adaptation, and you can’t necessarily prevent it, and neither would you want to – it is a design feature specially created for your baby’s comfort and growing power. Around 30 per cent of women experience this abdominal separation in the second trimester, with a further 66 per cent separating in the third trimester. Some research says that 100 per cent of women have some level of diastasis of the rectus abdominis by the third trimester (Gilliard and Brown 1996, Diane Lee 2013). Look at those stats again: 100 per cent of women have this happen at some point to some degree during pregnancy.
The extent of your abdominal separation depends on a number of factors:
•your abdominal tone pre-pregnancy
•whether or not you carried more than one baby
•whether or not you’ve previously had more than one baby
•whether or not you put on a lot of weight, or carried a big baby – the latter will have had less space and needed to ‘pop further out’
•your age: it can be worse if you’re over 35
•your exercise and fitness levels
•the quality of your diet
•daily posture – are you stooping/lifting constantly without care for your technique and form?
Mind the gap
Until quite recently healthcare and fitness professionals have talked in terms of ‘closing the gap’. But we now know that it’s not the presence or even the width of the gap that’s the issue: it’s whether or not there is deep tone of the supporting muscles and fascia (connective tissue). So you could have a three-finger gap, but as long as your core muscles are firing properly and you can manage your intra-abdominal pressure – the pressure in the space between your respiratory system (your diaphragm) and your reproductive system, placing load out into your belly or down into your pelvic floor – this gap is considered to be ‘functional’, i.e. not a problem. You may never ‘close the gap’ completely, but as long as you have tone, this is OK.
CASE STUDY

Miranda, mum of two
My diastasis recti gap wasn’t very big each time and seemed to close pretty naturally but it was good to be aware of exercises I shouldn’t do. The temptation with a wobbly tummy is to go straight into all the sit-up-type exercises to try to flatten the tummy, but these would have made it worse.
A problematic diastasis recti is one where there’s soft squishy tissue rather than tensile active tissue in the linea alba, therefore not supporting your core in movement, leaving you vulnerable to injury and pelvic floor issues. for the ‘rec check’, and for more detail about this.
Diastasis recti used to be considered a purely cosmetic issue – the ‘mum tum’ ‘postnatal pooch’ – and generally dismissed by GPs, ‘well you’ve had a baby what do you expect? Do some sit-ups.’ This has been very unhelpful for women. There is a direct correlation between a diastasis recti and the load placed on your pelvic floor and your spine. If you have a serious gap, this has an impact on the ability of your abdominals to control the balance of your pelvis and spine, with the result that you may also experience back pain and/or symptoms of pelvic floor dysfunction. (And you shouldn’t be doing sit-ups as you’ll make it worse.)
You might have noticed when you were pregnant that when you got out of bed or even up from sitting, there was a strange doming in your stomach, a bit like an alien pushing out, or a Toblerone-shaped triangle. You don’t want to see that doming any more. If you see it when you lift yourself out of bed or off the floor, make it a habit instead to roll over on to your side and push yourself up with your hands, rather than using your abdominals.
Crunches, sit-ups, planks, leg lowers, etc increase intra-abdominal pressure and therefore place a load down on your pelvic floor or out into your linea alba, so you may see doming or feel heaviness in your pelvic floor when performing them. These should be avoided – not forever, but until you’ve got your breathing and core control firing properly. Heavy lifting increases intra-abdominal pressure, too. If you have a toddler or a small child, chances are you’ll be lifting them regularly so you must commit to lifting correctly to reduce the load on your pelvic floor (see here).
Continue to avoid ‘regular’ exercises – even if you get the ‘all clear to exercise’ from the GP at your six-week check-up. Unless they have actually palpated your abdominals to check for DR, please don’t rush back into traditional ab exercises, oblique strengtheners (Twisting Curl-ups and Side Planks – see here), or twisting movements that feel challenging on the core. Avoid getting back into running or any other high-impact exercise just yet. Erring on the side of caution, while keeping active, is always the best policy – despite what some celebrity trainers might suggest on their glossy Instagram feeds.
Excessive abdominal training with a DR, particularly with twisting movements, such as oblique curl-ups, can cause a downward pressure in the abdomen through the pelvic floor, which will pull the already weakened linea alba further out to the sides.
Diastasis recti doesn’t always resolve itself on its own. The first eight weeks postnatally are where the main natural healing takes place, and if you still have a problem gap after this point it needs conscious training and dedicated deep core healing work.
Postnatal exercise
The ‘bounce back’ pressure is so toxic because it offers mums yet another area in which to feel like we’re failing. I really do understand how keen you are to get ‘back to your pre-baby self’. Body image is so intrinsic to happiness and identity, and postnatally this can take a real beating. There is so much healing going on under the skin, you need nurturing and kindness. If you do go to a Postnatal Boot Camp BODY BACK-type fitness class, your instructor should ideally check your abdominals for separation and at the very least ask you about your birth experience and how your pelvic floor is feeling. If the instructor omits any of these essential duty-of-care issues, and particularly if they focus on planking, crunches, ‘feeling the burn’, burpees, leg lowers, flat tummy exercises etc, please, do not do this class.
EXPERT ADVICE

I love being a mum. For me it was the most amazing, wonderful (and scary) thing that ever happened to me. I also love to run and as soon as I had my children, on both occasions, I wanted to get out there, clocking up the distance as soon as I could.
However, I am also a women’s health physiotherapist and I know just what a life-changing event pregnancy and childbirth is. Your body changes in incredible ways, and the reality is that EVERY woman will have a weaker pelvic floor, glutes, tummy muscles and altered posture. Such a cocktail can lead to urinary/faecal incontinence, pelvic organ prolapse, dyspareunia (pain in the genitals during sex), unresolving diastasis recti and musculoskeletal injuries, i.e. low back pain.
Even if you had the most beautiful, serene pregnancy and childbirth there is no getting away from such physiological changes. Even if you have no symptoms, i.e. urinary incontinence, it does not mean that six weeks post delivery you are ready to return to high-impact/-level exercise. Ladies, we need to think long-term prevention when it comes to postnatal recovery because unless these weaknesses are addressed, at some stage in life pelvic floor dysfunction can occur no matter who you are.
The stumbling block is that there is so much conflicting information out there and we do not receive the level of postnatal rehabilitation we need and deserve. If you had knee surgery you would always see a physiotherapist post op. I advocate that every woman regardless of delivery sees a women’s health physiotherapist anytime from six weeks post baby. The six-week GP check is not enough. Many women’s health physiotherapists now carry out a ‘Mummy MOT’. This involves a musculoskeletal assessment of your back, pelvis, global muscle strength, tummy check and, importantly, an internal assessment of your pelvic floor. From there, a programme is devised to put you on the right track to recovery, bespoke to you and your goals.
Before I returned to running I did just that. I visited a colleague who helped me retrain my pelvic floor and core. I did not return to running until six months after both of my children were born and for the vast majority of this time used Pilates to build up my foundations, which ensured that I could return to running without incurring any pelvic floor dysfunction or musculoskeletal issues.
It takes time to heal and regain your strength, you are only human. There is no shame in prioritising you and getting your body back safely and effectively. If you return to sit-ups, planks, high impact too soon you can do more harm than good. So ladies, please, ask your GP to refer you to a women’s health physiotherapist and look after YOU!
Emma (Physiomum) is a specialist women’s health physiotherapist, based in Oxted, Surrey. Her particular area of interest is in postnatal rehabilitation and working with women to return to high-impact exercise and running safely and effectively. You can follow her on Instagram: physiomumuk, Facebook: @physiomum.co.uk; or on Twitter @emma_physiomum
THE REC CHECK
Checking for DR is simple, but ask a professional to check you as well as having a feel for yourself. A DR gap is measured in finger distance, and can occur at any place along the linea alba. A gap of one to two fingers’ width is normal post delivery.
•Lie in Relaxation Position, taking one hand behind your head.
•Place three fingers just in the centre of your abdominals, above the navel.
•Palpate (press firmly down) to have a feel of the muscles.
•Gently lift your head and continue to press down, and feel how your muscles react.
•Relax the head down, then slide your leg away, still palpating your abdomen to notice for tension and recruitment of the muscles.

•As you lift your head, connect to your centre: engage your pelvic floor and TA, so that you can have an idea of the tone supporting the linea alba. By ‘tone’ I mean it should feel firm and springy in the space in between the sides of the rectus muscle. Even if there is a significant ‘gap’ of more than two fingers, the presence of tone indicates that it is functional, which is the most important thing.
•If it feels like you’re pressing deeply into a soft blancmange without any tension, that’s a serious gap that needs to be looked at by a physio; there is a proven link between DR and pelvic floor dysfunction – 66 per cent of women with DR also have a pelvic floor dysfunction (research from 2011 Lee, Hodges, Wiebe), so it’s not something to be ignored.
CASE STUDY

Hina, mum of two
I spent a month doing dedicated work on my diastasis recti and I am beyond thrilled that I healed it! I went from being able to put four fingers in the gap to barely being able to push a finger in and clearly feeling the muscle tone. I took guidance and did Pilates every day for about four weeks, and I am so blown away by what happened.
Your ribcage
Your ribcage contains your lungs and your heart. During pregnancy it flares to accommodate your baby, and your diaphragm and lungs are pushed up as your baby expands into the space. Your pregnancy posture may also have made your chest roll forwards, which compresses your breastbone and lungs, and it’ll take time to recalibrate. Breathing is so important. Aim for an umbrella breath – opening your lungs out 360 degrees as you breathe in and closing them on the out-breath. This begins to massage the intercostal muscles, in between each rib, to enable full movement of the ribcage.
Imagine a church bell sitting in the centre of your chest. When your ribcage is centred directly above your pelvis, in balance, the bell hangs silent. If you droop forwards, the bell clangs forwards. If you flare your ribcage, the bell clangs back. Take a moment to notice your alignment of your ribcage. Check in the mirror if you can – are you ‘ringing up’ or ‘ringing down’?
To help realign the ribcage with the pelvis, in order to begin to restore abdominal strength and heal diastasis recti, we often need to draw the bottom of the ribcage back in line with the top of the pelvis. Imagine softly hugging your lower ribs back in towards your heart: maintaining height, but drawing your ribs back so that they are in line with the hips. Use your hands: palpate the space between your lower rib and your hip bones.

Balanced rib–pelvis connection
Unbalanced rib-pelvis connection
Your feet
Another common yet surprising issue postnatally is your feet. In whole-body terms, foot problems can often contribute to general weakness and imbalance in the pelvic floor so it’s important to be aware of the way that you balance on your feet day to day. During pregnancy, the relaxin hormone affects the ligaments, and this can result in fallen arches. It’s therefore important to wear supportive shoes and regularly work on foot stability with balance work: try standing up on your tiptoes slowly and deliberately while the kettle is boiling, lower back down then repeat 10 times. Other good exercises are Pliés and Lunges.
Foot exercises are really important. Try these: Imagine playing the piano with your toes, moving each toe individually. Lift your big toes on their own. Lower back down. Lift your little toes. Lower back down. Try to grip and pick up a towel from the floor with your feet. Activities like this stimulate the muscles in your feet, work your arches and massage the connective tissue. When you’re standing, send your awareness to your feet, the triangle of connection of your big toe joint, your little toe joint, and your heel. There is a definite link between foot strength and the pelvic floor – if you’re able to properly ground through these points in your feet, this has a lifting and supporting effect on your pelvic muscles.
Long term, think about your feet as a starting point for all your posture awareness. Try to make sure you spend at least some time each day in bare feet, literally grounding yourself. Changes in foot stability and stiffness creeps up into your body and affects all of your movement patterns. Rolling your foot on a tennis ball daily is a great way to massage the fascia and encourage good foot – and therefore influence whole-body – function and health.
Plantar fasciitis
Plantar fasciitis – inflammation and tearing in the tissues on the bottom of the foot – is common. It can present as annoying foot or heel pain when standing up after sitting or lying down for a while (such as first thing in the morning, when you might hobble painfully getting out of bed). An easy way to help alleviate inflammation is to put a bottle of water in the freezer, and in the morning roll your foot along it.

Posture
Posture is such an integral part of our wellbeing, yet we can be completely oblivious to how we carry ourselves. When you think of posture you might think of ‘standing or sitting up straight’. But posture isn’t ‘held’ or static: it’s responsive, dynamic, constantly recalibrating according to what you’re doing (kind of like motherhood itself…).
Posture is the alignment of your skeleton and muscles. It’s also reflective of a state of mind: if you feel low, your shoulders will droop, your chest collapses and your heart and lungs are squashed. So many ‘mum duties’ involve hunching forwards, and over time this can have a cumulative negative impact on your sense of wellbeing and positivity without you even realising.
Pilates encourages you to check in with your posture every day, and ‘imprint’ better posture into your body awareness. Make use of a mirror – or take pictures on your phone or have your partner do so – and really observe the way you carry yourself. You have the power to change your postural habits, and therefore directly influence the way that motherhood challenges your body. When you’re standing and pushing your buggy/wearing your baby, check in with your posture often: soften your shoulders, lift up tall through the crown of your head, look up.
‘Ideal’ standing posture
•Your head is lengthened at the top of the spine, not tilted forwards or back.
•Your shoulder blades lie flat against your ribcage.
•The bottom of the ribcage is aligned with the top of your pelvis: not shifted forwards or tucked down, so the lungs have plenty of space for efficient breathing.
•The natural curves of the spine are preserved.
•The pelvis is neutral, not tilted forwards or back.
•The knee joints are in line with the hips and ankles.
•The head, ribcage and pelvis are balanced directly over the arch of your foot.

Common mum posture.
Your postnatal posture
Your body balance and centre of gravity changes throughout your pregnancy, and this altered ‘map’ of your muscles can remain long into motherhood unless actively reconditioned. Often, there’s an increased curve in the upper back (kyphosis), which is created by the extra weight of your boobs, not to mention all baby-related activities involving forward hunching, and there is often an increased curve (lordosis) in the neck and in the lumbar spine (lower back) due to the way you carried your baby and the forward tilting of the pelvis that often happens as a result of this.
In some women, during pregnancy the lumbar spine flattens and the pelvis tilts back in the opposite way, switching off the bottom muscles. This can be a common ‘mum posture’ when you’re constantly swinging a small person on to your hip or baby wearing a lot. Your joints and muscles are misaligned and all of your movement patterns are affected, which means aches and pains usually follow. Pilates is ideal for counterbalancing this load on your body, for noticing how you carry yourself and consciously deciding to rectify poor posture.
Protecting your back while lifting and carrying your baby/toddler
You need to be mindful of your posture while picking up your baby/lifting your toddler into the buggy, etc. Lifting your little one in and out of the cot/bath requires conscious stability. The same goes for car seats: they wreak havoc on our backs as they weigh a tonne, and commonly we lift them when we’re a bit stressed and being shouted at by a small person, so any mindful movement intention goes out the window.

Whenever you bend down to lift or dress your toddler/child, make sure that you squat down, bending your hips and knees, rather than hanging your spine forwards with straight legs. Try to make sure you’re standing as close as possible to your toddler when you pick them up, rather than reaching for them as they scarper away from you. When you lift, breathe out and engage your pelvic floor actively. Be aware of and try to avoid carrying your child repeatedly on the same side.
As mums, we tend to become pack horses without blinking: carrying buggies up stairs at stations, walking home from school carrying your toddler, her scooter, his trumpet and all your shopping... We pile up our physical duties without questioning it because we just have to get things done. This puts us at very real risk of back/shoulder/neck injury and pain.
Movements that combine twisting with bending (such as lifting your baby out of the bath) put the most pressure on the spine, and this is when you’re likely to injure yourself if you’re not mindful. Lifting and transporting a toddler can be a very challenging task, particularly if they’re playing dead, or planking. Always lift with care. Switch your baby changing bag to a rucksack and make sure you carry it on your back and not on one shoulder.
Tip
When you lift your child in and out of their cot/car seat/bath, connect to your centre first. Consider it an active pelvic floor/core functional exercise, rather than something you do without thought. All of my clients suffering from pelvic floor and diastasis recti issues heal faster and see more progress in their symptoms when they bring their body awareness into their daily movement habits.
ABCs: ALIGNMENT, BREATHING, CENTRING
The Pilates principles that should underpin all your sessions (and movement in life) are the ‘ABCs’ – alignment, breathing, centring. The following pages are some fundamental exercises suitable for all stages of your postnatal recovery, to lay the groundwork for your Pilates practice.
Alignment
Neutral pelvis and spine
Joe Pilates said, ‘If your spine is inflexibly stiff at 30, you are old. If it is completely flexible at 60, you are young.’
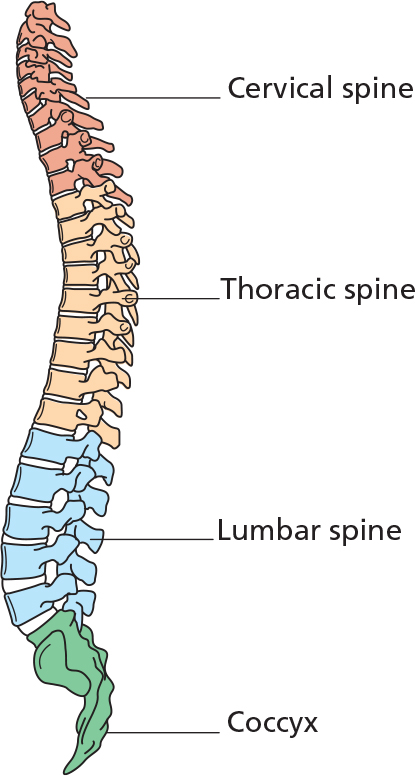
The key to maintaining the flexibility (and youth!) of your spine is creating optimum space between your vertebrae, to encourage length within the spine for the intervertebral discs to operate, which preserves their cushioning effect in the long term. Being in a ‘neutral’ position means that your spine is balanced in its natural curves: there is no compression or unwanted flexion or extension within the spine. Neutral is the optimum position for your spine to withstand the forces of gravity. Your spinal curves are your body’s shock absorbers, so if they are slightly out of kilter or continually held out of balance, that affects the way that your body will take the repetitive ‘shock’ of your daily movement.
Neutral pelvis and spine are interrelated, but not the same thing. Your pelvis can maintain neutral when your spine isn’t, for example during Curl-ups. Neutral pelvis is when your pelvis is lengthened at the end of your spine, with the hip bones (your ASIS: anterior and superior iliac spine) and pubic bone level with each other. Your tailbone is neither tucked nor arched. If your pelvis isn’t in neutral, your lumbar spine will either be flattened or will be arched, in response to the position of the pelvis.

Neutral standing pelvis (left) and Neutral lying pelvis (right)
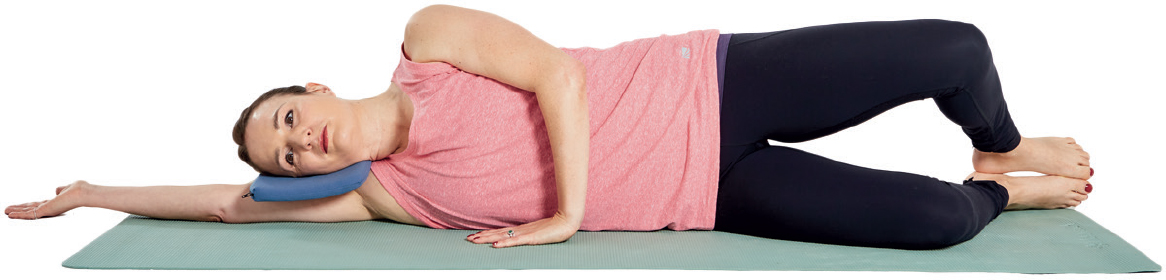
RELAXATION POSITION
Stage 1
This exercise prepares you for movement and relaxes your muscles, allowing you to settle into your neutral alignment and breathing. It’s also a wonderful way of softening the demands of motherhood: I recommend doing this every single day. You can do it even with your baby lying on you or your toddler climbing over you.
•Lie on your back, arms lengthened down by your sides, or resting your hands on your belly. Feet flat on the floor, knees bent, hip-width apart.

•Lengthen your body. Imagine you’re lying on soft sand; consider the imprint that your body would be making. Soften all 10 toes. Imagine the thigh bones dropping into their sockets. Feel the pelvis release heavily into the mat.
•Surrender your weight to the mat without collapsing: allow your position to have intention.
•Travel awareness up the spine: notice your lumbar curve. Is it flat towards the mat, or arched? Place the back of your hand into the small of your back to feel how much space you have there.
•Release the back of your ribcage. Bring a rhythm to your breath: in for a count of five, out for a count of six.
•Relax the shoulders and lengthen your neck. Make sure your face is parallel with the ceiling and your chin isn’t higher than your nose, or tucked towards your chest.
FINDING NEUTRAL – PELVIC TILTS
Stage 1
•Place your hands on your belly: connect your thumbs and fingertips to form a diamond shape, with the heels of your hands on your hip bones (bony parts of your pelvis) and your fingertips towards your pubic bone.

•Imagine your pelvis is a bowl of thick soup. At rest in neutral, the surface of your soup is level. Tuck your tailbone underneath you, tilt the pelvis and imagine the soup slowly tipping towards your belly button. Your lumbar spine releases into the mat, out of its natural curve.


•Send your tailbone away, visualise the soup tipping towards your heels. The lumbar spine is arched out of its natural curve.
•Come to a middle point where the soup is completely level. The pelvis is level. The lumbar spine is in its natural curve. This is neutral.


Breathing
Your breath is inextricably linked with your pelvic floor health and postnatal recovery. This might sound dull, but tweaking your breathing and focusing on it on a daily basis will mean that everything slots back into place quicker; it’s for this reason that if you visit a women’s health physio at this stage, the first session will focus on your alignment and breathing. What’s more, it also stimulates your nervous system response, which will calm your mind. This in turn releases tension in your body: a calm mind sends a signal to your body that it’s OK to switch off; it’s safe to heal.
Deep breathing is also useful if you’re trying to establish breastfeeding and it’s painful, or you’re generally feeling tense and anxious. Breathe out slowly and steadily while you put your baby on the breast, and soften into the discomfort rather than fighting it.
SCARF BREATHING
Stage 1
This exercise encourages you to find your full wide Pilates breath. The scarf gives you a feedback for where your ribcage is: you can feel your lungs opening and the intercostal muscles of your ribcage expanding as the ribcage widens into the scarf. You could also use a stretchy band or a yoga strap instead of a scarf.
•Sitting or standing, wrap a scarf or band around your lower ribs – just below your bra-strap area. Hold opposite ends of the band/scarf and pull it quite tight so you can feel there is comfortable tension around your ribcage and upper waist.
•As you breathe in, imagine your ribcage expanding to the sides like bellows. Allow the breath to expand into your ribs and then down into the abdomen.
Try not to overbreathe. Make sure your chest and shoulders stay soft and heavy.
•Sigh the breath out as if you’re trying to fog a window in front of you. Your hands should be able to draw the band across your body as the ribcage closes while the lungs empty.
Remember: breathe fully and naturally. If it feels forced, relax and allow it to soften into a more natural pattern. Pilates breathing will become normal with practice.

PISTON BREATH
Stage 1
Julie Wiebe is a physical therapist specialising in women’s health and postpartum recovery. She describes the Piston System of the diaphragm, pelvic floor and transversus abdominis (TA) working in conjunction with each other, in balance. The diaphragm is the starting point, needing space to open and perform its function effectively. That in turn creates space for the pelvic floor and TA to activate optimally.
Picture the torso as a cylinder. As you breathe in, visualise the diaphragm, and your pelvic floor and TA descending, like a piston. As you breathe out, the momentum is directly up, with the diaphragm and with the pelvic floor and TA. This is a natural functional momentum. If there is a weakness in the natural momentum, pressure will distend down or the abdominals will brace.

Inhalation
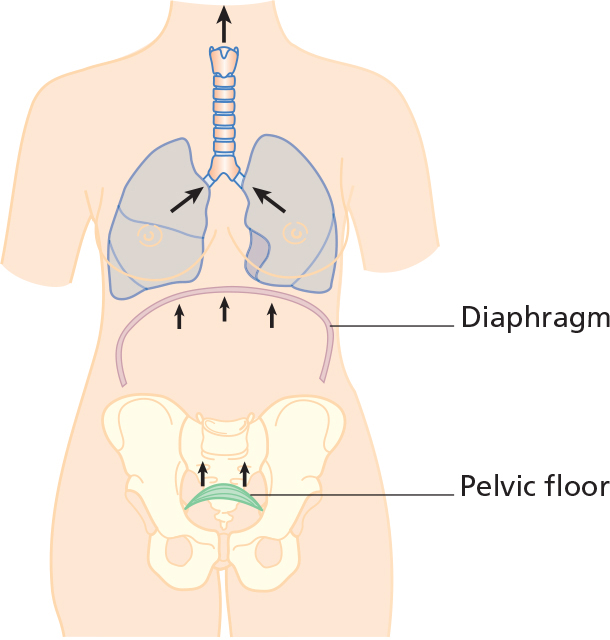
Exhalation
Tip
Take some time to notice your breath. Sit or lie with one hand on your belly, the other on your heart. Allow your hands to ‘listen’ to your body in stillness for a moment. Notice any movement through your torso with your breath. Allowing your diaphragm to fully descend, your abdomen will expand, and that is good – too many of us don’t ever release our abdominals, so they become tight and put pressure down into the pelvic floor – see Piston Breath, above, and also Sniff, Flop, Drop. This is one of the most important ways to begin allowing relaxation and release, and proper function of your abdominal/pelvic muscles.
Centring
Pelvic floor – finding your centre
How should it feel? How do I know if I’m doing it right? Remember Stage 1 of our postnatal journey. Pelvic floor awareness is key. You can’t strengthen what you can’t connect to.

Help! I can’t feel it!
Scar tissue from birth injury (whether vaginal or Caesarean birth) or overly tense core muscles may affect your awareness, control and sensation of your pelvic floor. So try not to feel frustrated with yourself if it seems impossible to find. It may be that there are physical or emotional factors blocking your connection. Try these tips:
⚬If you really can’t find your pelvic floor at all, try sucking your thumb, blowing on your hand, or coughing. This should trigger your natural pelvic floor lift. Persevere with the pelvic floor awareness exercises – it’s a subtle sensation, so it may simply be that you need to find that mindful connection to your body, and relax into it. Practise the Pelvic Floor Meditation every day to see if that helps.
⚬Palpate with your hands – on the outside of your pelvis, or inside your vagina (wash your hands first obviously): it’s your body! We’re quite squeamish about this part of our anatomy, but we really shouldn’t be, particularly after having a baby. Your own touch is very important post episiotomy or stitches to help break down scar tissue and encourage your sensation back. Find and visualise where the muscle attaches: feel your sit bones with your fingers, press your fingers around your pelvis.
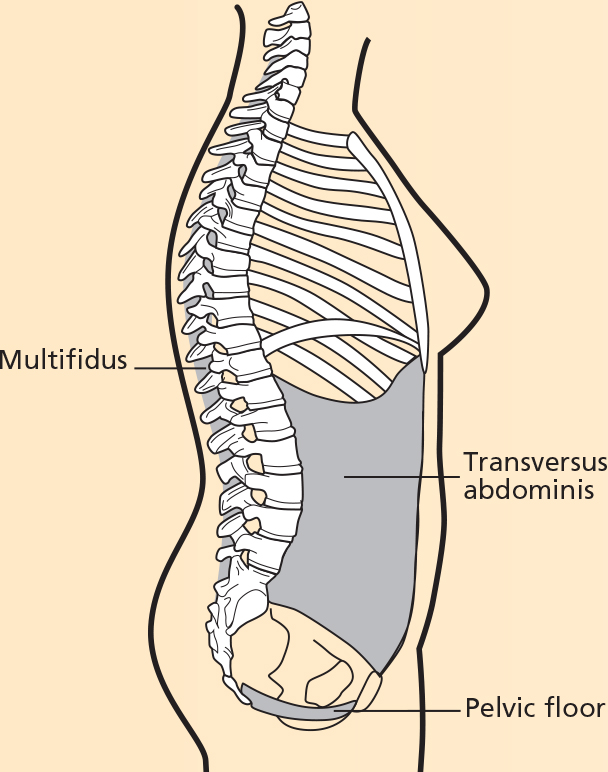
The ‘core’ muscles.
⚬Sit forwards a bit with a tall spine and then use your hands to pull your bum cheeks out from underneath you, to make sure you’re sitting on your sit bones. Hinge from the hips and lean slightly forwards. Imagine pulling all sides of your pelvic floor together and then up inside you through your vagina. It’s a very deep feeling, a bit like pulling up a tampon inside you. Try to pull up slowly, release and repeat 10 times, three times a day, every day. Then, once you’ve mastered a slow draw-up and hold, then try for 10 quicker ‘contract-release, contract-release’. There’s a hashtag started by the brilliant women’s health physio and stand-up comedian Elaine Miller (@gussetgrippers) #wewontpeewith10103: 10 slow-lift contractions, then 10 quicker contractions, three times a day – this genuinely will make a difference to your pelvic floor health if you actually do it.
⚬See how it feels to squeeze your finger inside you: if firing correctly, it should feel a bit like a baby sucking on your finger and you should be able to hold this for 5–10 seconds. If you cough, this squeeze should happen automatically. Having a tactile approach may help you to mentally connect to the engagement and unlock a physical sensation that was otherwise eluding you.
If you still struggle to connect – and particularly if you’ve found pelvic floor sensation elusive since your birth(s) or have been suffering from urinary or faecal incontinence – go to a women’s health physiotherapist without delay.

PELVIC FLOOR CONNECTION
Stage 1
Here we learn to soften to find your centre.
•Sit upright on a chair – or lie down if that helps you connect better. Your feet are hip-width apart, with your weight evenly released into your feet and sit bones.
•Sigh your breath out, then lift your back passage, as if you’re trying to stop breaking wind. Continue this lifting energy towards your pubic bone. Engage from back to front, up and in. We want to locate the full breadth of the muscles from the back to the front, and from the sides in. Imagine a diamond shape: the pubic bone at the front, the two sit bones either side and the tailbone at the back. Visualise the diamond shape drawing in and up from all points.
•Breathe in and let the engagement go: fully release it like dropping a marble into a glass of water.
•Repeat a few times.

Watchpoints
Scan your body for tension. Check that you haven’t also tensed your jaw, buttocks, inner thighs or are bracing your upper stomach. It’s an internal, outwardly invisible engagement. Yes, that includes your eyebrows. Keep them soft.
If you lose your connection, don’t feel frustrated. Take a breath and start again. With practice, it will become more natural.
Tip
Don’t practise this while sitting on the loo, stopping mid-flow while actually having a pee. That potentially creates bladder dysfunction by disrupting the message that you need to pee. You also might introduce the chance of a urinary tract infection. Please imagine stopping the flow of wee rather than actually doing it.
A note about pelvic organ prolapse and daily activities
Do you feel like daily baby duties, such as pushing your buggy, make your pelvic floor symptoms worse? If you have a vaginal prolapse, exertion can feel like it aggravates your prolapse symptoms*. Here are some tips if you’re struggling:
⚬Check your breathing. Are you holding your breath? Instead, try picturing your breath expanding out 360 degrees. On an inhalation, let your ribs expand and your tummy and pelvic floor soften. On the exhalation, allow for a gentle natural lift as you push the buggy up on to the pavement.
⚬Try a different tension strategy. Are you bracing and squeezing, trying to hold everything in as you exert effort? What happens if you ‘let go’ a bit?
⚬Try a change in position. Bring your hips back, or maybe forwards. Drop your ribs down, or broaden your chest. Can you feel a difference?
⚬Try to switch on your buttocks – this will help you to find the power to push. If you aren’t feeling your bum ‘kick in’ naturally, what happens if you actively try to engage your bum so that you can?
⚬Adopt a growth mindset: ‘I haven’t yet found the way to symptom-free buggy pushing so I’ll keep trying until I do’ versus ‘This is a disaster, I’ll never push my buggy without symptoms’. Challenge your limiting thoughts.
Essentially, do something different and see if it helps – this is always preferable to hoping something will magically get better on its own, or ignoring symptoms entirely. Your postnatal healing journey is not always about following set formulae and rules, but increasing your options and finding what works for you.
*Always go to a women’s health physio if you think you might have a prolapse.

PILATES TO BALANCE YOUR POSTNATAL BODY
Here are some key Pilates exercises that are perfect for the postnatal body. Master these, and you’ll be rebalancing your body and strengthening your core beautifully.
WALL POSTURE CHECK AND SIDE REACH
Stage 1
An easy one to build into your day to day as we are usually quite near a wall, and you can do this while making a cup of tea. Builds your general awareness of your posture, and stretches your spine, alleviating tension around the hips and pelvis.
•Stand with your back against a wall. Place your feet a comfortable distance away: about 30cm (12in) as a guide (but make sure it’s the right distance for your body proportions). The knees should be able to soften comfortably, directly above your ankles.
•Scan your natural posture. Is your head touching the wall? If not, don’t force it, just notice. In an ideal posture, the head lengthens upright away from the shoulder blades and therefore would be in contact with the wall, but in normal life we spend a lot of time stooped and this ideal alignment becomes more unnatural.
•Notice your upper spine. Can you feel your shoulder blades release into the wall? Can you feel the whole of the back of the ribcage or just part of it?
•Notice your lumbar spine. Is there a big gap away from the wall between your bottom and your shoulders, or are you almost flat against it? You can take your hand behind the small of your back and notice if you can thread your hand through the gap completely, or only slightly.
•Think about your pelvis. Is it level or tilted? Can you feel your sacrum (the ‘flat’ part of your pelvis) releasing back into the wall?
•Breathe in to float one arm out by your side, reaching the arm above your head.
•Breathe out to carry the arm across and lean on the diagonal. Maintain a connection with the wall with both shoulder blades.
•Breathe in to lengthen into the side stretch. Press your hips slightly in the opposite direction to increase the stretch in the side, if that feels OK to you.
•Breathe out to return to centre. Repeat on each side up to 5 times.


BACK STRETCH USING THE WALL/BUGGY
Stage 1
What mums need above all else is to stretch out, like a cat. You can do this stretch using a wall/counter top/buggy bar. It stretches your lower back and hamstrings, lengthens your waist, softens your shoulders and encourages you to breathe deeply and check in with your abdominal connection.
•Standing tall, at arms’ length away from the wall, place your palms flat against the wall/resting on the counter top/buggy bar.
•Send your bottom back so that your spine and arms are in one long line.
•Reach the arms away from the tailbone, keeping the neck in line with the spine – don’t collapse the head to look into your belly. Look down at the floor.
•Breathe slowly and deeply as you lengthen into the position. Allow your belly to soften, or draw it consciously in – experiment between the two to enhance your awareness of your centre engagement.
•With control, slowly restack your spine to upright.


SHOULDER STRETCH
Stage 1
We all suffer from shoulder tension, generally. Add mother duties to the mix – nappies, buggies, endlessly picking up toys and socks, continually holding your baby/toddler on one side – and you’re much more likely to hunch forwards. This is a blissful way of stretching out, massaging and mobilising your upper (thoracic) spine. It’s a great posture check on the go.
•You can do this standing or sitting. Take the hands on to the shoulders. Bring the elbows together. Imagine the collarbones are wide and open.

•Breathing normally, keep the elbows together and roll them up towards the ceiling. Allow your eye focus and nose to follow their trajectory and open your chest to the ceiling.

•Open the elbows wide and circle them out by your sides, as if you’re spreading wings.
•Bring the elbows back together and allow your head to restack on the top of the vertebrae of your spine.

•Repeat up to 5 times, then reverse the direction.
•Release one arm down and place the palm down on your inner thigh. Keep the other on the shoulder.

•Open your chest out to the side, then extend your arm up and away.
•Repeat up to 3 times. Breathe deeply and keep the lumbar spine lengthened, not tucked or arching.

SHOULDER STRETCH AGAINST THE WALL
Stage 1
This is a really amazing stretch, particularly for the first few months postnatally, although three years postnatal with my second, I still do this most days. It’s a must for opening the chest and releasing tension from buggy stoop. Be gentle with this if you are breastfeeding as the pull on your chest might make your boobs feel tender.
•Stand against a wall, side on. Place your hand on to the wall and then walk it up to shoulder height, then a little bit higher.

•Placing gentle pressure into the wall, keeping the arm softly bent, reach the fingertips away. You can lengthen the arm either in line with your shoulder, or reach higher in a diagonal – whichever feels better for your shoulder joint. Rotate as far as you can feel a stretch into the front of the chest/armpit. Breathe into the stretch.

•If it feels nice, and the mobility is available to you, you can add a full Arm Circle.

•Release your arm and then repeat on the other side.

PELVIC STABILITY
The following exercises are great ways of enhancing your core stability and building deep inner strength by introducing movement of the limbs to challenge your control of your pelvis.
LEG SLIDES
Stage 1
In Relaxation Position, you could rest your hands on your belly, to check for any movement of your pelvis. You can also do this with the ball underneath your pelvis, as for Compass, for extra challenge and feedback.
•Breathe in, lengthen your spine.

•Breathe out, stabilise and slide one leg along the floor, in line with your hip. Maintain your neutral pelvis and spine.

•Breathe in wide, stay active in your centre and return your leg to the start position.
Watchpoint
Make sure your pelvis and spine remain stable and heavy throughout; no rocking.
KNEE DROPS
Stage 1
Really concentrate on the quality of your movement with this exercise: notice whether your pelvis moves and see whether you can develop the strength and control to ensure your pelvis stays stable as you move the thighbones in their sockets.
•Start as for Leg Slides on previous page. Breathe in to prepare, stabilise. You may find that you need to ‘turn up’ your engagement appropriately, to control the movement.

•Breathe out and open one leg out to the side, allowing the foot to roll on to its side. Open the knee as far as you can without disturbing the pelvis. The hip bones (bony parts at the front of your pelvis) should remain parallel with the floor.
•Breathe in to return the leg back to centre.
•Repeat up to 5 times on either side.

Watchpoints
Control the movement. Try to avoid letting the stable leg wander out to the opposite side. Imagine your hip bones are headlights: they should stay shining up to the ceiling as you move the thighbone away from the body, not travel in the direction of the leg.
If it helps, you can bring your hands underneath your buttocks, palms down. Repeat the exercise and notice if you’re sinking your bottom into one hand as you open the leg. See whether you can connect to your centre to ensure you distribute the weight evenly through each side of the pelvis, even when moving the leg challenges this stability. This is core control.
BAND PULL WITH KNEE DROP
Stage 2
This exercise challenges your coordination and core strength. The opposite arm and leg movement creates a diagonal engagement across your torso from shoulder to opposite hip – Body Control Pilates® calls it the ‘X factor’ – which requires deep abdominal strength to keep you stable. Great for rehab for diastasis recti, it’s a low-impact, supported way of getting those abdominals working once more.
•Start lying in Relaxation Position. Hold a band or a scarf in both hands. Raise both arms up above the shoulder joints, with tension in the band.
•Breathe in to lengthen the spine.

•As you breathe out, open your left arm to the side, pulling the band, but keeping the right arm stable. At the same time, open your right knee out, keeping the pelvis stable.
•Breathe in to return to centre.
•Repeat up to 10 times on each side.
•You can also add Single Knee Folds and Leg Slides to the arm pull.

Watchpoints
Keep your pelvis stable and collarbones wide.
Keep the arm straight; try not to bend at the elbow or wrist as you open the band.
SINGLE KNEE FOLDS WITH PELVIC FLOOR WORK
Stage 2
This requires abdominal control. Keep in mind your neutral pelvis throughout.
•Lie in Relaxation Position

•On an out-breath, float one of your knees towards your chest. Maintain the angle at the knee; try not to let the heel slump towards your bottom. Let the thigh bone drop into its socket, but not so far that the thigh flops into the chest. The shin is parallel with the floor. Your pelvis remains neutral, tailbone heavy. If it feels too easy and there’s no effort at all, you’re probably cheating.

•Breathe in to release the foot down.
•Breathe out and repeat on the other leg.
•Experiment with your pelvic awareness: float one knee in, then tuck your pelvis underneath you.

•Using your core control, release your tailbone away from you.
•The thigh bone will move with the pelvis.

•Return back to neutral.
•Next, place your hand against the thigh. Breathe in to lengthen.
•As you breathe out, press your thigh into your hand and your hand into your thigh – as if you’re pushing with equal pressure from both sides. Engage your pelvic floor and lower abdominals strongly as you push.
•Breathe in and release the pressure. Relax. Repeat up to 5 times.

Watchpoints
Fold the knee in line with the hip, not out to the side or across the body.
When pushing into your thigh/hand, ensure that you’re not bracing anywhere else in your body. You should feel that your core is active and strong, but everywhere else is relaxed.
OYSTER
Stage 2
This exercise targets your deep gluteal muscles: such important stabilisers of the pelvis and the number one area that mums generally need to strengthen.
•Side-lying, take your feet in line with your bottom, lined up against the side of the mat. Place your top hand in front of your chest, palm down. Or, you may prefer to have your top hand resting on your top hip bone so that you can check for any movement of the pelvis.
•Breathe in, lengthen your spine.

•Breathe out and engage your buttock muscle to open the top knee. Imagine turning your thighbone in its socket like a key in a lock. Keep the feet connected, pressing towards each other like magnets. Your pelvis remains stable and upright. Breathe in and return the knee back to the start position. Imagine you’re working under water – there is resistance in the movement.
•Repeat up to 10 times, then change sides.
VARIATION
Stage 3
To add a bit more challenge to your stability and really find those deep gluteal muscles, lift the leg to hip height.
•Breathe out and turn out the leg in the same way, but with the leg lifted.

•Breathe in and rotate the thighbone the other way, turning the knee down towards the bottom leg.
•Repeat up to 5 times, then lower the leg back down.

Watchpoints
If you can’t feel this in your bum, don’t worry – bottoms are renowned for being lazy and hip muscles easily take over. Tip your pelvis slightly forwards to make sure your hip muscles aren’t working too hard, then try again. You should feel the bum working harder from this angle.
Only go as far as you can keep the pelvis still: the thigh moves independently of the pelvis.
RIBCAGE CLOSURE
Stage 1
Shoulders can get very tight, which can lead to neck and shoulder pain. Your ribcage flares during pregnancy to accommodate your baby growing higher within your torso. Postnatally we need to gently reset our postural patterns and be able to soften the ribs back to their pre-pregnancy position, to help to re-establish good breathing and optimum pelvic floor function. This exercise shows you how to isolate the movement of your shoulders from your torso, connect to your abdominals and become more aware of the stability of your ribcage. You can also do this with a band/scarf, as for ribcage closure with leg slides.
•Begin in Relaxation Position.
•Breathe in and raise both arms up towards the ceiling, palms facing forwards.

•As you breathe out, reach both arms back behind you. Maintain a space between your shoulders and your ears. Feel the back of the ribs melting down towards the mat, rather than rising up away.

•Breathe in and release the arms back towards the ceiling. Move with purpose and feel resistance in the air, as if you’re under water. Breathe out and lower them back towards the floor.
•Repeat up to 10 times.
Watchpoints
Only take your arms back in line with your ears.
Avoid arching the back as shown here: soften the ribs so that they don’t ‘follow’ the arms.

COMPASS
Stage 1
This exercise helps you to build awareness of your pelvic area and is great for gently building pelvic floor strength, stretching your hip flexor muscles and releasing tension in your back. You can also do this with a small Pilates ball underneath your pelvis for feedback.
•Start in Relaxation Position. Your lower belly is a compass. Your navel is north, your pubic bone is south and your hip bones on either side are east and west. Breathe in, lengthen the spine.

•Breathe out and tuck your tailbone underneath you, then tilt the pelvis to north, releasing the lumbar spine into the mat.

•Breathe in and roll towards south. The pubic bone moves away from your nose, tilting your pelvis forwards to allow the lumbar spine to softly arch.

•Breathing naturally, repeat this north–south movement a few times.
•Come back to neutral and relax the shoulders and hips. Breathe in to lengthen and prepare.
•Breathe out and this time, roll your pelvis across to east. The opposite buttock will slightly lift off the mat. Keep the feet heavy on the floor.

•Breathe in and roll across to the other side, softening your weight on to the other hip, rolling the pelvis to west.
•Repeat a few times. Become aware of when your pelvis is tilted and when it’s in a neutral position.

Watchpoints
Keep the knees still and the ribcage and shoulders heavy. Isolate the movement in the pelvis. Keep the waist long. Imagine you have a mirror above you: your torso remains at the same placement on the mat; it’s a pelvic rotation only so there should be no shortening of the waist. Imagine your pelvis moving around your thigh bones, rather than letting the thigh bones move from side to side. This is a great way of oiling the hip joint.
Check that you’re not moving too far south and uncomfortably arching the back.
CASE STUDY

Ella, mum of one
If I’m honest, I was in a state of physical and emotional shock after giving birth. I was really lucky to have a straightforward, natural, vaginal delivery but I remember feeling utterly traumatised by how broken my body felt after a three-day labour. I had done NCT classes and remember the NCT teacher saying that the first wee after labour would hurt but after that everything ‘down there’ would feel normal again… For me it took a good six months for things to feel anywhere near normal.
At three months postpartum I was diagnosed with a grade one uterine prolapse. The fact that this could happen to me, when I was young, healthy, not overweight and active both before and during pregnancy, was a total shock.
Pilates and women’s health physio really helped my recovery. I started going to a postnatal Pilates class about five months after the birth and I feel like I only really started to heal my body properly after discovering Pilates.
I have had several ‘aha moments’ during Pilates when I suddenly understood how to correctly engage my deep core and pelvic floor muscles; after months of thinking I was doing it right I realised actually I hadn’t been. In fact, I think Pilates has helped enhance my understanding of my entire body.
CENTRING IN FOUR-POINT KNEELING
Stage 1
This is one of the best positions to achieve deep lower abdominal recruitment, engaging your stabilising muscles without moving your spine. You spend a lot of time on all fours with babies and toddlers, so this gives you a way of making it a strengthening activity, checking in with how you carry yourself in your normal movement.
•Place your hands directly underneath your shoulders, your knees directly underneath your hips.
•Imagine you’re looking at your reflection in a mirror in front of you and lengthen the space from your nose to your breastbone, your breastbone to your navel, your navel to your pubic bone. Take care not to nod your head towards your reflection. If there were a pole placed on your back it would be in contact with your head, mid-back and pelvis.
•Reach the crown of your head forwards and the tailbone back in opposition.
•Try to release into the natural curves of your back. Imagine a friendly cat could curl up in the lumbar curve, but make sure you are not collapsing into an arch. Soften the shoulder blades and lengthen your neck, as if you’re a tortoise pushing its head out of its shell.
•Breathe in, allow your abdominals to soften and release. Make sure you don’t let the spine drop; stay lengthened.
•Breathe out and draw in from the back passage, bringing this engagement towards your pubic bone. Feel your belly lifting gently in, softening the lower rib towards the top of the pelvis but without moving the spine. Make sure there is no tucking of your pelvis. Think back to your reflection in front of you: the distances should remain even and the torso long.

PRONE LEG CIRCLES
Stage 2
This exercise opens the hip joint by working the gluteal muscles (buttocks). It encourages you to find mobility in the hip while keeping the pelvis stable.
•Lying on your front, rest your forehead on a pillow. Your legs are in parallel and hip-width apart. Place your fingertips underneath your hip bones. Feel the pressure that your body weight releases on to your hands. Through this exercise we are aiming to have the pressure stay level on both hands rather than dip into one hand more strongly than the other with the movement. It will take practice! If it’s uncomfortable, take your hands up in line with your head, palms down, with your forehead on your hands.
•Breathe in to lengthen the spine.

•Breathe out and draw in to your centre. Lengthen and lift one leg away from the floor, opening the hip. Imagine reaching your leg long, towards the wall, away rather than high. You should feel the pressure on that hand remains the same and your lower spine stays soft.
•Draw into your centre. Circle the thighbone 6 times in one direction, then change direction. Feel the movement coming from the top of the thigh, the bottom and hip.

•Breathe in to release back down.
•Repeat up to 3 times on each leg.
Watchpoints
Only lift the leg as high as you can without disturbing the pelvis and arching the back.
Try not to circle from the knee or ankle. Reach out from the hip and feel the buttock muscles fire up.
MOVEMENTS OF THE SPINE
A good Pilates session, however short, will incorporate all movements of the spine. This is to equip you well for your functional daily movement, such as when you’re getting up off the floor 300 times a day with baby-related tasks. In each workout, try to balance your body with some flexion (forward bending), extension (backward bending), lateral flexion (sideways bending) and rotation (twisting).
Spinal flexion
Pilates works on fluid sequential movement of the spine, each vertebra moving evenly and independently, like a string of pearls or a bicycle chain. Flexion is the forward rolling movement of the spine.
ROLL-DOWNS AGAINST THE WALL
Stage 2
Mobilise your spine, release tension and wake up your abdominals.
•Stand against the wall. Release your spine fully into the wall, allowing for your natural curve to lengthen, with your feet a comfortable distance away, knees softly bent.
•Breathe in. Lengthen the back of your neck, look down your nose and nod your chin.

•Breathe out, roll your spine forwards, soften your breastbone and peel the spine off the wall, bone by bone. Roll until you reach a point where your pelvis remains upright. Keep your bottom relaxed against the wall.
•If you wish, and feel you have the abdominal strength, allow your hips to hinge now and roll your spine all the way forwards. Keep the knees softly bent. Breathe in, soften your head and arms and relax your neck.

•Breathe out, lengthen the tailbone and unfurl the spine, wheeling back up against the wall, bone by bone. Release the ribcage against the wall, lengthen the head back on top of the spine.
•Repeat up to 5 times.

Watchpoints
Spread your weight evenly on your feet. Try not to rush. When you rebuild, your head is the last thing to restack on top of your vertebrae. Completely relax the neck and shoulders, allow them to hang towards the floor like a ragdoll.
CAT–COW
Stages 1–2
This is a great one to do at the end of a chaotic mothering day to soothe your system. And if you are feeling low or depressed, tapping into a feeling of strength by pushing actively into the floor with your hands can ground you and be a way of finding a sense of power.
•Begin in Four-point Kneeling.
•Breathe in to prepare and lengthen your spine.
•Breathe out and begin to send your tailbone through your legs, rolling the pelvis. Ripple the movement evenly through the spine, flexing each bone away from the one before it. Roll through the hips, the waist, the ribcage, then finally nod the chin softly towards your chest. It’s an even flexion of each section of the spine, creating a rainbow ‘C-curve’ shape.

•Breathe in wide into the back of the body as you maintain this shape.
•Breathe out and begin to lengthen the tailbone away from the crown of the head to open the front of your body back to a neutral position.

•Breathe in and lengthen your spine, and as you breathe out, allow the chest to open forwards as if you’re shining your heart forwards. The lower spine is supported and not collapsed: you are trying to extend into the upper back.
•Repeat up to 10 times, then press yourself back into Rest Position.

Watchpoints
Your body will want to press up into the ribcage area and fully hunch, which feels really satisfying: but try to focus more on the tuck of the pelvis, full flexion of the lumbar spine. Allow it to be a smooth, even curve throughout.
Make sure your shoulders aren’t hunched towards your ears.
Check that your arms aren’t locked: the soft part of your elbows should be facing towards each other, not to the front.
Make sure as you shine your heart forwards that you don’t overextend your neck: feel a soft pull forwards from the breastbone and allow the neck to stay aligned with your ribs.
REST POSITION
Stage 1
This position stretches the back, nourishes your internal organs and encourages your breath into the back of your body. Perfect for mums for two seconds’ peace. Releasing the forehead down is a lovely way to trigger your ‘rest and digest’ system. It’s also an easy way to turn yourself into a climbing frame ‘rock’ for your little ones while you take five deep breaths...
•Start in Four-point Kneeling.

•Breathe in and lengthen the spine.
•Breathe out, release your bottom back towards your heels, hinging at the hips. Lengthen your arms out in front of you, feeling a lovely stretch around the shoulder area. You can creep the fingertips forwards and pyramid them on the floor to increase the stretch if that feels comfortable for you. Allow your tailbone to feel heavy, releasing your sit bones towards your heels. Soften your thighs into your pillow if you have one there. If it feels more nourishing for you, float your arms around so that your hands rest on your feet and you give yourself a little hug. Relax the shoulders completely.
•Allow the forehead to soften into the mat, or on to a pillow. Relax your neck completely.
•Breathe in and allow the breath to travel all the way down your spine towards your pelvis. Relax your belly.

•Keep breathing here for a few breaths, allowing your bottom to release down more heavily with each breath.
•Gradually draw more energy into your centre and as you breathe out, slowly roll back up to sitting, releasing your bottom back onto your heels as you restack the vertebrae of your spine back to upright. Be careful not to come up too quickly, as you’ll get a head rush.
SPINE CURLS
Stage 2
This exercise irons out your spine and releases compression, offering you meditative space for breathing. Place a small ball between your knees for a bit more connection to your centre.
•Start in Relaxation Position.

•Breathe in. Lengthen your spine.
•Breathe out and roll your tailbone underneath you, releasing the lumbar spine into the mat. From there, press your feet into the floor as you peel your spine bone by bone, rolling evenly like a bicycle chain, until you reach the bottom of your shoulder blades – or slightly lower.

•Breathe in, sending the knees away over the toes.
•Breathe out, soften your breastbone and release your spine back down, keeping your buttocks lifted and pelvis tucked under until you reach the floor.
•Breathe in to let go of any tension in the shoulders and hips, before repeating on the out-breath.
•Repeat up to 10 times.
Watchpoints
Keep your feet heavy.
Try to find an even sequential movement of your spine: make sure you’re not bridging up through any sections as shown here.
Maintain an active connection in the front of your body: soften your bottom rib down into the body as if you’re tucking your top into your trousers. Imagine your ribs are connected to your hips with elastic bands: you want the bands to stay taut, not stretched too far.

BRIDGE WITH DOUBLE KNEE DROP
Stage 2
The beauty of this exercise is that we’re working in a ‘closed chain’, whereby your feet and arms are supported by the floor, so there is never too much load going through the pelvis or pressure on your abdominals, but it still really works your core. It also strengthens your buttocks, and challenges your pelvic stability. Be cautious with this variation if you’re still suffering from pelvic girdle pain (PGP).
•Start in Relaxation Position. Breathe in to prepare your body for movement and lengthen the spine.
•As you breathe out, press the hips and spine in one connected unit up off the mat, hinging from the hips, not rolling sequentially as for a Spine Curl. Ensure that your spine doesn’t arch, squeeze your glutes and soften your ribs.
•Breathe in to lengthen, relaxing your shoulders.

•Breathe out, and keeping the bottom lifted, open your right knee to the side, without allowing the right hip to dip. Keep the pelvis stable as if resting on a shelf. Breathe in to stay lengthened.
•Breathe out and open the other knee. Breathe in to lengthen the spine.

•Breathe out to bring the first knee back in, followed by the second. Then, as you breathe in lower the hips down in one go, with the knees apart.
•Push the hips back up on your out-breath. The knees are apart, like ‘frog’s legs’. Repeat 5 times, then bring one leg back to centre followed by the second, then lower the spine down with control.

MAKE IT HARDER
Vary the challenge by slowing down your movement, or making it quicker.
SPINAL EXTENSION
Extension is essential for strengthening the back muscles to counterbalance the motherhunch that all baby duties encourage: changing nappies, pushing buggies, feeding, scrolling on your phone... Small babies should be placed on their front regularly so that they develop these back muscles and create strength for movement – they’ll never learn to crawl if they aren’t placed on their front regularly – and good upright posture. Tummy time is just as essential for mums!
DART
Stage 2
The perfect mum-stoop antidote, this targets those mid-back muscles that are so important for good posture.
•Lie on your tummy. Rest your forehead on a folded towel, or a small flat cushion. Release your arms down by your sides, palms facing up. Your legs are relaxed with your toes together and heels releasing apart. Breathe in to lengthen and prepare.

•Breathe out. Initiate the movement first with your head lengthening away from your spine. Feel your chest open and shoulder blades drawing down on your ribcage, as you begin to peel your chest away from the floor. Stay in contact with the mat with your lower ribs. Your eye focus is down. Lift your arms to reach down by your sides, rotating them so that your palms now face the floor and your shoulder blades draw towards each other. Simultaneously, connect your heels together, engaging your inner thighs to bring your legs into parallel.
•Breathe in and lengthen the spine to maintain this long dart shape, reaching the crown of your head away from your toes.

•Breathe out and release your chest, head and arms back to the floor with control. Soften the legs open.
•Repeat up to 10 times, then release back into Rest Position.

Watchpoints
Your eye focus stays down towards the floor, neck long and in line with your upper back.
Feel this in the mid-back postural muscles, around the bra strap area, not lower, in your lumbar spine. Stay low and long to avoid compressing your lower back.
SPINAL ROTATION
Your ribcage is an area prone to stiffness, pain and tension throughout pregnancy and into motherhood. Twisting movements will help to alleviate some of this and keep the whole spine and the systems of your body balanced, healthy and functioning well. It’s so important for your postnatal recovery to encourage your breath wide into the ribcage to help stimulate optimum pelvic floor function.
Twisting is also the movement that you’ll do 73,000 times a day lifting your baby out of their cot or bath, or placing your toddler in the car seat (i.e. twisting while carrying a heavy weight), so it’s very important to make sure you’re mobile and strong enough not to injure yourself in these daily movements. Having badly injured my knee simply by standing up from crouching with my baby in the sling, I know how frustrating and pointless (yet common) that scenario is.
CHALK CIRCLES
Stages 1–2
This is a soothing exercise, supporting controlled mobilisation of the spine, stretching the chest, requiring fluid movements of the shoulder joint with rotation of the spine. It massages your internal organs, encouraging space within your torso. The perfect Pilates exercise for mums.
•Lie on your side. Place a cushion or small ball in between your knees. Make sure your head is in line with your spine: a couple of flat pillows or one bigger cushion should be fine. Lengthen your arms out in front of you, palm on top of palm.
•Breathe in and travel the top arm along the floor, up above your head. Rotate the head in line with the palm.

•Breathe out as you continue to move the hand above your head, drawing a circle along the mat or hovered slightly above. Open the chest to roll the spine back, allowing the arm to open back behind you. Keep looking towards your hand. The hips, knees and ankles remain stacked and still.

•Circle the arm back down towards your hip and then back to the start position.
•Repeat up to 8 times.

VARIATION
Stage 2
Add a leg extension to give a lush opening to the side of the body and add a bit more challenge to your strength and coordination.
As you begin to twist your torso and reach the arm in the diagonal above your head, lengthen your top leg away in opposition, so you’re drawing a straight diagonal line from your fingertips to your toes, squeezing the ball or cushion. Feel the length across the top of your body, while maintaining a strong centre.

Watchpoints
Make sure the movement comes from your torso twisting, not just from the arm reaching back. Only roll as far as you can maintain eye contact with your palm, as though your nose and your middle finger were connected by a puppet string.
Relax the shoulder away from your chin: there should be a space between the neck and the shoulder.
CASE STUDY

Elizabeth, mum of two, postnatal PT and doula @themummycoach.co.uk
In the months that followed my second child’s birth, with a toddler and a newborn to care for, I didn’t have much time or energy for exercise. For many months my routine focused solely on Pilates. I’m a runner and used to high-impact exercise so at first I found it slow and strange. It took me right back to basics, forcing me to focus on my breathing and posture and helping me to restore a solid foundation. I loved the fact that I could practise without leaving the house and didn’t need masses of equipment. Pilates truly felt like it nourished my post-baby body from deep within.
HIP ROLLS
Stage 2
This is a feel-good twisting exercise. Use your core muscles to roll with control, rather than using the momentum of rolling the legs from side to side. This exercise targets the oblique abdominals in the waist, and the inner thighs. If you have diastasis recti, be cautious of doing too many reps of this: overworking the oblique muscles places a pull on the linea alba, so build it up slowly, focusing on your deep core engagement. This version adds a much-needed chest opener by having the arms lengthened above your head in a Y shape – but if this is tricky for your shoulders or feels in any way uncomfortable across the upper body, bolster your arms with pillows or have the arms released down by your sides in a low upside down V (Stage 1).
•Lie in Relaxation Position, with your knees and feet connected: imagine you’re holding a diamond between your knees and you don’t want anyone to steal it. You can squeeze a pillow or small ball between your knees if it helps you to maintain the connection. Reach your arms up to the ceiling and lengthen them behind you, released on the floor in a wide Y shape. Palms up.

•Breathe in, lengthen the spine.
•Breathe out. Keeping the legs connected, roll your pelvis to the left, rolling your knees to the left. The right side of your bottom will lift as you roll. Keep the feet moving together – they will peel off the mat as the body rotates. The spine moves sequentially: pelvis, waist, ribcage, as for a Spine Curl.

•Breathe in and maintain the position. Feel the fingertips of your right hand reaching away in opposition.
•Breathe out, then ‘turn up the brightness’ of your centre to return your spine and knees back to the start position with control.
•Repeat on the other side, and to each side 5 times.

Watchpoints
Keep your waist long.
Soften the bottom rib towards the top of the pelvis, to ensure you’re not arching your back.
Keep your legs connected into your centre: try not to let them ‘hang’ off the pelvis without control.
LATERAL FLEXION
Involving side reaching, lengthening the waist and rolling the vertebrae of the spine to the side, lateral flexion is so important for mums to stretch tight hips and even out the body.
PLIÉS WITH SIDE REACH
Stage 2
A double boost – work on your buttock strength and ankle-knee-hip alignment, while at the same time doing a fabulous side stretch to open up your waist, challenge your balance a bit and release tension.
•Begin in Pilates Stance: stand tall, with your heels connected and your toes hip-width apart. ‘Zip up’ your connection between your inner thighs and gluteal muscles, as if you’re wearing a tight pencil skirt. Lengthen your spine and release your arms down by your side.
•Breathe out and bend the knees directly over your toes, into Plié. At the same time, lengthen your left arm up and out to the side and begin to bend your upper body over in a diagonal to the right. Only go as far as you can keep the pelvissquare.

•Breathe in to return to the centre, straighten the legs and lower the arm down. If you wish to add further challenge, keeping the heels and thighs working together, rise up onto your toes then release the heels back down.
•Repeat to the other side. Repeat up to 10 times in each direction.

Watchpoints
Ensure your spine doesn’t bend forwards, or twist. This should be a purely sideways reach.
Stay lifted in the supporting side of your waist, lengthening evenly in a diagonal as if between two panes of glass.
UPRIGHT HIP FLEXOR SIDE REACH
Stage 2
This is a wonderful stretch that is slightly challenging for your core as it requires balance and stability, so stick with the lying version of Hip Flexor Stretch in the next chapter if you feel any niggling in your lower back.
•Start in Four-point Kneeling, then bring your right foot forwards. Place your hands on your right thigh and lengthen yourself upright. Keeping a strong connection to your centre, release your weight slightly forwards to open up into the hip flexor.

•Breathing in, float the left arm up towards the ceiling, maintaining a space between the arm and the ear.
•Staying strong in your centre, breathe out as you reach the arm over to the right.
•Feel a stretch in the waist and hip. Breathe in to the stretch.
•Release back to centre. Repeat on the other side.
