CHAPTER 4
Concussion Assessment
While the diagnosis of a concussion needs to be made by a medical professional, a concussion is both a medical and an educational issue. Concussions may occur in an educational setting and therefore school personnel may serve as first responders. Further, this medical issue can lead to educational needs that must be addressed with school-based accommodations. School personnel need to be informed about concussion assessments that occur in the medical and athletic setting. They also need assessment tools to track a student’s recovery and evaluate the efficacy of academic adjustments.
In this chapter, the reader first learns about simple tools that can be used by school personnel to assess concussion symptomology at school. These include checklists that can be used by nurses or other school staff when a concussion is sustained at school. There is also information on the use of computerized neurocognitive assessments and sideline assessments for student athletes. Additionally, smartphone concussion evaluation apps are discussed and guidelines for appropriate use are described. The chapter also includes information related to the clinical evaluation of a concussion that a child might receive in a medical setting.
Next is information on how school personnel can conduct ongoing assessment of a student’s concussion symptoms, as well as progress monitoring of the efficacy of academic adjustments. The chapter concludes with a brief section on the future of concussion assessment. Readers are advised to stay current on this information, as medical and technological advances may soon lead to more sensitive tests that allow for more objective evaluations of concussions.
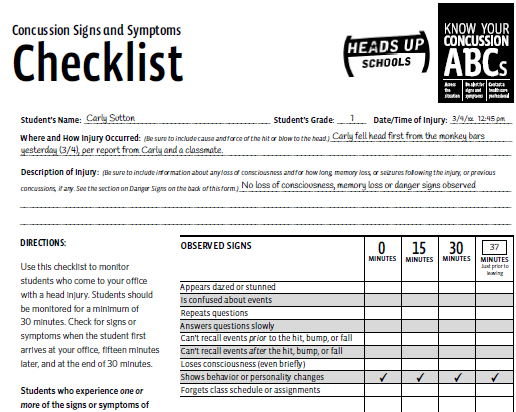
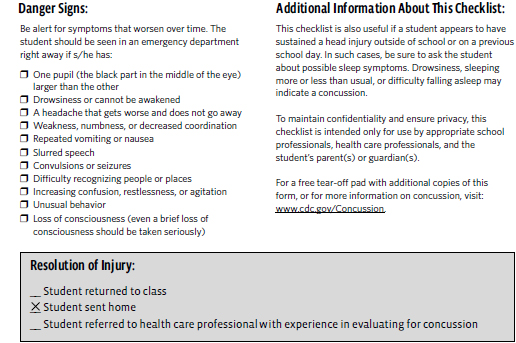
CONCUSSION SIGNS AND SYMPTOMS CHECKLISTS
Children and adolescents who have sustained a concussion will experience one or more symptoms from one or more of the symptom categories described in Chapter 2 (physical, cognitive, emotional, and sleep). The Concussion Signs and Symptoms Checklist (see Exhibit 4.1), provided free of charge from the Centers for Disease Control and Prevention (CDC), can be used to monitor observed signs (physical, cognitive, emotional) if a student sustains a possible concussion at school, or if the student arrives at school reporting a possible head injury that occurred earlier, outside of school or on a previous school day. It is recommended that the concussion team leader (CTL) and main office staff keep copies of these checklists on hand for use in the case of any suspected concussion.
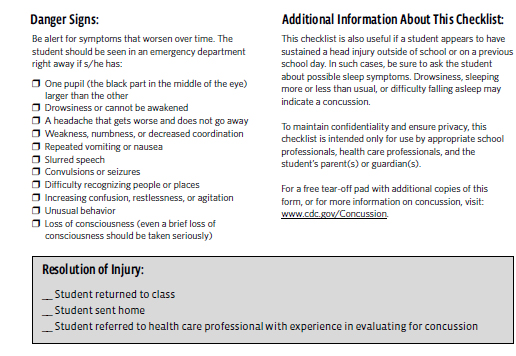
The evaluator uses the form to check for signs or symptoms upon arrival, 15 minutes later, at the end of 30 minutes, and before the student leaves. Children experiencing one or more signs should be referred to a health care professional with experience in evaluating concussions. The evaluator should provide a copy of the form to the parents to give to the doctor and keep a copy for school records.
In addition to listing possible signs of a concussion, the form has a section on Danger Signs, which indicate the student should be seen in the emergency department right away. The form also includes a section for documenting resolution of injury and comments. The name and title of the person completing the form are also included, which allows an outside medical professional to know the background of the person completing the form, be it the school nurse, an office aide, or someone else.
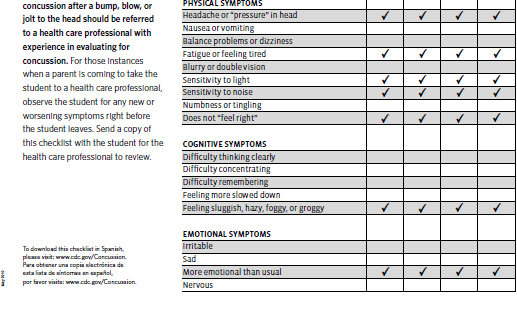
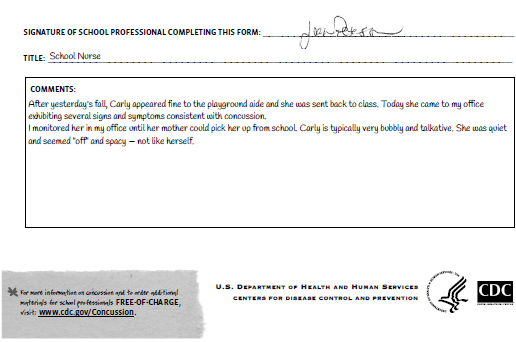
Carly
When Carly returned to school she told Mrs. Lang that she had a headache and felt “funny.” Mrs. Lang sent Carly down to the nurse’s office. The nurse completed the CDC’s Concussion Signs and Symptoms Checklist (Exhibit 4.2) based on how Carly appeared and what she was reporting at that time.
While it would have been better if this checklist had been completed upon injury, this documentation allowed the school staff to make a more informed decision about what to do next. They called her mother and recommended that she take Carly to the doctor to be evaluated for a concussion. They asked her to take a copy of the Signs and Symptoms Checklist with her and made a copy for their records.
EXHIBIT 4.1
Concussion Signs and Symptoms Checklist.
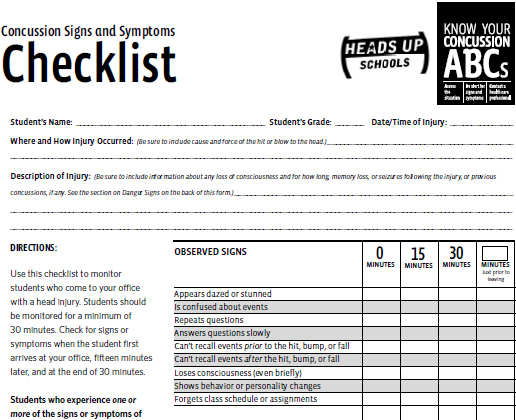
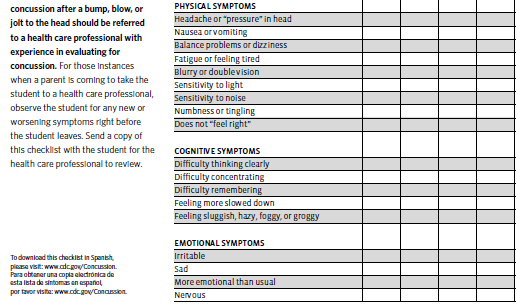
From Centers for Disease Control and Prevention.
The “takeaway” from this scenario is that the nurse does not have to be the one to complete the Signs and Symptoms Checklist. This tool, or a similar one, should be readily available to anyone in the school who might be informed about a student’s possible concussion, including all office staff. It is not used to make a definitive medical diagnosis, but it can be a valuable piece of information to give to the parents, who can then share it with the medical provider. There is a line on the form for the “title” of the person completing the form, so any medical provider reviewing the form would know if was completed by a nonmedical informant.
EXHIBIT 4.2
Carly’s concussion signs and symptoms checklist.
Another useful form from the CDC is the Acute Concussion Evaluation (ACE; Gioia & Collins, 2006) for initial evaluations (see Figure 4.1). The ACE can help the school concussion team obtain information regarding the injury, including the cause, severity, any amnesia, loss of consciousness, and any early signs. The form asks the patient to report the presence of symptoms in four categories: thinking/remembering, physical, emotional, sleep. It also assesses for risk factors, such as history of injury, developmental history, and psychiatric history; provides a warning of red-flags and applicable diagnostic codes; and encourages the development of a follow-up plan. Originally designed for medical providers, this form could be administered by the school psychologist or school nurse. It is more comprehensive than the Concussion Signs and Symptoms Checklist.
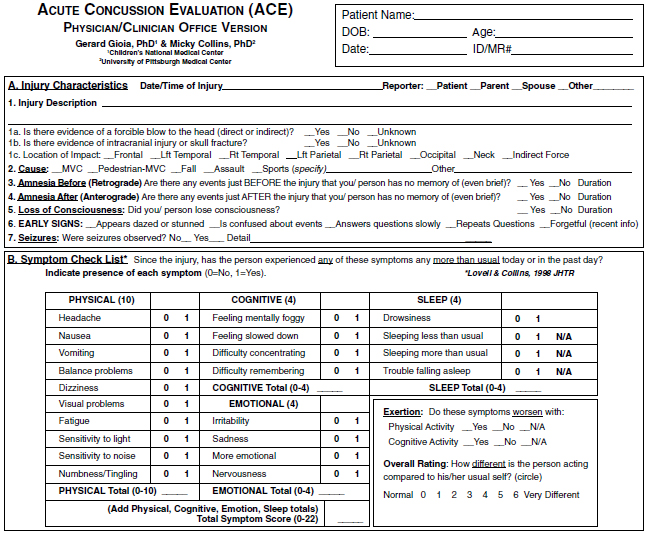
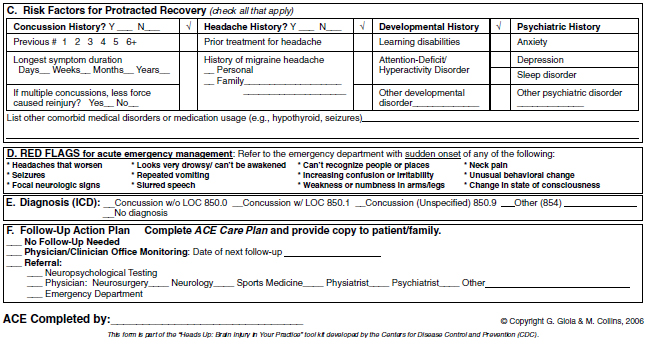
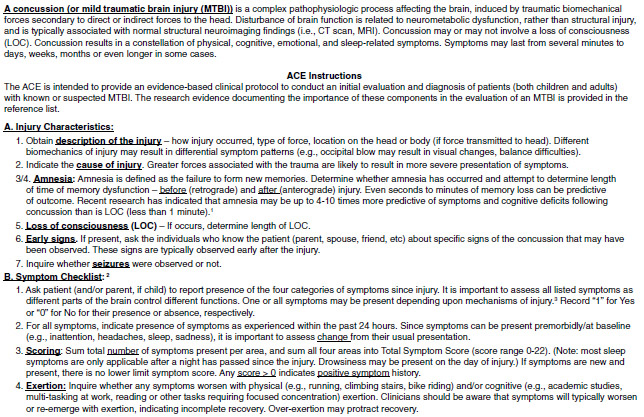
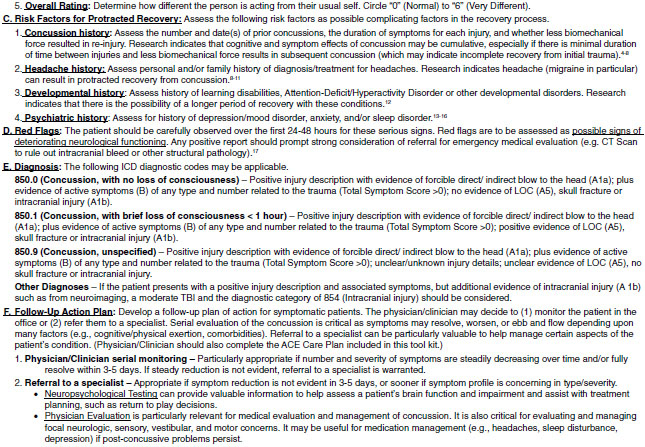
Figure 4.1. Acute Concussion Evaluation (ACE). Unlimited use granted for clinical and educational purposes. Centers for Disease Control and Prevention: Heads Up. Retrieved from www.cdc.gov/HEADSUP
NEUROCOGNITIVE COMPUTERIZED TESTING
Preseason baseline testing is used in many school districts with their student athlete population. The most widely used instrument is Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT, 2013). This is a 20-minute computerized assessment of neurocognitive abilities. Student athletes take the assessment preseason to document a baseline score. This provides a reference point for how the student athlete’s brain functions when it is healthy.
Several additional computerized neurocognitive tests on the market include CogSport (also known as Axon), Concussion Vital Signs, King-Devick Test for Concussions, and ANAM4 (Automated Neuropsychological Assessment Metrics, Version 4). The neurocognitive test monitors are typically athletic trainers, school nurses, athletic directors, team physicians, or psychologists—all professionals who should be designated as members of the school-based concussion team. These tests are relatively inexpensive, unobtrusive, and easy to administer.
The computerized neurocognitive assessment typically measures player symptoms, verbal/visual memory, attention span (sustained and selective), working memory, processing speed, response variability, nonverbal problem solving, and reaction time. If a student sustains a concussion, he or she can take the test again to compare the data to baseline scores. This helps determine the extent of the injury and to what degree recovery of cognitive processes postconcussion has occurred. Without an established baseline, managing a concussion can be difficult and involves more subjective guesswork. For example, if a student who sustained a concussion only takes a neurocognitive test after the concussion, but there is no baseline—the student’s “average” score may be taken as an indicator that the concussion has resolved. However, an established baseline may yield scores that were well above average. Thus, for such a student, an average score is a precipitous drop and indicates that the injury is still affecting cognition.
Although neurocognitive tests can be valuable tools, there are a few drawbacks. First, neurocognitive assessment is not recommended during the acute states of recovery because the cognitive stress of taking the test can slow recovery. While the student is symptomatic, the actual process of taking the test can make symptoms worse. Another issue is that student athletes may know what this test is for and sometimes will “fake bad” during baseline so they are not sidelined during future games and practices due to a drop in scores. Next, the most common baseline test, ImPACT, does not test balance or vision, two brain functions that can be key indicators of concussion.
Neurocognitive assessments should only be one of multiple tools used in making return-to-play decisions. Other tools may include an evaluation about conditions that affect concussion recovery, past concussion history, a symptom checklist and/or rating scale, and a complete neuropsychological examination, which generally includes balance testing.
SIDELINE ASSESSMENT
Districts may train staff members to use sideline assessment tools at sporting events to determine whether a student athlete may have sustained a concussion. A sideline assessment can provide a quick, objective way of evaluating whether an athlete should be removed from play. Sideline assessments can measure impairments of eye movements, attention, concentration, speech/language, and other correlates of impaired brain function. A more detailed neuropsychological evaluation, administered at a later time, would then be expected to guide return-to-play decisions.
Physicians, athletic trainers, and coaches are typically the ones responsible for determining whether a student athlete may have sustained a concussion and needs to be pulled from the game (following the mantra, “When in doubt, sit them out.”). This often involves a series of questions, with the intention of evaluating whether an athlete is oriented and knows what is going on. Inappropriate responses to simple questions, such as “What play were you were injured on?” “What’s the score?” and “What do you remember about what just happened?” help discern whether the athlete is alert to his or her surroundings and circumstances. The athletic and medical team may also conduct simple cognitive tests at the sidelines, such as having the student athlete repeat a series of digits forward and backward and completing simple balance tests. These may look similar to tests a police officer would give to someone suspected of drinking and driving: Can the person stand with feet in a heel-to-toe tandem position? Can the person stand on one foot? Can the person do that with his or her eyes open and then closed? With his or her hands on hips? The evaluator must take particular care when conducting informal sideline assessments with very young children, who may not understand slang terminology, such as getting their “bell rung,” and who may not even pay attention to the score of the game.
Screening tools such as the Sport Concussion Assessment Tool-3 (SCAT3), Standardized Assessment of Concussion (SAC), or Balance Error Scoring System (BESS) are frequently used sideline assessment tools. Such sideline assessments do have their share of false positives (pulling an athlete out of a game for a concussion when the athlete did not have one) and false negatives (not suspecting a concussion when the athlete actually had one). Symptoms of other conditions, such as dehydration, can mimic the symptoms of concussion. Thus, a brief sideline assessment cannot replace comprehensive testing or be used alone for concussion management. The following are examples of sideline assessments:
Sport Concussion Assessment Tool (SCAT3) and Child SCAT3 (McCrory et al., 2013a, 2013b)
 Compilation of Glasgow Coma Scale (GCS; Teasdale and Jennett, 1974), which measures the degree of brain impairment, the BESS (described in the following), a symptom checklist, and a neck evaluation
Compilation of Glasgow Coma Scale (GCS; Teasdale and Jennett, 1974), which measures the degree of brain impairment, the BESS (described in the following), a symptom checklist, and a neck evaluation
 Athlete documentation: Asks the player to report symptom severity on a chart; provides a list of signs to watch for and provides an explanation of what to expect postconcussion
Athlete documentation: Asks the player to report symptom severity on a chart; provides a list of signs to watch for and provides an explanation of what to expect postconcussion
 Medical evaluation documentation: Asks about signs experienced by the player; provides memory questions (e.g., What team did we play last? Which half is it? Who scored last?); includes cognitive assessment (five word recall, in which both immediate and delayed responses are tallied); conducts a neurologic screening (speech, eye motion and pupils, gait); provides an explanation of return to play guidelines
Medical evaluation documentation: Asks about signs experienced by the player; provides memory questions (e.g., What team did we play last? Which half is it? Who scored last?); includes cognitive assessment (five word recall, in which both immediate and delayed responses are tallied); conducts a neurologic screening (speech, eye motion and pupils, gait); provides an explanation of return to play guidelines
Balance Error Scoring System (BESS) (Riemann, Guskiewicz, & Shields, 1999)
 Three 20-second balance tests performed on firm surface and piece of medium-density foam, with eyes closed
Three 20-second balance tests performed on firm surface and piece of medium-density foam, with eyes closed
 The balance test positions include: standing flat on both feet with hands placed on the iliac crests, standing on a single leg on the nondominant foot, and standing flat on both feet with eyes closed
The balance test positions include: standing flat on both feet with hands placed on the iliac crests, standing on a single leg on the nondominant foot, and standing flat on both feet with eyes closed
 Measures central integration of vestibular, visual, and somatosensory information
Measures central integration of vestibular, visual, and somatosensory information
Standardized Assessment of Concussion (SAC) (McCrea, Kelly, & Randolph, 2000)
 Designed to take 5 to 10 minutes to administer
Designed to take 5 to 10 minutes to administer
 Measures orientation, memory, concentration, and delayed recall
Measures orientation, memory, concentration, and delayed recall
 Also includes a brief neurological screen (loss of consciousness, posttraumatic amnesia, coordination, movement)
Also includes a brief neurological screen (loss of consciousness, posttraumatic amnesia, coordination, movement)
King-Devick Test (Galetta et al., 2011)
 Two-minute test based on the time to perform rapid number naming
Two-minute test based on the time to perform rapid number naming
 Requires athletes to read single digit numbers on a tablet. Involves reading aloud a series of single digit numbers from left to right. Scores are compared to baseline
Requires athletes to read single digit numbers on a tablet. Involves reading aloud a series of single digit numbers from left to right. Scores are compared to baseline
 Screens for saccadic eye movements, attention, concentration, speech/language, and other correlates of suboptimal brain function
Screens for saccadic eye movements, attention, concentration, speech/language, and other correlates of suboptimal brain function
SMARTPHONE AND TABLET APPS
A number of concussion apps are increasingly available on the market. They generally offer a quick and easy way to assess youth for a suspected concussion. Many of these apps target parents and coaches, who would both benefit from having the lists of concussion signs and symptoms at their fingertips—on their phone that is always with them—as opposed to on a paper handout in the filing cabinet. While these apps can be quite convenient, it is important that they not be used as substitutes for comprehensive training on the signs and symptoms of concussion, as well as the danger signs. The following list is just a sampling of resources that are available for a smartphone or tablet.
 CDC “Heads Up” App, Version 1.0 (CDC, 2015). Aids in the detection of concussion and provides guidance on what to do if a concussion is suspected. Includes a three-dimensional helmet feature to help parents select and appropriately fit helmets for a variety of sports. The app includes a section on safety tips to prevent injuries at home, school, and play.
CDC “Heads Up” App, Version 1.0 (CDC, 2015). Aids in the detection of concussion and provides guidance on what to do if a concussion is suspected. Includes a three-dimensional helmet feature to help parents select and appropriately fit helmets for a variety of sports. The app includes a section on safety tips to prevent injuries at home, school, and play.
 PAR’s Concussion Recognition and Response: Coach and Parent Version, Version 1.2.2 (Gioia, Mihalik, & PAR, Inc., 2011). This app, designed by two of the leaders in the field of youth sports concussion, provides a checklist of concussion signs/symptoms designed to help coaches/parents determine whether to remove a child from the game/practice and seek a medical evaluation. Coaches can immediately e-mail a report of student concussion symptoms generated from the checklist; the app also features a “Dial 911”button for emergency situations and offers strategies for managing concussion beyond the acute phase of injury. The app contains six sections: Past Incidents; New Incident; Home Symptom Monitoring; Concussion Info/FAQs; ACE Post-Concussion Home/School Instructions; and Return-to-Play Guide.
PAR’s Concussion Recognition and Response: Coach and Parent Version, Version 1.2.2 (Gioia, Mihalik, & PAR, Inc., 2011). This app, designed by two of the leaders in the field of youth sports concussion, provides a checklist of concussion signs/symptoms designed to help coaches/parents determine whether to remove a child from the game/practice and seek a medical evaluation. Coaches can immediately e-mail a report of student concussion symptoms generated from the checklist; the app also features a “Dial 911”button for emergency situations and offers strategies for managing concussion beyond the acute phase of injury. The app contains six sections: Past Incidents; New Incident; Home Symptom Monitoring; Concussion Info/FAQs; ACE Post-Concussion Home/School Instructions; and Return-to-Play Guide.
 Play It Safe Concussion Assessment, Version 1.3 (Concussion Health, LLC, 2011). Play It Safe provides a simplified symptom checklist, Maddock’s Questions (orientation to time and space), word recall test, number reversal test, balance test, and vision test. The app includes a Dynamic Vision Test, which tests the vestibular ocular reflex. It also includes an established eye chart baseline and measures the subject’s ability to read the eye chart while moving their head.
Play It Safe Concussion Assessment, Version 1.3 (Concussion Health, LLC, 2011). Play It Safe provides a simplified symptom checklist, Maddock’s Questions (orientation to time and space), word recall test, number reversal test, balance test, and vision test. The app includes a Dynamic Vision Test, which tests the vestibular ocular reflex. It also includes an established eye chart baseline and measures the subject’s ability to read the eye chart while moving their head.
 ImPACT, Version 1.0 (ImPACT Applications, Inc., 2013). This application is designed to help identify concussion signs and symptoms at the site of a potential injury. It consists of brief cognitive tests and a symptom inventory on which the student is asked to rate severity of concussion symptoms.
ImPACT, Version 1.0 (ImPACT Applications, Inc., 2013). This application is designed to help identify concussion signs and symptoms at the site of a potential injury. It consists of brief cognitive tests and a symptom inventory on which the student is asked to rate severity of concussion symptoms.
 Return2Play, Version 1.5 (The University of Michigan, 2013). This app is used primarily by patients to track their recovery. It includes concussion myths and facts, signs and symptoms, what to do during recovery, return-to-play guidelines, a list of factors that may increase risk of concussion, and information on how to reduce concussion risk.
Return2Play, Version 1.5 (The University of Michigan, 2013). This app is used primarily by patients to track their recovery. It includes concussion myths and facts, signs and symptoms, what to do during recovery, return-to-play guidelines, a list of factors that may increase risk of concussion, and information on how to reduce concussion risk.
 American Academy of Neurology’s Concussion Quick Check, Version 2.2.0 (American Academy of Neurology, 2015). The Quick Check is designed to help parents/coaches and other nonmedical personnel determine if an athlete has a concussion and needs a medical evaluation. It contains a list of common signs and symptoms; a checklist of things to do if the athlete is knocked unconscious (check ABCs); a list of things to do if a concussion is suspected; and a brief discussion on return-to-play guidelines.
American Academy of Neurology’s Concussion Quick Check, Version 2.2.0 (American Academy of Neurology, 2015). The Quick Check is designed to help parents/coaches and other nonmedical personnel determine if an athlete has a concussion and needs a medical evaluation. It contains a list of common signs and symptoms; a checklist of things to do if the athlete is knocked unconscious (check ABCs); a list of things to do if a concussion is suspected; and a brief discussion on return-to-play guidelines.
 King-Devick Test, Version 1.0 (King-Devick, LLC, 2015). The King-Devick Test, described under “sideline assessments” presented earlier, can also be administered by parents. The King-Devick Test is a 2-minute test that requires an athlete to read single digit numbers displayed on a tablet or on an iPad. An athlete is given the test at baseline and again after a suspected concussion. If the time required to complete the test is any longer than the athlete’s baseline test time, it is recommended that the athlete be removed from play and evaluated by a licensed professional.
King-Devick Test, Version 1.0 (King-Devick, LLC, 2015). The King-Devick Test, described under “sideline assessments” presented earlier, can also be administered by parents. The King-Devick Test is a 2-minute test that requires an athlete to read single digit numbers displayed on a tablet or on an iPad. An athlete is given the test at baseline and again after a suspected concussion. If the time required to complete the test is any longer than the athlete’s baseline test time, it is recommended that the athlete be removed from play and evaluated by a licensed professional.
Julia
Julia’s coach conducted a sideline assessment at the soccer game in which she sustained her third concussion. After Julia was elbowed in the head by another player, she fell to the ground. Her coach administered the SAC to evaluate her orientation, immediate memory, and neurologic state. Julia was confused about the day of the week and time. She could not recall what happened right before and after the injury. She also appeared uncoordinated and weak. She had difficulty with immediate and delayed word recall, as well as ability to concentrate, as evidence by her impaired ability to repeat strings of digits or state the months of the year in reverse. Because of this assessment, Julia’s coach felt confident in her decision to pull her from the rest of the game and to refer her for an evaluation by a medical professional.
CLINICAL EVALUATION
Neurocognitive tests, sideline assessments, and smartphone apps can help district staff and parents determine the severity of a student’s symptoms. However, they are not a replacement for a complete medical evaluation to diagnose a concussion. Any student suspected of having a concussion should be seen as soon as possible by a health care provider with knowledge and experience in diagnosing concussions. A student who has sustained a concussion should then be under the continued care of a qualified medical professional throughout recovery. Results from any of the tools previously discussed should be provided to parents and to medical personnel to aid in diagnosis and treatment.
The primary tool for concussion diagnosis in a medical setting is confirmation of a constellation of signs and symptoms after an individual has sustained a blow to the head or body. A physician may conduct balance testing and other neurocognitive assessments. He or she may also conduct neuroimaging, and other physical and neurological exams to rule out more serious injuries. A neuropsychological assessment to assess cognitive functioning, memory, speed, and processing time may also be administered. Research on the effectiveness of neuropsychological tests for identifying and managing concussions, however, is mixed (Institute of Medicine & National Research Council, 2014).
ONGOING ASSESSMENT AT SCHOOL
Keeping an eye on a student who has sustained a concussion and collecting data from multiple sources can help safely and effectively manage a student through the course of recovery. Parents can monitor symptoms at home, medical personnel can monitor symptoms at check-ups, and the school team can implement active symptom progress monitoring at school to facilitate data-based decision making. This allows team members to:
 Assess and monitor the effects of cognitive exertion
Assess and monitor the effects of cognitive exertion
 Assess key parts of the day/key classes where symptoms worsen
Assess key parts of the day/key classes where symptoms worsen
 Gradually withdraw accommodations that are no longer needed
Gradually withdraw accommodations that are no longer needed
 Guide the overall return-to-learn and return-to-play decisions
Guide the overall return-to-learn and return-to-play decisions
Multiple sources of data help to safely assist a student who has sustained a concussion through the recovery process. The multidisciplinary team described in detailed in Chapter 3 lends itself well to facilitating the collection of data from a variety of sources.
Case Management
The CTL should keep track of all concussion cases brought to his or her attention. A simple spreadsheet, such as the one found in Exhibit 4.3, can be used to collect data on each student’s grade level, the person who provided notification, the date of injury, the date of referral, concussion details, and response notes. This type of form can be particularly helpful when tracking the progress of a student who has sustained multiple concussions, as it is easy to search by the student’s name for cases that were documented in previous years.
Each student recorded on the tracking log would also have a file containing the signed release of information, physician evaluations and recommendations, copies of ongoing symptom monitoring forms, and the academic adjustment plan.
EXHIBIT 4.3
Sample CTL Case Tracking
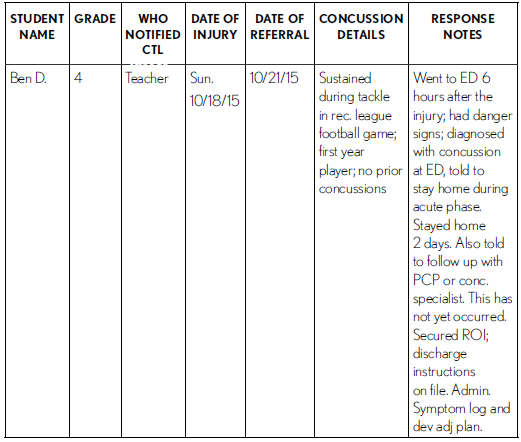
CTL, concussion team leader; ROI, release of information.
Symptom Progress Monitoring
Much of the return to school progression is dependent upon gradually increasing academic work without exacerbating symptoms. However, it can be difficult for teachers to discern how much cognitive exertion is too much, particularly when some teachers may only see students for short academic periods once a day. The team can facilitate a trial-and-error process that evaluates whether symptoms worsen when the task demands change. Teachers should only change one of the following task variables at a time:
1. Amount of work
2. Length of work
3. Difficulty of work
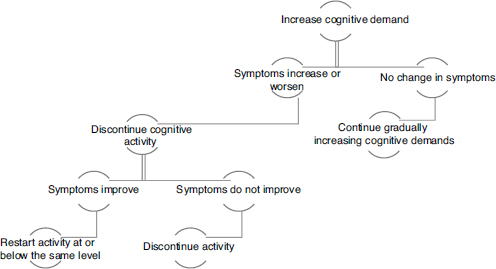
Figure 4.2. Decision tree for increasing task demands.
Adapted from Nationwide Children’s Hospital (2012).
Changing only the amount, length, or difficulty of work—one variable at a time—will help the concussion team determine if the increase exacerbates symptoms. As long as symptoms do not worsen, the student can gradually increase engagement in school (see Figure 4.2). However, if symptoms do increase, then the activity should be discontinued for at least 20 minutes and the student should be permitted to rest. If this rest period relieves symptoms, the activity can be attempted again (ideally, below the level that produced symptoms). However, if rest does not relieve symptoms, the student should discontinue activity for the day and reattempt the next day or when symptoms have lessened (Nationwide Children’s Hospital, 2012).
Julia
Julia’s history teacher, Mrs. Rogers, failed to recognize that taking an entire history exam may be too cognitively taxing for Julia while she was in the acute phase of recovering from her concussion. Mrs. Rogers gave Julia the exam, wished her good luck, and expected her to complete it along with the rest of the class. Consequently, Julia failed the history exam. During the exam, Julia was extremely frustrated because she could not remember the material. She also had trouble focusing—she had a terrible headache and the lights were bothering her. Her poor performance was unusual, as Julia was typically a straight A student. Mrs. Rogers did not adjust the amount, length, or difficulty of the work.
Julia’s math teacher, Mrs. Coffman, recognized that Julia should not be required to take an exam in the same environment and in the same amount of time as the other students in her class. Mrs. Coffman arranged for Julia to take the exam in the school counselor’s office. Mrs. Coffman also made Julia’s exam one third the length of her classmates’ test. Julia was able to demonstrate her knowledge and earned an A on the exam because of the adjustments Mrs. Coffman’s provided. Decreasing the length of the test allowed Julia to demonstrate her knowledge without undue cognitive exertion.
Progress monitoring tools can allow for careful, individualized clinical assessment and tracking from time of injury. A Concussion Symptom Tracking Log (see Exhibit 4.4) is a common way to evaluate the presence and severity of symptoms.
The school team then needs to select classroom adjustments based on the student’s specific symptom profile. If a student endorses any symptoms as “severe,” it likely warrants a referral to the nurse or parent. Such a student may benefit most from being sent home. Students with mild to moderate symptoms can be permitted to participate in the classroom, with appropriate adjustments. Additional information on the process of selecting and monitoring adjustments is provided in Chapter 6.
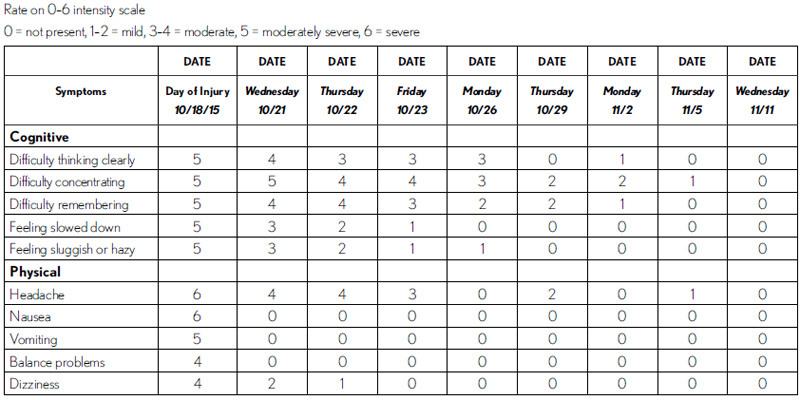
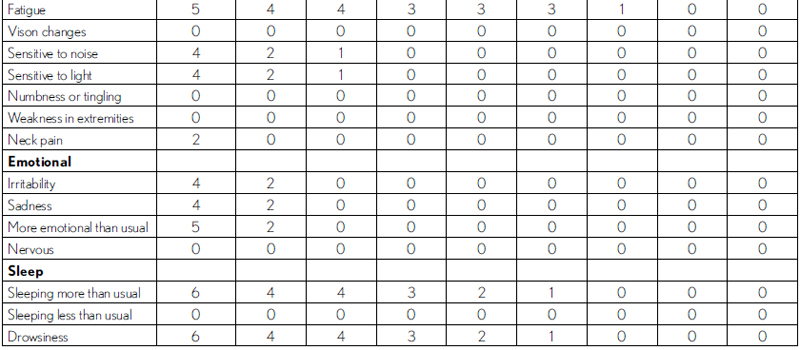
Ben
Ben’s concussion team completed the symptom tracking log (Exhibit 4.5) beginning with his first day back at school. The tracking log was administered daily upon return to school except on weekends, and then every few days toward the end of this recovery period. His symptoms resolved completely within 3 weeks.
With a quick glance it is clear that Ben’s symptoms were primarily cognitive, and that with the exception of a headache, his physical symptoms resolved fairly quickly. He was also tired and sleeping more than usual. His emotional symptoms—which peaked the night after his accident—dissipated by his second day back at school.
Informal Interviews
Interviews can also be used at school to engage a student in dialogue about symptoms. This is particularly helpful because symptoms can vary from day to day, from class to class—and even within a single class session. In-depth conversations with the student can help educators target specific barriers to the student’s functioning in an academic environment. Open-ended questions might include:
EXHIBIT 4.4
Progress Monitoring—Concussion Symptom Tracking Log
Concussion Symptom Tracking Log
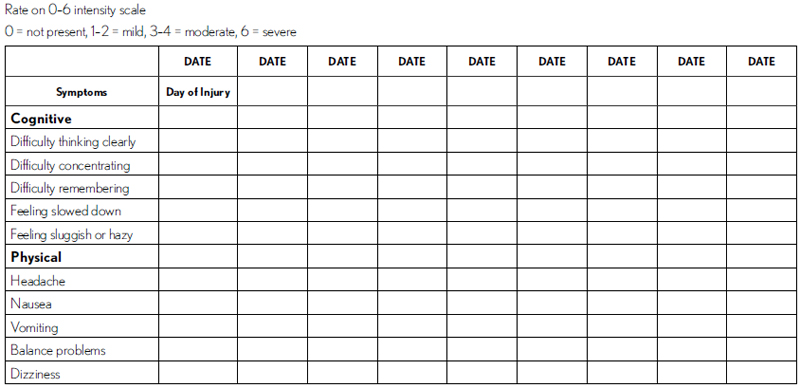
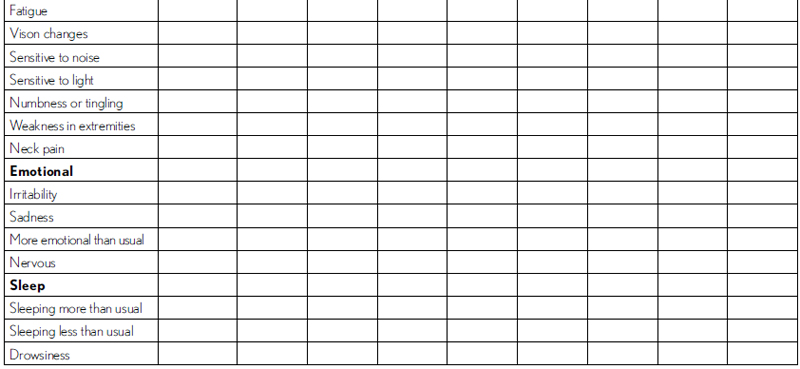
EXHIBIT 4.5
Ben’s Concussion Symptom Tracking Log
Concussion Symptom Tracking Log
 How is your headache (or other specific, bothersome symptom) today?
How is your headache (or other specific, bothersome symptom) today?
– Could add a scaling question: On a scale from 0 to 6 with 0 being “not at all” and 6 being “the worst pain imaginable,” how bad is the headache?
 Is anything making your headache worse?
Is anything making your headache worse?
– Could specify are ___ (e.g., loud noises or bright lights) making it worse?
 Are you having trouble paying attention in class?
Are you having trouble paying attention in class?
 Are you having trouble learning new things? Remembering old information?
Are you having trouble learning new things? Remembering old information?
– Can probe to determine whether there are specific content areas in which learning or retrieval of information is most difficult
 What is most difficult for you at school right now?
What is most difficult for you at school right now?
 How are things going in _____ (insert specific class)?
How are things going in _____ (insert specific class)?
– This can help discern whether the student would benefit from different adjustments in different classes. Perhaps the student has no symptoms or difficulty in math or science but is struggling in Spanish and language arts. In such a case, adjustments might be minimized or removed in certain classes but retained in others.
Questions can be altered based on the student’s age and concussion symptoms. For example, instead of asking a very young child, “Do you have a headache?” one might ask, “Does it feel like something is wrapped tightly around your head?” or instead of “Do you feel queasy?” one might ask, “Do you feel like you might throw up?” or “Does your tummy hurt?”
In considering developmental issues as it relates to our case studies, Julia and Damien could be asked, “On a scale from 0-6 with 0 being ‘no pain’ and 6 being ‘worst pain imaginable,’ how bad is your headache?” Because they are in Eleventh and eighth grade, Julia and Damien should be able to understand that scale. However, that question may be too difficult for a first- or fourth-grade student to understand. Carly and Ben could be asked, “Right now, how bad does your head hurt? Would you say, it doesn’t hurt, it kind of hurts, it really hurts, or it really, really hurts?”
Once the team has determined the areas that are causing the most significant difficulty for students, changes can be made to the plan. Continuous communication with students through these informal interviews can help them continue coursework without over-taxing their healing brain.
Observations
A student may not self-report symptoms if he or she has competing interests. Perhaps the student is anxious to return to sports practice, driving, technology use, or social engagement. Julia may want to get back to schoolwork so she doesn’t fall behind, or Damien may simply not want adults worrying about him (or pestering him with questions!). Thus, observations are essential for discerning whether a student’s symptoms are worsening. Educators should be on the lookout for the following signs that a concussion may be continuing to affect a student’s functioning in school (Nationwide Children’s, 2012, p. 10):
 Greater irritability
Greater irritability
 Increased problems paying attention or concentrating
Increased problems paying attention or concentrating
 More emotional than normal/emotional reactions that are disproportionate to the situation
More emotional than normal/emotional reactions that are disproportionate to the situation
 Less ability to cope with emotions than normally
Less ability to cope with emotions than normally
 Increased difficulty learning or remembering new information
Increased difficulty learning or remembering new information
 Difficulty organizing tasks
Difficulty organizing tasks
 Increased forgetfulness
Increased forgetfulness
 Inappropriate or impulsive behaviors during class
Inappropriate or impulsive behaviors during class
 Repeating himself or herself
Repeating himself or herself
Observations can help identify whether there are specific factors that may worsen a student’s symptoms. A few key questions included on the CDC’s fact sheet, Returning to School After a Concussion: A Fact Sheet for School Professionals (CDC, n.d., p. 9), include:
 Do some classes, subjects or tasks appear to pose greater difficulty than others (compared to preconcussion performance)?
Do some classes, subjects or tasks appear to pose greater difficulty than others (compared to preconcussion performance)?
 For each class, is there a specific time frame after which the student begins to appear unfocused or fatigued (e.g., headaches worsen after 20 minutes)?
For each class, is there a specific time frame after which the student begins to appear unfocused or fatigued (e.g., headaches worsen after 20 minutes)?
 Is the student’s ability to concentrate, read, or work at a normal speed related to the time of day (e.g., the student has increasing difficulty concentrating as the day progresses)?
Is the student’s ability to concentrate, read, or work at a normal speed related to the time of day (e.g., the student has increasing difficulty concentrating as the day progresses)?
 Are there specific things in the school or classroom environment that seem to distract the student?
Are there specific things in the school or classroom environment that seem to distract the student?
 Are any behavioral problems linked to a specific event, setting, (e.g., bright lights in the cafeteria or loud noises in the hallway), task, or other activity?
Are any behavioral problems linked to a specific event, setting, (e.g., bright lights in the cafeteria or loud noises in the hallway), task, or other activity?
Discussion Points
The team can discuss the data, taken together, and determine whether there are factors that exacerbate a student’s symptoms and whether steps can be taken to improve those factors. Such issues may include whether there are certain classes or tasks that pose more difficulty than others, whether there is a specific time of day that is most problematic, and whether there are aspects of the school environment that are particularly distracting or difficult (triggers of problems).
Damien
Damien would have benefited from having a school-based concussion team in place prior to his injury to create a more proactive plan. As it stood, the teachers, administrators, and related service personnel learned a great deal about concussions after the fact. The school psychologist was only assigned to the building one day per week and mostly worked on special education evaluations. The school counselor primarily dealt with class scheduling issues and college applications. Both of these school-based mental health providers wanted to offer services, but because of their large caseloads felt confined to traditional roles.
The district had an intern school psychologist who was interested in working with high school age students. The intern had received specific training related to concussion recognition and response during her graduate training and she had a number of resources for parents and teachers. She assisted with Damien’s school-based evaluation by observing him in the classroom setting. She also conducted interviews with Damien, his parents, and his teachers to gain a better comparison of his current functioning compared to baseline. Results of these informal assessments indicated that Damien was functioning well below baseline academically. Math and writing were now particularly difficult for Damien. Problems in these subject areas seemed compounded by the fact that both math and language arts were scheduled at the end of the day, when Damien was more fatigued. The cafeteria, hallway, and bus made Damien particularly edgy. These data helped the team create a plan that included switching his math and science classes so he had math in the morning, allowing him to eat lunch in an empty classroom with a friend, and riding to school with his mom or dad instead of on the bus.
The intern school psychologist also wanted Damien to switch classes before or after the rush of students in the hallway—which he had done until his cast was removed—but Damien refused to accept this accommodation that would make him stand out so much from his peers. Instead, he agreed to at least go directly to his next class and take his seat instead of lingering in the hallway until the bell rang.
While school concussion teams generally want to use permanent staff members as core team members, it is also advisable that districts use resources wisely. We may want every district to have school psychologists and school counselors working within the recommended student-to-provider ratios, but this is not happening in many districts. This means that such professionals do not have as many opportunities to engage in prevention and intervention activities. By allowing an intern to take the initiative and assume some of the leadership in this case, under the guidance of her supervisor, this school team engaged in creative problem solving and efficient use of resources. It also provided a good experience for the intern, who gained more confidence in taking on the leadership role. Because of this experience, she made sure her future employees had appropriate concussion management policies and school-based concussion teams in place.
NEWER ASSESSMENT TECHNIQUES: THE FUTURE OF CONCUSSION ASSESSMENT?
Readers are advised to keep abreast of research related to the efficacy of newer imaging techniques at detecting concussions. While typical CT scans and MRIs are generally unremarkable in individuals who have sustained concussions, newer techniques such as magnetic resonance spectroscopy, positron emission tomography, single-photon emission computed tomography, functional magnetic resonance imaging, and diffusion tensor imaging may be used in the future.
The use of serum biomarkers is another area yet to be explored in youth concussions. Following a brain injury, proteins may leak from damaged cells into the cerebrospinal fluid and then cross the blood–brain barrier, entering the bloodstream. While the technology is not yet available to detect and diagnose concussions through newer imaging techniques or serum biomarkers, scientific breakthroughs that allow detection through a medical test may be available in the near future.
REFERENCES
American Academy of Neurology. (2015). Concussion quick check (2.2). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/concussion-quick-check/id613178630?mt=8
Centers for Disease Control and Prevention. (n.d.). Returning to school after a concussion: A fact sheet for school professionals. Retrieved from: http://www.cdc.gov/concussion/pdf/TBI_Returning_to_School-a.pdf
Centers for Disease Control and Prevention. (2015). CDC heads up concussion and helmet safety (1.0). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/cdc-heads-up-concussion-helmet/id999504040?mt=8
Concussion Health, LLC. (2011). Play it safe concussion assessment (1.3) [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/play-it-safe-concussion-assessment/id441786934?mt=8
Galetta, K. M., Brandes, L. E., Maki, K., Dziemianowicz, M. S., Laudano, E., Allen, M., … Balcer, L. J. (2011). The King-Devick test and sports-related concussion: Study of a rapid visual screening tool in a collegiate cohort. Journal of the Neurological Sciences, 309(1–2), 34–39.
Gioia, G. A., & Collins, M. (2006). Acute concussion evaluation (ACE): Physician/clinician office version. Retrieved from http://www.cdc.gov/concussion/headsup/pdf/ace-a.pdf
Gioia, G. A., Mihalik, J., & PAR, Inc. (2011) Concussion assessment & response: Coach and parent version (1.1). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/concussion-assessment-response/id495161270?mt=8
ImPACT Applications, Inc. (2013). Sideline impact (1.0). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/sideline-impact/id660066713?mt=8
ImPACT (Immediate Post-Concussion Assessment and Cognitive Testing). (2013). The ImPACT test. http://www.impacttest.com/about/. Accessed September 20, 2015.
Institute of Medicine (IOM) and National Research Council (2014). Sports-related concussions in youth: Improving the science, changing the culture. Washington, DC: The National Academies Press.
King-Devick Test, LLC. (2015). King-Devick test in association with mayo clinic (1.0). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/king-devick-test-in-association/id1033607954?mt=8
McCrea, M., Kelly, J. P., & Randolph, C. (2000). Standardized assessment of concussion (SAC): Manual for administration, scoring, and interpretation (2nd ed.). Waukesha, WI: CNS Inc.
McCrory, P., Meeuwisse, W. H., Aubry, M., Cantu, B., Dvorak, J., Echemendia, R. J., … Turner, M. (2013a). Child-SCAT3. British Journal of Sports Medicine, 47(5), 263–266.
McCrory, P., Meeuwisse, W. H., Aubry, M., Cantu, B., Dvorak, J., Echemendia, R. J., … Turner, M. (2013b). SCAT3. British Journal of Sports Medicine, 47(5), 259–262.
Nationwide Children’s Hospital. (2012). An educator’s guide to concussions in the classroom (2nd ed.) Retrieved from http://www.nationwidechildrens.org/concussions-in-the-classroom
Riemann, B. L., Guskiewicz, K. M., & Shields, E. W. (1999). Relationship between clinical and forceplate measures of postural stability. Journal of Sport Rehabilitation, 8(2), 71–82.
Teasdale, G., & Jennett, B. (1974). Assessment of coma and impaired consciousness: A practical scale. Lancet, 304(7872), 81–84. doi: dx.doi.org/10.1016/S0140-6736(74)91639-0.
The University of Michigan. (2013). Return2Play for concussion (1.5). [Mobile application software]. Retrieved from https://itunes.apple.com/us/app/return2play-for-concussion/id555361650?mt=8