Leon Chaitow
Introduction
Muscle energy techniques (MET) originated in osteopathic medicine in the 1950s and include a group of methods that involve either isometric contractions, or isotonic eccentric contractions, in treatment and rehabilitation of musculoskeletal dysfunction.
The most basic and most widely used form of MET involves the careful positioning of an area of the body, just short of a restriction barrier (see notes on barriers in
Ch. 5
), followed by the use of a brief isometric contraction, in which the degree of moderate force employed by the patient, as well as the direction(s) and duration of that effort, are prescribed by the therapist.
After an isometric contraction (or sometimes during the contraction if an eccentric stretch is required), the soft tissues being treated are eased to a new position. The contraction effort produces changes – discussed below – that allow tissues to be moved or stretched more comfortably than before the isometric contraction.
The repositioning after the contraction commonly involves a degree of stretching, particularly in chronic settings, or might simply take advantage of a reduction in resistance to movement, that allows painless positioning at a new end-of-range barrier, without stretching.
The ‘non-stretch’ option – in which the tissues are taken to a new end-of-range – is suggested in acute clinical settings or in the treatment of joints (Chaitow 2013).
A reasonable question: Where does muscle end, and fascia begin?
This book focuses on fascial function and dysfunction
– which makes it reasonable to question why this chapter focuses to a large extent on ‘muscles’.
The response to that query is outlined below, but can be summarized as follows: there is no such thing as a muscle without fascia. ‘Muscle’
always
means ‘muscle and fascia’ – because they are indivisible. As Weppler and Magnusson (2010) explain:
‘Skeletal muscles comprise contractile tissue, intricately woven together by fibrous connective tissue that gradually blends into tendons
[that]
attach the muscle to bone. Although contractile tissue and tendons are sometimes evaluated separately for research purposes, they cannot be separated during routine clinical testing and stretching procedures, nor during functional activity
.’
•
Schleip (2003a, 2003b) has described fascia as:
‘… the dense irregular connective tissue that surrounds and connects every muscle, even the tiniest myofibril, and every single organ of the body forming continuity throughout the body’.
•
Illustrations of muscular activity in standard anatomical atlases usually involve images in which fascial elements having been removed to reveal what is commonly and inaccurately presented as the primary mechanical feature of movement – specific muscles. This practice ignores vital fascial connective continuities by means of which force is transmitted in multiple directions simultaneously: sometimes laterally, sometimes obliquely, and sometimes linearly. For example, as described in
Chapter 4
, structures normally described as the muscles of the hip, pelvis, and leg, interact with arm and spinal muscles via the thoracolumbar fascia, which allows effective load transfer between the spine, pelvis, legs and arms, in an integrated system.
•
Examples were given in
Chapters 1
,
2
and
4
of the many other ways in which force/load is transmitted via fascial pathways – for example from contracting hamstring muscles to the
ipsi- and contralateral thoracolumbar fascia (Franklyn-Miller et al. 2009) and from latissimus dorsi contraction to the contralateral gluteal muscles, and onward to the knee (Stecco et al. 2013). Global dysfunction may therefore emerge from unbalanced, excessive and/or inefficient load transfer. Key point
Key point
An understanding of the ‘muscle–fascia–tendon unit’ is important in the context of a chapter in which muscular forces (‘muscle energy’) of various types are at the heart of the methods described.
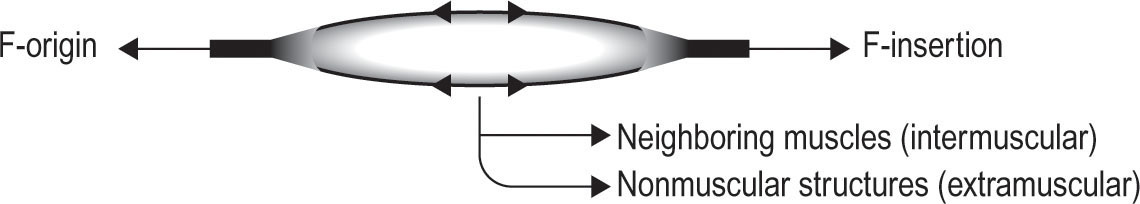
Extramuscular myofascial force transmission (MFT)
•
However, there is another load transfer process that is more intimate, rather than global, involving radial force transmission within muscles, and from muscle to local structures.
•
As an example consider the intramuscular connective tissue network of a muscle, and adjacent non-muscular structures (e.g. bone). This extramuscular myofascial force transmission provides evidence of the inseparable (apart from by dissection or surgery) bonding of muscle–fascia (Maas 2009) (
Fig. 12.1
).
•
These extramuscular connections are very powerful, for example: ‘
With intact extra-muscular connective tissues around the whole gastrocnemius and plantaris (PL) muscle–tendon complex, up to 40.5% of active force of the PL is transmitted onto the calcaneal bone, even after the PL tendon has been cut from this bone’
(Rijkelijkhuizen 2005).
•
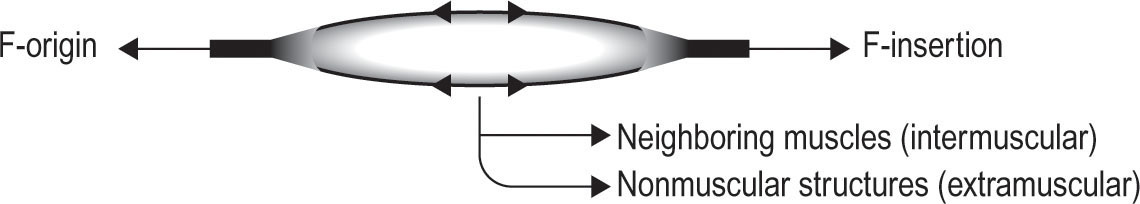
Radial stress involves 50% of longitudinal forces active in the soleus, medial gastrocnemius, and elbow flexor and extensor muscles during contractions (Findley et al. 2015) (
Fig. 12.2
).
•
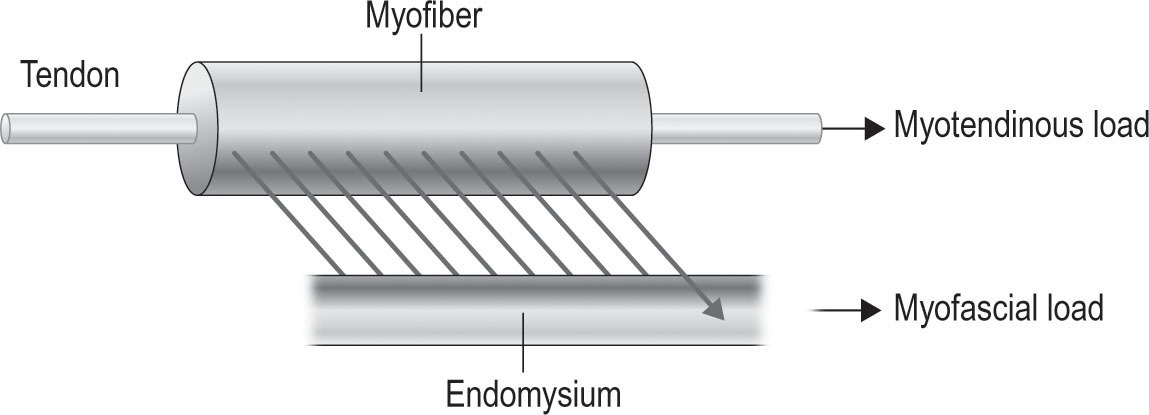
Also, within any muscle: ‘
Connections between sarcomeres and surrounding collagenous fibers are present along their full periphery
… [and]
… multiple reaction forces are exerted onto sarcomeres within a myofiber
’. These sideways connections supply a notable part of the reaction forces, producing force transmission onto the endomysium, described as myofascial force transmission (Huijing 2012) (
Fig. 12.3
).
Key point
Muscle and fascia are inseparable clinically. When MET is applied to muscle, the forces involved are spread in multiple directions, within the muscle, and to adjacent, and sometimes distant, structures.
Joint restrictions are usually soft-tissue restrictions
If all muscular problems, by definition, involve fascial features – what about joints?
•
Kappler (2003) has observed in relation to testing for end-of-the-range motion of joints: ‘
The term barrier may be misleading, if it is interpreted as a wall or rigid obstacle to be overcome with a push. As the joint reaches the barrier, restraints in the form of tight muscles and fascia, serve to inhibit further motion. We are pulling against restraints rather than pushing against some anatomic structure.’
Those
‘restraints’
are likely to involve a combination of muscle, fascia, ligament, tendon, etc. – with no way of identifying precisely which – apart from the use of high-tech imaging methods.
Figure 12.1
Extra and intramuscular force transmission.
Figure 12.2
Radial force transmission.
•
Mitchell (1998) – discussing the use of muscle energy techniques – suggests in relation to joint restrictions, that therapeutic efforts should be focused on the soft-tissue features:
‘Treating a joint motion restriction as if the cause are tight muscle(s) helps to restore normal joint motion. Regardless of the cause of restriction, MET treatment, based on a ‘short muscle’ paradigm, is usually completely effective in restoring normal range of motion, even when the blockage is due to non-muscular factors.’
Key Point
In the application of MET in treatment of restrictions, whether involving a joint, muscle, tendon, ligament or fascia – Mitchell’s advice (above) is commended: focus on normalizing the soft-tissue elements of tissues for optimal results.
MET definitions
Muscle energy technique
is defined as ‘a form of osteopathic manipulative diagnosis and treatment in which the patient’s muscles are actively used on request, from a precisely controlled position, in a specific direction, and against a distinctly executed counterforce’
(ECOP 2009).
Figure 12.3
Myofascial force transmission.
The terms used in MET require clear definition and emphasis:
1.
An isometric contraction
is one in which a muscle, or group of muscles, is called upon to contract, or move in a specified direction, and in which that effort is matched by the operator’s effort, so that no movement is allowed to take place. During the contraction, internal elements of the muscle – actin and myosin – interact to produce a shortening of the sarcomere, thereby stretching the
series elastic fascial component
of the sarcomere. In essence, the contraction stretches the intramuscular fascia.
2.
Isotonic eccentric contraction:
In this method the counterforce offered by the operator is greater than that offered by the patient – which effectively stretches the muscle while it is contracting.
3.
Isotonic concentric contraction:
In this method the origin and insertion of the muscle(s) are allowed to slowly approximate, as the effort exerted by the patient overcomes that of the operator. This has a tonic effect on the muscle(s) and is useful in toning weakened musculature. This can be performed slowly, or rapidly:

Slow eccentric isotonic stretch:
The operator offers greater counterforce than the patient, which slowly stretches the muscle while it is trying to shorten. The
series elastic fascial component
and the
parallel elastic fascial component
are simultaneously lengthened. The objective is to strengthen the muscle involved, and to relax it, while simultaneously inhibiting excess to its antagonists.
Slow eccentric isotonic stretch:
The operator offers greater counterforce than the patient, which slowly stretches the muscle while it is trying to shorten. The
series elastic fascial component
and the
parallel elastic fascial component
are simultaneously lengthened. The objective is to strengthen the muscle involved, and to relax it, while simultaneously inhibiting excess to its antagonists.

Rapid eccentric isotonic stretch (isolytic contraction).
This may be useful in cases where there exists a chronic degree of fibrotic change. The effect is to stretch and alter these tissues – inducing controlled microtrauma – thus allowing an improvement in elasticity, circulation and function during subsequent remodeling (Goodridge 1981).
Rapid eccentric isotonic stretch (isolytic contraction).
This may be useful in cases where there exists a chronic degree of fibrotic change. The effect is to stretch and alter these tissues – inducing controlled microtrauma – thus allowing an improvement in elasticity, circulation and function during subsequent remodeling (Goodridge 1981).
4.
Pulsed MET
is most useful where the practitioner is able to firmly control the area (usually a joint) being treated. The patient is requested to produce a series of 15 to 20 brief (less than a second) rhythmic, pulsed isometric contractions, against the firmly resisting hands of the operator. The pulsed efforts may be directed towards or away from a restriction barrier, or in a different direction altogether. After the series of pulsed contraction(s), the patient should participate in the movement as the joint is taken to a new, unforced, end-of-range position. See also
Box 12.2
, later in this chapter.
Notes on series and parallel elastic fascial components of muscle sarcomeres
•
The series elastic components of sarcomeres store energy when stretched, and contribute to elasticity. They comprise non-contractile – fascia/connective tissue – components of muscle that lie in series with muscle fibers. Tendons are examples of the
series elastic component,
as are the cross-bridges between
actin
and
myosin,
the sliding elements of muscle that allow shortening to occur (Huxley & Niedergerke 1954) (
Fig. 12.4
).
•
The parallel elastic component of sarcomeres provides resistive tension when a muscle is passively stretched. These are also non-contractile and consist of the muscle membranes (fascia), which lie parallel to the muscle fibers (see
Fig. 12.4
)
The origins of MET – quotes from the pioneers
MET was developed in osteopathic medicine in the USA, in the late 1940s, with strong influence from several key figures – some of whom are quoted below:

Figure 12.4
(A) The sarcomere at rest with the main elements – including three actin–myosin cross-bridges, as well as both the series and parallel elastic fascial components – at their resting lengths. (B) The sarcomere contracting isometrically – with actin and myosin sliding across each other as that part of the muscle contracts. The parallel elastic fascial component also shortens. However, because this is an isometric contraction and no overall length change occurs, the series elastic (fascial) component has to lengthen in order to accommodate the shortening of the other components. (C) This shows the changes when passive stretching is introduced. The parallel elastic and the actin–myosin components lengthen, while the stiffer series elastic component does not. (Note: The degree of separation of the actin/myosin components is exaggerated in this diagram).The overall message is that a degree of lengthening of the fascial elements of muscle occurs both during isometric contraction and during stretch. Adapted, with permission, from Lederman 1997
.
•
Fred Mitchell Jr DO:
‘Treating joint motion restriction as if the cause were tight muscle(s), is one approach that makes possible restoration of normal joint motion… Regardless of the cause of restriction, MET treatment based on a ‘short muscle’ paradigm is usually completely effective in eliminating blockage, and restoring normal range of motion, even when the blockage is due to non-muscular factors’
(Mitchell & Mitchell 1999).
•
Fred Mitchell Sr DO:
‘Muscle energy technique, with its many ramifications, is a most useful tool in preparation of soft tissues… before articular
[joint]
correction is attempted’
(Mitchell 1958).
•
Edward Stiles DO:
‘He
(Fred Mitchell Sr)
was focused on using muscles to
[treat]
restricted joint function. His main focus was not relaxing muscles but re-establishing joint mechanics’
(Stiles 2012, personal communication).
•
R.E. Kappler DO:
‘The term barrier may be misleading if it is interpreted as a wall or rigid obstacle to be overcome with a push. As a joint reaches the barrier, restraints in the form of tight muscles and fascia, serve to inhibit further motion.
We are pulling against restraints,
rather than pushing against some anatomic structure’
(Kappler 2003).
•
Fred Mitchell Jr DO:
‘The therapist’s force is always the counterforce. A common mistake is to ask the patient to ‘resist my effort’. This ignores the factor of intentionality that ensures that core muscles are re-educated and rehabilitated. What works best is to tell the patient the exact direction of the action, the amount of force, and when to stop’
(Fred Mitchell Jr interview, in Franke 2009).
•
Thomas Jefferson Ruddy DO:
Ruddy suggested the use of multiple mini-isometric contractions, [usually] towards the barrier, at a rate slightly faster than the pulse-rate. The patient is asked to introduce a series of these mini-contractions against [practitioner] resistance. For example…
‘contract-relax’, ‘contract-relax’, ‘contract-relax’
– 10 times. After this, as the
patient relaxes, the joint is eased to its new barrier. The process is repeated once more. These contractions should be performed without ‘wobble’ or ‘bounce’ (Ruddy 1962). See summary of Pulsed MET later in the chapter.
•
Karel Lewit MD:
‘Strong or moderate force contractions – as initially used in MET – recruited too many of the “wrong” motor units, and results were less that were hoped for. It was Karel Lewit who drastically reduced the force generated by muscle contractions’
(Mitchell Jr 2009).
•
John Goodridge DO:
‘
Muscle energy technique is not a wrestling match… A small amount of force should be used at first, with increase as necessary. This is much more productive than beginning with too much force… Localization of force is more important than intensity of force’
(Goodridge 1981).
•
Fred Mitchell Jr:
‘Isolytic
[eccentric isotonic]
contractions with vibratory counterforce, involves light to moderate force, sustained for no more than 15 seconds’
(Fred Mitchell Jr interview, in Franke 2009).
•
Gary Fryer PhD, DO:
‘The features that are required to ensure successful use of MET include: a precise positioning to the barrier; an active and appropriately formulated (strength, timing) muscle contraction, by the patient, against a defined resistance of the therapist, in a precise direction; the number of repetitions, and finally an accurate assessment of the therapeutic outcome’
(Chaitow 2013).
These quotes offer a sense of the evolution of MET, from fairly crude origins (where heavy degrees of patient effort were requested), to the use of subtle, low-force, specifically directed contractions of different types.
The ultimate focus remains the same, however – to normalize and rehabilitate the soft-tissue component of the body when dysfunctional, so allowing more normal, ideally pain-free, function – most particularly involving previously restricted joints. For a summary of the detail of MET application see
Box 12.2
, later in this chapter.
Basic MET
The elements that make up application of standard isometric MET
(see definitions above) always include:
•
Identification of a resistance barrier, whether this is the end-of-range of a muscle or a joint. The ‘end-of-range’ in MET (i.e. the barrier) represents the
very first sign of resistance to movement in any particular direction
(see
Ch. 5
),
and not
the physiological end of range, which, when identified, would always involve a degree of lengthening of the tissues being assessed. Basic MET is most effective when isometric contractions commence from an easy barrier, rather than an extended one.
•
Therefore an isometric – or sometimes isotonic eccentric – contraction is used, starting with the tissues just short of the resistance barrier, with the contraction directed towards or away from that barrier, or in another direction altogether.
•
In some instances the isometric contractions are achieved as a series of very brief, active rhythmic, ‘pulsing’ efforts, rather than sustained contractions. See the example later in the chapter.
•
Following an isometric contraction – a sustained single contraction for 5 to 7 seconds – or a series of pulsed efforts – the tissues are taken to a new barrier (if the condition is acute, or a joint is being treated) – or past the new barrier, into stretch if a chronic soft-tissue condition is being addressed.
•
A major effect of the isometric contractions has been described as producing a
‘reduced resistance to stretch’ – or ‘increased tolerance
to stretch’.
As discussed later in the section on
Fascial and other mechanisms of MET
(Magnusson et al. 1996).
•
MET
isometric
contractions should always involve the patient’s effort – against the therapist’s resistance. The same benefit will not be achieved if the patient is asked to resist the practitioner’s effort.
•
Where concentric
eccentric
stretching is used in MET, the patient partially resists the practitioner’s effort to stretch muscle, or to move a joint – so that a slow lengthening occurs of the contracting muscle(s).
•
Where eccentric stretching is used in MET, the practitioner overcomes the patient’s contraction effort, in order to stretch the contracting muscle(s).
Basic MET variations to try: instruction examples
1.
An example of a typical instruction when using an
isometric contraction
in treatment of levator scapula (
Fig 12.5
) might be:
Start gently and slowly to push your head backwards against my hand, and your shoulder blade upwards against the other hand – using no more than 30% of your available strength, until I ask you to slowly stop pushing.
2.
An example of a typical instruction when using an
isotonic eccentric contraction
of the hamstrings, with the patient lying supine and the leg held so that the hamstrings are just short of their easy resistance barrier (
Fig. 12.6
), might be:
Try to bend your knee against my resistance. Starting slowly, build up your effort, using no more than a third of your available strength, and maintain the effort for 5 to 7 seconds, while I gently stretch the muscles, and then slowly relax.
After releasing the contraction effort the leg would be straightened to a position where a small degree of stretch of the hamstrings (in this example) was achieved, and held there for between 5 and 30 seconds (depending on how chronic the problem is).
Figure 12.5
Hand positions and directions of resisted isometric contraction, and stretch application, in MET treatment of the right side levator scapula.
3.
A typical instruction when
pulsed MET
is being used might be:
Try to move the area that I am firmly holding, for less than one second, push and stop, push and stop, push and stop, etc., etc., OR pulse, pulse, pulse, etc. x20 – and then relax –
and then the joint should be gently moved to its new position (easy end-of-range) – and pulsations should be repeated in a different direction, against unyielding resistance from the operator.
It has been found that the most useful directions of effort, when pulsed MET (or indeed sustained isometric contractions) are used in treatment of a joint, is unpredictable since the particular soft tissues involved in the restriction are unknown. A variety of pulsed efforts should therefore be used to gain maximum improvement. Avoid any degree of effort that produces a wobble or bounce, nothing should be visible, just the practitioner’s sense of a pulsing effort against his/her very firm resistance.
Figure 12.6
Hand positions and directions of a slow eccentric stretch application in treatment of the shortened hamstring muscles.
4.
An example of a typical instruction when using an isotonic eccentric contraction involving the rectus femoris muscles – with the patient lying prone – might be:
Try to bend your knee using moderate force – and I will resist, and overcome your effort, by actually, slowly, straightening your leg as you try to flex it
(
Fig. 12.7
).
The patient needs to be taught to use just sufficient force to avoid the process from becoming stressful for either party. In this example it should allow a relatively slow, painless lengthening of the contracting rectus femoris. The abbreviation for this method is SEIS (slow eccentric isotonic stretch).
A more rapid version of this isotonic eccentric stretch is known as an isolytic contraction. The rationale and clinical usefulness of this is described later in the chapter – see discussion of the work of Parmar et al. (2011), under Clinical objectives of MET and evidence,
below.
Figure 12.7
Hand positions and directions of isotonic eccentric stretch application in MET treatment of rectus femoris.
Clinical objectives of MET and evidence
Pain relief, improved mobility, rehabilitation and reducing fibrosis
Some research has suggested that isometric contractions, as used in MET, even without subsequent stretching, may have powerful analgesic effects (Hoeger et al. 2011). Possible mechanisms for this are described later in the chapter under the heading: Fascial and other mechanisms of MET.
Lewit and Simons
(1984) used MET-type isometric contractions in treatment of 244 patients with myofascial pain, in whom trigger points (TrP) had been identified within affected muscles, which displayed tension and discomfort on stretching. The problematic muscle was passively stretched to a point just short of pain and then the patient performed a gentle isometric contraction for 10 seconds, followed by relaxation and further stretching, three to five times. Treatment resulted in immediate pain relief in 94% of patients, with lasting relief recorded in 63%.
Knebl
(2002) compared the use of the Spencer technique (
Box 12.1
) – an osteopathic sequence for passive mobilization of the shoulder – with the same protocol using MET in 29 elderly patients with chronic shoulder restrictions and pain. Eight treatment sessions lasting 30 minutes each were performed twice a week at weeks 2, 4 and 6, and once at weeks 10 and 14, over a 14-week period. Both forms of treatment (mobilization with, and mobilization without, MET) were found to produce improvements, but a greater increase was found in active and passive flexion in the group receiving MET. When participants were reassessed after the end of the treatment period, there was a trend for the range of motion (ROM) in the MET group to continue to increase, but also a trend for it to decrease in those treated with passive mobilization only (
Fig. 12.8
).
Figure 12.8
Spencer sequence: circumduction with compression.
Box 12.1 Exercise using circumduction of the shoulder joint, with compression – as part of the Spencer sequence
In addition to the method described below using MET with circumduction with compression, to treat shoulder restrictions, all other ranges of motion are tested and treated when
applied clinically: extension, flexion, internal and external rotation, adduction and abduction, and circumduction with traction.
NOTE:
If restriction or pain is noted during any of these movements, it is possible to evaluate which muscles would be active if precisely the opposite movement were undertaken and it is these which may be offering soft-tissue restriction to the movement. There may also be articular or capsular reasons for these restrictions and, if this is the case, soft-tissue involvement would be considered and assessed for.
In all of these variations the joint is moved through normal ranges until a sense of restriction is noted – at which time either a sustained isometric contraction,or pulsed MET is used to increase range – as in the description below.

The patient is sidelying with elbow flexed.
The patient is sidelying with elbow flexed.

The practitioner’s hand cups the shoulder while firmly compressing the scapula and clavicle to the thorax.
The practitioner’s hand cups the shoulder while firmly compressing the scapula and clavicle to the thorax.

The practitioner’s other hand grasps the elbow and takes the shoulder through a slow passive clockwise – and then a counter-clockwise – circumduction, while adding light compression through the long axis of the humerus.
The practitioner’s other hand grasps the elbow and takes the shoulder through a slow passive clockwise – and then a counter-clockwise – circumduction, while adding light compression through the long axis of the humerus.

This is repeated several times in order to assess range, freedom and comfort of the circumducting motion, as the humeral head moves on the surface of the glenoid fossa.
This is repeated several times in order to assess range, freedom and comfort of the circumducting motion, as the humeral head moves on the surface of the glenoid fossa.

Any discomfort or restriction is noted.
Any discomfort or restriction is noted.
Wherever in the circumduction resistance is noted, the patient should be asked to use very light pressure towards the direction of restriction – against the operator’s firm resistance – for 4 to 5 seconds.
On relaxing the circumduction, continue if some increased freedom of movement is noted. If not then the isometric contraction should be attempted away from the direction of restriction – or in a different direction altogether.
After relaxing the effort, the circumduction should be continued, if increased freedom of movement is noted. If not then a rhythmic pulsed series of isometric efforts should be made either towards, or away from, or in a different direction altogether, until increased range is regained.
The logic of using different directions of effort is that it is not possible to be certain which soft tissues are imposing a restricted range.
No pain should be experienced during any of these MET efforts. Similar strategies may be used in care of any joint restriction.
Hunt & Legal
(2010) conducted a randomized, single-blinded, controlled study, involving 80 subjects with piriformis spasm and pain, together with the presence of myofascial trigger points in that muscle. Twenty-eight subjects were treated using MET, with the objective of relaxing piriformis; a further 27 subjects were treated with a high velocity low amplitude (HVLA) thrust technique that applied rapid stretch to piriformis; the remainder (25 controls) were treated by a placebo measure. Outcomes involved assessment of pressure pain threshold (using algometry); hip internal rotation range (goniometry); and pain levels, using a visual analog scale. Both the MET and HVLA thrust methods produced an equally significant increase in piriformis extensibility, together with pain relief, compared with the placebo group.
Moore et al.
(2011) studied the effects of MET in treatment of shoulder ROM of amateur (college)
baseball players. A single application of MET was used on the glenohumeral joint (GHJ) horizontal abductors (19 subjects) and the GHJ external rotators (22 subjects), to improve ROM. The results showed that a single application of a MET procedure, on collegiate baseball players, for the GHJ horizontal abductors provided immediate improvements in both GHJ horizontal adduction and internal rotation ROM.
Parmar et al.
(2011) report on the use of slowly applied isotonic eccentric stretching (SEIS) compared with passive manual stretching (PMS) in knee rehabilitation following hip surgery. These orthopedic surgeons noted that while there was no difference in the significantly increased ROM that was eventually achieved (when comparing MET with PMS), those receiving MET showed significantly more rapid pain reduction. They describe the technique used as follows: ‘
With the patient in a side lying position, the hip was maintained in neutral with adequate stabilization of the pelvis. The knee was then taken to a range where the first resistance barrier was reached. The patient was then instructed to use 20 to 25% of the knee extensor force to resist the therapist applied flexion force. The knee was then moved to a new
[end of]
range, till a second resistance barrier was reached and held in that position for 15 seconds and then returned back to full extension. This technique was applied for 5 to 7 repetitions once daily.
’
Two key elements to note in this example are:
•
The easy end of range –
‘first sign of resistance’
– was used. As has been emphasized, this is a MET characteristic, unlike some other approaches where end of range is described as
‘first sign of discomfort’.
•
The patient’s attempt to extend the knee from that position – using 20–25% of available strength (not full strength) – was overcome by the practitioner, making this an isotonic eccentric stretch.
The rationale for use of SEIS and isolytic contractions (ILC) post-surgically is described as follows: ‘In immediate post-surgery groups we used SEIS in order to prevent excessive pain and to also allow gradual gentle lengthening, thereby assisting in the remodeling of the injured, as well as the surrounding, soft tissue. In the chronic phase, we used ILC which is more vigorous, in order to assist in breaking the fibrotic adhesions by controlled microtrauma, thus allowing improvement in elasticity and circulation during remodeling.
’
MET and hyaluronic acid (HA).
As described in
Chapter 1
, the sliding function of fascia requires the ample production of lubricants such as HA. This is stimulated by frictional, vibratory mechanisms – something easily incorporated into the application of isolytic or SEIS type stretches (Kuchera & Kuchera 1992).
Wilson et al.
(2003) suggest a form of pulsed MET for achieving rehabilitation focused on the intrinsic muscles of the spine (such as the rotatores, intertransversarii) – as this can offer marked benefits in terms of spinal stabilization and proprioceptive reeducation. ‘
A dysfunction of these muscles can lead to incorrect afferent input to the central nervous system, resulting in a distorted view of the spatial relationships of the motion segments. This can lead to an ineffective use and/or disuse of the primary dynamic stabilisers of the spine
’.
Description of the MET protocol recommended by Wilson et al. (2003) is too lengthy for this chapter. It can be found in full in
Chapter 9
of Chaitow (2013). What is required of the patient is explained as follows:
It is important for the patient to provide a very small contraction. The focus is to strengthen the small intersegmental muscles. These will quickly become overpowered by the larger prime mover muscles if too great a contraction is elicited. The clinician should bear in mind that the core musculature will activate before the periphery, therefore the muscle contraction
should be measured in ‘ounces’ (grams) instead of ‘pounds’ (kilos). The following are some examples of useful instructions to give to the patient:
•
‘Meet my force as I pull your leg towards the ceiling, but do not overpower me.’
•
‘Push into my hand as if you were pushing on an egg you did not want to break’
(Wilson et al. 2003).
NOTE:
Pulsed MET offers an ideal model for this protocol.
Lederman
(2011), among others, believes that the best means of resolving dysfunction, such as low back pain, should involve rehabilitation strategies, motor re-education and behaviorally focused methodologies – rather than manual modalities that may provide limited short-term effects. However, the opposite may also be true because – unless mobility, strength, motor control, and endurance features are restored to dysfunctional tissues, by means of methods such as MET – normal, pain-free function may be far more difficult to achieve.
Fascial and other mechanisms of MET
Fryer (2013) has summarized the major elements thought to be involved in MET efficacy. Current theories include:
•
Reflex muscle relaxation:
although some studies support the theory that muscle relaxation occurs after isometric contractions, there appears to be only a brief ‘post isometric relaxation’ effect, with other studies showing – paradoxically – that isometric contractions result in increased, rather than lowered, EMG activity in muscles. It seems probable therefore that
‘increased extensibility must occur due to other factors, such as viscoelastic change or increase to stretch tolerance’.
•
Viscoelastic or muscle property changes:
there is evidence that the addition of an isometric contraction increases the effects of passive stretching, possibly involving the parallel and series elastic components of sarcomeres. Changes in both the series elastic and parallel elastic elements of sarcomeres (as discussed above) take place during the active and passive phases of MET, contributing to muscle elongation, and increased range of motion (Milliken 2003; see
Fig. 12.4
).
•
In addition, processes such as hysteresis (see descriptions in
Ch. 1
,
Box 1.2
) may be involved in elastic changes; particularly, it is suggested, in younger individuals (Reid & McNair 2004). While not ruling it out as a contributory factor to increased tissue extensibility, viscoelastic change requires far more research to clarify its role in this process.
•
Stretch tolerance changes:
although the evidence lacks any specific explanation, studies have demonstrated that following MET the increase in the ability to lengthen tissues is due to
‘a tolerance of greater stretching force to extend the muscle’.
In other words, after an isometric contraction it is possible to lengthen previously restricted soft tissues more comfortably than before the contraction. If the same degree of force involved in stretching a hamstring after an isometric contraction was used before the contraction, it would not have been as well tolerated. This does not, however, explain the mechanism(s) involved!
Other possible mechanisms and explanations include:
•
As described in
Chapter 5
, hydraulic effects involving the extrusion of water from connective tissue, during contractions and stretching – allow increased freedom of movement for up to 30 minutes – during which time mobilization and/or exercise can be more efficiently achieved (Klingler et al. 2004).
•
Fryer and Fossum (2010) suggest that MET stimulates mechanoreceptors that initiate pain-
relieving responses, via both ascending and descending pain pathways. Additionally, MET induces mechanical stretching of fibroblasts that increases local blood flow and also alters interstitial osmotic pressure, reducing concentrations of pro-inflammatory cytokines, helping to desensitize pain receptors (Havas et al. 1997).
•
Wilson (in Chaitow 2013) has shown that MET has marked pain relieving effects in cases of acute low back pain: MET ‘
not only inhibits the alpha motor neuron, but the technique’s gentle stretching also inhibits Ia afferent nerves via post-activation depression. This is due to muscle energy technique’s ability to decrease the sensitivity of muscle spindles to stretch. This effect has been shown to last for more than 2 days
(Avela et al. 1999a,b).
This evidence fortifies the argument for the use of MET over other techniques in that the effects are not only longer lasting, but also because MET resolves the pain/spasm cycle by acting on both the efferent and afferent nerves.’
•
Natural analgesics, such as endorphins and/or endocannabinoids (as discussed in
Chapter 5
) appear to be released in response to MET (McPartland 2008).
•
As noted in
Chapter 5
– it is not possible to manually stretch the sheets of deep dense fascia; for example, in the thoracolumbar fascia. However, using MET makes it possible to reduce the tensional load imposed by hypertonic muscles on such sheets – so reducing the relative stiffness of the fascial planes.
Neurological, mechanical, endocrine, hydraulic – and possibly other – mechanisms appear to contribute jointly to the efficacy of MET.
How and where to acquire skills in MET?
All osteopathic schools teach MET, although not all introduce the more subtle versions, e.g. pulsed MET.
Physical therapists are usually taught elements of MET and are commonly also introduced to MET’s distant relation – proprioceptive neuromuscular facilitation (PNF) – although this approach has major differences from MET, as described in this chapter.
Other methods that are similar to MET include approaches described by different names (and with little or no reference to the osteopathic origins), such as ‘contract–relax’ (CR), ‘agonist contract–relax’ (ACR), contract–relax–agonist–contract (CRAC). Whatever the names used, these are all versions of MET, and are widely available as short courses and via books and video instruction.
The protocol list in
Box 12.2
summarizes the essentials of MET.
NOTE
: Most of the items in the protocol are based on clinical experience of the author of this chapter.
Box 12.2 Protocol summary
Q. What is ‘PIR’ in relation to MET?
A. Post-isometric relaxation (PIR) was the theoretical model for the mechanism thought to be involved in MET when the target tissues, the muscle(s) that require ‘release’, were involved in the isometric contraction. Post-isometric relaxation has been shown to occur, but to be too short-lived
to account for the ‘relaxation’ changes following MET use (Ballantyne et al 2003).
Q. What is ‘RI’ in relation to MET?
A. Reciprocal inhibition (RI) was the theoretical model for the mechanism thought to be involved in MET when the antagonists to the target tissues, the antagonists to the muscle(s) that require ‘release’, were involved in the isometric contraction. This effect (RI) has been shown to occur, but is too short-lived to account for the ‘relaxation’ changes following MET use (Ballantyne et al. 2003).
Q. Which barrier should be used in MET application?
A. Tissues should be taken to a point just short of the resistance barrier – i.e. to a point before any sense of tension (‘bind’) is noted (Mitchell 1998).
Q. How strong a contraction should be requested from the patient?
A. Less than one-third of available strength (Lewit 1999).
Q. For how long should an isometric contraction be maintained?
A. 5 to 7 seconds – or less than a second in pulsed MET – repeated for 10 seconds or so (Mitchell 1998).
Q. Should the isometric contraction involve agonist (‘PIR’) or antagonist (‘RI’)?
A. Use of the agonists – the tissues requiring release or lengthening – offers the best results, but pain may prevent their use, in which case the antagonists should be employed – or other muscles that might influence the restriction may be used.
Q. Should the direction of the isometric contraction be towards the barrier – or away from the barrier?
A. This is effectively the same as the previous question. If the effort is directed away from the barrier it involves the agonist muscles and ‘PIR’. If the contraction effort is towards the barrier it involves the antagonists and therefore ‘RI’.
Q. Is breathing cooperation required (respiratory synkinesis)?
A. In basic MET (i.e. not when eccentric stretching is involved), stretching or moving to a new barrier is usual on an exhalation – except in the case of quadratus lumborum because it fires on exhalation (Lewit 1999).
Q. Should there be a pause following the contraction before movement or stretching is introduced?
A. Yes – a moment of relaxation before the stretch commences is advised.
Q. After the isometric contraction should tissues be taken to the new barrier, or past the new barrier – and if so how far, and for how long?
A. In an acute situation there is no stretch – tissues are taken to a new barrier following the isometric contraction. In chronic settings the movement is to just past the barrier, for between 5 and 30 seconds – patient assisted if possible.
Q. How many repetitions should there be of the process described above?
A. 1–2; there seems to be little benefit in repeating the process beyond a second MET application.
Q. Describe a slow eccentric isotonic stretch (SEIS)
A. Tissues are taken towards a mid-range position, in the direction of restriction, and the patient should be requested to maintain that position as the operator slowly stretches the contracting muscles – to a new barrier of resistance, so stretching muscles as they contract. This is also commonly applied to the possibly inhibited antagonists of shortened muscle groups, so toning them.
Q. Describe a rapid isotonic eccentric MET stretch (isolytic)
A. The same as the previous description only performed rapidly in order to deliberately create micro-trauma in the contracting sarcomeres – reducing cross-linkages, fibrosis, etc. – to be followed by careful rehabilitation.
Q. Describe pulsed MET
A. Tissues around a restricted joint are firmly held at an easy end-of-range, and a request is made for a small degree of effort towards, or away from, the restriction barrier (or in another direction) that lasts for less than a second. Once the degree and direction of the brief effort has been successfully learned, the patient is asked to produce a series of 10–20 such contractions, rhythmically, against a firm counter-pressure, after which a new barrier is identified and used as a starting point for a further 15–20 mini-contractions (Ruddy 1962).
References
Avela J et al 1999a Reduced reflex sensitivity after repeated and prolonged passive muscle stretching. J Appl Physiol 86:1283–1291
Avela J et al 1999b Reduced reflex sensitivity persists several days after long-lasting stretch-shortening cycle exercises. J Appl Physiol 86:1292–1300
Ballantyne F Fryer G McLaughlin P 2003 The effect of muscle energy technique on hamstring extensibility: the mechanism of altered flexibility. J Osteopath Med 6(2):59–63
Chaitow L 2013 Muscle energy techniques, 4th edn. Churchill Livingstone Elsevier, Edinburgh
Educational Council on Osteopathic Principles (ECOP) 2009 Glossary of osteopathic terminology. American Association of Colleges of Osteopathic Medicine, Chevy Chase, MD
Findley T et al 2015 Transmission of muscle force to fascia during exercise. J Bodyw Mov Ther 19(1):19–123
Franke H 2009 The history of MET. In: Muscle energy technique history-model-research. Interview with Fred Mitchell Jr. Verband der Osteopathen Deutschland, Wiesbaden.
Franklyn-Miller A et al 2009 In: Fascial research II: Basic science and implications for conventional and complementary health care. Elsevier GmbH, Munich
Fryer G 2013 MET: efficacy and research. In: Chaitow L (ed) Muscle energy techniques. Churchill Livingstone Elsevier, Edinburgh
Fryer G, Fossum C 2010 Therapeutic mechanisms underlying muscle energy approaches. In: Fernández-de las-Peñas C et al (eds) Tension-type and cervicogenic headache: pathophysiology, diagnosis, and management. Jones and Bartlett, Sudbury, MA, pp 221–229
Goodridge J 1981 Muscle energy technique: definition, explanation, methods of procedure. J Am Osteopath Assoc 81:249–254
Havas E et al 1997 Lymph flow dynamics in exercising human skeletal muscle as detected by scintography. J Physiol 504:233–239
Hoeger B et al 2011 Pain perception after isometric exercise in women with fibromyalgia. Arch Phys Med Rehabil 92:89–95
Huijing P 2012 Myofascial force transmission: An introduction . In: Schleip R, Findley T, Chaitow L, Huijing P (eds) Fascia: the tensional network of the human body. Churchill Livingstone, Edinburgh
Hunt G, Legal L 2010 Comparative study on the efficacy of thrust and muscle energy techniques in the piriformis muscle. Osteopatía Scientífica 5(2):47–55
Huxley AF, Niedergerke R 1954 Structural changes in muscle during contraction: interference microscopy of living muscle fibres. Nature 173(4412):971–973
Kappler R 2003 Thrust (high-velocity/low-amplitude) techniques. In: Ward RC (ed) Foundations for osteopathic medicine, 2nd edn. Lippincott, Williams & Wilkins, Philadelphia, pp 852–880
Klingler W, Schleip R, Zorn A 2004 European Fascia Research Project Report. 5th World Congress Low Back and Pelvic Pain, Melbourne, November 2004
Knebl J 2002 Improving functional ability in the elderly via the Spencer technique, an osteopathic manipulative treatment: a randomized, clinical trial. J American Osteopathic Assoc 102(7):387–400
Kuchera WA, Kuchera ML 1992 Osteopathic principles in practice. Kirksville College of Osteopathic Medicine Press, Kirksville, MO
Lederman E 1997 Fundamentals of manual therapy. Churchill Livingstone, Edinburgh
Lederman E 2011 The fall of the postural-structural-biomechanical model in manual and physical therapies: Exemplified by lower back pain. J Bodyw Mov Ther 15:130–152
Lewit K, Simons DG 1984 Myofascial pain: relief by postisometric relaxation. Arch Phys Med Rehabil 65:452–456
Lewit K 1999 Manipulation in rehabilitation of the locomotor system. Butterworths, London
McPartland JB 2008 Expression of the endocannabinoid system in fibroblasts and myofascial tissues. J Bodyw Mov Ther 12(2):169
Maas H 2009 Mechanical interactions between skeletal muscles. In: Shinohara M (ed) Advances in neuromuscular physiology of motor skills and muscle fatigue. Research Signpost, Kerala, India, pp 285–302
Magnusson S et al 1996 A mechanism for altered flexibility in human skeletal muscle. J Physiol 497(1):291–298
Milliken K 2003 The effects of muscle energy technique on psoas major length. Unpublished MOst Thesis. Unitec New Zealand, Auckland, New Zealand
Mitchell FL 1958 Structural pelvic function. In: Barnes MW (ed) Yearbook of the Academy of Applied Osteopathy. American Academy of Osteopathy, Indianapolis, IN, pp 71–90
Mitchell Jr FL 1998 PKG The muscle energy manual, vol 2. MET Press, East Lansing, p 1
Mitchell Jr FL, Mitchell PKG 1999 The muscle energy manual, vol 3. MET Press, East Lansing
Mitchell Jr FL 2009 Influences, inspirations, and decision points. In: Franke H (ed) Muscle energy technique. History – Model Research, Marixverlag, Wiesbaden
Moore S et al 2011 The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. J Orthop Sports Phys Ther 41(6):400–407
Parmar S et al 2011 The effect of isolytic contraction and passive manual stretching on pain and knee range of motion after hip surgery: a prospective, double-blinded, randomized study. Hong Kong Physiotherapy Journal 29:25–30
Reid D, McNair P 2004 Passive force, angle, and stiffness changes after stretching of hamstring muscles. Med Sci Sports Exercise 36:1944–1948
Rijkelijkhuizen 2005 Extramuscular myofascial force transmission for in situ rat medial gastrocnemius and plantaris muscles in progressive stages of dissection. J Exp Biol 208:129–140
Ruddy T 1962 Osteopathic rapid rhythmic resistive technic. Academy of Applied Osteopathy Yearbook, Carmel, CA, pp 23–31
Schleip R 2003a Fascial plasticity: a new neurobiological explanation. Part I. J Bodyw Mov Ther 7(1):11–19
Schleip R 2003b Fascial plasticity: a new neurobiological explanation. Part II. J Bodyw Mov Ther 7(2):104–116
Stecco A et al 2013 The anatomical and functional relation between gluteus maximus and fascia lata. J Bodyw Mov Ther 17(4): 512–517
Weppler CH, Magnusson SP 2010 Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther 90:438–449
Wilson E et al 2003 Muscle energy technique in patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther 33:502–512


Slow eccentric isotonic stretch:
The operator offers greater counterforce than the patient, which slowly stretches the muscle while it is trying to shorten. The
series elastic fascial component
and the
parallel elastic fascial component
are simultaneously lengthened. The objective is to strengthen the muscle involved, and to relax it, while simultaneously inhibiting excess to its antagonists.
Slow eccentric isotonic stretch:
The operator offers greater counterforce than the patient, which slowly stretches the muscle while it is trying to shorten. The
series elastic fascial component
and the
parallel elastic fascial component
are simultaneously lengthened. The objective is to strengthen the muscle involved, and to relax it, while simultaneously inhibiting excess to its antagonists.

Rapid eccentric isotonic stretch (isolytic contraction).
This may be useful in cases where there exists a chronic degree of fibrotic change. The effect is to stretch and alter these tissues – inducing controlled microtrauma – thus allowing an improvement in elasticity, circulation and function during subsequent remodeling (Goodridge 1981).
Rapid eccentric isotonic stretch (isolytic contraction).
This may be useful in cases where there exists a chronic degree of fibrotic change. The effect is to stretch and alter these tissues – inducing controlled microtrauma – thus allowing an improvement in elasticity, circulation and function during subsequent remodeling (Goodridge 1981).






The patient is sidelying with elbow flexed.
The patient is sidelying with elbow flexed.

The practitioner’s hand cups the shoulder while firmly compressing the scapula and clavicle to the thorax.
The practitioner’s hand cups the shoulder while firmly compressing the scapula and clavicle to the thorax.

The practitioner’s other hand grasps the elbow and takes the shoulder through a slow passive clockwise – and then a counter-clockwise – circumduction, while adding light compression through the long axis of the humerus.
The practitioner’s other hand grasps the elbow and takes the shoulder through a slow passive clockwise – and then a counter-clockwise – circumduction, while adding light compression through the long axis of the humerus.

This is repeated several times in order to assess range, freedom and comfort of the circumducting motion, as the humeral head moves on the surface of the glenoid fossa.
This is repeated several times in order to assess range, freedom and comfort of the circumducting motion, as the humeral head moves on the surface of the glenoid fossa.

Any discomfort or restriction is noted.
Any discomfort or restriction is noted.