CHAPTER 1
The Big Picture
I completed my medical training in the 1990s, as the obesity epidemic approached crisis proportions. Incredibly, two out of three American adults had become excessively heavy. For the first time in medical history, type 2 diabetes (previously termed “adult onset diabetes”) had begun striking children as young as ten years old. And economic forecasts predicted that the annual medical costs of obesity would soon exceed $100 billion. Amid these disturbing developments, I decided to specialize in obesity prevention and treatment.
Like many young doctors, I had received virtually no instruction in nutrition. Then, as now, medical schools focused almost exclusively on drugs and surgery, even though lifestyle causes most cases of heart disease and other chronic disabling conditions. In retrospect, my lack of formal knowledge of nutrition was a blessing in disguise.
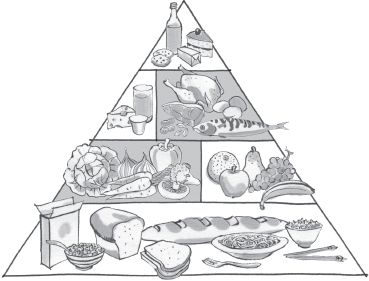
The 1990s were the height of the low-fat diet craze, exemplified by the original Food Guide Pyramid, published in 1992 (see figure here). Based on the notion that all calories are alike, the pyramid advised us to avoid all types of fat because they contain twice the calories of other major nutrients. Instead, we were told to load up on carbohydrates, including six to eleven servings each day of bread, cereal, crackers, pasta, and other grain products. Luckily, I hadn’t been indoctrinated in these conventional teachings and began my career in research and patient care with an open (and mostly empty) mind when it came to nutrition.
The Food Guide Pyramid of 1992
My first professional research position was in a basic science laboratory conducting experiments with mice. Soon after starting this work, I became amazed by the beauty and complexity of the systems that control body weight. If we fasted a mouse for a few days, it would, of course, lose weight. Then, when given free access to food, the animal ate voraciously until it had regained all of the lost weight—no more, no less. The opposite was also true. Force-feeding could temporarily make a mouse fat, but afterward it would avoid food until its weight dropped back to normal. Based on these and other experiments, it seemed as if an animal’s body knew precisely what weight it wanted to be, automatically altering food intake and metabolism to reach a sort of internal set point, like a thermostat that keeps a room at just the right temperature.
Our most interesting scientific experiments explored how this “body weight set point” could be manipulated. If we modified certain genes, administered drugs, or altered diet in particular ways, the mice predictably gained weight to a new stable level. Other changes caused permanent weight loss, without apparent signs of distress. These experiments demonstrated a fundamental principle of the body’s weight-control systems: Impose a change in behavior (for example, by restricting food), and biology fights back (with increased hunger). Change biology, however, and behavior adapts naturally—suggesting a more effective approach to long-term weight management.
In the midst of my stint in basic research, I helped develop my hospital’s newly established family-based weight management clinic, called the Optimal Weight for Life (OWL) program. Like virtually all specialists at the time (and many to this day), our team of doctors and dietitians focused at first on calorie balance, instructing patients to “eat less and move more.” We prescribed a low-calorie/low-fat diet, regular physical activity, and behavioral methods to help people ignore hunger, resist cravings, and stick with the program. When they returned to the clinic, my patients usually claimed to have followed recommendations. But with few exceptions, they kept gaining weight—a depressing experience for everyone involved. Was it the patients’ fault for not being honest with me (and perhaps themselves) about how much they ate and how little they exercised? Or was it my fault for lacking the skills to motivate patients to change? I felt ashamed of judging my patients negatively and felt like a failure as a physician. I dreaded going to the clinic, and I’m sure some of my patients felt the same way. I suspect many doctors and patients at weight loss clinics throughout the country can relate.
After about a year of this schizophrenic existence—fascinated with biology in the lab, frustrated with behavior change among my patients in the clinic—I began to wonder about the disconnect. Why did basic scientists think one way about obesity and practicing clinicians another? Why did we disregard decades of research into the biological determinants of body weight when treating patients? And why were we using an approach to weight loss based on a “calories in, calories out” model that hadn’t changed since the late 1800s, when bloodletting was still in vogue?
So I launched into an intensive examination of the literature, from popular diet book authors like Barry Sears (The Zone Diet) and Robert Atkins (Dr. Atkins’ New Diet Revolution) to George Cahill, Jean Mayer, and other preeminent nutrition scientists of the last century. I spent hundreds of hours poring over musty volumes in Harvard’s medical library, rediscovering provocative but neglected theories about diet and body weight. And I began to realize just how little evidence there was to support standard obesity treatment.
Soon, my entire perspective shifted. I came to see food as so much more than a delivery system for calories and nutrients. Although a bottle of cola and a handful of nuts may have the same calories, they certainly don’t have the same effects on metabolism. After every meal, hormones, chemical reactions, and even the activity of genes throughout the body change in radically different ways, all according to what we eat. These biological effects of food, quite apart from calorie content, could make all the difference between feeling persistently hungry or satisfied, between having low or robust energy, between weight gain or loss, and between a lifetime of chronic disease or one of good health. Instead of calorie counting, I began to think of diet in an entirely different way—according to how food affects our bodies and, ultimately, our fat cells.
MY PERSONAL TESTIMONIAL
At that time, I was in my thirties and, like so many Americans, had gained an extra pound or two each year since high school. For most of my life, I was fit and lean, and ate reasonably well, at least according to conventional standards: not too much fat, lots of whole-grain products, several servings a day of vegetables and fruits, and relatively little sugar. But after several years of steady weight gain, I had approached the threshold for becoming overweight, a body mass index (BMI) of 25.*
For my first clinical research study, I experimented on myself, guided by my rapidly evolving understanding of nutrition. I doubled my intake of fat, with generous servings of nuts and nut butters, full-fat dairy products, avocado, and dark chocolate, and ate vegetables drenched in olive oil. I increased protein just a bit and cut back on my starchy staples, including bread, cereal, pasta, and pastries. I made a few other changes, none especially difficult, but no attempt to reduce calories, eliminate all carbohydrates, or deprive myself in any way.
Within a week, I felt an astonishing improvement in energy and vitality, and a robust sense of well-being that lasted throughout the day—as if some previously unknown but important metabolic switch had finally been flipped on. Four months later, I had lost 20 pounds and needed a new wardrobe two pants sizes smaller. Most remarkably, all this had occurred with no hunger and no carbohydrate cravings. Previously, I would be famished by late afternoon, and usually staved off hunger in the lab with a four p.m. break for a carb-laden vanilla scone from the local bakery. But with my new diet, I felt full for hours after eating. For the first time in my life, I completely lost interest in bread, which used to accompany my every breakfast, lunch, and dinner. And when it was time for a meal, I’d experience a pleasant, stimulating interest in food, entirely different from feeling starved and in desperate need of calories.
The successful outcome of this self-experiment, coupled with new insights into nutrition, renewed my enthusiasm for patient care, with the exciting prospect of something that might actually work in the clinic. Over the next few years, I transitioned out of the animal laboratory and into clinical research. I made it my mission to explore alternative diets under scientifically controlled conditions and have continued that line of research to this day.
FORGET CALORIES
Virtually all weight loss recommendations from the U.S. government and professional nutritional organizations rest on the notion that “a calorie is a calorie”1—a strategy with appealing simplicity. “Just eat less and move more,” they say. “Consume fewer calories than you burn off, and you’ll lose weight.” There’s just one problem: This advice doesn’t work—not for most people over the long term. Obesity rates remain at historic highs, despite an incessant focus on calorie balance by the government, professional health associations, and the food industry (witness the “100 calorie pack”). Furthermore, the customary method to reduce calorie consumption since the 1970s—a low-fat diet—has failed miserably.
Although the focus on calorie balance rarely produces weight loss, it regularly causes suffering. If all calories are alike, then there are no “bad foods,” and the onus is on us to exert self-control. This view blames people with excess weight (who are presumed to lack knowledge, discipline, or willpower)—absolving the food industry of responsibility for aggressively marketing junk food and the government for ineffective dietary guidance.
All too often, people hear the message, “It’s your fault that you’re fat”—as if they could simply will away the extra weight. In a sense, being heavy has become prime evidence of a weakness of character, provoking prejudice and stigmatization. Overweight children commonly experience teasing, abuse, and bullying from peers, sometimes with tragic consequences.2 Adults face endless indignities, from workplace discrimination to insensitive characterizations on television. Not surprisingly, high BMI is sometimes accompanied by major psychological distress, including anxiety, depression, and social isolation.3
The “calorie is a calorie” concept also has prompted development of some patently bizarre products, such as “low-fat” candy, cookies, and salad dressings, typically containing more sugar than the original full-fat versions. Are we really to believe that, for someone on a diet, a cup of cola with 100 calories would make a better snack than a 1-ounce serving of nuts containing almost 200 calories?
New research has revealed the flaws in this way of thinking. Recent studies show that highly processed carbohydrates adversely affect metabolism and body weight in ways that can’t be explained by their calorie content alone. Conversely, nuts, olive oil, and dark chocolate—some of the most calorie-dense foods in existence—appear to prevent obesity, diabetes, and heart disease. In truth, the obesity epidemic is not about willpower or weakness of character. All this time, we’ve been diligently following the diet rules, but the rulebook was wrong!
In a recent study published in the Journal of the American Medical Association (JAMA),4 my colleagues and I examined twenty-one young adults with high BMI after they had lost 10 to 15 percent of their weight on diets ranging from low fat to low carbohydrate. Despite consuming the same total calories on each diet, the participants burned about 325 calories a day more on the low-carbohydrate diet than on the low-fat diet, amounting to the energy expended in an hour of moderately vigorous physical activity. So the type of calories we eat can affect the number of calories we burn.
Over the last few years, we seem to have been moving toward the tipping point, with reputable scientists acknowledging the previously unthinkable possibility that all calories aren’t alike. Even Weight Watchers, for decades the leading advocate of calorie counting, now assigns “0 Points” to fruit.5 Meaning that if you had the fortitude, you could eat a 10-pound watermelon containing most of your daily calorie requirement “for free”—in flagrant defiance of the calorie-counting approach to weight loss. The entire concept of calorie balance seems to be tottering!
It’s time for a new approach, but which way do we turn?
FOCUS ON THE FAT CELL
Just as food is much more than the calories and nutrients necessary for survival, so are fat cells much more than passive storage sites for excess calories. Fat cells take in or release calories only when instructed to do so by external signals—and the master control is insulin. Too much insulin causes weight gain, whereas too little causes weight loss. So if we think about obesity as a disorder involving fat cells, then a radically different view emerges:
Overeating doesn’t make us fat. The process of becoming fat makes us overeat.
In other words, hunger and overeating are the consequences of an underlying problem.6 Though this proposition sounds radical, consider what happens in pregnancy. The fetus doesn’t grow because the mother eats more; she eats more because the fetus is growing. With pregnancy, this is normal and healthy. With obesity, it’s not.
How and why does this happen? For many people, something has triggered fat cells to suck up and store too many calories from the blood. Consequently, fewer calories are available to fuel the energy needs of the body. Perceiving a problem, the brain unleashes the starvation response, including measures to increase calorie intake (hunger) and save energy (slower metabolism). Eating more solves this “energy crisis” but also accelerates weight gain. Cutting calories reverses the weight gain temporarily, but inevitably increases hunger and slows metabolism even more.
One obvious source of the problem is highly processed carbohydrates—the bread, breakfast cereals, crackers, chips, cakes, cookies, candy, and sugary drinks that flooded our diets during the low-fat era. Anything containing primarily refined grains, potato products, or concentrated sugar digests rapidly, raising insulin levels excessively and programming fat cells to hoard calories. But refined carbohydrates aren’t the only problem. Other aspects of our highly processed diet and elements of our modern lifestyle—including stress, sleep deprivation, and sedentary habits—have forced fat cells into calorie-storage overdrive.
Fortunately, these negative effects are reversible.
TAKE BACK CONTROL
The conventional calorie balance approach fails because it’s focused on the wrong target. The fundamental problem isn’t having too many calories in the body; it’s having too few in the right place, circulating in the bloodstream and available for our immediate needs. Highly processed carbohydrates overstimulate fat cells, driving them into a frenzy. They become greedy and consume more than their fair share of calories. While fat cells feast, the rest of the body starves. Like unruly children with indulgent parents, these cells run the show and wreak havoc on our metabolism. Under these conditions, we become quite powerless.
Sure, we can cut back our calories for a while. But further limiting the calories available to the body actually makes matters worse. Before long, our bodies rebel against enforced deprivation. It’s not a matter of willpower so much as biology and time. Eventually, we succumb and overeat, typically on all the wrong foods, fueling a vicious cycle of weight gain.
The conventional approach, the calorie-restricted diet, aims to force calories out of the fat cells so that we lose weight—but in that battle fat has the upper hand. Before those cells will shrink, the body must suffer. Our mind may say “eat less,” but our metabolism responds “NO!”—a battle that the mind rarely wins.
The solution is to make a truce with our fat cells, help them calm down, and convince them to cooperate with the rest of the body. The way to do this is by changing what we eat, not how much. Here’s the basic strategy:
1. Turn off the starvation response by eating whenever you’re hungry and until fully satisfied.
2. Tame your fat cells with a diet that lowers insulin levels, reduces inflammation (insulin’s troublemaker twin), and redirects calories to the rest of your body.
3. Follow a simple lifestyle prescription focused on enjoyable physical activities, sleep, and stress relief to improve metabolism and support permanent behavior change.
Think of this plan as obedience training for your fat cells. I’ll show you how to do it, step by step, in part 2.
GAIN WHILE LOSING
Many people associate the word “diet” with suffering, and for good reason. Most diets demand great sacrifice in the present (food deprivation, hunger) in exchange for the promise of an abstract benefit at some seemingly distant point in the future (being thin, avoiding diabetes). That’s a recipe for failure. We may begin a diet with the best of intentions, but soon succumb to cravings if our sacrifice isn’t rewarded. It’s human nature.
The Always Hungry Solution in part 2 aims to put the science of metabolism on your side and by doing so, provide maximum benefit with minimum effort. When what we eat supports our body’s metabolism, the benefits begin right away, even before the first pound is shed—less hunger, fewer cravings, longer-lasting satisfaction from food, improved energy, and more stable mood. It’s like finally shifting your bicycle into the right gear. Suddenly, you move much faster and with less exertion. This way, enjoyment of life increases even as weight loss proceeds.
You might be wondering how anyone could enjoy a weight loss diet. Isn’t the problem that we’ve given in to pleasure too often and can’t resist tasty food? Why would we overeat if it weren’t so enjoyable?
Of course, we do all sorts of things for a bit of pleasure now, at the cost of long-term suffering later. That’s the nature of addiction. For many people, eating involves constant swings from unpleasantly hungry to uncomfortably full. On this roller-coaster ride, highly processed food may provide a few minutes of enjoyment, but it quickly sets us up for the next downward swing, with negative effects on our physical and mental well-being. Fortunately, unlike many classic addictions, we can quickly free ourselves from this vicious cycle and increase overall enjoyment, even as we lose weight. When we fill up on luscious, satisfying foods, there’s little room left for the other stuff.
SENSATIONAL VERSUS SUSTAINABLE WEIGHT LOSS
All too often, popular diets today promise extreme weight loss. Most never live up to expectation. But even if they did, what’s the benefit of losing 14 pounds in ten days, if you’re starving, fatigued, and struggling to keep the weight off? These diets can also take a big psychological toll. Many of us are, in a sense, estranged from our bodies and have learned to disregard critically important feedback signals that provide information about our internal state. Calorie-restricted diets require you to ignore one such signal—hunger—providing an endless array of behavioral tricks to do so. Drink lots of water, call a friend, go for a walk—anything to take your mind off your hunger. Or serve meals on a small plate, so that you’ll believe you’ve eaten more than you have. The problem is, this strategy makes the body-mind disconnect worse.
In reality, we’ve outsourced control of our bodies to the “experts.” But no diet book author could possibly know what level of calorie intake is right for everyone. People’s needs vary based on age, size, physical activity level, and individual metabolic differences. And some people, perhaps for genetic reasons, simply can’t tolerate rapid weight loss.
The Always Hungry Solution is designed to work from the inside out, creating the internal conditions for weight loss to occur naturally. Follow the meal plan, eat when hungry, and stop when satisfied but before becoming uncomfortably full. This way, your body will find the rate of weight loss right for you—2 pounds a week or more for some people, perhaps just half a pound a week for others. But without deprivation or hunger, these results will be progressive and sustainable.
My team and I conducted a 16-week pilot test of the Always Hungry Solution with 237 women and men, including 137 employees of Boston Children’s Hospital and 100 people who responded to a call for participants that appeared in a national health magazine. In addition to weight loss, participants consistently reported other benefits that predict long-term success, including:
• Decreased hunger
• Longer-lasting satiety after eating
• Great satisfaction with food
• More stable mood
• Improved overall well-being
• Reduced weight-related complications
You’ll read about the experiences of these participants throughout the book and especially in part 2.
WINDING UP, GETTING STARTED
In full disclosure, this diet—like all other diets—hasn’t been fully proven. The pilot project didn’t include a control group and wasn’t intended as scientific research. We can’t be sure how these outcomes would apply to the general public. But the ideas presented in this book culminate a century of research questioning the calorie balance model of obesity, and represent a fundamentally different way to understand why we gain weight and what we can do about it.7 For those of you with a scientific bent, I’ve included hundreds of supporting studies from many research teams among the references.
The central concept of Always Hungry? is that while cutting calories will decrease weight for a short while, the body resists by increasing hunger and slowing metabolism. Sooner or later we succumb, and weight tends to pop back up, like an air-filled balloon being pushed into a bucket of water. In contrast, improving the quality of what we eat will reprogram fat cells to store fewer calories, in effect reducing the “body weight set point.” As a result, weight lowers naturally, as the balloon would if some water were drained from the bucket in which it floats.
I base this book on my twenty years of experience as a physician and researcher at Harvard Medical School. During that time, I have overseen dozens of diet studies, authored more than one hundred peer-reviewed scientific articles, and cared for thousands of patients struggling with their weight. I am convinced of the power of this approach and believe it will help you lose weight, feel better, avoid type 2 diabetes and other chronic diseases, and improve the overall quality of your life—without the struggle so common to conventional diets.
The stories you’ll read about people following this program are real, and represent their authentic experience. Pilot participants provided their stories freely and received no financial compensation.
Now I invite you to forget calories, focus on the quality of your food, and judge for yourself if this program works for you.