BLISTERS (VESICLES AND BULLAE)
![]()
The GP overview
Blisters are skin swellings containing free fluid. Up to 5 mm they are called vesicles, larger than 5 mm they are called bullae. The fluid can be lymph, serum, extracellular fluid or blood. Some conditions cause both kinds of blister, but others mainly one or other type. Pustules are dealt with elsewhere (see p. 403).
![]()
Differential diagnosis
COMMON
 trauma: skin friction, burns (thermal and chemical), insect bites
trauma: skin friction, burns (thermal and chemical), insect bites
 herpes simplex
herpes simplex
 herpes zoster
herpes zoster
 childhood viruses: hand, foot and mouth disease, chickenpox
childhood viruses: hand, foot and mouth disease, chickenpox
 eczema (pompholyx and other acute eczemas)
eczema (pompholyx and other acute eczemas)
OCCASIONAL
 pemphigus and pemphigoid
pemphigus and pemphigoid
 dermatitis herpetiformis
dermatitis herpetiformis
 secondary to leg oedema (various causes)
secondary to leg oedema (various causes)
 bullous impetigo
bullous impetigo
 drug reactions, e.g. ACE inhibitors, penicillamine, barbiturates
drug reactions, e.g. ACE inhibitors, penicillamine, barbiturates
 erythema multiforme
erythema multiforme
RARE
 pemphigoid (herpes) gestationis
pemphigoid (herpes) gestationis
 porphyria
porphyria
 toxic epidermal necrolysis (Lyell’s syndrome)
toxic epidermal necrolysis (Lyell’s syndrome)
 epidermolysis bullosa
epidermolysis bullosa
 allergic vasculitis
allergic vasculitis
![]()
Ready reckoner

![]()
Possible investigations
There are unlikely to be any investigations that will prove useful in primary care. Usually, the problem is either self-limiting or the cause obvious; in obscure cases, referral may result in skin biopsy to establish the diagnosis. Patch testing may also be useful to identify possible allergens in contact dermatitis, especially if occupational.
TOP TIPS
 Herpes zoster involving the ophthalmic division of the trigeminal nerve will affect the eye in about 50% of cases. The likelihood is increased if there are blisters on the side of the nose. Ensure that the patient knows to seek help urgently if the eye becomes red or painful, or there is blurring of vision.
Herpes zoster involving the ophthalmic division of the trigeminal nerve will affect the eye in about 50% of cases. The likelihood is increased if there are blisters on the side of the nose. Ensure that the patient knows to seek help urgently if the eye becomes red or painful, or there is blurring of vision.
 In uncomplicated herpes zoster, explain the natural history of the condition to the patient, resolving any worries (old wives’ tales abound) and warning about the possibility of post-herpetic neuralgia.
In uncomplicated herpes zoster, explain the natural history of the condition to the patient, resolving any worries (old wives’ tales abound) and warning about the possibility of post-herpetic neuralgia.
 Follow up unexplained rashes. The bullae of pemphigoid, for example, may be preceded by itching, erythema and urticaria by several weeks.
Follow up unexplained rashes. The bullae of pemphigoid, for example, may be preceded by itching, erythema and urticaria by several weeks.

 Herpes simplex and varicella zoster infections can become severe and disseminated in the immunosuppressed: admit. Similarly, herpes simplex can result in a serious reaction (Kaposi’s varicelliform eruption) in patients with atopic eczema.
Herpes simplex and varicella zoster infections can become severe and disseminated in the immunosuppressed: admit. Similarly, herpes simplex can result in a serious reaction (Kaposi’s varicelliform eruption) in patients with atopic eczema.
 Pregnant women with chickenpox are at significant risk of severe varicella pneumonia; there are also risks to the foetus. Follow the detailed guidance in the ‘Green Book’ (Immunisation against Infectious Disease, Her Majesty’s Stationery Office) when dealing with pregnant women who have been in contact with chickenpox.
Pregnant women with chickenpox are at significant risk of severe varicella pneumonia; there are also risks to the foetus. Follow the detailed guidance in the ‘Green Book’ (Immunisation against Infectious Disease, Her Majesty’s Stationery Office) when dealing with pregnant women who have been in contact with chickenpox.
 Toxic epidermal necrolysis (scalded skin syndrome) can develop rapidly in infants and children, causing serious illness. Admit urgently if you suspect this diagnosis.
Toxic epidermal necrolysis (scalded skin syndrome) can develop rapidly in infants and children, causing serious illness. Admit urgently if you suspect this diagnosis.
 Pemphigus is a serious condition affecting a younger age group (usually middle-aged) than pemphigoid. Inpatient care is usually required.
Pemphigus is a serious condition affecting a younger age group (usually middle-aged) than pemphigoid. Inpatient care is usually required.
ERYTHEMA
![]()
The GP overview
Erythema is a reddening of the skin due to persistent dilation of superficial blood vessels, and can be local or generalised. It is distinguished from flushing (see p. 197) by its permanence: flushing is transient.
![]()
Differential diagnosis
COMMON
 cellulitis
cellulitis
 gout
gout
 burns: thermal, chemical, sunburn
burns: thermal, chemical, sunburn
 toxic erythema: drugs (e.g. antibiotics, NSAIDs), bacteria (e.g. scarlet fever), viruses (e.g. measles, slapped cheek syndrome)
toxic erythema: drugs (e.g. antibiotics, NSAIDs), bacteria (e.g. scarlet fever), viruses (e.g. measles, slapped cheek syndrome)
 rosacea
rosacea
OCCASIONAL
 palmar erythema, e.g. pregnancy, liver disease, thyrotoxicosis
palmar erythema, e.g. pregnancy, liver disease, thyrotoxicosis
 phototoxic reaction to drugs, e.g. phenothiazines, tetracyclines, diuretics
phototoxic reaction to drugs, e.g. phenothiazines, tetracyclines, diuretics
 ‘deck-chair legs’ (prolonged immobility)
‘deck-chair legs’ (prolonged immobility)
 erythema multiforme (various causes)
erythema multiforme (various causes)
 systemic lupus erythematosus (erythematous, photosensitive butterfly rash)
systemic lupus erythematosus (erythematous, photosensitive butterfly rash)
 erythema ab igne (reticulate pattern)
erythema ab igne (reticulate pattern)
RARE
 fixed drug eruption
fixed drug eruption
 livedo reticularis: connective tissue disease
livedo reticularis: connective tissue disease
 seroconversion rash of HIV
seroconversion rash of HIV
 erythema nodosum: sarcoidosis, streptococci, tuberculosis, drugs
erythema nodosum: sarcoidosis, streptococci, tuberculosis, drugs
 erythema induratum (Bazin’s disease: tuberculosis)
erythema induratum (Bazin’s disease: tuberculosis)
 erythema chronicum migrans: Lyme disease
erythema chronicum migrans: Lyme disease
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: uric acid (if possible gout).
POSSIBLE: FBC, ESR/CRP, LFT, TFT.
SMALL PRINT: autoimmune studies, serology, CXR, ASO titre.
 FBC/ESR/CRP: WCC and ESR/CRP raised in significant infection; Hb may be reduced (normochromic normocytic) in connective tissue disorder.
FBC/ESR/CRP: WCC and ESR/CRP raised in significant infection; Hb may be reduced (normochromic normocytic) in connective tissue disorder.
 Autoimmune studies: if connective tissue disorder a possibility.
Autoimmune studies: if connective tissue disorder a possibility.
 Serology: may help if suspect infective cause for erythema multiforme; also useful in assessing immune status in a pregnant woman exposed to slapped cheek syndrome, and in diagnosis of HIV infection and Lyme disease.
Serology: may help if suspect infective cause for erythema multiforme; also useful in assessing immune status in a pregnant woman exposed to slapped cheek syndrome, and in diagnosis of HIV infection and Lyme disease.
 Uric acid: to confirm clinical suspicion of gout (when attack has subsided) especially if considering allopurinol.
Uric acid: to confirm clinical suspicion of gout (when attack has subsided) especially if considering allopurinol.
 LFT, TFT: if palmar erythema present in non-pregnant patient – to detect alcohol excess or hyperthyroidism.
LFT, TFT: if palmar erythema present in non-pregnant patient – to detect alcohol excess or hyperthyroidism.
 Other investigations for erythema nodosum: if a non-drug cause is possible, investigations likely to include CXR (for TB, sarcoidosis) and ASO titre (for streptococcal infection).
Other investigations for erythema nodosum: if a non-drug cause is possible, investigations likely to include CXR (for TB, sarcoidosis) and ASO titre (for streptococcal infection).
TOP TIPS
 Toxic erythema caused by drugs tends to be itchy; if due to infection, it does not irritate but is accompanied by fever.
Toxic erythema caused by drugs tends to be itchy; if due to infection, it does not irritate but is accompanied by fever.
 Remember that there is often a delay before a drug causes toxic erythema – therefore, symptoms may only appear after a course of treatment (especially antibiotics) has been completed.
Remember that there is often a delay before a drug causes toxic erythema – therefore, symptoms may only appear after a course of treatment (especially antibiotics) has been completed.
 ‘Deck-chair legs’ is erythema of the lower legs, sometimes with oedema and blistering, in the immobile. It tends to be mistakenly diagnosed as persistent or recurrent cellulitis.
‘Deck-chair legs’ is erythema of the lower legs, sometimes with oedema and blistering, in the immobile. It tends to be mistakenly diagnosed as persistent or recurrent cellulitis.
 A violent local erythema, rapidly darkening and blistering and recurring at the same site, suggests a fixed drug eruption.
A violent local erythema, rapidly darkening and blistering and recurring at the same site, suggests a fixed drug eruption.
 Erythema nodosum and multiforme may be caused by significant disease, including, very occasionally, malignancy. If the patient is generally unwell or has other significant symptoms, investigate urgently or refer.
Erythema nodosum and multiforme may be caused by significant disease, including, very occasionally, malignancy. If the patient is generally unwell or has other significant symptoms, investigate urgently or refer.
 Take a travel history: Lyme disease is endemic in forested areas. If not diagnosed and treated early, it can have significant complications.
Take a travel history: Lyme disease is endemic in forested areas. If not diagnosed and treated early, it can have significant complications.
 Erythema multiforme with blistering and ulceration of the mucous membranes is Stevens–Johnson syndrome. Though rare, it is a very serious illness requiring urgent hospital treatment.
Erythema multiforme with blistering and ulceration of the mucous membranes is Stevens–Johnson syndrome. Though rare, it is a very serious illness requiring urgent hospital treatment.
 Enquire about joint symptoms: many causes of erythema (e.g. erythema multiforme, butterfly rash, livedo reticularis) are linked to a connective tissue isorder.
Enquire about joint symptoms: many causes of erythema (e.g. erythema multiforme, butterfly rash, livedo reticularis) are linked to a connective tissue isorder.
 Remember to take a drug history, including over-the-counter medications. This may reveal the underlying cause in toxic erythema, erythema nodosum and multiforme, and phototoxicity.
Remember to take a drug history, including over-the-counter medications. This may reveal the underlying cause in toxic erythema, erythema nodosum and multiforme, and phototoxicity.
 Remember that parvovirus can cause serious problems in pregnancy – check serology in women with suggestive symptoms, or exposure to a case.
Remember that parvovirus can cause serious problems in pregnancy – check serology in women with suggestive symptoms, or exposure to a case.
MACULES
![]()
The GP overview
A macule is a flat, demarcated, abnormally coloured area of skin of any size. It may be red (e.g. drug eruption), dark red (e.g. purpura), brown (e.g. a flat mole) or white (e.g. pityriasis versicolor). Purpura is described elsewhere (see p. 400). There is some crossover between erythema (see p. 390) and red macules.
![]()
Differential diagnosis
COMMON
 drug reaction/allergy
drug reaction/allergy
 flat mole (junctional naevus)
flat mole (junctional naevus)
 non-specific viral exanthem
non-specific viral exanthem
 sun-induced freckles (including solar lentigines)
sun-induced freckles (including solar lentigines)
 chloasma
chloasma
OCCASIONAL
 measles and rubella
measles and rubella
 post-inflammatory hypo- or hyperpigmentation
post-inflammatory hypo- or hyperpigmentation
 café au lait spot (creamy brown) and Mongolian spot (brown or slate-grey)
café au lait spot (creamy brown) and Mongolian spot (brown or slate-grey)
 Berloque dermatitis (brown: chemical photosensitisation, e.g. bergamot oil)
Berloque dermatitis (brown: chemical photosensitisation, e.g. bergamot oil)
 depigmentation: vitiligo, pityriasis versicolor, pityriasis alba
depigmentation: vitiligo, pityriasis versicolor, pityriasis alba
RARE
 infections: macular syphilide, tuberculoid leprosy, typhoid (rose spots in 40%)
infections: macular syphilide, tuberculoid leprosy, typhoid (rose spots in 40%)
 Albright’s syndrome
Albright’s syndrome
 neurofibromatosis (associated with more than six café au lait spots)
neurofibromatosis (associated with more than six café au lait spots)
 pathological freckles: Hutchinson’s freckle, Peutz–Jeghers syndrome
pathological freckles: Hutchinson’s freckle, Peutz–Jeghers syndrome
 naevus anaemicus (permanent vasoconstriction due to neurovascular abnormality)
naevus anaemicus (permanent vasoconstriction due to neurovascular abnormality)
![]()
Ready reckoner

![]()
Possible investigations
There are very few relevant investigations to consider and they would be required only exceptionally, as the diagnosis is usually clinical: skin scrapings for mycology or fluorescence under Wood’s light may help in the diagnosis of pityriasis versicolor; acute and convalescent serum samples may confirm rubella; serology for syphilis may be appropriate with an unusual macular rash; and very occasionally, a skin biopsy may be required to clinch an obscure diagnosis.
TOP TIPS
 A drug eruption can take 2 weeks to appear from the time of the first dose – so don’t be misled by the fact that a course of antibiotics may have been completed some days before the related drug rash develops.
A drug eruption can take 2 weeks to appear from the time of the first dose – so don’t be misled by the fact that a course of antibiotics may have been completed some days before the related drug rash develops.
 Pityriasis versicolor may be misdiagnosed as vitiligo. If in doubt, take scrapings for mycology or examine under Wood’s light.
Pityriasis versicolor may be misdiagnosed as vitiligo. If in doubt, take scrapings for mycology or examine under Wood’s light.
 Odd lines of hyperpigmentation on the sides of the neck are likely to be Berloque dermatitis – a photosensitive rash caused by oil of bergamot, present in perfumes.
Odd lines of hyperpigmentation on the sides of the neck are likely to be Berloque dermatitis – a photosensitive rash caused by oil of bergamot, present in perfumes.

 Hutchinson’s freckle is a giant, variegated freckle, seen in elderly sun-exposed skin. There is a high risk of malignant change, so refer.
Hutchinson’s freckle is a giant, variegated freckle, seen in elderly sun-exposed skin. There is a high risk of malignant change, so refer.
 Rubella is rare, but may become commoner as a result of media coverage of ‘immunisation scares’. Establish whether or not a young woman presenting with a rubella-type rash is pregnant – if she is, confirm her rubella status.
Rubella is rare, but may become commoner as a result of media coverage of ‘immunisation scares’. Establish whether or not a young woman presenting with a rubella-type rash is pregnant – if she is, confirm her rubella status.
 A child with very many freckles on and around the lips may have Peutz–Jeghers syndrome. This is associated with small bowel polyposis.
A child with very many freckles on and around the lips may have Peutz–Jeghers syndrome. This is associated with small bowel polyposis.
 Vitiligo tends to have a poor prognosis in Caucasians, especially if it is widespread and affecting lips and extremities.
Vitiligo tends to have a poor prognosis in Caucasians, especially if it is widespread and affecting lips and extremities.
NODULES
![]()
The GP overview
Skin nodules are larger than papules – more than 5 mm diameter. However, their depth is more significant clinically than their width. Some are free within the dermis; others are fixed to skin above or subcutaneous tissue below. The causes are various; the patient is usually concerned about the cosmetic appearance or malignant potential.
![]()
Differential diagnosis
COMMON
 sebaceous cyst
sebaceous cyst
 lipoma
lipoma
 basal cell carcinoma (BCC)
basal cell carcinoma (BCC)
 warts
warts
 xanthoma
xanthoma
OCCASIONAL
 dermatofibroma (histiocytoma)
dermatofibroma (histiocytoma)
 squamous cell carcinoma
squamous cell carcinoma
 nodulocystic acne
nodulocystic acne
 kerato-acanthoma
kerato-acanthoma
 gouty tophi
gouty tophi
 chondrodermatitis nodularis chronica helicis
chondrodermatitis nodularis chronica helicis
 rheumatoid nodules and Heberden’s nodes
rheumatoid nodules and Heberden’s nodes
 pyogenic granuloma
pyogenic granuloma
RARE
 malignant melanoma (becoming more common in the UK)
malignant melanoma (becoming more common in the UK)
 vasculitic: erythema nodosum, nodular vasculitis, polyarteritis nodosa
vasculitic: erythema nodosum, nodular vasculitis, polyarteritis nodosa
 atypical infections (e.g. leprosy, treponema, lupus vulgaris, fish tank and swimming pool granuloma, actinomycosis)
atypical infections (e.g. leprosy, treponema, lupus vulgaris, fish tank and swimming pool granuloma, actinomycosis)
 lymphoma and metastatic secondary carcinoma
lymphoma and metastatic secondary carcinoma
 sarcoidosis
sarcoidosis
 pretibial myxoedema
pretibial myxoedema
![]()
Ready reckoner

![]()
Possible investigations
LIKELY: none (skin biopsy or cytology if doubt about the lesion or clinical diagnosis of possible carcinoma).
POSSIBLE: lipid profile, FBC, ESR/CRP, urate, rheumatoid factor, urinalysis.
SMALL PRINT: TFT, Kveim test, further investigations guided by clinical picture (see below).
 Excision biopsy is the definitive investigation for achieving a diagnosis; cytology from skin scrapings can be used to diagnose BCC.
Excision biopsy is the definitive investigation for achieving a diagnosis; cytology from skin scrapings can be used to diagnose BCC.
 Lipid profile: xanthomata require a full lipid profile to define the underlying hyperlipidaemia.
Lipid profile: xanthomata require a full lipid profile to define the underlying hyperlipidaemia.
 Urinalysis: if suspect inflammatory or vasculitic skin lumps, as may reveal proteinuria if associated with systemic and renal disorders.
Urinalysis: if suspect inflammatory or vasculitic skin lumps, as may reveal proteinuria if associated with systemic and renal disorders.
 FBC and ESR/CRP: ESR/CRP raised in inflammatory disorders and malignancy; may also reveal anaemia of chronic disease or malignancy (including lymphoma).
FBC and ESR/CRP: ESR/CRP raised in inflammatory disorders and malignancy; may also reveal anaemia of chronic disease or malignancy (including lymphoma).
 Check urate if gouty tophi are clinically likely.
Check urate if gouty tophi are clinically likely.
 Rheumatoid factor: nodules are usually associated with positive rheumatoid factor.
Rheumatoid factor: nodules are usually associated with positive rheumatoid factor.
 TFT: to diagnose Graves’s disease with pretibial myxoedema.
TFT: to diagnose Graves’s disease with pretibial myxoedema.
 Kveim test: may contribute to a diagnosis of sarcoidosis.
Kveim test: may contribute to a diagnosis of sarcoidosis.
 Further investigations according to clinical picture: some lesions, such as erythema nodosum, may require further investigation to establish the underlying cause; histological confirmation of skin secondaries may similarly require further assessment, although the overall condition of the patient may mean this is a futile exercise.
Further investigations according to clinical picture: some lesions, such as erythema nodosum, may require further investigation to establish the underlying cause; histological confirmation of skin secondaries may similarly require further assessment, although the overall condition of the patient may mean this is a futile exercise.
TOP TIPS
 Look at the lesion under the magnifying glass – this may reveal suspicious signs such as ulceration or a rolled, pearly edge.
Look at the lesion under the magnifying glass – this may reveal suspicious signs such as ulceration or a rolled, pearly edge.
 In uncertain cases which do not require urgent attention, record your findings carefully (including precise dimensions) and review in a month or two.
In uncertain cases which do not require urgent attention, record your findings carefully (including precise dimensions) and review in a month or two.
 Stoical patients may underestimate the significance of a suspicious lesion, particularly if you discover it during a routine examination – if you are referring them for biopsy, impress upon them the need to attend their appointment.
Stoical patients may underestimate the significance of a suspicious lesion, particularly if you discover it during a routine examination – if you are referring them for biopsy, impress upon them the need to attend their appointment.
 Establish the patient’s concern, which will usually centre on worries about cosmetic appearance or cancer. This will result in a more functional consultation and a more satisfied patient.
Establish the patient’s concern, which will usually centre on worries about cosmetic appearance or cancer. This will result in a more functional consultation and a more satisfied patient.

 Night sweats and itching with skin nodules raises the suspicion of lymphoma. Examine lymph nodes, liver and spleen carefully.
Night sweats and itching with skin nodules raises the suspicion of lymphoma. Examine lymph nodes, liver and spleen carefully.
 The elderly patient complaining of a lesion in a sun-exposed area which ‘just won’t heal’ may well have a squamous or basal cell carcinoma.
The elderly patient complaining of a lesion in a sun-exposed area which ‘just won’t heal’ may well have a squamous or basal cell carcinoma.
 The appearance of a nodule in a mole is highly significant and requires referral.
The appearance of a nodule in a mole is highly significant and requires referral.
 A patient with nodulocystic acne requires referral to a dermatologist for possible treatment with 13-cis-retinoic acid.
A patient with nodulocystic acne requires referral to a dermatologist for possible treatment with 13-cis-retinoic acid.
 The unwell middle-aged or elderly patient who develops bizarre and widespread skin nodules over a period of a few weeks probably has an underlying carcinoma.
The unwell middle-aged or elderly patient who develops bizarre and widespread skin nodules over a period of a few weeks probably has an underlying carcinoma.
PAPULES
![]()
The GP overview
Papules are solid, circumscribed skin elevations up to 5 mm in diameter. If they are larger, they are called nodules – these are dealt with elsewhere (see p. 395). (Clearly, many nodules start life as a papule; to avoid confusion, if they are generally ‘nodular’ by the time they present to the GP, then they are dealt with in that section, and not repeated here.) They are usually round but the shape, and the colour, may vary. They may be transitional lesions, e.g. becoming vesicular, or about to ulcerate.
NOTE: there are more causes of papules than can be listed here. This is a sensible selection.
![]()
Differential diagnosis
COMMON
 acne
acne
 scabies
scabies
 viral wart and molluscum contagiosum
viral wart and molluscum contagiosum
 Campbell de Morgan spot
Campbell de Morgan spot
 skin tag
skin tag
OCCASIONAL
 viral illness
viral illness
 milia
milia
 insect bites
insect bites
 early seborrhoeic wart
early seborrhoeic wart
 xanthomata
xanthomata
 guttate psoriasis
guttate psoriasis
 pityriasis lichenoides chronica, lichen planus
pityriasis lichenoides chronica, lichen planus
 prickly heat
prickly heat
 keratosis pilaris
keratosis pilaris
RARE
 malignant melanoma, early basal cell carcinoma, Kaposi’s sarcoma
malignant melanoma, early basal cell carcinoma, Kaposi’s sarcoma
 Darier’s disease
Darier’s disease
 acanthosis nigricans
acanthosis nigricans
 pseudoxanthoma elasticum
pseudoxanthoma elasticum
 tuberous sclerosis
tuberous sclerosis
![]()
Ready reckoner
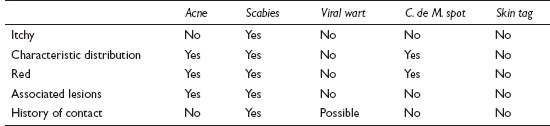
![]()
Possible investigations
In practice, very few investigations are needed with this presentation: a lipid screen is required in the presence of xanthomata; genital warts require referral for screening for other STDs; thorough investigation may be needed in the very rare case where underlying malignancy is possible (e.g. acanthosis nigricans); and obscure rashes or solitary papules may occasionally require excision biopsy for a definitive diagnosis.
TOP TIPS
 Bear in mind that skin cancer is usually uppermost in the patient’s mind, especially in subacute or chronic cases – so provide appropriate reassurance.
Bear in mind that skin cancer is usually uppermost in the patient’s mind, especially in subacute or chronic cases – so provide appropriate reassurance.
 In obscure solitary lesions, record clinical findings carefully and arrange to review in due course.
In obscure solitary lesions, record clinical findings carefully and arrange to review in due course.
 Itchy, asymmetrical grouped papules are likely to be insect bites, although the patient may take some convincing!
Itchy, asymmetrical grouped papules are likely to be insect bites, although the patient may take some convincing!

 An enlarging dark blue or blue-black papule may be a malignant melanoma, blue naevus or Kaposi’s sarcoma. Refer for urgent opinion.
An enlarging dark blue or blue-black papule may be a malignant melanoma, blue naevus or Kaposi’s sarcoma. Refer for urgent opinion.
 Brown, skin-coloured papules crowded around the nose of a child may be tuberous sclerosis. This can be associated with serious systemic pathology so refer for expert opinion.
Brown, skin-coloured papules crowded around the nose of a child may be tuberous sclerosis. This can be associated with serious systemic pathology so refer for expert opinion.
 An intensely itchy papular rash which is worse at night and has no other obvious cause is likely to be scabies, even if scabetic burrows are not evident – treat on suspicion.
An intensely itchy papular rash which is worse at night and has no other obvious cause is likely to be scabies, even if scabetic burrows are not evident – treat on suspicion.
PURPURA AND PETECHIAE
![]()
The GP overview
Purpura are reddish-purple lesions which do not blanch with pressure. When less than 1 cm in diameter, they are called petechiae; if larger, they are known as ecchymoses. The problem often presents as ‘bruising easily’ – a common ‘while I’m here’ complaint in primary care. Most cases are normal, with causative minor trauma simply being forgotten or unnoticed.
![]()
Differential diagnosis
COMMON
 trauma
trauma
 senile purpura
senile purpura
 liver disease (especially alcoholic cirrhosis)
liver disease (especially alcoholic cirrhosis)
 increased intravascular pressure, e.g. coughing, vomiting, gravitational
increased intravascular pressure, e.g. coughing, vomiting, gravitational
 drugs, e.g. steroids, warfarin, aspirin
drugs, e.g. steroids, warfarin, aspirin
OCCASIONAL
 vasculitis, e.g. Henoch–Schönlein purpura, connective tissue disorders
vasculitis, e.g. Henoch–Schönlein purpura, connective tissue disorders
 thrombocytopenia, e.g. idiopathic thrombocytopenia purpura (ITP), bone marrow damage (e.g. lymphoma, leukaemia, cytotoxics), aplastic anaemia
thrombocytopenia, e.g. idiopathic thrombocytopenia purpura (ITP), bone marrow damage (e.g. lymphoma, leukaemia, cytotoxics), aplastic anaemia
 renal failure
renal failure
 infective endocarditis
infective endocarditis
RARE
 paraproteinaemias, e.g. cryoglobulinaemia
paraproteinaemias, e.g. cryoglobulinaemia
 inherited clotting disorders, e.g. haemophilia, Christmas disease, von Willebrand’s disease
inherited clotting disorders, e.g. haemophilia, Christmas disease, von Willebrand’s disease
 infections, e.g. meningococcal septicaemia, Rocky Mountain spotted fever
infections, e.g. meningococcal septicaemia, Rocky Mountain spotted fever
 vitamin C and K deficiency
vitamin C and K deficiency
 disseminated intravascular coagulation (DIC)
disseminated intravascular coagulation (DIC)
 congenital vessel wall abnormalities, e.g. Ehlers–Danlos syndrome
congenital vessel wall abnormalities, e.g. Ehlers–Danlos syndrome
![]()
Ready reckoner
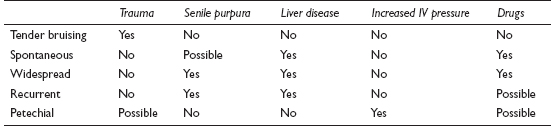
![]()
Possible investigations
LIKELY: FBC, ESR/CRP, INR (if on warfarin).
POSSIBLE: LFT, U&E, coagulation screen, plasma electrophoresis.
SMALL PRINT: autoimmune testing, further hospital investigations (see below).
 FBC, ESR/CRP: FBC may reveal thrombocytopenia or evidence of blood dyscrasia. ESR/CRP and WCC may be raised in blood dyscrasia, connective tissue disorder and infection.
FBC, ESR/CRP: FBC may reveal thrombocytopenia or evidence of blood dyscrasia. ESR/CRP and WCC may be raised in blood dyscrasia, connective tissue disorder and infection.
 LFT, U&E: for underlying liver or renal disease.
LFT, U&E: for underlying liver or renal disease.
 INR: if on warfarin.
INR: if on warfarin.
 Autoimmune testing: if possible connective tissue disease causing vasculitis.
Autoimmune testing: if possible connective tissue disease causing vasculitis.
 Coagulation screen: to test haemostatic function, e.g. bleeding time, prothrombin time, activated partial thromboplastin time.
Coagulation screen: to test haemostatic function, e.g. bleeding time, prothrombin time, activated partial thromboplastin time.
 Plasma electrophoresis: for hypergammaglobulinaemia, paraproteinaemia and cryoglobulinaemia.
Plasma electrophoresis: for hypergammaglobulinaemia, paraproteinaemia and cryoglobulinaemia.
 Further investigations (usually secondary care): to investigate underlying cause, e.g. skin biopsy to confirm vasculitis, bone marrow biopsy if possible marrow infiltrate.
Further investigations (usually secondary care): to investigate underlying cause, e.g. skin biopsy to confirm vasculitis, bone marrow biopsy if possible marrow infiltrate.
TOP TIPS
 Multiple bruises of varying ages on the legs of young children who are otherwise well and have no other stigmata of clotting disorder or abuse are likely to be non-pathological.
Multiple bruises of varying ages on the legs of young children who are otherwise well and have no other stigmata of clotting disorder or abuse are likely to be non-pathological.
 Senile purpura should be easy to diagnose from the history and examination. Reassurance, rather than investigation, is required.
Senile purpura should be easy to diagnose from the history and examination. Reassurance, rather than investigation, is required.
 A few petechiae on or around the eyelids of a well child can be caused by vigorous coughing or vomiting. If the history is clear, explain the cause to the parents – but emphasise that the appearance of an identical rash elsewhere requires urgent attention.
A few petechiae on or around the eyelids of a well child can be caused by vigorous coughing or vomiting. If the history is clear, explain the cause to the parents – but emphasise that the appearance of an identical rash elsewhere requires urgent attention.
 The distribution of purpura can give useful clues to the diagnosis. On the legs, platelet disorders, paraproteinaemias, Henoch–Schönlein purpura or meningococcal septicaemia are likely; lesions on the fingers and toes indicate vasculitis; and senile and steroid purpura tend to affect the back of the hands and arms.
The distribution of purpura can give useful clues to the diagnosis. On the legs, platelet disorders, paraproteinaemias, Henoch–Schönlein purpura or meningococcal septicaemia are likely; lesions on the fingers and toes indicate vasculitis; and senile and steroid purpura tend to affect the back of the hands and arms.
 Purpura caused by vasculitis tend to be raised palpably above the skin.
Purpura caused by vasculitis tend to be raised palpably above the skin.
 Remember that the rash of meningococcal septicaemia can appear before a child is obviously systemically unwell. If there is any suspicion that this might be the diagnosis, give parenteral penicillin and admit immediately.
Remember that the rash of meningococcal septicaemia can appear before a child is obviously systemically unwell. If there is any suspicion that this might be the diagnosis, give parenteral penicillin and admit immediately.
 The absence of a family history does not exclude a significant inherited bleeding disorder: these disorders can arise spontaneously.
The absence of a family history does not exclude a significant inherited bleeding disorder: these disorders can arise spontaneously.
 Take very seriously the pale patient with purpura: a bone marrow problem is likely. Arrange an urgent FBC or admit.
Take very seriously the pale patient with purpura: a bone marrow problem is likely. Arrange an urgent FBC or admit.
 Always do a full surface examination of a child with bruising, not forgetting the anogenital area. Keep non-accidental injury in mind.
Always do a full surface examination of a child with bruising, not forgetting the anogenital area. Keep non-accidental injury in mind.
 Never give an IM injection if a serious bleeding disorder is suspected.
Never give an IM injection if a serious bleeding disorder is suspected.
PUSTULES
![]()
The GP overview
Pustules are raised lesions less than 0.5 cm in diameter containing a yellow fluid. They signify infection to most people, and will often present in an urgent appointment, as they are likely to have appeared suddenly. Patients will often expect antibiotic treatment. This will not always be necessary, so be prepared to offer a clear explanation and an appropriate alternative.
![]()
Differential diagnosis
COMMON
 impetigo
impetigo
 other staphylococcal infections, e.g. early boils, folliculitis, sycosis barbae
other staphylococcal infections, e.g. early boils, folliculitis, sycosis barbae
 herpes simplex and zoster
herpes simplex and zoster
 acne vulgaris
acne vulgaris
 rosacea
rosacea
OCCASIONAL
 perioral dermatitis
perioral dermatitis
 hidradenitis suppurativa (axillae and groins)
hidradenitis suppurativa (axillae and groins)
 candidiasis (satellite vesicopustules around moist eroded patch)
candidiasis (satellite vesicopustules around moist eroded patch)
 pustular psoriasis (palmar and plantar commoner than generalised pustular psoriasis of von Zumbusch)
pustular psoriasis (palmar and plantar commoner than generalised pustular psoriasis of von Zumbusch)
RARE
 dermatitis herpetiformis
dermatitis herpetiformis
 Behçet’s syndrome
Behçet’s syndrome
 viral: cowpox and orf (Note: chickenpox is vesicular, not pustular)
viral: cowpox and orf (Note: chickenpox is vesicular, not pustular)
 hot tub folliculitis (superficial Pseudomonas infection)
hot tub folliculitis (superficial Pseudomonas infection)
 drug induced
drug induced
![]()
Ready reckoner

![]()
Possible investigations
There are very few investigations likely to prove useful or necessary in primary care. The presence of widespread or recurrent candidal or staphylococcal lesions might necessitate a urinalysis or blood sugar to exclude diabetes; a swab of pus may help confirm a clinically suspected infective agent; and in very obscure cases, a skin biopsy might prove helpful.
TOP TIPS
 Take time to explain to the patient the nature of the problem in recurrent staphylococcal infections. Exclude diabetes, check carrier sites and reassure that the patient’s ‘hygiene’ is not in question. A prolonged course of antibiotics may be helpful.
Take time to explain to the patient the nature of the problem in recurrent staphylococcal infections. Exclude diabetes, check carrier sites and reassure that the patient’s ‘hygiene’ is not in question. A prolonged course of antibiotics may be helpful.
 Check self-treatment in rosacea and perioral dermatitis. Treatment with OTC topical steroids will exacerbate the problem. Warn the patient that the condition may worsen before it improves on withdrawal of this inappropriate treatment.
Check self-treatment in rosacea and perioral dermatitis. Treatment with OTC topical steroids will exacerbate the problem. Warn the patient that the condition may worsen before it improves on withdrawal of this inappropriate treatment.
 Papules and pustules around the mouth and eyes, often with a halo of pallor around the lip margin, are caused by perioral dermatitis. Treat with antibiotics, not topical steroids.
Papules and pustules around the mouth and eyes, often with a halo of pallor around the lip margin, are caused by perioral dermatitis. Treat with antibiotics, not topical steroids.

 Widespread, severe and recurrent staphylococcal lesions suggest diabetes or possible immunosuppression.
Widespread, severe and recurrent staphylococcal lesions suggest diabetes or possible immunosuppression.
 Localised pustular psoriasis can be very resistant to standard treatments, so have a low threshold for referral. The very rare generalised form can make the patient dangerously ill: admit urgently.
Localised pustular psoriasis can be very resistant to standard treatments, so have a low threshold for referral. The very rare generalised form can make the patient dangerously ill: admit urgently.
 Remember that herpes simplex or zoster infections in the immunocompromised can become disseminated and severe.
Remember that herpes simplex or zoster infections in the immunocompromised can become disseminated and severe.
 Ocular problems in rosacea can be complicated and troublesome: refer to an ophthalmologist.
Ocular problems in rosacea can be complicated and troublesome: refer to an ophthalmologist.
SCALES AND PLAQUES
![]()
The GP overview
Skin scales represent an abnormally fast piling up of keratinised epithelium. Scales and plaques are common at all ages and have a variety of causes. The presentation will centre on cosmetic appearance, itching, fears about serious disease or a combination of these.
![]()
Differential diagnosis
COMMON
 psoriasis
psoriasis
 eczema (in all its various forms)
eczema (in all its various forms)
 fungal infections (e.g. scalp, body, feet)
fungal infections (e.g. scalp, body, feet)
 seborrhoeic dermatitis
seborrhoeic dermatitis
 seborrhoeic keratosis
seborrhoeic keratosis
OCCASIONAL
 lichen simplex
lichen simplex
 lichen planus (usually scaly only on legs)
lichen planus (usually scaly only on legs)
 solar keratosis
solar keratosis
 pityriasis versicolor and rosea
pityriasis versicolor and rosea
 juvenile plantar dermatosis
juvenile plantar dermatosis
 guttate psoriasis (scaly papules)
guttate psoriasis (scaly papules)
RARE
 malignancy: Bowen’s disease and mycosis fungoides (cutaneous T-cell lymphoma)
malignancy: Bowen’s disease and mycosis fungoides (cutaneous T-cell lymphoma)
 drug induced (e.g. β-blockers and carbamazepine)
drug induced (e.g. β-blockers and carbamazepine)
 ichthyosis (various forms)
ichthyosis (various forms)
 keratoderma blenorrhagica (part of Reiter’s syndrome)
keratoderma blenorrhagica (part of Reiter’s syndrome)
 pityriasis lichenoides chronica
pityriasis lichenoides chronica
 secondary syphilis
secondary syphilis
![]()
Ready reckoner
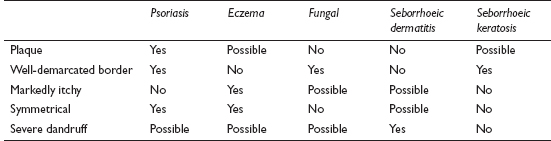
![]()
Possible investigations
LIKELY: none.
POSSIBLE: Wood’s light, skin scrapings/hair samples, patch testing.
SMALL PRINT: skin biopsy, syphilis serology, FBC, ESR/CRP, fasting glucose or HbA1c.
 Green fluorescence under UV (Wood’s) light is diagnostic of microsporum fungal infection.
Green fluorescence under UV (Wood’s) light is diagnostic of microsporum fungal infection.
 Skin scrapings and hair samples for mycology: will help differentiate fungal infections from similar rashes.
Skin scrapings and hair samples for mycology: will help differentiate fungal infections from similar rashes.
 Skin biopsy: may be the only way to achieve a firm diagnosis in obscure rashes, and is essential if malignancy suspected.
Skin biopsy: may be the only way to achieve a firm diagnosis in obscure rashes, and is essential if malignancy suspected.
 Patch testing: to establish the likely allergen in allergic contact eczema.
Patch testing: to establish the likely allergen in allergic contact eczema.
 Syphilis serology: if justified by clinical features or obscure pattern.
Syphilis serology: if justified by clinical features or obscure pattern.
 FBC and ESR/CRP: may suggest significant underlying disease (e.g. T-cell lymphoma); ESR/CRP also elevated in Reiter’s disease.
FBC and ESR/CRP: may suggest significant underlying disease (e.g. T-cell lymphoma); ESR/CRP also elevated in Reiter’s disease.
 Fasting glucose or HbA1c: check for diabetes in recurrent fungal infections.
Fasting glucose or HbA1c: check for diabetes in recurrent fungal infections.
TOP TIPS
 To help distinguish between fungal and eczematous rashes, look at the symmetry and edges of the lesions. Fungal rashes are usually asymmetrical with a scaly, raised edge.
To help distinguish between fungal and eczematous rashes, look at the symmetry and edges of the lesions. Fungal rashes are usually asymmetrical with a scaly, raised edge.
 In the presence of a fungal rash, look for infection elsewhere (e.g. groins and feet) and treat both areas, otherwise the problem is likely to recur.
In the presence of a fungal rash, look for infection elsewhere (e.g. groins and feet) and treat both areas, otherwise the problem is likely to recur.
 In uncertain cases, explain to the patient that the real diagnosis may only become apparent as the rash develops (the typical example being the herald patch of pityriasis rosea looking like initially tinea corporis) – invite the patient to return for reassessment if your initial treatment proves unsuccessful.
In uncertain cases, explain to the patient that the real diagnosis may only become apparent as the rash develops (the typical example being the herald patch of pityriasis rosea looking like initially tinea corporis) – invite the patient to return for reassessment if your initial treatment proves unsuccessful.
 A symmetrical, glazed, scaly and fissured rash on the soles of a trainer-loving child or adolescent is juvenile plantar dermatosis.
A symmetrical, glazed, scaly and fissured rash on the soles of a trainer-loving child or adolescent is juvenile plantar dermatosis.
 Eight per cent of people with psoriasis will have arthropathy, which is usually also associated with nail changes. Check the nails and ask about joint symptoms in patients with psoriasis.
Eight per cent of people with psoriasis will have arthropathy, which is usually also associated with nail changes. Check the nails and ask about joint symptoms in patients with psoriasis.
 Erythroderma – universal redness and scaling caused, rarely, by psoriasis, eczema, mycosis fungoides and drug eruptions – renders the patient systemically unwell. Urgent inpatient treatment is required.
Erythroderma – universal redness and scaling caused, rarely, by psoriasis, eczema, mycosis fungoides and drug eruptions – renders the patient systemically unwell. Urgent inpatient treatment is required.
 A solitary, well-defined, slowly growing scaly plaque on the face, hands or legs of the middle-aged or elderly patient is probably Bowen’s disease – but it can easily be mistaken for an isolated patch of eczema or psoriasis.
A solitary, well-defined, slowly growing scaly plaque on the face, hands or legs of the middle-aged or elderly patient is probably Bowen’s disease – but it can easily be mistaken for an isolated patch of eczema or psoriasis.
 If a pityriasis rosea-like rash extends to the palms and soles, with fever, malaise, sore throat and lymphadenopathy, consider secondary syphilis.
If a pityriasis rosea-like rash extends to the palms and soles, with fever, malaise, sore throat and lymphadenopathy, consider secondary syphilis.