Thou shalt make me hear of joy and gladness; that the bones which Thou hast broken may rejoice.
Book of Psalms LI, verse 10
Hundreds of patients have visited my practice with signs and symptoms of CFS/ME. All of them share common structural and physical signs, while complaining of strikingly similar symptoms. This cannot be dismissed purely as coincidence.
My theory for the diagnosis and treatment of CFS/ME started with a patient: this case was the first and perhaps the most dramatic of all the CFS/ME patients I have treated. In 1989 an executive, who shall be referred to as Mr E, walked into my city centre practice, in Manchester, where I ran a clinic specialising in treating sports injuries. He had been a top cyclist, racing for one of the premier teams in the Northwest of England.
He had suffered from a recurring, low back pain, which, after examination, I had diagnosed to be a strain of the pelvic joints. While treating his pelvis, I noted that his dorsal spine was particularly restricted. I enquired whether or not he had any problems in his upper back, and he acknowledged that for years, during his cycling, he had experienced a dull ache across his shoulders and at the top of his back. This in itself was nothing significant, as it was very common to find cyclists with pelvic problems and a stiff and bent dorsal spine. What was interesting was the fact that, for the past seven years, Mr E had been diagnosed as suffering from CFS/ME.
Mr E complained of tingling in both hands and a ‘muzzy’ feeling in his head. He suffered general fatigue and an ache in his knees, as well as the pain in his back and shoulders. He had been forced to stop racing since the onset of the disorder.
This patient was one of many who came to me after being diagnosed by their doctor, or specialist, as suffering from CFS/ME. At that time, although I had helped other patients with CFS/ME, I had done no research into the disease, and I had no specific treatment programme for the disorder.
With only five treatments, Mr E’s back was better, but, most incredibly, the signs and symptoms of CFS/ME had drastically improved. He was symptom-free after a mere two months from the start of treatment. He still remains healthy and the last news I heard of him was that he had moved to Holland, cycling with the same power and zeal that he used to enjoy prior to his illness.
It was after helping this patient that I realised that there must be a relationship between the mechanical strain on the thoracic spine and CFS/ME. Although I had not set out to cure the fatigue signs and symptoms in this patient, I had done exactly that by improving the posture and movement in the upper back. My thoughts turned to the other CFS/ME patients that I had treated. The restriction of the dorsal spine was a common factor that could not be ignored.
Professional sportsmen, and people who are keen on sporting events, usually start participating in their discipline at an early age. These competitive individuals are more likely to suffer from developmental disorders commonly associated with overtaxing growing bones and joints.
One such disorder is osteochondritis. This is an inflammatory disorder of the bone and cartilage, which often affects an active, growing spine, and is a frequent cause of backache in adolescents. The disorder usually leaves a slight permanent deformity in the spine, especially in the thoracic area, with an associated restriction of the affected region. This stiffened area may be asymptomatic for the rest of the person’s life, but it may lead to other mechanical problems of the back. This condition could eventually cause permanent irritation of the surrounding sympathetic nerves, and thus be a further reason for the high incidence of CFS/ME in active, sporty men and women.
I am now going to summarise my theory of the diagnosis and treatment of CFS/ME. If you don’t enjoy reading or, because of CFS/ME you are unable to concentrate on long texts, this one chapter is for you. If, after reading it, you wish to understand what CFS/ME is all about, the rest of the book is waiting to be read. I endeavour to keep the explanations as simple as possible in this first chapter.
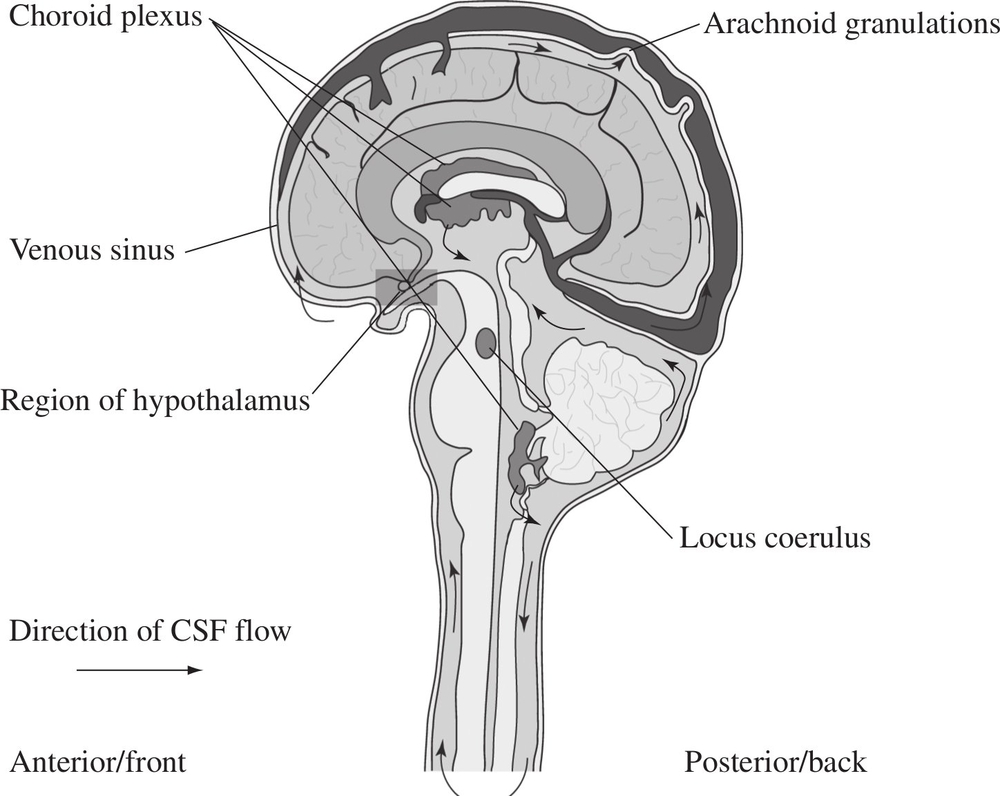
Figure 1. Flow of cerebrospinal fluid and the position of the hypothalamus.
The fluid’s journey is shown from its production at the choroid plexus around the brain and spinal cord with most of the CSF draining into the venous sinuses. Further drainage takes place via the lymphatics.
Fact 1: Fluid flow
A fluid flows around the brain and continues up and down the spinal cord: this is the cerebrospinal fluid. This fluid has many functions, for example, as a protective buffer to the central nervous system and for supplying nutrients to the brain. However, one function has been known about since the 1860s1 but has only received significant attention in recent years,2–15 and that is the drainage of poisons (toxins) out into the lymphatic system.
Fact 2: Getting the toxins out
The lymphatic system is an organization of tubes around the body that provides a drainage system secondary to the blood flow. Why does the body need a secondary system to cope with poisons or foreign bodies in the tissue? Are the veins not good enough? The answer in one important word is ‘size’. The blood system does process poisons and particles, but the trouble is that foreign material enters it via the walls of the microscopic blood vessels, known as the capillaries. Their walls resemble a fine mesh, which acts as a filter, thus allowing only small molecules to enter the bloodstream itself. This process is known as filtration. When the blood reaches the liver, detoxification takes place, cleansing the blood of its impurities. The capillary beds of lymphatic vessels, known as terminal lymphatics, take in any size of toxin, via a wall that resembles the gill of a fish, opening as wide as is necessary to engulf the foreign body. These large molecules of toxins often need breaking down before entering the blood stream: and so they begin the process of detoxification in the lymph nodes on the way to drainage points just below the collar bone into two large veins (the subclavian veins), with most of the body’s lymph draining into the left subclavian vein (see Fig. 2). Once the toxins have drained into the subclavian veins, they eventually find their way into the liver and, as is the case with normal circulatory toxins, are broken down by the liver16.
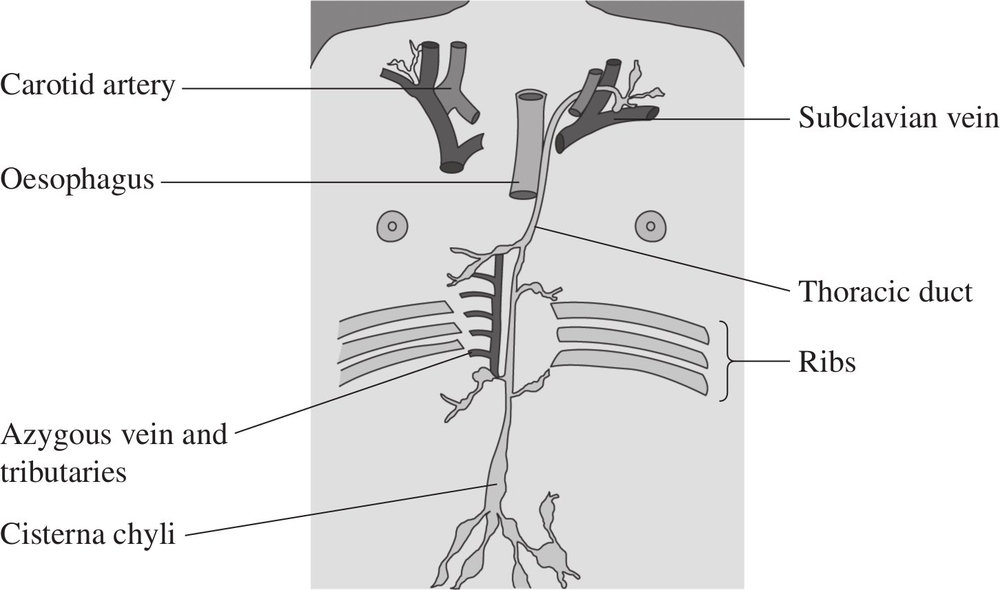
Figure 2. The thoracic duct (the central lymphatic drainage system into the blood).
Fact 3: The pumping mechanism
For a long time after it was discovered, the lymphatic system was thought not to have a pump of its own. Its flow was believed to depend on the massaging effect of the surrounding muscle and the blood vessels lying next to the lymphatics, akin to squeezing toothpaste up the tube. However, Professor John Kinmonth, a London chest surgeon, discovered in the 1960s that the main drainage of the lymphatics, the thoracic duct, has a pumping mechanism in its walls17,18,19 and that this is controlled by the sympathetic nervous system.20 If there is a disturbance of the sympathetic nervous system, the pump may push the lymph fluid in the wrong direction and lead to a further build-up of toxins in the body.
Fact 4: The sympathetic nervous system
The sympathetic nervous system is part of the autonomic nervous system, which deals with all the automatic functions of the body. The sympathetic nervous system is important in controlling blood flow and the normal functioning of all the organs of the body such as the heart, kidney, and bowel. We know it is vital for healthy lymphatic drainage. In CFS/ME sufferers the sympathetic nervous system will have been placed under stress for many years before the onset of the signs and symptoms of the illness. This stress may be of a physical nature due to postural strain or an old injury, it may be emotional, environmental such as pollution, or it may be due to stress on the immune system due to infection or allergy (Fig. 3).
The sympathetic nerves spread out from the thoracic spine to all parts of the body and are ultimately controlled by a small site in the brain, the hypothalamus (see Fig. 1), which also controls all the hormones of the body.
Fact 5: Biofeedback
The hypothalamus controls hormones by a process called biofeedback. This mechanism can be explained with the following example. If the sugar levels in the body are too low, that may be due to a rise in the hormone insulin, which is produced in the pancreas under control of the hypothalamus. Insulin, like other hormones, is a large protein molecule that travels through the blood and stimulates the breakdown of sugar. It passes from the blood into the hypothalamus, which will calculate if more or less insulin production is required and, accordingly, send a message to the pancreas to make the necessary adjustments.
The region of the hypothalamus is the only section of the brain that allows the transfer of large molecules into the brain from the blood. In all other parts of the brain there is a filter known as the blood-brain barrier, similar to the fine mesh in the small blood vessels mentioned earlier. The blood-brain barrier prevents toxins and other harmful material entering the brain’s cells from the blood. However, this barrier is naturally weakened at the hypothalamus to enable the biofeedback mechanism to work and allow the transfer of hormones. Unfortunately, this weakness means that large toxic molecules can invade the brain and wreak havoc on the normal functioning of the central nervous system.21–26

Figure 3. Long-term build-up of internal and external stress.
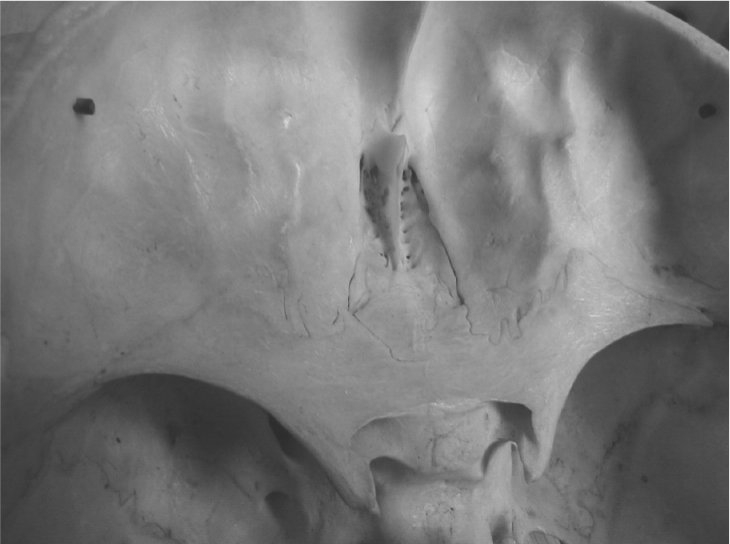
Figure 4. Superior view of the cribriform plate with observed perforations.
The perforations seen above allow the passage of blood vessels, nerves and cerebrospinal fluid from the cerebrum to the nasal sinuses situated directly below the ethmoid bone. This drainage problem appears to arise from a prior defect in the skull, usually in the frontal/nasal region due to either a congenital, hereditary or traumatic aetiology. This may be exacerbated by chronic sinusitis, leading to further congestion affecting the lymph channels in the mucous membranes of the nasal sinuses.
Fact 6: What goes wrong
The central nervous system, composed of the brain and the spinal cord, is the only region in the body that has no lymphatic system. The role of the lymphatics in the rest of the body is to capture and process large invading molecules: so what can the central nervous system do if attacked by large toxins? The cerebrospinal fluid (see Fact 1) drains toxins along minute gaps next to blood vessels through perforations in the skull, with the largest amount draining through a bony plate situated above the nose (known as the cribriform plate, Fig. 4).3,12,14,15 The toxins then drain into lymphatic vessels in the tissue around the nasal sinuses. There is further drainage down similar channels next to the optic, auditory and trigeminal nerves in the eye, ear and cheek respectively and down the spine and outward.4,5,7 The lymphatic vessels take the toxins away via the thoracic duct (see Fig. 2) into the blood and the liver where they are broken down.
Fact 7: Build-up of toxins
In CFS/ME it is these drainage pathways, both in the head and the spine, that are not working sufficiently, leading to a build-up of toxins within the central nervous system. The reasons for drainage problems can vary from patient to patient. It may be trauma to the head from an accident, it may be hereditary or due to a problem at birth. The spine may become out of alignment – especially in very active teenagers – which can lead to a disturbance in the normal drainage (Fig 5.). If the spine and brain are both affected, the increased toxicity will reduce hypothalamic function and thus will further affect sympathetic control of the central lymphatic vessel. This in turn pumps more toxins back into the tissues and the brain, which further affects sympathetic control. With this, a vicious circle (see Fig. 6) has started.27,28,29
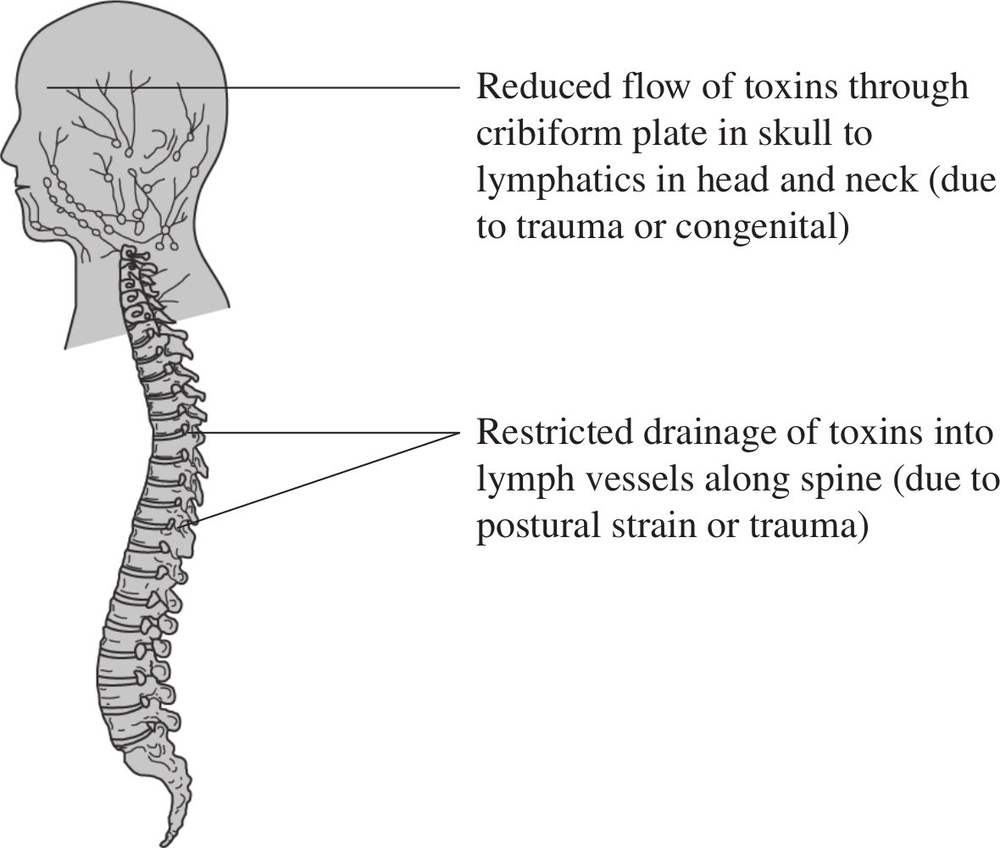
Figure 5. Restricted drainage of toxins from the central nervous system.

Figure 6. The downward spiral into CFS/ME.
Conclusion
CFS/ME is very much a structural disorder with clear and diagnosable physical signs, including disturbed spinal posture, swollen lymph vessels and specific tender points related to sympathetic nerve disturbance and backflow of lymphatic fluid. The fluid drainage from the brain to the lymphatics moves in a rhythm that can be palpated using cranial osteopathic techniques. A trained practitioner can feel a disturbance of the cranial rhythm in CFS/ME sufferers.29,30
The Perrin Technique helps drain the toxins away from the central nervous system and incorporates manual techniques that stimulate the healthy flow of lymphatic and cerebrospinal fluid and improve spinal mechanics. This in turn reduces the strain on the sympathetic nervous system, which aids a return to good health.
Notes
1. Scwalbe G. Die Arachnoidairaum ein Lymphraum und sein Zusammenhang mit den Perichorioidairaum. Zbl med Wiss Zentralblatt fur die medizinschen Wissenschaften. 1869; 7:465–467.
2. Kida S, Pantazis A, Weller RO. CSF Drains Directly from the Subarachnoid space into Nasal Lymphatics in the Rat. Anatomy, Histology and Immunological Significance. Neuropathology and Applied Neurobiology 1993; 19: 480–488.
3. Johnston M, Zakharov A, Papaiconomou C, Salmasi G, Armstrong D: Evidence of connections between cerebrospinal fluid and nasal lymphatic vessels in humans, non-human primates and other mammalian species. Cerebrospinal Fluid Research 2004; 1: 2.
4. Miura M, Kato S, Von Ludinghausen M. Lymphatic drainage of the cerebrospinal fluid from monkey spinal meninges with special reference to the distribution of epidural lymphatics. Arch Histol Cytol 1998; 61: 277–286.
5. Bozanovic Sosic R, Mollanji R, Johnston MG. Spinal and cranial contributions to total cerebrospinal fluid transport. American Journal of Physiology 2001; 281, 3–2: R909–R916.
6. Boulton M, Flessner M, Armstrong D, Hay J, Johnston M. Determination of volumetric cerebrospinal fluid absorption into extracranial lymphatics in sheep. American Journal of Physiology 1998; 274: 1 (2). R88–96.
7. Bradbury MWB, Cole DF. The role of the lymphatic system in drainage of cerebrospinal fluid and aqueous humour. Journal of Physiology 1980; 299: 353–365.
8. Mokri B, Aksamit AJ, Atkinson JL. Paradoxical postural headaches in cerebrospinal fluid leaks. Cephalalgia 2004; 24(10):883–7.
9. Czerniaswska A. Experimental investigations on the penetration of 198Au from nasal mucous membrane in to cerebrospinal fluids. Acta Otolaryngologica. 1970; 70: 58–61.
10. Silver, I, Li, ., Szalai, J, Johnston M. Relationship between intracranial pressure and cervical lymphatic pressure and flow rates in sheep. American Journal of Physiology 1999. 277,6–2:R1712–R1717.
11. Jones HC, Lopman BA. The relation between CSF pressure and ventricular dilatation in hydrocephalic HTx rats. European Journal of Pediatric Surgery. 1998, 8; S1: 55–58.
12. Cserr HF, Knopf PM. Cervical Lymphatics, the blood-brain barrier and immunoreactivity of the brain: a new view. Immunology Today 1992; 13: 507–512.
13. McComb JG, Davson H, Hyman S, Weiss MH. Cerebrospinal fluid drainage as influenced by ventricular pressure in the rabbit. Journal of Neurosurgery 1982; 56: 790–797.
14. Knopf PM, Cserr HF. Physiology and Immunology of lymphatic drainage of interstitial and cerebrospinal fluid from the brain. Neuropathology and applied Neurobiology 1995; 21: 175–180.
15. Koh L, Zakharov A, Johnston M. Integration of the subarachnoid space and lymphatics: Is it time to embrace a new concept of cerebrospinal fluid absorption? Cerebrospinal Fluid Research 2005, 2:6.
16. Bell GH, Emslie-Smith D, Paterson CR. 1980. Textbook of Physiology, 10th edition, Churchill Livingstone, Edinburgh, pp. 72 and 96.
17. Kinmonth JB. The Lymphatics, 2nd edition. Edward Arnold, London. pp 80. 1982.
18. Kinmonth JB. Some aspects of cardiovascular surgery. Journal of the. Royal College of Surgeons Edinburgh 1960; 5: 287–297.
19. Kinmonth JB. Sharpey-Schafer. Manometry of Human Thoracic Duct. Journal of Physiology 1959; 177: 41.
20. Browse NL. Response of lymphatics to sympathetic nerve stimulation. Journal of Physiology 1968; 19: 25.
21. Rogers S. Tired or Toxic. Syracuse, New York. Prestige Publishing 1990.
22. Lopachin RM, Aschner M. Glial-neuronal interactions: relevance to neurotoxic mechanisms. Toxicology and Applied Pharmacology 1993; 118: 141–158.
23. Iacono RF, Berria MI, Lascono EF. A triple staining procedure to evaluate phagocytic role of differentiated astrocytes. Journal of Neuroscience Methods 1991; 139: 225–230.
24. Morganti-Kossman MC, Kossman T, Wahl SM. Cytokines and Neuropathology. Trends in Pharmaceutical Sciences 1992; 13: 286–291.
25. Lindholm D, Castren E, Kiefer R, Zafra F, Thoenen H. Transforming growth factor-B1 in the rat brain; increase after injury and inhibition of astrocyte proliferation. Journal of Cell Biology 1992; 117: 395–400.
26. Sawada M, Suzumura A, Ohno K, Marunouchi T. Regulation of astrocyte proliferation by prostaglandin E2 and the a-subtype of protein kinase C. Brain Research 1993; 613: 67–73.
27. Perrin RN. Chronic fatigue syndrome: a review from the biomechanical perspective. British Osteopathic Journal 1993; 11: 15–23.
28. Perrin RN, Edwards J, Hartley P. An evaluation of the effectiveness of osteopathic treatment on symptoms associated with Myalgic Encephalomyelitis. A preliminary report. Journal of Medical Engineering and Technology 1998; 22, 1: 1–13.
29. Perrin RN. The Involvement of Cerebrospinal Fluid and Lymphatic Drainage in Chronic Fatigue Syndrome/ME (PhD Thesis). University of Salford, UK. 2005.
30. Perrin RN. Lymphatic drainage of the neuraxis and the CRI: a hypothetical model. Journal of the American Osteopathic Association. In press (accepted Jan 2007).