The Physiology of Yoga
Although yoga is not a science, it can be studied. The principles of its function—how it has the effects it does have—can be understood. After all, fishing is not a science but we can investigate why it works and how to improve it, how to make it more effective. In fact, yoga’s traditional practice of stretching muscles and joints and remaining in positions for extended periods of time exploits powerful reflexes and produces a number of salutary effects. These nearly universal responses are as good a place as any to begin.
Reflexes
Three common reflexes are used in most of the hundreds of widely practiced yoga poses. The first two reflexes, a system of checks and balances, are almost always a part of yoga. You might have learned about them in high school.
Every muscle in the body has a pair of reflexes that govern its activity. Whenever a muscle is stretched, one reflex—the stretch or myotatic reflex—stimulates the muscle to contract; the other—the Golgi tendon reflex—inhibits muscular contraction in response to stretch. Both reflexes start from tiny sense organs within each muscle and tendon that relay information back to the spinal cord.
When the reflexes that promote or facilitate muscle contraction get triggered, the muscles pull back. They are the ones that respond when the doctor strikes the tendon just below your kneecap. That quick little stretch of the quadriceps muscle results in a tightening of the muscle, contracting it and raising your lower leg. These reflexes are initiated by sense organs, the intrafusal fibers, but these organs also have tiny muscles within them! This allows them to adjust how strongly they stimulate the contraction of large skeletal muscles.
Another set of sense organs in each muscle’s tendon—the Golgi tendon organs—inhibit muscle contraction. When there is a tug on a muscle, be it by the hand of a good friend, the swing of a tennis racket, gravity, or yoga, these sense organs contact the spinal and pontine motor centers in the brain to modulate down the tone and actual contraction of every one of the body’s muscles.1
One basic mechanism in many yoga postures—entering them slowly and holding them—utilizes the fact that the intrafusal (stimulating) fibers are dynamic. Their response is adjustable and proportional to the speed of the stretch. Since they adjust internally to tension, they generally respond less to slow movements and have their greatest influence early in the process of muscle stretching.2 Their influence fades fast, though, especially if the muscle just stays at its new length.3 The inhibitory Golgi tendon organs damp down muscle contraction with a force that is weaker than the positive contraction-producing stimulus of the intrafusal fibers. But they continue to exert the same amount of inhibitory influence, at their original strength, over long periods of time.4 After a while, their constant input outstrips the diminishing influence of the intrafusal fibers. This naturally tends to reduce a muscle’s contractile force as a yoga pose is held.

After a short time—less than two minutes—the muscle will become quiet and stretch more easily and less painfully. Any sustained muscle stretch will eventually bring about a relaxation response in any muscle.5 Naturally, any painful stimuli that appear during that same time period will have a contrary, unsettling, and excitatory effect.6 The yoga poses that have lasted over the centuries succeed in accomplishing sustained stretch and relaxation without undue antagonistic, painful, or arousing stimuli.
Speaking of antagonistic, a third reflex is also, albeit very generally, at work during yoga postures. Every skeletal muscle has an antagonist, or direct counterpart: one set of muscles clasps the hand, another opens it. In order for one group of muscles to create a bend at the elbow, the muscles that straighten it must relax. This phenomenon, the agonist-antagonist reflex, is coordinated in the central nervous system and is nearly ubiquitous in Iyengar and Anusara Yoga. If you care to stretch the hamstring muscles, proceed by tightening the quadriceps, and the hamstrings will miraculously relax.7
Tightening the quadriceps to straighten the leg at the knee will stretch the hamstring muscles and their golgi tendon organs too, and soon the hamstrings will relax and stretch more and more easily.
Overview
There are several advantages to relaxed and extended muscles in a comfortable and calm individual. In people with arthritis of any type, and really in anyone threatened with decreased range of motion, reducing resistance to motion is an obvious (and painless) means to increase that range. But when arthritis grossly reshapes, distorts, or tightens joints—when just stretching muscles will not do the trick—yoga will render the process of increasing mobility more pleasant and calming, and therefore easier to endure.
However, in the vast majority of joints with restricted motion, where a leathery resistance is felt at the endpoints of movement, the cause is not a deformed joint but constricted joint capsules, tightened ligaments, or muscle shortening. Yoga is the perfect “minimal medicine”in such situations. It is now time to analyze the joints and the most common conditions that come up in arthritis, and then demonstrate the actual remedies that yoga has to offer.
The largest joints in the body are the knees; the smallest are between the bones in the ear. But all moving joints, whether in the wrists, the spine, or the jaw, have the same parts: bones, with cartilage at their interfaces; ligaments that hold them together; and tendons that cross the joints, attaching muscles to the various bones in order to move them when they contract. But there’s more to it. All this is described and pictured in Chapter 1.
Osteoarthritis from a Medical Perspective
Osteoarthritis grows from mechanical defects in the surfaces of the joint cartilage and from irregular spawning of new cartilage by the underlying cartilage-making cells.8 This makes for an uneven distribution of pressures within the joints, and irregular force on the bones beneath the cartilage, which also slowly disrupts the bone substance beneath the joint’s cartilage. Subsequently there is further irregularity in the cartilage and yet further distortion of the bone beneath. This process occurs with normal wear and tear in all of us, but our genetic makeup, our activity, and the environment in which we live influence the effects on our joints.
Typically, the cartilage seems to suffer first. In the knee, for example, the normal space between the femur (thigh bone) and the tibia is a centimeter or more. But as time goes on, and at any rate by the mid-fifties, the inner part of most knee joints shows no more than seven or eight millimeters of separation. The medial meniscus, the cartilage that lies on the upper inner surface of the tibia, has begun to thin. Does this happen because the cells making cartilage, the chondrocytes, have slowed down? Or is there some intrinsic change in the quality of the collagen that the cells are producing? Is it just that pressures have, over the years, simply compressed all of the healthy elements together so that they take up less space? Does the underlying bone change on its own? Or are there individually unrecognizable traumas that cumulatively mount to destroy the original arrangement of blood vessels, the subsequent order of the chondrocytes in the cartilage itself, and the matrix of collagen and background fluids until they are no longer adapting to and cushioning the movements of the joint? Do age, strength, activity, hormones, nutrition, exposure to the sun, or even attitude figure into it?
The answer to all these questions is yes, but it is a qualified yes: Different genetic combinations and body types make some factors more important in one individual than in another, and variations in some of the factors change the impact of others. For example, if you do not have enough protein in your system, no amount of exercise will nourish the cartilage sufficiently. If you are hyperthyroid, your cartilage will grow beyond its normal confines. But a good deal of low-impact joint movement is bound to improve circulation and range of motion, almost no matter what.9
How Does Osteoarthritis Progress?
Cartilage has a unique type of collagen called type II collagen. It is made of a long, thin string of proteins (proteoglycans) with complex side-chain glycosaminoglycans attached. The arrangement resembles a bottle-washing brush, with a protein at the center and the glycosamino-glycans acting as bristles.
The glycosaminoglycans have negative charges which attract water molecules between them. When there is pressure on the joint, and consequently on the cartilage, the water molecules are reluctantly released, cushioning the pressure and giving a wonderful resilience to the cartilage.10 Changes in the molecular structure of the proteoglycans are thought to be the basic force in osteoarthritis.11 These changes accelerate the process of degeneration and impede repair at the surfaces of cartilage, and they might be involved in the unusual and restricting boney formations and ligamentous damage that are so often seen in degenerative arthritis throughout the body.12
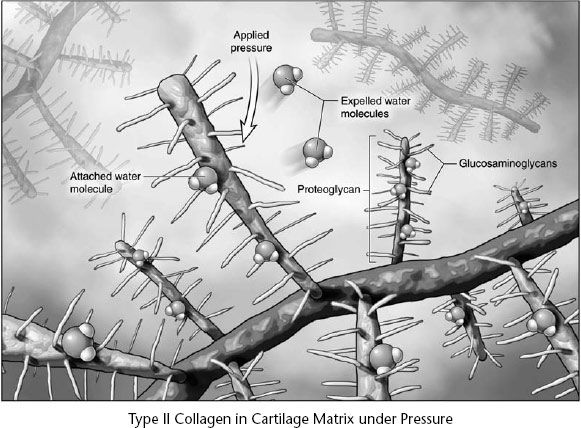
Figure 4. Proteins attract the water molecules between their side branches. The water resists as it is squeezed out under pressure. Once the pressure ends, the water returns, the proteins stiffen and expand again. The entire process makes the cartilage elastic and protects the joint.
Adult chondrocytes no longer multiply, but they do respond to damage, “eating”the degenerated cartilage and using the molecular building blocks to create new, healthy strands of it. The enzymes that help digest the old cartilage are more abundant where osteoarthritis is present.13 Metabolism in general is up. The processes of degeneration and repair are going on simultaneously, but over time the repair cannot keep up with the degeneration. Less elastic forms of cartilage appear, which increases the stresses on the bone below, causing microfractures. After the microfractures heal, the bone is less supple and less elastic. This concentrates the shock waves of pressure inherent in so many forms of action, focuses them on the cartilage, and promotes even more degeneration.
This process also produces sufficiently great pressures on the bones that they react, as bones must, by laying down new bone substance in the areas of greatest stress. The production of osteophytes may be the response of bone to the eccentric stresses brought about by the degenerative process. Unfortunately, just as the cartilage is getting thin, the underlying bone is changing shape, altering still further the patterns of stress for which the joint was originally so well adapted.
There is more to learn about osteoarthritis. It was recently shown that brief stimulation “winds up”neurons inside the joint and at the spinal cord and brain, making them more reactive to future stimuli. In addition, peripheral and central sensitization, in effect, make a person feel greater pain from the same cause.14 Further, the stimulated pain fibers in the joint actually give off substances that attack cartilage.15 Like eddies in a rushing stream, in arthritis one vicious cycle leads to others. These silent destructive forces may have an equally silent and equally effective antidote.
There is good reason to believe that the calming effect of yoga is beneficial here. Soothing, relaxing physical activity is beneficial after cardiac events and in people with asthma or hypertension. Where hyperexcitability of the nervous system is part of the problem, yoga has often been part of the solution. But this has yet to be demonstrated empirically. Verifying the efficacy of practical yoga solutions to medical problems is now a reality.16 Sometimes significant advances are made by practitioners like you.
But to become a practitioner, one must practice. In the next chapter we offer you some guidance based on our experience that will make yoga safer, maximally effective, and more fun.