
Age is not a disease. It is a state to which most of us aspire. But advancing years do not come without a price. For many of us, one price of a long life is osteoarthritis, a painful and often debilitating condition caused by decades of wear and tear on the joints. In fact, by the time we reach age sixty-five, knee X-rays for at least a third of us will show some signs of osteoarthritis,1 the most common of a group of diseases collectively referred to simply as arthritis.
Literally translated “joint inflammation,” arthritis in its many forms affects more than seventy million (or one in three) American adults, according to estimates by the Centers for Disease Control and Prevention in Atlanta. Arthritis is the leading cause of disability in this country, limiting everyday activities for more than seven million adults.2

Although the specifics of the different types of arthritis vary, they have a common thread: all affect the joints, those nearly 150 ingenious—and essential—structures located where two or more bones come together. With a few exceptions, these joints (when working properly) are easily movable, allowing us to bend, flex, sit, grasp, open and close our mouths, lift, turn, get out of bed, and walk—or run—where we need to go.
In healthy joints, articular cartilage—a tough, shock-absorbing padding with a slick surface—enables the ends of the bones to glide effortlessly past each other. This gliding is facilitated by a viscous lubricating fluid (a natural WD-40, of sorts) called synovial fluid, which is secreted by a thin membrane, the synovium, that lines the joint. Bones are held together at the joints by strong, inelastic bands of tissue, called ligaments, that help keep the joint aligned. Tough cords of tissue, the tendons, connect muscle to bone. Muscles work in opposing pairs to bend and straighten joints. While muscles are not technically part of a joint, they are important because strong muscles help support and protect joints and cause bones to move. Outside the joints, fluid-filled sacs called bursae cushion and safely separate the bones and tendons around the joints, enabling them to move smoothly and freely.
Osteoarthritis can be the result of so many different factors that it might often appear to have no identifiable cause. In a way, that is what people mean when they say it is due to “wear and tear.” They mean that just living will lead to osteoarthritis.
We have already mentioned trauma and overuse as special cases where a cause can be identified. Deficiencies in the chemical structures that make up the cushions, the glycosaminoglycans, are another special cause. Many other genetic, hormonal, and environmental factors are also relevant: somatotropin C, growth hormone, thyroxine, testosterone, corticosteroids, and estrogen, to name a few.
Whereas osteoarthritis usually develops over time from the processes of wear and tear, factors such as a severe injury to the joint that damages the cartilage or throws off the alignment of the bones can cause cartilage to wear unevenly and start the osteoarthritis process earlier. Also, research has shown that some people have inherited defects in joint cartilage, such as Ehlers-Danlos syndrome and Marfan syndrome, that predispose them to the early development of osteoarthritis.3,4 For our purposes—relieving the pain and limitation that come with arthritis—we focus on the actual sites of damage: the joints.
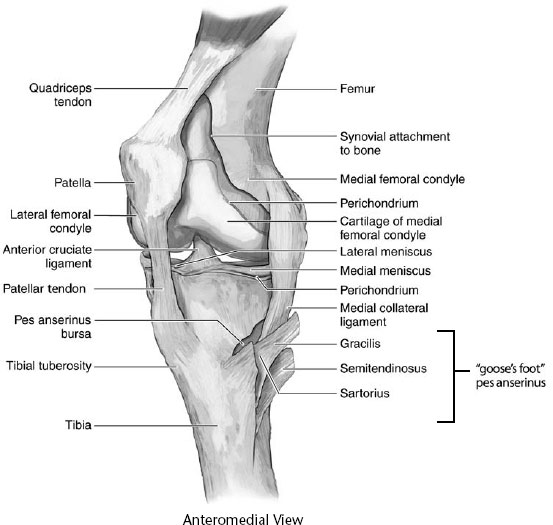
Figure 1. A representative joint—the knee. The pes anserinus bursa is so named because the three tendons that join there resemble a goose’s foot. Bursae separate bones from the muscles that cross them, protecting each from the other. Arthritic movement patterns, however, may inflame the bursae, causing pain exactly where they normally prevent it.
Over the course of a lifetime, the cartilage that covers the ends of the bones can begin to wear away. But cartilage is mainly inanimate—it is a lifeless product of live cells, like nails and hair. Just like hair, it is in continuous production. And just like nails, the distribution and condition of the underlying cells determine the quality and elasticity of the cartilage.
A good quantity of viscous lubricating fluid bathes the joint, making its movements smooth and easy. A capsule of connective tissue encloses the joint like a gasket, containing the joint fluid. Synovial cells at the inner surface of the capsule secrete the joint fluid. Another special layer of cells, the perichondrium, lies beneath the cartilage, between it and the bone. Replete with blood vessels, it serves to nourish the chondrocytes, the cartilage-producing cells that dwell within the cartilage. The cartilage itself has no blood vessels.5
Cartilage located elsewhere in the body—not at joints—has perichondrium on both sides. For example, in the windpipe, perichondrium lines the inside as well as the outside of the cartilage rings. In contrast, joint cartilage is supported only from beneath, from the bone it grows out of, not from above, not at the actual point of bone-to-bone contact. Joint cartilage has no inner layer of supportive cells. Yet the inner surface of the cartilage is what actually comes in contact with its counterpart on the other bone, the part that sustains the pressures of movement. This cartilage may be where the need for nourishment and the building blocks for repair is greatest!
The joint fluid brings the essential supplies for nourishment and repair to the chondrocytes. The inner lining of the joints (the synovial membrane) not only makes the fluid, but also delivers oxygen, glucose, proteins, and other necessities to that fluid and absorbs the products of their metabolism. The beauty is that the very movement that serves the joint’s function also circulates the fluid that makes continued movement possible. Circulation is good for the joint.6 As Arthur Abrahamson, former chairman of the Department of Physical Medicine and Rehabilitation at Albert Einstein College of Medicine, was fond of saying, “Function breeds function.”
One thing that yoga does for sure is move the joints into extreme but safe positions, allowing the obscure corners and crevices of each joint to be awash with its lubricating, life-sustaining fluid.
Without good circulation of the synovial fluid, the smooth surfaces of cartilage can fall into states of disrepair. The chondrocytes will not keep up with the pace of normal wear and tear. Fibers of collagen, which are what give cartilage its elastic properties, are not replaced quickly enough, and soon the cartilage loses its supple resilience. The surfaces become rough and cracked, which leads to more wearing away. (Chapter 3 has more on this important subject.)
Naturally, other factors, including hormonal and hereditary factors, and the frequency, intensity, and pattern of use, overuse, and trauma, are at work here too. All of these elements can add up to enough of a departure from a joint’s normal, or homeostatic, condition to produce inflammation. It usually occurs without any infection, without anything actually breaking. This further compromises the cartilage, and actually stimulates the bone underlying it. In response to inflammation, and possibly in an effort to repair the damage, the ends of the bones might thicken and the bone might form outgrowths, called spurs or osteophytes, which can interfere with function and give the joint an enlarged, knobby appearance.
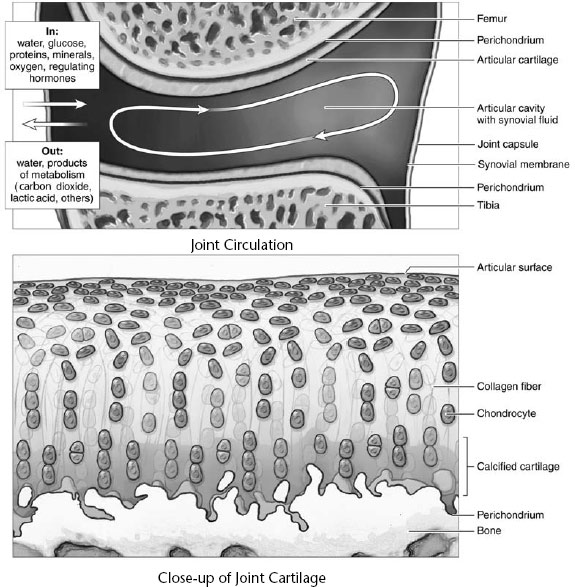
Figure 2. Circulation of synovial fluid is critical to the well-being of cartilage. Joint movement through exercise is the only way to produce it.
In joints between vertebrae at the cervical and lumbar levels, these osteophytes can obstruct the openings through which the nerves exit the spine, causing neurological signs and symptoms. The appropriate yoga for this lies in Chapters 8 and 9.
As cartilage is worn away, bone rubs more and more against bone. Pieces of cartilage and bone can break loose inside the joint, causing the joints to catch and to become stiff and noisy. If they are very active joints, such as the shoulders, or weight bearing, like the knees, this condition, known as chondrocalcinosis dessicans, can be extremely painful.
Osteoarthritis can affect a single joint or many. The most commonly affected joints are those of the knees, hips, neck, lower back, fingers, and the base of the thumb and big toe.
If anything good can be said for osteoarthritis, it is that the disease typically spares younger people and its effects are confined to the joints. With some other forms of arthritis, the debilitating effects can come during what should be the most productive years of life—the peak earning and child-rearing years—or even earlier. In addition to their effects on joints, some forms of arthritis can also cause damage to the skin, eyes, blood vessels, and internal organs.
Let us take a look at some of the other more common forms of arthritis.
Next to osteoarthritis, the most common form of arthritis is rheumatoid arthritis, affecting an estimated 2.1 million Americans.7 Unlike osteoarthritis, which is largely a disease of mechanical wear and tear, rheumatoid arthritis is believed to be an autoimmune disease—that is, a disease in which the body’s immune system turns against and destroys healthy tissue. In rheumatoid arthritis, the primary targets of the attack are the synovial linings of the joints and sometimes the similarly designed membranes lining the blood vessels, heart, and lungs.
In a joint affected by rheumatoid arthritis, both the synovial lining and the fluid it secretes become infiltrated with white blood cells from the lymph nodes, spleen, thymus, and circulating blood. These cells normally help protect the body from harmful invaders such as viruses, bacteria, and other microorganisms collectively known as antigens. But in rheumatoid arthritis a number of types of white blood cells can cause harm.
B cells (so named because they mature in the bone marrow) are responsible for the production of antibodies, proteins designed specifically to destroy a particular foreign substance. While antibodies help rid our bodies of infection, misdirected antibodies cause damage. Many people with rheumatoid arthritis have an abnormal antibody called rheumatoid factor (RF) in their blood. High levels of RF are generally associated with a more severe course of the disease. Other antibodies also target healthy tissue.
Mast cells, secreters of destructive enzymes, contribute to damage and dysfunction in both osteoarthritis and rheumatoid arthritis. Recently, they were found to occur in greater numbers in joints affected by osteoarthritis than in traumatically injured joints or even in joints with rheumatoid arthritis,8 suggesting a special inflammatory role for them in osteoarthritis, and possibly another avenue for prevention and treatment in the future.
T cells (so named because they mature in the thymus) come in many forms. Some are responsible for helping B cells produce antibodies. Some are responsible for stopping the immune system’s attack once the invader has been eliminated. Still others engulf and destroy antigen particles in the blood, destroy cell debris, or produce powerful chemical secretions that trigger or help regulate the body’s immune response. They also present foreign material to the B cells for destruction, expediting the production of antibodies. In rheumatoid arthritis, some of this “foreign” material belongs to the person whose cells they are—not only is it not foreign, it is essential to the normal operation of the cell!
Macrophages are called scavenger cells because they clean up the mess left by B cells and T cells by eating up antigen particles left in the blood. They also secrete chemicals called cytokines that signal the immune system to either rev up or slow down its attack. In rheumatoid arthritis and many other forms of arthritis, a dysregulation of these chemicals and their signals contributes to symptoms and damage.
Neutrophils are white blood cells that fight infection and produce powerful enzymes that break down cell debris in the blood. These enzymes can be so virulent, in fact, that they can damage the synovial membranes that line the joints, and the cartilage that cushions them. Neutrophils also produce substances that increase blood flow to the affected area. Increased blood flow and internal fluids cause the affected joints to swell, and deliver other white blood cells that take part in the damaging attack, generally known as inflammation.
Unless the immune system’s attack is stopped, rheumatoid arthritis can progress to damage not only the synovium but also the joint cartilage, underlying bone, and ligaments and tendons, causing deformity and disability.
Rather than a single form of arthritis, the spondylarthropathies comprise a group of diseases that affect the spine, the sacroiliac joints (where the lower end of the spine attaches to the pelvis), and the structures that join ligaments and tendons to bone. These diseases can also affect other joints, such as those of the arms, legs, feet, and hands, and body tissues, including the skin, eyes, bowel, and genitourinary tract.
It is estimated that between 354,000 and 412,000 Americans over age fifteen have a spondylarthropathy.9 Following are the most common of these diseases.
Largely a disease of young men, ankylosing spondylitis usually begins gradually with back pain, which can range from mild to severe and is generally worse at night or first thing in the morning. Some people also have pain that radiates down the legs.
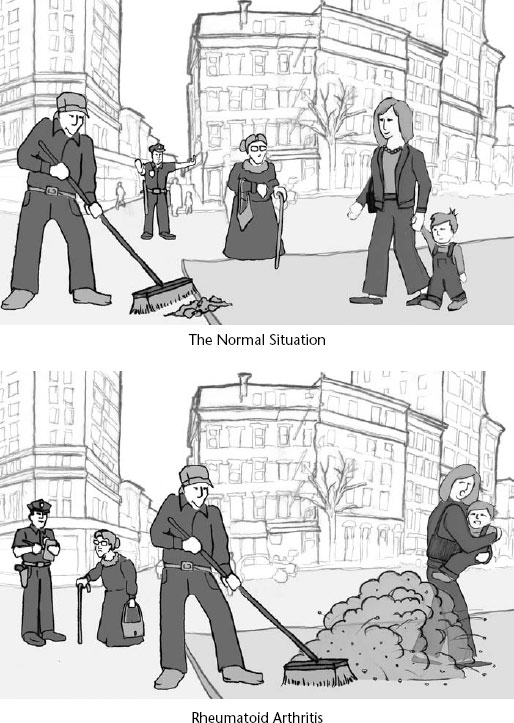
Figure 3. In rheumatoid arthritis the immune system retains its potency, but it performs its lethal tasks on the very cells it normally defends.
Ankylosing spondylitis typically begins with inflammation around the sacroiliac joints, which might then progress up the spine. The ligaments and tendons that keep the bones of the spine in place and attach the muscles to the limbs and ribs can turn to bone, or ossify, causing the spine to become stiff or even rigid. In advanced cases, the spine may become fused into a stooped position, making bending or even turning the head impossible. The chest wall may also become rigid, making it difficult to breathe.
The treatment goal for ankylosing spondylitis is to reduce inflammation and to retain functional abilities. This means keeping the joints of the spine as flexible as possible and, if the spine is fused into rigidity, maximizing the flexibility and strength of the arms and legs. Good posture is important. It is also important for people with ankylosing spondylitis to strengthen the muscles that support the spine.
Also called Reiter’s syndrome, reactive arthritis is so named because it occurs in reaction to an infection in another part of the body, typically the intestines, or kidneys, bladder, and genitals. For many people, reactive arthritis is preceded by a bout of diarrhea. It can also occur following urethritis (inflammation of the tube leading from the bladder through the penis that transports and discharges urine and semen) in men or cystitis (inflammation of the bladder) in women.
Reactive arthritis is characterized by inflammation of the joints as well as the surrounding ligaments, tendons, and muscles. It most commonly affects the joints of the legs and feet, but it can also affect other joints, including those of the fingers. Other common characteristics of the disease include a rash on the soles of the feet and palms of the hands, sores in the mouth or on the genitals, and inflammation of the eyes.
The joint inflammation of reactive arthritis often comes and goes. For some people the disease is chronic. In others it resolves and disappears completely over time. It represents another example of the immune system gone awry, this time initiated by an infection, a perfectly legitimate arousal of the body’s immune defenses.
Psoriatic arthritis is a form of arthritis that affects 23 percent of people who have the skin disease psoriasis, according to the Psoriasis Foundation’s 2001 Benchmark Survey.10
As with other forms of arthritis, psoriasis might be mediated by the immune system. However, recent evidence in experimental mice suggests that a certain part of chromosome 19, JunB, might be mutant or deleted in people with this disease.11 These genes are known to regulate the speed of reproduction and stress response of the deeper layers of skin, and deleting the gene sequence in mice actually produced the signs and symptoms of psoriasis.
A normal skin cell matures and falls off the body’s surface in twenty-eight to thirty days. But a psoriatic skin cell takes only three to four days to mature and move to the surface. Instead of falling off, the psoriatic cells pile up and form lesions. Depending on the specific form of psoriasis, the lesions can be raised and scaly, dotlike, intensely red and inflamed, or weeping.
In joints the disease process is a little more complicated, since both T cells and B cells play a role. It is likely that the immune system is somehow out of control here too.12 Contemporary research suggests that in normal development, macrophages actually mark “extra” cells for death, and it is possible that this mechanism is working too hard in hereditary autoimmune illnesses as well.13
In addition to the joints of the spine, the arthritis that accompanies psoriasis can affect the fingers, toes, knees, and ankles. Psoriatic arthritis is similar to rheumatoid arthritis in that it is the body’s own protective elements, the skin and the immune system, that do it ill. But psoriatic arthritis is generally milder. In psoriatic arthritis, the joints and the soft tissue around them become inflamed and stiff. However, severe psoriatic arthritis can be disabling and cause irreversible damage to joints.
Once associated with royalty, gout occurs when a bodily waste product called uric acid rises to such high levels in the bloodstream that it seeps out and deposits as sharp crystals in the joint tissue, much the way sugar settles to the bottom of a glass of iced tea. Uric acid is a result of the breakdown of purines, chemicals derived from nucleic acid in the cells. Many meats, especially organ meats, are high in purines. Your body also produces purines, which it then breaks down into uric acid.
Normally, the kidneys filter uric acid from the blood. Problems result when the body produces too much uric acid, or the kidneys cannot effectively eliminate excess uric acid.
Although gout can affect many joints—the feet, knees, elbows, and sometimes the finger and wrist joints—it typically begins with a single attack or periodic attacks in the big toe, a condition called podagra. During an attack, white blood cells rush to the joint, causing inflammation. The joint tissue swells and the skin over the joint becomes tight, shiny, and crimson. The pain can be excruciating. In his book The Duke University Medical Center Book of Arthritis, David Pisetsky writes, “One patient told me during an attack he noticed a housefly in the bedroom and couldn’t take his eyes off that fly, terrified it would settle on his toe. Another worried that a piece of peeling paint from the ceiling was going to drop off on his toe.”14
Gout affects an estimated 2.1 million Americans.15 At middle age and younger, men are more likely than women to have gout. After menopause, the risk of developing gout for women is roughly that of men.
Unless gout is treated, attacks can become more frequent and severe and progress to affect more joints. For some people, fortunately, the proper diet (low in purine-rich foods and alcohol), exercise, and weight loss are effective at treating or even preventing the disease. In a twelve-year study of 47,150 men, doctors found that higher levels of meat and seafood consumption are associated with an increased risk of gout, whereas a higher level of consumption of dairy products is associated with a decreased risk.16 A separate study of the same population showed that the risk of gout increased as body mass index increased. Men who lost ten pounds over the course of the twelve-year study cut their risk of gout almost in half, while those who gained thirty pounds since age twenty-one almost doubled their risk.17
Advances in recent years have made it possible for people with many forms of arthritis to live longer, more productive, and less painful lives. A variety of analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs), available both over the counter and by prescription, help ease the pain of virtually any form of arthritis.
Strong immunosuppressive drugs or newer biological agents such as etanercept (Enbrel) and infliximab (Remicade) can help stop the disease processes of rheumatoid arthritis and the spondyloarthropathies. Corticosteroid medications such as prednisone and methylprednisolone (Medrol) can help halt inflammation that threatens the joints and internal organs in people with rheumatoid arthritis or other inflammatory forms of disease.
And for people with gout, anti-inflammatories (including NSAIDs), cochicine, corticosteroids, or adrenocorticotropic hormone (ACTH) can help ease the pain and inflammation of acute attacks, while other drugs that slow the production of uric acid or help the kidneys excrete it more efficiently can prevent—or at least lessen the frequency, duration, and severity of—future attacks.
When, despite the best medical treatment, joints are irreparably damaged and pain and stiffness limit daily activities, surgically replacing the joint with a prosthesis made of metal, plastic, or ceramic material can relieve pain and restore form and function.
Despite these treatment advances, which relieve pain, prevent damage, and preserve function, none is without a downside. Analgesics can become addictive. NSAIDs can cause stomach upset and ulcers, and recent reports show that some are not safe for our hearts.18 Cortico-steroids, though they are powerful against inflammation, can cause a wide range of problems, including weight gain, thin skin, cataracts, and brittle bones. Immunosuppressives and biological agents, too, have their downsides, ranging from injection-site reactions to increased risk of serious infections. Great advances? No doubt. Life saving? In some cases, yes. Perfect? Far from it.
Certainly there are cases where medications are necessary to control a disease that is threatening one’s joints or even life. But relying on medication to the exclusion of other therapies and healthy lifestyle habits is a mistake. Study after study shows the benefits of exercise for many forms of arthritis. Exercise will improve strength and increase range of motion in affected joints. It will reduce the excess weight that contributes to the development of some forms of arthritis19 and adds stress to painful joints. Exercise improves general well-being and mood and even etiolates signs of disease activity. This goes for many forms of arthritis, including osteoarthritis and gout.20
Then there is the combination of the two: medication and exercise. Although nonsteroidal and other medications do have side effects, and surely can be abused, there is little question of their beneficial influence on people suffering from arthritic disease. And they can be combined with yoga,21 substantially amplifying the benefits of each. In some people, continued use of both is best; in others, medication can ease the pain and difficulty of beginning exercise, which, after a while, is sufficiently successful that it eliminates the need for medicines. In still others, medication and exercise can be used intermittently, as conditions permit and require.
In a progressively disabling condition such as arthritis, a multidisciplinary, integrative approach is quite effective; using everything available that is helpful, and avoiding overreliance on any one form of relief. Even with exercise there is that one caveat: don’t overdo it. Exercise that is jarring or too strenuous can put stress on the joints and can make the problem worse, not better. That’s why we recommend yoga.
Ready to give exercise a shot? Then let’s get moving … gently.