

• Abnormally large or painful conglomerates of vessels, supporting tissues, and overlying mucous membrane or skin of the rectal area
• Bright red bleeding on the surface of the stool, on the toilet tissue, and/or in the toilet bowl
In the United States and other industrialized countries, hemorrhoids are extremely common. Estimates have indicated that 50% of those over 50 years of age have symptomatic hemorrhoidal disease, and up to one-third of the total U.S. population has hemorrhoids to some degree. Although most individuals may begin to develop hemorrhoids in their 20s, hemorrhoidal symptoms usually do not become evident until the 30s.
Causes
The causes of hemorrhoids are similar to the causes of varicose veins (see the chapter “Varicose Veins”): genetic weakness of the veins and/or excessive pressure on the veins.
Because the venous system that supplies the rectal area contains no valves, factors that increase venous congestion in the region can lead to hemorrhoid formation. These factors include increased intra-abdominal pressure (caused by defecation, pregnancy, coughing, sneezing, vomiting, physical exertion, or portal hypertension due to cirrhosis); an increase in straining during defecation due to a low-fiber diet; diarrhea; and standing or sitting for prolonged periods of time.
Classification of Hemorrhoids
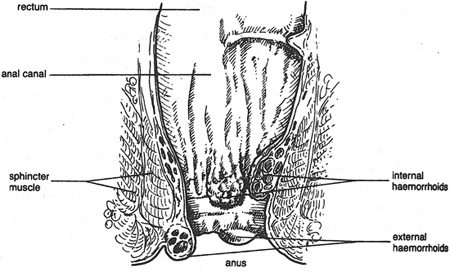
Hemorrhoids are typically classified according to location and degree of severity. External hemorrhoids occur below the anorectal line—the point in the 3-cm-long anal canal where the skin lining changes to mucous membrane. They may be full of either blood clots (thrombotic hemorrhoids) or connective tissue (cutaneous hemorrhoids). A thrombotic hemorrhoid is produced when a hemorrhoidal vessel has ruptured and formed a blood clot (thrombus), while a cutaneous hemorrhoid consists of fibrous connective tissue covered by anal skin. Cutaneous hemorrhoids can be located at any point on the circumference of the anus. Typically, they are caused by the resolution of a thrombotic hemorrhoid: that is, the thrombus becomes organized and replaced by connective tissue.
Internal hemorrhoids occur above the anorectal line. Occasionally, an internal hemorrhoid enlarges to such a degree that it prolapses and descends below the anal sphincter. Internal hemorrhoids are graded by the degree of prolapse:
Grade I: No prolapse
Grade II: Prolapses upon defecation but spontaneously reduces
Grade III: Prolapses upon defecation and must be manually reduced
Grade IV: Prolapsed and cannot be manually reduced
Internal-external, or mixed, hemorrhoids are a combination of contiguous external and internal hemorrhoids that appear as baggy swellings. The following types of mixed hemorrhoids can occur:
• Without prolapse: Bleeding may be present, but there is no pain.
• Prolapsed: Characterized by pain and possibly bleeding.
• Strangulated: The hemorrhoid has prolapsed to such a degree and for so long that its blood supply is occluded by the anal sphincter’s constricting action; strangulated hemorrhoids are very painful and usually become filled with blood clots (thrombosed).
Diagnostic Considerations
The symptoms most often associated with hemorrhoids include itching, burning, pain, inflammation, irritation, swelling, bleeding, and seepage. Itching is caused when there is mucous discharge from prolapsing internal hemorrhoids; tissue trauma resulting from excessive use of harsh toilet paper; Candida albicans; parasitic infections; and food allergies. Pain occurs when there is acute inflammation of external hemorrhoids. However, as there are no sensory nerve endings above the anorectal line, uncomplicated internal hemorrhoids rarely cause pain. Bleeding is almost always associated with internal hemorrhoids and may occur before, during, or after defecation. When bleeding occurs from an external hemorrhoid, it is due to rupture of an acute thrombotic hemorrhoid. Bleeding hemorrhoids can produce severe anemia due to chronic blood loss.
Therapeutic Considerations
Conventional medical treatment of acute hemorrhoids may be appropriate.
• Rubber band ligation is a procedure in which elastic bands are applied to an internal hemorrhoid to cut off its blood supply. Within a week the hemorrhoid simply falls off. This technique is inexpensive, is simple, and has a cure rate of about 87%.
• Sclerotherapy involves the injection of a scar-forming agent into the hemorrhoid, causing the vein walls to collapse and the hemorrhoid to shrivel up. The success rate four years after treatment is 70%.
• A number of cautery methods (electrocautery, infrared radiation, laser, and cryosurgery) have been shown to be effective for hemorrhoids.
• Hemorrhoidectomy is surgical excision of the hemorrhoid. It is used only in severe cases because it is associated with significant postoperative pain and usually requires two to four weeks for recovery.
Hemorrhoids are rarely seen in parts of the world where diets rich in high-fiber, unrefined foods are consumed. A low-fiber diet, high in refined foods, like that common in the United States, contributes greatly to the development of hemorrhoids.1
Individuals who consume a low-fiber diet tend to strain more during bowel movements, since their smaller, harder stools are more difficult to pass. This straining increases the pressure in the abdomen, which obstructs venous blood flow. The intensified pressure increases pelvic congestion and may significantly weaken the veins, causing hemorrhoids to form.
Hemorrhoids
A high-fiber diet is perhaps the most important component in the prevention of hemorrhoids. A diet rich in vegetables, fruits, legumes, and grains promotes rapid transit of the feces through the intestine. Furthermore, many fiber components attract water and form a gelatinous mass that keeps the feces soft, bulky, and easy to pass. The net effect of a high-fiber diet is significantly less straining during defecation. The importance of fiber is discussed in more detail in the chapter “A Health-Promoting Diet.”
Natural bulking compounds can also be used to reduce fecal straining. These fibrous substances, particularly psyllium seed husks and guar gum, possess mild laxative action, owing to their ability to attract water and form a gelatinous mass. They are generally less irritating than wheat bran and other cellulose-fiber products. Several double-blind clinical trials have demonstrated that supplementing the diet with bulk-forming fiber can significantly reduce the symptoms of hemorrhoids (bleeding, pain, itching, and prolapse) and improve bowel habits.2,3 A meta-analysis of seven studies showed that the use of fiber helps relieve overall symptoms and bleeding in the treatment of symptomatic hemorrhoids.2
A warm sitz bath (a partial-immersion bath of the pelvic region) is an effective noninvasive therapy for uncomplicated hemorrhoids. The temperature of the water should be between 100 and 105°F. The warm sitz bath is soothing, but as with creams and ointments, its relief is short-lived.
Topical treatments, in most circumstances, will provide only temporary relief, but even temporary relief is better than no relief at all. Topical treatments include suppositories, ointments, and anorectal pads. Many over-the-counter products for hemorrhoids contain primarily natural ingredients, such as witch hazel, aloe vera gel, shark liver oil, cod liver oil, cocoa butter, Peruvian balsam, zinc oxide, live yeast cell derivative, and allantoin.
Flavonoid preparations have been shown to relieve hemorrhoids by strengthening the veins. Early studies featured rutin. More-recent and much more extensive studies have been performed using hydroxyethylrutoside (HER). Rutin and citrus bioflavonoid preparations can be viewed as providing effects similar to those of HER, but probably not as potent.
In several double-blind clinical studies, HER has been found helpful in the treatment of varicose veins and hemorrhoids.4,5 Some of the studies involved pregnant women; HER was shown to be of great benefit in improving venous function and helping relieve hemorrhoidal signs and symptoms during pregnancy. In one study, 90% of the women who were given HER (1,000 mg per day for four weeks) experienced relief from symptoms, compared with only 12% in the placebo group. Similar results have been reported for the use of HER to treat hemorrhoids not associated with pregnancy.
Micronized diosmin and flavonoid-rich extracts such as those from grape seed or pine bark are also suitable choices.
Any of the botanicals described in the chapter “Varicose Veins,” and particularly butcher’s broom (Ruscus aculeatus), are useful for enhancing the integrity of the veins of the rectum. In one multicenter study of 124 patients with hemorrhoids, 69% of the patients and 75% of the treating physicians rated a formula containing butcher’s broom extract as having good or excellent efficacy, and 92% of physicians rated the treatment as safe and well tolerated.6 Significant positive effects were observed after seven days of treatment.
![]()
QUICK REVIEW
• The veins in the rectal area contain no valves, so factors that increase congestion of blood flow or pressure in the region can lead to hemorrhoid formation.
• Common causes of anal itching include tissue trauma from excessive use of harsh toilet paper, Candida albicans, parasitic infections, and food allergies.
• A high-fiber diet is perhaps the most important component in the prevention of hemorrhoids.
• Flavonoid preparations have been helpful in relieving hemorrhoids by strengthening the veins.
![]()
As with all diseases, the primary treatment for hemorrhoids is prevention. This goal involves reducing the factors that may be responsible for increasing pelvic congestion: straining during defecation, sitting or standing for prolonged periods of time, or underlying liver disease. A high-fiber diet is crucial for the maintenance of proper bowel activity. Fiber supplements, flavonoids, and various botanical medicines such as butcher’s broom are appropriate supplementary measures.
Warm sitz baths and topical preparations help relieve the discomfort but have only temporary effects.
The recommendations in the chapter “A Health-Promoting Diet” are very important in preventing and treating hemorrhoids. The diet should contain liberal amounts of soluble dietary fiber and flavonoid-rich foods, such as blackberries, citrus fruits, cherries, and blueberries, to strengthen vein structures.
• A high-potency multiple vitamin and mineral formula as described in the chapter “Supplementary Measures”
• Psyllium seed husk: 5 g at bedtime with 6 to 8 ounces of water
• Vitamin C: 500 to 1,000 mg three times per day
• Flavonoids, one or more of the following:
![]() HER: 1,000 to 3,000 mg per day
HER: 1,000 to 3,000 mg per day
![]() Citrus bioflavonoids, rutin, and/or hesperidin: 3,000 to 6,000 mg per day
Citrus bioflavonoids, rutin, and/or hesperidin: 3,000 to 6,000 mg per day
![]() Micronized diosmin: 500 to 1,000 mg per day
Micronized diosmin: 500 to 1,000 mg per day
![]() Grape seed extract (>95% procyanidolic oligomers): 150 to 300 mg per day
Grape seed extract (>95% procyanidolic oligomers): 150 to 300 mg per day
![]() Pine bark extract: 150 to 300 mg per day.
Pine bark extract: 150 to 300 mg per day.
• Butcher’s broom (Ruscus aculeatus) extract (9%% to 11% ruscogenin content): 100 mg three times per day
• Hydrotherapy: warm sitz baths to relieve uncomplicated hemorrhoids