

• Permanent cessation of menstruation in older women
• Average age of onset: 51
• Common complaints of menopause: hot flashes, headaches, atrophic vaginitis, frequent urinary tract infections, cold hands and feet, forgetfulness, inability to concentrate
Menopause is the permanent cessation of menstruation in women, which occurs on average around age 51 but may occur as early as 40 and as late as 55 years of age or even later. Six to 12 months without a menstrual period is the commonly accepted rule for diagnosing menopause. The time prior to menopause is referred to as perimenopause, and the time after menopause is referred to as postmenopause. During perimenopause, many women ovulate irregularly, owing to either decreased secretion of estrogen or resistance of the remaining follicles to ovulatory stimulus.
Many conventional doctors still see menopause as a disease rather than a normal physiological process. This view is in stark contrast to the perspective of many cultures, where menopause is viewed as a natural part of the life process and a positive event in a woman’s life. In fact, in many parts of the world, most women do not experience the symptoms Americans tend to associate with menopause. This observation raises some interesting questions about menopause as a sociocultural event. However, there are certainly important dietary and environmental factors to consider as well.
Despite considerable research questioning its value, the current medical treatment of menopause primarily involves the use of hormone replacement therapy (HRT), utilizing a combination of estrogen and progesterone. The obvious question is whether hormone replacement therapy is necessary. The goal of this chapter is to answer that question and provide a natural approach to menopause and the postmenopausal period.
Causes
Menopause is thought to occur when there are no longer any viable eggs left in the ovaries. At birth, a woman has about 1 million eggs. This number drops to around 300,000 or 400,000 at puberty, but only about 400 of these ova will actually mature during the reproductive years. By the time a woman reaches the age of 50, few eggs remain.
With age, the absence of active follicles (the cellular housing of the egg) results in reduced production of estrogen and progesterone. In response to this drop in estrogen, the pituitary gland increases secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). After menopause, FSH and LH are secreted continuously in large quantities, even though there are no longer any follicles to stimulate. These two hormones cause the ovaries and the adrenal glands to secrete increased amounts of androgens (male sex hormones), which can be converted to estrogens by the fat cells of the hips and thighs. Converted androgens account for most of the circulating estrogen in the postmenopausal woman, but total estrogen levels are still far below the levels in women still in their reproductive years.
Major Symptoms
Many of the symptoms of menopause, especially hot flashes, appear to be a result of altered function of the hypothalamus, a mass of tissue at the center of the brain that serves as the bridge between the nervous system and the hormonal (endocrine) system. The hypothalamus is responsible for the control of many body functions, including body temperature, metabolic rate, sleep patterns, reactions to stress, libido, mood, and the release of pituitary hormones. Critical to proper functioning of the hypothalamus are the endorphins, the body’s own mood-elevating and pain-relieving compounds. Endorphins are also thought to play a role in hot flashes. Several natural measures are thought to exert some of their beneficial effects against hot flashes by enhancing endorphin output. Two of the most effective measures are exercise and acupuncture.
Hot flashes are the most common symptom of menopause. The term hot flash refers to dilation of the peripheral blood vessels, which leads to a rise in skin temperature and flushing of the skin. In the typical hot flash, the skin, especially of the head and neck, becomes red and warm for a few seconds to a few minutes, with cold chills coming thereafter. Hot flashes can be accompanied by other symptoms, including increased heart rate, headaches, dizziness, weight gain, fatigue, and insomnia.
In the United States, 65 to 80% of women around menopause experience hot flashes to some degree. Hot flashes are often the first sign that menopause is approaching, as they may begin prior to the cessation of menses. In most cases, hot flashes are at their most uncomfortable in the first and second years after menopause. As the body adapts to decreased estrogen levels, hot flashes typically subside.
Headaches, especially migraines, often accompany menopause owing to increased instability of the blood vessels. Headaches often accompany hot flashes.
After menopause, the vaginal lining may become thin and dry owing to the lack of estrogen. As a result, menopausal and postmenopausal women may experience painful intercourse, an increased susceptibility to infection, and vaginal itching or burning.
Women with atrophic vaginitis should try to avoid substances that tend to dry the mucous membranes, including antihistamines, alcohol, caffeine, and diuretics. In addition, it is critical that the body stay well hydrated. Drink at least 32 to 48 fl oz water per day.
Underwear made from natural fibers, particularly cotton, is often recommended, as it allows the skin to breathe, thus decreasing the incidence of vaginal infections.
Regular sexual intercourse is also beneficial, as it increases blood flow to vaginal tissues; this blood flow helps improve tone and lubrication. However, good lubrication must be maintained; there are many oil- and water-based lubricants available, such as K-Y jelly.
About 15% of menopausal women experience frequent bladder infections. Apparently there is a breakdown in the natural defense mechanisms that protect against bacterial growth in the urinary tract. The primary goal in the natural approach to treating bladder infections is to enhance a woman’s normal resistance to urinary tract infection. Specifically, increase the flow of urine through proper hydration, promote a pH that will inhibit the growth of microorganisms, and prevent bacteria from adhering to the endothelial cells of the bladder. In addition, there are several botanical medicines that can be employed. See the chapter “Cystitis and Interstitial Cystitis/Painful Bladder” for further information.
Cold hands and feet are common among women in general, not just menopausal women. During the menopausal period they become even more common. In most instances, there are three major causes of cold hands and feet: hypothyroidism, low iron levels in the body, and poor circulation. It is important to rule out hypothyroidism by measuring blood levels of thyroid hormones. Along with a CBC (complete blood count) and chemistry panel that includes LDL/HDL cholesterol levels, there should also be a test for serum ferritin levels, the best indicator of body iron stores. A complete physical exam is also required, with particular attention to any other signs of decreased blood flow. Once the cause is identified, the treatment is straightforward.
Forgetfulness and an inability to concentrate are common symptoms of menopause. Often these symptoms are simply a result of decreased oxygen and nutrient supply to the brain, due not to menopause per se but rather to atherosclerosis (hardening of the arteries) of the blood vessels supplying oxygen and nutrition to the brain.
The brain is highly dependent on a constant supply of oxygen and nutrients. Although it weighs only 3 pounds, the brain utilizes about 20% of the oxygen supply of the entire body. To deal with symptoms of forgetfulness and inability to concentrate, the goal is to improve the supply of blood, oxygen, and nutrients to the brain.
Menopause as a Social Construct
While there is undeniably a physiological process involved in menopause, menopause is much more than simply a biological event. Social and cultural factors contribute greatly to how women react to menopause. Modern society has placed great value on the allure of youth, resulting in a deeply entrenched cultural devaluation of older people, particularly women. Advocates of a social and cultural explanation of menopause often point to this cultural devaluing of older women as the root of the negativity associated with achieving menopause.
In contrast, in many cultures of the world, women look forward to menopause because it brings with it greater respect.1 Achieving an advanced age is viewed as a sign of divine blessing and great wisdom. Studies of menopausal women in many traditional cultures demonstrate that most will pass through menopause without hot flashes, vaginitis, and other symptoms common to menopausal women in developed countries. Even osteoporosis is extremely rare, despite the fact that the average woman in many traditional cultures lives longer than the average woman in the United States.
Cross-cultural research clearly demonstrates that the cultural view of menopause is directly related to the symptoms of menopause.2 If the cultural view of menopause is largely negative, as in the United States, symptoms are quite common. In contrast, if menopause is associated with little negativity or viewed in a positive light, symptoms are far less frequent.
One of the most detailed studies of the effects of culture on menopause involved rural Mayans.2 Detailed medical histories and examinations, including a physical examination, hormone-level measurement, and bone-density studies, were performed on 52 postmenopausal women. None of these women experienced hot flashes or any other menopausal symptom, and not one woman showed evidence of osteoporosis, despite the fact that their hormonal patterns (levels of the various female sex hormones) were identical to those of postmenopausal women living in the United States.
The researchers felt that the Mayan women’s attitude toward menopause was responsible for their symptomless passage. The Mayan women saw menopause as a positive event that would provide them acceptance as respected elders, as well as relief from childbearing. This attitude is much different from the dominant attitude toward menopause that is common in industrialized societies. If our society adopted a different cultural view of older women, it is likely that the symptoms of menopause would cease to exist.
In 1966, Robert A. Wilson, M.D., released his landmark book Feminine Forever, which introduced the theory that menopause is an estrogen-deficiency disease that needs to be treated with estrogen to compensate for the normal decline of estrogen levels with aging. According to Wilson, without estrogen replacement therapy women were destined to become sexless “caricatures of their former selves . . . the equivalent of a eunuch.”
Wilson’s theory of menopause as a disease is still the dominant medical view of menopause, even within many alternative medical circles touting “bioidentical” hormones as a way for women to remain “forever feminine.” These views place women who are entering menopause in a difficult situation: should they pass through this period of time naturally, or should they use hormonal therapy? Before this question can be answered, the benefits and risks of estrogen replacement therapy must be considered, as well as the natural alternatives.
Therapeutic Considerations
As we’ve noted, the current conventional medical treatment of menopause remains the short-term use (one to four years) of hormone replacement therapy for menopausal symptoms.
The use of HRT was widely accepted until 2002, when the National Institutes of Health (NIH) halted a major clinical trial designed to prove that HRT benefited postmenopausal women. This study, the Women’s Health Initiative (WHI), found just the opposite and concluded that the risks of taking combined estrogen and progestin outweighed the benefits, increasing the risk of stroke, coronary heart disease, and breast cancer.3
HRT was shown to produce a:
• 26% increase in invasive breast cancer
• 41% increase in strokes
• 29% increase in heart attacks
• Doubling of the rate of blood clots in legs and lungs
• Two- to threefold increase in gallstone formation and liver disease
Once this study made the headlines, many doctors and the public became aware of other studies reporting similar alarming statistics. For example, HRT not only stimulates the growth of invasive breast cancers but also makes it harder to spot the potentially deadly tumors on mammograms, as the breast tissue remains denser on HRT; it doubled the risk of developing Alzheimer’s and increased the risk of life-threatening blood clot formation.
While the WHI was viewed as a major revelation on the safety and efficacy of HRT, the reality is that this study and others only confirmed was what already known about the dangers of synthetic hormones.4–8
Despite the results of the Women’s Health Initiative and other studies showing the long-term problems associated with HRT, it is a sad fact that approximately 30 million prescriptions for HRT were still filled each year after 2002. Why on earth would doctors continue to prescribe HRT? Unfortunately, they are just not aware of effective natural strategies to deal with menopausal symptoms or reduce the risk of osteoporosis.
While there is no question that HRT is effective at relieving the symptoms of menopause, many health experts believe that long-term HRT is rarely justified in most women due to its risks. The only possible exception is women who are at high risk of developing osteoporosis (in the Women’s Health Initiative study, women taking HRT had a 34% lower risk of hip fracture), but even then there are natural approaches that can dramatically reduce the risk of this bone disease. To determine your risk for osteoporosis and for more information on natural approaches, see the chapter “Osteoporosis.”
Most women on HRT have no idea they are taking unnatural forms of estrogen and progesterone. Premarin, for example, contains forms of estrogen isolated from the urine of pregnant mares and includes more than 200 substances mostly foreign to humans. Animal rights activists also have long claimed that the methods used in Premarin’s production cause suffering to the mares involved. The major health problem for women taking Premarin and other common forms of conjugated estrogens is that they are metabolized in the body to 17-beta-estradiol, the form of estrogen most strongly associated with cancer. The synthetic versions of progesterone used in HRT, such as megestrol, norethindrone, and norgestrel, are likely to be even more problematic than the conjugated estrogens.
Most naturopathic physicians prefer to use a type of HRT known as bioidentical hormone therapy. The bioidentical hormones most commonly used in menopause include estradiol, estrone, estriol, progesterone, and to a lesser extent, testosterone and dehydroepiandrosterone (DHEA). Bioidentical hormones are made from either beta-sitosterol extracted from soybeans or from diosgenin extracted from wild yam (Dioscorea villosa). These compounds are then processed to create hormones that are biochemically identical to human hormones. Bioidentical hormones require a prescription and are available from regular pharmacies or from compounding pharmacies. Using compounded forms of hormones offers a greater array of dosing and delivery options—customized doses of a particular hormone are available that pharmaceutical companies do not make; the hormones can be provided as capsules, sublingual lozenges or pellets, creams, gels, vaginal creams/gels or tablets, nasal sprays, injections, and pellets implanted under the skin; and any combination of estradiol, estriol, estrone, progesterone, testosterone, and DHEA can be formulated in a prescription optimized to the specific needs of each woman.
The basic concept behind bioidentical hormone therapy is that some of the detrimental effects of HRT may be related to the inherent problem in the synthetic forms of hormones being used. In addition, the dosage of hormones used with bioidentical hormone therapy is generally considerably less than that used in conventional HRT. However, even though there is a lot of circumstantial evidence of a better safety profile with bioidentical hormones, at this time there are no definitive studies proving that bioidentical hormone therapy is better than or safer than HRT. Because bioidentical hormones are natural, they are not patentable—hence, there are no big drug companies promoting them. Without the promise of a financial windfall it is highly unlikely that the large trials necessary to conclusively show the advantages of bioidentical hormones will ever be conducted. Nonetheless, it makes more sense to use bioidentical hormones if hormonal support is required. Because we suggest prescription forms, we recommend consulting with your physician or seeking the counsel of a naturopathic physician.
A critical factor in hormone replacement—whether natural or conventional—is to not only measure hormone levels but also determine the makeup of their metabolites after detoxification. These can be tested in the saliva, blood, and urine.
Exercise
The health benefits of exercise for menopausal and postmenopausal women are extensive. In addition, regular physical exercise definitely reduces the frequency and severity of hot flashes. In one study, women who spent an average of 31/2 hours per week exercising had no hot flashes whatsoever, whereas women who exercised less were more likely to have hot flashes.10 Women can also achieve substantial reductions in cardiovascular disease, decrease their breast cancer risk, increase their bone density, and lower body fat and body mass index, as well as experience an improved sense of well-being.11–13
Health Benefits of Regular Exercise in Menopause
Relief from hot flashes
Decreased bone loss
Improved heart function
Improved circulation
Reduced blood pressure
Decreased blood cholesterol levels
Improved ability to deal with stress
Improved oxygen and nutrient utilization in all tissues
Increased self-esteem, mood, and frame of mind
Increased endurance and energy levels
Diet
The dietary guidelines discussed in the chapter “A Health-Promoting Diet” are very much indicated in helping improve menopausal symptoms. Perhaps the most important dietary recommendation may be to increase consumption of plant foods, especially those high in phytoestrogens, while reducing the consumption of animal foods. Phytoestrogens are plant-derived substances that are able to weakly bind to the estrogen receptors in mammals and have a very weak estrogen-like effect in some tissues and a weak antiestrogenic effect in other tissues. Soybeans and flaxseeds contain high amounts of phytoestrogens. Many other foods, such as apples, carrots, fennel, celery, parsley, and other legumes, contain smaller amounts of phytoestrogens. A high dietary intake of phytoestrogens is thought to explain why hot flashes and other menopausal symptoms appear to occur less frequently in cultures where the diet is predominantly plant-based. In addition, such a diet is promising for disease prevention, with some research showing a lower incidence of breast and prostate cancer in those consuming high-phytoestrogen diets.
Soy Products. Soy foods may be useful in menopause primarily for their potential benefits for hot flashes, but they may also slow bone loss, lower cholesterol and blood pressure levels, and reduce the risk of breast cancer. Some but not all clinical studies have shown eating soy foods (the equivalent of 2/3 cup soybeans per day) or taking a soy supplement to be effective in relieving hot flashes and vaginal atrophy.14–19 Those studies that do show a benefit indicate that increased soy intake can help reduce hot flashes and/or night sweats by 30 to 55%.
One study explains why results with soy are so inconsistent.20 In this six-month double-blind study, 66 women were given 135 mg soy isoflavones and 30 women were given a placebo. After one week, the women in the soy group were tested and further divided into two subgroups based upon their ability to metabolize the isoflavones into the phytoestrogen compound equol. Both of these subgroups were then given 135 mg isoflavones per day for six months. Compared with the results in the placebo group, symptoms of hot flashes and excessive sweating were significantly reduced after three months and total symptoms were significantly decreased after six months, but only in the group that broke down the isoflavones into equol. At six months, symptom scores had decreased by 84% in the equol-producing group, 58% in the non-equol-producing group, and 66% in the placebo group. Studies that had a higher percentage of women who were equol producers would show positive effects with soy supplementation, but if the study contained a lot of women who did not produce equol the results would have no effect.
So what determines the conversion of soy isoflavones into equol? It is the gut flora. It is thought that a higher level of health-promoting bacteria such as lactobacilli and bifidobacteria ensures proper conversion. Hence, we recommend that women using soy isoflavones to improve menopausal symptoms also take a probiotic supplement providing 5 billion to 20 billion live Lactobacillus and Bifidobacterium organisms.
Currently, a host of soy products can be found in most grocery stores, and even more in natural foods stores. They include dried soybeans, soy oil, soy milk, soy flour, roasted soy nuts, tofu, tofu paté, tempeh, miso, soy sauce, natto, edamame, soy ice cream, soy cheese, soy candy bars, soy burgers and hot dogs, and even soy marshmallows. For the greatest benefit, we recommend focusing on dietary sources vs. taking a supplement. Nonetheless, supplements containing soy isoflavones can also be used to deal with menopausal symptoms as well as possibly promote bone and cardiovascular health. The dosage should be in the same range as the dietary level of isoflavones in the traditional Asian diet: 45 to 90 mg per day of isoflavones.
Isoflavone Content of Soy Foods |
||
SOY FOOD |
AMOUNT |
ISOFLAVONES (MG) |
Roasted soy nuts |
1/4 cup |
60 |
Tofu, low-fat and regular |
1/2 cup |
35 |
Tempeh |
1/2 cup |
35 |
Soy beverage powders |
1–2 scoops |
25–90 |
Regular soy milk |
1 cup |
30 |
Low fat soy milk |
1 cup |
20 |
Roasted soy butter |
2 tbsp |
17 |
Cooked soybeans |
1/2 cup |
150 |
Flaxseeds. Another significant dietary source of phytoestrogens is flaxseed. Flaxseed contains the lignans matairesinol and secoisolariciresinol, which are known to have estrogenic activity. In addition, these lignans are modified by intestinal bacteria to form other lignans that are absorbed in the circulation and have both estrogenic and antiestrogenic activity.21,22 Although there is a lot of research on the protective effect of flax lignans against breast cancer, only a small amount of research has been done in the area of flaxseed and hot flashes. One study showed that women who consumed 2 tbsp of flaxseed twice per day halved their number of hot flashes within six weeks and reduced the intensity of the hot flashes by 57%.23
Nutritional Supplements
Fish Oils. In a study of fish oil supplementation in women between 40 and 55 years old with hot flashes and moderate to severe psychological distress, 120 women were randomly assigned to receive either a fish oil supplement providing 1,200 mg EPA + DHA or a placebo. The baseline level of hot flashes was an average of 2.8 per day. After eight weeks, the hot flash frequency decreased by an average of 1.58 per day (a 55% drop) in the fish oil group but by only 0.50 per day in the placebo group (25%). There was also a greater responder rate in the EPA + DHA group (58.5%) compared with the placebo group (34.4%).24
Vitamin C and Flavonoids. Combined with vitamin C, hesperidin and other citrus flavonoids may be effective in relieving hot flashes. In one clinical study, 94 women suffering from hot flashes were given a formula containing 900 mg hesperidin, 300 mg hesperidin methyl chalcone (another citrus flavonoid), and 1,200 mg vitamin C per day.25 At the end of one month, hot flashes were significantly reduced in 53% of the patients and reduced in 34%. Improvements in nocturnal leg cramps, nosebleeds, and easy bruising were also noted. The only side effect was a slightly offensive body odor with a tendency for the perspiration to discolor the clothing.
Perhaps more useful than hesperidin are preparations containing procyanidolic oligomers (PCOs) such as extracts from grape seeds or pine bark. In a double-blind study, 230 perimenopausal Taiwanese women ages 45 to 55 were given either a placebo or 100 mg PCOs from pine bark (Pycnogenol) twice per day for six months.26 Compared with the placebo, PCOs significantly improved both the severity and the frequency of problems relating to depression, vasomotor symptoms, memory, anxiety, sexual function, and sleep as soon as one month after the treatment was started.
Gamma-Oryzanol. Gamma-oryzanol (ferulic acid) is a growth-promoting substance found in grains and isolated from rice bran oil. In the treatment of hot flashes, its primary action is to enhance pituitary function and promote endorphin release by the hypothalamus. Gamma-oryzanol was first shown to be effective in menopausal symptoms, including hot flashes, in the early 1960s.27 Subsequent studies have further documented its effectiveness.28
In one of the earlier studies, 8 menopausal women and 13 women whose ovaries had been surgically removed were given 300 mg per day of gamma-oryzanol. At the end of the 38-day trial, more than 67% of the women had a 50% or greater reduction in menopausal symptoms.27 In a later study, the benefit of a 300 mg dose of gamma-oryzanol was even more effective, in that 85% of the subjects reported improvement in menopausal symptoms.28
Gamma-oryzanol is an extremely safe natural substance. No significant side effects have been produced in experimental and clinical studies. In addition to being helpful in improving the symptoms of menopause, gamma-oryzanol has also been shown to be quite effective in lowering blood cholesterol and triglyceride levels.29
Vitamin E. In the late 1940s, several clinical studies found vitamin E to be effective in relieving hot flashes and menopausal vaginal complaints compared with a placebo.30–32 Unfortunately, there have been no further clinical investigations. In one study, vitamin E supplementation was shown to improve not only those symptoms but also the blood supply to the vaginal wall when taken for at least four weeks.30 A follow-up study published in 1949 demonstrated that vitamin E (400 IU per day) was effective in about 50% of postmenopausal women with atrophic vaginitis.31 Vitamin E oil, creams, ointments, or suppositories can be used topically to provide symptomatic relief of atrophic vaginitis. Vitamin E may be effective in relieving the dryness and irritation of atrophic vaginitis as well as other forms of vaginitis.32
Botanical Medicines
There are a number of botanicals with a long history of use in menopausal women. Rather than exerting a drug-like effect, these substances are thought to nourish and tone the female hormonal system and reproductive organs. Much of their effect is thought to be a result of phytoestrogens in the plants as well as the plants’ ability to improve blood flow to the reproductive organs. This nonspecific mode of action makes many of these botanicals useful in a broad range of conditions.
Phytoestrogen-containing herbs offer significant advantages over the use of estrogens in the treatment of menopausal symptoms. Although both synthetic and natural estrogens may pose significant health risks, phytoestrogens have not been associated with these side effects. In fact, epidemiological data and experimental studies have demonstrated that phytoestrogens are extremely effective in inhibiting breast tumors, not only because they occupy estrogen receptors but also through other, unrelated anticancer mechanisms (see the chapter “Breast Cancer [Prevention]”).
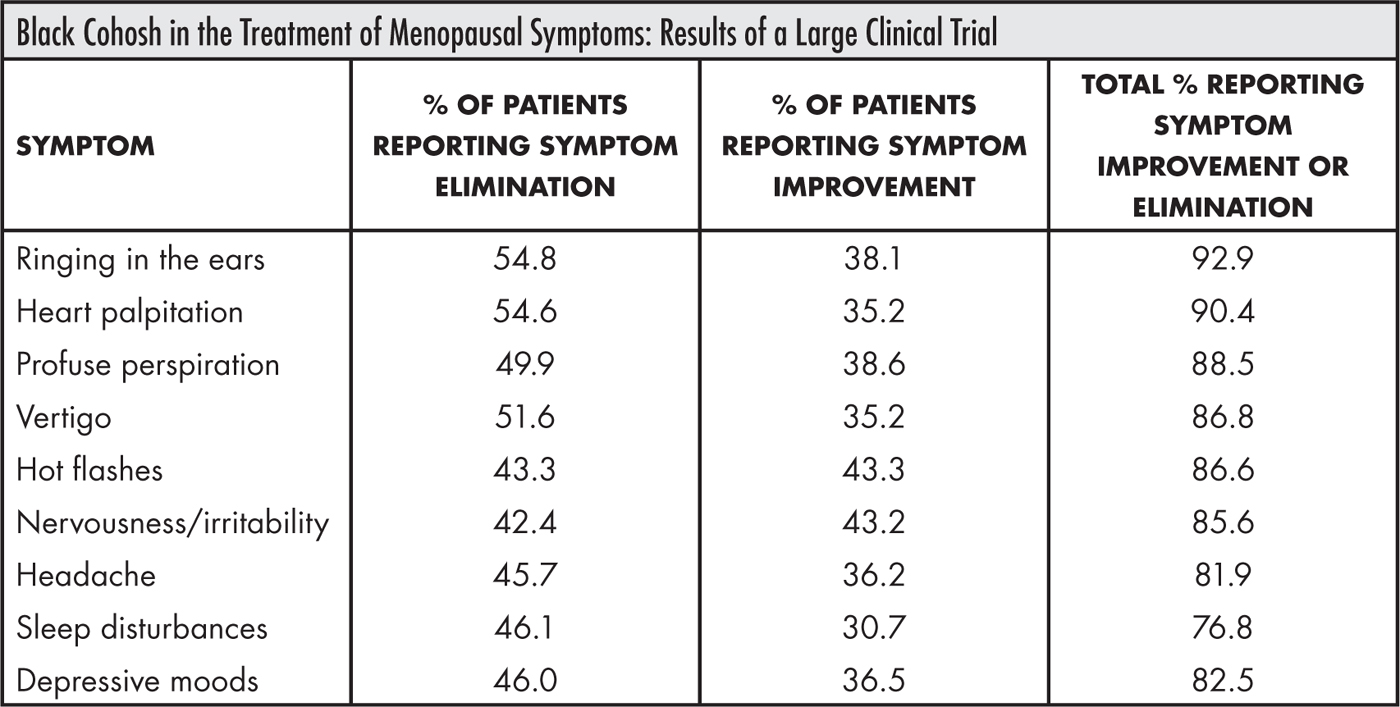
Black Cohosh. In the last 30 years, black cohosh (Cimicifuga racemosa) has emerged as the most frequently studied of the herbal alternatives to hormone replacement therapy for menopausal symptoms. The collective findings of studies involving black cohosh and long-term clinical anecdotal evidence indicate that it is most effective for hot flashes (both during the day and at night), mood swings, sleep disorders and body aches.33
In one of the largest studies, 629 women with menopausal complaints were treated with black cohosh.34 As early as four weeks after the therapy began, a clear improvement in the menopausal ailments was seen in approximately 80% of the women. After six to eight weeks, symptoms completely disappeared in approximately 50%.
In perhaps the most detailed double-blind study to date, black cohosh extract was evaluated for its effect on menopausal symptoms, bone metabolism, and the lining of the uterus (endometrium).35 The 62 postmenopausal women were treated either with black cohosh extract (40 mg per day), 0.6 mg conjugated estrogens, or a placebo for three months. Results indicated that the black cohosh extract was equal to the conjugated estrogens and superior to the placebo in reducing menopausal complaints. Both black cohosh extract and the conjugated estrogens produced beneficial effects on bone metabolism, but the black cohosh extract had no effect on endometrial thickness, which was significantly increased by the conjugated estrogens (increased endometrial thickness is associated with a higher rate of uterine cancer). Vaginal superficial cells were increased with both black cohosh and conjugated estrogens. These results seem to confirm that black cohosh extracts contain substances with selective estrogen-receptor-modifying activity—that is, it shows positive effects in the brain/hypothalamus, bone, and vagina, but has no cancer-causing effects on the uterus.
Some recent studies have used black cohosh extract in combination with other botanical extracts. For example, healthy perimenopausal women who had typical symptoms and had not been on HRT for at least the previous three months were given black cohosh extract equivalent to 1 mg terpene glycosides and Saint-John’s-wort extract equivalent to 0.25 mg hypericin.36 Hot flash symptom scores at 4 and 12 weeks were significantly lower in the treatment group compared with the placebo group, though vaginal dryness and low libido did not improve.
A clinical trial involving 125 menopausal women showed that a combination of 40 mg black cohosh extract, 12 mg isoflavones from red clover, 60 mg isoflavones from soy, 30 mg chasteberry extract, 250 mg valerian extract, and 121 mg vitamin E resulted in a significant lowering of menopausal symptoms after four and six months.37 These results suggest that it may take considerable time before women experience relief from black cohosh and other herbal approaches to menopausal symptoms.
Maca. Maca (Lepidium meyenii) is an herbal remedy from Peru most often thought of as enhancing male sexuality, but it also has effects on women. Research on menopausal women indicates that unlike HRT and phytoestrogenic botanicals, maca can increase the body’s production of estrogen—vs. simply adding estrogen replacement to the body—and reduce levels of cortisol.38 What makes this especially interesting is that the herb appears not to contain plant estrogens or hormones.39,40 It has been suggested that maca’s therapeutic actions rely on plant sterols stimulating the hypothalamus, pituitary, adrenal glands, and ovaries, and therefore also affecting the thyroid and pineal gland. Thus maca tends to work on all of a woman’s menopausal symptoms instead of on any one specific symptom alone, such as hot flashes.
In one double-blind, randomized, four-month study of women in early a postmenopause, patients were given either a placebo or two 500-mg capsules of Maca-GO twice per day for a total of 2g per day.38 After two months, estrogen (specifically estradiol) production had increased and FSH and cortisol had decreased. The maca also had a small effect on increasing bone density and alleviated numerous menopausal symptoms including hot flashes, insomnia, depression, nervousness, and diminished concentration.
Another double-blind trial of 14 postmenopausal women was completed using 3.5 g of powdered maca for 6 weeks or a placebo for 6 weeks.41 Measurements of estradiol, FSH, LH, and sex-hormone-binding globulin were taken at baseline and weeks 6 and 12. There were no changes in hormone levels, but there was a significant reduction in anxiety, depression, and sexual dysfunction with maca consumption compared with the baseline and the placebo.
Red Clover. Red clover (Trifolium praetense), a member of the legume family, has been used worldwide as a source of hay for cattle, horses, and sheep and by humans as a source of protein (leaves and young sprouts). Historically, it has also been recognized as a medicinal plant for humans and, more recently, as a menopausal herb. The principal effective substances in red clover are isoflavones and coumestans.
At least six clinical trials have been conducted on the effect of red clover isoflavones on vasomotor symptoms; about half show benefit and the others do not.42 To have an effect, red clover isoflavones probably require the same sort of healthful gut flora discussed above under “Soy Products.” In fact, the inconsistent results with red clover are very similar to those seen with soy. The first two published studies on red clover and hot flashes showed no statistically significant difference between the red clover standardized extract and a placebo during a three-month period, although both groups did improve.43,44 Two other studies using 40 mg standardized extract of red clover showed good effects. In the first study red clover extract produced a 75% reduction in hot flashes after 16 weeks in 30 women.45 In the second study the red clover group had a 54% reduction in hot flashes after two months vs. a 30% reduction in the placebo group.46 Two more recent studies continue the contradictions. In the first study, 80 mg isoflavones per day resulted in a significant reduction in hot flashes as compared with baseline.47 Another recent study compared two different doses of red clover isoflavones (82 mg and 57 mg per day) with a placebo for 12 weeks, and no difference was observed between the groups.48
Dong Quai. Dong quai (Angelica sinensis) is one of the most famous herbal remedies in China, where it is often referred to as “female ginseng.” By far the most popular use of dong quai is in the treatment of menopausal complaints. Although a double-blind, placebo-controlled study in women showed no significant benefit, the preparation used (a dried aqueous extract) was clearly lacking some of the important volatile compounds, though it was standardized for ferulic acid content.49 In addition, traditionally angelica has been used in combination with other plants. A study conducted in China showed that a combination of A. sinensis, along with other herbs (Paeonia lactiflora, Ligusticum monnieri, Atractylodes chinensis, Sclerotium poriae, and Alisma orientalis) was effective in roughly 70% of women experiencing menopausal symptoms.50 Though not double-blind, this study shows promise for using angelica in combination with other compounds in the management of menopausal symptoms. Also, in a double-blind study, the combination of 100 mg dong quai extract, 60 mg soy isoflavones, and 50 mg black cohosh extract significantly reduced menstrual migraines.51
Saint-John’s-Wort. Saint-John’s-wort (Hypericum perforatum) extract research has focused on the area of mild to moderate depression. Several studies of menopausal symptoms have also been conducted. A recent randomized, double-blind, placebo-controlled clinical trial studied Saint-John’s-wort in perimenopausal/menopausal hot flashes.52 Fifty women (average age 50) received 20 drops three times per day of Saint-John’s-wort extract (hypericin 0.2 mg/ml) and 50 women received a placebo. Clinical exams and interviews were performed at baseline, four weeks, and eight weeks. In women taking Saint-John’s-wort, the frequency of hot flashes began to decline during the first month and showed more improvement during the second month. The decline in duration and severity of hot flashes was statistically significant at week eight and the decline was much more evident in the Saint-John’s-wort group.
Another double-blind randomized clinical trial studied the effect of Saint-John’s-wort extract on the symptoms and quality of life of 47 symptomatic perimenopausal women age 40 to 65 with three or more hot flashes per day.53 Women were randomly assigned to receive a Saint-John’s-wort extract (900 mg three times per day) or a placebo. After 12 weeks of treatment, a nonsignificant difference in favor of the Saint-John’s-wort group was observed in daily hot flash frequency and hot flash score. After three months of treatment, women in the Saint-John’s-wort group reported significantly better quality-of-life scores and significantly fewer sleep problems compared with the placebo group.
One study of women with menopause symptoms using 900 mg Saint-John’s-wort extract for 12 weeks found that about three-quarters of the women experienced improvement in both psychological and psychosomatic menopausal symptoms as well as a feeling of sexual well-being.54 And several double-blind studies (described above) have used a combination of Saint-John’s-wort and black cohosh extract.
For information on possible drug interactions with Saint-John’s-wort, see the chapter “Depression.”
![]()
QUICK REVIEW
• In many parts of the world, most women do not experience the symptoms associated with menopause in the United States.
• Social and cultural factors contribute greatly to how women react to menopause.
• In the United States, 65 to 80% of menopausal women experience hot flashes to some degree.
• Women with atrophic vaginitis (vaginal drying and irritation due to lack of estrogen) should avoid substances that tend to dry the mucous membranes, including antihistamines, alcohol, caffeine, and diuretics.
• Rather than use estrogens to artificially counteract the symptoms of menopause, the natural approach focuses on improving physiology through diet, exercise, nutritional supplementation, and the use of botanical medicines.
• Regular exercise may reduce hot flashes.
• An especially important dietary recommendation in the relief of hot flashes and atrophic vaginitis, as well as the prevention of breast cancer, is to increase consumption of foods rich in phytoestrogens.
• Several nutrients have been shown to be effective in relieving hot flashes and atrophic vaginitis in clinical studies, including fish oils; hesperidin (a flavonoid) in combination with vitamin C; pine bark extract; gamma-oryzanol; and vitamin E.
• Black cohosh extract is the most widely used and thoroughly studied herbal alternative to hormone replacement therapy in menopause.
• Saint-John’s-wort extract improves mood and sleep quality and reduces anxiety in menopause.
EstroG. EstroG is an herbal product containing a mixture of standardized extracts of Cynanchum wilfordii, Phlomis umbrosa, and Angelica gigas that has shown favorable results in clinical studies. In the most detailed double-blind study, 64 pre-, peri-, and postmenopausal women were randomly assigned to take either EstroG (517 mg per day) or a placebo for 12 weeks.55 Menopausal symptoms were evaluated with the Kupperman menopause index (KMI) that includes 11 symptoms. After 12 weeks the mean KMI score was significantly reduced in the EstroG group, from 29.5 at baseline to 11.3, while there was no significant change in the placebo group. Statistically significant improvement in vaginal dryness in the EstroG group was also observed.
![]()
TREATMENT SUMMARY
Menopause is a normal and natural part of aging and each woman experiences it in her own unique way. However, premature menopause, surgical menopause, or medication-induced menopause is not normal, and the benefits and risks should be addressed individually under the guidance of a physician.
Many natural measures can help alleviate the most common symptoms of menopause. In most cases, HRT is not necessary to address these symptoms. However, for women at high risk for osteoporosis and women who have already experienced significant bone loss and also have menopause symptoms or do not tolerate osteoporosis medications, hormonal therapy may be indicated. In those circumstances, we definitely favor the use of biodentical hormones over conventional HRT, and we recommend that their metabolites be measured and optimized to maximize estrogens that work against cancer rather than promote it.
Engage in a regular exercise program according to the recommendations in the chapter “A Health-Promoting Lifestyle.”
The guidelines discussed in the chapter “A Health-Promoting Diet” are very much indicated in helping improve menopausal symptoms. Perhaps the most important dietary recommendation may be to increase consumption of plant foods, especially those high in phytoestrogens, while reducing the consumption of animal foods.
• A high-potency multiple vitamin and mineral formula as described in the chapter “Supplementary Measures”
• Key individual nutrients:
![]() Vitamin C: 500 to 1,000 mg per day
Vitamin C: 500 to 1,000 mg per day
![]() Vitamin E (mixed tocopherols): 800 IU per day until symptoms have improved, then 200 to 400 IU per day
Vitamin E (mixed tocopherols): 800 IU per day until symptoms have improved, then 200 to 400 IU per day
• Fish oils: 1,000 mg EPA + DHA
• One of the following:
![]() Grape seed extract (>95% procyanidolic oligomers): 200 to 300 mg per day
Grape seed extract (>95% procyanidolic oligomers): 200 to 300 mg per day
![]() Pine bark extract (>95% procyanidolic oligomers): 200 to 300 mg per day
Pine bark extract (>95% procyanidolic oligomers): 200 to 300 mg per day
![]() Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
Some other flavonoid-rich extract with a similar flavonoid content, super greens formula, or another plant-based antioxidant that can provide an oxygen radical absorption capacity (ORAC) of 3,000 to 6,000 units or higher per day
![]() Gamma-oryzanol: 300 mg per day
Gamma-oryzanol: 300 mg per day
For general symptom relief, one or more of the following:
• Black cohosh extract: equivalent of 2 mg 27-deoxyacteine twice per day
• Maca: 1,000 mg gelatinized maca extract twice per day, or dosage equivalent to 3,500 mg dried powdered maca root per day
• Red clover extract: 40 to 80 mg per day
• Estro-G: 517 mg per day
If symptoms of anxiety or depression are significant, add:
• Saint-John’s-wort extract standardized to 0.3% hypericin 900 to 1,800 mg per day
If symptoms of vaginal atrophy do not respond after two months of treatment with other botanicals, or if you are experiencing menopausal migraines:
• Black cohosh extract (if not previously used): see the dosage levels above
• Soy isoflavones (if no soy in the diet): 45 to 90 mg
• Dong quai (Angelica sinensis)
![]() Powdered root or as tea: 1 to 2 g two or three times daily
Powdered root or as tea: 1 to 2 g two or three times daily
• Tincture (1: 5): 4 ml (1 tsp) two or three times daily
• Fluid extract: 1 ml (1/4 tsp) two or three times daily
• Dry powdered extract: 250 mg two or three times per day