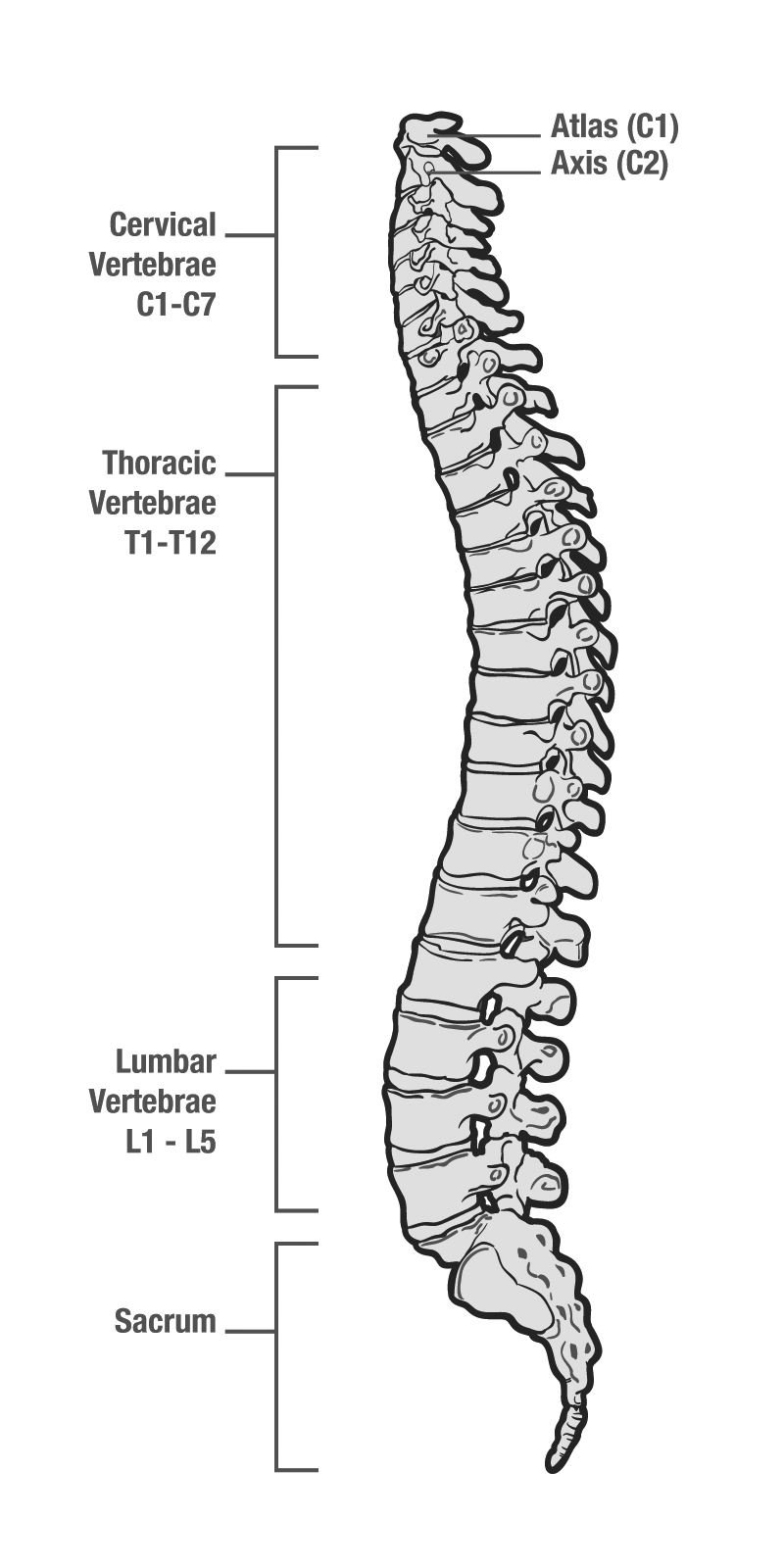
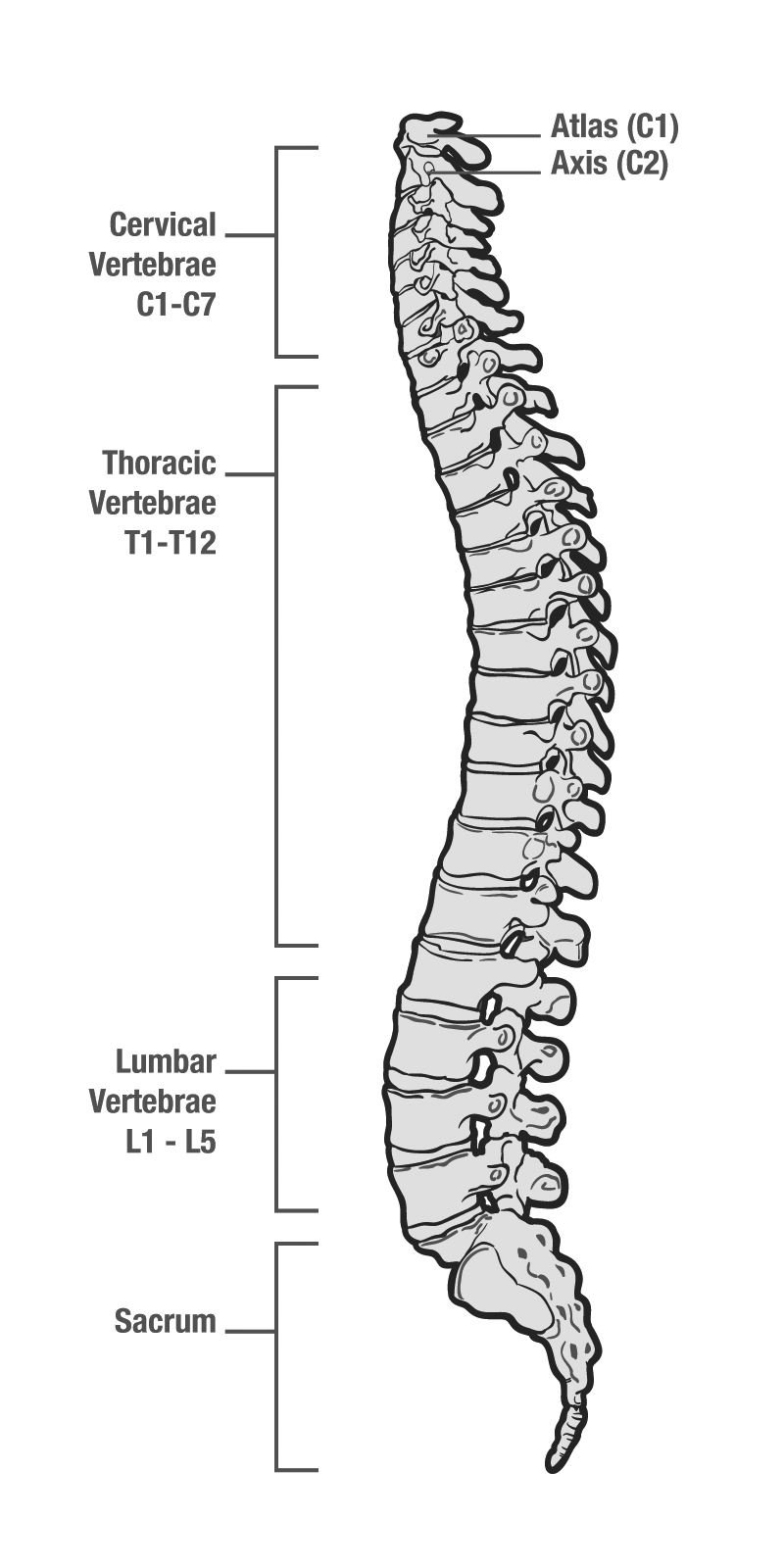
The spine is a series of square or rectangular bones beginning with the first cervical vertebra (spine bone, plural vertebrae) at the base of the skull and extending down through the coccyx (tailbone) (Figure 5-1). Vertebrae differ from other bones discussed in this book in that they are not long bones, like the femur (thigh bone), humerus (upper arm bone), or digits (finger bones). While the long bones of the body are usually used as fulcrums to promote movement around a joint via ligaments, the bones of the spine permit less movement. While there are joints between these bones and there is motion, the range is substantially less than with other joints, and the primary purpose is as much protection of the spinal cord running along these bones as it is movement.
There are seven cervical vertebrae. The seventh of these has a distinctive bump that can be felt at the bottom of the neck. Following the seventh cervical vertebra, there are twelve thoracic vertebrae that generally correspond to the chest level of the torso. Below this are five lumbar vertebrae that make up the lower back. The fifth lumbar vertebra attaches to the sacrum. The coccyx represents a vestigial tail, and consists of three or more small bones that help anchor the pelvis. These bones in sequence are illustrated in Figure 5-1.
Spinal injuries are one of the most feared consequences of a fall or of some object striking a climber. While bony fractures of the spine can be very painful, the greatest fear is of associated injury to the spinal cord, the mechanism by which all nerves communicate with the body below the neck to transmit sensation and motor function. For generations, EMS and climbing medicine authorities have recommended a very conservative approach to identifying spinal injuries and possible threats to the spinal cord. This included immobilization of patients’ spine to prevent causing or exacerbating a spinal cord injury. In many cases, a “mechanism of injury” that might be thought to cause a spinal injury has been enough to warrant immobilization of the spine.
However, in the modern era, emergency medicine and EMS clinical scientists have more extensively explored ways that spinal injuries can best be identified and managed. A major landmark in this research was the publication in 1998—and validation in 2000—of the NEXUS (National Emergency X-Radiography Utilization Study) criteria for cervical spine injury (Hoffman 1998, Hoffman 2000). These criteria identified specific characteristics requiring X-ray imaging of the cervical spine for possible fracture. If none of the findings were present, no X-ray was needed. More than 34,000 patients were enrolled in this study, and only two patients with significant cervical spine injury were missed using the criteria. This meant that the NEXUS criteria were 99.6% effective in ruling out a significant cervical spine injury without the use of any X-ray machinery.
Prior to this, many wilderness medicine schools were teaching techniques to “clear” the spine of injury, but these techniques did not have significant scientific validation. The benefit of the NEXUS Group’s study was the proof that if a specific set of scientifically validated criteria were not present, significant cervical spine injury could be excluded in more than 99% of cases. In these cases, prehospital immobilization would not be helpful, since no further testing would be done at the hospital anyway and all immobilization tools would simply be removed. Fortunately, the NEXUS criteria requires no special equipment and can be applied anywhere, including climbing environments. The criteria can be represented by the mnemonic INDIAN (Hawkins 2010).
I = Intoxication (if patients are intoxicated, their expressions of possible pain, tenderness, or neurological deficit described below cannot be trusted)
N = Neurological deficit (problems with nerve conduction, i.e., numbness or paralysis or weakness in one body part)
DI = Distracting Injury (an injury away from the spine so dramatic or painful that it could distract a climber from possible pain, tenderness, or neurological deficit remote from the more significant-appearing injury)
A = Altered level of consciousness (patients whose level of consciousness is altered or who are confused cannot, as described in intoxication above, reliably express possible pain, tenderness, or neurological deficits)
N = Neck tenderness or pain (technically, according to the criteria, only tenderness, and only on the midline bony parts of the neck, but to be more conservative we would recommend not only tenderness but also any pain)
Other publications followed the NEXUS criteria in emergency medicine literature, including the Canadian c-spine study in 2004 (CCC Study Group 2004) and its out-of-hospital validation in 2009 (Vaillancourt 2009). Together, they contribute to our current understanding that simple physical examination techniques can exclude the possibility of a clinically significant fracture. The term “clinically significant” is important here. A common misunderstanding is that these criteria exclude neck injuries altogether. In fact, they only exclude bony injuries that would result in a change in management; for example, surgery or further immobilization. Radiological technology has improved to the point where even tiny fractures or disruptions can be seen in bones on advanced generations of CT scanning or magnetic resonance imaging (MRI). However, if these injuries do not alter the management of a patient—or require further immobilization or treatment—they are not considered “clinically significant,” and thus also would not require special prehospital precautions. In the opinion of the authors, despite further refinements and suggestions such as algorithms that combine the NEXUS and Canadian C-spine criteria (Weingart 2011), the original NEXUS criteria as embodied in the INDIAN mnemonic remain reliable for the climber to use to determine when a clinically significant spinal fracture can be excluded.
For patients with clinically significant fractures, spinal cord compromise may be present, and this often appears in the form of neurological deficits. Healthcare providers are trained to recognize patterns of various deficits and how they relate to specific injuries. But for climbers without healthcare training, it is enough to know that any new numbness, weakness, or paralysis of a specific body part after a fall or blunt trauma should be presumed to be related to a spinal cord injury unless another source of the deficit is obvious (e.g., numbness in a finger that has a major laceration and no suggestion that the numbness could be from a back or arm injury). Sensory losses may be very specific and subtle, such as isolated loss of ability to tell the position of a body part in space or loss of the ability to sense vibrations.
These clinical research milestones, begun around 2000, help identify situations where a clinically significant spinal injury can be ruled out. About a decade later, a further series of clinical research findings also changed our understanding of the treatment of patients who may have a clinically significant spinal injury.
Traditionally, spinal immobilization techniques (maneuvers to prevent any spinal movement after a suspected injury) were the accepted field intervention for potential spinal fracture. However, researchers are now demonstrating that these techniques rarely succeed in actually immobilizing the spine, and that when spinal immobilization is in fact achieved, the evidence suggests the patient experiences more harm than benefit. This represents a fundamental paradigm change in our wilderness management of trauma, overturns many of the most long-standing teachings about patient immobilization, and, like suspension syndrome (described in Chapter 2), represents a victory of evidence-based medicine over dogma and traditional practice for its own sake without evidence. Chapter 18 discusses these scientific findings in more detail, along with more modern techniques of spinal motion restriction (reducing motion of the spine, usually using pain as a threshold, without specific attempt to completely immobilize). If the identification tools above flag an injury as needing spinal motion restriction, follow the recommendations outlined in Chapter 18.
Any bony injury to the back benefits from analgesia (pain control). If patients do not require spinal motion restriction, analgesia may help a climber become more mobile and functional in their own rescue.
Historically, steroidal medications (particularly methylprednisolone) have been considered to be a standard of care for spinal cord injuries. However, in a very recent change in the medical community, most professional consensus guidelines now discourage or minimize their use, including the Congress of Neurological Surgeons, the American Association of Neurological Surgeons, the American College of Surgeons, and the Canadian Association of Emergency Physicians (Hadley 2013, Chin 2016). They should certainly only be used in the out-of-hospital care of a climber if a professional healthcare provider is specifically prescribing and providing them.
In contrast to the growing amount of skepticism over the benefit of early immobilization, there is growing evidence that early mobilization of patients with spinal injuries may be beneficial (Epstein 2014). A fascinating historical footnote to this concept is the story of Hans Kraus (Schwartz 2015). Kraus was simultaneously one of the premier rock climbers of the twentieth century, putting up many of the first ascents in the Shawangunks in the United States, and one of the premier orthopedic back surgeons of his era, serving as the private back doctor for John F. Kennedy and many celebrities of the mid-twentieth century. Though he was featured on the cover of TIME magazine and twice identified as “Man of the Year” by that publication, his legacy is now largely forgotten. But a key element of his back rehabilitation strategies—frequently used for climbers, skiers, and mountaineers—was the concept of early mobilization, often enhanced with ethyl chloride, a topical numbing analgesic spray still available today.*
A complete discussion of packaging and evacuation of spinally injured patients can be found in Chapter 18. All patients with suspected spinal injuries require evacuation within the context of risk-benefit analysis. Those found to have neurological deficits following a traumatic injury involving the spine need professional medical attention and follow-up. Positive outcomes are often related to the quality of initial surgical/medical attention; however, professional rehabilitation (and compliance with rehabilitation recommendations and regimens) is often equally important, or perhaps even more important, to successful outcomes and return to outdoor sports, including climbing.
* http://www.gebauer.com/ethylchloride