If injured climbers are found in dangerous positions, they must be extricated, presuming such extrication does not expose rescuers to unacceptable risk. Examples of such dangerous locations include rockfall areas, avalanche areas, or swift water.
Extrication often requires technical rescue skills. Climbers expecting that they may have to deliver patient care in environments requiring technical rescue skills should enroll in a class specifically designed to prepare them for operating safely in such terrain. This includes not only high-angle technical rescue training for climbing rescues and avalanche rescue training for avalanche rescues, but also training for other environments more peripheral to the climbing world, such as swift water rescue training for swift water rescues. In the absence of such training, a risk-benefit analysis is essential, with significant weight placed on not putting rescuers in great danger. For example, a tragically high number of all drownings are actually would-be rescuers who are attempting to rescue a patient—as high as 6% of drownings in China (Zhu 2015), and 17 deaths over a five-year period in Australia (Franklin 2011).
Extrication may require short-distance carries and involve consideration of spinal immobilization. Litters and carries are discussed in more detail in Chapter 19, and spinal immobilization and motion restriction were introduced in Chapter 5, with more detail later in this chapter.
For extremely limited short-term movement, the BEAM technique is better than log rolling or ad hoc backboarding for movement. Boissy has shown the BEAM technique reduces spinal movement more than log rolling (Boissy 2011), and BEAM is now the preferred technique recommended by evidence-based Wilderness Medical Society practice guidelines over the log roll (recommendation grade 1C) (Quinn 2014). In the BEAM technique, rescuers interlace arms underneath a patient and move the patient in a raise, lift, and lower sequence.
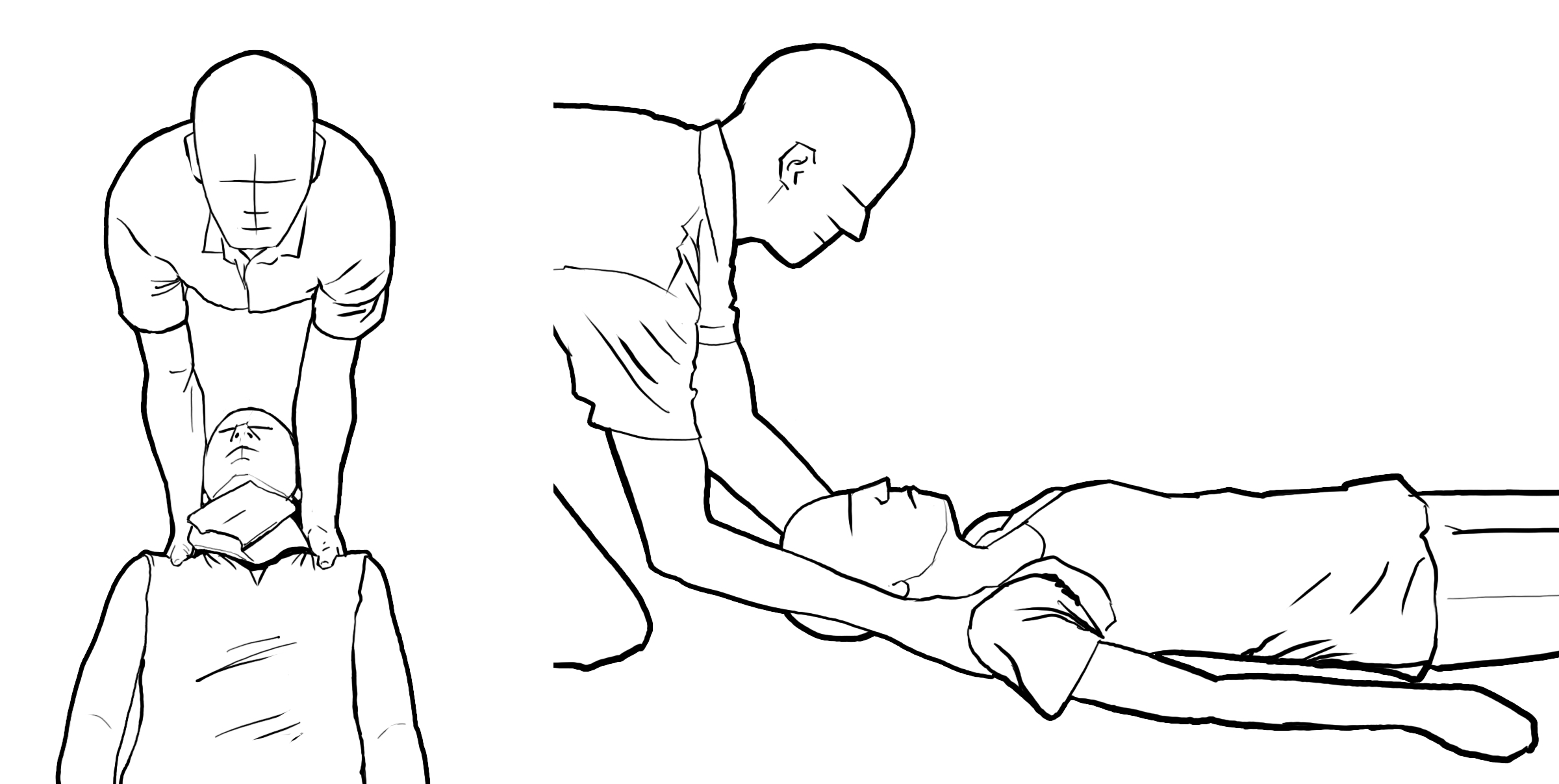
FIGURE 18-1. SPINAL TRAP TECHNIQUE
In addition, research from motor vehicle crashes has shown that, in cases of suspected spinal injury, patients moving themselves (walking) entails less manipulation of the spinal column than immobilization and passive movement of the patient controlled by rescuers (Shafer 2009, Dixon 2013). Thus, potential spinal cord injury patients may be able to take a more active role in their own rescue, reducing spinal movement based on their own pain rather than undergoing active spinal immobilization by a rescuer.
If immobilization or significant spinal motion restriction is desired of the cervical spine, Wilderness Medical Society practice guidelines (based on Boissy’s work) also recommend a “trap” method utilizing engagement of the trapezius muscle, illustrated in Figure 18-1, over the more traditional hands-to-the-ears cervical spine immobilization method traditionally taught (recommendation grade 1C) (Boissy 2011, Quinn 2014).
In wilderness medicine, the decision to evacuate a patient to a higher level of care is often more complex than in a frontcountry or urban environment. There may be more consequences or risks to a decision to seek higher medical care than in the frontcountry. Examples of significant consequences include abandoning an expedition already underway or splitting up a group and its resources. Examples of increased risk include the hazards to a group as they attempt to evacuate a patient, hazards to rescuers if deploying a high risk rescue resource like a helicopter, or hazards in attempting routes or environments that would not normally be engaged were an evacuation not necessary.
Medical decision-making regarding evacuation and seeking better medical care is also somewhat different in a wilderness setting. Measuring the risks and benefits of an evacuation may suggest that ailments for which healthcare would normally be sought—such as a toothache or a fever—might be managed entirely in the field, since the risks of evacuation might exceed the benefit. But other conditions that could more likely deteriorate—such as severe abdominal pain or an infected wound—might be evacuated for medical care at a lower threshold than that for which medical care would be sought in a frontcountry situation. Furthermore, climbing groups and expeditions often take medical supplies and providers with them on trips. The scope and sophistication of such supplies and providers often increase with the length or complexity of the planned expedition. Clearly, the medical supplies and training available on-site influences the decision whether or not to evacuate. See Appendix A for a more complete discussion of medical kits and equipment for various environments and trip lengths.
Whereas seeking medical care in the frontcountry is one of the simplest decisions, with minimal consequences and multiple opportunities for reconsideration, it is one of the most complex decisions in the wilderness, with significant consequences, including the potential for activating multiple additional wilderness rescuers. Individual chapters in this book discuss the thresholds for evacuation for various conditions. The remainder of this chapter will discuss how to evacuate a patient once that decision has been made.
Historically, the decision about whether an injured patient requires spinal immobilization has been a crucial element in the medical decision-making that calculates the risks and complexity of evacuation and also the technical expertise needed to actually prepare a patient for evacuation.
Following traditional EMS instruction since the 1970s, wilderness medical providers were taught to spinally immobilize anyone with a possible back or neck injury.
In the ensuing years, two major forces began to influence emergency medical services (EMS) decisions about spinally immobilizing patients. These forces reflected growing sophistication of both hospital-based emergency medicine and wilderness medicine as medical subspecialties.
On the one hand, in hospitals, emergency medicine practitioners began to scrutinize the time, cost, and radiation exposure to the patient associated with trauma radiological studies. Seeking ways to reduce unnecessary testing, they explored protocols that might permit them to rule out spinal injury without radiological testing. The NEXUS and Canadian C-spine criteria evolved out of this effort. As discussed in Chapter 5, these guidelines can effectively rule out clinically significant spinal fractures and injuries.
On the other hand, in wilderness-based environments where patients were receiving treatment prior to traditional EMS care, providers realized that applying such rules could help to avoid unnecessary immobilization and its additional complexities and risks to a wilderness operation. Put simply, if a patient with a neck or back injury would not undergo any testing or further intervention beyond pain control in the hospital, then no immobilization is needed prior to that hospital care either. Utilizing this principle, wilderness medical practitioners have, for decades, avoided spinal immobilization of patients who would have been immobilized by traditional EMS providers. Although historically this practice was called “clearing the spine,” more modern terminology is “selective spinal immobilization,” acknowledging that field providers without radiological equipment cannot truly “clear” a patient of a spinal injury. They can only selectively decide when to immobilize or not.
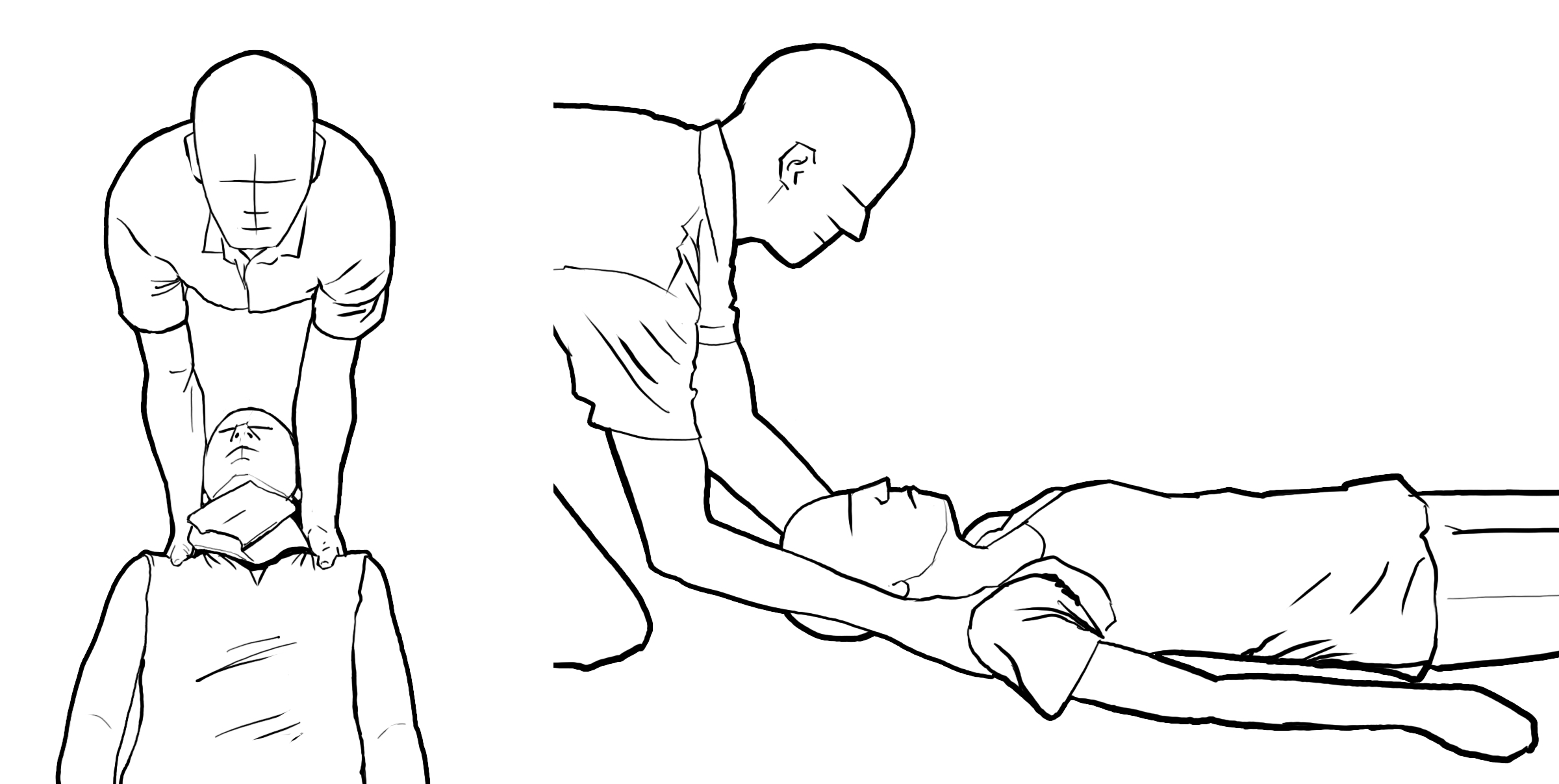
However, the most current evidence in the emergency medicine, EMS, and wilderness medicine communities suggests that field spinal immobilization of any sort, in any patient, is likely to be not only unnecessary, but possibly even harmful. This is a dramatic and challenging change for anyone with field trauma training. Hauswald has been one of the leading authors and researchers on this topic, and has published truly heroic works challenging the existing paradigm. In 1998 he showed that, controlling for injury severity, patients in Bangladesh who were not backboarded had lower incidents of neurological deficits than backboarded patients in Albuquerque (Hauswald 1998). However, his tour de force was the publication of “A Reconceptualisation of Acute Spinal Care” (Hauswald 2013). This work, using basic Newtonian physics and actual cadaver research, demonstrates why spinal immobilization as a goal is likely flawed in the first place. As Figure 18-2 demonstrates, most vertebral fractures are unlike long bone fractures, and his cadaver research showed movement of fractured bones was unlikely to cause additional spinal trauma unless similar forces were applied as the ones causing the injury in the first place (i.e., normal physiological movement should not be dangerous). His seminal work in these and other publications, along with that of many other researchers and EMS physicians, has led most major professional societies and many wilderness training programs—including the National Association of EMS Physicians, the American College of Surgeons Committee on Trauma, the Wilderness Medical Society, the American College of Emergency Physicians, and the Wilderness EMS Medical Director Course—to adopt guidelines discouraging spinal immobilization in out-of-hospital medical care. (NAEMSP/ACS 2013, Quinn 2014, ACEP 2015, WEMSMDC 2017). Many frontcountry EMS systems, including some entire American state EMS systems, have discontinued use of backboards altogether as medical tools (although they are sometimes still used as extrication tools).
FIGURE 18-2. VERTEBRAL FRACTURES
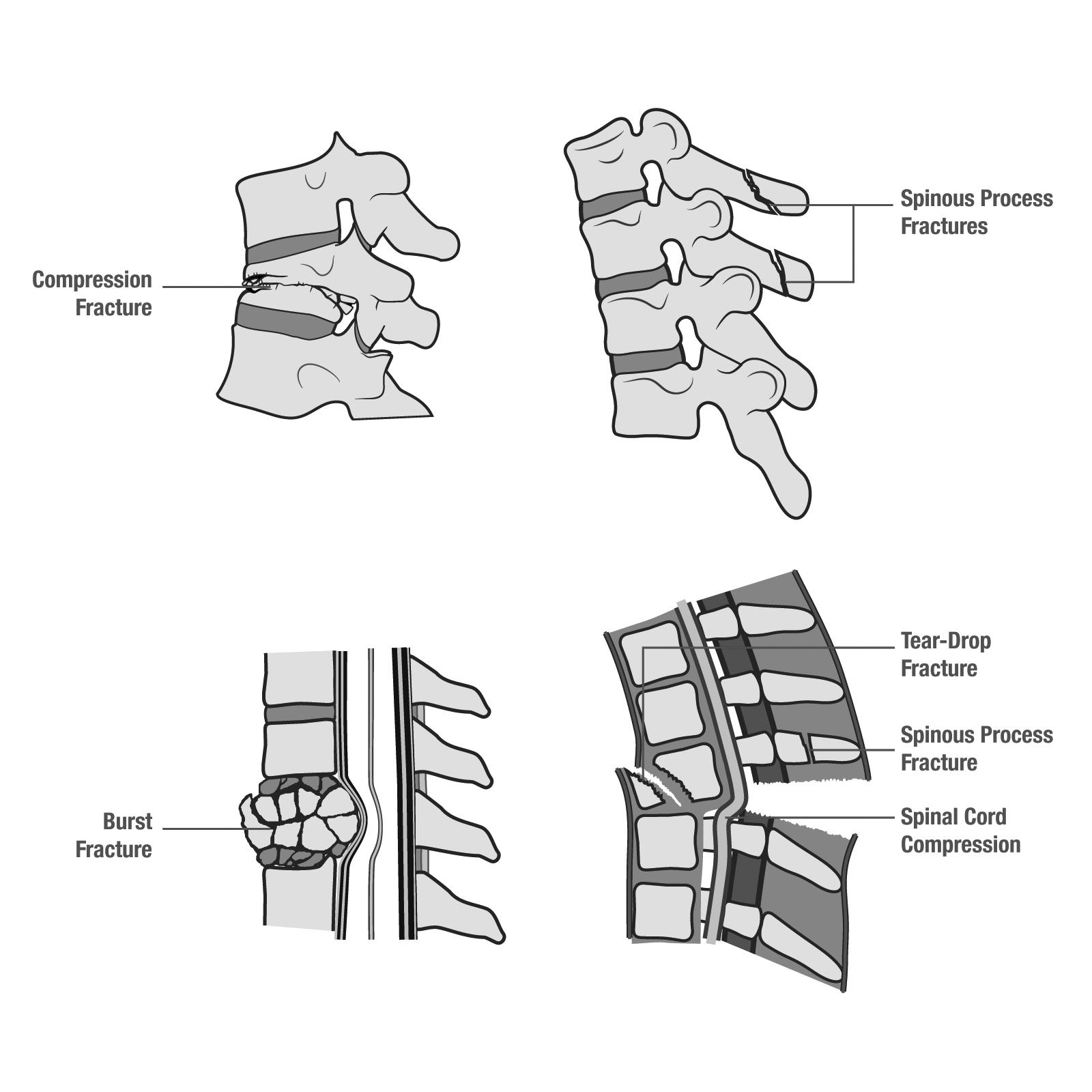
FIGURE 18-3. C-SPINE FRACTURES/COLLAR PROBLEM
Left: Normal physiology showing normal C1-C2 (top) and normal spine curvature (bottom).
Right: Collar effect showing cervical vertebral separation (top) and spasmed/straightened loss of curvature (bottom).
Furthermore, concerns have been raised about rigid cervical collars as immobilization tools (Bledsoe 2015). First, cervical collars have been shown to be poor immobilizers of the cervical vertebrae (Hughes 1998, Perry 1999, Holla 2012, Sundstrøm 2014). Second, to the degree they do immobilize it, they replicate spasm physiology (Figure 18-3). Since it is now believed that inflammation and spasm are more responsible for secondary neurological damage than physical cord compression via movement, any spasm or inflammation caused by unnatural neck positioning may be worse than normal physiological movement. Third, high cervical vertebral fractures (at the C1 and C2 level, often considered to be particularly dangerous neck fracture) have been shown to be pulled apart in potentially dangerous ways more significantly when cervical collars are applied (Ben-Galim 2010). These concerns are illustrated in Figure 18-3. Fourth, cervical collars can restrict breathing (Goutcher 2005) and increase brain pressure (Davies 1996, Mobbs 2002), both potentially dangerous after major trauma. Wilderness EMS (WEMS) authorities have recommended that WEMS teams deploying to climbing incidents, including mountain rescue teams, should not routinely apply rigid cervical collars, either commercial or improvised, to patients (Smith 2018).
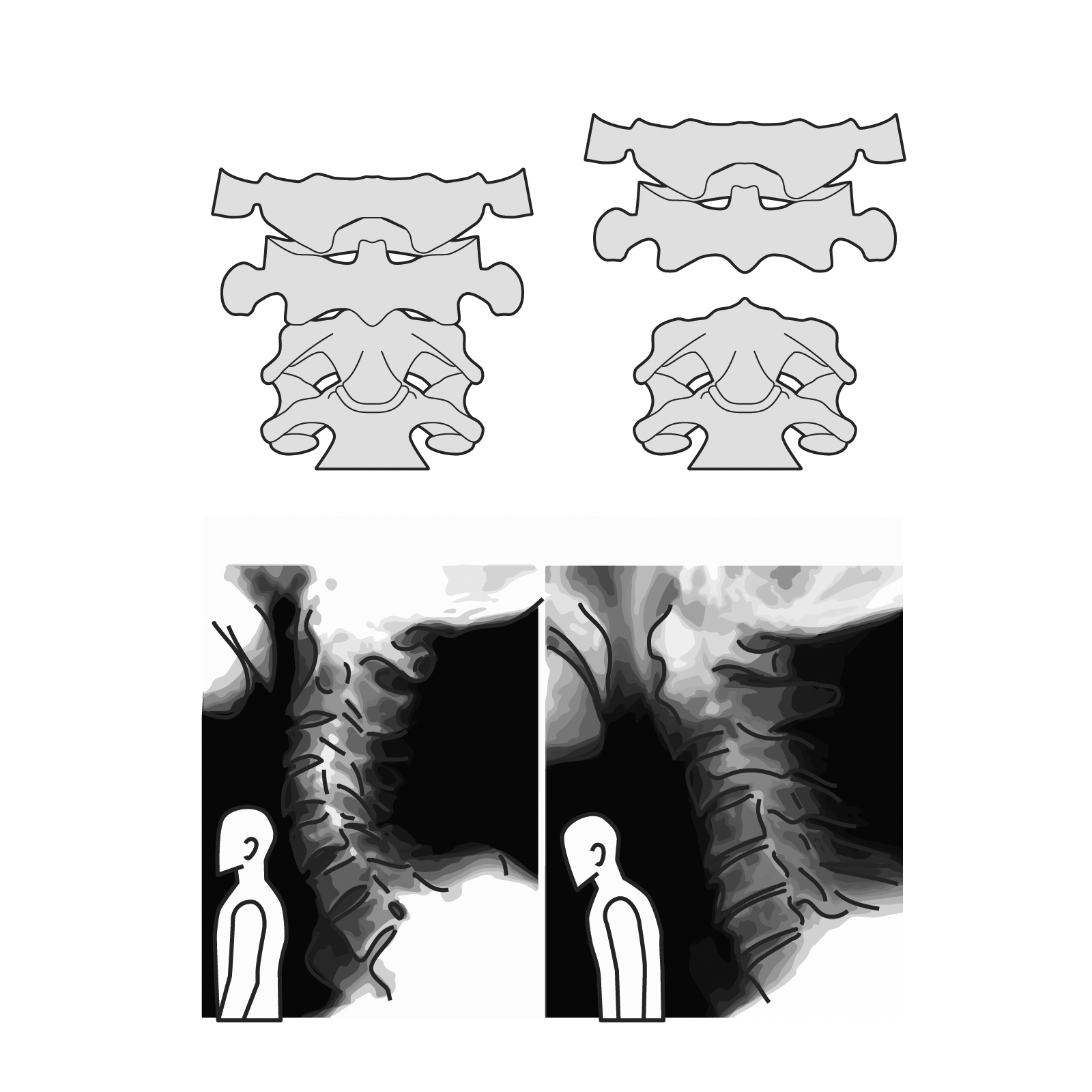
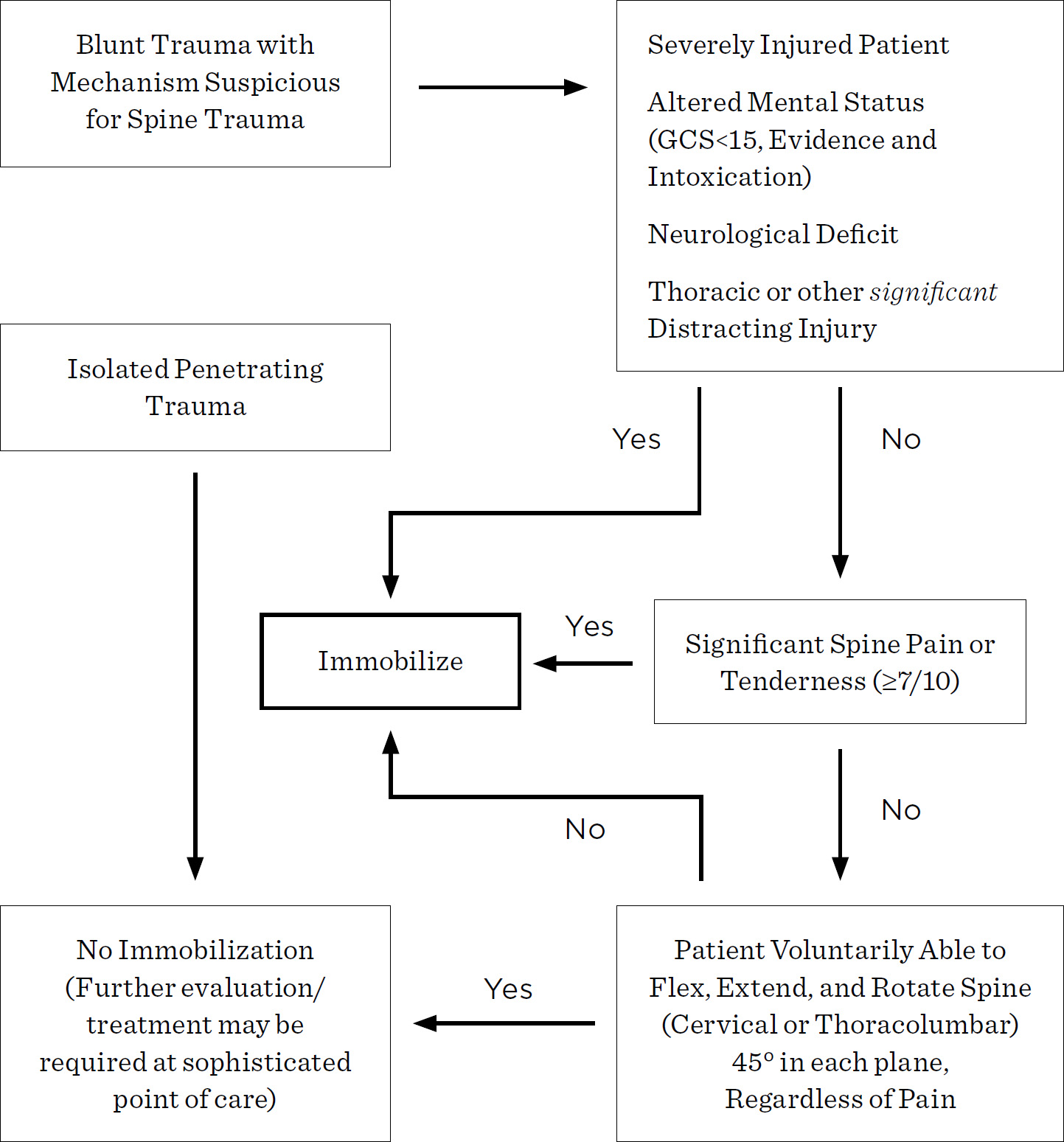
FIGURE 18-4. WILDERNESS MEDICAL SOCIETY RECOMMENDATIONS FOR SPINAL EVALUATION AND IMMOBILIZATION IN THE AUSTERE ENVIRONMENT
On the basis of this evidence, it is our conviction that formal or ad hoc backboards and full “immobilization” should be used only for extrication from a technical entrapment and not for transport. We disagree with the philosophy that spinal immobilization is a desirable goal in cases of potential spinal injury, and instead believe that interventions should be taken to reduce spinal motion rather than to fully immobilize it.
In medicine, the standard of care (and medicolegal standard) sometimes lags behind medical evidence and contemporary medical science. We recognize that many certification courses, such as Advanced Wilderness Life Support and many wilderness EMS certifications (Wilderness First Responder, Wilderness EMT, etc.), still teach algorithms for selective spinal immobilization. For those who still wish to apply selective spinal immobilization, we would recommend implementing the Wilderness Medical Society’s algorithm for spinal immobilization, outlined in Figure 18-4 (Quinn 2014).