61
Bone and joint disorders
Congenital abnormalities of the hip and feet
Developmental dysplasia of the hip, DDH
Hip is dislocatable, dislocated and/or has shallow acetabulum.
Incidence
- 6 per 1000 live births have abnormal clinical examination on screening.
- 0.5–2 per 1000 live births are treated.
Risk factors, clinical examination and initial management
These are described in Chapter 17.
Treatment
- Pavlik harness for 1–3 months (Fig. 61.1):
- – maintains flexion and abduction and limits adduction
- – redirects femoral head towards acetabulum.
- Orthoses or open reduction and derotation femoral osteotomy may be required.

Fig. 61.1 Pavlik harness for treatment of developmental dysplasia of the hip.
Outcome
- 80–95% identified on screening do not need surgery.
- 5% of treated cases develop avascular necrosis (ischemic damage) of the femoral head.
- Impact of neonatal screening on need for surgery is uncertain.
Talipes equinovarus
Anatomy
Foot held in rigid equinovarus position (Fig. 61.2a and b). Needs to be distinguished from positional talipes (see Chapter 21).
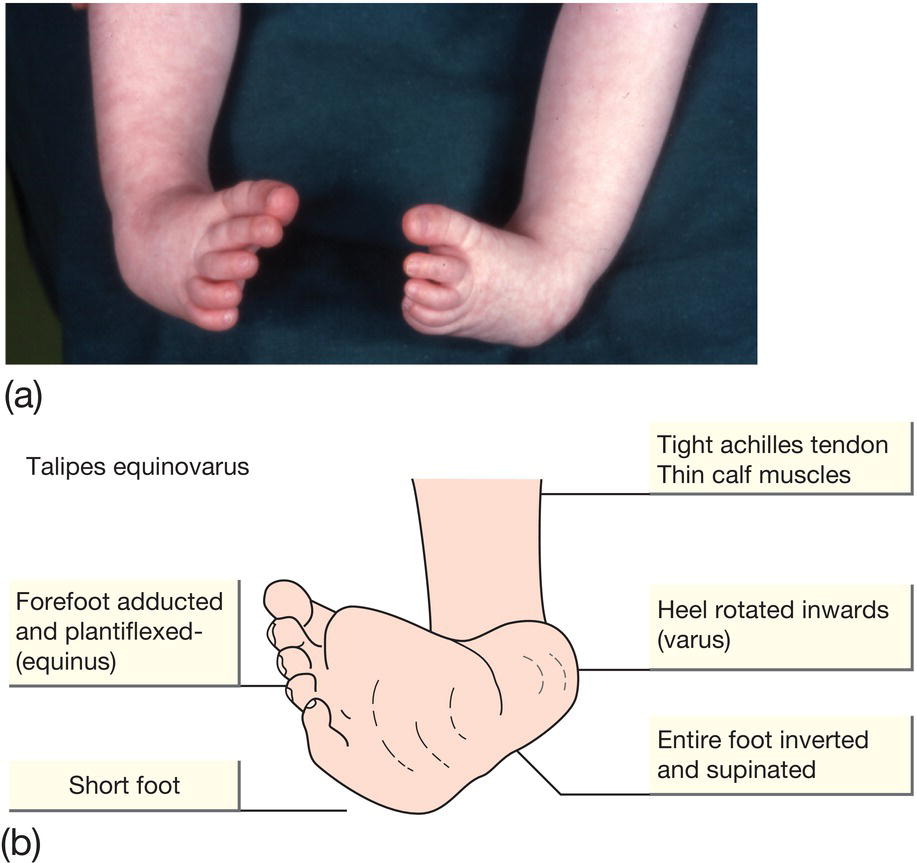
Fig. 61.2 (a and b) Talipes equinovarus. The foot is inverted and supinated and the forefoot is adducted. The affected foot is shorter and the calf muscles thinner than normal. The position of the foot is fixed and cannot be corrected by passive manipulation.
Incidence
1 in 1000 live births. Bilateral in 50%.
Risk factors
- Multifactorial inheritance.
- 3–4% risk if affected parent.
- 2% risk for subsequent siblings.
- May be secondary (20%):
- – oligohydramnios
- – neuromuscular disorder, e.g. spina bifida
- – malformation syndrome.
- May be associated with developmental dysplasia of the hip, but this has recently been questioned.
Management
- Refer to orthopedic surgeon as soon after birth as possible.
- Ponseti regimen now followed worldwide as highly successful and avoids surgical correction:
- Initially, foot is manipulated into the maximum position of correction and held in a plaster cast (Fig. 61.3). Changed regularly to correct deformity of the midfoot and forefoot.
- If foot still in equinus position, Achilles tenotomy performed.
- If correction is complete, “boots and bar” to hold feet abducted, externally rotated and dorsiflexed, worn all the time for about 3 months, then at night until 4 years old.
- Monitor for recurrence. Tibialis anterior tendon transfer may be required for supination of the forefoot.
- Foot should be supple and corrected; may be smaller and calf thinner than unaffected side.

Fig. 61.3 Treatment of talipes equinovarus with serial plaster casts.
(courtesy of Mr Brian Scott)
Infection
Septic arthritis
- Rare in newborn.
- Usually via extension from underlying bone infection, rather than primary infection of the joint but can be from hematogenous spread.
Signs
- Decreased joint movement.
- Joint is swollen, warm, red (Fig. 61.4). Effusion may be present.
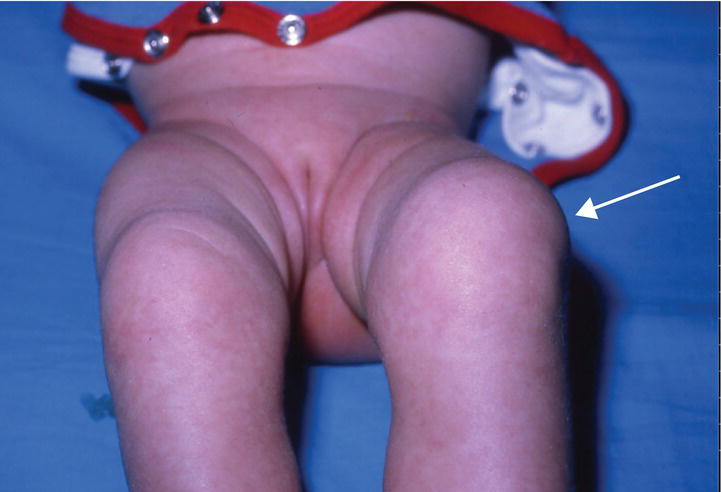
Fig. 61.4 Septic arthritis showing swollen left knee (arrow).
Diagnosis
Joint aspiration for cell count, >50 000 white blood cells/mm3 (>50 white blood cells × 109/L), Gram stain, culture.
Imaging
- Ultrasound – fluid in joint space.
- Radionuclide bone scan, if indicated – hot spot.
- MRI scan of bone if necessary.
Plain X-ray is of limited value – may show widened joint space.
Treatment
- Single or repeated joint aspiration.
- Surgical drainage of hip joint if no improvement.
- Antibiotics – prolonged course for 3–6 weeks.
Long-term complications
- Erosion of articular surface. Joint ankylosis.
Osteomyelitis
- Rare in newborn.
- Most are hematogenous in origin, in metaphysis.
- Usually presents within first 2 weeks of life.
Pathogens
Commonest are Staphylococcus aureus and streptococci.
Signs
- No movement (pseudoparalysis) of limb.
- Red, warm, swollen, painful limb.
Diagnosis
- Blood culture positive.
- Bone aspiration for cultures if indicated.
Imaging
- Ultrasound – periosteal elevation and soft tissue swelling.
- Radionuclide bone scan, if indicated – hot spot (needle aspiration does not produce positive bone scan).
- Plain X-ray – limited use at this stage, as only shows periosteal elevation and soft tissue swelling.
- MRI scan of bone if necessary.
Treatment
Antibiotics – prolonged course for approximately 6 weeks. Continued for 2–3 weeks after symptoms resolve and CRP normalizes.
Skeletal dysplasias
There are several hundred, with shortening of the limbs and spine resulting in short stature.
Achondroplasia
- Short bowed limbs, normal trunk, large head.
- Midface hypoplasia, frontal bossing.
- Trident hand (short and broad), protuberant abdomen.
Osteogenesis imperfecta
- Inherited disorder of type 1 collagen formation.
- Rare – 1 in 20 000 live births.
Clinical features
- Increased bone fragility, susceptibility to fracture from mild to lethal, depending on sub-type (Fig. 61.3), scoliosis and kyphosis.
- Blue sclerae, defective tooth formation in some patients.
- Hearing loss.

Fig. 61.5 X-ray of osteogenesis imperfecta showing multiple fractures.