MEDICAL / FIRST AID
Challenge
Your spouse awakens you during the night complaining of chest pain and difficulty breathing. Should you administer aspirin, and if so, how much? Should you have him/her sit down, lie down, or stand up? Should you call emergency services or rush your spouse to the hospital? If he/she suddenly collapses and stops breathing, do you know how to correctly perform CPR?
Medical concerns are important every day, but even more so during times of disaster because services and supplies may be limited. Hospitals may quickly become overloaded, or worse yet, inaccessible. Doctors and pharmacists may be compelled to close their practices in order to handle their own family emergencies. This shortage of staff and supplies could force your family to rely on its own first-aid abilities and existing stockpile of medicines.
If anyone in your family has a serious existing medical condition, maintaining a stockpile of medicine may be critical to their survival. When a disaster occurs, you may be unable to gain timely access to a doctor or pharmacist, meaning that whatever supplies you have on hand must last until the situation improves. A few of the many possible concerns include insulin for diabetics, respiratory inhalers for asthmatics, opioids for those suffering chronic pain, and nitroglycerin for people with heart conditions.

Treat medicines similar to food; maintain a minimum of a thirty-day supply.
A reasonable approach to preparing is to handle medications in a manner similar to food—stockpiling a minimum of a thirty-day supply. If your customary prescriptions don't support this, explain your preparedness rationale to your doctor to receive the additional prescriptions. Just as with food, rotate the newest medicine to the back and use that which is oldest. If a crisis causes you to experience a shortage of medicine, make every effort to inform your doctor and family of your predicament before the issue becomes serious.
Medical emergencies are to be expected when times are especially challenging. This is in part due to the immediate dangers posed by the threats, but also from having to adapt to difficult living conditions. Connecting a generator, foraging for water, cooking with portable stoves, and shoring up damaged shelters are all examples of activities that introduce additional risk of injury.
To better handle medical emergencies, take the following preparations:
• Teach everyone in the family how to call for emergency medical assistance (see “How to Call for Help”). This includes all children old enough to hold and dial a phone.
• Ensure that all adults in the household learn and practice basic first aid.
• Compile well-stocked first-aid kits for your home and automobiles.
• Share information about any serious, existing medical conditions with family and friends.
• Memorize driving directions to at least two emergency medical facilities.
• Investigate which hospitals offer the best services and equipment. For example, some hospitals have specialized cardiac care centers, improving a heart patient's chances for survival.

The United States uses 911 as its three-digit emergency number. This number can be called without charge from any landline, payphone, or cell phone (active or not). Once received, an operator or dispatcher requests that the caller specify the nature of the call: police, fire, or medical services. In the case of an operator, the call is then forwarded to the correct emergency service center. A dispatcher is specially trained to dispatch emergency services as well as provide urgent lifesaving advice.
Note that 911 is not a universal emergency number outside the United States. Every country has one or more of its own emergency phone numbers. For example, much of Europe uses 112.

Calling 911 from a landline helps the dispatcher to quickly locate you.
When placing an emergency call, it is better to use a conventional landline rather than a cell phone. A landline enables the emergency operator to immediately identify your location. Location determination is slower and less precise when you call from a mobile phone.
The most important thing to remember when calling for emergency service is to remain calm. It may feel like the world is tumbling down around you, but staying calm improves your chances of a successful outcome, whether that is saving someone's life or getting the police to your home as quickly as possible. Explain your situation clearly, follow the dispatcher's directions, and do not hang up until directed to do so.
There are many health conditions that require emergency medical services. Recognizing those conditions is critical to increasing the victim's chances of survival. Most life-threatening conditions can be recognized by one or more basic warning signs. Consider the following list of symptoms that often indicate a medical emergency.199 If you witness or experience any of these symptoms, immediately call for emergency medical assistance.

Symptoms of a Medical Emergency
 Loss of consciousness
Loss of consciousness
 Chest or severe abdominal pain
Chest or severe abdominal pain
 Sudden weakness or numbness in face, arm, or leg
Sudden weakness or numbness in face, arm, or leg
 Sudden changes in vision
Sudden changes in vision
 Difficulty speaking
Difficulty speaking
 Severe shortness of breath
Severe shortness of breath
 Bleeding that does not stop after ten minutes of direct pressure
Bleeding that does not stop after ten minutes of direct pressure
 Any sudden, severe pain without an obvious cause
Any sudden, severe pain without an obvious cause
 A major injury such as a head trauma or broken limb
A major injury such as a head trauma or broken limb
 Unexplained confusion or disorientation
Unexplained confusion or disorientation
 Bloody diarrhea with weakness
Bloody diarrhea with weakness
 Coughing or vomiting blood
Coughing or vomiting blood
 A severe or worsening reaction to an insect bite, food, or medication
A severe or worsening reaction to an insect bite, food, or medication
 Suicidal feelings
Suicidal feelings
First aid is defined as the initial medical assistance given to someone who is ill or injured. It may be required at home, in the workplace, or while traveling the roadways; medical emergencies can happen any-where. In the case of minor illnesses or accidents, treatment can usually be rendered without any outside medical assistance. More serious conditions require that you stabilize the patient and call for emergency medical assistance.

As a caregiver, your role begins with an understanding of the six first aid priorities:200
1. Assess the situation quickly but calmly.
2. Don't put yourself or the patient in additional danger.
3. Prevent cross contamination by cleaning your hands, using sterile supplies, and equipping yourself with protective clothing.
4. Provide comfort and reassurance to the patient.
5. Administer life-saving treatment first (e.g., stop the bleeding, clear the airway, administer chest compressions) before taking any other actions.
6. Never hesitate to call for emergency medical assistance, even if the victim is reluctant to have you do so.
First-aid training can be acquired from your local Red Cross or medical “how to” manuals. With that said, there is no substitute for hands-on experience. Reading about injuries is one thing; feeling the flow of warm blood over your fingers as you try to stop the bleeding from a major wound is something altogether different. Beyond professional training, the single best way to become proficient at first aid is to practice. For example, to become proficient at applying bandages, take every opportunity to apply bandages over a variety of wound types.
Above all, follow the doctor's dictum, primum non nocere… first do no harm. The human body does a remarkable job of healing itself from many injuries, so be judicious when deciding your course of action. Perhaps the most important rule to remember is that if you are unsure about what to do, stabilize the person and seek medical assistance.

Be judicious with your first-aid treatment to avoid causing additional injury.
Step-by-step treatments for a variety of first-aid situations are outlined in this chapter. Recognize that gaining proficiency in administering first aid is very different from becoming a self-prescribed emergency room doctor. For serious medical situations, you should always seek a trained physician in a fully-equipped facility. With that said, there are times when you may have to handle medical emergencies on your own—even if it is only to stabilize the patient until help arrives.
This chapter should serve as a good start to your first-aid preparations. The bulk of this material describes symptoms and treatments for a host of common first-aid situations. For each situation, recommended actions are provided based on a number of reputable medical sources.200,201,202,203 A list of supplies necessary to treat each condition is also given. The lists of supplies have been combined into a comprehensive first-aid kit at the end of the chapter. The goal of organizing it this way is to ensure that you know how to use everything in your first-aid kit.
Note: For ease of writing, the terms “him” and “he” are used throughout the descriptions of medical conditions, but they are meant to refer to both male and female patients.
Anaphylaxis is a severe allergic reaction that can result in respiratory distress and circulatory shutdown. Anaphylactic shock can occur immediately or take several hours from the time of exposure. In an anaphylactic reaction, blood vessels dilate, causing the victim's blood pressure to fall and air passages to constrict. Additional symptoms may include: hives; swelling of the lips, eyes, tongue, and throat; wheezing and gasping; dizziness; abdominal cramping; nausea; vomiting; and diarrhea. There exists a wide variety of allergens, but some of the most common are nuts, insect stings, shellfish, latex, and eggs.
1. Call 911 for emergency medical assistance.
2. Check to see if the patient is carrying an epinephrine auto-injector.
3. If epinephrine is available and the patient is conscious, help him to use the auto injector.
4. If the patient is unconscious or nonresponsive, administer epinephrine as directed:
• Remove the safety cap.
• Hold the injector in your fist and place the tip firmly against the patient's thigh—the shot can be given through most clothing.
• Release the medicine and hold the injector in place for at least 10 seconds.
• Massage the injection site to increase absorption.
5. Have the patient sit in whatever position feels most comfortable for his breathing. If he begins to appear pale or weak, have him lie on his back with his feet elevated about 12 inches.
6. Administer an over-the-counter antihistamine pill with a little water if the patient is able to swallow it without choking.
7. Loosen any tight clothing and cover the patient with a blanket. Do not give him anything else to drink.
8. If the patient begins vomiting or bleeding from the mouth, turn him on his side to prevent choking.
9. If the patient stops breathing, perform CPR.
• Epinephrine auto-injector—requires a doctor's prescription
• Antihistamine pills (e.g., Benadryl)
Domestic pets are the source of most animal bites. Dog bites occur more often, but cat bites are more likely to cause infection. Any bite from a wild or non-immunized animal should be immediately treated by a medical doctor due to the increased risks of infection, tetanus, and rabies. Bites from immunized animals that break the skin should also be treated. Rabies is most common in raccoons, skunks, bats, and foxes, and less likely in rodents, rabbits, and squirrels. Reptiles, fish, and birds do not carry rabies. Human bites can also cause infection or transfer potentially deadly viruses, such as HIV/AIDS, and should therefore be treated immediately by medical personnel.
Animal bites
1. If the bite is from a wild animal, or if the immunization of the animal is unknown, seek medical care immediately. Rabies is a fast-acting, deadly disease that requires immediate diagnosis for the greatest chance of survival.
2. If the bite doesn't break or barely breaks the skin and is from an immunized, domesticated animal, wash the wound with soap and water (or Betadine antiseptic if water is unavailable), apply an antibiotic cream, and cover with a clean bandage.
3. If the bite is a deeper wound (i.e., punctured or torn), apply pressure with a clean cloth or bandage to stop the bleeding, then seek emergency medical care.
4. As the wound heals, if you notice signs of infection, such as swelling, redness, or oozing, seek medical attention.
• Soap and water, or Betadine
• Antibiotic cream
• Adhesive bandages
A black eye is caused by bleeding under the skin around the eye. Most black eye injuries are not serious and can be handled without assistance.
1. To reduce swelling, gently apply a cold pack or ice-filled cloth to the area. Apply it as soon as possible, and continue using the cold pack a few times a day for twenty-four to forty-eight hours.
2. If the patient experiences vision problems (e.g., blurring, double vision), severe pain, bleeding within the eye, or bleeding from the nose, seek emergency medical care.
3. If both eyes become black, seek emergency medical care since it may indicate a skull fracture.
• Cold pack
Blisters are typically caused by friction (e.g., your foot rubbing against your shoe) or heat (e.g., grease splashing onto your hand from a hot pan). Most blisters are not serious and can be handled without medical assistance.
1. Wash the blister and surrounding area with clean water. Gently pat dry with a soft, clean cloth.
2. If the blister isn't too painful, try to avoid popping it. Keeping the skin intact will help to prevent infection.
3. If the blister is small, cover it with an adhesive bandage. Larger blisters can be covered with porous, non-stick gauze pads.
4. If the blister must be drained due to its size or location, follow these steps:
a) Wash your hands with soap and water.
b) Apply iodine or rubbing alcohol to the blister.
c) Sterilize a clean needle with alcohol.
d) Use the needle to puncture the blister at several places near the blister's edge. Let it drain, but try to keep the overlying skin intact.
e) Apply an antibiotic cream, and cover with an adhesive bandage or porous, non-stick gauze pad.
f) After several days, it may be possible to use sterile scissors and tweezers to gently cut away the top skin. After doing so, apply more antibiotic ointment and a fresh bandage.
g) Seek medical attention if signs of infection develop, such as pus, redness, increased pain, or warm skin.
• Antibiotic cream or ointment
• Adhesive bandages
• Porous, non-stick gauze pads
• Rubbing alcohol
• Needle
Bruises are pools of blood just beneath the skin, usually caused by a physical blow of some sort. They fade within a few days and are not a serious medical concern. Generally, the older a person is, the more easily bruising occurs.
1. If the skin isn't broken, there is no need to cover a bruise with a bandage. However, some patients may prefer to cover particularly unsightly bruises.
2. To help a bruise heal faster:
a) Elevate and rest the injured area if possible.
b) Apply a cold pack to the bruise several times a day for twenty-four to forty-eight hours. Do not apply ice directly to the skin.
3. After about forty-eight hours, apply a warm washcloth for ten minutes, twice a day, to help increase blood flow. This allows the skin to reabsorb the blood more quickly.
4. Seek medical attention if the bruise is unusually large or painful—particularly if the patient can't remember suffering any trauma to the region.
5. Seek emergency medical attention if the patient is experiencing abnormal bleeding elsewhere, such as from the nose, gums, or eyes, or if blood is present in the stool or urine.
• Cold pack
• Warm washcloth
Burns are described by three classifications: first degree, second degree, and third degree. Each increase in degree indicates an increase in severity (i.e., third degree is more serious than second degree). The classification is based on the depth of the burn. It is important to recognize the symptoms of each type of burn because their respective treatments are different.
First-degree burns (a.k.a. superficial burns) damage only the outermost layer of skin, the epidermis. The affected area is usually red, swollen, and painful. Mild sunburn is the most common type of superficial burn. First-degree burns are generally treated as minor burns as outlined below. However, if the burn covers a large portion of the hands, feet, face, groin, buttocks, or a major joint, seek medical attention.
Second-degree burns (a.k.a. partial-thickness burns) damage down to the second layer of skin, the dermis. Symptoms include blisters, intensely red and splotchy skin, pain, and swelling. If the burn is smaller than three inches across, treat it as a minor burn as outlined below. If the burn is larger than three inches across, or is located on the hands, feet, face, groin, buttocks, or over a major joint, treat as a major burn.
Third-degree burns (a.k.a. full-thickness burns) are serious burns that involve all layers of the skin and sometimes even muscle and bone. The area may appear waxy, pale, or charred. Full-thickness burns require immediate emergency medical care and should be treated as major burns.
1. Immediately cool the burn by holding the area under cool running water for ten to fifteen minutes. If this is difficult to do because of the burn's location, soak the affected area in cool water or apply cold compresses. Do not apply ice directly to the burn.
Three degrees of burns (Wikimedia Commons/K. Aainsqatsi)
2. Cover or wrap the burn loosely with a non-stick gauze bandage. Try to avoid breaking any blisters.
3. Administer an over-the-counter pain reliever as needed.
4. Watch for signs of infection such as increased pain, redness, fever, swelling, or oozing. If infection occurs, seek medical attention.
5. To minimize pigmentation color changes, apply sunscreen on the burned area for at least one year.
1. Call for, or seek, emergency medical assistance.
2. Cool the injury by flooding the area or entire body with cold water. Be careful about overcooling the patient, especially when dealing with babies and the elderly.
3. Do not touch the injured area. If possible, remove any burned clothing as well as any watches or jewelry that might become constricting if the limb should swell. If there is a risk of injury, leave the clothing in place, but be sure that it is fully extinguished.
4. Cover the burned area with a non-stick gauze or gel-soaked bandage, such as those from Water-Jel. If bandages are not available, cover the wound with plastic wrap to keep out infection.
5. Reassure the patient and treat for shock if necessary.
6. If the patient stops breathing, administer CPR.
• Non-stick gauze or gel-soaked burn bandage
Cardiopulmonary resuscitation (CPR) is a lifesaving treatment used on a person whose breathing or heartbeat has stopped. If you are interested in receiving formal CPR training, contact the American Heart Association at 1-800-AHA-USA1 or your local American Red Cross.
CPR consists of chest compressions and mouth-to-mouth rescue breathing. For adult patients, experts now recommend that untrained people only administer chest compressions, rather than the combination of compressions and rescue breathing. The reason for this change is that for the first five minutes after an adult's heart stops, the blood remains oxygen rich, and chest compressions are the highest priority for survival. The chest compressions help keep oxygenated blood flowing to the brain and organs until emergency personnel arrive.

Administering chest compressions
For infants and children, however, both chest compressions and rescue breathing are necessary. The differences in treatment are outlined in the steps below.
1. Check to see if the person is unconscious by touching him and asking, “Are you okay?” Be sure he isn't just sleeping!
2. If he doesn't respond, have someone call for emergency medical assistance while you start CPR. If you are the only person on the scene and have immediate access to a phone, make the call before beginning CPR. However, if the patient is unconscious due to suffocation or drowning, or if the patient is a child, administer CPR for one full minute before calling for emergency assistance.
3. If you suspect the patient has suffered a heart attack, and an Automatic External Defibrillator (AED) is available, retrieve the unit, push the ON button, and follow the voice prompts. Otherwise, administer manual CPR as outlined below.
4. Before administering CPR, check to be sure that the patient's airway is clear and that he is not currently breathing.
a) Lay him on his back.
b) Kneel next to his shoulders.
c) Tilt back his head using his chin and forehead.
d) Check for breathing using the look, listen, feel technique. Look for chest motion; listen for breathing; feel for breath on your cheek. If he is breathing, wait for emergency personnel to arrive while monitoring his condition.
e) If the patient is not breathing, look to see if his airway is obstructed. If it is visibly obstructed, or you know the patient choked, follow the steps outlined in “Choking.” Otherwise, begin administering CPR.
5. Adolescent/Adult Patient: Administer chest compressions.
a) Place the heel of one hand over the center of the patient's chest directly between his nipples. Place your other hand on top of the first.
b) Keeping your elbows straight, use your upper body weight to quickly compress the chest about two inches. Repeat at a rate of 100 compressions per minute.
c) Continue chest compressions until the patient revives or medical personnel arrive.
6. Child Patient (age 1–8): Administer chest compressions and rescue breathing.
a) Administer chest compressions using the heel of one hand placed directly between the child's nipples. The compression should compress the child's chest by about one third. Administer thirty compressions at a rate of 100 compressions per minute.
b) Administer rescue breathing by tilting the child's head back, pinching his nose closed, and placing your lips around his mouth. Blow steadily for one second; the chest should rise. Remove your mouth, take a breath, and administer a second rescue breath.
c) Continue repeating thirty chest compressions followed by two rescue breaths until the child revives or rescue personnel arrive.
d) If alone, repeat the cycle five times before calling for emergency medical assistance.
7. Infant Patient (<1 year old): Administer chest compressions and rescue breathing.
a) Administer chest compressions using the two fingers of one hand placed directly between the infant's nipples. The compression should compress the child's chest by about one third. Administer thirty compressions at a rate of 100 compressions per minute.
b) Administer rescue breathing by tilting the infant's head back, and placing your lips around the infant's mouth and nose. Blow a gentle breath for one second; the chest should rise. Remove your mouth, take a breath, and administer a second rescue breath.
c) Continue repeating thirty compressions followed by two rescue breaths until the infant revives or rescue personnel arrive.
d) If alone, repeat the cycle five times before calling for emergency medical assistance.
• Optional: rescue breathing masks or face shields
Chemical splashes in the eye can cause serious injury if not treated quickly. It is important to thoroughly flush the eye with water or saline solution as rapidly as possible.
1. Turn the patient's head sideways under a gentle running faucet (or shower), flushing the eye thoroughly with water for up to ten minutes. Orient the patient so that the affected eye is down toward the sink, preventing the contaminants from washing over into the uninjured eye. With a young child, it might be easier to have him lay back while you gently pour water onto his forehead or the bridge of his nose.
2. After cleaning his eye, wash your hands and have the patient wash his hands to remove any possible chemical contamination.
3. Have him remove any contact lenses if they haven't been removed already.
4. Try to prevent any rubbing of the eye, as this may cause damage.
5. If pain or irritation continues, seek emergency medical care. Take the bottle of chemical contaminant with you.
• Water or saline solution
Chest pain can be an indication of many different medical conditions, ranging from minor to deadly. An accurate diagnosis is often very difficult for a layperson to make. A few of the many possible causes for chest pain are given below:
• Heartburn—stomach acid rises into the esophagus
• Sore muscles, injured ribs, or pinched nerves
• Heart attack—an artery providing oxygen to the heart becomes blocked
• Angina—plaque buildup causes reduced blood flow in the heart
• Pulmonary embolism—a blood clot lodges in an artery of the lungs
• Aortic dissection—a tear develops in the inner layer of the aorta (the heart's large blood vessel)
• Costochondritis—pain in the chest wall causes tenderness around the cartilage that connects the ribs to the sternum
• Pleurisy—membrane lining the chest wall becomes inflamed, causing sharp, localized chest pain, especially when inhaling
1. If someone experiences unexplained chest pain that lasts for more than a few minutes, seek emergency medical care. Either call for emergency medical assistance and wait for an ambulance, or immediately drive the patient to the nearest emergency room. A patient should not be allowed to drive himself in case his condition worsens.
2. If you suspect the chest pain is due to a heart attack, follow the steps given under “Heart Attack.”
• None
Choking is usually the result of something lodged in the throat, partially or fully blocking the airflow. With adults, the cause is often a piece of food, but with children it can also be a toy, coin, or other small object. Teach everyone in your family the universally accepted sign for choking—clutching their throat with both hands. Symptoms of choking can include inability to talk or cough, difficulty or noisy breathing, skin and lips turning blue or dusty-looking, and loss of consciousness. Choking is a potentially deadly condition that requires immediate attention.
1. Ask the patient if he is choking. If he is able to talk or cough forcefully, allow him to dislodge the food himself. Do not administer abdominal thrusts if the patient is coughing.
2. If you determine that his airflow is blocked, administer standing abdominal thrusts—see below.
3. If the patient collapses unconscious, examine his airway to see if the obstruction can be removed. If so, attempt to remove it, but be careful not to push it further into the airway.
4. If you cannot remove the object, administer prone abdominal thrusts—see below.
5. If you fail to clear the obstruction, call for emergency medical assistance, and administer CPR until emergency personnel arrive.
Stand behind the patient and bend him slightly forward at the waist. Wrap your arms around his waist, making a fist with one hand and grabbing it with the other. Place your fist slightly above the patient's navel. Press hard up into the abdomen with a quick thrust—as if you are trying to lift him off his feet. In the case of an obese or pregnant patient, position your hands slightly higher.
If the patient is unconscious, deliver abdominal thrusts by straddling the patient and placing the heel of your hand just above his navel. Place your other hand on top of the first. Keeping your elbows straight, give several quick upward thrusts until the object is expelled.
Delivering abdominal thrusts, standing and prone
1. Sit down, and place the infant face down on your forearm, resting the supporting arm on your thigh. The infant's head should be lower than his trunk.
2. Using your heel of your palm, thump the infant five times in the middle of his back.
3. If back blows fail to relieve the choking, roll the infant over and check his mouth and throat. Remove any obvious obstructions with your fingertips—don't sweep the object, since that may push the object further down the throat.
4. If the obstruction cannot be removed with your fingers, keep the infant face-up on your forearm with his head lower than his trunk. Using two fingers, give up to five quick chest compressions at the center of the infant's breastbone. The purpose of the compressions is to dislodge the blockage.
5. If chest compressions do not free the obstruction, call for emergency medical assistance and repeat this routine of five back blows followed by five chest thrusts until the object clears or emergency personnel arrive.
6. If the infant loses consciousness, administer CPR.
• None
Minor cuts and scrapes occur frequently and can usually be treated without medical assistance. However, if you can't stop the flow of blood, or if it seems to spurt out, seek emergency medical care. Likewise, if the wound is deeper than about ¼ inch or is gaping open, seek emergency medical care to receive stitches or other treatment.
1. Most small cuts and scrapes will stop bleeding on their own, but if they don't, apply gentle pressure with a clean bandage or cloth for twenty to thirty minutes. If possible, elevate the wound above the patient's heart.
2. Clean the wound by rinsing it with clean water. You can also use soap (or alcohol wipes) to clean the area, but try to keep the soap or alcohol out of the wound. If dirt or debris remains in the wound after rinsing, use tweezers dipped in alcohol to remove the debris.
3. Apply a thin layer of antibiotic cream or ointment to the cut or scrape.
4. Cover the wound with a clean bandage.
5. Change the bandage at least once daily or when it becomes wet or dirty.
6. Once the wound has healed sufficiently to make infection less likely, remove the bandage and expose it to the air to speed healing.
7. If you see signs of infection, such as redness, increasing pain, drainage, or swelling, seek medical attention.
• Bandages
• Antibiotic ointment
• Soap and water
• Rubbing alcohol
• Tweezers
Bones can dislocate as a result of a blow or fall. This type of injury occurs frequently in contact sports, such as football or hockey. Dislocation can occur in major joints, such as the shoulder or knee, or in smaller joints, such as the fingers and toes. Torn ligaments, damage to the synovial membrane, and fractured bones can also accompany dislocated joints.
1. Do not move the bone or try to reposition it back in the joint. Keep the limb stationary in the position that causes the patient the least amount of pain. If possible, use a splint or sling to prevent movement.
2. Apply a cold pack to the injured joint to reduce swelling.
3. Seek emergency medical care immediately.
• Splint, sling
• Medical tape
• Cold pack
Minor electrical shock (i.e., one that causes no noticeable symptoms) doesn't usually require medical treatment. However, a major electrical shock can cause serious complications, including cardiac arrest, respiratory failure, burns, seizures, and loss of consciousness. A patient who receives a shock by alternating current (AC) may be unable to let go of the electrified object. Direct current (DC) tends to produce a single violent muscular contraction that throws the patient away from the electrified object.
If you witness someone being shocked or encounter someone who you suspect has been shocked, use extreme caution to prevent injury to yourself. Electricity can arc through the air from person to person or from object to person if you get too close. High-voltage power lines, for example, can arc through the air up to 60 feet.
1. Carefully inspect the situation. Do not touch the person until you are certain that he is no longer being shocked.
2. If the patient is being shocked by a high-voltage power line, do not approach him. Call for emergency assistance immediately.
3. If the patient is being shocked by a house appliance or outlet, unplug the source or throw the circuit breaker. If that is not possible, use a non-conducting object, such as a wood broomstick, to push the source away from the person.
4. Check to see if the patient is breathing. If he isn't breathing, begin administering CPR and call for emergency medical assistance.
5. If the patient is injured but still breathing, treat for shock by laying him down and elevating his legs. Then call for emergency medical assistance.
• None
Fainting is a brief loss of consciousness caused by a temporary reduction in blood flow to the brain. It can be brought on by dehydration, lack of food, exhaustion, reaction to pain, or emotional stress. It may also occur when standing up quickly after sitting for a long period of time because blood may pool in the legs and be unable to reach the brain fast enough. A person who faints is typically unconscious for only a brief time (less than one minute) until blood flow to the brain improves.
1. If someone says he feels faint, have him sit or lie down. Do not have him put his head between his legs while sitting because he may fall and become injured. If he chooses to lie down, elevate his feet slightly.
2. If someone faints, first check to see if he is breathing. If he is not breathing, immediately begin administering CPR and call for emergency medical assistance.
3. If he is unconscious but breathing, lay him on his back and elevate his feet above his heart level by about 12 inches. Loosen any constrictive clothing, and monitor his breathing.
4. Once he regains consciousness, have him rest a moment before slowly standing up.
5. If he does not regain consciousness within one minute, call for emergency medical assistance.
• None
Fever is a symptom of many different medical conditions but is most often caused by a bacterial or viral infection. Every person's normal body temperature is slightly different, with the average being 98.6°F. A moderate fever is not usually harmful to adults but may introduce seizures in young children.
Many doctors recommend not treating fevers below 102°F with medications. They argue that the body's elevated temperature will help fight off infection, but only at the expense of added discomfort for the patient.
1. Keep the patient cool and comfortable, preferably remaining in bed.
2. Provide cool beverages to drink (non-alcoholic, caffeine-free).
3. Treat with fever reducers or pain medicine as needed.
• Adult fevers can be treated with acetaminophen, ibuprofen, or aspirin (assuming there are no allergies).
• Children over six months of age can be treated with ibuprofen or acetaminophen. Do not give aspirin to children because it might trigger Reye's syndrome—a rare but deadly disorder.
• Children under six months of age should only be treated with acetaminophen.
4. Seek medical care if any of the following conditions apply:
• A baby younger than three months has a rectal temperature of 100.4°F or higher. A rectal reading is generally about 1 degree higher than oral readings
• A baby older than three months has a temperature of 102°F or higher
• A newborn has a rectal temperature below 97°F
• A child younger than age two has a fever longer than one full day, or a child older than age two has a fever longer than three days
• An adult has a temperature of more than 103°F or has a fever for more than three days
Caution: Be very careful to give the correct dose of acetaminophen. Overdosing of acetaminophen can lead to liver failure and death. Tens of thousands of Americans are rushed to emergency rooms every year from acetaminophen overdose.204 Be aware that acetaminophen may also be present in other medicines, such as cough suppressants, that when combined with fever-reducing medicine, can lead to a dangerous overdose.
• Fever-reducing medicine
A foreign object can become stuck in the ear and cause pain or hearing loss. Common objects include cotton swabs and insects. In most cases, foreign objects can be safely removed without medical assistance, but care must be taken not to injure the patient's ear or push the object deeper into the ear canal.
1. If the object is clearly visible, attempt to gently remove it using tweezers. Do not try to remove the object using a cotton swab, matchstick, or other ill-suited tool; you risk pushing it further into the ear and causing damage.
2. If you can't easily pull it out, try tilting the patient's head such that his ear faces the ground, and then gently try to dislodge it.
3. If the object is an insect (alive or dead), fill the ear with warm water, mineral oil, baby oil, or olive oil to float the insect out. Do not use this method if there is any pain, bleeding, or discharge from the ear.
4. If these simple methods fail to remove the object, seek medical attention.
• Tweezers
• Mineral, baby, or olive oil
Most eye injuries involve the cornea—the clear protective coating at the front of the eye. Dust, dirt, sand, wood shavings, or other particles can scratch, cut, or become lodged in the cornea. Corneal abrasions are painful, but most are not serious unless they become infected or inflamed. Symptoms may include tearing, blurred vision, headache, and eye redness.
1. Have the patient sit facing a bright light so that you can more easily inspect his eye.
2. Wash your hands with soap and water.
3. Using your thumb and forefinger, gently separate his eyelids (pulling the top one up and the bottom one down). Have the patient look left, right, up, and down, while you are examining the eye for foreign objects.
4. If you see a foreign object on the surface of the eye, rinse the eye with saline solution (or clean water if saline isn't available).
5. If rinsing is not successful, try to lift the object out by gently dabbing with a clean moist cotton swab. Try not to rub the eye, which can cause additional scratching.
6. You can also have him pull the upper eyelid over the lower one to help dislodge anything stuck on the undersurface of the upper eyelid.
7. Don't try to remove anything that is embedded in the eyeball.
8. If you are unable to remove the foreign object, or if it is embedded in the eyeball, cover the eye with sterile eye pad or gauze, and seek emergency medical care.
• Saline solution or eye wash
• Eye pad
• Bright light
• Cotton swab
Children are especially likely to lodge a small object in their noses. Common obstructions include marbles, candy, toys, or batteries. If the object is sharp, it can cause tissue damage, which can lead to infection. Likewise, batteries can cause tissue burns. Small objects lodged in the nose can usually be removed without medical assistance; however, care must be taken to ensure that the object isn't pushed further into the airway.
1. Have the patient breathe through his mouth, preventing him from inhaling the object.
2. Have him blow his nose gently. If the obstruction is affecting only one nostril, plug the other nostril when blowing.
3. If the object can be easily grabbed, carefully use tweezers to remove it. Do not use a cotton swab or other ill-suited tool to try to pry the object out.
4. If the object is a marble and it will not blow out, try gently pinching the nose from the top down, pressing the marble down and out of the nose.
5. If you are unable to remove the object, seek emergency medical care.
• Tweezers
Splinters of wood, metal, glass, or fiberglass can become lodged in the skin. It is important to remove the splinter to prevent infection. Getting a splinter out can usually be done without medical assistance.
1. Wash your hands and the affected area with soap and water. Sterilize a needle and tweezers using isopropyl alcohol.
2. If the splinter juts out above the skin, use tweezers to draw the object out in a straight line opposite the direction that it went in.
3. If the splinter is completely embedded in the skin, use a small sterilized needle to break the skin above it. Then gently lift the tip of the splinter out, and use tweezers to remove the object.
4. Gently squeeze the area to stimulate a little bleeding, which helps to flush out the wound.
5. Wash and dry the area again.
6. Apply a thin layer of antibiotic ointment and a small adhesive bandage as needed.
• Tweezers
• Needle
• Isopropyl alcohol
• Antibiotic ointment
• Adhesive bandage
Most small foreign objects that are swallowed will usually pass through the digestive system without complications. However, sharp objects may become lodged in the esophagus (the tube connecting the throat to the stomach). Also, button batteries used in watches, calculators, and toys, can cause tissue damage and should be removed by a medical professional immediately. Finally, swallowing multiple magnets may cause internal complications and requires immediate medical consultation.
1. If the object is small and doesn't cause choking, contact your family doctor. He will likely recommend that you allow the item to pass through the body.
2. If the object is sharp, lodged in the esophagus, or a battery, seek emergency medical care.
3. If the object causes choking, treat the patient as outlined under “Choking.”
• None
A fracture is a break or crack in the bone. Open (compound) fractures are those where the broken bone penetrates the skin, whereas closed (simple) fractures leave the skin intact. Open fractures are particularly susceptible to infection. Fractures may be characterized by bleeding, swelling, deformity, bruising, pain, and difficulty in moving the limb. Fractures require professional medical attention.

Fractured hand (Wikimedia Commons/Roberto J. Galindo)
1. If the fracture is on the arm, hand, or foot, and there is no bleeding, immobilize the limb using a sling or structural aluminum malleable (SAM) splint. Apply a cold pack to the area, and seek emergency medical care.
2. If the fracture is elsewhere on the body, such as the neck, back, leg, or hip, call for emergency medical assistance and have the patient remain still until emergency personnel arrive.
3. If the fracture is bleeding, carefully apply pressure to the wound with a clean cloth or bandage, and call for emergency medical assistance. Keep the area immobilized, and do not try to realign or push a protruding bone back in.
4. If the patient feels faint, treat him for shock by laying him on his back and elevating his feet.
• SAM splint
• Sling
• Tape
• Cold pack
• Clean cloth or bandage
Frostbite is the result of the skin being exposed to very cold temperatures. Extremities such as hands, feet, nose, and ears are most likely to be affected. If left unchecked, frostbite can cause loss of sensation and tissue death. Symptoms include the skin appearing white or grayish-yellow, being very cold to the touch and having a hard or waxy feel. Itching, burning, or numbness may also be present. As the skin thaws, it becomes red and painful. Frostbite is often accompanied by hypothermia, which must also be treated (see “Hypothermia”).
1. Immediately get the patient out of the cold. Try to keep him from walking on frostbitten feet or toes.
2. Warm the affected area. You can warm hands or feet by placing them under your armpits. Hands and feet can also be warmed by placing them in lukewarm (not hot) water. Cover ears, nose, and face with warm hands.
3. Raise the affected limb to reduce any swelling.
4. Do not rub the affected area as this can cause skin and tissue damage.
5. Administer over-the-counter pain medicine as needed.
6. Seek emergency medical assistance if numbness remains after warming or if skin damage is present.
• Over-the-counter pain medicine
Gastroenteritis is a general term used to describe the inflammation of the stomach and intestines. There are many possible causes, including viruses, food- or water-borne bacteria, and stress. Symptoms may include nausea, vomiting, diarrhea, abdominal cramps, and occasionally a low-grade fever. The symptoms may last from twenty-four hours to more than a week. See Chapter 2 and Chapter 3 for additional information on food poisoning and water-borne contamination.
1. Have the patient rest and drink plenty of liquids to prevent dehydration.
2. Have him gradually ease back into eating, starting with bland foods, such as crackers, toast, gelatin, bananas, and chicken soup. Have him avoid dairy products, caffeine, alcohol, nicotine, and fatty foods for a few days.
3. Generally, do not administer anti-diarrheal medications early in the sickness because they may slow the elimination of contaminant from the digestive system.
4. Seek medical care for any of the following conditions:
• Vomiting persists for more than two days or turns bloody
• Diarrhea persists for more than a week or turns bloody
• High fever develops
• Confusion, lightheadedness, or fainting occurs
5. Additionally, seek emergency medical care for a child for any of the following conditions:
• Child becomes unusually drowsy
• Child shows signs of dehydration such as marked thirst, sunken eyes, crying without tears, if the soft spot on an infant's head starts to become sunken, or if diapers remain dry for eight or more hours
• Fever remains longer than one day for child under age two, or fever remains longer than three days for child over age two
• Thermometer
A headache may accompany many illnesses, particularly those with fevers. Headaches may also be the result of stress, fatigue, or excessive alcohol consumption. Most headaches are minor and can be treated with over-the-counter pain medications. However, headaches can also signal dangerous medical conditions, such as meningitis or a stroke.
1. Have the patient sit or lie down in a quiet room. Provide a cold compress for his head.
2. If the headache is minor, consider treating with over-the-counter pain medication:
• Treat adult headaches with acetaminophen, ibuprofen, or aspirin (assuming there are no allergies).
• Treat a child's headache only with acetaminophen or ibuprofen. Do not give aspirin to children because it might trigger Reye's syndrome—a rare but deadly disorder.
• Treat infants younger than six months of age with acetaminophen. Be very careful to administer the correct dose.
3. Seek emergency medical care for any of the following:
• A severe headache develops suddenly
• The headache is accompanied with a fever, stiff neck, rash, confusion, seizures, vision changes, dizziness, weakness, paralysis, or difficulty speaking
• The headache is the result of a head injury or fall
• The headache progressively worsens throughout the day or persists for several days
• Over-the-counter pain reliever
Minor abrasions and cuts to the head are treated as they would be to any other part of the body (see “Cuts and Scrapes”). However, in the case of a more severe head injury, the patient requires careful monitoring because head trauma may cause more serious medical conditions, including a skull fracture, concussion, and bleeding in the brain.
1. If the head trauma is minor, treat the abrasions as detailed in “Cuts and Scrapes.” An ice pack can also be applied to reduce localized swelling.
2. If any of the following symptoms occur at the time of the injury, or become evident within twenty-four hours, call for emergency medical assistance immediately:
• Severe head or facial bleeding
• Bleeding from the nose or ears (other than from a minor injury to the nose or exterior of the ears)
• Severe headache
• Loss of consciousness for more than a few seconds
• Black and blue discoloration below the eyes or behind the ears
• Cessation of breathing
• Confusion
• Loss of balance
• Weakness or inability to use an arm or leg
• Unequal pupil size
• Vomiting
• Slurred speech
• Seizures
3. While awaiting emergency personnel, keep the patient still, stop any bleeding by applying pressure using a clean cloth or bandage, and stay alert for any changes in breathing.
4. If the patient stops breathing, administer CPR.
• Bandages
• Antibiotic ointment
• Cold pack
A heart attack occurs when the artery supplying blood to the heart becomes partially or completely blocked. The loss of blood flow causes damage to the heart muscle. Symptoms can include any of the following: chest pressure; pain in the upper abdomen or back; pain spreading from the chest to shoulders, neck, jaw, and one or both arms; shortness of breath; dizziness; sweating; and nausea. The earliest warning sign may be episodes of chest pain that occur during physical exertion but are relieved by rest. However, a heart attack can also occur without any warning signs.
1. If you suspect that someone is having a heart attack, call for emergency medical assistance.
2. Have the patient sit down, rest, and try to remain calm.
3. Have him chew one regular strength aspirin tablet (assuming no allergy), or if he has been prescribed nitroglycerin or other heart medication, have him take it as directed. Do not administer nitroglycerin to someone who has not had it prescribed.
4. If the patient stops breathing, administer CPR while waiting for emergency personnel.
5. If you are in a public building that has an automatic external defibrillator (AED), have someone else retrieve it while you administer CPR. Training is certainly desired when using an AED, but even if you are not trained, don't be afraid to use it on a patient who has stopped breathing. It is their best chance for survival.
Using an AED: An AED analyzes a patient's heart rhythm and determines if an electrical shock is required. After switching the unit on, attach the two pads to the correct location: one just under the patient's right collarbone, and the other along his left ribcage. Get everyone to stand clear while the AED analyzes his heart rhythm. The AED will then advise whether a shock is needed. If advised to do so, press the Shock button on the AED control box to administer the shock. The AED will then direct you to continue administering CPR for two minutes before it reanalyzes the patient's heart rhythm again. If at any time the patient starts to breathe, stop using the AED (but leave it attached), and help him to be comfortable while awaiting emergency personnel.
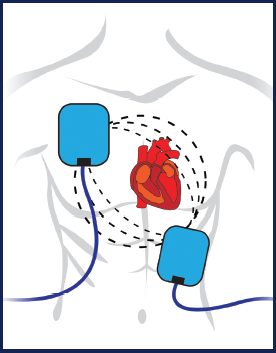
AED pad placement
• Aspirin
• AED (if available)
Heat cramps are the first stage of hyperthermia (see Chapter 7) and consist of painful involuntary muscle spasms. They are most often the result of overexertion in hot environments. Inadequate fluid intake also contributes to heat cramps.
1. Move the patient to a cool environment to rest.
2. Have him drink cool liquids that do not contain caffeine or alcohol.
3. Gently stretch and massage the affected muscle group.
4. Advise the patient to wait a few hours after the heat cramps subside before resuming any strenuous activity.
5. Seek medical care if the cramps don't go away within an hour.
Supplies needed:
• Cool liquids
Heat exhaustion is the second stage of hyperthermia (see Chapter 7). It is typically a result of overexertion in hot conditions. Symptoms often begin suddenly and may include heavy perspiration, dizziness, nausea, a rapid but weak heartbeat, low blood pressure, cool skin that may look pale, low-grade fever, heat cramps, headache, dark urine, and fatigue.
1. Get the patient out of the sun and into a cooler location.
2. Lay the patient down and elevate his feet about 12 inches. Loosen any tight clothing.
3. Have him drink cool liquids that do not contain caffeine or alcohol.
4. Cool the patient by gently spraying or sponging him with water.
5. Monitor his temperature and condition for signs of heatstroke.
6. If any of the following symptoms occur, call for emergency medical assistance:
• Fever greater than 102°F
• Fainting
• Confusion
• Seizures
• Cool liquids
• Thermometer
Heatstroke is the third and most severe stage of hyperthermia (see Chapter 7). It is often a result of continue overexertion in hot conditions combined with inadequate fluid intake. Young children, older adults, and obese people are at higher risk of suffering from heatstroke. Heatstroke can also result from the use of some drugs, such as Ecstasy. The main symptom of heatstroke is an elevated body temperature, generally higher than 104°F. This condition may result in personality changes, confusion, coma, and even death. Other symptoms can include rapid heartbeat, shallow breathing, cessation of sweating, dizziness, headache, nausea, and fainting.
1. Move the patient out of the sun to a cooler location, and remove as much of his outer clothing as possible.
2. Call for emergency medical assistance.
3. Have him drink cool liquids that do not contain caffeine or alcohol.
4. Cool the patient by covering him with damp sheets, or gently spraying with cool water and then fanning him.
5. Once the patient's temperature returns to normal, replace the wet sheets with a dry one. If his temperature rises again, repeat the cooling process.
6. If the patient loses consciousness, continue cooling while monitoring his pulse and breathing.
7. If the patient stops breathing, administer CPR.
• Cool liquids
• Sheets
Hypothermia is a condition that occurs when the body temperature falls below 95°F, caused by prolonged exposure to the cold (see Chapter 7). Severe hypothermia, in which the core body temperature falls below 89°F, is usually fatal. Becoming wet or not covering your head in cold weather increases your chances of suffering hypothermia. Symptoms include shivering, slurred speech, slowed breathing, cold pale skin, loss of coordination, fatigue, and confusion. Symptoms usually develop slowly, with a gradual loss of mental acuity and physical ability. Older adults, infants, young children, and people who are very lean are at higher risk of hypothermia. Alcohol and drugs can exacerbate the condition. If a person is submerged in cold water, hypothermia can develop very quickly.
1. Move the patient out of the cold, preferably into a warm, sheltered location. If you must lay him on the ground, place a pad or other insulating material beneath him.
2. Call for emergency medical assistance.
3. Remove his wet clothing and replace it with something warm and dry. Handle the patient very gently, since rubbing frostbitten skin can cause severe damage.
4. Warm the patient gradually. Do not apply direct heat, such as a hot water, heating pad, or heat lamp. Instead, warm slowly with warm compresses to the trunk of the body. Do not attempt to directly warm the arms and legs because that can cause a fatal condition in which cold blood flows back to the heart, lungs, and brain.
5. Give the patient something warm to drink as well as a small quantity of high-energy food, such as chocolate, to eat.
6. While awaiting medical help, monitor the patient's breathing. If he stops breathing, administer CPR.
• Warm liquids
• High-energy food, such as chocolate
• Dry clothing
Most insect bites and stings cause only mild symptoms, such as itching, stinging, or swelling, and can be safely treated without medical assistance. Only a small percentage of people develop severe reactions to insect venom (see “Anaphylaxis”).
1. Move the patient away from the area to avoid additional stings.
2. If visible, remove any stinger with tweezers, or scrape it out using a playing card or other flat object. Be careful not to squeeze the stinger, which might inject additional venom.
3. Wash the area with soap and water.
4. Apply a cold pack or cloth filled with ice to reduce swelling and pain. Raise the infected limb above heart level if possible.
5. Have the patient take an antihistamine containing diphenhydramine (e.g., Benadryl).
6. Apply hydrocortisone cream, calamine lotion, or baking soda paste (3 teaspoons baking soda to 1 teaspoon water) several times a day until the symptoms subside.
7. For severe reactions, call for emergency medical assistance and follow the steps under “Anaphylaxis.”
8. If the sting occurs on the throat, give the patient ice water to sip. If swelling starts to occur, seek emergency medical assistance.
• Tweezers or flat card
• Cold pack
• Hydrocortisone cream, calamine lotion, or baking soda
• Antihistamine with diphenhydramine
Most nosebleeds are not serious and are easily treated without medical assistance. In older adults, however, some nosebleeds originate from deeper within the nose and may be a result of hardened arteries or high blood pressure. These deeper nosebleeds can be difficult to stop and may require medical assistance.
1. Have the patient sit upright and lean forward to avoid swallowing blood.
2. If bleeding is the result of an injury that may have broken the nose, seek emergency medical assistance.
3. Have him pinch his nose for five to ten minutes to stop the bleeding.
4. If re-bleeding occurs, have him blow out forcefully to clear his nose of blood clots. Then spray nose with a decongestant nasal spray containing oxymetazoline (e.g., Afrin). Then have him pinch his nose for another five to ten minutes.
5. If bleeding persists for more than twenty minutes, seek emergency medical assistance.
• Decongestant nasal spray containing oxymetazoline
Poisons are toxic substances that once introduced into the body, can cause sickness and death. They can be ingested, inhaled, splashed into the eyes, or absorbed through the skin. The specific effects of each poison are unique, but common reactions are: vomiting and nausea (ingested poisons), breathing difficulties (inhaled poisons), blurred vision and watering eyes (splashed poisons), and skin irritation (absorbed poisons). Other effects, including seizures, dizziness, and pain are also possible.
Poison symbol
1. If you suspect poisoning of any kind, immediately call the Poison Control Center at 1-800-222-1222. If the patient is already unconscious, call 911 for emergency medical assistance.
2. If a poison was ingested, remove anything still remaining in the patient's mouth. If possible, ask him what was swallowed. If he is unable to answer, look for clues, such as leaves, berries, pill bottles, or containers. Do not give the patient anything to induce vomiting unless directed to do so by the Poison Control Center.
3. If the patient was exposed to poisonous fumes, such as carbon monoxide, immediately move him to an area with fresh air.
4. If the poison spilled onto the patient's clothing or skin, or splashed into his eyes, remove the clothing and flush the skin and eyes with water.
5. If the patient stops breathing, administer CPR.
• None
A puncture wound, such as a nail through the foot, usually does not cause excessive bleeding but can be serious due to the depth of the wound and risk of infection. The puncturing object may have spores of tetanus or other bacteria, especially if exposed to the soil. Puncture wounds from mammals carry the additional risk of rabies (see “Animal Bites”).
1. Apply gentle pressure to help stop the bleeding as needed. If bleeding persists, seek emergency medical assistance.
2. If the object remains embedded, seek emergency medical attention.
3. If the object is not embedded, flush the wound with clean water. Use tweezers disinfected in alcohol to remove any superficial particles. Clean around the wound with soap and water. If debris remains in the wound, seek emergency medical assistance.
4. Apply a thin layer of antibiotic ointment.
5. Cover the wound with a clean bandage.
6. Change the bandage at least daily or when it gets wet or dirty.
7. Watch for signs of infection including redness, drainage, or swelling. If infection occurs, seek medical care.
8. If the puncture is deep, or from an animal or human bite, or in the foot, seek emergency medical assistance. The doctor may recommend a tetanus booster or a series of rabies vaccinations.
• Tweezers
• Antibiotic ointment
• Isopropyl alcohol
• Bandages
• Soap and water
Trauma can result in severe external bleeding, which can be distressing for both you and the patient. Keeping calm is critical to administer life-saving first aid successfully. If the bleeding is not stopped quickly, the patient will lose consciousness and die.
1. Call for emergency medical assistance.
2. If possible, wash your hands and put on rubber or latex gloves.
3. Have the injured person lie down, and cover him to prevent loss of body heat.
4. Treat for shock by elevating his legs about 12 inches.
5. Remove or cut away clothing to expose the wound.
6. Remove any obvious dirt or debris from the wound. Do not try to remove any deeply embedded objects.
7. Using a clean cloth or thick sterile bandage, such as a trauma pad or bloodstopper compress, apply direct pressure to the wound until bleeding stops (at least twenty minutes). If a bandage or cloth is not available, use your hands directly (preferably with gloves on). If there is an object embedded in the wound, press to either side of it.
8. If possible, elevate the wound above the patient's heart while applying pressure.
9. If the bleeding continues and seeps through the bandage, do not remove it. Instead, add absorbent material over it.
10. If the bleeding doesn't stop, use one hand to compress a main artery that feeds the limb by pressing it against the bone. Use the other hand to maintain pressure on the wound:
• Artery pressure points on the arm are on the inside of the arm, one above the elbow and one below the armpit.
• Artery pressure points on the leg are behind the knee and in the groin.
11. Once the bleeding has stopped, secure the bandage with tape or gauze, and immobilize the injured part until emergency personnel arrive.
• Thick, sterile bandages such as trauma pads, bloodstopper compress bandages, or multi-trauma dressings
• Conforming gauze rolls
• Rubber or latex gloves
Shock is a life-threatening condition most often caused by a significant loss of blood (i.e., more than two pints). It may also be a result of trauma, heatstroke, allergic reaction, infection, poisoning, electric shock, heart failure, hypothermia, hypoglycemia, or severe burns. When in shock, a person's vital organs, such as his brain and heart, aren't getting enough oxygen. This deprivation can lead to organ damage and death. Initial symptoms of shock may include: cool, clammy skin; weak, rapid pulse; and sweating. As shock develops, additional symptoms may include nausea, thirst, confusion, weakness, gasping for air, and loss of consciousness. If not treated, the patient's heart will eventually stop.
1. If you suspect that a person is going into shock, call for emergency medical assistance.
2. Have the patient lie on his back and remain still. Elevate his feet about 12 inches.
3. Reassure the patient. Keep the patient warm and comfortable by loosening clothing and covering with a blanket.
4. If the patient begins to vomit or bleed from the mouth, turn him on his side to prevent choking.
5. Monitor the patient's breathing and heart rate. If he stops breathing, administer CPR.
• Blanket
Fortunately, most North American snakes are not poisonous. Obvious exceptions are the rattlesnake, coral snake, water moccasin, and copperhead, all of which can deliver fatal bites. Snakes do not carry rabies.
1. Call for emergency medical assistance immediately.
2. Do not try to capture the snake, but do try to remember its color and shape so you can describe it to emergency personnel. Also, note the exact time of the bite.
3. Have the patient sit upright and remain calm. Reassure him as needed.
4. Keep the bite below the level of the patient's heart if possible.
5. Remove any jewelry on the limb, and cover the wound with a clean, dry bandage.
6. Immobilize the bitten limb using a splint if possible. If a splint is not available, wrap the limb with heavy gauze up past the joint to prevent bending.
7. Do not use a tourniquet, apply ice, cut the wound, or try to suck out the venom.
• Splint
• Bandage
• Gauze roll
Injuries to the spine may involve the vertebrae, the disks of tissue separating them, the surrounding muscles and ligaments, and the spinal cord and associated nerves branching off from it. The most serious risk exists when the spinal cord is damaged, which can lead to temporary or permanent paralysis. Spinal injuries are often the result of an impact, such as falling off a ladder or horse, landing awkwardly on a trampo-line, diving into a shallow pool, or suffering a misplaced football tackle. Symptoms often include pain in the neck or back, irregularity in the normal curve of the spine, paralysis, abnormal sensations, and loss of bladder or bowel control.
1. If spinal injury is suspected, call for emergency medical assistance.
2. Keep the patient still. Brace his head on both sides using rolled up clothes or towels. Do not roll him over or straighten him out; instead, leave him in the position that you found him.
3. If the patient is wearing a helmet, do not remove it.
4. Provide emergency first aid if needed, such as stopping any bleeding. But try to do so without moving the patient's head or neck.
5. Monitor the patient's vital signs. If he stops breathing, administer CPR—chest compressions only.
• Towels
A strain is an injury to the muscles or tendons, and is the result of the muscle being overstretched. The muscle can be partially torn or fully ruptured. The injury often occurs at the junction between the muscle and the tendon that joins it to the bone.
A sprain is an injury to the ligaments connecting bones together or holding joints in place. The ligament can be stretched, partially torn, or completely separated. Ankle and knee sprains are the two most common types. Sprains cause rapid swelling and can be very painful. Generally, the greater the pain, the more severe the sprain. Most minor sprains can be treated without medical assistance by keeping the swelling down and treating the pain.
1. Help the patient sit or lie down. Support the injured limb in a comfortable raised position using pillows or other soft materials.
2. Apply a cold pack to the area immediately after injury.
3. Compress the area with an ACE bandage or neoprene wrap.
4. Elevate the injured limb above the patient's heart whenever possible to prevent swelling.
5. Use over-the-counter anti-inflammatories/pain relievers to help with swelling and pain.
6. The injured person may require the use of crutches or splints for two to three days. During this time, apply a cold pack for ten to fifteen minutes at a time, four times a day.
7. If the sprain isn't improving after three days, consult a doctor.
8. If a fever develops, or if the joint feels unstable, seek emergency medical assistance.
• Cold pack
• ACE bandage or neoprene wrap
• Over-the-counter anti-inflammatories, pain relievers
• Crutches
Strokes are the third most common cause of death in the United States. The condition is more common in older people and is often associated with circulatory system disorders such as high blood pressure.
A stroke is caused from bleeding in the brain or when the blood flow into the brain is interrupted (usually by a clot in a blood vessel). Within minutes, blood cells start dying—a process that may continue for several hours. The best ways to prevent brain damage are to recognize the symptoms and quickly seek emergency medical treatment.
Symptoms of a stroke may include:
• Sudden weakness or numbness in the face, arm, or leg on one side of the body
• Sudden dimness, blurring, or loss of vision, particularly in one eye
• Trouble talking or understanding speech
• Sudden and severe headache
• Dizziness
1. Ask the patient to smile while you are looking at his face. If he is having a stroke, one side of his mouth may droop.
2. Ask the patient to raise both his arms out to his sides. If he is having a stroke, he may be able to lift only one arm out straight.
3. Ask the person several questions and see if he responds intelligibly. If he is unable to understand you or reply coherently, he may be suffering from a stroke.
4. Based on your assessment, if you suspect a person is having a stroke, call for emergency medical assistance.
• None
Overexposure to the sun can cause sunburn. Numerous medicines, including some antibiotics and chemotherapy drugs, can trigger hypersensitivity to the sun, making the skin burn very easily. Sunburn is prevented by staying in the shade or applying protective sunscreen. Symptoms of sunburn usually appear within a few hours and may include pain, redness, swelling, and blistering. If sunburn covers a large portion of the body, it can also cause headache, fever, and fatigue.
1. Cover the burn with a cool wet cloth, or have the patient take a cool bath.
2. Apply aloe vera, calamine, or moisturizing lotion several times a day. Do not use petroleum jelly, butter, or other home remedies.
3. Leave any blisters intact to speed healing and avoid infection. Apply antibiotic ointment to any that burst.
4. Administer over-the-counter pain reliever for pain as needed.
5. If complications develop, such as rash, fever, or blistering, seek medical care.
• Aloe vera, calamine, or moisturizing lotion
• Over-the-counter pain reliever
If an adult tooth is knocked out, it may be possible to replant it in the socket, either at home or at the dentist's office. Proper handling of the tooth is critical to improving the chances of a successful replanting.
1. Retrieve the tooth, handling it only by the top, not the roots.
2. Do not rub or scrape the tooth to remove debris since this might damage the roots.
3. Rinse away any dirt with milk (or lukewarm water if milk is unavailable).
Save-A-Tooth
4. Try to replant the tooth back into the socket. If it doesn't fully reseat, have the patient bite down slowly and gently on a gauze or moistened tea bag. Have him hold the tooth in place while traveling to the dentist or hospital.
5. If you can't replace the tooth in the socket, put it in a plastic bag or container along with some milk or the patient's saliva. If you have a Save-A-Tooth preserving kit, use it.
6. Regardless of whether replanting is successful or not, seek immediate care from a dentist or hospital.
• Save-A-Tooth preserving system
• Gauze
• Milk
Toothaches are often the result of tooth decay. The first signs might be a painful sensation when eating something sweet, hot, or cold. When these early symptoms become evident, the patient should seek out dental care to address the underlying cause. If an injury to the mouth causes tooth pain, the patient should see his dentist immediately.
1. Have the patient rinse his mouth with warm water, and then use dental floss to remove any food particles that might be wedged between teeth.
2. Administer over-the-counter pain reliever as needed. You can also apply an over-the-counter antiseptic containing benzocaine directly to the irritated tooth or nearby gum.
3. Call the dentist or seek emergency care if:
• There are signs of infection such as swelling, pain, red gums, or foul discharge
• The pain persists for more than a day
• A fever is present
• The patient has trouble breathing or swallowing
• The toothache is a result of injury to the mouth
• Over-the-counter pain reliever
• Antiseptic containing benzocaine
A good first-aid kit is one stocked with items that you know how to use. There is no point in having a huge stockpile of medical supplies if you can't put them to use safely and effectively.
The following first aid kit is compiled to treat the first-aid conditions described above (as well as many others). For the most part, the supplies are readily available from your local drug store or through online medical supply stores. The quantities listed are completely subjective, based on family size, likelihood of injury, and types of expected injuries. You should stock your kit with enough supplies to meet your family's needs. It is also recommended that you build up a smaller first-aid kit, primarily focused on trauma, for inclusion in your roadside emergency kit (see Chapter 13).
To keep your medical supplies fresh, as well as maintain familiarity with your kit's contents, use your first-aid kit for your family's daily medical needs. As long as you are vigilant at replacing supplies as they are consumed, daily use in no way compromises your preparation for a more significant first aid emergency.
First-aid Kit |
||
Qty |
Item |
Use |
1 |
Large first-aid bag with individual compartments |
Contain your first-aid supplies |
1 |
Bottle of alcohol or alcohol wipes |
Disinfect tweezers, needles, or around wounds |
1 |
Bottle of Betadine or hydrogen peroxide |
Clean wounds when soap and water is unavailable |
1 |
Bottle of hand sanitizer or sanitizer wipes |
Sanitize hands when water is not available |
1 |
Bottle of mineral or baby oil |
Float insects out of ear |
1 |
Bottle of saline solution or eye wash |
Flush contaminant from eye |
1 |
Bottle of decongestant spray |
Clean blood clots from nose |
1 |
Tube of antiseptic containing benzocaine |
Apply for mouth pain |
10 |
Individual doses of burn gel (e.g., Water Jel) |
Treat burns, sunburn |
1 |
Bottle of aloe vera lotion or gel |
Treat sunburn |
1 |
Bottle of calamine lotion |
Treat poison ivy, sunburn |
1 |
Tube of hydrocortisone cream |
Treat insect bites or itchy rashes |
1 |
Tube of antibiotic cream or ointment |
Apply to wounds or broken blisters to prevent infection |
2 |
Pairs of rubber or latex gloves |
Protect against infection |
1 |
Tweezers |
Remove foreign objects |
1 |
Needle in protective case |
Remove splinters |
Penlight |
Examine eyes, ears, throat |
|
1 |
Bandage scissors |
Cut gauze, tape |
1 |
Rescue shears |
Cut away clothing |
1 |
Magnifying glass |
Examine wounds, foreign objects in eye and skin |
6 |
Safety pins or bandage clips |
Secure bandages |
1 |
Digital thermometer |
Measure temperature |
1 |
Small plastic bag |
Dispose of trash, bloody bandages |
1 |
Plastic measuring spoon |
Administer correct dosages of liquid medicines |
1 |
Roll of medical tape, 1 in. × 10 yds. |
Secure bandages and splints |
1 |
Bulb syringe, 3 oz. |
Remove congestion from nose; irrigate wounds |
1 |
Small package of cotton swabs (Q-tips) |
Clean around wounds; remove foreign object from eye |
3 |
Instant, disposable cold packs |
Reduce swelling; relieve pain |
1 |
SAM splints, 1 finger, 1 large (36 in.) |
Immobilize limb |
1 |
Roll of duct tape |
Immobilize limb |
1 |
Rescue blanket |
Treat for shock |
1 |
Epinephrine auto-injector |
Administer for anaphylactic shock |
1 |
Save-A-Tooth storage system |
Transport tooth to dentist or hospital |
1 |
Pocket mask |
Protect against infection when administering rescue breathing |
Bottle of acetaminophen or ibuprofen tablets |
Relieve pain in adults |
|
1 |
Bottle of acetaminophen or ibuprofen liquid |
Relive pain in children |
1 |
Bottle of aspirin |
Treat heart attack |
1 |
Bottle of diphenhydramine anti-histamine pills |
Treat allergic reaction |
1 |
Package of pink bismuth tablets (or bottle of liquid) |
Treat upset stomach, diarrhea, and indigestion |
50 |
Adhesive bandages, assorted sizes |
Cover minor scrapes, cuts, and punctures |
20 |
Gauze pads, assorted sizes |
Cover wounds; clean around wounds; insert lost tooth |
20 |
Non-stick gauze pads, assorted sizes |
Cover burns, blisters, wounds |
2 |
Conforming gauze rolls, 4 in. wide |
Secure bandages; compress joints |
2 |
Eye pads |
Protect injured eye |
10 |
Trauma pads, 5 in. × 9 in and 8 in. × 10 in. |
Stop bleeding of deep wounds |
1 |
Multi-trauma dressing, 10 in. × 30 in. |
Protect and pad major wounds |
2 |
Bloodstopper compress dressings |
Stop bleeding of deep wounds |
2 |
Water-Jel burn dressings, 4 in. × 4 in., 4 in. × 16 in. |
Treat burns |
20 |
Fingertip and knuckle bandages |
Protect wounds on fingers and toes |
1 |
Triangle bandage, 40 in. |
Cover large wounds; secure limbs |
25 |
Butterfly wound closure strips, assorted sizes |
Hold wound edges together |
1 |
Notepad and pen |
Write down patient information, vital signs |
1 |
First-aid manual |
Guide your actions |
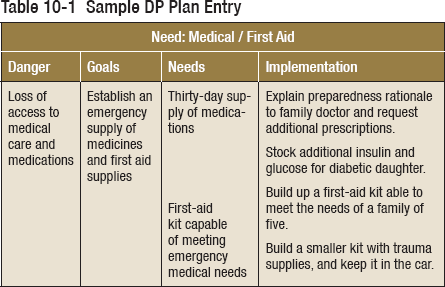
Quick Summary—Medical/First Aid
 Keep a minimum of a thirty-day supply of medicine for everyone in your family. Give special consideration to any critical medicinal needs, such as insulin, nitroglycerin, or pain medicine.
Keep a minimum of a thirty-day supply of medicine for everyone in your family. Give special consideration to any critical medicinal needs, such as insulin, nitroglycerin, or pain medicine.
 Everyone in your family should learn first aid. Critical life-saving first aid includes: administering CPR, stopping heavy bleeding, recognizing the signs of a stroke, treating for shock, responding correctly to poisoning, and delivering abdomen thrusts to a choking victim.
Everyone in your family should learn first aid. Critical life-saving first aid includes: administering CPR, stopping heavy bleeding, recognizing the signs of a stroke, treating for shock, responding correctly to poisoning, and delivering abdomen thrusts to a choking victim.
 When placing an emergency call, try to use a landline so the dispatcher can immediately determine your location.
When placing an emergency call, try to use a landline so the dispatcher can immediately determine your location.
 First-aid care is not meant to replace professional emergency medical treatment.
First-aid care is not meant to replace professional emergency medical treatment.
 An effective first-aid kit is one that contains medical supplies that you know how to use.
An effective first-aid kit is one that contains medical supplies that you know how to use.