3.9 Neuropsychological and Psychiatric Examination
Many neurologic illnesses are associated with more or less severe
disturbances of cognitive and emotional function. The organic neurologic
clinical picture is only complete when any psychopathologic abnormalities
that may be present have been thoroughly assessed and documented. The goal
of the neuropsychological examination is to reveal cognitive deficits
(especially aphasia, agnosia, and apraxia) and processing disturbances that
imply the presence of a focal brain lesion.
3.9.1 Psychopathologic Findings
The examiner should first determine whether the patient is awake and
alert. If not, he or she will be unable to receive and process incoming
stimuli in the normal way. The patient may have an impairment of consciousness ranging in severity from drowsiness
to coma, as described in ▶ Table 3.10.
Table 3.10 Degrees of impairment of consciousness,
and other abnormal states of consciousness
|
Designation
|
Features
|
|
Normal consciousness
|
Oriented to place, time, and person (self), answers
questions promptly and appropriately, follows commands
correctly
|
|
Drowsiness
|
Mostly awake, responds to questions and commands slowly
but usually correctly (after repetition if necessary), moves
in response to a sufficiently intense stimulus, usually
oriented and coherent
|
|
Somnolence
|
Mostly asleep, arousable with a moderately intense
stimulus, generally requires repetition of questions or
commands but then responds correctly, reacts slowly and
after a delay but usually correctly
|
|
Stupor
|
Asleep unless awakened, can only be awakened with a strong
(auditory) stimulus or perhaps only with a mechanical
stimulus, cannot answer questions or follow commands or does
so only after intense repetition, and then only
incompletely
|
|
Coma
|
Unconscious, cannot be awakened, does not respond to a
verbal or auditory stimulus, may respond to painful stimuli
of graded intensities with specific (localizing)
self-defense, nonlocalizing withdrawal of a limb, or
abnormal flexion or extension responses
|
|
Confusion
|
Inappropriate spontaneous behavior and responses to
questions and commands, deficient orientation to place,
time, and/or person (self); the confused patient may be
fully conscious, less than fully conscious, or agitated (see
below)
|
|
Agitation
|
Motor unrest, inappropriate spontaneous behavior, cannot
be calmed by verbal persuasion, more or less disoriented,
does not follow commands appropriately
|
In addition to the patient’s level of consciousness and
attention, the examiner should assess his or her orientation, concentration, memory, drive, affective state, and cognitive
ability. The overall psychopathologic picture is composed of
these elements. If mental functioning is disturbed by an underlying
neurologic illness (so-called psycho-organic
syndrome or organic brain syndrome),
the manifestations often progress in a characteristic sequence, regardless
of the etiology. At first, short- and long-term memory, concentration, and
attention are impaired; the patient is easily fatigued and has difficulty
processing new information or performing complex tasks. Later, the patient
becomes progressively disoriented, first to time, then to place, and then to
person (self). Reactive depression is common at this stage. Ultimately, all
spontaneous activity ceases; the patient loses interest, lacks drive, and
becomes permanently confused. Disturbances of this type can often be
discerned in the patient’s behavior before the formal examination begins,
growing increasingly evident to the examiner during history-taking and
physical examination. Further details of the patient’s history from the
family can often help. The Mini-Mental State
Examination ( ▶ Table 3.11, ▶ Fig. 3.36) and the clock test
( ▶ Table 3.12)
are widely used to assess cognitive function; the MOCA test is a
well-validated alternative (see www.mocatest.org). For acquired dementia,
see section ▶ 6.12.
Table 3.11 Mini-Mental State Examination
|
Parameter
|
Questions
|
|
Name of patient:
Date of birth:
Date of examination:
1 point for each correct answer
|
|
Orientation in time
|
|
1.
|
|
|
2.
|
|
|
3.
|
|
|
4.
|
|
|
5.
|
|
|
Orientation to place
|
|
6.
|
|
|
7.
|
|
|
8.
|
|
|
9.
|
|
|
10.
|
|
|
Retentiveness
|
|
“Please repeat the following words” (to be spoken at one
word per second; to be performed only once)
|
|
11.
|
|
|
12.
|
|
|
13.
|
|
|
Attention and calculations
|
|
14.
|
“Please count from 100 backward by sevens” (serial-7
test). One point for each correct subtraction, maximum five
points
|
|
Recent memory
|
|
15.
|
“Which three words did you repeat earlier?” One point for
each word correctly recalled
|
|
Language, naming
|
|
16.
|
|
|
17.
|
|
|
18.
|
|
|
Language comprehension, motor
execution
|
|
19.
|
|
|
20.
|
|
|
21.
|
|
|
Reading
|
|
22.
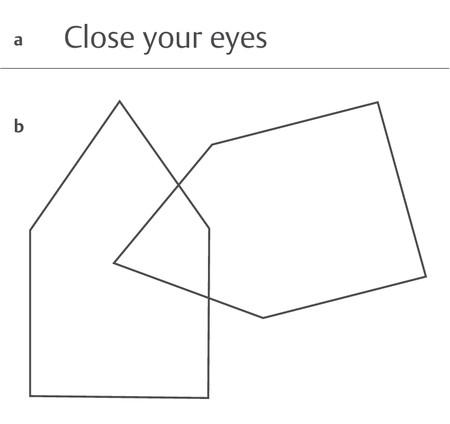
|
“Please do what it says on this card” (show card: “Close
your eyes”) ( ▶ Fig. 3.36a)
|
|
Writing
|
|
23.
|
“Write any sentence” (the patient is given a piece of
paper and something to write with)
|
|
Drawing
|
|
24.
|
“Please copy this drawing” (overlapping pentagons, ▶ Fig. 3.36b;
all 10 edges of the two pentagons must be drawn, and the
pentagons must overlap, for the patient to receive one point
for this task)
|
|
Level of wakefulness:
|
|
Total points achieved:
|
Table 3.12 The clock test
|
Task
The patient is given a piece of paper with an
empty circle drawn on it and is asked to complete the
drawing of a clock, including numbers and hands. The time
shown should be 10 minutes past 11 o’clock.
|
|
Interpretation
|
Points if correct
|
|
Are all 12 numbers present?
|
1
|
|
Is the number “12” at the top?
|
2
|
|
Are two hands of different lengths present?
|
2
|
|
Is the indicated time correct?
|
2
|
|
Note: A score of 5 or below raises the
suspicion of dementia.
|
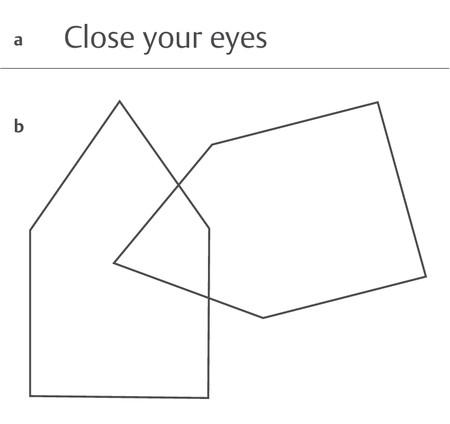
Fig. 3.36 Forms for the
Mini-Mental State Examination. a A written command for
the patient to follow (Task 22 in ▶ Table 3.11). b Pentagons to be copied (Task 24 in ▶ Table 3.11). (Reproduced from Mattle H, Mumenthaler
M. Neurologie. 13th ed. Stuttgart: Thieme; 2013.)
3.9.2 neuropsychological Examination
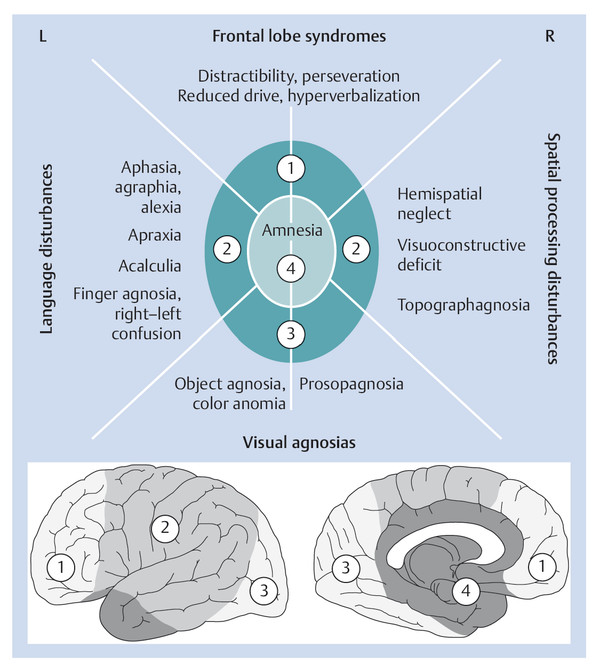
The localizing significance of various neuropsychological deficits is
shown in ▶ Fig. 3.37. An overview of important neuropsychological
terms and syndromes is provided in ▶ Table 3.13.
Table 3.13 Important neuropsychological terms and
syndromes
|
Aphasia
|
Cortical disturbance of language, usually due to a
left-hemispheric lesion
|
|
Spatial processing
disturbance
|
Difficulty drawing or copying three-dimensional figures
(cube, house, five-pointed star); neglect of the left side
of space or the left side of the body (so-called hemispatial
neglect); usually due to a right-hemispheric lesion
|
|
Apraxia
|
Disturbance of the goal-directed execution of complex
behaviors or behavioral sequences, or of the use of
tools:
More common with left-hemispheric than with
right-hemispheric lesions
|
|
Agnosia
|
Disturbance of the ability to recognize and correctly
interpret various kinds of sensory stimuli, despite intact
sensory function.
-
Visual agnosia: inability
to recognize objects visually despite intact vision.
Special types: color agnosia, prosopagnosia
(inability to recognize faces). The responsible
lesion is located in the occipital or
occipitotemporal visual cortex
-
Tactile agnosia: objects
cannot be recognized by touch with the eyes
closed
-
Anosognosia: deficit of
self-awareness, i.e., denial or trivialization of
one’s own pathologic deficits
|
Aphasia
Language is a complex process encompassing numerous individual
functions ( ▶ Table 3.14).
Table 3.14 Functions that are needed for normal
language
|
Function
|
Disturbance
|
|
Hearing
|
Hearing impairment, deafness
(section ▶ 12.6.1)
|
|
Comprehension
|
Sensory aphasia
|
|
Construction of words and thoughts
|
|
|
Construction of speech
|
Motor aphasia
|
|
Phonation and articulation
|
Hoarseness (section ▶ 12.7), dysarthria (see
sections ▶ 3.9.1, ▶ 5.5.5, and ▶ 12.9)
|
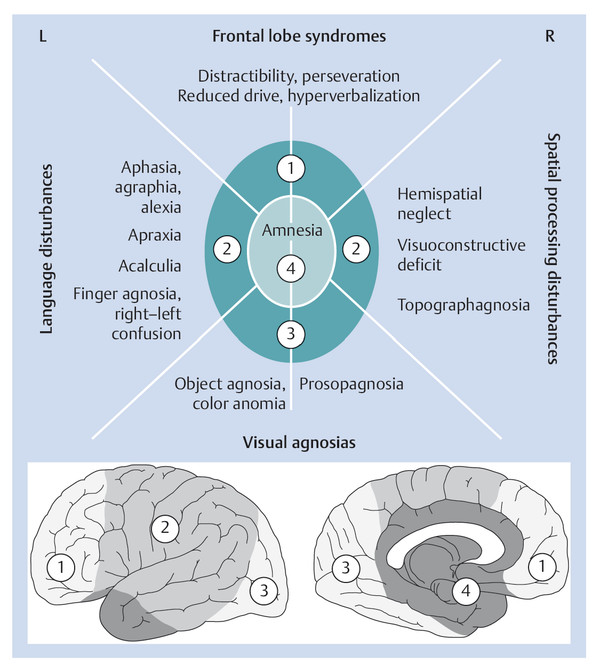
Fig. 3.37 Cognitive
deficits that typically result from various focal
brain lesions. (Adapted from Schnider A. Verhaltensneurologie.
2nd ed. Stuttgart: Thieme; 2004.)
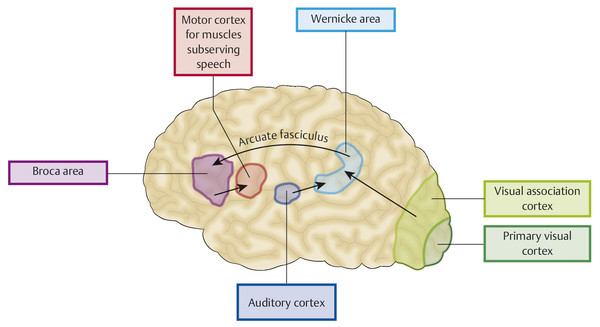
Cortical disturbances of language are called aphasia and are due to a lesion in the language-dominant
hemisphere. The left hemisphere is dominant for language in nearly all
right-handers and in most left-handers as well. The clinical varieties
of aphasia are:
-
Disturbances of language production (motor aphasia or Broca aphasia; ▶ Fig. 3.38 and
▶ Fig. 4.12): the
patient’s spontaneous speech is not fluent, even though the
“organic prerequisites” for speech production (phonation,
breathing, orofacial musculature) are all apparently
unimpaired.
-
Disturbances of language comprehension (sensory aphasia or Wernicke aphasia;
▶ Fig. 3.38 and
▶ Fig. 4.12): the
patient has trouble understanding speech despite intact hearing
and auditory processing. The patient’s spontaneous speech is
fluent.
-
Disturbances of speech repetition. The patient cannot
correctly repeat words or sentences spoken by the
examiner.
-
Nearly all patients with aphasia have difficulty with naming
and word-finding.
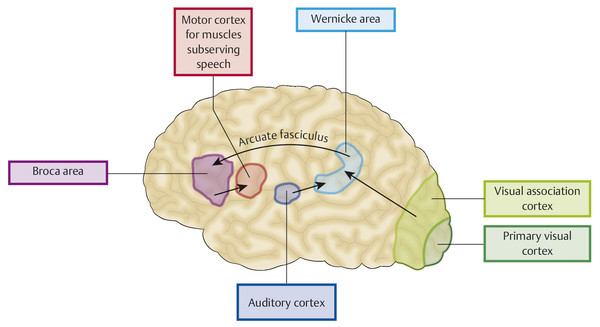
Fig. 3.38 Brain
structures that participate in language
function.
The examiner begins to assess the patient’s spontaneous
speech while taking the history; if necessary, the patient can be given
specific language tasks, for example, “Describe this picture.” Various
kinds of abnormality may be noted. The patient’s utterances may be found
to be unusually poor in meaning-bearing words and overloaded with
connectives and “function words.” Sentences may be faultily constructed
(paragrammatism). The flow of speech may be
either considerably greater than normal or slow and hesitant (telegraphic speech). Individual words may be
deformed in certain characteristic ways (e.g., sound substitutions or
phonemic paraphasias, such as “cog” for
“dog”), or words may be used in place of other words from the same
semantic category (semantic paraphasias, e.g.,
“table” for “chair”). Some words may be replaced by invented pseudowords
(neologisms). Impaired language
comprehension may be manifested by the patient’s inability to point out
various objects in the room, including parts of his or her own body,
when these are named by the examiner. Complex commands are an even more
sensitive functional test. The patient can be asked, for example, to
place a certain named object in between two other named objects, or to
interpret a complicated sentence, such as the following: “Not in the
closet, but on top of it, was where he had put his hat. Where was the
hat?” Aphasic patients often make mistakes when they repeat spoken
sentences or name objects (including parts of the body) that are pointed
out to them. Reading and writing may also be impaired, often to a
greater extent than spoken language.
The different types of aphasia are classified by the characteristics
of the patient’s spontaneous speech, comprehension and repetition of
speech, word-finding, and naming ( ▶ Table 3.15). An aphasic patient whose
spontaneous speech lacks fluency speaks slowly, with effort, in short
sentences containing many meaning-bearing words, with paraphasias and
altered melody of speech (dysprosody). An aphasic patient with fluent
spontaneous speech speaks at normal speed, effortlessly, and with the
normal melody of speech (prosody), but the sentences are of normal
length but contain relatively few meaning-bearing words in relation to
meaningless filler words and literal and semantic paraphasias.
Table 3.15 The classification and differential
diagnosis of aphasia
|
Type of aphasia
|
Spontaneous speech
|
Comprehension
|
Repetition
|
Naming, word-finding
|
|
Motor aphasia
(Broca)
|
Nonfluent
|
Normal
|
Impaired
|
Impaired
|
|
Sensory aphasia
(Wernicke)
|
Fluent
|
Impaired
|
Impaired
|
Impaired
|
|
Conduction aphasia
|
Fluent
|
Normal
|
Impaired
|
Impaired
|
|
Global aphasia
|
Nonfluent
|
Impaired
|
Impaired
|
Impaired
|
|
Transcortical motor aphasia
|
Nonfluent
|
Normal
|
Normal
|
Impaired
|
|
Transcortical sensory aphasia
|
Fluent
|
Impaired
|
Normal
|
Impaired
|
|
Anomic aphasia
|
Fluent
|
Normal
|
Normal
|
Impaired
|
Dysarthria is not a disturbance of
language, but of the mechanical process of speech production
(articulation); the content of speech is normal. When the motor
apparatus of speech is affected by a central paresis or a muscular
coordination disorder, the patient’s speech becomes unclear or slurred,
perhaps even unintelligible.
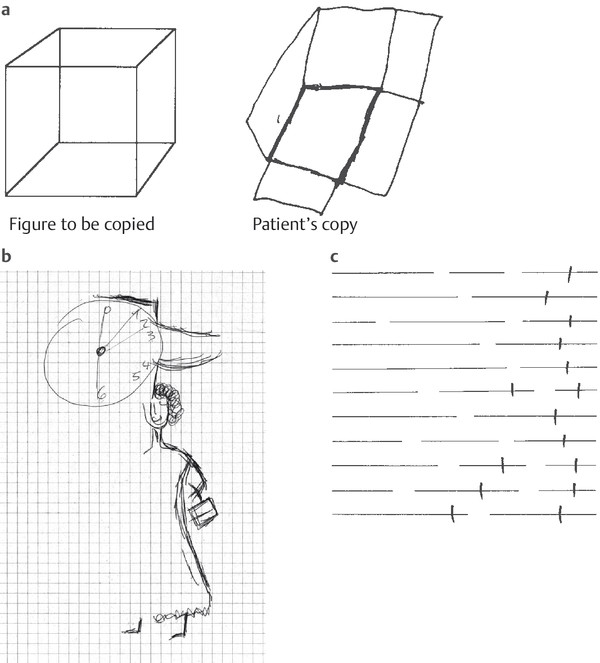
Disturbances of Spatial Processing
Disturbances of spatial processing are usually caused by
right-hemispheric lesions. They are manifested, for example, by unusual
difficulty in spontaneously drawing or copying three-dimensional figures
(cube, house, etc.) ( ▶ Fig. 3.39a). Deficits of
this kind are often accompanied by neglect of the left side of space and
the left half of the patient’s own body (hemispatial
neglect; ▶ Fig. 3.39b,c).
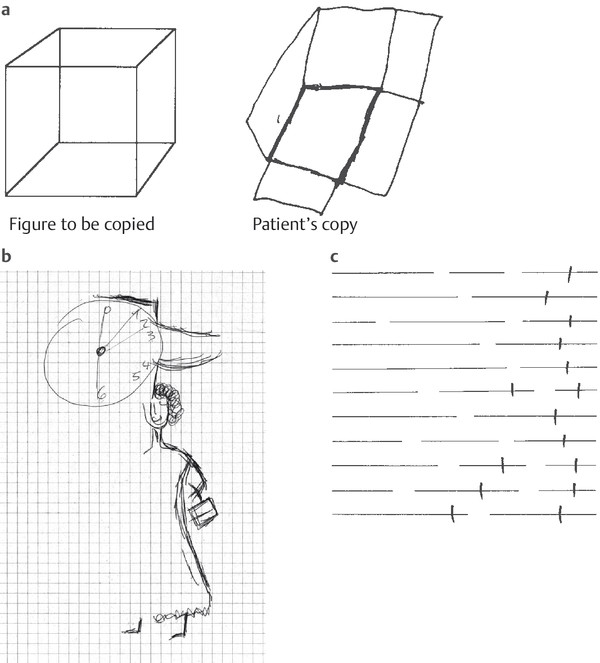
Fig. 3.39 Spatial
processing and neglect. a Cube-drawing as a test of spatial
processing. This drawing is by a patient with a right
parietal lesion. b Drawings of a clock and a
woman. The left half of each is missing, indicating
severe left hemineglect. The patient had sustained an acute
hemorrhage in the right parietal lobe. c
Line-dividing test. The patient was a university
professor with left-sided neglect due to a tumor (astrocytoma)
in the right hemisphere. (Reproduced from Mattle H, Mumenthaler
M. Neurologie. 13th ed. Stuttgart: Thieme; 2013.)
Memory and Amnesia
Memory enables us to store and recall information; it makes
learning possible. There is a somewhat arbitrary distinction between
short- and long-term memory; the
latter, in turn, is divided into recent and old
memory.
Short-term memory, also called working
memory, is that which we are able to keep in mind at any one
moment. Its content is rapidly lost unless it is kept active by
repetition and transferred to long-term memory.
The examiner gains a first impression of the patient’s short- and
long-term memory while taking the history. To test short-term memory, one can ask the patient to repeat
sequences of numbers forward and backward or to take mental note of a
sequence of 3 to 10 words and repeat them, immediately and a few minutes later.
Old memory can be tested by asking
the patient to state autobiographic data that can be checked against
other sources, facts about his or her own family, or information about
historical dates, political events, or public figures. The findings
should be interpreted in the light of the patient’s premorbid level of
intelligence and education.
Short-term memory and verbal memory are mainly subserved by the limbic
system (section ▶ 5.5.4) and
hippocampus. Memory disturbances are called amnesia.
Amnesia is the inability to
store or recall conscious memories. Anterograde amnesia is the inability to lay down new
memories from the moment of a brain injury onward. Retrograde amnesia is the inability to recall
information that was acquired before the brain injury. Persistent
amnesia is the main clinical manifestation of dementia
(section ▶ 6.12).
Apraxia
Disturbances in the goal-directed execution of complex
actions or sequences of actions, or in the use of objects, are known as
apraxia. If the individual components of a
single action cannot be put together
correctly, the patient is suffering from ideomotor
apraxia. Different parts of the body can be affected
individually. In facial apraxia, for example, the patient may be unable
to follow commands to execute certain motor tasks with the face, e.g.,
drinking through a straw or clicking the tongue. A patient with
ideomotor apraxia of the upper limbs may be unable to salute or to mime
the action of slapping someone in the face; a patient with ideomotor
apraxia of the lower limbs may be unable to kick an imaginary football.
In ideational apraxia, individual actions can
be performed, but cannot be combined into more complex sequences. A
patient might thus be unable to ready a letter for mailing, as this
requires several steps: folding the letter, putting it in the envelope,
sealing the envelope, and putting a stamp on it. Cortical lesions
causing apraxia are usually on the left side.
Agnosia
Agnosia is an inability to recognize and correctly
interpret incoming stimuli in a particular sensory modality, even though
sensation as such is intact. A patient with visual
agnosia, for example, has no visual impairment but cannot
recognize objects on sight; the patient can name an object only after
feeling or hearing it (e.g., the jangling of a bunch of keys). Special
types of visual agnosia include an inability to recognize colors (color
agnosia) or faces (prosopagnosia). The responsible lesion is in the
visual association cortex, that is, in the occipital or occipitotemporal
region, in one or both hemispheres.
Stereognosis is tested by putting a familiar object (key,
pair of scissors) in the patient’s hand and asking him or her to palpate
and name it (with eyes closed). An inability to do this despite intact
sensation is called tactile agnosia. Further
special types of agnosia are finger agnosia and autotopagnosia
(difficulty recognizing parts of one’s own body).
Anosognosia is the denial or
trivialization of one’s own neurologic deficits, for example, hemiplegia
or even blindness.
Higher Cognitive Functions
For an individual to thrive in his or her social environment and cope
adequately with the demands of everyday life, more is needed than just a
properly functioning interaction of the basic neuropsychological
functions described earlier. A person’s fund of knowledge, memory,
intelligence (i.e., the capacity for abstract thought and
problem-solving), personality, and social behavior are all of vital
importance, as are his or her mood and motivation. The assessment of
these higher cognitive functions requires careful weighing of biographic
historical information (particularly useful when derived from persons in
the patient’s social environment: family, friends, colleagues), as well
as standardized neuropsychological testing. For example, there are
specific tests for the patient’s fund of knowledge, logical thinking,
and cognitive skills such as difference recognition, category formation,
and the interpretation of symbolic information, for example, proverbs.
These higher integrative functions are performed by the cerebral cortex
in collaboration with other, deeper regions of the brain.