Chapter V
MEDICAL
WARNING: These emergency medical procedures are for survival situations. Obtain professional medical treatment as soon as possible.
1. Immediate First Aid Actions
Remember the ABC a of Emergency Care:
Airway Breathing Circulation
a. Determine responsiveness as follows:
(1) If unconscious, arouse by shaking gently and shouting.
(2) If no response—
(a) Keep head and neck aligned with body.
(b) Roll victims onto their backs.
(c) Open the airway by lifting the chin (Figure V-1).
(d) Look, listen, and feel for air exchange.
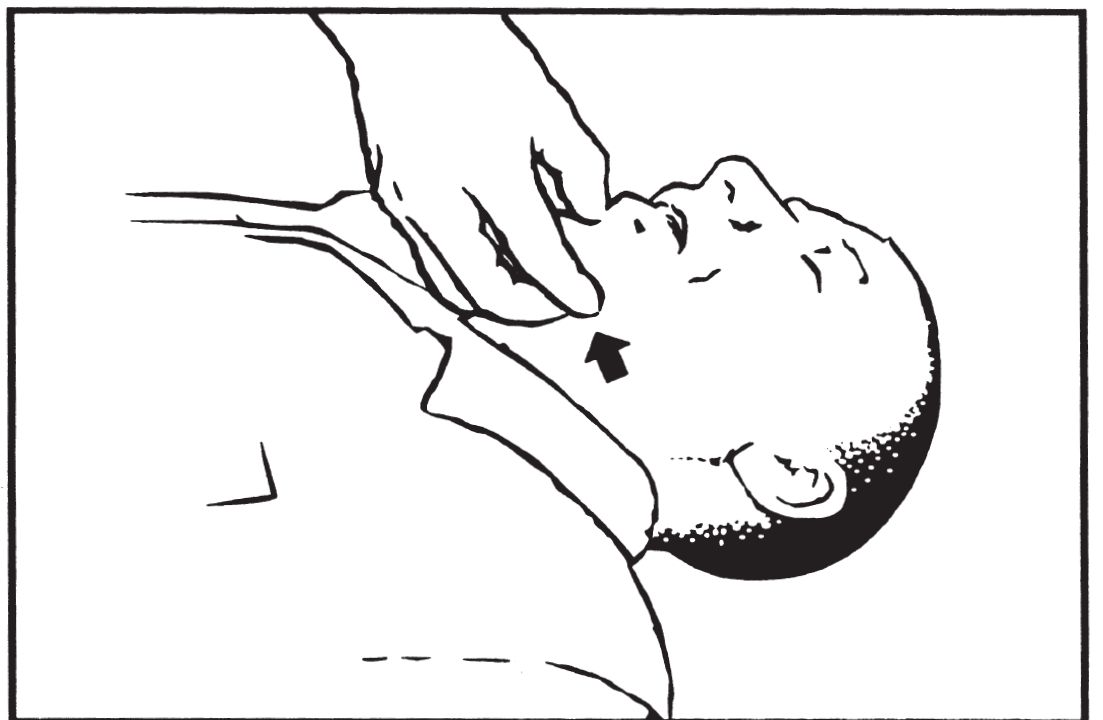
Figure V-1. Chin Lift
(3) If victim is not breathing—
(a) Check for a clear airway; remove any blockage.
(b) Cover victim’s mouth with your own.
(c) Pinch victim’s nostrils closed.
(d) Fill victim’s lungs with 2 slow breaths.
(e) If breaths are blocked, reposition airway; try again.
(f) If breaths still blocked, give 5 abdominal thrusts:
•Straddle the victim.
•Place a fist between breastbone and belly button.
•Thrust upward to expel air from stomach.
(g) Sweep with finger to clear mouth.
(h) Try 2 slow breaths again.
(i) If the airway is still blocked, continue (c) through (f) until successful or exhausted.
(j) With open airway, start mouth to mouth breathing:
•Give 1 breath every 5 seconds.
•Check for chest rise each time.
(4) If victim is unconscious, but breathing—
(a) Keep head and neck aligned with body.
(b) Roll victim on side (drains the mouth and prevents the tongue from blocking airway).
(5) If breathing difficulty is caused by chest trauma, refer to page V-7, paragraph 1d, Treat Chest Injuries.
CAUTION: DO NOT remove an impaled object unless it interferes with the airway. You may cause more tissue damage and increase bleeding. For travel, you may shorten and secure the object.
b. Control bleeding as follows:
(1) Apply a pressure dressing (Figure V-2).
(2) If STILL bleeding—
(a) Use direct pressure over the wound.
(b) Elevate the wounded area above the heart.
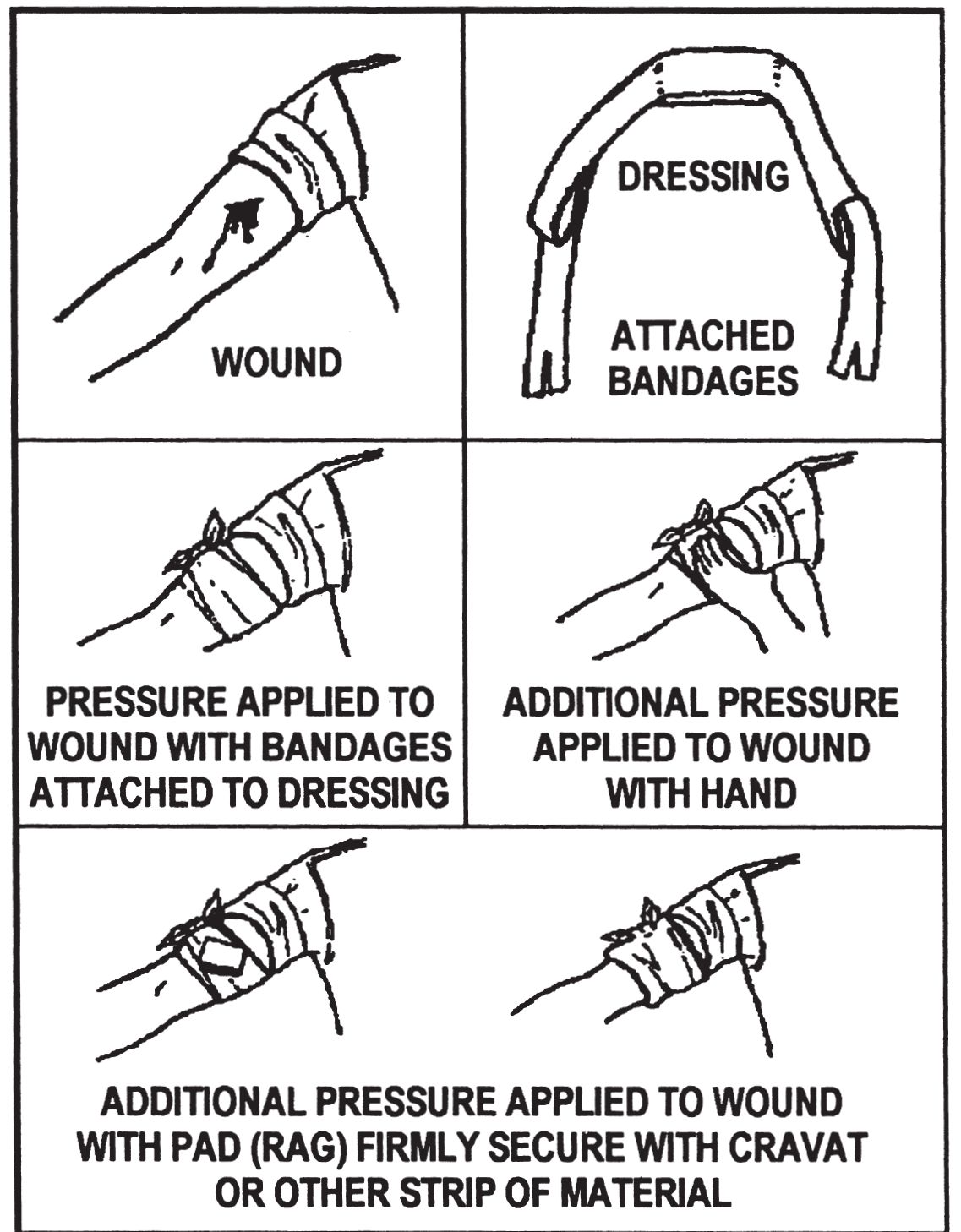
Figure V-2. Application of a Pressure Dressing
(3) If STILL bleeding—
(a) Use a pressure point between the injury and the heart (Figure V-3).
(b) Maintain pressure for 6 to 10 minutes before checking to see if bleeding has stopped.
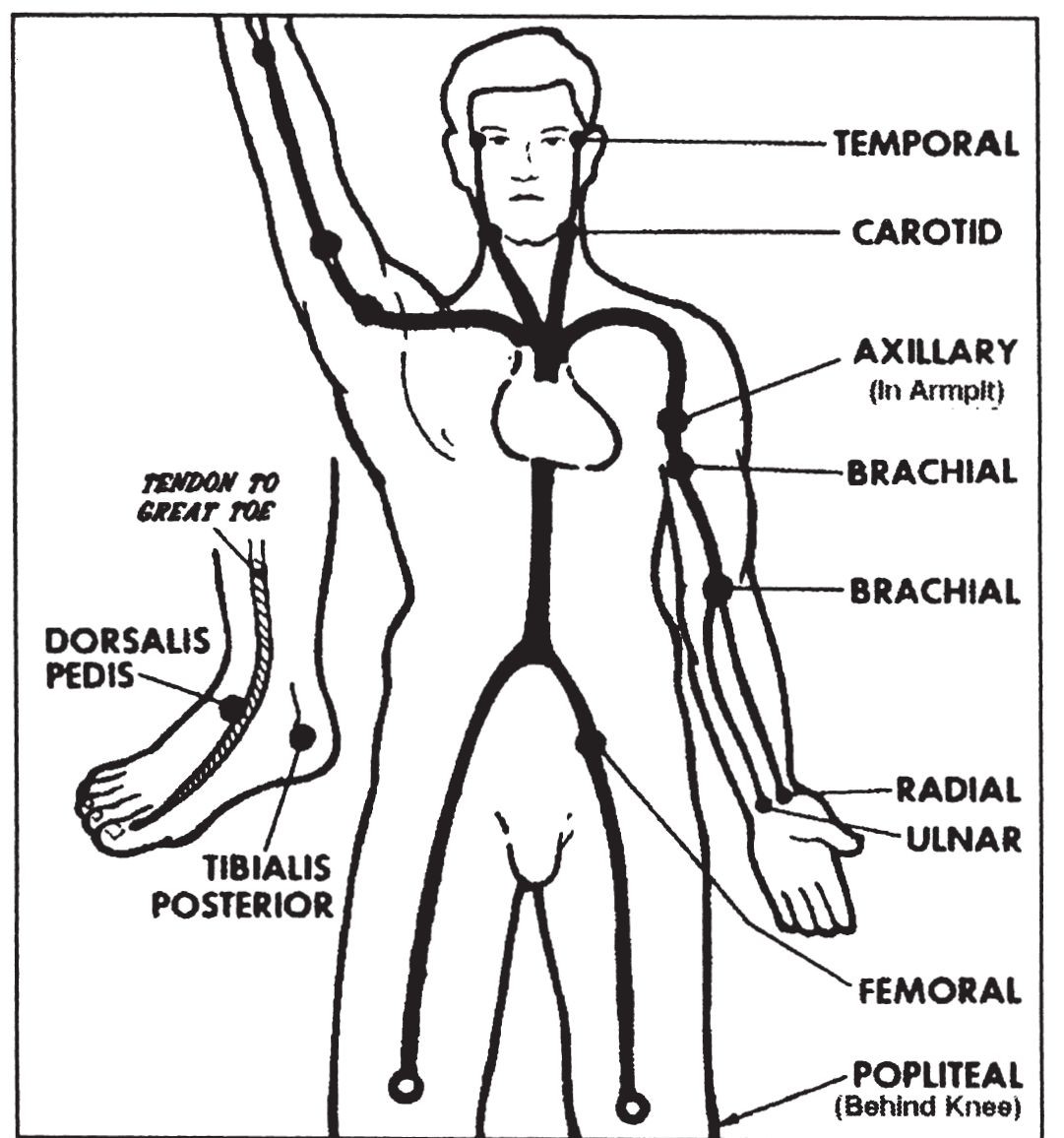
Figure V-3. Pressure Points
(4) If a limb wound is STILL bleeding—
CAUTION: Use of a tourniquet is a LAST RESORT measure. Use ONLY when severe, uncontrolled bleeding will cause loss of life. Recognize that long-term use of a tourniquet may cause loss of limb.
(a) Apply tourniquet (TK) band just above bleeding site on limb. A band at least 3 inches (7.5 cm) or wider is best.
(b) Follow steps illustrated in Figure V-4.
(c) Use a stick at least 6 inches (15 cm) long.
(d) Tighten only enough to stop arterial bleeding.
(e) Mark a TK on the forehead with the time applied.
(f) DO NOT cover the tourniquet.
CAUTION: The following directions apply ONLY in survival situations where rescue is UNLIKELY and NO medical aid is available.
(g) If rescue or medical aid is not available for over 2 hours, an attempt to SLOWLY loosen the tourniquet may be made 20 minutes after application. Before loosening—
•Ensure pressure dressing is in place.
•Ensure bleeding has stopped
•Loosen tourniquet SLOWLY to restore circulation.
•Leave loosened tourniquet in position in case bleeding resumes.
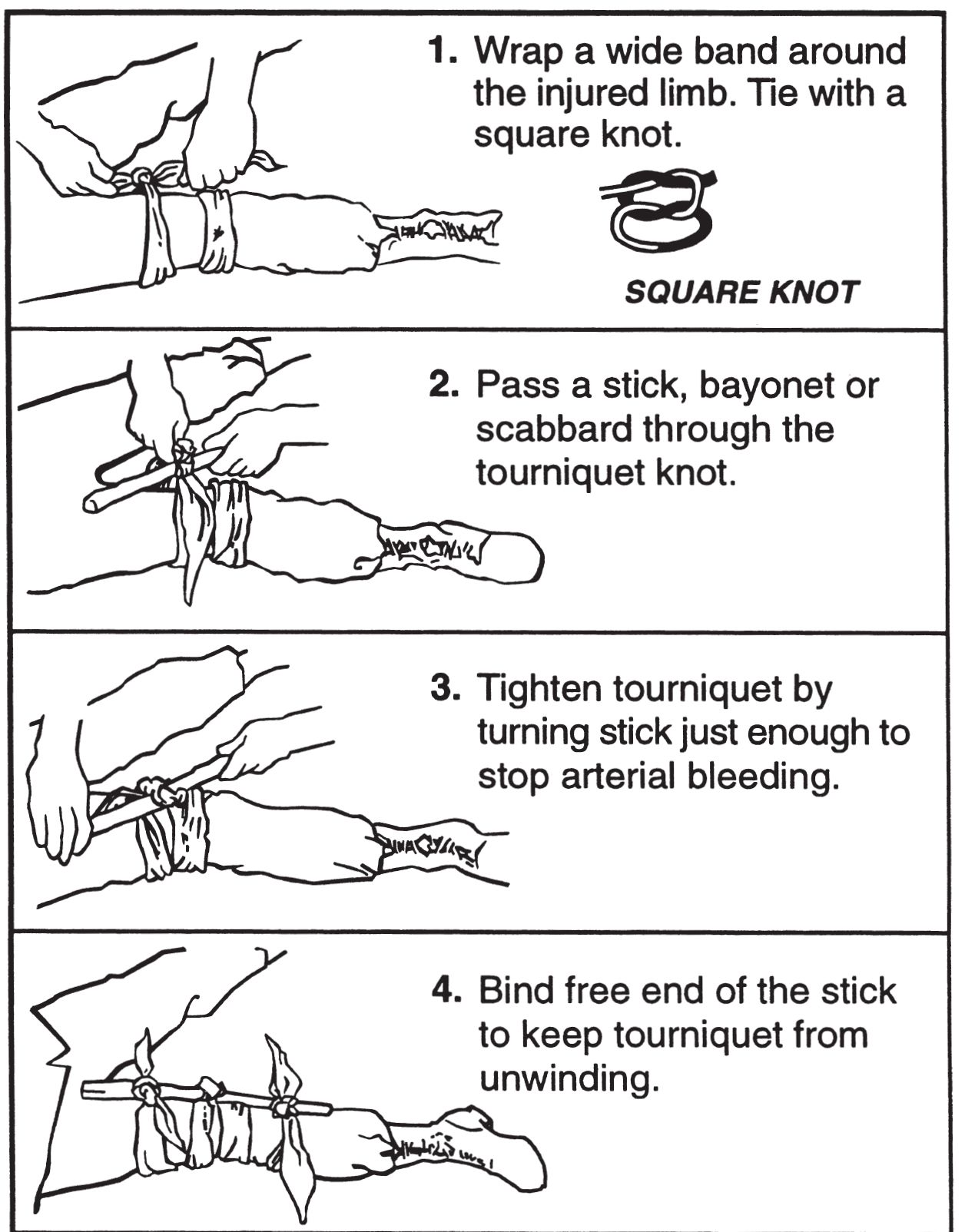
Figure V-4. Application of a Tourniquet
c. Treat shock. (Shock is difficult to identify or treat under field conditions. It may be present with or without visible injury.)
(1) Identify by one or more of the following:
(a) Pale, cool, and sweaty skin.
(b) Fast breathing and a weak, fast pulse.
(c) Anxiety or mental confusion.
(d) Decreased urine output.
(2) Maintain circulation.
(3) Treat underlying injury.
(4) Maintain normal body temperature.
(a) Remove wet clothing.
(b) Give warm fluids.
•DO NOT give fluids to an unconscious victim.
•DO NOT give fluids if they cause victim to gag.
(c) Insulate from ground.
(d) Shelter from the elements.
(5) Place conscious victim on back.
(6) Place very weak or unconscious victim on side, this will—
(a) Allow mouth to drain.
(b) Prevent tongue from blocking airway.
d. Treat chest injuries.
(1) Sucking chest wound. This occurs when chest wall is penetrated; may cause victim to gasp for breath; may cause sucking sound; may create bloody froth as air escapes the chest.
(a) Immediately seal wound with hand or airtight material.
(b) Tape airtight material over wound on 3 sides only (Figure V-5) to allow air to escape from the wound but not to enter.
(c) Monitor breathing and check dressing.
(d) Lift untapped side of dressing as victim exhales to allow trapped air to escape, as necessary.
(2) Flail chest. Results from blunt trauma when 3 or more ribs are broken in 2 or more places. The flail segment is the broken area that moves in a direction opposite to the rest of chest during breathing.
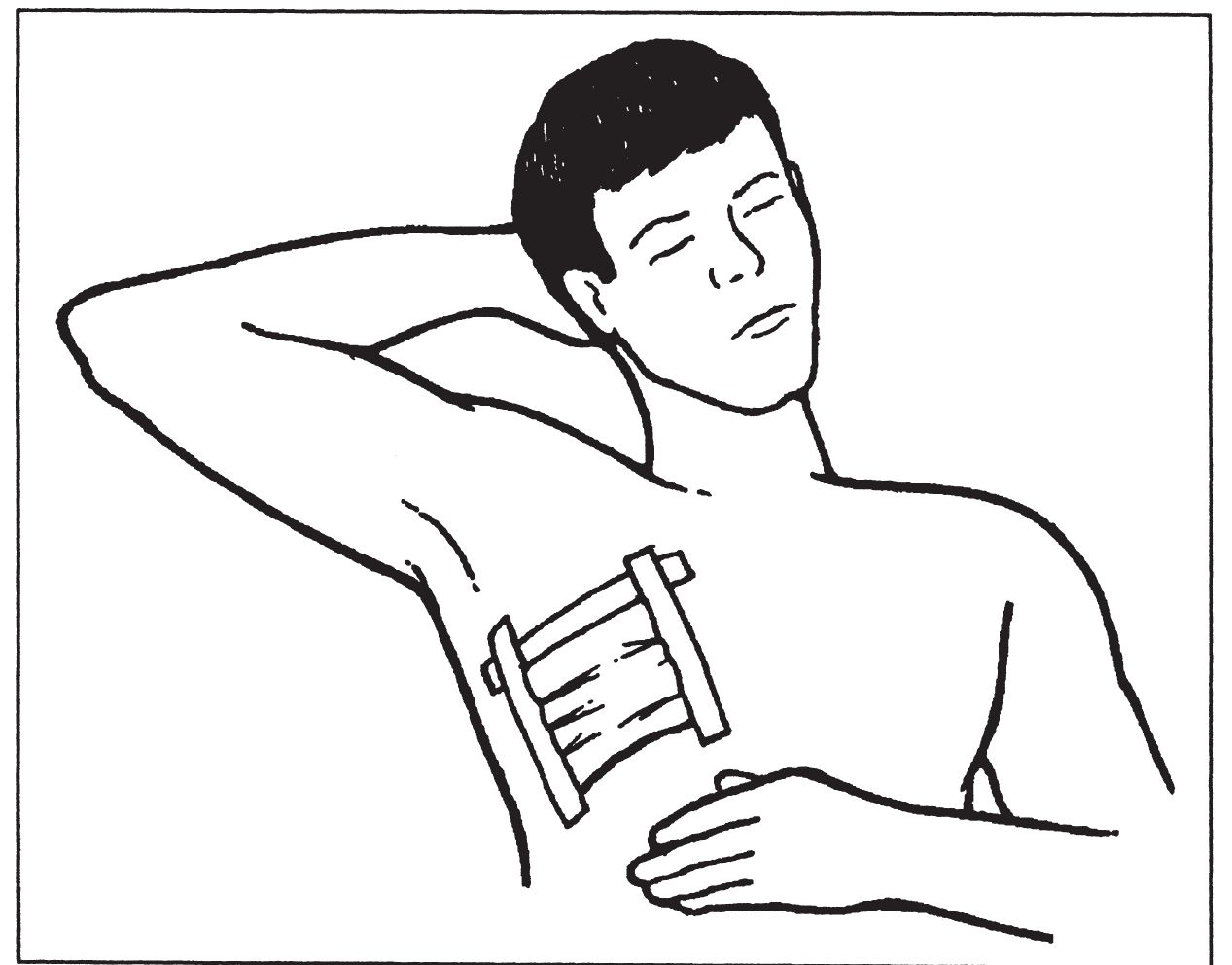
Figure V-5. Sucking Chest Wound Dressing
(a) Stabilize the flail segment as follows:
•Place rolled-up clothing or bulky pad over site.
•Tape pad to site
•DO NOT wrap tape around chest.
(b) Have victim keep segment still with hand pressure.
(c) Roll victim onto side of flail segment injury (as other injuries allow).
(3) Fractured ribs.
(a) Encourage deep breathing (painful, but necessary to prevent the possible development of pneumonia).
(b) DO NOT constrict breathing by taping ribs.
e. Treat fractures, sprains, and dislocations.
(1) Control bleeding.
(2) Remove watches, jewelry, and constrictive clothing.
(3) If fracture penetrates the skin—
(a) Clean wound by gentle irrigation with water.
(b) Apply dressing over wound.
(4) Position limb as normally as possible.
(5) Splint in position found (if unable to straighten limb).
(6) Improvise a splint with available materials:
(a) Sticks or straight, stiff materials from equipment.
(b) Body parts (for example, opposite leg, arm-to-chest).
(7) Attach with strips of cloth, parachute cord, etc.
(8) Keep the fractured bones from moving by immobilizing the joints on both sides of the fracture. If fracture is in a joint, immobilize the bones on both sides of the joint.
CAUTION: Splint fingers in a slightly flexed position, NOT in straight position. Hand should look like it is grasping an apple.
(9) Use RICES treatment for 72 hours.
(a) Rest.
(b) Ice.
(c) Compression.
(d) Elevation.
(e) Stabilization.
(10) Apply cold to acute injuries.
(11) Use 15 to 20 minute periods of cold application.
(a) DO NOT use continuous cold therapy.
(b) Repeat 3 to 4 times per day.
(c) Avoid cooling that can cause frostbite or hypothermia.
(12) Wrap with a compression bandage after cold therapy.
(13) Elevate injured area above heart level to reduce swelling.
(14) Check periodically for a pulse beyond the injury site.
(15) Loosen bandage or reapply splint if no pulse is felt or if swelling occurs because bandage is too tight.
2. Common Injuries and Illnesses
a. Burns.
(1) Cool the burned area with water.
(a) Use immersion or cool compresses.
(b) Avoid aggressive cooling with ice or frigid water.
(2) Remove watches, jewelry, constrictive clothing.
(3) DO NOT remove embedded, charred material that will cause burned areas to bleed.
(4) Cover with sterile dressings.
(5) DO NOT use lotion or grease.
(6) Avoid moving or rubbing the burned part.
(7) Drink extra water to compensate for increased fluid loss from burns. (Add 1/4 teaspoon of salt [if available] to each quart of water.)
(8) Change dressings when soaked or dirty.
b. Eye injuries.
(1) Sun/snow blindness (gritty, burning sensation, and possible reduction in vision caused by sun exposure).
(a) Prevent with improvised goggles. (See Chapter VI, page VI-3, Figure VI-2.)
(b) Treat by patching affected eye(s).
- Check after 12 hours.
- Replace patch for another 12 hours if not healed.
(c) Use cool compresses to reduce pain.
(2) Foreign body in eye.
(a) Irrigate with clean water from the inside to the outside corner of the eye.
(b) If foreign body is not removed by irrigation, improvise a small swab. Moisten and wipe gently over the affected area.
(c) If foreign body is STILL not removed, patch eye for 24 hours and then reattempt removal using steps (a) and (b).
c. Heat injury.
(1) Heat cramps (cramps in legs or abdomen).
(a) Rest.
(b) Drink water. Add 1/4 teaspoon of salt per quart.
(2) Heat exhaustion (pale, sweating, moist, cool skin).
(a) Rest in shade.
(b) Drink water.
(c) Protect from further heat exposure.
(3) Heat stroke (victim disoriented or unconscious, skin is hot and flushed [sweating may or may not occur], fast pulse).
CAUTION: Handle heat stroke victim gently. Shock, seizures, and cardiac arrest can occur.
(a) Cool as rapidly as possible (saturate clothing with water and fan the victim). Remember to cool the groin and armpit areas. (Avoid overcooling.)
(b) Maintain airway, breathing, and circulation.
d. Cold injuries:
(1) Frostnip and frostbite—
(a) Are progressive injuries.
●Ears, nose, fingers, and toes are affected first.
●Areas will feel cold and may tingle leading to—
●●Numbness that progresses to—
●●●Waxy appearance with stiff skin that cannot glide freely over a joint.
(b) Frostnipped areas rewarm with body heat. If body heat WILL NOT rewarm area in 15 to 20 minutes, then frostbite is present.
(c) Frostbitten areas are deeply frozen and require medical treatment.
CAUTION: In frostbite, repeated freezing and thawing causes severe pain and increases damage to the tissue. DO NOT rub frozen tissue. DO NOT thaw frozen tissue.
(2) Hypothermia—
(a) Is a progressive injury.
●Intense shivering with impaired ability to perform complex tasks leads to—
●Intense shivering with impaired ability to perform complex tasks leads to—
●●Violent shivering, difficulty speaking, sluggish thinking go to—
●●●Muscular rigidity with blue, puffy skin; jerky movements go to—
●●●●Coma, respiratory and cardiac failure.
(b) Protect victim from the environment as follows:
- Remove wet clothing.
- Put on dry clothing (if available).
- Prevent further heat loss.
●●Cover top of head.
●●Insulate from above and below.
- Warm with blankets, sleeping bags, or shelter.
- Warm central areas before extremities.
●●Place heat packs in groin, armpits, and around neck.
●●Avoid causing burns to skin.
CAUTION: Handle hypothermia victim gently. Avoid overly rapid rewarming which may cause cardiac arrest. Rewarming of victim with skin-to-skin contact by volunteer(s) inside of a sleeping bag is a survival technique but can cause internal temperatures of all to drop.
e. Skin tissue damage.
(1) Immersion injuries. Skin becomes wrinkled as in dishpan hands.
(a) Avoid walking on affected feet.
(b) Pat dry; DO NOT rub. Skin tissue will be sensitive.
(c) Dry socks and shoes. Keep feet protected.
(d) Loosen boots, cuffs, etc., to improve circulation.
(e) Keep area dry, warm, and open to air.
(f) DO NOT apply creams or ointments.
(2) Saltwater sores.
(a) Change body positions frequently.
(b) Keep sores dry.
(c) Use antiseptic (if available).
(d) DO NOT open or squeeze sores.
f. Snakebite.
CAUTION: This snakebite treatment recommendation is for situations where medical aid and specialized equipment are not available.
(1) Nonpoisonous. Clean and bandage wound.
(2) Poisonous.
(a) Remove constricting items.
(b) Minimize activity.
(c) DO NOT cut the bite site; DO NOT use your mouth to create suction.
(d) Clean bite with soap and water; cover with a dressing.
(e) Overwrap the bite site with a tight (elastic) bandage (Figure V-6). The intent is to slow capillary and venous blood flow but not arterial flow. Check for pulse below the overwrap.
(f) Splint bitten extremity to prevent motion.
(g) Treat for shock (page V-7, paragraph 1c).
(h) Position extremity below level of heart.
(i) Construct shelter if necessary (let the victim rest).
(j) For conscious victims, force fluids.
g. Marine life.
(1) Stings.
(a) Flush wound with salt water (fresh water stimulates toxin release).
(b) Remove jewelry and watches.
(c) Remove tentacles and gently scrape or shave skin.
(d) Apply a steroid cream (if available).
(e) DO NOT rub area with sand.
(f) Treat for shock; artificial respiration may be required
(page V-1, paragraph 1a).
(g) DO NOT use urine to flush or treat wounds.
(2) Punctures.
(a) Immerse affected part in hot water or apply hot compresses for 30-60 minutes (as hot as victim can tolerate).
(b) Cover with clean dressing.
(c) Treat for shock as needed.
h. Skin irritants (includes poison oak and poison ivy).
(1) Wash with large amounts of water. Use soap (if available).
(2) Keep covered to prevent scratching.
i. Infection.
(1) Keep wound clean.
(2) Use iodine tablet solution or diluted betadine to prevent or treat infection.
(3) Change bandages as needed.
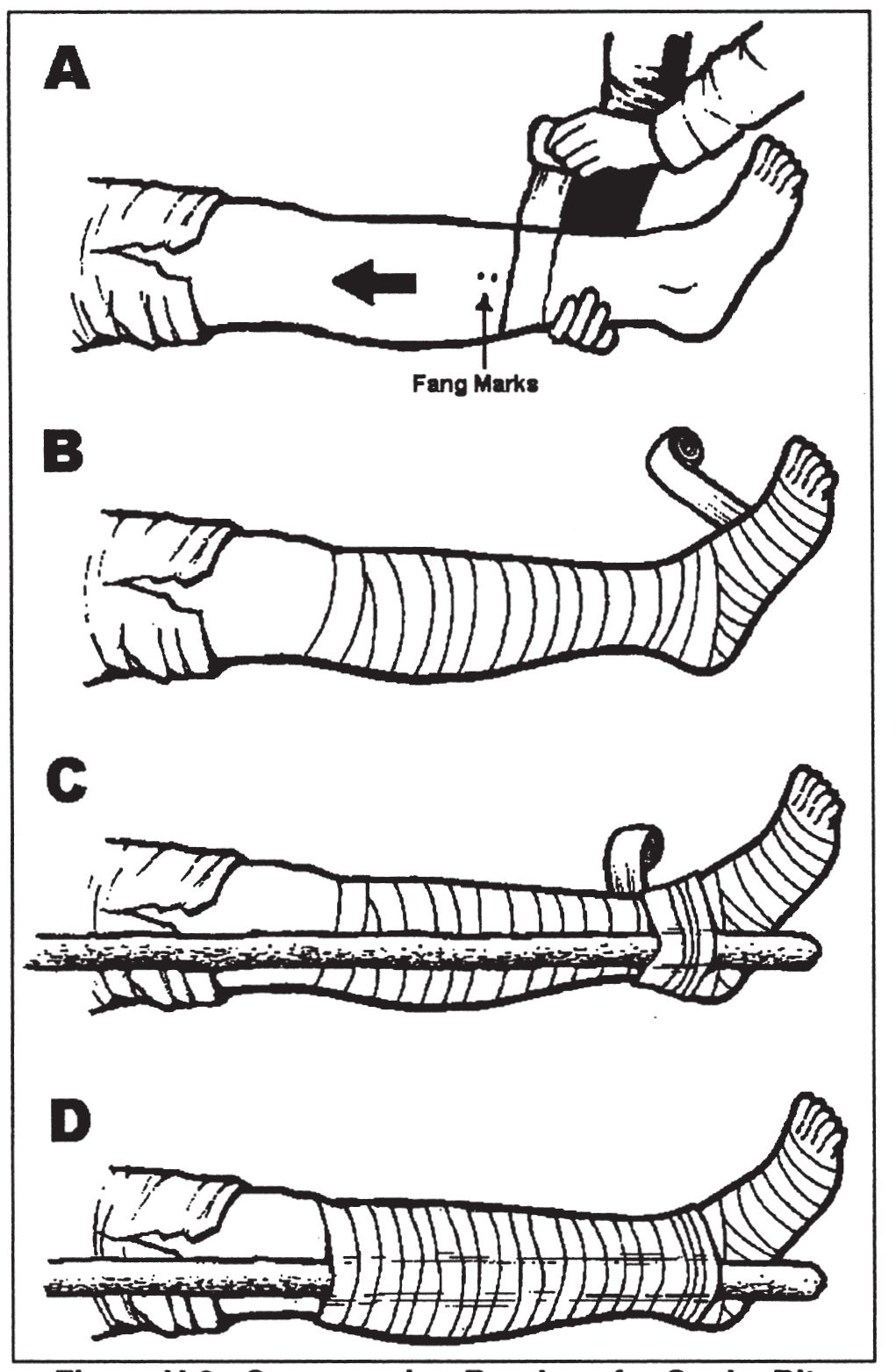
Figure V-6. Compression Bandage for Snake Bite
j. Dysentery and diarrhea.
(1) Drink extra water.
(2) Use a liquid diet.
(3) Eat charcoal. Make a paste by mixing fine charcoal particles with water. (It may relieve symptoms by absorbing toxins.)
k. Constipation (can be expected in survival situations).
(1) DO NOT take laxatives.
(2) Exercise.
(3) Drink extra water.
3. Plant Medicine
a. Tannin.
(1) Medical uses. Burns, diarrhea, dysentery, skin problems, and parasites. Tannin solution prevents infection and aids healing.
(2) Sources. Found in the outer bark of all trees, acorns, banana plants, common plantain, strawberry leaves, and blackberry stems.
(3) Preparation.
(a) Place crushed outer bark, acorns, or leaves in water.
(b) Leach out the tannin by soaking or boiling.
- Increase tannin content by longer soaking time.
- Replace depleted material with fresh bark/plants.
(4) Treatments.
(a) Burns.
- Moisten bandage with cooled tannin tea.
- Apply compress to burned area.
- Pour cooled tea on burned areas to ease pain.
(b) Diarrhea, dysentery, and worms. Drink strong tea solution (may promote voiding of worms).
(c) Skin problems (dry rashes and fungal infections). Apply cool compresses or soak affected part to relieve itching and promote healing.
(d) Lice and insect bites. Wash affected areas with tea to ease itching.
b. Salicin/salicylic acid.
(1) Medical uses. Aches, colds, fever, inflammation, pain, sprains, and sore throat (aspirin-like qualities).
(2) Sources. Willow and aspen trees (Figure V-7).
(3) Preparation.
(a) Gather twigs, buds, or cambium layer (soft, moist layer between the outer bark and the wood) of willow or aspen.
(b) Prepare tea as described in paragraph 3a(3).
(c) Make poultice.
- Crush the plant or stems.
- Make a pulpy mass.
(4) Treatments.
(a) Chew on twigs, buds, or cambium for symptom relief.
(b) Drink tea for colds and sore throat.
(c) Use warm, moist poultice for aches and sprains.
- Apply pulpy mass over injury.
- Hold in place with a dressing.
c. Common plantain.
(1) Medical uses. Itching, wounds, abrasions, stings, diarrhea, and dysentery.
(2) Source. There are over 200 plantain species with similar medicinal properties. The common plantain is shown in Figure V-7.
(3) Preparation.
(a) Brew tea from seeds.
(b) Brew tea from leaves.
(c) Make poultice of leaves.
(4) Treatments.
(a) Drink tea made from seeds for diarrhea or dysentery.
(b) Drink tea made from leaves for vitamin and minerals.
(c) Use poultice to treat cuts, sores, burns, and stings.
d. Papain.
(1) Medical uses. Digestive aid, meat tenderizer, and a food source.
(2) Source. Fruit of the papaya tree (Figure V-7).
(3) Preparation.
(a) Make cuts in unripe fruit.
(b) Gather milky white sap for its papain content.
(c) Avoid getting sap in eyes or wounds.
(4) Treatments.
(a) Use sap to tenderize tough meat. (b) Eat ripe fruit for food, vitamins, and minerals.
e. Common Cattail.
(1) Medical uses. Wounds, sores, boils, inflammations, burns, and an excellent food source.
(2) Source. Cattail plant found in marshes (Figure V-7).
(3) Preparation.
(a) Pound roots into a pulpy mass for a poultice.
(b) Cook and eat green bloom spikes.
(c) Collect yellow pollen for flour substitute.
(d) Peel and eat tender shoots (raw or cooked).
(4) Treatments.
(a) Apply poultice to affected area.
(b) Use plant for food, vitamins, and minerals.
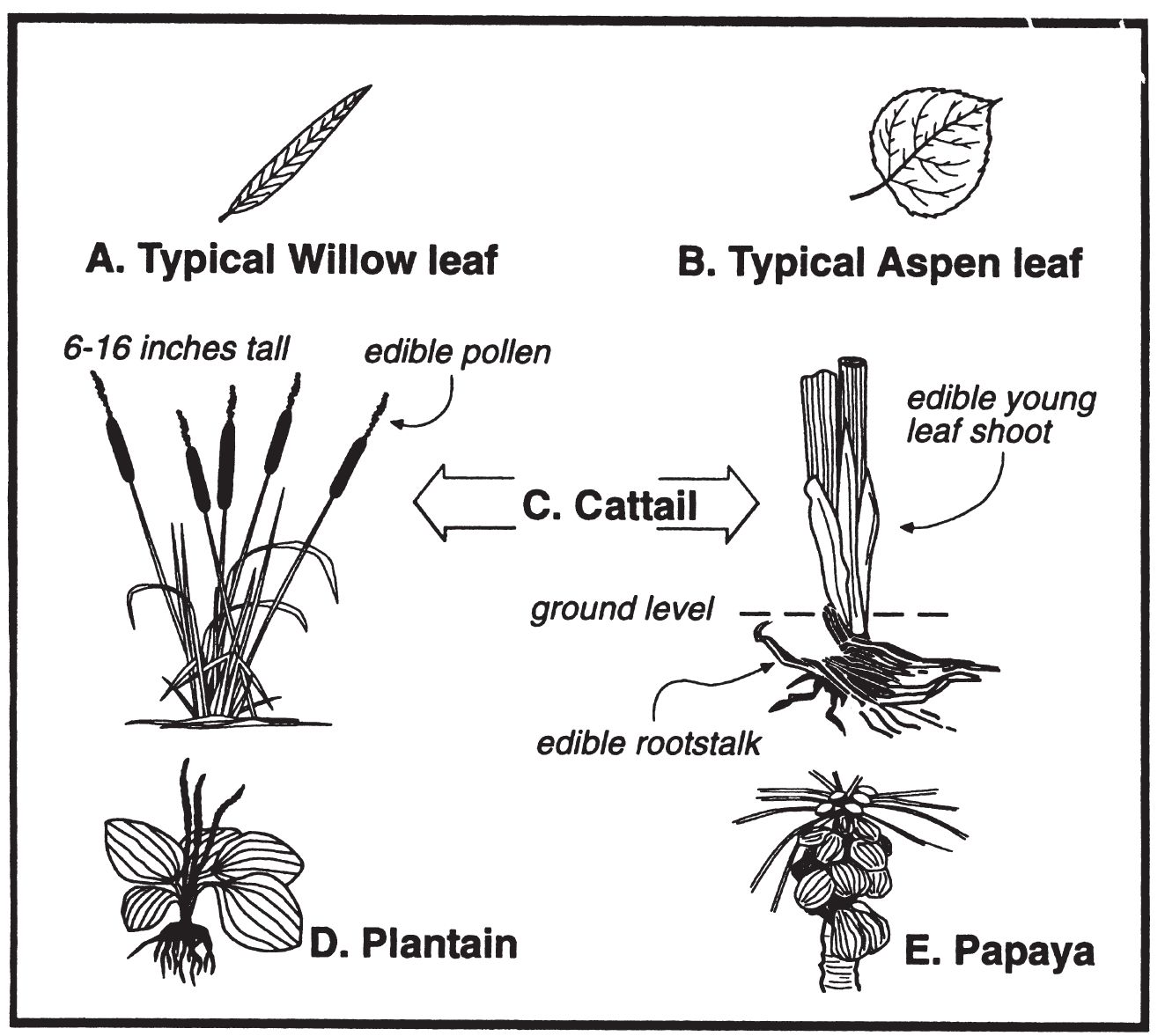
Figure V-7. Useful Plants
4. Health and Hygiene
a. Stay clean (daily regimen).
(1) Minimize infection by washing. (Use white ashes, sand, or loamy soil as soap substitutes.)
(2) Comb and clean debris from hair.
(3) Cleanse mouth and brush teeth.
(a) Use hardwood twig as toothbrush (fray it by chewing on one end then use as brush).
(b) Use single strand of an inner core string from parachute cord for dental floss.
(c) Use clean finger to stimulate gum tissues by rubbing.
(d) Gargle with salt water to help prevent sore throat and aid in cleaning teeth and gums.
(4) Clean and protect feet.
(a) Change and wash socks
(b) Wash, dry, and massage.
(c) Check frequently for blisters and red areas.
(d) Use adhesive tape/mole skin to prevent damage.
b. Exercise daily.
c. Prevent and control parasites.
(1) Check body for lice, fleas, ticks, etc.
(a) Check body regularly.
(b) Pick off insects and eggs (DO NOT crush).
(2) Wash clothing and use repellents.
(3) Use smoke to fumigate clothing and equipment.
5. Rules for Avoiding Illness
a. Purify all water obtained from natural sources by using iodine tablets, bleach, or boiling for 5 minutes.
b. Locate latrines 200 feet from water and away from shelter.
c. Wash hands before preparing food or water.
d. Clean all eating utensils after each meal.
e. Prevent insect bites by using repellent, netting, and clothing.
f. Dry wet clothing as soon as possible.
g. Eat varied diet.
h. Try to get 7-8 hours sleep per day.