

Testosterone? That’s the male hormone isn’t it? Testosterone? That’s the one that makes you grow a mustache, isn’t it? Testosterone? That’s the one that causes your voice to get deep, isn’t it? Testosterone? That’s the one that causes liver damage, isn’t it? How often have you read or heard these warnings about testosterone? These are all old myths, based on synthetic hormones in doses designed for men, not women. Women’s ovaries also make testosterone before menopause, and women lose, on average, about at least 50 percent of their normal testosterone with the decline in hormone production after menopause. Women need testosterone, too—it is the hormone that activates the sexual circuits in the brain for men and women and promotes healthy sexual desire. It also has a lot of other positive effects on women’s bodies, as we shall see in this chapter. So now that I have your attention, we’ll explore together some important information about testosterone for women. I find that most women have heard all the negatives but know very little about the many beneficial roles testosterone plays in a woman’s body. Listen to the voice of this young woman:
I just don’t have any desire for sex. I feel terrible about this. I would like to be interested in it, I love my husband and I am very attracted to him. I enjoy sex when we have it, but I just don’t feel interested. It frustrates me and it frustrates my husband. It’s like somebody turned off a switch.
—MG, 33 years old
Her blood level of testosterone turned out to be less than 10 ng/dl. Her low blood level corresponds with the way she described feeling. For women to have an optimal sex drive and interest in sex, testosterone blood levels need to be about 40 to 60 ng/dl, although the range of what is “normal” for a given woman can vary quite a bit within, or even below, this range. For comparison, men’s testosterone levels normally run about 500–1200 ng/dl. Most men don’t experience a loss of libido until testosterone drops down to around 500 or less, although this may vary slightly depending on what is “normal” for a given man. Because women’s optimal ranges for testosterone are so much lower and narrower, women are more sensitive to a smaller degree of change: A slight drop of only 10–15 ng/dl can make an enormous difference in whether a woman will feel her usual sexual spark. A comment about the numbers I have given above: You may find different books quoting ranges for testosterone that will seem quite different from those I have given here. The differences occur because laboratories may use different units of measure. Throughout this book, I use nanograms per deciliter in the testosterone ranges I give; ranges that are reported in units per milliliter will appear to be different, when in fact, they simply need to be converted to the same scale.
When the young woman above talked with her primary physician about her loss of libido, she said he told her: “Well, I guess you’ll need some marital therapy. It must be a problem in your relationship.” When she asked about having her hormones tested, she was told “there’s no way to do that, and it doesn’t mean anything anyway.” When she had her consultation with me, an integral part of my evaluation was to measure her blood levels of testosterone. I check serum levels of both total testosterone and free testosterone together. I’ll explain more about what this means later in the chapter. Not only is the actual blood level very helpful in determining whether a testosterone supplement may be indicated, it also helps guide me in planning the appropriate amount for each patient. This all made a great deal of sense to MG and helped her see that there is a systematic way to evaluate her needs. She was quite willing to consider the necessity of marital therapy, but not until the hormonal aspects of her problem were at least checked. In her body wisdom, it appeared more likely to her that the problem was a physical change, since she honestly felt her relationship was a good one, there weren’t any marital problems that had occurred, and her previous enjoyment of sex had been high.
A patient recently wrote me that she asked her doctor about checking her testosterone level. He told her that it “couldn’t be done,” and anyway, it “didn’t matter,” since her level would be normal for a fifty-five-year-old. Her letter to me commented, “I said to him, ‘What if I want a level of a 25 year old woman?’ He then said to me ‘That’s ridiculous!’ At that point, I realized this discussion wasn’t going anywhere at all and I gave up.” It may appear from experiences like this that the men who have dominated the hormone decisions, medical research, and the rest of women’s health have been a little afraid for us women to have access to testosterone and a vital, normal, healthy, active sex drive as we grow older. After all, their testosterone, and erectile function, is often declining as they grow older, and they are quite often ashamed to discuss this problem with their doctors. And, for generations, the standard medical teaching was that it was abnormal for women to have a sex drive. Women (“good girls” and “ladies”) were supposed to be passive recipients of the sex act and were considered “loose” if they appeared to actually desire sex.
Many of these myths and age-old stereotypes lie just beneath the surface in women’s encounters with health professionals today. I know that seems like a strange idea, given the relatively open sexuality of our culture today. But these hidden messages about women’s sexuality and how women are “supposed” to act are deeply embedded in our culture and especially in the traditional medical teachings. If you doubt me on this, just notice the mixed messages about women’s sexuality in many ads—women are portrayed as “innocent” and sexy at the same time. Take a look at these examples, some from a long time ago and some more recent.
Dr. W. W. Bliss (1870), in keeping with the thinking of the times, made a rigid distinction between a woman’s reproductive ability and a woman’s sexuality. Female sexuality was seen as unwomanly and detrimental to the supreme role and function of reproduction. Dr. Bliss in his writings warned against “any spasmodic convulsion” (i.e., orgasm) by a woman during sexual intercourse to avoid interfering with conception.
Dr. Mary Wood-Allen, a woman physician of the same era, wrote that women should embrace their husbands “without a particle of desire.” Doctors were taught that women were not meant to enjoy the sex act, and a “ladylike” woman should certainly never initiate the sexual act. Even though the physicians of the time denied that there were female sexual feelings and desires, there still appeared to be an undercurrent of male fear of women’s potentially insatiable lust, which, if ever aroused, might then become uncontrollable.
Things haven’t gotten much better in more recent medical textbooks. Consider this quote from a textbook of gynecology used when I was in medical school in 1977 (and think about all the physicians practicing medicine today who were trained when such textbooks were in use):
There seems to be little doubt that libido, which is well-developed among normal males, appears to be less highly developed among females. Certainly the majority of cases of dyspareunia [painful intercourse] or frigidity, or both, undoubtedly fall into the psychogenic category. The treatment for frigidity must usually stress the educational and psychotherapeutic aspects rather than the patient’s pelvic or endocrine [hormonal] status. The female should be advised to allow her male partner’s sex drive to set their pace and she should attempt to gear hers satisfactorily to his. . . . The importance of the [sex] act to her husband in both physical and emotional aspects should be stressed [i.e., by the physician].
The emphasis on the man’s sexual needs being met, and a woman’s sexual problems as primarily psychogenic, viewed from our perspective today seems quite strikingly unbalanced. As a third-year medical student, I was, like the rest of my classmates, appropriately deferential to the teachings of the “authorities,” the “experts in the field,” even though these teachings did not fit with my own experience or what I was hearing from my patients. Yet, these attitudes persist when women seek help for sexual problems from many gynecologists (male and female) in practice today. Daily, even in the year 2000, I hear such stories from women seeking hormone evaluations in our offices. Last week, a woman told me that after getting the results of the lab tests I had ordered, she asked about improving her testosterone level to a more range to improve her libido. Her male gynecologist said “Why do you want to have a high level like that? You are fifty-four, not thirty!” Needless to say, she was furious at this attitude.
Listen to the voice of this recently married sixty-seven-year-old woman who had a consultation about her problems with vaginal dryness and decreased sexual desire:
My gynecologist just seemed to dismiss my concerns. He just told me that’s what happens when you get older. I don’t want to lose the sexual part of my life. I have a new husband, I love him, and we want to enjoy our sex. I just don’t seem to have the interest I used to, and it hurts because I’m so dry.
She reported that she had been offered a vaginal estrogen cream and marital counseling had also been recommended. When she asked about having her hormones checked, her physician’s reply was, “That’s not necessary. It won’t tell us anything.” When I evaluated her, her estradiol level was less than 30 pg/ml (a desirable level would be at least 80–90 pg/ml), and her testosterone level was reported as “nondetectable,” which means below the sensitivity of the test at about 10 ng/dl. You may recall that I said testosterone is optimal for women from about 40–60 ng/dl). It helped this woman and her husband to find out that her hormone levels were so low, because it confirmed that the sexual difficulties were not due to a relationship problem or her dissatisfaction with her new husband. You can imagine how much relief they both felt with this news.
Now, I ask you, is it reasonable to ignore these concerns and to dismiss a patient’s request for a perfectly appropriate blood test? Particularly when, in this case, the patient has concerns that may be so easily alleviated with readily available natural forms of hormones to restore her premenopausal balance. Before sending her to a therapist, this woman should have at least been given the information that (1) we do have reliable and useful tests to measure hormone levels, and (2) we have a variety of bioidentical hormone options to enhance her sex life for this new phase of her life. After being started on a low dose of supplemental testosterone and estradiol, she came in a month later and described, “I feel like a new woman. I have my old spark back, and now I want—and enjoy—sex again.” She also told me that her quality of orgasms had improved, it was easier to have an orgasm, and she now had no difficulty with arousal and lubrication. Her estradiol level at the three-month follow-up visit was 98 pg/ml, and her testosterone level was now 25 ng/dl, which were good levels for her, based on her self-reports of restored libido and healthy sexual responses.
Testosterone is one of a group of hormones called androgens, from the Greek “andros” meaning malelike. The word androgen refers to any steroid molecule with nineteen carbon atoms that is able to bind to the androgen hormone receptor sites in the brain and body. All of the androgens are made from cholesterol by the female ovary, the male testes, and, to a lesser extent, by the adrenal glands in both men and women. Androgens are also made from chemical “building blocks,” or precursor molecules, in body-fat tissue, muscle, the liver, skin, and the brain. But these precursor molecules are produced in the ovaries and adrenal glands, so it really ends up that the ovaries and adrenal glands together are responsible for either directly or indirectly making all of a woman’s testosterone. In a Gallup poll of American women, conducted for the North American Menopause Society in 1993, only 5 percent of the women polled knew that their bodies make androgens and that the amount made declines after menopause. Doctors used to think that testosterone isn’t very important for women, so the whole issue of testosterone therapy for women is relatively new. The amount of circulating active androgens in women is obviously much lower than in men, but these compounds are important for quite an array of vital functions in women’s bodies. Many studies over the last thirty years or so have shown what powerful effects testosterone has on a woman’s sexuality, mood, zest, and vitality, and on maintaining healthy muscle and bone, to name a few of its functions. Fortunately today, more women are aware of the importance of androgens like testosterone and DHEA and are asking physicians for more information about how to measure them and what options there are for adding back what the body formerly made.
TYPES OF ANDROGENS
• dihydrotestosterone (DHT)
• testosterone
• dehydroepiandrosterone (DHEA)—ovary
• dehydroepiandrosterone-sulfate (DHEA-S)—adrenal
• androstenedione
© Elizabeth Lee Vliet, M.D., 1955
Over the course of a woman’s life, the ovary makes on average about one-third of a woman’s total circulating androgens, in addition to producing the female hormones estrogen and progesterone. But beginning several years before a woman’s ovary becomes menopausal, the adrenal glands have already decreased androgen production by about 50 percent, and the ovary levels of testosterone have already started to decrease. That means your sexual desire and ability to become sexually aroused can be significantly diminished several years before you actually stop menstruating at menopause. If you have a hysterectomy with removal of the ovaries before you are actually at menopausal hormone levels, the change is even more drastic. Concentrations of testosterone in the bloodstream fall markedly within twenty-four to forty-eight hours after surgery. Since you no longer have the ovaries to make more testosterone, or to efficiently convert adrenal DHEA to testosterone, there is an abrupt loss of this important hormone. That’s a big shock to the body, and there are potentially major unpleasant effects from the loss of testosterone: loss of sex drive, fatigue, decrease in muscle mass, decreased bone density, depressed mood, achy joints, and changes in feelings of well-being to name a few. Even if one or both ovaries are left in place, newer studies have shown that the hormone production reaches menopausal levels within three to four years in as many as 60–70 percent of women, even if they are only in their thirties when the uterus is removed. This more rapid decline in hormones after the uterus is removed is thought to be due to decreased blood flow to the ovaries as a result of having to cut and tie off the uterine artery during surgery.
In addition, if you are then started on just estrogen therapy, the amount of free, biologically active testosterone falls even further, since estrogen increases SHBG, sex-hormone-binding globulin, that “binds up” more of the testosterone molecules. This is one reason that many women lose sex interest, sex drive, and energy after hysterectomy and then think these losses are due to the surgery. It isn’t usually the surgery per se that caused the problems. It is generally that you need more optimal hormone replacement to restore the desirable levels of what you had before surgery. And often, women who have had their ovaries removed will need testosterone added to the estradiol prescription. But if your doctor doesn’t check the hormone levels, mistakenly assumes you are “just depressed,” and prescribes a medication like Zoloft, Paxil, Celexa, or Prozac, the results on your sex life can be disastrous. All of these serotonin-augmenting medications drastically reduce sex drive and orgasm ability in women who have normal levels of testosterone, much less women who have lost their testosterone. How do doctors really know what a woman needs after surgery if no one ever checks hormone levels or considers that the loss of crucial hormones may cause these changes I have described?
Women who become naturally menopausal and have decreased ovary production of all the hormones lose about 50 percent of their androgen source, especially the testosterone. I wonder how many men would like to go around for the last thirty or forty years of life with only half their normal testosterone! One reason there is less of the active form of testosterone after menopause is that an important precursor molecule, androstenedione, decreases more than 50 percent when the ovary ceases its hormone production. Many doctors do not realize that when women have a decline in estrogen production, it also results in a decrease in testosterone production, due to the loss of precursors usually made by the ovary. If you don’t have functioning ovaries due to either natural menopause or a condition that causes premature ovarian decline (viral syndromes, tubal ligation, cigarette smoking, excessive exercise, to name a few), or if your ovaries have been removed in surgery, remember that you can’t produce optimal levels of testosterone or estrogen by taking DHEA supplements alone, since it is in the ovary that most of the enzymes and pathways exist for us to be able to convert DHEA to testosterone or, to a lesser extent, estradiol.
There are noticeable effects of the changing hormone balance during the climacteric or midlife years: Lower estrogen relative to the amount of testosterone present allows for the testosterone effects to be “unmasked,” producing changes in facial hair, voice, sex drive, energy level, and distribution of body fat. With loss of estrogen, the androgens that are left will be shifted more into the “free” portion in the bloodstream, and will therefore be more biologically active. So even if you have less testosterone and DHEA present than you did before menopause, you now have more in the active state and will therefore see more of the androgen influences on your body. This means women having more facial hair, losing scalp hair, and experiencing a shift in body fat from the “pear” or gynecoid (female) pattern to the “apple” or male pattern of body fat around the waist and trunk (see chapter 2 for a diagram of these body-shape changes). It may not be just that you “don’t have the willpower to lose weight”; it may be that your hormone ratios are now working against you. This is especially true if you are taking over-the-counter DHEA supplements that usually come in doses too high for women to use on a daily basis.
Contrary to the popular myths and incorrect information about hormones perpetuated in a number of books and articles, it isn’t the estrogen that is typically the culprit in weight gain at midlife. There are several bigger culprits in weight gain for women: (a) the changing ratios of the ovarian estrogen and testosterone, (b) taking excess progesterone relative to estrogen, (c) the effects of excess adrenal androgens and cortisol relative to estradiol, (d) increased insulin levels as we age and lose the beneficial regulating effects of estradiol, and (e) the gradual decline in thyroid function as we age. All of these hormone changes combine to give us a slower metabolism. A lower metabolic rate combined with less physical activity and usually more food intake than is needed as we age, all add up to excess pounds. In addition, once you start gaining weight, there tends to be more insulin production, which in turn promotes more fat storage around the middle of the body. The characteristic premenopausal balance of estradiol, testosterone, progesterone, thyroid hormones, cortisol, and insulin are important in order to reduce these undesirable body changes in later years.
Without the proper balance of estrogen, androgens from the adrenal gland and fat tissue begin to produce even more unwanted body changes for women: increasing blood pressure, increasing total cholesterol, and decreasing HDL (“good”) cholesterol, along with increasing LDL (“bad”) cholesterol. All of these changes contribute to the increasing risks of heart disease, hypertension, and diabetes in women in over age thirty-five. You will read more about this in chapter 13. At first, we thought that testosterone itself was responsible for these negative effects on the cholesterol ratios. Newer studies have shown, however, that when given with the right balance of estradiol, testosterone actually helps maintain the normal mechanisms involved in vasodilatation that serves to help lower blood pressure. Testosterone, and other androgens such as DHEA, if given alone appear to promote buildup of artery-clogging plaque (atherosclerosis). If the androgens are given with estrogen, however, they have the opposite effect on the arterial wall and actually help prevent buildup of plaque in the arteries.
Throughout a woman’s life, testosterone has important functions in maintaining muscle tissue—that wonderful “fat burning,” machinery—in women. Lower testosterone levels mean less muscle building, even if we are exercising several times a week. Testosterone also plays a key role to help build bone and prevent osteoporosis, an even more crucial function as women lose the effects of estrogen in maintaining bone density. Furthermore, testosterone plays a key role in keeping a woman’s energy level optimal. Decline or loss of this critical hormone is one of the frequently unrecognized factors in the midlife problem of “chronic fatigue.” Many women have multiple medical evaluations and spend hundreds or thousands of dollars on tests and therapies to diagnose and treat “chronic fatigue” (CFS, CFIDS) and never have a blood-level test for testosterone.
Mrs. C., a delightful woman in her early sixties who loved to ski every winter, had noticed a significant decrease in her stamina and energy on the slopes over the past two or three seasons. During her consultation to discuss her questions about hormone therapy, she mentioned that she had experienced a noticeable decline in her strength and endurance for skiing. She had never had anyone check her hormone levels, although she had asked about having this done. Along with an estradiol that was too low in spite of her being on Premarin 0.625 mg, she also had a testosterone level of less than 10 ng/dl. I suggested she add testosterone to her therapy, and I also changed her to a bioidentical form of 17-beta estradiol, using a skin patch delivery. She began using 2.5 mg of natural micronized testosterone oral sustained release capsules, along with the Climara transdermal estradiol patch, 0.1 mg every five days, and has now been on this combination for the past several years. From a medical standpoint (and her preference), she did not need to take progesterone since she had a hysterectomy many years ago. Within the first six months, she described a marked increase in her energy level, and what she described as “my old spark coming back.” The next year at her follow-up visit, she gleefully told me that when she returned to the ski slopes the season after starting testosterone, her ski instructor commented on the noticeable improvements in her strength and stamina. He asked her what her new training regimen had been over the summer. She smiled and said “I never told him what really made the difference, but I know it was the testosterone. I could feel my muscles getting stronger with the exercise, and this was different from the way my muscle strength developed when I was just on the Premarin!” She didn’t have any adverse side effects on this dose of testosterone, and her cholesterol profile has continued to be in a healthy range. She also commented “I just feel better. It’s hard to describe, but I just have such a good change in my overall feeling of well-being and energy again. I didn’t realize I had lost some of that until I got it back! I really feel like my usual self.”
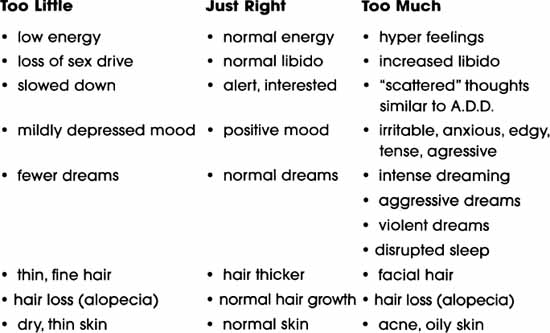
Our psychological sense of well-being is also enhanced by testosterone. In some women, what appeared to be a depression turned out to be a deficiency of testosterone. Yes, this hormone does lift moods when the amounts are present at normal levels for women. As testosterone levels rise higher than needed for optimal balance (whether from overproduction in the body or from supplemental hormones), women report increased facial hair usually above the lip, increased dreaming and/or nightmares, difficulty falling asleep, and perhaps more sex drive than usual. At high levels, and in doses used in steroid abuse for muscle building, both men and women develop toxic behavioral effects such as extreme irritability, volatile/explosive moods, aggressiveness or assaultiveness. Again, balance is key.
Remember from my discussion in chapter 5, synthetic simply means “produced by putting together,” not necessarily “artificial,” as it has come to be used. Remember the example of human insulin from the previous chapter? Another illustration is human growth hormone, which scientists have been able to synthesize in the laboratory, so that we can now give the human form to children deficient in this hormone. These are examples of synthetic (i.e., made in the laboratory) medications being used because they are the bioidentical to the ones found in human bodies. Molecules that are the same as those made by the body, even if synthesized in a laboratory, are better tolerated, more effective, and have fewer side effects. Then there are synthetic hormone medications that are truly artificial in the sense that they are chemically different from the molecules the body makes.
Methyl testosterone is an example of a form of testosterone created in the laboratory and not found in the human body. This compound was developed by scientists trying to find a way to make testosterone able to be used in an oral tablet. In the past, we did not have a way to give natural testosterone orally because it would be broken down and lost in the digestive process before getting into the bloodstream. It is the addition of the methyl group to testosterone that makes it possible to be absorbed orally without being completely lost in the digestive tract first, and then produce its androgenic (testosterone-like) effects at the receptors throughout the brain and body. But, it is also this methyl group that increases the potential for liver toxicity. Methyl testosterone has worked well for the majority of male patients needing testosterone but not as well for women, because the commercial doses available were designed for men and are simply too high for most women to use on a daily basis.
In recent years pharmacists began making a form of natural testosterone in a micronized form that produces particles small enough to survive digestion and be absorbed into the bloodstream. Micronization is also used to make native human preparations of progesterone and estradiol as I talked about in earlier chapters, since all of these hormones are inactivated or destroyed by digestion when taken orally. The source for all of these natural, bioidentical forms of human hormones is actually from plants: soybeans and yams. The chemical precursors are extracted, purified, synthesized into molecules identical to those made in the human body, and then compounded into standardized tablets so that you know the amount of hormone you are getting. This approach, I feel, allows better fine-tuning of hormone therapy than trying to get enough active hormone from plant/herbal sources, since you really are not able to determine how much you are taking, and whether the amount is right for you.
Testosterone can also be made by pharmacists in a wide variety of other forms: skin cream, skin gel, sublingual tablets (to dissolve under the tongue), and vaginal suppositories. The way that testosterone is given will determine (a) the amount absorbed, (b) the metabolism to different forms, (c) the development of desirable effects, as well as (d) the presence of adverse side effects. I generally don’t recommend the rapidly absorbed forms of testosterone, such as gels and sublingual tablets or troches, since these are more likely to make you feel like you have been hit by a Mack truck when the blood levels rise so fast. A rapid rise in testosterone to high levels typically causes marked irritability, edginess, muscle tension, and aggressive, angry feelings. I have found that these unwanted testosterone effects are decreased by using either oral testosterone in a sustained-release capsule or tablet, or a low-dose cream form that is more slowly absorbed. I have listed in Appendix II several experienced, reputable pharmacists who will work with you and your physician to determine the proper amount of natural testosterone for you as well as provide educational resources and telephone question/answer services to assist patients and physicians in determining the most appropriate options.
Most of the women I see have already heard comments like those I made at the beginning of this chapter: Testosterone causes a mustache, a beard, a deep voice, liver damage, and “oversexed women.” A key factor most women don’t know is that all of these problems are related to the dose and type of testosterone used, not just testosterone itself. In the United States, until very recently, we have had only synthetic methyl testosterone or other androgen compounds that are not made in the human body. These synthetic androgens are chemically different molecules and are far more potent than the natural hormones made by the ovary and adrenal gland.
Until more recently, doctors did not realize that women needed much lower doses of testosterone than had been thought, based on doses used for men. In the United States, we have not even had commercial tablets available in doses low enough for women. As an example, in the past, 10–15 mg has been a typical dose of methyl testosterone prescribed for women. On average, I am using doses of 1.25 mg to about 3 mg a day of the natural micronized testosterone. Obviously, this is quite a difference. These lower doses are based on the physiologically natural range of testosterone production in women. When using a more appropriate woman’s dose, my patients tell me they feel more energy, have a return of their normal sex drive, and do not have the unwanted side effects described above. In addition, I monitor cholesterol blood levels and have not had any patients who have had a negative effect on their cholesterol levels if we keep the dose in the usual range for women, and check to see that blood levels are not getting too high.
Currently, there is a natural testosterone patch in a dose designed for women being developed with the same technology that has made estrogen and progestin patches available. It is not yet on the market, and the testosterone patches for men are far too high a dose for women to use. Future directions for androgen research in the United States are focusing on the role of testosterone in Alzheimer’s disease, in improving cognitive function in older people without dementia, in treating bone loss for men and women, in lipid disorders and breast cancer. With greater recognition of the important role testosterone plays in our health as both men and women get older, and the benefits documented with the transdermal testosterone patch for men, it would be quite helpful if we had a patch form of testosterone suitable for women to use.
DHEA has had a great deal of publicity in recent years, and is available in the United States in a wide variety of over-the-counter products of varying quality and potency. Since the over-the-counter DHEA is not regulated by the FDA, it is difficult for you to know exactly what you are getting when you buy it, and most of the doses are much more than women need for daily use. DHEA is also recommended by many alternative and “natural hormone” practitioners as the “Mother Hormone” precursor for the body to make estradiol and testosterone, and is suggested by some fibromyalgia specialists as a way to treat FMS or chronic fatigue. But remember what I said earlier: You have to have functioning ovaries for the “Mother Hormone” to be made into estrogen and testosterone. Behind the headlines touting the benefits of DHEA on everything from brain-power to sex, there is very little good science to back up the claims. This situation is very different from the extensive body of science showing the many beneficial effects of estrogen for women, and good data on the risks that may occur with long-term use of various estrogens. What dose of DHEA is safe is also a critical unanswered question. This is far different from having such good information available about doses and routes for estrogen. So, before you jump on the bandwagon and buy your “superhormone” at the grocery store, remember this is a potent steroid with profound effects throughout the brain and body. Make sure you have done your homework before you swallow all the claims . . . or the pill!
DHEA use has some special concerns and cautions for women that I want to briefly address here. I don’t have space to go into all the pros and cons, or to describe in detail the research findings. I will cover the highlights, and if you would like to read more about DHEA from a well-respected DHEA researcher, I recommend the review article “Dehydroepiandrosterone Replacement in Postmenopausal Women: Present Status and Future Promise,” by Peter R. Casson, M.D. and colleagues. This excellent article was published in Menopause: The Journal of the North American Menopause Society, vol. 4, 1997, pp. 225–231. While this is a medical article for a medical audience, it will give you a balanced and reliable view of what we know and what we don’t yet know about the safety and effectiveness of DHEA for women. Dr. Casson has been systematically researching DHEA for many years and has published a wide variety of well-balanced and carefully done studies, so his articles are a reliable resource for you to read if you want more in-depth information than I have provided here.
DHEA, like other precursor hormones, requires enzymes found in healthy ovaries for the DHEA to be changed into testosterone or estradiol by the body. If for whatever reason, your ovaries are not functioning optimally, you won’t be able to adequately convert DHEA to the other hormones further down the pathway. When that happens, women tend to have the “excess androgen” side effects I showed in the summary chart for testosterone effects later in this chapter. Too much DHEA can cause exactly the same side effects as too much testosterone. In addition, neuroendocrine research has found that women’s testosterone receptors need to be “primed” with estradiol in order for the androgens to have optimal effects. So if you are given DHEA, but your estradiol levels are too low, you again have the risk of adverse side effects as well as increased irritability and restless sleep seen with excess testosterone. In FMS and CFS the issue is even more problematic: Women tend to experience worsening muscle pain and spasm if the androgens (either DHEA or testosterone) are replaced prior to having optimal estradiol. Remember your basic body chemistry and the differences between men and women . . . you need a woman’s balance restored.
Both men and women lose DHEA with age, and by the time we reach about age seventy, DHEA levels are only about 10 percent of what they were in our peak reproductive years. We don’t yet know for certain whether this decline in adrenal androgens, called adrenopause, represents just an effect of getting older, or whether the decline itself causes the problems we thought were due to aging, such as loss of muscle strength, loss of optimal immune function, loss of cognitive “sharpness,” loss of bone, and many other effects. Most of the current studies available showing benefits of DHEA have been conducted on animals, and there are problems with using animal models: doses used are often much greater than what would be appropriate “replacement” for humans, and the animal model itself is flawed, since animals don’t go through the same adrenopause as humans do. But, in spite of these difficulties, a lot of what you read about DHEA’s benefits has been the result of studies done on animals.
In human studies, important differences for men and women are emerging. A 1988 study on five young men by Nestler and colleagues showed that these young men given high-dose oral DHEA over a month had a decrease in body fat and a decrease in “bad” (LDL) cholesterol. The same study was then conducted in women by Mortola and colleagues: No benefits were seen for the women. In fact, the women became “androgenized” with increased facial and body hair, acne, decline in good (HDL) cholesterol and increase in bad (LDL) cholesterol, decreased sex-hormone-binding globulin, and increased insulin resistance. Remember, insulin resistance helps make you fatter around the middle of your body—not a good thing cosmetically or from a health standpoint. Dr. Casson did a subsequent study using a much lower dose of DHEA (50 mg) for women and found that even this dose (commonly seen in over-the-counter products) caused excessively high testosterone serum levels in women. He reported that this finding indicated the need for further dose reduction if DHEA was being given to women. Earlier studies have suggested a cardio-protective effect of DHEA, again, this was in men and the positive effects were not seen in women. The data on this point continue to be conflicting. In addition to the possibility of weight gain with excess DHEA, there is a concern emerging from animal studies about possible adverse liver effects of long-term oral DHEA use, particularly at the high doses being promoted for women in the over-the-counter products.
Now that I have pointed out some pitfalls to watch for, what about promises for DHEA? DHEA has been promoted as the “feel-good” hormone, improving one’s sense of well-being, energy, memory, and mental sharpness. Unfortunately, the few carefully done, placebo-controlled studies of possible cognitive benefits with DHEA have also been disappointing, with no clear evidence of improved mental function, sense of well-being, or memory increase. Some clinicians have proposed that DHEA may help prevent osteoporosis, but again, we don’t yet have good data on a bone-sparing effect from using DHEA. Dr. Casson’s group studied DHEA replacement effects on various markers of bone, and found no change in urinary hydroxyproline, hydroxylysine, or collagen crosslink excretion, and no improvement in bone mineral density on DEXA testing at the six-month point.
Evidence to date does not support DHEA being given routinely to healthy postmenopausal women for hormone replacement, but there are some situations in which DHEA does appear to have an important role. One of those is systemic lupus erythematosis. Studies at UCLA using DHEA replacement for lupus have been promising in reducing pain and other manifestations of the disease, but at the high doses used, many of the women in the studies developed unwanted side effects (facial hair, acne, irritability, for example). It may be that future studies will show that lower doses maintain the benefits without causing so many side effects. In a 1999 study published in the New England Journal of Medicine, Arit and colleagues in Germany studied the effects of DHEA supplementation in twenty-four women with adrenal insufficiency (AI) to determine effects on sexuality and well-being. Fourteen of the women had primary adrenal insufficiency, and all were taking corticosteroid replacement. Of the group, there were seventeen women who were either hypogonadal (estrogen-deficiency) or postmenopausal, and thirteen of these women were also taking estrogen-progestin replacement therapy. The women were given either 50 mg DHEA or a placebo for four weeks and then crossed over to the opposite treatment to compare responses. The women were not told which treatment they were receiving.
These investigators from Germany found that supplemental DHEA produced increases in serum DHEA, DHEA-sulfate, and testosterone, but no increase in estrogen levels. Sex-hormone-binding globulin was decreased (which meant more of the sex hormones were pushed into the free fraction in the serum). Total cholesterol decreased, but an unwanted finding was that HDL cholesterol also decreased on DHEA therapy. Objective measures, as well as the women’s self-reports, showed improvement in overall well-being, depression, anxiety, and sexual thoughts, sexual interest, and sexual satisfaction. Side effects that occurred were the well-known ones of excess androgens: acne, oily skin, increased body/facial hair, and loss of scalp hair (alopecia) during the time of active hormone treatment. Decreasing the dose of DHEA helped to minimize or eliminate these unwanted side effects. The researchers concluded that DHEA replacement was an appropriate therapeutic option for women with well-documented adrenal insufficiency, even though this is an uncommon condition. Regular daily use of corticosteroids is much more common than is adrenal insufficiency, since these medications are given to people who suffer from osteoarthritis, rheumatoid arthritis, lupus, asthma, and other medical conditions. Taking corticosteroids daily will suppress the adrenal (and ovary) production of DHEA, so women who are taking corticosteroids over a long period of time may also benefit from DHEA supplementation.
I recommend that if you want to take DHEA, you should have a thorough evaluation by your physician, and have the appropriate blood tests done for hormone levels, lipids, and liver function. Then, work with your physician to determine an appropriate dose formulated to your needs by your physician and a compounding pharmacist, and be sure you use prescription-grade DHEA. You should keep in mind that over-the-counter DHEA is food-grade, not the pharmaceutical grade quality that is used in research studies. Not all over-the-counter brands deliver the amount they state on the label, and many products contain excessive doses for women. Since there is the potential for significant adverse side effects and long-term risks of DHEA use, it should be monitored by a physician who checks your serum levels of hormones, fasting lipids, and liver function at appropriate intervals. You need to pay attention also to what is happening to your quality of sleep and scalp hair—both of which can be disrupted and lost by too much DHEA. And if you start taking DHEA and are gaining weight around the middle of your body or craving sweets, you need to talk with your physician and cut back on the dose. A key point with DHEA is to start low and go slow with the amount you are using.
To help you make the important decisions about what is best for you and your health needs, I have summarized in the following table benefits of adding testosterone to a hormone therapy regimen. I have also given you some pointers on what to look for as effects of too little and too much testosterone, or DHEA. Most women need only very small amounts of testosterone to achieve these benefits. I generally start my patients on 1.00–1.25 mg of oral sustained-release micronized testosterone, and then gradually increase the dose based on the woman’s description of how she is feeling and what we are achieving in her serum levels. I find that most women I see will achieve the desirable response at a dose somewhere between 2–4 mg a day. I recommend rechecking the testosterone blood level before going higher on the dosage. Sometimes oral doses may still not be absorbed well enough to give desirable blood levels or will cause adverse changes in cholesterol, and I will suggest changing to a transdermal, gradually absorbed cream to improve the overall response. The transdermal cream form of testosterone (and DHEA, when appropriate) is less likely to cause the negative changes in HDL cholesterol, since absorption into the bloodstream through the skin bypasses the liver “first-pass” metabolism. Cream forms are an option for testosterone therapy that I find useful for women with high cholesterol or low HDL who still need to have the other benefits of testosterone. Cream forms require much lower doses than the oral route, since more is absorbed and less is lost by liver conversion to other compounds. A safe rule of thumb for a starting point is that a dose of the cream form of the hormone should be about 10 percent of an oral dose. The amount should then be adjusted based on your response and your serum hormone levels.
In addition to the natural micronized testosterone that can be compounded for you by pharmacists who provide this individualized service, there are a number of commercial methyl testosterone products available in the United States. These are summarized in the table below. A word of caution about the injectable testosterone preparations: It is more difficult to achieve the right dose for women with these, and as a result, they are more frequently associated with the unwanted side effects I have described. Injectable forms also give high levels at the beginning and wear off rather unpredictably, making it difficult to feel like you are on an even keel when you are using these forms. Testosterone pellets can be prepared to give a lower dose and more gradual absorption than the injectable forms, but the pellets also wear off unpredictably and make it harder to keep you feeling “even” without getting too much testosterone at the beginning and too little at the end. An even more important reason I don’t use these preparations for women is that I like to use methods that the woman herself can easily control, based on how she is feeling. With pills or creams (or patches when available), each woman decides whether to use it that day; with the pellets and injections, you are stuck with them until either you go back to the doctor and have the pellet taken out or the injection wears off. In my opinion, you need to be the one with more flexibility and control over your hormone management!
SUMMARY OF TESTOSTERONE AND DHEA EFFECTS
© Elizabeth Lee Vliet, M.D., 1995, revised 2000
COMMERCIAL TESTOSTERONE PREPARATIONS
TESTOSTERONE ALONE: |
Doses Available |
Oreton, Metandren, Test-Red (methyltestosterone) |
5mg, 10mg, 25 mg (oral tablets) |
Halotestin, Ora-Testryl (fluoxymesterone) |
5 mg, 10 mg (oral tablets) |
Testopel (Testosterone pellets) |
75 mg (inserted under skin) |
Delatest, Testone LA, Depo-Testadiol (testosterone enanthate) |
100 mg/ml (injectable) |
Depo-Test (testosterone cypionate) |
50 mg/ml (injectable) |
NOTE: Injectable steroid hormones are now more difficult to obtain since Sterls Pharmaceuticals closed approximately 1998; generally are now made by appropriately equipped compounding pharmacies.
TESTOSTERONE-ESTROGEN COMBINATIONS:
Estratest: esterified estrogens |
1.25 mg (oral tablets) |
and methyltestosterone |
2.5 mg |
Estratest HS: esterified estrogens |
0.625 mg (oral tablets) |
and methyltestosterone |
1.25mg |
Depo-Testadiol: estradiol cypionate |
2 mg (injectable) |
with testosterone cypionate. |
50 mg |
Discontinued by the manufacturer, approximately 1997: |
|
Premarin with methyltestosterone (MT) |
0.625mg E, 5 mg MT and |
© Elizabeth Lee Vliet, M.D., 1995, revised 2000
In my opinion, Premarin with methyl testosterone had far too much testosterone for most women, particularly when you consider the much lower dose of estrogen included in the tablet, and the fact that Premarin delivers such a small amount of the most active form of estrogen, 17-beta estradiol. Since these high doses of testosterone were commonly used in the past by the dominant estrogen manufacturer, I think this is one of the primary reasons that oral testosterone therapy got such a bad name and was associated with so many unwanted and potentially serious side effects. As you see from the table, one tablet strength had 5 mg methyl testosterone, and the other had 10 mg methyl testosterone. I have never used even 5 mg of methyl testosterone, much less 10 mg of this more potent form of testosterone, in prescribing androgen therapy for women. Doses this high of oral methyl testosterone for women may commonly cause development of facial hair, acne, voice changes, loss of scalp hair (male pattern baldness), elevated total and LDL cholesterol, decreased HDL cholesterol, elevated triglycerides and insulin, as well as more body fat deposited around the waist. If your doctors are concerned about such side effects when you ask about testosterone therapy now, it is likely that they are remembering what happened with the older forms and higher doses of testosterone therapy. They may not realize that micronized testosterone, in the bioidentical (“natural”) form the ovary made, is only about one third to one quarter the potency of methyl testosterone, and we are using even lower doses today as well.
Although the brand Estratest has become much more popular and widely used in recent years, thanks to increased awareness by physicians and consumers of the importance of testosterone for women, I think there are problems with this product you need to keep in mind. Estratest contains esterified estrogens that are converted primarily to estrone and very little of the 17-beta estradiol, which means less than optimal estrogen effect, and it contains the more potent methyl testosterone. Acne or oily skin, flare-ups of fibromyalgia pain, irritability, insomnia and feeling anxious or tense, not sleeping well, and hair loss are common side effects women tell me about their experiences with Estratest. Since it doesn’t have an adequate amount of 17-beta estradiol to properly balance the amount of testosterone it contains, in my experience, I am not surprised to hear these negative comments from women who try it and decide not to continue.
Estratest illustrates a common problem with any medication that comes in a fixed-dose combination of different hormones or medications. There may not be enough of one thing and too much of the other for everyone to have the right blend. As a result of these problems, I rarely use the fixed-dose combination estrogen-testosterone such as Estratest. In my opinion, these fixed-dose products do not allow for individualized adjustments of hormone therapies tailored to each woman. I find it works much better to adjust each hormone separately so that you get exactly the right amount of each hormone for your body needs. Taking each one separately also allows you to make changes in only one at a time, based on what you are experiencing with desirable or undesirable effects, or interactions with other medications (such as antibiotics, asthma meds, etc.), or effects of situational stresses on your hormone metabolism.
If, however, you want to have the convenience of a combination estrogen-testosterone tablet available at your local drugstore or you want a prescription that is more likely to be covered by your health insurance, I have found that it can work fairly well to start first a 17-beta estradiol prescription (patch or tablet) and then use the combination estrogen-testosterone tablet (i.e., Estratest HS) just two to three times a week rather than every day. This approach minimizes the adverse side effects of the higher dose, more potent methyl testosterone and yet provides a more consistent level of 17-beta estradiol than is provided by Estratest. This option seems to work well for some women. Other women can use these combination products daily and find that they provide the desired benefits without unwanted side effects. The key is finding what is best for you. I would expect your “recipe” would likely be slightly different from what works for your friends.
If you decide to take testosterone, remember that each woman’s body is different. Trust your body wisdom, and what you know about how you feel. You may also check the summary chart on indications of too much versus too little testosterone, ask your doctor to check a blood level and to work with you to adjust your dose to one that feels good for you. You and your physician need to be effective partners in the process of maximizing your benefits from hormone therapy and minimizing any undesirable side effects. There are good options available now to help you achieve your goals for enhanced well being and improve your sexual zest, too!
Objective laboratory testing allows hormone doses to be specifically tailored to meet your needs as an individual. What should you be looking for as a desirable target range for testosterone? In my clinical experience, women typically experience their optimal normal energy level and libido when serum levels of total testosterone are between 40–60 ng/dl, with a free testosterone serum about 1 to 2 percent of the total testosterone. I now regularly check the blood level of free testosterone as well as the total. Free testosterone is the biologically active, unbound portion circulating in the blood, and the ratio of total to free is important in helping to determine the amount needed and the effects of other hormones on the testosterone balance. Imbalances between total and free testosterone give clues as to the direction to take in making dose adjustments to improve response or reduce side effects. Levels below about 20 ng/dl are generally too low to maintain your usual libido and energy. The majority of menopausal women I have evaluated, particularly those who have had surgical removal of the ovaries in their thirties and forties, have had testosterone levels of less than 10–15 ng/dl. This is certainly an understandable factor in fatigue or low energy, loss of muscle strength, and marked decrease in sexual desire.
As I said earlier, I haven’t found the saliva tests to be very reliable or useful, particularly for testosterone. The most current research has shown that it is not only the free testosterone that is biologically active at the receptor sites. The portion that is weakly bound to serum albumin is also now known to be active at certain of the testosterone receptors. So, if you just measure the free portion in the saliva (which is all this test can measure), you miss having the important added information provided by the serum test: total amount available for immediate release to the receptors as needed, weakly bound portion available for activating certain receptors, and the free portion that is most biologically active. If you don’t know all of these dimensions of your “testosterone account,” it is difficult to determine the correct dose and avoid side effects. In the patients I have tested saliva and serum at the same time, the results are so far apart that it is a major concern to me that women are making important hormone decisions based on only the saliva test of free hormone.
If you are going to the expense and effort of having your hormone levels checked, I encourage you to work with your physician to have the gold standard serum tests. This approach will give you the best picture possible of your hormonal balance. In my opinion, serum hormone tests are helpful, efficient, cost-effective, and provide psychological benefit by identifying a physical cause of the disturbing symptoms women may experience at midlife and around menopause. I feel strongly that such tests should be available to women, especially those who have had their ovaries removed. There are too many “hidden” medical, psychological, and relationship costs if you don’t know your physiological measures. You may find that it is too expensive not to have this information as you plan how to best achieve your health goals.
A healthy, vital, invigorating sexual responsiveness is an important dimension of your optimal well being throughout your adult years, whether it results from having a partner or self-pleasuring if you are alone. There are many books totally devoted to this subject, so I will hit only the highlights in my discussion of sexual vitality here.
Lifestyle habits are really important to review. Thieves of sexual vitality abound in our modern lifestyle. Cigarette smoking (and use of chewing tobacco) is a big culprit robbing you of sexual vitality. Nicotine in all forms of tobacco products constricts blood vessels and decreases blood flow to the pelvic organs in men and women, which causes impaired sexual arousal and performance. Vasoconstriction from nicotine affects men by decreasing blood flow to the penis, which markedly diminishes fullness and firmness of erections, especially as men get older and vascular damage from use of nicotine increases. Talking with men about this effect of tobacco has been one of my effective motivators to get men to stop smoking. Most of my male patients had never had a physician tell them that cigarette smoking adversely affects quality of erections as men grow older.
Alcohol is another thief of sexual vigor. Too much alcohol robs you of your sexual desire and your ability to respond normally. Alcohol is a depressant drug that dampens down the brain centers for arousal and orgasm. A small amount of alcohol may initially release your inhibitions and make you feel relaxed and “in the mood for sex.” After that, alcohol begins to make it harder to reach full arousal and orgasm. Men who have had too much alcohol often have difficulty achieving an erection that is full and rigid enough to allow satisfying intercourse.
Stress is another frequently overlooked thief of sexual interest and responsiveness when you have a hectic lifestyle. You may be simply too exhausted to relax and become aroused. Remember, the “flight or fight” adrenaline response evolved to help us escape danger, not to relax and become aroused for sex. If your adrenaline system is working overtime to keep up with the demands in your life, your sexual drive will be nil. Take time out to “get away,” slow down, relax, and enjoy the physical pleasures of relaxed foreplay and sexual exploration. Notice I said take time, not find time. You have to establish your priorities and take the time for what is important to you—it doesn’t just happen, given the busy lives we all lead today. And another thing: Get up and move your body. Exercise has a lot of well-publicized health benefits, including revving up your sexual energy and clearing away the sluggish feeling from stress overload. Besides, a fit body just feels sexier, to you and to your partner.
Medication side effects and medical disorders are other thieves of sexual vitality, sexual desire, and ability to have orgasm. Medicines such as serotonin-boosting antidepressants, mood stabilizers, beta blockers, blood pressure medication, diuretics, high progestin birth control pills, high dose progesterone creams, antianxiety and sleeping medications may all cause reduced sexual desire and difficulty having an orgasm. Unrecognized medical disorders such as diabetes are other causes of loss of sexual desire and problems with orgasm. It really is important to have a thorough medical checkup and appropriate laboratory tests if you have noticed a significant change in your sexual desire; painful intercourse; vaginal dryness, burning, or itching; or diminished ability to have an orgasm (or for men, diminished ability to achieve an erection). This checkup should include a physical examination by your primary care physician or specialist, laboratory tests of general blood chemistries, blood glucose, liver function tests, tests for sexually transmitted diseases, and hormone blood tests (especially thyroid, estradiol, and testosterone). If your hormone levels are too low, talk with your physician about an appropriate hormone regimen to help you regain your sexual vitality. More information on hormone therapy regimens is found in chapters 5 and 15. Healthy lifestyle changes I described above are your primary foundation, so be sure to address these. Hormones do help many women immensely, as my patients tell me after they experience the balance right for them: “It’s like someone turned the light switch back on! I just feel better.”
Relationships often change at midlife, and many women find themselves back in the dating arena after many years in a stable relationship. I feel it is important to address the issue of sexually transmitted diseases (STDs), all of which are far more common today than when many of us baby-boomers were becoming sexually active. Bacterial vaginitis, trichomonas, chlamydia, herpes, human papilloma virus (“venereal warts”), gonorrhea, syphilis, and now AIDS. The list is daunting. While AIDS is the most feared STD, the others are many times more common and may result in a variety of symptoms that rob you of sexual pleasure and vitality. And yet, women are still frequently too shy about asking male sexual partners to wear a condom for fear of hurting their feelings. Women wake up! You are the only one who can take steps to protect yourself. I will tell you bluntly that if a man is worth sharing your body with, he should be concerned enough about your health to wear a condom. This is particularly true in new relationships, or even in long-standing relationships if there is any indication that your partner has had sexual encounters outside of your relationship. With proper use of a latex condom, you markedly decrease your risk of getting STDs, unless you have unprotected oral sex with a partner who has an active infection. For best protection against STDs, use of a high-quality latex condom should be combined with use of a spermicidal foam or jelly. In recent studies, the most widely used spermicide, nonoxynol-9, has been shown to kill all of the bacteria and viruses listed above. If you are concerned about whether your partner will have a condom available, you can always carry your own supply and be in control of having one when you need it.
The incidence of AIDS in women in this country has been largely underestimated until recently due to the fact that women in the early stages of the disease suffer different manifestations such as chronic vaginal infections. This wasn’t even initially included as one of the criteria symptoms of AIDS. Another factor is that virtually all the research on AIDS has been done on homosexual men, the population in which it first developed. Women with AIDS also frequently die of different causes and infectious illnesses than do men. Men with AIDS have been twice as likely to get AZT as women, a drug that clearly prolongs survival. Not surprisingly, the survival rate of women with AIDS is significantly lower than that of men, according to a study conducted by the Maryland Department of Health in Baltimore. If the current trends continue, AIDS will be the fifth leading cause of death next year for women between the ages of fifteen and forty-four. Not using a condom may be potentially life threatening. Be aware, and be prepared.
Often, patients tell me that their doctors have never asked about their sexual activity or changes in sexual function. Many physicians are still embarrassed to initiate this discussion with patients, particularly women in midlife and beyond. Then I hear physicians say that they assume their patients will tell them if they are having sexual problems, but most women tell me they are too embarrassed to bring this issue up when they see their doctor. So it ends up being a stand off, and the discussion doesn’t happen. I urge you to be proactive and bring up your sexual questions and concerns when you see your physician. Take responsibility for your health and ask. If sex has become painful, you may want to consider using one of the nonhormonal lubricants such as Astroglide or Replens. If these don’t do the trick and sex is still painful, it would help to read chapter 12 about the effects on the vagina and bladder as we lose estradiol and testosterone. I have outlined a number of ways to use topical hormone preparations to improve the health of the vagina, reduce vaginal and bladder infections that make sex painful, and also help alleviate the pain of vulvodynia and vestibulitis.
One of the most common problems I encounter in my medical practice is primarily a lack of knowledge about the human sexual response in men and women; concerns over what is “normal” and culturally derived unrealistic performance expectations. Consequently, I have included a list of resources in appendix II that will give you additional ideas for enhanced sexual vitality and rekindling the sexual fires. My patients, men and women of all ages, tell me that the ones listed have been helpful, well written, and beautifully descriptive of the wide variety of sensual pleasures. Dr. Miriam Stoppard’s book, The Magic of Sex, is the best I have seen as a comprehensive, beautifully illustrated, and sensitively written guide for sexual enjoyment for men and women.
Another resource you may find helpful is the Sensate Focus Experience. This series of sexual pleasuring exercises is designed to help you and your partner explore each other’s bodies and communicate your feelings to each other so as to help each of you learn what is most pleasing, arousing, and desirable for the other. You may also do this alone if you do not have or want a partner. This series of exercises is described in more detail in many of the books I have included on the resource list. Briefly, the Sensate Focus Experience establishes a structure to help both of you relax and not feel pressured to perform sexually. You and your partner commit to a specified amount of time, for example thirty minutes or an hour. Select a time and place when you won’t be interrupted and are able to “tune out” stressful stimuli. You may want to help create the desired mood with music, candles, pleasant fragrances, and sensuous fabrics. One person begins as the receiver of the sensate pleasuring, and the other person is the giver. In the next time together, you alternate roles. During the entire time of the session, the giver caresses, touches, and explores the receiver’s body. The receiver gives positive feedback about what feels pleasurable, what is less desirable, and what is uncomfortable. What does one do during these pleasuring times? Be creative! You may also have to redo the “mental tapes” from childhood prohibiting touching various body areas. Nothing is off limits for you as an adult unless it causes discomfort or pain for the partner. You may find ideas in some of the resource books in appendix II.
I encourage couples to proceed, at your own pace, through the following levels of Sensate Focus Experience:
Level I: nonerotic, nongenital pleasuring
Level II: erotic, nongenital pleasuring
Level III: erotic and genital pleasuring
Level IV: pleasuring that proceeds to intercourse
Prior to reaching Level IV, couples agree to abide by the guidelines of no intercourse, no matter how sexually aroused you become. Keeping this agreement helps build trust and reduce performance anxiety. If you commit to this process, and communicate with each other positively and sensitively, you will likely find the “fires” rekindled in your sexual encounters.
Sexuality does not have to decline as we age. There are many avenues for keeping your sexual interest and vitality alive and well. Some of these approaches you control, and some of these options are ones you will need to explore with your physician. Before you visit your doctor, you may find it helpful to explore your feelings about your sexuality in the self-check questionnaire in appendix III: “How’s My Sexuality?” Jot down whatever comes to mind about each of these questions. This will give you a list of topics when you go in for your medical visit and may help you focus your questions in the time you have with your doctor. If your physician doesn’t seem interested or knowledgeable in these areas, then seek other resources for help. Don’t just suffer silently. Know that help is available and that you deserve to enjoy your sexuality, whatever your age!