Calculating the ketogenic diet requires a combination of a full nutritional assessment and an understanding of the child’s medical condition, mixed with experience and intuition. In each case, a child’s individual needs must be taken into account. At Johns Hopkins, we meet as a group a week in advance of every ketogenic diet week and discuss each patient’s needs (e.g., ratio, possibility of fasting, calories, medications, etc.). Because each child is different, this really helps guide management.
Calculating the caloric requirements of an individual child requires consideration of both the child’s current and desirable weight as well as the patient’s activity level. However, calculating the caloric needs of children going on the ketogenic diet should not be any different than calculating their needs if they were on a regular diet. The dietitian needs to look at history of weight and length gain over the years and evaluate the child’s current eating habits and patterns before estimating their nutritional needs. A 3-day food record with the exact amounts of food eaten plus a growth chart or detailed weight history is essential in figuring out a child’s caloric intake. We often match the ketogenic diet calories to the prior 3-day food record calories.
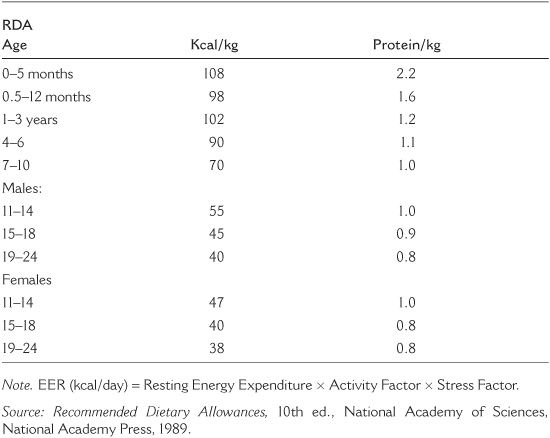
The ketogenic diet is generally based on the recommended daily allowance (RDA) of calories for a child’s weight, but it can be modified to allow for such factors as the child’s activity level and natural rate of metabolism. The goal of the diet is to provide optimal seizure control and maintain adequate nutrition for growth. When we make our initial estimates of a child’s dietary needs, we begin by assessing the age, weight, height, health, activity status, and a current 3-day food record for each child. The ketogenic diet may be beneficial when a patient maintains their growth percentiles and doesn’t gain weight or lose weight too rapidly.
Underweight children need to gain weight in order to have sufficient fat reserves to burn for ketosis between meals. Obese children may need to lose weight because if there is too much body fat, a child may have difficulty obtaining sufficient ketosis to control seizures. Severely handicapped children may be smaller in size and weight than average for their age. That is just the start; because a child’s activity level is also an important determinant of caloric needs, a very active child may need more calories than a less active one. Profoundly handicapped children, who sometimes are very inactive, usually require fewer calories than an average child.
There is limited evidence that calorie restriction makes much of a difference in seizure control. Although this may be true in animals put on ketogenic diets, we don’t always see that in children. In fact, on the modified Atkins diet, many children eat more calories than before they were treated! However, there are some children who seem to respond to cutting calories. Every child is different (see Table 8.1).
Recommended daily protein allowances are calculated for average children of a given height and weight and an average activity level. The goal is to reach as close to the RDA for age of protein as possible. In adolescents it may be difficult to achieve the proper fat to carbohydrate ratio if 1 gram of protein per kilogram of bodyweight is given. In this case we may use as little as 0.75 grams of protein per kilogram. Growth is closely monitored every 3 to 6 months and is used as a guide of adequate nutrition. The evidence, however, suggests that the biggest impediment to growth is overketosis, rather than insufficient protein.
TABLE 8.1
Estimating Energy Requirements (EER)
Anecdotally, in the past it was thought that a fluid restriction on the ketogenic diet may help with increased seizure control. This probably was due to concentration of the urine and, therefore, apparently higher levels of urine ketosis. Recent studies and years of evidence have determined that fluid restriction has no effect on seizure control. Therefore, we try and maintain as close as possible to 100% of fluid maintenance values. These numbers are based on the child’s weight in kilograms and are more of a goal fluid volume than a restriction.
Fluid intake should be individualized and increased with an increase in activity or a hot climate. Children in warmer countries may need more fluids than colder climates. Fluids are encouraged during illness. Monitor your child for signs and symptoms of dehydration like cracked lips, decreased urination, and a dry mouth.
The case of James illustrates the thought process of a dietitian evaluating an individual coming in for ketogenic diet initiation:
James is a 4-year and 7-months-old male with a history of infantile spasms (myoclonic seizures) and developmental delay. Seizure onset was at 12 months of age. Seizure frequency is 100–150 jerks/day.
CURRENT MEDICATIONS: Topamax® 75 mg BID, Depakote® 375 mg TID, Tranxene® 0.9 mg daily. Supplements: Bugs Bunny multivitamin/mineral.
LABS: No current labs available.
FEEDING ABILITY: No impairment—James feeds himself—no problems with chewing, swallowing, etc. No history of pneumonia or aspiration.
James’s mother reports his appetite to be poor and states that he is a “picky eater.” James normally eats a great deal of starches (pasta, bread, etc.) as well as vegetables. He does not like meat very much. He eats three meals and two snacks daily. Food preferences were recorded. Activity is low to normal—James participates in physical therapy once a week and recess at school. His bowel movements are normal for the most part. No known food allergies or intolerances.
THREE-DAY FOOD RECALL: Average intake 1,290 kcal, 42 gram protein, vitamin/mineral consumption adequate with the exception of calcium.
WT: 18.4 kg (HEIGHT 111.8 cm (40.5 lbs) 44 inches)
WT FOR AGE: 50–75%
HT FOR AGE: 75–90%
WT FOR HT: 25–50%
James’s growth pattern has been relatively normal—both height and weight were proportional following the 75% to 90% curve until 6 months ago. His mother said that James has been the same weight for 6 months now, despite an increase in height. She attributes his lack of weight gain to a decreased appetite since the addition of Topamax®.
PHYSICAL ASSESSMENT: No physical signs of deficiencies. James appears to be well nourished, although quite lean.
James does not appear to be at nutritional risk at this point. Despite not gaining weight for 6 months, he is still 95% of his ideal weight, and weight has crossed only 1 percentile. He looks healthy and is consuming what is recommended for age for protein, macro- and micronutrients (with the exception of calcium intake of only 700 mg). Caloric intake is obviously a bit too low as seen by the lack of weight gain and the fact that James is under his ideal body weight. It is reasonable to start him at his current caloric intake (and increase later if necessary) at a 4:1 ratio. We do not want him to lose weight, and the high ratio will allow us to provide the fat needed for ketosis via the diet.
1,300 kcal, 4:1 ratio, 1,400 cc total fluid daily. To be given in three equal meals and two snacks of 75 kcal during the day.
KCAL: 1,300 (70.7 kcal/kg body weight)
TOTAL PROTEIN: 24.5 gram
TOTAL CARBOHYDRATE: 8 gram
TOTAL FAT: 130 gram
TOTAL FLUID: 1,400 cc (100% of estimated maintenance needs)
1. Seizure control.
2. Maintaining current growth curve. Increasing kcal in small increments (5% to 10% of kcal every 2 to 4 weeks) should be sufficient to attain this goal provided that seizures are well controlled. James will probably not only have improvement of appetite, but hopefully of activity as well if his seizures can be controlled.
3. Maintaining optimal nutritional status (maintaining growth and overall nutritional status long term).
4. Weaning medications once the diet is fine-tuned satisfactorily.
1. Implement diet, educate parents.
2. Attain biochemical indices to check nutritional status (visceral protein status, anemias, electrolytes, hydration, renal function, etc.).
3. Discuss Topamax® wean with physicians after 1 month of the diet. Weaning this medication aggressively might help improve James’s appetite.
4. Order multivitamin/mineral supplement that meets patient’s recommended micronutrient needs 100%.
5. Continue to track height, weight, seizure control, etc., via phone/email/fax.
6. See James at 3-month follow-up visit.
Once judgments are made about ideal weight, ketogenic ratio, and liquid allotment, the ketogenic diet can be calculated.
1. Decide on an optimal level of calories. This should be done using a thorough medical and nutritional history and the dietitian and physician’s professional judgment. Variables such as the child’s activity level, frame size, medical condition, recent weight gain or loss, and so forth, must be taken into account.
2. Set the desired ketogenic ratio. Most children ages 2–12 years old are started on a 4:1 ketogenic ratio. Medically compromised children may be started on a 3:1 ratio of fat to combined protein and carbohydrates. Children under 2 years of age and adolescents are usually started on a 3:1 ratio.
3. Fluid levels should be set at about 90–100% of maintenance for healthy, active children. Liquids are increased for fragile children and infants under 1 year of age.
4. Always strive to attain RDAs for protein (and never allow protein to fall below World Health Organization [WHO] standards).
5. The ketogenic diet must be supplemented daily with calcium, vitamin D, and a carbohydrate-free multivitamin with minerals. The diet is not nutritionally sufficient without supplementation.
Because this book is written for both parents and medical professionals, and because we believe that the diet works best with informed parents as part of the team, we believe it is important to know as much about the diet as possible. However, …
THE KETOGENIC DIET should never be attempted without careful medical and nutritional supervision.
Roseanne is a girl who almost died because her parents started her on the ketogenic diet without consulting a doctor. She was 5 years old when she was admitted to Hopkins’s intensive care unit with pneumonia, dehydration, and a very low pulse rate. There were major concerns about whether she would survive the night. She appeared wasted and fatigued and looked as though she had been starved by her parents.
The nurse called the child abuse team. The parents arrived a few minutes later, having followed the ambulance from the referring hospital. They seemed very nice and very concerned. They said that Roseanne had suffered from lack of oxygen at birth and was quite developmentally delayed. At 5, she still could not sit by herself or communicate. Roseanne had experienced seizures since she was 6 months old and had been treated with many medications without much success. Her parents had come to the conclusion that not only were the medications not helping, but their side effects were part of the reason for Roseanne’s lack of progress.
“All those doctors were doing was experimenting on our daughter,” they said.
Then the parents had seen Jim Abrahams’s TV movie about a diet for epilepsy that would “get you off the medications.” When they called Hopkins, they were told that Hopkins would not be able to put Roseanne on the diet for 3 months. Her parents felt they couldn’t wait that long, so they started the diet by themselves.
“It wasn’t so hard at first,” they said, and the seizures were better, until the last month when she just didn’t seem to want to eat. Then she started throwing up and breathing funny. “I guess now you’ll have to take her!” the parents said.
Roseanne had pneumonia but was also severely acidotic, malnourished, and dehydrated. With intensive care over the course of a week she gradually came around and was able to be discharged home, but not on the diet. Until she had built up her reserves and had become better nourished, we felt that the diet posed too much of a risk. Frustration with the medical profession and impatience with the processes involved almost resulted in the child’s death.
1. AGE AND WEIGHT. Fill out the following information:
Age __________
Weight in kilograms __________
Mary has been prescribed a 4:1 ketogenic diet. She is 4 years old and currently weighs 15 kilograms (33 pounds). Her dietitian has determined that this weight is appropriate for Mary.
2. CALORIES PER KILOGRAM. After a full medical and nutritional assessment, a dietitian will assign a calorie per kilogram level for diet initiation.
The dietitian has set Mary’s diet at 72 kcal/kg. (Note that this figure involves a dietitian’s judgment; it is usually based on comparing the child’s current intake with the RDA.)
3. TOTAL CALORIES. Determine the total number of calories in the diet by multiplying the child’s weight by the number of calories set per kilogram.
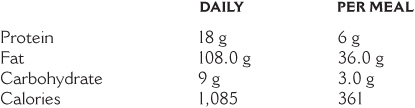
Mary, age 4 and weighing 15 kilograms, needs a total of 72 × 15 or 1,085 calories per day.
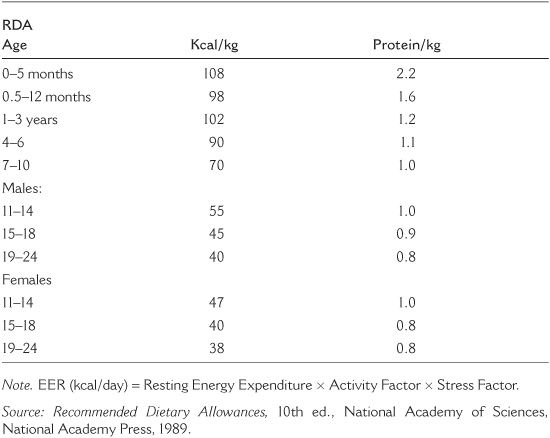
4. DIETARY UNIT COMPOSITION. Dietary units are the building blocks of the ketogenic diet. A 4:1 diet has dietary units made up of 4 grams of fat to each 1 gram of protein and 1 gram of carbohydrate. Because fat has 9 calories per gram (9 × 4 = 36), and protein and carbohydrate each have 4 calories per gram (4 × 1 = 4), a dietary unit at a 4:1 diet ratio has 36 + 4 = 40 calories. The caloric value and breakdown of dietary units vary with the ketogenic ratio:
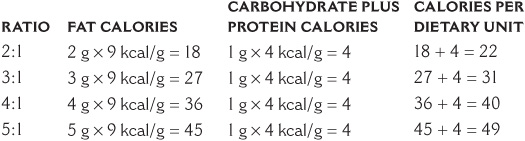
Mary’s dietary units will be made up of 40 calories each because she is on a 4:1 ratio.
5. DIETARY UNIT QUANTITY. Divide the total calories allotted (Step 3) by the number of calories in each dietary unit (Step 4) to determine the number of dietary units to be allowed daily.
Each of Mary’s dietary units on a 4:1 ratio contains 40 calories, and she is allowed a total of 1,085 kcal/day, so she gets 1,085/40 = 27 dietary units per day.
6. FAT ALLOWANCE. Multiply the number of dietary units by the units of fat in the prescribed ketogenic ratio to determine the grams of fat permitted daily.
On her 4:1 diet, with 27 dietary units/day, Mary will have 27×4, or 108 grams of fat per day.
7. PROTEIN + CARBOHYDRATE ALLOWANCE. Multiply the number of dietary units by the number of units of protein and carbohydrate in the prescribed ketogenic ratio, usually one, to determine the combined daily protein + carbohydrate allotment.
On her 4:1 diet, Mary will have 27 × 1, or 27 grams of protein and carbohydrate per day.
8. PROTEIN ALLOWANCE. The dietitian will determine optimal protein levels as part of the nutritional assessment, taking into account such factors as age, growth, activity level, medical condition, etc.
Mary’s dietitian has determined that she needs 1.2 gram of protein per kilogram of body weight (18 grams total).
9. CARBOHYDRATE ALLOWANCE. Determine carbohydrate allowance by subtracting protein from the total carbohydrate + protein allowance (Step 7 minus Step 8 above). Carbohydrates are the diet’s filler and are always determined last.
Mary’s carbohydrate allowance is 27 – 18 = 9 grams of carbohydrate daily.
10. MEAL ORDER. Divide the daily fat, protein, and carbohydrate allotments into the desired number of meals and snacks per day. The number of meals will be based on the child’s dietary habits and nutritional needs. It is essential that the proper ratio of fat to protein + carbohydrate be maintained at each meal.
Mary’s dietitian has decided to give her three meals and no snacks per day:
Note: This example is simplified for teaching purposes. In reality, most 4 year olds would be prescribed one or two snacks in addition to their three meals. The snacks would be in the same ratio (4:1) and the meals reduced by the number of calories in each snack.
11. LIQUIDS. Multiply the child’s desirable weight by the value shown on the chart listed earlier in this chapter to determine the daily allotment of liquid. Liquid intake should be spaced throughout the day. Liquids should be noncaloric, such as water, or decaffeinated zero-calorie diet drinks. In hot climates the cream may be excluded from the fluid allowance (in other words, liquids may be increased by the volume of the cream in the diet). The liquid allotment may also be set equal to the number of calories in the diet.
Mary, who weighs 15 kg, is allowed 1000 + (50 × 5) = 1250 ml × .9 = 1125 cc of fluid per day, including her allotted cream.
12. DIETARY SUPPLEMENTS. The ketogenic diet is deficient in some nutrients. Multivitamin and mineral supplements are required. In choosing a supplement it is important to consider carbohydrate content. Children who are not medically compromised can usually be adequately supplemented with an over-the-counter, reputable multivitamin and mineral supplement and a separate calcium supplement. Most children do well with commercially available supplements, although these have been alleged to lack some micronutrients.
Calculating the meal plan, in contrast to the diet prescription, is a fairly straightforward procedure. There are currently two different ways of calculating the meal plans: by hand or by computer.
The hand calculation method uses exchange lists and rounded nutritional values for simplicity. This method is cumbersome, time-consuming, and based to a certain extent on nutritional averages. It is, however, the method that was used at Johns Hopkins and elsewhere with much success before the availability of personal computers. It is important that dietitians become familiar with the hand calculation method in order to fully understand the logic of meal planning, and in case a computer is not available in a pinch.
There are several computer programs available at many centers that are used by the dietitian to create meal plans. One such program is KetoCalculator (see Chapter 9). Because the computer program uses data about the precise nutritional content of specific foods, whereas the hand calculation method relies on averages in order to simplify the math, the computer program may result in slightly different numbers of calories and grams for a given meal than the hand calculation method.
NO PROGRAM SHOULD be initiated or changed without the oversight of a dietitian to be certain that the nutritional information is up-to-date.
Generic Group A and B vegetables and fruits can be exchanged with both methods of meal calculation. It is easy for parents to switch from one Group A vegetable to another or one 10% fruit to another, depending on the child’s whims or what is available in the grocery store. The exchange lists assume that there will be some variety in the diet. If the child only likes carrots and grapes—which contain the highest carbohydrate levels on the exchange lists—then she could end up with less than optimal seizure control. In this case the meal plans should be recalculated specifically for carrots and grapes.
The precision of the computer calculations shows the minor differences between the content of, say, broccoli and green beans. For most children these minor differences are of little importance. Therefore, once the computer has calculated a meal plan, and assuming that the child is doing well on the diet, exchanges may still be made among the foods on the fruit and vegetable exchange lists. If better seizure control is needed, however, in some cases it may be achieved through the use of specific meal plan calculations instead of exchange lists.
With the availability of the computer program, we no longer use meat exchange lists. The fat and carbohydrate contents of meats vary too greatly. The exchange lists are still used with hand calculations.
The dietitian provides parents with a set of basic meal plans before they go home from the hospital. When parents call the dietitian to discuss meal plans, they can refer to these basic meals by title. The basic meal plans are:
1. Meat/fish/poultry, fruit/vegetable, fat, cream
2. Cheese, fruit/vegetable, fat, cream
3. Egg, fruit/vegetable, fat, cream
The meat and cheese should be designated specifically (i.e., chicken, fish, parmesan) in actual meal plans. When specifics are added, the result will probably be a basic set of six or eight meal plans sent home from the hospital with the parents.
AVERAGE FOOD VALUES FOR HAND CALCULATIONS
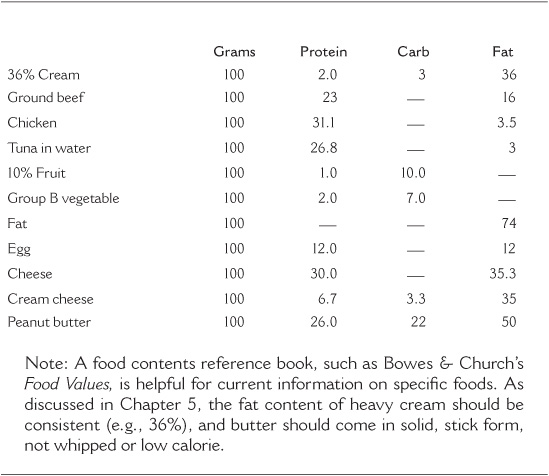
CROSS MULTIPLICATION: THE KEY TO USING THE FOOD LIST
Question: If 100 gram of 36% cream contains 3.0 gram carbohydrate, how much cream contains 2.4 gram of carbohydrate?
Answer: 80 gram of 36% cream contains 2.4 gram of carbohydrate.
1. Jeremy, a 9-year and 3-month-old boy, is to be placed on a 4:1 ketogenic diet. His actual weight is 32 kg, and his height is 134 cm. According to the standard charts, he is at 50% for height but 90% for weight. His ideal weight is estimated at 29 kg.
2. The dietitian estimated Jeremy’s calorie allotment at 60 calories per kilogram. One of the dietitian’s goals was to have Jeremy gradually achieve his ideal weight. Toward this end, Jeremy’s total calorie allotment is set by multiplying his ideal weight by 60: 29 × 60 = 1,740 calories per day.
3. Each of Jeremy’s dietary units will consist of:
4 gram fat (9 calories per gram) = 36 calories
1 gram carbohydrate + protein (4 calories per gram) = 4 calories
Total calories per dietary unit = 40 calories
4. Jeremy’s dietary units will be determined by dividing his total daily calorie allotment (Step 2) by the calories in each dietary unit: 1,740 calories/40 calories per dietary unit = 43.5 dietary units per day.
5. Jeremy’s daily fat allowance is determined by multiplying his dietary units (Step 4 above) by the fat component in his diet ratio (4 in a 4:1 ratio): 43.5 × 4 = 174 gram fat.
6. Jeremy’s protein needs are at a minimum 1 gram of protein per kilogram of body weight. His ideal weight is 29 kg, so he needs at least 29.0 gram protein daily.
7. Jeremy’s daily carbohydrate allotment is determined by multiplying his dietary units (Step 4 above) by the 1 in his 4:1 ratio, then subtracting his necessary protein (Step 6 above) from the total: 43.5 - 29 = 14.5 gram carbohydrate per day.
Jeremy’s complete diet order will read as follows:
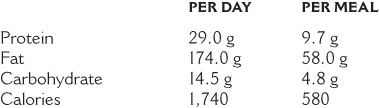
Note: Most children are now given a meal plan that includes one or two snacks, which would diminish the quantity of food in the three main meals. If Jeremy does not lose weight, is not in sufficient ketosis, or turns out to not be as active as originally thought, the caloric amounts will be recalculated during the fine-tuning period.
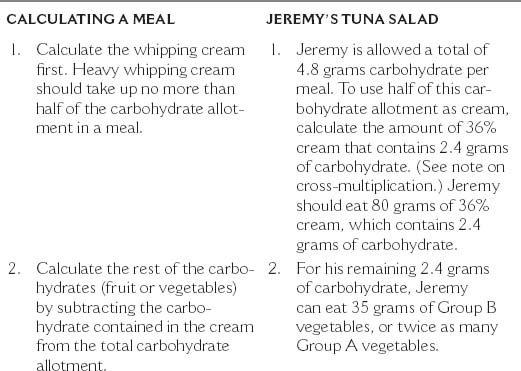
CALCULATING A MEAL JEREMY’S TUNA SALAD
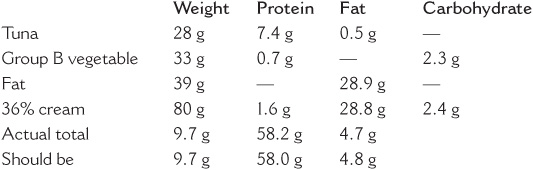
The 4:1 ketogenic ratio of this menu may be double-checked by adding the grams of protein + carbohydrate in the meal and multiplying by 4. The result should be the amount of fat in the meal, in this case 58 grams. Since (9.7 + 4.8) × 4 = 58, the ratio is correct.
• Jeremy likes his cream frozen in an ice cream ball (slightly whipped), flavored with vanilla and saccharin, and sprinkled with a little cinnamon.
• Jeremy’s mom arranges the vegetables in thin-sliced crescents or shoestring sticks around the tuna.
• If Jeremy doesn’t like as much mayonnaise with his tuna, some of his fat allowance in the form of oil can be calculated and whipped into the cream one hour after it goes into the freezer. The fats on the exchange list can be used interchangeably—a meal’s fat can be provided as all mayonnaise, half mayonnaise and half butter, or the oil may be calculated and mixed with the butter, depending on the child’s taste and what makes food sense. In the case of hiding fat in ice cream, oil works nicely because it is liquid and has little flavor.
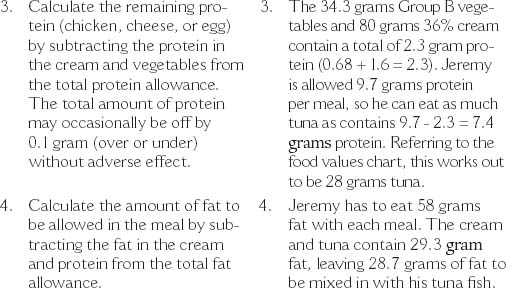
Q. How do you add extra ingredients to a meal plan when calculating by hand?
A. Take the tuna salad as an example. Suppose Jeremy wants to sprinkle baking chocolate shavings on his ice cream and bacon bits on the tuna salad. You would add a line for bacon and a line for baking chocolate in your hand or computer calculation. Then choose a small quantity, perhaps 5 grams of bacon and 2 grams of baking chocolate, and fill in the values for protein, fat, and carbohydrate of each. The quantities of other ingredients would then have to be juggled downward until all the columns add up to the proper totals. Bacon, which contains protein and fat, will take away from the meal’s tuna and mayonnaise allotment. Baking chocolate, which is primarily fat and carbohydrate with a little protein, will take away from the amount of tomatoes in the meal. As the overall carbohydrate allotment is very small and the nutritive value of chocolate is less than that of vegetables, no more than 2 grams of chocolate should be used in a meal on the 4:1 ratio. With the accompanying computer program, an additional ingredient may simply be filled in on a blank line and the other ingredients adjusted until the actual totals match the correctly prescribed ones.
Q. When is it necessary to make calorie adjustments?
A. Weight should be monitored on a weekly basis for the first month, and height on a monthly basis. Infants should be weighed and measured accurately at the pediatrician’s office about every 2 weeks. At least during the first 3 months, the ketogenic diet team should be informed monthly of a child’s height and weight changes and any other relevant information. Once a child is started on the diet, changes in the diet order are usually made in response to the child’s own performance—weight loss or gain, growth in height, seizure control, and so forth. We evaluate in this manner and may make adjustments based on these factors throughout her time on the diet.
Q. How often should a child eat on the ketogenic diet?
A. The number of meals and snacks included in a child’s diet should approximate her pre-diet eating habits (when possible), the family’s schedule, and always take into account her nutritional needs. Infants will need to be given about six bottle feedings a day. Toddlers will probably need three meals and one or two snacks. Older children might need three meals and only one snack. Some children gain better ketosis overnight and achieve early morning seizure control by having a bedtime snack. Snacks are sometimes used to test how many extra calories are needed for a child who is losing weight and whether the extra calories cause any seizure activity problems.
Sarah was doing well on the diet, eating three meals and one afternoon snack. Her seizures were virtually gone during the day, but she was still having seizures early every morning. At her follow-up checkup the dietitian learned that Sarah was eating dinner at about 5:30 P.M., going to bed around 7:30, and waking up at 7:00 for breakfast. It seemed that in the 13.5 hours between dinner and breakfast, Sarah was running out of fats to make ketones! The dietitian offered the family the choice of having Sarah eating dinner later, or of having an evening snack. They decided on the snack. Once Sarah started eating her snack at bedtime, the early morning seizures disappeared.
Q. Is it necessary to use half of the carbohydrate allotment as cream?
A. Using up to half of the carbohydrate allotment as cream is a guideline, not a hard and fast rule. It’s meant to replace milk for children who drink milk, and cream can be an easy way to fit a lot of fat into the diet in a way that most children enjoy. However, children who do not like milk do not have to drink the cream; they will just have to have more mayonnaise, butter, or oil. Some children like to eat fat, some don’t. Some children love cream, some don’t. As long as the diet makes food sense, there is no need to use half of the carbohydrate allotment as cream.
Lily is 24 months old and weighs 12 kilos. She is 86.5 cm. tall. Both her height and weight are at the 50th percentile. She is going to start on a 4:1 ketogenic diet. What will her diet order read?
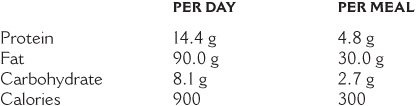
1. At age 2 years, Lily’s calorie per kilogram requirement will be approximately 75 calories per kilogram. (As indicated previously, calorie requirements vary with the metabolism and activity level of the child and must be individually assessed.) Her ideal weight is the same as her actual weight, 12 kilograms. So Lily’s total calorie allotment is 75 × 12 = 900 calories per day.
2. Lily’s dietary units will consist of 40 calories each, the standard for a 4:1 diet.
3. Lily’s dietary units are determined by dividing her total calorie allotment by the calories in each dietary unit. So she will have 900 / 40 = 22.5 dietary units per day.
4. Lily’s daily fat allowance is determined by multiplying her dietary units (22.5) by the fat component in her ratio (4 in a 4:1 ratio). She will thus be allowed 22.5 × 4 = 90 gram fat per day.
5. Lily’s protein and carbohydrate allotment is 22.5 grams per day, determined by multiplying her dietary units (22.5) by the 1 in her 4:1 ratio. As a young, growing child she may need 1.1–1.5 grams of protein/kg. Her weight is 12 kg, so allowing 1.2 grams of protein per kilogram per day makes her protein allotment 14.4 grams per day.
6. Lily’s daily carbohydrate allotment is determined by subtracting her protein allotment (14.4 grams) from the total protein and 1 carbohydrate allowance (22.5 grams): 22.5–14.4 = 8.1 grams carbohydrate per day.
Lily’s complete diet order will read as follows:
Note: As mentioned previously, most 2 year olds eat one or two snacks in addition to their three meals a day. This example has been simplified for teaching purposes.
For dinner, Lily would like to eat grilled chicken with fruit salad and a vanilla popsicle. How would you calculate this meal?
1. Start from the per-meal diet order. Lily is allowed a total of 2.7 grams carbohydrate per meal. To use half of this allotment as 36% cream, her popsicle should contain 45 grams cream, which will provide 1.35 grams carbohydrate.
2. To provide her remaining 1.35 grams carbohydrate, she can have 13 g of 10% fruit.
3. The 10% fruit and 36% cream contain a total of 1.03 grams protein. Lily’s total protein allotment for the meal is 4.8 grams, so she can eat as much grilled chicken as will provide 4.8–1.03 = 3.77 grams protein. This works out to 12 grams chicken.
4. Lily is allowed 30 grams of fat in each meal. The chicken and cream contain a total of 16.5 grams fat. Lily should eat 17 g of butter or mayonnaise to provide the additional 13.5 grams fat allotment.
Lily’s dinner plan will read as follows:
CHICKEN CUTLET WITH FRUIT SALAD
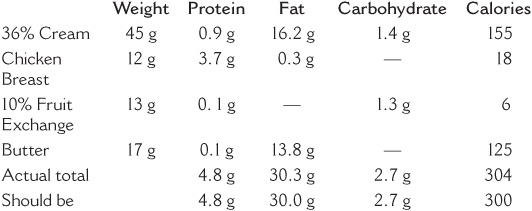
Notes on Lily’s meal: The chicken can be pounded to be very thin to make it look bigger on the plate. The fruit salad will be pretty if composed of small chunks of water-packed canned peaches and fresh strawberries. Lily thinks it is fun to pick up the chunks with a toothpick. The cream can be diluted with some allotted water, sweetened with saccharin, flavored with four or five drops of vanilla and frozen in a popsicle mold in advance of the meal. Lily loves butter; she will eat it straight or it can be spread over her chicken. A small leaf of lettuce can be added to the meal for extra crunch.
The consistency of the ketogenic diet can be modified for all children, with various diets prior to admission. It can be calculated for bottle-fed infants, small children making the transition from bottle to soft food, or children with special feeding problems. The ketogenic diet can be formulated in any texture—liquid, soft, solid, or a combination—and can be easily used even by children who need to be fed by nasogastric or gastrostomy tube. Multiple studies stress how easy, well-tolerated, and beneficial it can be to use the ketogenic diet as a formula-only treatment.
As discussed previously, seizures or the side effects of anticonvulsant medications may affect a child’s ability to eat properly. If the seizures are controlled or medications can be reduced while on the ketogenic diet, the child may be able to work with different therapists to transition from a soft diet to a diet with more textures. The process of calculating the diet and of establishing calorie levels and the grams of fat, protein, and carbohydrate permitted on the ketogenic diet is the same regardless of the consistency of the food.
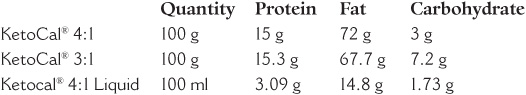
There are many options for using formula for the ketogenic diet. Based on the formula that the child is on prior to diet initiation, a comparable keto formula is chosen. The formula can consist of three components mixed together with water to equal the correct calorie and ratio or KetoCal®, manufactured by Nutricia North America, which comes as a ready-to-feed liquid (in “tetra-paks”) or as a powder. The KetoCal® Liquid comes in a 4:1 ratio, is nutritionally complete for children over 1 year of age, vanilla flavored, contains fiber, has no trans fats, and has only 15% saturated fats. KetoCal® powder is formulated in either a 3:1 or 4:1 version and is nutritionally complete for children over 1 year of age. All KetoCal® products are milk based and can be taken orally or via enteral feedings. There is also a new formula called KetoVolve® that is not on the market at time of publication but is manufactured by Solace Nutrition. This formula will have no trans fats, is 100% whey protein versus casein/whey mixture, and is lactose free. The company also states that it will be kosher and halal certified.
The Modular formula consists of three parts:
1. Ross Carbohydrate-free (RCF)®
—Soy-based protein, avoids symptoms of cow’s milk sensitivities
—Available through Abbott in a concentrated liquid: 13 fluid ounce cans; 12 per case
2. Microlipid® (Mead Johnson)®
—A safflower-oil emulsion that mixes easily in solution
—Available in 89 ml bottles; 48 bottles per case
3. Polycose® Powder (Abbott)®
—Source of calories derived solely from carbohydrate
—Available through Abbott in powder form (350 gram cans); 6 per case
In the case of multiple food allergies or stomach intolerances to intact proteins, there is another formula that can be used in the modular formula instead of RCF®.
4. Complete Amino Acid Mix®
—Essential and nonessential amino acids
—Indicated for patients with milk protein allergy
—Needs complete vitamin supplementation
—From SHS-Nutricia
Carbohydrate-free multivitamins and minerals, calcium supplements, and sterile water are added to complete the mixture.
FOOD VALUES FOR LIQUID DIET CALCULATION
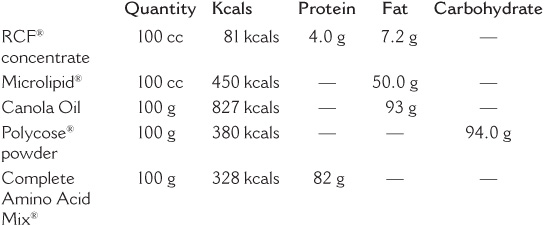
Because it is emulsified, Microlipid® mixes easily with the other ingredients compared to oil. However, Microlipid® can be more expensive than corn oil or canola oil. Vegetable oil (e.g., canola) may be used for larger (older) children or when expense is a factor. MCT oil may also be added to a formula if the dietitian thinks it is needed, for instance, to loosen stools or boost ketosis. (More details on MCT oil in Chapter 20.)
Emily was a 13-month-old girl admitted for the ketogenic diet in an attempt to achieve better control of her intractable seizures that had continued despite heavy medications. She had been fed by gastrostomy tube since she was 8 months old. She was started on a 3:1 ratio at 80/kg and protein at 1.6/kg of desirable body weight.
Emily’s age: 13 months
Length: 29.7 inches (76 cm), 50th percentile for age
Weight: 26.4 lbs (12 kg), 95th percentile for age
Weight/length: 98th percentile
Calories/kg: 80
Protein requirement: 1.6 grams, per kg
Ketogenic ratio: 3:1
Using the above numbers in the formula described earlier in this chapter, we calculate the diet order via the following steps (note: numbers are rounded to 0.1 grams.)
1. Calories: 80 (kcal/kg) × 12 (kg ideal weight) = 960 calories per day
2. Dietary unit: 980 (kcal) / 31(kcal/dietary unit) = 31.6 units per day
3. Fat allowance: 3 (as in 3:1) × 31.6 (dietary units) = 94.8 grams, fat
4. Protein: 1.6 (grams, per kg ideal weight) × 12 = 19.2 grams, protein
5. Carbohydrate: 31.6 (protein 1 carbohydrate) – 19.2 (protein) = 12.4 gram carbohydrate
Emily’s daily diet order follows. This will be divided into the number of meals or bottles she regularly gets in a 24-hour period.
Daily: Protein 19.2 grams, fat 94.8 grams, carbohydrate 12.4 grams, calories 960
Ketogenic diet for Emily using a modular formula:
1. Calculate the amount of RCF® needed to satisfy the child’s protein requirement by cross-multiplying.
Emily is 12 kg. Emily’s protein requirement is 1.6 grams per kilogram of desirable body weight, or 1.6 × 12 = 19.2 grams per day. 100 cc of RCF® formula contains 4.0 grams of protein. Emily will need 480 cc RCF® concentrate to meet her 19.2 grams protein requirement.
2. Calculate the fat in RCF® by cross-multiplying, and calculate enough Microlipid® to make up the difference.
100 ml RCF® contains 7.2 grams fat. Emily’s 480 cc of RCF® contains 34.5 grams. Subtract the 34.5 grams fat from the total 94.8 grams fat needed (94.8 – 34.5 = 60.3 grams). Remaining fat is 60.3 grams.
3. To calculate the Microlipid® needed to make up the remaining 60.3 grams fat in Emily’s diet, cross-multiply. There are 50 grams of fat in 100 ml Microlipid® = Emily will need 120.6 ml Microlipid®
4. Calculate an amount of Polycose® powder sufficient to meet Emily’s carbohydrate requirement.
5. The liquid allotment is set at 90 cc per kilogram, giving Emily 1100 cc liquid per day.
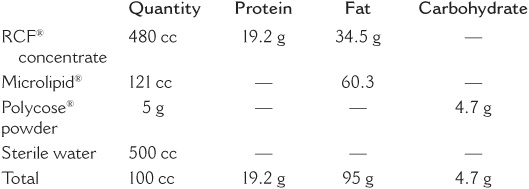
Emily’s RCF® and Microlipid® total 601 cc (480 cc RCF® + 121 cc Microlipid®). Her water allotment will therefore be 1100 – 601 = 499 cc. This will be rounded to 500 cc.
EMILY’S DAILY FORMULA
Note: In practice this meal would be rounded to the nearest gram for convenience in measuring.
1. Measure the RCF® concentrate and Microlipid® separately in a graduated cylinder.
2. Weigh the Polycose® powder on a gram scale and blend with above ingredients.
3. Add sterile water, reserving 10–15 cc per feeding to flush the tube. Shake or stir.
4. Divide into the number of equal feedings the child will receive in a 24-hour period and refrigerate, or refrigerate full amount and divide into individual portions at feeding time.
5. Bring to room temperature or warm slightly before feeding.
6. Remember to supplement this formula with vitamins and minerals.
Samuel is a 9-month-old male with infantile spasms. He is on Enfamil 20 calories per ounce, drinking about 4–5 ounces every 3–4 hours, including overnight bottle feeds. On average, per the parents’ report, Samuel is taking in 30 ounces per day. Samuel was admitted to start the ketogenic diet to reduce his spasms.
Weight: 8.1 kg (17.8 pounds) 5–10th percentile
Length: 70 cm (27.5 inches) 20th percentile
Weight/length: 25%
Samuel will be started on a 3:1 ratio and using KetoCal® 3:1. His average intake of calories was 600 per day, which provides him with 75 calories per kilogram. The dietitian makes the decision to continue with the same calorie amount.
To prepare this formula using KetoCal®:
Because Samuel is on a 3:1 ratio, we will use KetoCal® 3:1. There are 699 calories per 100 grams of KetoCal® 3:1. Because Samuel needs 600 calories, divide that number by 6.99.
86 gram of KetoCal® 3:1, 815 cc of water
Parents should continue giving Samuel 4–5 ounces every 3–4 hours. Once Samuel starts to gain some feeding abilities, we will work with speech therapy and feeding therapy on starting some baby food and oils.
Liquid feedings may be given orally or through a tube. They may be given by continuous feeds or as periodic bolus feedings. The tubes may be flushed with sterile water as needed. It may be beneficial to continue the exact same feeding regimen that the child was on prior to initiating the diet.
Children on liquid feedings who do not have a swallowing difficulty, such as growing babies, may be transitioned to soft foods by gradually substituting the equivalent soft foods for a portion of their bottle feedings.
The liquid ketogenic formula is relatively expensive. However, because the liquid ketogenic diet is considered a therapy rather than a food, a family can try and have their insurance or WIC cover the cost. There is a sample letter at the back of the book that can help you.