The significant problems we face cannot be solved at the same level of thinking we were at when we created them.
—Albert Einstein
Included among the Gram-positive pathogens are methicillin-resistant Staphylococcus aureus and S. epidermidis, vancomycin-resistant Enterococcus faecium and E. faecialis, and the rapidly growing mycobacteria. In the past five years, however, no fewer than four novel agents have been approved that have clinical activity versus these bacteria. It is really among the multidrug-resistant Gram-negative bacteria that we find growing unmet medical need, and only a single new agent has been approved in well over a decade.
—Steven Projan, Bacterial Resistance to Antimicrobials
Many people believe that there will always be antibiotics and that if the ones we have now aren’t working, others will be discovered that will work just as well, so no need to worry. The truth, unfortunately, is very different. There are virtually no new antibiotics in development, and there are unlikely to be. Pharmaceutical companies have almost completely given up the search for them. There are a number of reasons for this, the main one being, of course, financial.
In spite of cultural beliefs to the contrary, physicians can cure relatively few of the conditions that plague us. For high cholesterol they prescribe anticholesterol drugs, for arthritis anti-inflammatories, and so on. These drugs artificially alter the condition of the body, but they do not cure the underlying condition. In consequence, the drugs are often taken for decades; they are a never-ending source of money for the companies that make them. (And the profit of the top 12 pharmaceutical companies in the world in 2009? 100 billion dollars.)
Antibiotics, on the other hand, are too successful. They are used for a short period of time, the disease is eradicated, the patient cured. They are a victim of their own success. Brad Spellberg, author of Rising Plague, notes: “For many years now, leading members of the Infectious Diseases Society of America (IDSA) have been aware that antibiotics were no longer being developed by many pharmaceutical companies. Indeed, many pharmaceutical companies have actually completely eliminated their research and development programs for antibiotic drug discovery.”1 Stuart Levy, perhaps the foremost researcher on resistant organisms in the United States, comments that “the problem is the pharmaceutical industry has left the discovery field and so new antibiotics are not coming along.”2 He says, rather matter-of-factly, that it is just more profitable for the drug companies to develop medications for long-term conditions such as heart disease and arthritis than it is to find new antibiotics.
Research by Spellberg’s group found that between 1983 and 2008, investment in antibiotic research and development in the United States fell by 75 percent. His team found only five to seven new antibiotics in the pipeline, most expected to reach the market by 2012, and all of them just slightly altered versions of existing antibiotics.
And no, biotechnology companies are not doing any better. In 2004 all biotech companies combined had only one antibiotic in any kind of development stage. Worse, every one of the antibiotics expected to reach market by 2012 are for Gram-positive bacteria. There are none in any stage of development that can treat Gram-negative organisms, the fastest growing category of resistant pathogens. After 2012? That’s it. There are none in any stage of development and no plans for any, a fact that shocks most people. They just don’t believe that the drug companies would be so complacent—or that they would care so little. I mean, they are in the business of helping people … aren’t they?
There is a very old story—it’s about greed actually, and just a little bit about mathematics—of a king and the man who saved his life. The king was very grateful and told the man he would reward him with anything he wished. The man told the king that the only thing he wanted was some rice. He then asked the king if he played chess. The king replied that yes, he did. So the man said he would like to use the chess board to determine the amount of rice with which he would be rewarded. He wanted the king to put one grain of rice on the first square, then two on the second, four on the next, and so on. The king said sure, that sounds like a good idea, and he told his councilors to arrange it. They came back a bit later and very hesitantly told the king that they couldn’t do it. The king was pretty upset and asked why and was told that by the last square the man would receive more rice than existed in the entire kingdom. (I’m not sure, but I think the king beheaded the man who made the request—nobody likes a smart-ass.)
Bacterial resistance grows exponentially, just like those grains of rice. In practical terms that means we will be fine for a while (say from 1945 to 2010) because, as you can see, it takes a while to get into the big numbers. Welcome to big-number territory.
MRSA, once limited to the very young, the old, and the immunocompromised, has not only emerged in the general community; it is now exceptionally virulent and infecting the healthiest population of all—young adults. As Spellberg comments, “The highly publicized outbreaks of MRSA infections are dwarfed by the enormous number of cases that occur every day across the United States and throughout the world. Overall, healthy children, adolescents, and teenagers have been particularly heavily hit by MRSA infections, and these cases had gone unheralded until very recently.”3
Young people, completely healthy, begin to fall ill, enter emergency rooms, and are found to have out-of-control MRSA infections. After just a simple skin break, their arms swell with cellulitis, or the infection becomes systemic and infects the blood (bacteremia), the heart (endocarditis), spinal cord (myelitis), or bones (osteomyelitis). In 2007 the state of Virginia closed 21 high schools to try to stop an MRSA infection that had killed one student and sickened others.
The situation will only get worse. We are within 5 years of MRSA being completely untreatable by any antibiotics at all.
Thirty percent of all E. coli urinary tract infections are resistant to treatment, up from 5 percent 10 years ago. The resistance rate has increased 50-fold in the last decade. One of the more troubling resistance mechanisms in E. coli is what is called “extended-spectrum beta-lactamase” resistance, or ESBL. ESBL bacteria are highly virulent and strongly resistant to a class of antibiotics called beta-lactams, some of the most potent antibiotics still useful for Gram-negative bacteria. Beta-lactamase is an enzyme that the bacteria create and use to deactivate the antibiotics. All the bacteria in the Gram-negative family have begun acquiring that genetic resistance information. E. coli and Klebsiella are two of the forerunners.
ESBL resistance in E. coli in 1990 was only 3.6 percent, by 1993 it was 14.4 percent, by 1995 it was 25 percent in Europe and as high as 40 percent in France. The only antibiotic that until recently could still treat the ESBL-resistant strains of Klebsiella was carbapenem and a much older antibiotic, polymyxin, that is only partially effective and often causes severe kidney damage.
Fully resistant strains of Klebsiella have now (as of 2011) become common and are often, like MRSA, referred to by an acronym, CRKP. It stands for carbapenem-resistant Klebsiella pneumoniae. It is virtually untreatable; 40 percent of those infected with it die. “These are very serious infections, hugely complicated by the fact that the treatment options are severely limited,” is how Dr. Ajun Srinivasan of the Centers for Disease Control in Atlanta, Georgia, puts it. The first isolated reports of CRKP occurred in 1999 in New Jersey. As of 2010, Srinivasan says, “we are seeing reports of this organism from all over the country.”4
In March of 2010 a severe outbreak of CRKP occurred in Southern California (another occurred in March of 2011 in Los Angeles just as I was completing this manuscript). Brad Spellberg, speaking from the Los Angeles Biomedical Research Institute near Torrance, California, commented, “In the next decade there isn’t going to be anything that becomes available that’s going to be able to treat these bacteria…. [There] is no current treatment for CRKP bacteria, and there might not be any in the future either.”5
Neil Fishman, president of the Society for Healthcare Epidemiology of America, is more blunt: “We have lost our drug of last resort.”6
Pan-resistant Pseudomonas and Acinetobacter are similarly dangerous. Pseudomonas has also begun to develop resistance to carbapenem antibiotics; the bacteria are now reliably treatable only by polymyxin. Acinetobacter, E. coli, and Klebsiella have also been promiscuously sharing a new plasmid, NDM-1, that confers resistance along a wide range of antibiotics, including carbapenem. “In many ways, this is it,” says Timothy Walsh, a microbiologist and resistant bacteria specialist at Cardiff University in the UK. “There are no antibiotics in the pipeline that have activity against NDM-1-producing Enterobacteriaceae. We have a bleak window of maybe ten years.”7
Enterococcal organisms, once readily treatable, are so no longer. George Eliopoulos in the Division of Infectious Diseases at Beth Israel Deaconess Medical Center in Boston, Massachusetts, observes:
Ominously, in recent years, enterococci resistant to multiple antimicrobial agents have become increasingly prevalent in the hospital environment…. More than half of these enterococcal isolates were resistant to tetracycline, levofloxacin, and quinupristin-dalfopristin; 28 percent were resistant to ampicillin; and approximately 20 percent were nonsusceptible to vancomycin. From ICUs in the United States, even higher rates of vancomycin resistance have been reported…. Vancomycin resistance genes originating in enterococci have now been found in several clinical isolates of S. aureus. This validates concerns expressed more than a decade ago that VRE may serve as a reservoir of genes that could confer upon staphylococci resistance to glycopeptides, the principal antibiotics [remaining] for treatment of infections caused by methicillin-resistant strains [MRSA].8
There are no new antibiotics being developed to treat these resistant strains. The most recent, tigecycline, entered the market in 2005. It is active against resistant forms of Acinetobacter but not resistant Pseudomonas. Only tigecycline and that rather dangerous older antibiotic, polymyxin, can now treat Acinetobacter, and polymyxin itself has begun to encounter resistant forms of the bacteria. But then, so has tigecycline.
As Spellberg comments, “If we did not have tigecycline, these infections would be essentially untreatable.” But as he continues, “tigecycline resistance spread within two years of the drug’s availability. Indeed, on a recent trip to visit a hospital on the East Coast, I was told that nearly all the hospital’s Acinetobacter is already fully resistant to tigecycline.”9
People who now enter hospitals, even for very minor treatments, are at serious risk of contracting untreatable infections. Over 70 percent of all pathogenic bacteria in hospitals are at least minimally resistant; the ones discussed herein are considerably more so, being resistant to most major groups of antimicrobials. As oncology nurse Sue Fischer says, “These kids come in for a short treatment and the next day they complain about a pain in their side and the next day they’re gone. We open them up and find their whole body shot through with resistant bacteria that have attacked nearly every organ. Nothing works to stop it and it happens as quick as that.”10
The first edition of this book covered 12 resistant pathogens that researchers were concerned about. There are 21 on this new list and that doesn’t count the various subspecies in each genus that are now resistant (at least 40, not including variants) or several others that are lurking out there on the horizon. The problem, as many epidemiologists have warned, is increasing exponentially and there is no end in sight.
Some of these organisms, such as methicillin-resistant Staphylococcus aureus (MRSA), are already causing significant problems in hospitals and communities throughout the world. Others, such as Clostridium difficile, are becoming increasingly widespread and dangerous. And still others, such as Stenotrophomonas maltophilia, are just beginning their run as resistant organisms.
Most of the resistant pathogens are either Gram-positive or Gram-negative bacteria—a list is included under the respective headings that follow; there are, in addition, one parasitic protist (the malarial parasite), one mold (aspergillus), and one yeast (candida) that have now become dangerously resistant. The parasitic protist is Plasmodium falciparum, which causes malaria; the mold is Aspergillus spp. (A. fumigatus, A. flavus, A. terres); the yeast is Candida spp. (Candida albicans is dominant, but most species are now resistant).
Gram-positive and Gram-negative organisms are denoted as such because of their ability to take a Gram stain, one way of identifying them. Of much more importance are the differences in their cellular structure.
Just as we have skin, bacteria have an external membrane surrounding their bodies, a.k.a. the cell wall. Their interior is called the cytoplasm; then there is the cytoplasmic membrane, which covers the cytoplasm, then the cell wall. The cell wall consists primarily of a polymer called peptidoglycan. If the bacteria happen to be Gram-negative, they will have a second wall called the outer membrane. Between the two membranes in Gram-negative bacteria is a compartment, the periplasmic space. Gram-positive bacteria, because they lack that other membrane, have much thicker cell walls to protect them from outside events.
Because Gram-positive bacteria have only a single cell wall, even though it’s thicker, they are, in general, much easier to treat. With Gram-negative bacteria, two cell walls have to be penetrated, not just one. In essence, the bacteria have two chances to identify and deactivate an antibacterial that is hostile to them. Even if an antibiotic gets into the periplasmic space, it usually will not kill the bacteria. It still has to penetrate the second wall.
Gram-negative bacteria have a series of highly synergistic reactions to antibiotics, in essence using three primary mechanisms, all highly coordinated, to resist antibiotics. The first is the double cell wall. The second is a special group of enzymes, beta-lactamases, that are especially effective in deactivating beta-lactam antibiotics (the antibiotics most often used against them). The third is a variety of multidrug efflux pumps. These efflux pumps essentially act like sump pumps; they pump out the antibiotic substances just as fast as they come in so that the bacteria are unaffected by them.
Gram-positive bacteria rely on their thicker cell wall and very, very fast efflux pumps since they don’t have a periplasmic space in which to hold the antibiotics while they deal with them. Some Gram-positive bacteria, such as the staphylococci, have incorporated the use of beta-lactamases, which they learned about from Gram-negative organisms.
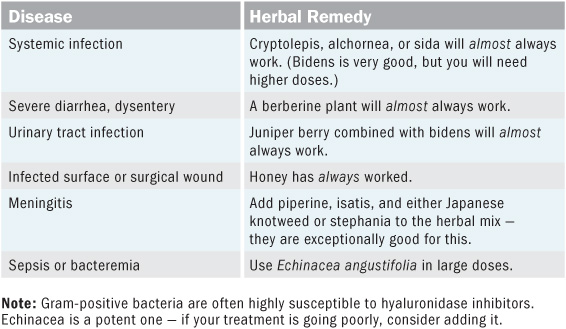
Here are some general thoughts to keep in mind when you are approaching treatment of a resistant pathogen. Always remember that you are dealing with virulent, highly pathogenic microbial infections—your treatment must be focused and continual and unremitting until the outcome is decided, one way or the other.
As a general rule of thumb, follow these recommendations when dealing with a resistant infection.
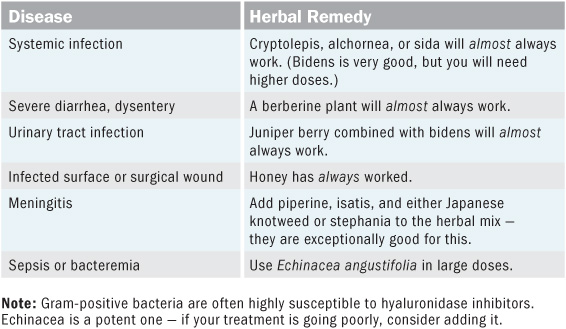
Endotoxins generally come from the outer wall of Gram-negative bacteria and are released into the body when the bacteria die. In a number of diseases, bubonic plague for example, it is not the bacteria that kill you but the endotoxins that are released when they die. If you are treating a systemic infection by a Gram-negative bacteria, the use of an endotoxin scavenger and protectant is often important. Isatis (though not discussed in this book) is perhaps the best herb for this (ginger is also good). It should be included if endotoxin release may be a problem.
If you are treating a difficult infection, especially if it is Gram-negative, use a synergist to enhance the treatment. There are two forms of synergists: the first is active against the efflux pumps in the bacteria, the second helps move the herbs across the intestinal membrane and strongly into the blood. Licorice is the best synergist for Gram-negative bacteria. Piperine will potently move herbal compounds across the intestinal membrane, significantly increasing their presence in the blood. See chapter 6 for more specifics.
Always work to increase the body’s natural immune function through the use of immune herbs or an immune formulation. These should be taken daily. The formulations suggested in this section were generated by looking at immune herbs that were also active against the specific organisms—kind of a two-for-one thing. Nevertheless, don’t get obsessed by these, as other immune herbs that don’t have any specific antibacterial activity will work, often better than these, in increasing immune function. These are only guidelines.
A note about the suggested formulations: The formulations that I have included to treat the various bacteria and the types of infections they cause are only suggestions. They can be varied considerably. Don’t get stuck in thinking that any of these formulations are the only way to go. Read the book and the monographs on the herbs themselves. Tremendous sophistication is possible. These are just guidelines.
Finally, don’t forget that human love and caring are an essential part of the healing process—they are medicines that you must also dispense to those you are working to heal. There is perhaps nothing that the ill need more than to know that they are supported in their suffering. It is very difficult to live without love, and nearly impossible to truly heal without it.
The rest of this chapter is concerned with the individual resistant bacteria, what herbs are effective in treating them, and then some actual specific suggestions for treatment. These are the main ones you need to know about to be able to take care of yourself and your family.
Subsequent chapters explore the individual herbs in depth; examine what other organisms they are active against; explore what else they can do medicinally; and then show how to grow, harvest, and prepare them as medicines so that you can take complete charge of your own health care if you wish to do so.
Chapter 7 contains in-depth explorations on the immune-enhancing herbs that you can use to keep your immune system strong—a number of which are also potently effective against resistant pathogens. And chapters 8 and 9 will tell you more than you ever wanted to know about making just about any kind of herbal medicine you might ever need.
The major resistant Gram-positive organisms are:
• Clostridium difficile
• Enterococcus spp. (E. faecalis, E. faecium)
• Mycobacterium tuberculosis
• Staphylococcus aureus
• Streptococcus spp. (S. pyogenes, S. pneumoniae)
Note: All the formulations given for treating each type of bacteria are meant to be taken simultaneously. Some offer immune support, some are directly antibacterial, some are for a specific symptom picture.
The Clostridium genus comprises about 100 different species of bacteria; four of them are human pathogens. They often form spores that, once they enter a cut or the GI tract, lead to a number of potentially dangerous diseases.
C. botulinum is the source of botulism poisoning in food (and of the drug Botox) and sometimes also causes infections in wounds; C. perfringens can cause anything from food poisoning to gas gangrene; and C. tetani is the cause of tetanus. C. difficile is the main resistant pathogen. The organism flourishes in people who have been on long antibiotic therapies, especially in hospitals, and because it is exposed to so many antibiotics, it is highly resistant to treatment. At the present most C. difficile infections are confined to hospitals, but their numbers are increasing exponentially. The disease causes severe diarrhea and inflammation of the colon and sometimes death.
The primary herbs to use to treat the condition, listed in order of strength against the organism, are the berberine plants, cryptolepis, isatis, usnea, lomatium, licorice, and echinacea. Because juniper berry is active against C. perfringens, I would suggest its use for C. difficile as well.
Formulation 1 (antibacterial) Cryptolepis or any berberine plant tincture: 1 tsp–1 tbl, 3–6x daily, depending on severity of symptoms
Formulation 2 (immune support) Echinacea, ginger, and licorice (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 (antidiarrheal/colon soothing) Blackberry root and marsh mallow root (equal parts) standard infusion: up to 6 cups daily (Note: Elm bark porridge will also help ease colon inflammation tremendously.)
This genus was considered to be part of the streptococcus genus until it was reclassified in the 1980s. Although both E. casseliflavus and E. raffinosus may sometimes cause human infections, the major problematical species are E. faecalis and E. faecium. These enterococcal organisms are often highly resistant to antibiotics, especially in hospitals. They don’t respond very well to beta-lactam antibiotics (penicillins and cephalosporins), aminoglycosides, and, increasingly, vancomycin.
Enterococcal organisms cause urinary tract infections, bacteremia, bacterial endocarditis, diverticulitis, and meningitis. The primary herbs to treat them are sida, alchornea, cryptolepis, bidens, ginger, echinacea, juniper berry, usnea, Artemisia annua, honey (I know, it’s not exactly an herb), licorice, oregano oil, and Acacia aroma. If you are treating a really tough vancomycin-resistant enterococcal infection, add ginger juice to your formulation; it strongly inhibits resistance mechanisms in these bacteria.
Formulation 1 (antibacterial) Sida, alchornea, or cryptolepis tincture: 1 tsp–1 tbl, 3–6x daily, depending on severity of symptoms (Note: Bidens tincture will work but requires higher doses and must be prepared properly; see monograph, page 127.)
Formulation 2 (immune support) Licorice, astragalus, and rhodiola (equal parts) tincture: 1 tsp, 3x daily (Note: Echinacea tincture will also be of benefit for immune support.)
For systemic enterococcal infections, diverticulitis, and endocarditis: Formulations 1 and 2
For enterococcal UTI: Formulation 1 plus juniper berry–bidens tincture (1 part juniper, 2 parts bidens), 30 drops, 3–6x daily, depending on severity
For enterococcal bacteremia: Formulation 1 plus Echinacea angustifolia tincture, ½ tsp–1 tbl in minimal water, every half hour to hour
For enterococcal meningitis: Formulations 1 and 2, plus formulations 3 and 4 below
Formulation 3 Piperine: 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M.
Formulation 4 Isatis leaf (or root) and either Japanese knotweed or stephania (equal parts) tincture: 1 tsp, 3–6x daily
This is the primary cause of tuberculosis (TB), which has become increasingly resistant and difficult to treat. There are, however, some 130 species of mycobacteria, a number of which can cause human disease. The members of this genus are a bit different than other Gram-positive bacteria. They don’t stain well, but they also don’t possess the double membrane structure of the Gram-negative bacteria. Their membrane is waxy and thicker than that of other Gram-positive bacteria, making them tougher overall. Of the 130 or so species, there are eight that can cause TB. M. leprae causes leprosy and the M. avium complex often causes pulmonary infections in AIDS patients and has been implicated in Crohn’s disease.
Mycobacterium tuberculosis has been developing increasing resistance for decades. MDR-TB (multidrug-resistant TB) is resistant to the two main first-line drugs used to treat it, isoniazid and rifampicin. Some 450,000 people contract this disease each year. XDR-TB (extensively drug-resistant TB) is resistant to all of the most effective anti-TB drugs. About 45,000 people a year contract this form of the disease; the death rate is about 90 percent.
The herbs effective for treating resistant and nonresistant TB are cryptolepis, sida, bidens, piperine, Artemisia annua, berberine plants, juniper, usnea, lomatium, licorice, echinacea, and rhodiola.
Formulation 1 (systemic antibiotic) Cryptolepis and sida (equal parts) tincture: 1 tsp–1 tbl, 3–6x daily, depending on symptoms
Formulation 2 Piperine: 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M.
Formulation 3 (immune support) Lomatium, licorice, and rhodiola (equal parts) tincture: 1 tsp, 3x daily
Methicillin-resistant Staphylococcus aureus (MRSA) has become an increasingly common infectious disease. It is now present in both hospitals and the general community and is passing between people, wherever they congregate, with great abandon. Individuals with compromised immune function, even if they appear healthy, are at greater risk of serious infections. There are numerous strains of the bacteria, some more resistant than others. In many respects MRSA should mean “multidrug-resistant,” not merely “methicillin resistant.”
Most MRSA infections in the general community initially present as small red bumps that are similar to pimples or perhaps spider bites or small boils. There may be fever or even a rash. As the disease progresses, the bumps become larger and very painful, eventually breaking open into deep, pus-filled boils. In those in whom antibiotic treatment fails, the boils continue to spread and the infection goes deeper, sometimes necessitating amputation of affected limbs.
In hospitals MRSA can infect open wounds, intravenous catheters, the urinary tract, and the lungs; the infection can be quite dangerous, spreading throughout the whole system. Unchecked, it can infect the valves of the heart, the bones and joints, the organs, and the blood (bacteremia or sepsis) and cause toxic shock syndrome and necrotizing (flesh-eating) pneumonia. Many people worldwide die from it each year.
The main herbs to treat MRSA are cryptolepis, sida, alchornea, bidens, black pepper, the berberines, usnea, juniper berry, isatis, licorice, ginger, ashwagandha, echinacea, red root, reishi, honey, and Artemisia annua.
Formulation 1 (internal systemic antibacterial) Cryptolepis tincture: 1 tsp–1 tbl, 3–6x daily, depending on severity
Formulation 2 (immune support) Ginger, reishi, and licorice (2 parts ginger, 2 parts reishi, 1 part licorice) tincture: 1 tsp, 3x daily
For MRSA UTIs: Formulations 1 and 2 plus juniper berry–bidens tincture (1 part juniper, 2 parts bidens), 30 drops, 3–6x daily
The main species of streptococcal bacteria that cause disease in human beings are S. pyogenes, which causes strep throat, acute bacterial glomerulonephritis, and necrotizing (flesh-eating) fasciitis; S. pneumoniae, which causes bacterial pneumonia, otitis media, sinusitis, meningitis, and peritonitis; and S. agalactiae, which causes pneumonia, meningitis, bacteremia, intestinal infections, and infections of the female reproductive tract. Of these, the first two are the most common causes of infections in people.
The primary herbs used to treat streptococcal bacteria are cryptolepis, sida, alchornea, bidens (though you’ll need to use larger doses, for longer), the berberine plants, juniper, usnea, lomatium, honey, echinacea, licorice, ginger, and red root.
Formulation 1 (antibacterial) Echinacea angustifolia tincture: 1 tbl in minimal water, every hour
Formulation 2 Cryptolepis, sida, or alchornea tincture: 1 tbl, every hour
Formulation 3 Lomatium, rhodiola, and eleuthero (equal parts) tincture: 1 tsp, 4x daily
For streptococcal glomerulonephritis: Formulations 1, 2, and 3, plus juniper berry tincture, 10 drops, up to 6x daily
For streptococcal bacteremia, necrotizing fasciitis, pneumonia, peritonitis, and infections of the female reproductive tract: Formulations 1, 2, and 3
For strep throat: ½ tsp Echinacea angustifolia tincture, undiluted, held in the mouth until saliva is well stimulated, then allowed to dribble slowly down throat, over the affected areas; repeat every hour
For streptococcal necrotizing fasciitis (topical): Honey is best (see monograph, page 188). If it’s not available, combine equal parts Echinacea angustifolia root powder, berberine plant powder, juniper berry powder, and lomatium root powder; mix well, apply as poultice, replace every 2 hours.
For streptococcal intestinal infection: Tincture of equal parts berberine plant, cryptolepis, and lomatium, 1 tsp–1 tbl, 3–6x daily, depending on severity of infection
For streptococcal meningitis: Treat as you would enterococcal meningitis (see page 50).
One of the most important things to remember in treating Gram-negative infections is that the use of a synergist will significantly increase the impact of the herbs on the bacteria. For instance, when treating diseases caused by Shigella spp., Serratia marcescens, Salmonella spp., Klebsiella spp., Enterobacter spp., or E. coli, add licorice to the mix. It strongly inhibits several of the main efflux pumps in this family of bacteria (AcrAB-TolC). You can use piperine when dealing with a non–gastrointestinal tract infection, but this is important: Don’t use it with a GI tract infection such as E. coli or cholera. Piperine allows more of the herbs to pass through the GI tract, increasing the presence of their antibacterial compounds in the body.
The Gram-negative organisms are:
• Acinetobacter baumannii
• Campylobacter jejuni
• Enterohemorrhagic E. coli (E. coli O157, E. coli O157:HM, E. coli O157:H7)
• Haemophilus influenzae
• Klebsiella pneumoniae
• Neisseria gonorrhoeae
• Proteus spp. (P. vulgaris, P. mirabilis)
• Pseudomonas aeruginosa
• Salmonella spp. (S. typhi, S. enteritidis, S. typhimurium)
• Serratia marcescens
• Shigella spp. (S. dysentariae, S. flexneri, S. sonnei)
• Stenotrophomonas maltophilia
• Vibrio cholerae
Of the many species in this genus that can infect humans, Acinetobacter baumanii, the most common, is multidrug resistant; its name is often abbreviated as MDRAB. As of this writing it has become resistant to nearly all the antibiotics that can affect it. The only drugs still useful for fully resistant MDRAB are the older polymyxins that have not been in use for decades due to their toxicity—tigecycline has been the most recent drug of choice but Acinetobacter’s resistance to it is increasing rapidly. In some hospitals it won’t work at all. It is inevitable that as they are used more regularly to treat the bacteria, the polymyxins will also become ineffective.
Acinetobacter spp. are highly responsive to the exchange of DNA strands with other bacteria that contain both resistance and virulence factors. Many of the soldiers wounded in combat overseas tend to return with active MDRAB infections that then spread across hospitals. The bacteria enter the body through wounds, breathing tubes, catheters, injection sites, anything that breaks the surface and allows foreign pathogens in. They are generally spread by health-care workers and are especially troublesome because they can live on hospital surfaces (and the hospital staff’s hands) for up to 5 months.
Most hospital infections from these bacteria, aside from those due to combat, come from the insertion of contaminated breathing tubes during hospital procedures; 82 percent of these patients develop severe pneumonia and die as a result. Catheter insertion can cause severe infections of the urinary tract. Injections, blood draws, intravenous lines, surgical drains, and open wounds invite infection of the bloodstream, a.k.a. bacteremia.
These bacteria like to live in aquatic conditions and are often found in the irrigating and intravenous solutions used by the physicians; they love the lungs. They may enter the peritoneal fluid during peritoneal dialysis and can also find their way into the cerebral spinal fluid under some circumstances.
The herbs active against Acinetobacter are alchornea, cryptolepis, sida, juniper, isatis, ginger, lomatium, honey, oregano essential oil, epigallocatechin, Acacia aroma, Zuccagnia punctata, and Sechium edule fluid extract.
Note: Ginger juice taken internally is especially effective in reducing the resistance of Acinetobacter organisms. It is crucial to use if the infection is serious and has not responded to antibiotics.
Formulation 1 (antibacterial) Cryptolepis, alchornea, or sida tincture: 1 tsp–1 tbl, 3–6x daily, depending on severity of symptoms
Formulation 2 Lomatium, astragalus, and rhodiola (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 (important) Fresh ginger juice, stabilized with 20 percent alcohol (see page 227): 1 tbl in hot water, 6x daily
Formulation 4 Oregano or juniper essential oil inhalation as aromatherapy: 3x daily
For Acinetobacter pneumonia: Formulations 1, 2, 3, and 4
For Acinetobacter surgical wound infections: Formulations 1 and 2, plus daily topical honey dressings (see monograph, page 188)
For Acinetobacter UTIs: Formulations 2 and 3, plus juniper berry–bidens tincture (1 part juniper, 2 parts bidens), 30 drops, 6x daily (or oregano essential oil, 3 drops in water, 3x daily)
For Acinetobacter septicemia: Formulations 1, 2, and 3, plus Echinacea angustifolia tincture, ½ tsp–1 tbl, every half hour to hour
Campylobacter infections generally cause enteritis accompanied by abdominal pain, diarrhea, fever, and malaise. They are not usually fatal but can be debilitating. The organism is increasingly resistant to antibiotics.
The herbs for campylobacter are cryptolepis (strongly), sida, ginger, and the berberines.
Formulation 1 (antibacterial) Cryptolepis or sida tincture: 1 tsp, 3x daily
Formulation 2 Any strong tannin-containing plant (oak, geranium, krameria, pine needles) as a decoction: 6 ounces, up to 6x daily
There are, roughly, three kinds of E. coli to be aware of. The first is the enterohemorrhagic E. coli strains (E. coli O157, E. coli O157:HM, and so on). The second is the kind that cause urinary tract infections, especially ST131. And finally, there are the E. coli B2 strains that cause what are called extraintestinal infections.
Of the current strains of enterohemorrhagic E. coli, O157 is the best known. All of them create similar conditions after infection; that is, hemorrhagic diarrhea and occasionally kidney failure. The infection is generally foodborne, most frequently arising from contaminated ground beef. It can also be contracted by drinking contaminated water or juices, eating contaminated vegetables, or swimming in contaminated pools.
The early signs are abdominal cramps, then acute diarrhea, often hemorrhagic. In some cases the red blood cells in the body are destroyed and the kidneys fail. Death is most common in the very young and the elderly.
A number of E. coli strains, both O157 and non-O157 strains, produce a shiga toxin (very similar to those made by Shigella species—all named after Kiyoshi Shiga, who discovered the shigella bacteria in the late nineteenth century). The toxins cause hemolytic-uremic syndrome; hemolytic anemia, acute renal failure, and low platelet counts all occur. Sida is essential to use if there is anemia/red blood cell damage.
The E. coli strains that cause UTIs have been fairly easy to treat, but a new strain of E. coli, ST131, emerged in 2008 and has begun to spread widely. It is strongly resistant and extremely virulent. The strain is, at this writing, only one resistance gene short of being untreatable. Unlike O157, ST131 causes urinary tract infections, generally in hospital settings, that sometimes lead to death.
The B2 group causes extraintestinal infections in the body, things like sepsis, meningitis, bacteremic pneumonia, peritonitis, and ascending cholangitis.
The first two strains are relatively easy to treat, but severe extraintestinal infections call for much more focus and care.
The herbs that are effective for E. coli are the berberines, cryptolepis, sida, alchornea, bidens, nearly all artemisias, juniper, honey, usnea, lomatium, isatis, licorice, ginger, ashwagandha, and reishi. All oak species (Quercus) and pomegranate (Punica granatum) fruit rind or tree bark are also highly effective against the E. coli O157:H7 strains. They are highly bacteriostatic and bactericidal and are very effective in killing the organisms and correcting the diarrhea. If you can’t find any of the other plants I’ve listed, use oak bark; oak species grow nearly everywhere.
Formulation 1 (antibacterial) Berberine plant tincture: 1 tsp–1 tbl, 3–6x daily, depending on severity
Formulation 2 Blackberry root or oak bark decoction: 3 tbl–½ cup, 2–4x daily (Note: If the intestines are highly inflamed and sore, add powdered elm bark gruel.)
For enterohemorrhagic E. coli with red blood cell damage: Formulations 1 and 2 plus sida tincture, 1 tsp, 6x daily, along with ginger, licorice, and reishi (equal parts) tincture, 1 tsp, 3x daily
Formulation 1 (antibacterial) Juniper berry–bidens tincture (1 part juniper, 2 parts bidens): 30 drops, 3–6x daily
Formulation 2 Cryptolepis and either sida or (if you can’t get sida) berberine plant (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 Ginger, licorice, and reishi (equal parts) tincture: 1 tsp, 3x daily
Formulation 1 (antibacterial) Cryptolepis and sida (equal parts; sida is important here) tincture: 1 tbl, 2–4x daily
Formulation 2 Echinacea angustifolia tincture: ½ tsp–1 tbl, every half hour to hour
Formulation 3 Ginger, licorice, and reishi (equal parts) tincture: 1 tsp, 3x daily
For E. coli B2 with sepsis: Formulations 1, 2, and 3
For E. coli B2 with meningitis: Treat as you would enterococcal meningitis (see page 50).
For E. coli B2 with bacteremic pneumonia: Formulations 1, 2, and 3, plus eucalyptus or juniper berry essential oil inhalation as aromatherapy, 4–6x daily
For E. coli B2 with peritonitis: Formulations 1, 2, and 3
For E. coli B2 with ascending cholangitis: Formulations 1, 2, and 3
Four species in this genus are the main sources of Haemophilus infection in people, the primary one being Haemophilus influenzae, in specific H. influenzae type B. Widespread vaccination in the United States and Europe began in 1988 and rates of infection from this particular organism have since fallen, though it is still common in the rest of the world.
The four species that cause infections in people are H. influenzae, H. parainfluenzae, H. aphrophilus, and H. ducreyi. H. influenzae has a number of types that cause disease: the encapsulated types, identified as A through F (B being the most problematical), and the unencapsulated, non-typeable strains.
The encapsulated strains, especially type B, cause invasive infections: pneumonia, meningitis, epiglottitis, septic arthritis, osteomyelitis, facial cellulitis, and bacteremia, generally in children, generally under 5 years of age. Pneumonia and meningitis are the most common. These forms of infection are generally spread by inhalation of infectious respiratory droplets—in other words, someone coughs, someone else breathes in.
The unencapsulated strains generally cause otitis media (ear infections) in children and lower respiratory tract infections in both children and immunocompromised adults—often those with existing lung diseases such as cystic fibrosis. They can also cause acute sinusitis and acute exacerbations of chronic bronchitis. A unique form, H. influenzae biogroup aegyptius, causes purulent conjunctivitis and sepsis in children, usually 1 to 4 years of age, following conjunctivitis infection.
H. parainfluenzae typically has low virulence but does occasionally cause endocarditis and bacteremia. However, it carries resistance genes that help increase resistance in other members of this genus. H. aphrophilus, uncommonly, causes endocarditis and brain abscesses. H. ducreyi causes chancroid, a sexually transmitted disease accompanied by shallow and painful genital ulcers and inguinal lymphadenitis (buboes).
Haemophilus organisms are common in most people. They usually become a problem only when a person becomes immunocompromised. However, the genus is growing increasingly resistant to antibiotics; it appears that while type B is becoming less of a problem due to vaccination programs, the other types are growing more problematical. Resistant respiratory infections are more common every year and the organisms, once more invasive of children, have now shifted to infecting adults in nearly equal numbers.
An additional concern is that influenza viruses are highly synergistic with Haemophilus. Dual infection is considerably more dangerous than with either alone. There is some evidence that the 1918 influenza epidemic involved a highly activated synergy with Haemophilus; even immunocompetent individuals become highly susceptible to the bacteria when the two activate together. This synergistic capacity seems inherent in Haemophilus; other studies have found the same kind of synergy between it and other respiratory pathogens such as Moraxella catarrhalis, respiratory syncytial virus, human parainfluenza virus 3, and rhinovirus.
Importantly, Haemophilus are what are called fastidious bacteria, meaning they need an iron source to grow, and unlike most other bacteria, they usually get it from the hemoglobin in our blood to which iron is bonded (giving blood its red color). Protecting the blood cells through the use of something like sida is crucial in treating this kind of infection.
The herbs that have been found active against Haemophilus are ginger, licorice, isatis, lomatium, honey, eucalyptus essential oil, eucalyptus leaf, and basil essential oil. Unfortunately, cryptolepis, sida, and alchornea have not been tested against this organism. However, I believe that, due to their activity against similar Gram-negative bacteria, they are usable for Haemophilus infections, especially sida, given its strong protective effects on red blood cells. I would use them myself without hesitation.
Formulation 1 (antibacterial) Sida tincture: 1 tsp, 3–6x daily
Formulation 2 Isatis, ginger, licorice, and red root (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 Fresh ginger juice tea (see page 228): 4–6x daily
For Haemophilus pneumonia: Formulations 1, 2, and 3
For Haemophilus epiglottitis and facial cellulitis: Formulations 1, 2, and 3
For Haemophilus chancroid: Formulations 1, 2, and 3. Add a topical wash of an infusion of eucalyptus and lomatium and honey 4x daily. If ulcers are severe, apply honey dressings after using the topical wash.
For Haemophilus meningitis: Formulations 1 and 2, along with piperine, 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M. Also add isatis leaf (or root) and either Japanese knotweed or stephania (equal parts) tincture, 1 tsp, 3–6x daily. Echinacea will also be of benefit, as for bacteremia.
For Haemophilus bacteremia and osteomyelitis: Formulations 1, 2, and 3, along with Echinacea angustifolia tincture, ½ tsp–1 tbl, every half hour to hour
For Haemophilus septic arthritis: Formulations 1, 2, and 3, along with E. angustifolia and teasel root (equal parts) tincture, ½ tsp, 3x daily
For Haemophilus otitis media: Use Formulations 2 and 3 plus oil ear drops as follows: Make an oil infusion with lomatium. When done as per recipe, add 10 drops eucalyptus essential oil and 10 drops basil essential oil. Place 2–3 drops in ear 2x daily.
For Haemophilus purulent conjunctivitis: Use isatis or isatis-honey eyedrops.
The main species that causes human infection is K. pneumoniae, but K. oxytoca and K. rhinoscleromatis occasionally do, too. Most infections occur in the lungs, but they also can occur in the urinary tract, the biliary tract, the lower respiratory tract, and surgical wounds. The organism can cause pneumonia, bacteremia, urinary tract infections, diarrhea, cholecystitis, osteomyelitis, meningitis, thrombophlebitis, and respiratory infections. Generally, infections are caused by hospital staff from bacteria on their hands or bacterial colonization of invasive apparatus, and sometimes patients’ GI tracts are contaminated.
When Klebsiella infect the lung tissue, necrosis, inflammation, and hemorrhage often occur, giving rise to a thick, bloody mucus; it looks something like currant jelly (so they say).
Klebsiella organisms are often multidrug resistant, producing extended-spectrum beta-lactamases (ESBL). These strains are highly virulent and spread promiscuously. The mortality rate is around 50 percent, irrespective of antibiotic use. They are one of the fastest-growing resistant infections in U.S. hospitals and are common throughout the world. The newest resistant form is referred to as CRKP (carbapenem-resistant Klebsiella pneumoniae). Very dangerous.
The herbs useful for Klebsiella are cryptolepis, alchornea, bidens, black pepper, juniper, the berberine plants, Acacia, Artemisia annua, reishi, licorice, and honey.
Formulation 1 (antibacterial) Cryptolepis and alchornea (equal parts) tincture: 1 tsp–1 tbl, 6x daily
Formulation 2 (to thin mucus) Ginger juice tea (page 228): 4–6x daily
Formulation 3 (immune support) Reishi, red root, licorice, and Echinacea angustifolia (equal parts) tincture: 1 tsp, 6x daily
Formulation 4 Juniper essential oil inhalation as aromatherapy: 4–6x daily
For Klebsiella pneumonia and respiratory infections: Formulations 1, 2, 3, and 4
For Klebsiella osteomyelitis: Formulations 1, 2, and 4, plus Echinacea angustifolia tincture, ½ tsp–1 tbl, every half hour to hour
For Klebsiella meningitis: Treat as you would enterococcal meningitis (see page 50).
For Klebsiella surgical wound infections: Formulations 1, 2, and 4, plus daily topical honey dressings (see monograph, page 188)
For Klebsiella bacteremia: Instead of the formulations above, use Echinacea angustifolia tincture, ½ tsp–1 tbl, every half hour to hour; cryptolepis tincture, 1 tbl, 6x daily; and piperine, 20 mg, 2x daily (the first dose in the morning 30 minutes before taking the other formulations and the second dose at 4 P.M.).
For Klebsiella UTIs: Instead of the formulations above, use juniper berry–bidens tincture (1 part juniper, 2 parts bidens), 30 drops, 3–6x daily; and cryptolepis–berberine plant tincture (equal parts), 1 tsp, 3x daily.
For Klebsiella diarrhea: Instead of the formulations above, use a berberine plant tincture, 1 tsp, 3–6x daily.
This organism causes gonorrhea, which is sexually transmitted. The main herbs effective for it are cryptolepis and sida.
Formulation Cryptolepis and sida (equal parts) tincture: 1 tsp, 3x daily for 14 days
The two most troublesome Proteus species are P. vulgaris and P. mirabilis. Both are resistant. P. mirabilis generates 90 percent of Proteus infections in people. Proteus infections can cause alkaline kidney stones, but more seriously, when contracted in hospitals they can cause wound infections, urinary tract infections, septicemia, and pneumonia.
The herbs that are effective for proteus are cryptolepis, sida, alchornea, Artemisia annua, juniper, usnea, Acacia aroma, lomatium, ginger, and honey.
Formulation 1 (antibacterial) Juniper berry and bidens tincture (1 part juniper, 2 parts bidens): 30 drops, 3–6x daily
Formulation 2 Cryptolepis, sida, or alchornea tincture: 1 tsp, 3–6x daily
Formulation 3 Ginger, rhodiola, and red root (equal parts) tincture: 1 tsp, 3x daily
Formulation 4 Piperine: 20 mg, 2x daily (the first dose in the morning 30 minutes before taking the other formulations and the second dose at 4 P.M.)
Formulation 1 (antibacterial) Cryptolepis, sida, or alchornea tincture: 1 tsp, 6x daily
Formulation 2 (to prevent septic shock) Isatis tincture: 1 tbl, 3–6x daily
Formulation 3 Echinacea angustifolia tincture: ½ tsp–1 tbl, every half hour to hour
Formulation 4 Lomatium, rhodiola, and red root (equal parts) tincture: 1 tsp, 3x daily
Formulation 1 (antibacterial) Cryptolepis, alchornea, and sida (equal parts) tincture: 1 tsp, 6x daily
Formulation 2 Lomatium, rhodiola, and red root (equal parts) tincture: 1 tsp, 3–6x daily
Formulation 3 Daily topical honey dressings (see monograph, page 188)
Formulation 1 (antibacterial) Cryptolepis, alchornea, and sida (equal parts) tincture: 1 tsp, 6x daily
Formulation 2 Ginger juice tea (page 228)
Formulation 3 (immune support) Lomatium, licorice, red root, and Echinacea angustifolia (equal parts) tincture: 1 tsp, 6x daily
Formulation 4 Juniper essential oil inhalation as aromatherapy: 3x daily
This species is another opportunistic pathogen that takes advantage of hospital settings. It can live, even thrive, on most surfaces and is common on most medical equipment, including catheters, on which it often enters the human body. It can grow in diesel and jet fuel and survive temperatures up to 108°F, so fevers don’t affect it much. It can live in oxygen, partial oxygen, or no oxygen. It can even live in distilled water in which virtually no nutrients exist. It’s tough and very, very resistant to antibiotics.
Pseudomonas can infect nearly any part of the body; all it needs is an opening (which hospitals often give it). It causes pneumonia, septic shock, urinary tract infections, otitis media, gastrointestinal infections, and skin and soft tissue infections. The most common infections are from burns, surgical wounds, urinary tract infections, and otitis media. Low phosphate levels in the human body are highly stimulatory of its growth.
The primary herbs useful for treating Pseudomonas aeruginosa are isatis, alchornea, bidens, cryptolepis, sida, black pepper, Artemisia annua, the berberines, juniper, ginger, Acacia aroma, honey, lomatium, ashwagandha, echinacea, and reishi.
Formulation 1 (antibacterial) Cryptolepis and alchornea (equal parts) tincture: 1 tsp–1 tbl, up to 6x daily
Formulation 2 Ginger juice tea (page 228)
Formulation 3 (immune support) Ginger, isatis, red root, and Echinacea angustifolia (equal parts) tincture: 1 tsp, 6x daily
Formulation 4 Juniper essential oil inhalation as aromatherapy: 3x daily
Formulation 1 (antibacterial) Cryptolepis and alchornea (equal parts) tincture: 1 tbl, 6x daily
Formulation 2 (immune support) Ginger, isatis, and red root (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 Echinacea angustifolia tincture: ½ tsp–1 tbl, every half hour to hour
Note: To reduce septic shock from endotoxin release, isatis tincture can be used in much larger doses: 1 tbl, up to 6x daily.
Formulation 1 (antibacterial) Cryptolepis and a berberine plant (equal parts) tincture: 1 tsp–1 tbl, 3–6x daily depending on severity
Formulation 2 Ginger, red root, and Echinacea angustifolia (equal parts) tincture: 1 tsp, 6x daily
Formulation 1 (antibacterial) Juniper berry and bidens (1 part juniper, 2 parts bidens) tincture: 30 drops, 3x daily
Formulation 2 Berberine plant tincture: 1 tsp, 3x daily
Formulation 3 Ginger, licorice, and red root (equal parts) tincture: 1 tsp, 3x daily
Formulation 1 (antibacterial) Piperine: 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M.
Formulation 2 Cryptolepis and alchornea (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 (immune support) Ginger, licorice, and red root (equal parts) tincture: 1 tsp, 6x daily
Formulation 4 Daily topical honey dressings (see monograph, page 188)
Formulation Ear formulation with lomatium, honey, berberine plant, or cryptolepis or use ear infection glycerite (page 345) with the addition of lomatium: 1–3 drops topically, up to 6x daily
Closely related to both shigella and E. coli, salmonella organisms cause typhoid fever (S. typhi), paratyphoid fever (S. paratyphi), and salmonellosis, a.k.a. food poisoning. Most infections come from contaminated foods.
Salmonella can survive outside a host for years—active organisms have been identified in dried two-and-a-half-year-old feces. They are not destroyed by freezing and have to be heated to at least 130°F for 1 hour to kill them (or 10 minutes at 170°F). Poultry, pork, cattle, and many fruits and vegetables are now commonly infected with the bacteria. About 150,000 people in the United States sicken from eating infected chicken eggs each year.
The bacteria inhibit the innate immune system as they penetrate the body to better enable their survival. General symptoms are diarrhea, vomiting, fever, severe abdominal cramps. Sepsis and infection of other organs can occur in severe cases.
The organisms, due to heavy antibiotic use in both plant and animal agriculture, have developed multidrug resistance and are becoming much more difficult to treat.
The primary herbs effective for salmonella are cryptolepis, sida, alchornea, bidens, the berberines, juniper, honey, licorice, lomatium, and ginger.
Formulation 1 (antibacterial) Cryptolepis, sida, or alchornea tincture: 1 tsp–1 tbl, 3–6x daily depending on the severity of the infection
Formulation 2 Berberine plant tincture: 1 tsp–1 tbl, 3–6x daily, depending on symptom picture
Formulation 3 (immune support) Licorice tincture, rhodiola tincture, and ginger juice (equal parts) combined: 1 tsp, 3x daily
Note: Juniper-evergreen and sida teas are especially useful for treating salmonella.
For salmonella with sepsis: Formulations 1, 2, and 3, and add Echinacea angustifolia tincture, ½ tsp–1 tbl, each half hour to hour.
This is primarily a hospital-acquired infection. The bacteria can colonize the urinary tract (causing UTIs, from catheters), surgical wounds, the blood (bacteremia), the eye (conjunctivitis), the respiratory tract (pneumonia), the CNS (meningitis), the bones (osteomyelitis), and the heart (endocarditis). It is becoming highly resistant.
The primary herbs active against the organism are juniper, bidens, licorice, lomatium, Coptis chinensis, honey, oregano oil, Tribulus terrestris, and Emblica officinalis. The following plants are also active: Trichosanthes cucumerina, Cassia didymobotrya, Blumea lacera, Moringa oleifera, Isodon spp., Dendrophthoe falcata, Zuccagnia punctata, and Phrygilanthus acutifolius.
Note: For all Serratia infections, use piperine, 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M.
Formulation 1 (antibacterial) Juniper berry and bidens (1 part juniper, 2 parts bidens) tincture: 30 drops, 6x daily for 10 days
Formulation 2 Bidens fresh plant juice or tincture; or Coptis chinensis tincture; or Tribulus terrestris tincture; or a combination of the three (equal parts): ½ tsp, 3x daily
Formulation 3 (immune support) Ginger, licorice, and rhodiola (equal parts) tincture: ½ tsp, 3x daily
Formulations 2 and 3 for Serratia UTI infections (above), plus topical honey dressings daily (see monograph, page 188)
Formulation 1 (antibacterial) Bidens fresh juice: 1–3 drops applied to the eye, up to 6x daily
Formulation 2 (immune support) Lomatium, licorice, and ginger (equal parts) tincture: ½ tsp, 3x daily
Formulation 1 (antibacterial) Echinacea angustifolia tincture: ½ tsp–1 tbl, every half hour
Formulation 2 (immune support) Lomatium, licorice, and ginger (equal parts) tincture: 1 tsp, 3x daily
Formulation 3 Bidens fresh juice or plant tincture: 1 tbl, 6x daily
Formulation 1 (antibacterial) Bidens fresh plant juice or tincture: 1 tsp, 6x daily
Formulation 2 (immune support) Lomatium, ginger, licorice, and red root (equal parts) tincture: 1 tsp, 6x daily
Formulation 3 Juniper or oregano essential oil inhalation as aromatherapy: 3x daily
Formulations 1 and 2 for Serratia pneumonia (above), plus topical honey dressings daily (see monograph, page 188)
Formulations 1 and 2 for Serratia pneumonia (above), plus formulation 3 below:
Formulation 3 Isatis leaf (or root) and either Japanese knotweed or stephania (equal parts) tincture: 1 tsp, 3–6x daily
Note: Echinacea will also be of benefit, as for Serratia bacteremia.
The main Shigella species are Shigella dysentariae, S. flexneri, S. boydii, and S. sonnei. Shigella, E. coli, and salmonella are all closely related; all usually cause some form of severe diarrhea. S. flexneri causes about 60 percent of the shigella infections in the nonindustrialized nations, and S. sonnei about 80 percent of those in the industrialized. S. dysentariae is the cause of most epidemics of dysentery.
Shigella organisms destroy the cellular lining of the intestinal mucosa and invade the body; the disease is generally accompanied by mild to severe diarrhea and/or dysentery. There are some 165 million shigella infections a year and about a million deaths. The main route of transmission is fecal/oral. There is frequent loose-stool diarrhea consisting mostly of blood and mucus accompanied by fever, pain, and bowel cramping. Sepsis, intestinal perforation, toxic megacolon, dehydration, hyponatremia, encephalopathy, hemolytic-uremic syndrome, and pneumonia are common acute complications from the infection. If untreated, persistent dysentery, severe protein loss, and malnutrition commonly occur, even in uncomplicated cases. Fever, malaise, and body aches are common no matter the severity of the infection. Some strains produce shiga toxins, which exacerbate the symptoms considerably.
S. dysentariae is very prone to antimicrobial resistance and soon passes the information on to the other species in the genus (as well as to E. coli and Salmonella spp.). Most strains are now resistant to nearly all low-cost antibacterials. The bacteria developed resistance in much of the world to the last low-cost antibacterial, quinolone NA, within 6 months after it was used to treat an epidemic outbreak.
The herbs that are effective for shigella are cryptolepis, sida, alchornea, bidens, the berberines, juniper, honey, licorice, lomatium, and ginger.
Formulation 1 (antibacterial) Cryptolepis, sida, or alchornea tincture: 1 tsp–1 tbl, 3–6x daily depending on the severity of the infection
Formulation 2 Berberine plant tincture: 1 tsp–1 tbl, 3–6x daily, depending on symptom picture
Formulation 3 (immune support) Lomatium tincture, licorice tincture, and ginger juice (mixed in equal parts): 1 tsp, 3x daily
Note: Juniper/evergreen needle and sida teas are especially useful for GI tract shigella infections.
For shigella with sepsis: To the above formulations, add Echinacea angustifolia tincture, ½ tsp–1 tbl, each half hour to hour.
Once considered to be Pseudomonas maltophilia, then identified as Xanthomonas maltophilia, now this newly emerging resistant bacteria is called Stenotrophomonas maltophilia. It usually occurs in hospitals, where it can cause infections in surgical wounds, pneumonia, bacteremia, endocarditis, and meningitis. Few herbs have been tested for activity against it as of 2011. Here is what is known to be active so far: Berberis spp., alchornea, boneset, honey, epigallocatechin (green tea constituent), Scorzonera sandrasica (aerial parts), eucalyptus essential oil, eucalyptus leaf tincture, thyme essential oil, oregano essential oil, Acacia aroma, Zuccagnia punctata, Sechium edule fluid extract, Salvia spp., Menyanthes trifoliata, Artemisia dracunculus, Mammea americana, Oedogonium capillare, Centaurea cariensis, Artemisia arborescens, Artemisia afra, rosemary, garlic, and devil’s claw (Harpagophytum procumbens).
Formulation 1 (antibacterial) Alchornea tincture: 1 tsp, 3–6x daily, depending on severity of symptoms
Formulation 2 Fresh garlic juice: ¼–1 tsp, up to 4x daily
Formulation 3 Thyme, rosemary, eucalyptus, and oregano essential oils (blended in equal parts), inhalation as aromatherapy: 3–6x daily
Formulation 4 Eucalyptus leaf infusion: 8 ounces, up to 6x daily
Formulation 5 (immune support) Boneset, licorice, and red root (equal parts) tincture: 1 tsp, 6x daily
Formulation 6 Piperine: 20 mg, 2x daily, with the first dose in the morning 30 minutes before taking the other formulations, and the second dose at 4 P.M.
For S. maltophilia pneumonia: Formulations 1 through 6
For S. maltophilia bacteremia: Formulations 1, 2, 4, 5, and 6 (omitting formulation 3). Add Echinacea angustifolia tincture, ½ tsp–1 tbl, every half hour to hour.
For S. maltophilia wound infections: Formulations 1, 2, 4, 5, and 6 (omitting formulation 3). Add daily honey dressings (see monograph, page 188).
For S. maltophilia meningitis: Formulations 1, 2, and 6. Add tincture of isatis leaf (or root) and either Japanese knotweed or stephania (equal parts), 1 tsp, 3–6x daily. Echinacea will also be of benefit, as for bacteremia.
Cholera organisms infect the small intestine and cause extensive watery diarrhea (10 to 20 quarts a day—usually without cramping), generalized muscle cramps, and sometimes vomiting (clear fluid), which in turn lead to dehydration and electrolyte imbalances. (One of the most important interventions in cholera treatment is fluid replacement.) About five million people a year suffer from cholera, but before antibiotics cholera epidemics were much worse. Generally, contaminated water or food is the culprit.
Prior to 1977, there were no reports of resistance in cholera organisms, but now they are common. Most cholera strains, including O1 Inaba, O139, O138, and El Tor, are now resistant to many antibiotics, including tetracycline, ampicillin, kanamycin, streptomycin, sulphonamides, trimethoprim, and gentamicin.
The herbs useful against cholera are the berberines, cryptolepis, licorice, ginger, Geranium mexicanum (or any of the geranium species’ roots), Psidium guajava (guava) leaf and bark tea or ethanol extract, and Punica granatum (pomegranate) fruit peel or bark as tea or ethanol extract. Basil (Ocimum basilicum), nopal cactus (Opuntia ficus-indica), Acacia famesiana, and Artemisia ludoviciana are also very active against cholera organisms. Extracts of those four plants (and the geraniums as well) disrupt the cell membranes of the cholera organisms, increase membrane permeability, decrease cytoplasm pH and cell membrane hyperpolarization, and decrease cellular ATP concentration in all strains tested. In fact, nearly any of the acacias will do for this use.
Formulation 1 (antibacterial) Cryptolepis and berberine plant (equal parts) tincture: 1 tsp, 6x daily
Formulation 2 Geranium root strong decoction: 3 tbl, every hour
Formulation 3 Guava leaf or bark and pomegranate peel or bark (equal parts) tea: as much as possible
Alternative Effective Decoction Acacia bark decoction: 3 tbl, every hour; basil and artemisia infusion: 8 ounces, every hour
The three resistant nonbacterial variants are the candidas, malaria, and the aspergillus mold.
Candida species are a type of yeast that form a normal part of the human intestinal and urinary tracts and skin flora. The main species is usually Candida albicans. Antibiotic overuse has stimulated tremendous problems with this organism. Overgrowth in the intestinal and urinary tracts is common. Candida has traditionally been treated with antifungals and azoles, but the last 20 years have seen significant resistance emerge across the entire genus.
Resistant candida infections cause urinary tract infections, vaginal infections, mouth infections (thrush)—they love mucous membrane systems. Itching, burning, soreness, irritation, and whitish patches or discharge are common symptoms. In some instances candida can become systemic and affect multiple organs. Infections are much more serious in people whose immune systems are compromised.
The herbs to treat candida are sida, alchornea, bidens, cryptolepis (minimally), Artemisia annua, the berberines, juniper, honey, usnea, black pepper, lomatium, isatis, licorice, red root flowers, reishi, echinacea, chaparro amargosa (Castela emoryi), and desert willow (Chilopsis linearis).
Formulation Berberine plant, alchornea, or sida tincture: 1 tsp, 3x daily; or juniper berry–bidens tincture (1 part juniper, 2 parts bidens): 30 drops, 3x daily; or lomatium, isatis, and echinacea (equal parts) tincture: 1 tsp, 3x daily
Formulation 1 (antibacterial) Alchornea or sida tincture: 1 tsp, 3x daily
Formulation 2 Lomatium, isatis, and echinacea (equal parts) tincture: 1 tsp, 3x daily
Formulation 3 Berberine tincture diluted in water, used as a douche (see page 162): 2x daily, in the morning and again in the evening
Formulation 1 (antibacterial) Lomatium, isatis, and echinacea (equal parts) tincture: 1 tsp, 3x daily
Formulation 2 One ounce berberine tincture diluted in 6 ounces water, take 1 tablespoon to wash mouth and gums thoroughly: 3x daily
Formulation 1 (antibacterial) Alchornea or sida tincture: 1 tsp, 3x daily
Formulation 2 Licorice, reishi, and echinacea (equal parts) tincture: 1 tsp, 3x daily
Formulation 3 Desert willow and chaparro amargosa (equal parts) tincture: 1 tsp, 3x daily
There are some 200 or more species of plasmodia, parasitic protists that infect red blood cells. Eleven of the species infect people. The disease is transmitted by mosquito bites. The organisms grow in the liver, then infect the red blood cells. Fever, shivering, shaking, muscle pain, headache, anemia, enlarged spleen and liver, and malaise are typical symptoms. Vomiting is sometimes present. In severe infections brain damage, convulsions, and death can occur. Given their life cycle, latent parasites can emerge later. This is why treatment for Plasmodium is often repeated after 14 days.
Worldwide, there are some 250 million cases of malaria each year, resulting in nearly a million deaths, and 80 percent of them come from Plasmodium falciparum. The malarial organisms are often resistant to antibiotics, hence the development of artemisinin from Artemisia annua. However, the use of that isolated constituent is now provoking resistance worldwide, so the constituent is often combined with antibiotics to retard resistance development. In the treatment of malaria, the whole herb or mixtures of herbs are preferable for just that reason.
The herbs effective for malaria are cryptolepis, sida, alchornea, bidens, Artemisia annua, juniper, isatis, and licorice.
Formulation Cryptolepis, sida, or alchornea tincture: 1 tbl, 3x daily for 7 days, repeat in 14 days; or artemisinin: 1,000 mg the first day, 500 mg daily for 4 more days, repeat in 14 days
Aspergillus, especially A. fumigatus, is an increasing source of resistant infections. This rather common mold can cause bronchopulmonary infections and chronic sinusitis. In hospital settings or among the immunocompromised it usually causes pulmonary disease and to a lesser extent surgical wound infections. It is resistant to most available drugs—polyenes, azoles, and echinocandins. Mortality rates in hospitals run 50 percent to 60 percent on average and as high as 90 percent in some populations (such as leukemia patients).
The herbs effective for aspergillus are sida, alchornea, cryptolepis, juniper, lomatium, isatis, ginger, honey, Artemisia giraldii, and Sechium edule fluid extract.
Formulation 1 (antibacterial) Cryptolepis, sida, or alchornea tincture, or a combination of the three: 1 tsp, 3x daily
Formulation 2 (immune support) Ginger, licorice, and rhodiola (equal parts) tincture: 1 tsp, 3x daily
Formulation 3 Nasal spray formula for sinus infections (see page 181) prepared with just juniper essential oil; or juniper essential oil inhalation as aromatherapy: 3–6x daily
For sinusitis and bronchopulmonary conditions: Formulations 1, 2, and 3
For systemic treatment in the immunocompromised, pulmonary infection, or pneumonia: Formulations 1, 2, and 3; increase the dosage for formulations 1 and 2 to 1 tsp–1 tbl, up to 6x daily
For surgical wound infections: Formulations 1 and 2, plus topical honey dressing daily (see monograph, page 188)