Figure 4.1 Sir Almroth Wright. (Wikimedia Commons)
Pathology may be defined as the study and diagnosis of disease. The word pathology is from Greek πάθος, pathos, “feeling, suffering”; and λογία -logia “the study of”.
Although not a frontline service directly dealing with the wounded being brought into the various medical facilities, it should not be thought that “pathology”, which is an encompassing term for laboratory medicine concerned with the cause and effect of disease, did not make a significant contribution to the British and Allied war effort.
Many extremely distinguished doctors worked in this area of medicine, and their contribution to the understanding of a variety of conditions which affected soldiers, both wounds and disease, will be highlighted within the relevant sections of this chapter. Some topics will be discussed in detail, and an attempt will be made to put them into perspective from nearly one hundred years later. It was only by understanding the mechanisms of damage to cells and tissues, as well as the body’s response to injury and disease, that there could be the scientific development needed to understand and treat the wounds and illnesses that occurred during the Great War.
Fighting conditions experienced by the British Army during the Great War differed from those encountered in any previous conflict in which they had been involved. Since the Battle of Waterloo in 1815, a number of small colonial wars had been fought, mainly in Asia and Africa. However, only the Crimean War and the Second Boer War could be considered to be on the scale of major conflicts, although neither approached the magnitude of events between 1914 and 1918. Lessons had been learned from the Crimean War (1853-1856) and the Second Boer War (1899-1902) about the risk to troops of infectious diseases and the necessity of good hygiene (see Chapter 1). This knowledge was supplemented by observations of what occurred during the American Civil War (1861-65) and the Russo-Japanese War (1904-05). Arguably much more could, and should, have been learned from these conflicts. For example, this particularly applies to the management of abdominal wounds sustained by the Russians in the Russo-Japanese War, as will be discussed in Chapter 7.
Pathology in 1914 was at a fairly early stage of its development, both as a science and as a branch of medicine. Rudolf Virchow was a German doctor who is considered to be the father of histopathology, which is the study of disease at a cellular level. Virchow initially described the concept in 1854, and had died in 1902, just a few years before the start of the Great War.
Of particular importance for the development of surgery was the introduction of anti-septic surgery. This really started in 1867 when it was introduced by Joseph Lister, Professor of Surgery at the University of Glasgow. Anti-sepsis reduced the risk of patients developing infections after undergoing surgery although the reasons why this worked were not fully understood. The first micro-organism, a bacterium, was only identified in 1876 when Robert Koch, another leading German doctor who had studied under Virchow, demonstrated the bacteria which caused the disease anthrax. Koch was subsequently awarded the Nobel Prize for Medicine for his work in 1910. Further developments in the study and identification of bacteria led to specific ways of seeing bacteria under the microscope by staining them with special chemicals. Two keys methods of doing this were by means of the “acid fast” and Gram’s stains, which were introduced in 1882 and 1884, respectively.
It is important to remember that although bacteria had now been identified as the cause of infections, antibiotics to kill them would not be available for many years to come. However, innovative doctors and scientists tried using a variety of chemicals which were administrated to patients to kill bacteria, usually without success. Notable exceptions were the developments of Atoxyl to treat sleeping sickness and Salvarsan to treat syphilis. Salvarsan was developed in 1909 by Paul Ehrlich, who was born in East Prussia (now partly Poland, partly Russia). It was the first really successful chemical treatment for syphilis, and a chemical that did not damage the patient! After being introduced into clinical practice in 1910, it became one of the most commonly prescribed drugs in the world until it was replaced by penicillin more than 30 years later. Ehrlich, too, was awarded a Nobel Prize for his contribution to medicine.
Surgical histopathology became established in the 1880s. There was one very famous example illustrating the early difficulties encountered using histopathological diagnosis. In January 1887, the Crown Prince Frederick of Germany, who was married to Victoria, the eldest daughter of Queen Victoria, became persistently hoarse, and a small lump was removed from his vocal cords. A cancer was suspected by his German doctors, and Dr Ernst von Bergmann was involved in his treatment. Originally Bergmann was from what is now Latvia and had been professor of surgery in Dorpat and Würzburg before moving to Berlin in 1882. Von Bergmann played a key role in the advance of surgery by introducing the sterilisation of surgical instruments.
He recommended to the Crown Prince that surgery was necessary to remove the affected area of the vocal cords and this would be a major undertaking. Therefore, before proceeding with the surgery, it was decided that a further opinion should be sought from Dr Morell MacKenzie, a British doctor who was regarded as “the greatest living authority on diseases of the throat”. MacKenzie had studied in Paris, Vienna and Budapest where significant and rapid advances were being made in many branches of medicine, and he had acquired great experience. His practice was at the London Hospital.
Summoned to Berlin in May 1887, Mackenzie insisted that unless the growth could be proved (by taking a sample of tissue called a biopsy) to be cancer, then the radical and extensive surgery proposed should be cancelled. A biopsy was taken from the Crown Prince’s larynx, and was examined by Dr Virchow, who was then Director of the Pathological Institute of Berlin. Virchow pronounced the growth to be benign, but he was incorrect in his diagnosis. It was in fact malignant, as the Crown Prince’s subsequent clinical progress confirmed. The tumour gradually grew, and obstructed his airway until he was unable to breathe properly.
It became necessary to perform a tracheotomy (making a cut in the neck directly into the trachea or windpipe) and a silver tracheotomy tube was inserted into his trachea so that he could breathe. This was of course a palliative measure, and his cancer relentlessly and, painfully, progressed, finally resulting in the death of Frederick who had by then become Emperor Frederick III of Germany, albeit only for a short-lived reign. This medical error may well have been an important contributory factor in the background to the Great War, because it alienated Frederick’s son Wilhelm, who became Kaiser Wilhelm II on his father’s death, and helped fuel mounting Prussian antagonism towards Britain.1
It is worth noting that the Royal Army Medical Corps was only formed in 1898; this is discussed in some detail in Chapter 1. Prior to this, in 1860, the Army Medical School had been established, although the study of bacteria – bacteriology – was only included in the curriculum in the 1890s. This delay reflects what was happening simultaneously in the general curricula that were being offered to medical students in the medical schools of the British universities at that time.2 Under the leadership of Almroth Wright, Professor of Pathology from 1892 to 1900, the Army Medical School was established at the leading edge of research in bacteriology and hygiene.
Wright was born in 1861, and graduated from Trinity College Dublin in 1883. He was appointed Professor of Pathology at the Army Medical School, Netley in 1892 and rapidly took an interest in typhoid, and in particular the possibility of developing a bactericidal antibody directed against the bacterium which causes typhoid, salmonella typhi, by injecting heat-killed bacteria into the body as a vaccine, to stimulate the body to make antibodies against this bacterium, thus enabling it to destroy it should there be subsequent exposure. This followed the example set by Louis Pasteur to protect against the bacterium responsible for causing anthrax. Although trials were successful, his proposal to inoculate all soldiers with the vaccine who were going to be travelling to South Africa for the Second Boer War was rejected and only 4% of soldiers were protected in this way. In the three years of the war, there were 57,000 recorded cases of typhoid and this resulted in 9,000 deaths.
Further studies demonstrated the worth of inoculation against typhoid so that in the Great War every soldier was encouraged to be protected against the disease. As a result, only 20,000 cases and 1,191 deaths were seen in this much larger conflict. Wright had moved to St Mary’s Hospital, London, as Professor of Pathology and Bacteriology, a position he held until 1946, the year before his death at the age of 85. After the outbreak of the Great War, he established a laboratory in the Casino at Boulogne and took particular interest in wound infections, receiving help from another famous doctor, Alexander Fleming.
Alexander Fleming was born in Darvel, Ayrshire in 1881 and studied medicine at St Mary’s Hospital, London, graduating in 1906. He became assistant bacteriologist to Almroth Wright and served in the RAMC. He demonstrated that antiseptics were counter-productive in treating deep-seated anaerobic infections and he is best remembered for his work after the Great War – the serendipitous discovery of the antibiotic penicillin in 1928 which was the basis for his Nobel Prize, awarded in 1945.
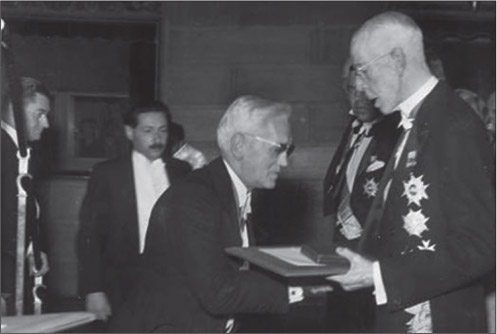
Figure 4.2 Sir Alexander Fleming receiving the Nobel Prize for medicine. (Wikimedia Commons)
A leading protagonist in the development of this scientific basis for medicine was David Bruce, an Australian by birth but who graduated from the University of Edinburgh in 1881. He made major contributions to the understanding of tropical diseases and was commandant of the Army Medical College during the Great War. His name lives on in the disease Brucellosis (a disease which chiefly affects cattle, but can cause undulant fever in humans) and in Trypanosoma brucei, (the cause of sleeping sickness).
Practical application of these disciplines in the British Army lagged behind that of the French and German armies. When speaking in 1914 Sir William Osler, a Canadian who had been Professor of Medicine at the University of Oxford since 1905, observed that in the Second Boer War, the “microbe killed more than the bullet”.3 Indeed he was correct because in that conflict, 14,048 soldiers died of disease, compared with about half that number – 7,994 – who were either killed in action or died of wounds.4 This happened because soldiers had not been immunised against typhoid, despite the excellent work of Almroth Wright.
Pathology in the period of the Great War was a medical specialty which encompassed several different areas of laboratory medical specialties. Nowadays, doctors who focus on laboratory medicine work in their own highly specialised areas for the benefit of patients, for example, histopathology (the study of tissues removed from the body which are examined microscopically to allow a disease to be diagnosed), microbiology (the study of microorganisms such as bacteria, fungi and viruses which cause disease), biochemistry (the study of the various chemicals which are in the blood and the different body tissues) and haematology (which is the study of the cells in the blood stream and the bone marrow where they are produced). The doctors and staff working in pathology during the Great War had a broad overview of laboratory medicine, in the same way that surgeons were “general”, and able to turn their hands to any procedure. Specialisation had yet to develop at that point in time.
Laboratories were involved in diverse areas, especially microbiology, which was concerned both with the identification of bacteria responsible for wound infections, (such a major problem during the Great War), as well as trying to ensure the maintenance of good (or as best as was possible) general health in soldiers. They did this through prevention and diagnosis of the normal range of infections to which large numbers of young men, who were kept in fairly close contact, would be liable to develop, for example, measles and tuberculosis. In 1914, tuberculosis was a disease responsible for killing great numbers of people, and was rightly feared. But what about measles, which today is generally regarded as of little importance, although it may have the most serious of consequences? When men of the 51st (Highland) Division, went to Bedford near London to complete their training before embarking for the Western Front, there was an outbreak of measles. There were 529 cases of measles, and 65 men died of the disease, a mortality of 10.8%, which may well be surprising to the reader. The epidemic was more deadly in the case of men from the more northern parts of Scotland, and from the Western Isles, according to the Official History of the 51st Division.5
There was a high prevalence of venereal (sexually transmitted) diseases, with official statistics recording a total of 416,891 cases of venereal disease in all theatres of war between 1914 and 1918.6 From August 1914 to December 1918, there were 153,531 admissions to hospitals in France as a result of soldiers contracting sexually transmitted infections. Prevention of venereal disease was thought to be best achieved by “moral persuasion”. What exactly does that mean? The official policy was to encourage men to spend their recreational hours engaged in wholesome pursuits in “places of healthy amusement” and so they would be better placed to resist “temptation”. For example, skittle alleys, organised sports, libraries and gyms were provided for the men as an alternative to sexual activity. The prevention of venereal diseases was generally regarded as much a moral issue as it was a medical one. There was a variety of health guides available for the soldiers, which encouraged virtues such as “cleanliness, moderation, pure air and self control”. If men were diagnosed with a venereal disease, their pay was stopped and leave was withheld for 12 months, and for the first two years of the war the patient’s family were informed of the fact that their relative had a venereal disease. Furthermore, there were random checks made where men would have to lower their trousers and be inspected for signs of these diseases – in front of their superiors. This was called a “dangle parade” but will not be discussed further here!
There was extensive debate about how to reduce the increasing numbers of soldiers who were contracting venereal diseases, for example, licensing and medical checks of those who worked in brothels, putting soldiers through a chemical decontamination process after they had visited brothels or even giving each soldier six “preventive outfits” (chemicals to use on themselves with the intention of destroying the causative bacteria) when they went on leave. Furthermore, these should only be supplied to “those who deliberately set out to gratify their sexual desires”.7 There was certainly a great need to overcome prejudice and to apply the scientific basis of medicine to help in the prevention of venereal disease rather than by some of the methods that were employed!
A number of apparently newly-identified disease entities were recognised during the Great War, and their patho-physiology investigated, and as far as possible defined. The reader is referred to the History of the Great War based on Official Documents, Medical Services, Pathology edited by Major Sir W.G. MacPherson and others, and published in 1923.8 Alexander Fleming, Robert Muir and Almroth Wright were amongst the contributors to this volume. Robert Muir was Professor of Pathology at the University of Glasgow, and was a Lieutenant-Colonel in charge of the pathological and bacteriological work at the 3rd and 4th Scottish General Hospitals during the Great War. Later, he went on to write a textbook of pathology, which became of such importance that it is still available in updated format in the 21st Century for the current generation of pathologists and medical students to use.
The experiences of the British Army in the Second Boer War, notably the significant number of deaths from enteric fevers (typhoid fever and paratyphoid fever), influenced thinking in the RAMC, especially in terms of sanitation and the supply of pure water to the troops. A recommendation was made by the Sanitary Advisory Board that all troops should receive anti-typhoid inoculations, but this was not followed by the Army Council.
In 1908 it became apparent that only six posts were available to officers qualified as specialists in microbiology, although 31 such were qualified in this field. Although the Sanitary Advisory Board recommended that all hospitals with more than 100 beds should appoint a clinical pathologist, no attempt was made to increase the number of army appointments. Unsurprisingly, the existing resources in the army for the provision of pathology services were inadequate for the scale of war which rapidly developed between 1914 and 1916, and most civilian laboratories sent the bulk of their staff to serve in the army.
In 1914, the post of Advisor in Pathology to the Director-General of Medical Services, British Forces in France, was established. The first incumbent was Sir William Leishman, a graduate of the University of Glasgow, who had previously identified the causal organism of Kala-Azar (Leishmaniasis), which is a tropical disease caused by a microscopic parasite called a protozoan, and is transmitted by the bite of sandflies.
By the outbreak of the Great War, the Royal Army Medical College had recognised the importance of providing microbiological support to the armed forces at home and abroad, particularly in tropical areas of the Empire, through junior and senior courses in pathology. On completion of the latter three-month course, officers might choose a further three-month course covering all areas of microbiology, resulting in registration as a specialist in microbiology. Only around 50 men worked in the laboratories at home and abroad, with a smaller number held in the reserve.
Although large numbers of casualties with serious wound infections, including tetanus and gas gangrene, were noted in the initial phases of the war where there was a great mobility of troops, it was impossible to develop proper microbiology services at this stage. As trench warfare became established, and the movement of troops and their units reduced, it became possible to set up laboratories in relationship to the medical facilities. These were mobile laboratories, the first being a bacteriology laboratory which reached France in October 1914. This was followed by a hygiene laboratory the following month, and by 1915, each army was allocated two bacteriology laboratories, and one hygiene facility. Static hospital laboratories were established, initially at No. 2 and No. 4 General Hospitals at Le Havre and Versailles, respectively. Eventually, three types of laboratory were established.
These were truly mobile and could support the forward area, particularly the casualty clearing stations. This mobile capacity was of great value during the retreat during the German Spring Offensives of 1918, and Allied advances in the autumn offensives during the final one hundred days of the war (see Chapter 1). Mobile units were equipped to a level which would allow them to function autonomously. They carried autoclaves (machines using steam under pressure for sterilising surgical instruments), incubators (for growing bacteria on special plates and allowing their identification) and centrifuges. Twenty-five such laboratories were supplied, and eighteen were allocated to the Western Front, seven being divided between Salonika, Egypt and East Africa. Their work lay largely in the routine diagnosis of patients with suspected enteric fevers (typhoid and para-typhoid fevers), dysentery, diphtheria and meningitis. Sputum and urine examination and blood counts were carried out, and autopsies (post-mortem examinations) were also required.
The requirement for microbiology services related to wounds clearly varied depending on how busy the casualty clearing stations were, being obviously much greater during periods of heavy fighting.
Post-mortem studies were of great importance in helping to understand the effects brought about by different wounds and how these resulted in the death of a soldier. This is well illustrated in Chapter 7, which deals with abdominal wounds, and will be fully explained in that part of the book. Post-mortem studies performed on soldiers dying from abdominal wounds revealed that haemorrhage (bleeding) was the main cause of death, usually occurring soon after the wound had been inflicted. In contrast, infection caused deaths a few days after the wound had been sustained. This new knowledge impacted on treatment, leading directly to early operative intervention in these patients, with considerable improvement in prognosis.
These were key parts of all general hospitals of 520 beds and over, and each had a single microbiologist. The duties of this laboratory were similar to those of the mobile unit, but the balance shifted towards the management of soldiers with severe wound infections. While it was suggested that economies of scale might be achieved by concentrating services in large general hospital bases, the benefits of close liaison amongst the patient, the responsible clinician and the microbiologist were considered to mitigate against such centralisation. However, a central mortuary and autopsy facility was established at Étaples. It is interesting to note that there are similar debates regarding centralisation of services in many areas within the National Health Service at the present time.
No thought had been given initially to the provision of central research laboratories, which could be freed from the burden of day-to-day routine analyses of samples so that they might advance understanding and help in the development of new treatments. Colonel Sir Almroth Wright in effect established the first research laboratory at No 13 General Hospital, which was located in Boulogne. Assisted by colleagues from St Mary’s Hospital London, including Alexander Fleming, he made significant contributions, for example to wound healing and to the understanding of gas gangrene. Wright’s major contribution to the understanding of shock has already been discussed at length in Chapter 3. This clearly illustrates the great importance of research laboratories in helping to understand the causes of clinical problems and by so doing, helping to find solutions and improve treatment.
Whilst this was happening, hospitals in the UK required pathological expertise to cope with the needs of men undergoing military training and the increasing flow of men who had been wounded and were returning home to the UK. General military hospitals were often established in, or close to, existing civilian hospitals and medical schools, and utilised their laboratories services. Staff members from civilian hospitals were often commissioned into the RAMC or the Territorials.
The principles of wound healing, effectively the production of granulation tissue (discussed in chapters 2 and 6), fracture callus (the body’s healing process for fractured bones) and epithelial regeneration (healing of skin), were already known before the outbreak of the war, and no major advances in these areas were made. From a pathological standpoint, wounds were classified by pathologists during the Great War as falling into one of four categories
• Wounds where tissue had been avulsed, and carried away, for example the ripping away of an arm or leg, usually by a large irregular metal fragment of exploding shell casing,
• Perforating and fracturing wounds, where a projectile had struck bone and fragmented it, these fragments either leaving through an exit wound or if not, forming irregular cavities within the tissues (see Chapter 6 for the example of compound fracture of the femur),
• Sutured amputation wounds, with collection of pus deep to the flaps of skin which had been stitched back together,
• Implunging wounds caused by nearly spent pieces of shrapnel ball, bullet or shell casing having enough residual energy to penetrate the skin.
Regardless of this classification, and in contrast to the experience of surgeons dealing with the wounded in the Second Boer War of 1899 to 1902 which had been fought on the hot dry battlefields of South Africa, it became clear early in the war fought on the arable soil of the Western Front, that almost every type of wound sustained in the manured fields of France and Flanders could became infected.
Infections with the bacteria streptococcus were very common and led to diffuse infection and inflammation of the tissues called cellulitis. This is a rapidly spreading infection through the skin and subcutaneous tissue adjacent to the site of a penetrating wound. The skin of the entire limb may become red, indurated, and feel very hot to the touch. The infection may spread to the lymph nodes, and to the bloodstream (septicaemia) with fatal consequences.
The poet Rupert Brooke sailed with the British Mediterranean Expeditionary Force on 28 February 1915, but developed septicaemia from an infected mosquito bite. He died on 23 April 1915 in a French hospital ship moored in a bay off the island of Skyros in the Aegean on his way to Gallipoli. He lies buried “in some corner of a foreign field that is forever England”. There were no antibiotics in 1915 but had there been, Brooke and many others who developed septicaemia may well have survived. Gas Gangrene
There were numerous cases of gas gangrene, an infection characterised by spreading necrosis (death) of tissue with the production of gas. Gas gangrene was seen frequently in the early months of the war, and indeed occurred in around 10% of the wounded. It presented with two distinct clinical patterns. The first pattern was seen when the infection spread in the subcutaneous plane (under the skin) with the formation of gas and fluid-filled bullae (loose, baggy, fluid filled blisters in the skin). The second pattern of presentation involved deep infection within skeletal muscle, the limb becoming cold and hard and death following invariably, unless the limb was amputated immediately with complete removal of all involved tissue. The buttocks, calves and hamstrings were particularly common sites for gangrene, the trunk being seldom affected. The surgical prevention of gas gangrene, and its treatment once established, is discussed in detail in Chapters 2 and 6.
The pathology of gas gangrene was investigated urgently as this was a major clinical problem.9 Impairment of the blood supply to muscle resulted in a deficiency or absence of oxygen in the tissues, which was an ideal milieu for the growth of bacteria, which only thrive in the absence of oxygen (anaerobic bacteria). These bacteria produced toxins which in turn caused further muscle damage culminating in the death of muscle. The tissues affected rapidly became very oedematous with the accumulation of fluid within them, later to be followed by the death (coagulative necrosis) of the muscle fibres.
Coagulative necrosis is a term used to describe death of cells which has been caused by loss of their blood supply. It is characterised by a “ghostly” appearance of the cells under the microscope, and reflects death of the cells due to absence of oxygen. In time, the bacteria invade and grow within these necrotic fibres. Culture of many of these anaerobic organisms outside the body (in vitro) was difficult, although not for Clostridium welchii, one of the principal organisms responsible for gas gangrene. Consequently, laboratory diagnosis was carried out by inoculation of an emulsion of necrotic muscle and oedema fluid into animals previously treated with specific anti-toxins. The clinical state of the animal and histological examination of its tissues gave information as to the likely causative bacterium of the infection.
A move to early surgery with radical wound excision led to a dramatic reduction of these overwhelming and lethal infections, so that only 1% of wounded developed this complication by 1918. Also, by 1918 an anti-toxin against Clostridium perfringens (another bacterium causing gas gangrene) was used, but with limited success. It became clear that this was at best an aid to surgical therapy, and not a substitute for it.
Almost 100 years later, gas gangrene remains a problem in civilian and military medicine to this day.10
Tetanus
Significant advances were made in the understanding of the pathology of tetanus. Like the organisms responsible for gas gangrene, the bacteria causing tetanus are anaerobic. There was a problem growing and identifying these bacteria in the laboratory, given that they only grew in the absence of oxygen. Anaerobic culture was made simpler however, by the finding that oxygen need not be excluded if fragments of meat were added to the culture medium, forming a “meat broth”. Several subtypes of Clostridium tetani were identified, but all appeared to produce the same toxin, which could be neutralised by the same anti-toxin. It became clear that Clostridium tetani could be isolated from many wounds in patients who did not suffer from tetanus, and that the disease might follow many months after the wound had been sustained due to germination of spores. Spores are produced as part of the bacterium’s life cycle where it can exist and survive in an almost inert state for long periods of time before it begins to grow and multiply. This resurgence in activity, growth and multiplication of the bacterium can be provoked by further tissue damage, be it mechanical, chemical or due to co-infection, especially with other anaerobic bacteria. As has already been discussed in Chapter 2 this explains why many cases of tetanus occurred long after the casualties returned to the UK.
Most importantly, routine administration of tetanus antitoxin (serum from an animal infected with the disease, and therefore by anti-tetanus toxin antibodies) to the wounded resulted in a great reduction in the incidence of tetanus, to approximately one-sixth of that seen early in the war. In addition, the mortality of those who developed the disease despite prophylaxis was greatly reduced.
A number of clinical entities were “discovered” during the Great War, and some of the more important ones are discussed in the following paragraphs. While these examples go into detailed histopathology, of principal interest to the specialist pathologist, it should be appreciated that pathology research laboratories responded vigorously to these new entities, and did so “despite there being a war on” in order to help the war effort by understanding disease and helping to point the way towards finding solutions to problems.
In the spring of 1915 in Flanders, the first patients affected by this disease were described by Graham11 with a more complete clinical account by Hunt and Rankin following shortly thereafter.12 The term was coined by soldiers themselves and although it was not confined to those serving in the trenches, that is where it first appeared. Clinically, the soldiers with the disease were characterised by a fever lasting 5 to 7 days, often followed by a single short relapse after which the soldier was fit to return to duty. Subsequently, some patients were noted to suffer from a shorter period of fever but with more frequent and severe relapses that resulted in a longer period of incapacity.13 In addition, those affected complained of headaches, skin rashes, experienced pain in their bones and there was often enlargement of the spleen (splenomegaly). There were no deaths from this condition and therefore no autopsies were carried out, other than in those who had been affected by the disease but were dying of other causes, usually severe wounds. The disease occurred widely within France, affecting French and German soldiers and referred to as “fièvre des tranchées” and “febris Wolhynica” and appears to have been transferred to the Salonika Front in the autumn of 1915. Overall, almost one million soldiers appear to have been affected during the war.
From the outset an infective cause was considered likely, perhaps related to enteric fevers. Standard bacteriological techniques were employed, to try and track down the causative organism. These tests included culture agglutination techniques, which were negative, and initial haematological examinations showed only leucocytosis (an increase in the number of white blood cells to combat infection). In 1916 His and colleagues described dumb-bell shaped bodies some 1-2 microns in length lying free or within the red blood cells, especially during episodes when the patient had a fever. These dumb-bell shaped bodies resembled similar bodies described in Rocky Mountain Spotted Fever and in Typhus Fever.
An important pathologist who was keen to understand and learn more about disease was John McNee, who was born near Glasgow in 1887. He graduated from Glasgow University in 1909 and as Major McNee of the RAMC, served as assistant advisor in pathology to the 1st Army before later returning to Glasgow as Professor of Practice of Medicine. Experimental pathology was carried out by McNee and his colleagues initially by inoculation of experimental animals, but, as it became clear that there was no threat to life attempts were then made to transmit the disease to volunteers, which were successful.14 Transfer of whole blood from patients to volunteers by the intravenous or subcutaneous route resulted in the development of the disease.
The mechanism of transmission in the trenches was explored further by Hunt and McNee, and as the disease continued during the winter of 1915-16, flies were exculpated. Circumstantial evidence suggested the body louse, pediculus corporis, was the vector and this was confirmed by a series of British and American experiments during 1917 and 1918. Additionally, the microscopic bodies described on blood films were demonstrated within the faeces of lice by Topfer in 1916.
Figure 4.5 Sir John McNee. (With permission of the University of Glasgow Archive Services GB0248 UP1/357/1)
Subsequently, the infective agent was identified as Rickettsia Quintana (so called because of the periodicity of the fever of 5 days), and now reclassified as Bartonella Quintana. It may be of interest to note that “urban trench fever” is found in the homeless in the present time15 and, perhaps, more so to those interested in military history of the Napoleonic Wars, within La Grande Armée.16 The common factor, of course, linking the trenches of France and Flanders with the homeless of today, is the body louse. The histological features include perivascular lymphocytic infiltrates, and granulomatous inflammation within lymph nodes, akin to those seen in cat-scratch fever.17
A standard pastime of troops in the trenches was to rid themselves of lice whenever they could. Lice were frequently referred to as “chats” and men would gather in groups to de-louse themselves (ie ‘to chat’). One favoured method of eradicating lice was to quickly run a lit candle along the seams of clothing, where lice would typically converge.
This disease first appeared in early 1915, especially affecting troops in the trenches18, and reaching a maximum of 100 per 100,000 troops in December 1916. It was noted that officers were seldom affected and cases in civilians in areas of high prevalence were not identified. German, Austrian and then French soldiers were also subject to this disorder, which was not seen in the trenches of Gallipoli. It was the most important renal (kidney) disorder of the war and accounted for 5% of medical admissions.
Previously healthy soldiers rapidly became unwell with proteinuria (the presence of protein in the urine, and indicative of kidney damage), facial oedema (swelling of the face), often fever and dyspnoea (breathlessness), headache and sore throat. Examination of the urine confirmed the proteinuria and also revealed haematuria (blood in urine) and the presence of urinary casts. Urinary casts are cylindrical structures produced by the kidney and are present in the urine in certain disease states.
While most patients recovered rapidly some developed recurrences and progressed to subacute nephritis and a significant number died; many of those who died were subjected to post-mortem examination. Dunn and McNee described the renal lesions in 35 fatal cases, all dying within 2 weeks of onset.19 Unsurprisingly, the main abnormality was glomerular.
A glomerulus is a capillary tuft that performs the first step in filtering blood to form urine. The glomeruli were enlarged and hypercellular, with enlargement and proliferation of endothelial cells with fibrin thrombi. There was a mild infiltration of polymorphonuclear leucocytes and lymphocytes. Crescents were seldom seen in the acute phase. The initiating event in all glomerular crescents is the development of a physical gap, or hole, in the glomerular capillary wall. The presence of crescents in glomeruli is a histologic marker of severe injury. The appearances were therefore those of an acute glomerulonephritis, or active inflammation of the glomeruli. Secondary changes were found in the lungs with oedema, and formation of diffuse alveolar damage (damage to the air sacs in the lung), and a non-specific response to damage to the alveolar walls. The appearances, for example, were noted to be similar to those seen in chlorine gas inhalation. Unfortunately of course, pathologists had an opportunity to study the effects of exposure to chlorine gas, which was first employed by the Germans on the Western Front on 22 April 1915, during the Second Battle of Ypres.
In later stages, glomerular sclerosis with crescent formation was seen, with secondary changes of atrophy and dilatation of the renal tubules and fibrosis and lymphocytic infiltration of the interstitium. While these histological details will really only be of interest to pathologists, they serve to illustrate that research laboratories were able to devote time to understanding the behaviour of a “new disease”, and could do so while there were enormous clinical pressures being exerted elsewhere in the service.
It was very important to have surgeons and anaesthetists working on the never-ending numbers of wounded. It was equally important to have pathologists working in the relatively protected environment of research laboratories, trying to help resolve new clinical problems as they cropped up.
Unfortunately, as often happens in medicine, the aetiology of trench nephritis has never been established with conviction, although a post-infective cause seems most likely.20 Interestingly, a similar form of nephritis appears to have affected soldiers in the American Civil War.
Two outbreaks of fever and jaundice which occurred during the Great War were shown to be due to infection by the spirochaete, Leptospira icterohaemorrhagica (a particular type of bacterium). Although sporadic cases occurred in 1915 and later in the war, the first main epidemic occurred near Ypres in the summer of 1916, and the other in the British Army in Italy. In Japan in 1916 it became clear that the spirochaete was responsible and that the common rat was the animal host, the organism being excreted in the urine. From an accidental laboratory transmission, the incubation period was shown to be 6 to 8 days, and the clinical features were of fever, malaise, myalgia (muscle pain), conjunctivitis and headache, followed by jaundice.
In the Flanders outbreak, fewer than 10% of patients who were infected died. In those, autopsy showed severe jaundice, haemorrhage within viscera (abdominal organs) and serous membranes and consistent changes within the kidneys of acute tubular necrosis (reflecting acute kidney failure) and acute interstitial nephritis, an inflammation of the kidney. The liver changes were variable, in some there being marked centrilobular necrosis which is a particular pattern of cell death, with lack of cohesion of the liver cells and white blood cell infiltration, while in others there was little abnormal.
Again, while the detailed histopathology may only be of interest to medical readers, the wider issue here is that a potentially fatal cause of infective jaundice was identified and analysed by laboratory studies. As a result of this important research, Captain Philip Gosse was appointed to the post of “Rat Officer” to the British 2nd Army, with a remit to draw up schemes for the catching and destruction of rats. Schools of sanitation ran “rat classes”, and there were “rat lectures”, all designed to help rid the trenches of the vermin, thus reducing the probability of contracting a potentially fatal disease.
Although Landsteiner described what became known as the ABO blood groups and their incompatibilities in 1900, in general, blood transfusion was seldom used in civilian practice before 1914. Its major impact came in the last two years of the war, and the contribution of two military doctors, one Canadian and one American, was very significant.21
The first, Lawrence Bruce Robertson, a surgeon who served in the Canadian Corps of the British 3rd Army from 1915 to 1917, described blood transfusion of non-crossmatched blood directly from donor to recipient, albeit by a syringe–cannula technique rather than direct artery to vein contact.22 Although death could occur as a result of acute haemolysis where the red blood cells were broken down, the effects were strikingly beneficial to those who did not have a transfusion reaction. The limitations of direct transfusion in a war zone are obvious, and his namesake, the American Oswald Hope Robertson, introduced the use of previously stored citrated (to prevent clotting) blood during the Battle of Cambrai in 1917.23 Initially, only Group O blood was used (at that time classified as Group 4) and was given in a casualty clearing station. Of the 20 transfused patients, all of whom were expected to die, 11 survived. By 1918, transfusions were administered closer to the front than casualty clearing stations, including in a field ambulance.24
It is often correctly stated that more people died in the influenza pandemic of 1918 to 1919 than in the Great War itself. Estimates of the number of deaths that occurred worldwide vary at between 50 and 100 million. It was called Spanish ‘Flu because Spain was a nonbelligerent nation, and being a neutral country, had no reason to exert censorship on the truth by concealing the numbers of its citizens who had succumbed to the disease. It was no more common in Spain than elsewhere. Nor did it have its origin in Spain. Indeed, the pandemic probably had its origin in the conflict, possibly at the British military base at Étaples, where 100,000 men mixed with pigs, ducks and geese may have been the source.25 There was little doubt at the time that the sporadic cases of purulent bronchitis and bronchopneumonia described in the winters of 1916 to 1918 reflected the same process as some aspects of the influenza pandemic.
Hammond and colleagues described a series of fatal cases of purulent bronchitis in February and early March 1917, this accounting for 71 out of 156 consecutive autopsies.26 The changes were most marked in the smaller bronchi which were filled with pus, and whose epithelium, initially intact, was shed and replaced by inflamed granulation tissue. In some, but not all patients, the inflammatory process had spread to adjacent lung parenchyma giving bronchopneumonia. The influenza bacillus (Haemophilus influenzae) could be identified on gram-staining, but this of course was not the primary causative agent. Similar findings were reported from Aldershot, from Canadian troops at Boulogne and from American recruits in camps in Texas and Iowa in the winter of 1917 to 1918. Notably, an infiltrate of mononuclear cells, especially small lymphocytes, occurred within the bronchial wall. In time, it was shown by Abrahams and colleagues, who had reported the Aldershot cases, that the changes of purulent bronchitis were identical to the post-mortem findings in fatal cases of influenza.27
These contemporary descriptions of the pathological findings of influenza are only a small part of the story. They are a description of post-mortem findings of patients who died as a result of bacterial infections of the bronchi and lungs, which were secondary phenomena, and were complications of the primary viral illness. The viral cause was not isolated until 1933.
There were two waves in the 1918 Spanish Influenza pandemic, the first in the spring, and the second in the autumn. This in itself is unusual, most influenza outbreaks occurring in the winter months. The spring outbreak followed the expected course, causing complications in the very young, immunologically immature, and in the very old, immunologically compromised. Secondary purulent bronchitis and broncho-pneumonia were responsible for deaths in these two groups, and the contemporary pathological descriptions outlined above apply to victims of this wave. Young, fit individuals usually dealt with the disease without difficulty.
The second autumn wave was much deadlier, the virus having mutated to a lethal form. This time, it behaved in a very different way, affecting particularly strong, fit, young individuals causing a significant mortality in that young adult group. It also killed them very quickly, with descriptions of soldiers being well one day, and dying the next, drowning in their own secretions. It may well have represented a strong immune response to the virus, the very strength and vigour of the response ironically causing release of inflammatory mediators in what may be described as a “cytokine storm” resulting in pulmonary oedema and death. Post-mortem studies revealed a “wet lung” sometimes with haemorrhagic appearances. This may be described as an adult respiratory distress syndrome described elsewhere in this book.
The spread of this deadly mutant was assisted by the circumstances of the war. In civilian life, those who get very sick stay at home, isolating themselves. During the Great War, those who became very sick were sent on crowded trains to even more crowded general hospitals, concentrating the deadlier virus in these locations, and thus facilitating its spread amongst the troops, and carried to all parts of the world from that dense reservoir of deadly virus.
It is particularly ironic, given the terrible wounds inflicted by high explosive shells and bullets, in what was an appalling illustration of the destructive effects of industrial warfare, that it should be a disease that carried off more people worldwide than all the ordnance that belligerent nations could hurl at each other.
In conclusion, pathology services during the Great War made a very important contribution to the war effort. They did so firstly in the day-to-day service provided by mobile and hospital laboratories. Of particular importance, an understanding of the pathology of abdominal wounding led to improved management of these patients, with better chances of survival. Secondly, pathology research laboratory facilities gave brilliant scientific minds an opportunity to develop new ideas, and make original contributions to the clinical problems encountered during four years of conflict. Young Alexander Fleming, working in Colonel Sir Almroth Wright’s research unit at No13 General Hospital in Boulogne, would go on in later years to make a major impact on management of wounds in the Second World War. He would discover penicillin.
1 McInnis, W.D., W. Egan & J.B. Oust. “The management of carcinoma of the larynx in a prominent patient, or did Morell Mackenzie really cause World War I?”, American Journal of Surgery 1976; 132: pp.515-22.
2 Atenstaedt, R.L., “The development of bacteriology, sanitation science and allied research in the British Army 1850-1918: equipping the RAMC for War”, Journal of the Royal Army Medical Corps, 2010; 156: pp.154-8.
3 Cushing, H., The Life of Sir William Osler Volume 2. Oxford: Oxford University Press, 1925, pp.427-428.
4 Mitchell, T.J. & G.M. Smith, History of the Great War based on Official Documents. Medical Services. Casualties and Medical Statistics. London: HMSO, 1931, p.270.
5 Bewsher, F.W., The History of the 51st (Highland) Division. Edinburgh: Blackwood, 1921, pp.4-5.
6 Mitchell & Smith, op.cit, p.74.
7 Ibid, p.78.
8 MacPherson, W.G., S.L. Cummins & W.B. Leishman (eds.), History of the Great War based on Official Documents. Medical Services. Pathology. London: HMSO, 1923.
9 McNee, J.W. & J.S. Dunn, “The method of spread of gas gangrene into living muscle”, British Medical Journal 1917; 1: pp.727–729.
10 Titball, R.W., “Gas gangrene: an open and closed case”, Microbiology 2005; 151: pp.2821–2828.
11 Graham, J.H.P., “A note on a relapsing febrile illness of unknown origin”, The Lancet 1915; ii: pp.703-4.
12 Hunt, G.H. & A.C. Rankin, “Intermittent fever of obscure origin occurring among British soldiers in France. The so-called “trench fever””, The Lancet 1915; ii: pp.1133-6.
13 McNee, J.W., A. Renshaw & E.H. Brunt, “Trench Fever”, British Medical Journal 1916; 1: pp.225-234.
14 Ibid.
15 Foucault, C., K. Barrau, P. Brouqui & D. Raoult, “Bartonella quintana bacteraemia among homeless people”, Clinical Infectious Diseases 2002; 35: pp.684-9.
16 Raoult, D., O. Dutour, L. Houhamdi, R. Jankauskas, P.E. Fournier, Y. Ardagna et al. “Evidence for louse-transmitted diseases in soldiers of Napoleon’s Grand Army in Vilnius”, Journal of Infectious Diseases 2006; 193: pp.112-20.
17 Maurin, M. & D. Raoult, “Bartonella (Rochalimaea) quintana infections”, Clinical Microbiology Reviews 1996; 9: pp.273-92.
18 Raw, N., “Trench nephritis. A record of five cases”, British Medical Journal 1915; 2: p.468.
19 Dunn, J.S. & J.W. McNee, “A contribution to the study of war nephritis”, British Medical Journal 1917; 2: pp.745-51.
20 Atenstaedt, R.L., “The medical response to trench nephritis in World War One”, Kidney International 2006; 70: pp.635–640.
21 Stansbury, L.G. & J.R. Hess, “Blood Transfusion in World War I: The Roles of Lawrence Bruce Robertson and Oswald Hope Robertson in the ‘Most Important Medical Advance of the War’”, Transfusion Medicine Reviews 2009; 23: pp.232-236.
22 Robertson, L.B., “The transfusion of whole blood. A suggestion for its more frequent employment in war surgery”, British Medical Journal 1916; 2: pp.38-40.
23 Robertson, O.H., “Transfusion with preserved red blood cells”, British Medical Journal 1918; 1: pp.691-695.
24 Guiou, N.M., “Blood transfusion in a field ambulance”, British Medical Journal 1918; 1: pp.695-696.
25 Oxford, J.S., R. Lambkin, A. Sefton A., “A hypothesis: the conjunction of soldiers, gas, pigs, ducks, geese and horses in Northern France during the Great War provided the conditions for the emergence of the “Spanish” Influenza pandemic of 1918-1919”, Vaccine 2005; 23: pp.940–945.
26 Hammond, J.A.R., W. Rolland & T.H.G. Shore, “Purulent Bronchitis: a Study of Cases Occurring amongst the British Troops at a Base in France”, The Lancet 1917; 2: pp.41–45.
27 Abrahams, A., N. Hallows & H. French, “A further investigation into Influenza Pneumococcal and Influenza Streptococcal Septicaemia: Epidemic Influenza Pneumonia of highly fatal type and its relation to Purulent Bronchitis”, The Lancet 1919; 1: pp.1–9.