CHAPTER 21 NATUROPATHIC MEDICINE
The doctor of the future will give no medicine, but will interest his patient in the care of the human frame, in diet and in the cause and prevention of disease.
This section describes the background, context, and clinical approaches of select alternative therapeutic systems as developed throughout European and American history. These chapters describe individual approaches as suggested from contemporary Western research, both within and beyond the biomedical paradigm. Where these systems and approaches can be understood in light of the contemporary biomedical paradigm, this view is examined; where they cannot be understood in these terms, this paradox is addressed. When and how these medical systems are embedded in the natural curative environment is clarified, as well as when and how they are embedded in technology. In each case, these medical practices are presented as products of history that make sense in terms of that history.
For example, homeopathy is a highly systematized method of healing that utilizes the principle of “use likes to treat likes” practiced by licensed physicians and other health care professionals throughout the world. In the United States, homeopathic medicines are protected by federal law, and most are available over the counter. The greatest challenge that homeopathy may pose to conventional medicine and science is the common use of extremely diluted medicinal substances.
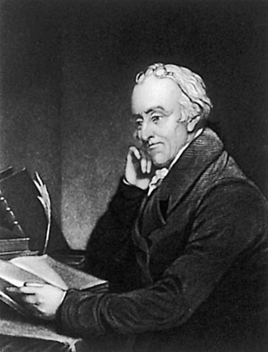
Thomas Edison’s insightful prediction is proving true today, as natural medicine finds itself in the midst of an unprecedented explosion into mainstream health care. Consumers are spending more annually out of pocket for alternative medicine than for conventional care. In particular, naturopathic medicine as the model for integrative primary care natural medicine is undergoing a powerful resurgence. With its unique integration of vitalistic, scientific, academic, and clinical training in medicine, the naturopathic medical model is a potent contributing factor to this health care revolution.
HISTORY OF “REGULAR” MEDICINE AND NATUROPATHIC MEDICINE*
“Regular” Medicine
Conventional or “regular” medicine and natural medicine have shaped and helped to define each other throughout history, often in reaction, and perhaps nothing has had as much influence on naturopathic medicine as the rise of regular medicine. Much as naturopathic doctors today may trace some of their roots to Hippocrates, regular physicians also generally consider his view of health and disease to have contributed to the basis of today’s medicine, primarily because of his rejection of supernatural or divine forces as the cause of illness, which resulted in the transition to a more physiological and rational approach to wellness. However, in contrast to naturopathic medicine, for which it is a core belief, regular medicine has come to reject Hippocrates’ concept of the healing power of nature, a principle that may have done more to define and shape naturopathic medicine than anything else.
Of course regular medicine has made extraordinary leaps since the time of Hippocrates, particularly during the last century, and many aspects of today’s education, scientific understanding, and therapeutic modalities would be unrecognizable to an MD only 100 years ago. We have also seen an unprecedented explosion in the size and role of the health care system in the United States, with over 800,000 MDs practicing as of the year 2000 (American Medical Association, n.d.), and $2.1 trillion spent on health care in 2006 (U.S. Department of Health and Human Services, n.d.). By comparison, in the year 1800 there were only 200 graduates of the elite medical schools in the United States, along with 300 immigrants with European diplomas (Kaptchuk et al, 2001). The consistent thread that ties the regular doctors of the past to those practicing today may be a philosophy of allegiance to scientific principles and adoption of a basic biomedical orientation to illness, but coupled with disregard for the body’s innate healing capacity.
In the European countries from which American medical education was derived, medicine first became institutionalized in the twelfth and thirteenth centuries, following a low ebb during the Dark Ages of ad 500 to 1050. Sarleno, Italy, was one of the earliest centers of medical training, followed by universities in Paris and England, where some of the first hospitals were built (Cruse, 1999). Although a graduate from Oxford in the 1500s had received up to 14 years of university education, very poor training was offered in the practice of medicine and patient care (Magee, 2004). When the Enlightenment arrived at the far reaches of Europe in Scotland it was a mature intellectual movement emphasizing observation (empiricism) and reason (rationality). The Scottish Enlightenment of the eighteenth century produced advancements in thinking about economics (Adam Smith, The Wealth of Nations, 1776) and law (David Hume) as well as the roots of the Industrial Revolution with the application of the steam engine (James Watt), based on principles used for the steam distillation of scotch whiskey. The “rational medicine” movement was embodied in the school of medicine at the University of Edinburgh from whence Drs. William Hutchison and John Morgan came to establish the first school of medicine in the United States in 1767 at the College of Philadelphia (now the University of Pennsylvania), following the establishment of the first hospital in the nation by Benjamin Franklin and Dr. Thomas Bond during the prior decade in 1752 (Figure 21-1).

Figure 21-1 Pennsylvania Hospital, the nation’s first hospital, founded in 1752.
(Courtesy the Pennsylvania Hospital, Philadelphia.)
In general, however, in the 1700s little had improved—doctors had limited diagnostic ability, and aside from feeling the pulse, inspecting the tongue, and examining the urine and stool, physicians did not touch their patients and often did not even see them (Magee, 2004). There were no consistent theories to explain the cause of illness, nor could the modalities used to treat them be agreed upon. As a result the medical landscape in the 1800s remained incredibly diverse.
This situation was not inconsistent with the political climate at the time, however. Like today, the cultural values of the early nineteenth century greatly influenced the practice of medicine. In the era of “Jacksonian democracy,” beginning in the late 1820s, American society had begun to reject any form of “elitism,” and the “elites” often included physicians, in large part because regular doctors were mostly available only to the wealthy in society (see Box 1-2). Much of the public harbored a fervent antiintellectualism coupled with belief in the tenet of economic freedom. As a consequence, laws controlling medical practice were viewed by the public as a form of class legislation; a general belief that citizens should have the right to choose their own medical care was combined with a distrust of the motives of “regular physicians” (Ober, 1997). Medical licensing became effectively irrelevant. For most of America’s Colonial period, anyone could practice medicine, without a license, regardless of qualification or training. By 1850, all but two states had removed medical licensing statutes from the books (Whorton, 2002). Numerous conflicting claims of efficacy were made by a variety of practitioners, and an intense and heated competition often left patients confused by and dissatisfied with their experience with all types of physicians. The result has been described as both “medical anarchy” (Ober, 1997) and “a war zone” (Kaptchuk, 2001). Because regular medicine was often ineffective and frequently toxic, many patients and physicians defected to other “alternatives.”
Partially in response, and after prior attempts, in 1847 a group of physicians founded an organization to serve as the unifying body for orthodox medical practitioners, the American Medical Association (AMA). Physicians who belonged to the AMA considered themselves regular practitioners and adhered to therapeutics termed heroic medicine (Rutkow, 2004). It was their treatments that may have most distinguished these regular doctors to their patients, because these often consisted of bleeding and blistering in addition to administering harsh concoctions to induce vomiting and purging, treatments that at the time were considered state of the art. The motivation behind such harsh treatments was a commitment to medical theory and a move away from empirically based medicine. Also, because regular doctors did not share belief in the concept of the healing power of nature (the vis medicatrix naturae), they felt that a physician’s duty was to provide active, “heroic” intervention. Because the majority of patients recovered notwithstanding their treatments, this had the ironic effect of encouraging both regular doctors’ belief in heroic treatments and irregulars’ belief in the inborn capacity for self-healing, despite the further injuries caused by many regular treatments. Much like physicians today are pressured to provide an active treatment that may sometimes be unnecessary (such as an antibiotic for a viral infection), regular doctors of the 1800s also felt pressure to give the heroic treatments for which they were known. As James Whorton (2002) writes, “it was only natural for MDs to close ranks and cling more tightly to that tradition as a badge of professional identity, making depletive therapy the core of their self-image as medical orthodoxy.”
Although the AMA initially held no legal authority, it began a major push during the second half of the nineteenth century to create legislation and standards of medical education and competency. This process culminated in 1910 with the publication of Medical Education in the United States and Canada, compiled by Abraham Flexner (Figure 21-2), also known as the Flexner Report. It has been described as “a bombshell that rattled medical and political forces throughout the country” (Petrina, 2008). It criticized the medical education of its era as a loose and poorly structured apprenticeship system that generally lacked any defined standards or goals beyond commercialism (Ober, 1997). In some of his specific accounts, Flexner described medical institutions as “utterly wretched . . . without a redeeming feature” and as “a hopeless affair” (Whorton, 2002). Many of the regular medical institutions were rated poorly, and most of the irregular schools fared the worst. After this report, nearly half of the medical schools in the country closed, and by 1930 the remaining schools had 4-year programs of rigorous “scientific medicine.”
Following the Flexner Report a tremendous restructuring of medical education and practice occurred. The remaining medical schools experienced enormous growth: in 1910 a leading school might have had a budget of $100,000; by 1965 it was $20 million and by 1990 it could have been $200 million or more (Ludmerer, 1999). Faculty were now called upon to engage in original research, and students not only studied a curriculum with a heavy emphasis on science, but also engaged in active learning by participating in real clinical work with responsibility for patients. Hospitals became the locus for clinical instruction. As scientific discovery began to accelerate, these higher educational standards helped to bridge the gap between what was known and what was put into practice, and more stringent licensing provided a greater degree of confidence in the competence of the nation’s doctors. During this same time period, the suppression and decline of alternative schools of health care occurred, as both public and political pressure increased.
The post-World War II era has been one of undeniable and astonishing achievements by scientific medicine, which has coincided with great strides in public health, sanitation, and living conditions. As understanding of basic clinical science has grown, the biomedical model has continued to evolve, and so has the capacity to make accurate diagnoses and interventions. Today’s physician faces new challenges, however, and some of the deficiencies of regular doctors in the past have reared their heads once again. In an era of managed care and health maintenance organizations, it has become increasingly difficult for physicians to spend quality time with patients or to focus on preventative medicine, and the treatment of chronic disease has suffered. Also, physicians must be vigilant against the constant and insidious efforts of the pharmaceutical industry to corrupt medical science, education, and practice for commercial gain. In addition, the increase in specialization and the decline of primary care is a growing problem that shows no sign of slowing. Today’s regular doctors are also not easily defined—they have been referred to as “mainstream,” “orthodox,” “conventional,” “allopathic,” “scientific,” and “authoritarian,” all of which have their own positive and negative connotations, and none is universally accepted or accurate as individual MDs are more and more becoming receptive to developing new “integrative” models of health care (Berkenwald, 1998; Kaptchuk, 2001). It is also increasingly being recognized that although regular doctors have presented themselves as the “scientific” branch of medicine throughout recent history, the mantle of science cannot be claimed or exclusively worn by any one field of medicine, and integration of various medical specialties and philosophies benefits all.
A pluralistic health care setting is reemerging. Optimally, it will value the organization, structure, and science-based approach of regular medicine, along with qualities regular medicine has typically been lacking, including a patient-centered and individualized care that reaffirms the importance of the relationship between practitioner and patient, recognition and support of innate healing systems, and a broadening of the scientific approach to allow for the evaluation and incorporation of traditional and natural medicines into current health care delivery in a way that makes use of all appropriate therapeutic approaches, health care professionals, and disciplines. “We find ourselves,” John Weeks, the editor of The Integrator, wrote recently, “in an era beyond the polarization of alternative medicine and conventional medicine,” with “an opportunity to become a seamless part of an integrated system that might rightfully be called, simply, health care” (The Integrator Blog, n.d.).
Although naturopathic medicine traces its philosophical roots to many traditional world medicines, its body of knowledge derives from a rich heritage of writings and practices of Western and non-Western nature doctors since Hippocrates (circa 400 bc). Modern naturopathic medicine grew out of healing systems of the eighteenth and nineteenth centuries. The term naturopathy was coined in 1895 by Dr. John Scheel of New York City to describe his method of health care. However, earlier forerunners of these concepts already existed in the history of natural healing, both in America and in the Austro-Germanic European core. Naturopathy became a formal profession after its creation by Benedict Lust in 1896. The profession has now celebrated its 115th birthday.
Over the centuries, natural medicine and conventional medicine have alternately diverged and converged, shaping each other, often in reaction. During the past hundred years the naturopathic profession progressed through several fairly distinct phases, as follows:
The per capita supply of alternative medicine clinicians (chiropractors, naturopaths and practitioners of Oriental medicine) will grow by 88% between 1994 and 2010, while allopathic physician supply will grow by 16%. . . . The total number of naturopathy graduates will double over the next five years. The total number of naturopathic physicians will triple” (Cooper et al, 1996).
Founding of Naturopathy
Naturopathy, as a generally used term, began with the teachings and concepts of Benedict Lust. In 1892, at age 23, Lust came from Germany as a disciple of Father Sebastian Kneipp (the greatest practitioner of hydrotherapy) to bring Kneipp’s hydrotherapy practices to America. Exposure in the United States to a wide range of practitioners and practices of natural healing arts broadened Lust’s perspective, and after a decade of study, in 1902 he purchased the term naturopathy from Scheel of New York City (who coined the term in 1895) to describe the eclectic compilation of doctrines of natural healing that he envisioned was to be the future of natural medicine. Naturopathy, or “nature cure,” was defined by Lust as both a way of life and a concept of healing that used various natural means (selected from various systems and disciplines) of treating human infirmities and disease states. The earliest therapies associated with the term involved a combination of American hygienics and Austro-Germanic nature cure and hydrotherapy.
In January 1902, Lust, who had been publishing the Kneipp Water Cure Monthly and its German-language counterpart in New York since 1896, changed the name of the journal to The Naturopathic and Herald of Health and began promoting a new way of thinking of health care with the following editorial:
We believe in strong, pure, beautiful bodies . . . of radiating health. We want every man, woman and child in this great land to know and embody and feel the truths of right living that mean conscious mastery. We plead for the renouncing of poisons from the coffee, white flour, glucose, lard, and like venom of the American table to patent medicines, tobacco, liquor and the other inevitable recourse of perverted appetite. We long for the time when an eight-hour day may enable every worker to stop existing long enough to live; when the spirit of universal brotherhood shall animate business and society and the church; when every American may have a little cottage of his own, and a bit of ground where he may combine Aerotherapy, Heliotherapy, Geotherapy, Aristophagy and nature’s other forces with home and peace and happiness and things forbidden to flat-dwellers; when people may stop doing and thinking and being for others and be for themselves; when true love and divine marriage and pre-natal culture and controlled parenthood may fill this world with germ-gods instead of humanized animals.
In a word, Naturopathy stands for the reconciling, harmonizing and unifying of nature, humanity and God.
Fundamentally therapeutic because men need healing; elementary educational because men need teaching; ultimately inspirational because men need empowering.
Benedict Lust
According to his published personal history, Lust had a debilitating condition in his late teens while growing up in Michelbach, Baden, Germany, and had been sent by his father to undergo the Kneipp cure at Woerishofen. He stayed there from mid-1890 to early 1892. Not only was he “cured” of his condition, but he became a protégé of Father Kneipp. He emigrated to America to proselytize the principles of the Kneipp water cure (Figure 21-3).
Figure 21-3 Curative baths, one form of hydrotherapy, were a popular form of natural healing in the late nineteenth century.
(Courtesy Wellcome Institute Library, London.)
By making contact in New York with other German Americans who were also becoming aware of the Kneipp principles, Lust participated in the founding of the first “Kneipp Society,” which was organized in Jersey City, New Jersey, in 1896. Subsequently, through Lust’s organization and contacts, Kneipp societies were also founded in Brooklyn, Boston, Chicago, Cleveland, Denver, Cincinnati, Philadelphia, Columbus, Buffalo, Rochester, New Haven, San Francisco, the state of New Mexico, and Mineola on Long Island. The members of these organizations were provided with copies of the Kneipp Blatter and a companion English publication Lust began to put out called The Kneipp Water-Cure Monthly. In 1895 Lust opened the Kneipp Water-Cure Institute on 59th Street in New York City.
Father Kneipp died in Germany, at Woerishofen, on June 17, 1897. With his passing, Lust was no longer bound strictly to the principles of the Kneipp water cure. He had begun to associate earlier with other German American physicians, principally Dr. Hugo R. Wendel (a German-trained “Naturarzt”) who began, in 1897, to practice in New York and New Jersey as a licensed osteopathic physician. Lust entered the Universal Osteopathic College of New York in 1896 and became licensed as an osteopathic physician in 1898.
Once he was licensed to practice as a health care physician in his own right, Lust began the transition toward the concept of “naturopathy.” Between 1898 and 1902, when he adopted the term naturopath, Lust acquired a chiropractic education; changed the name of his Kneipp Store (which he had opened in 1895) to “Health Food Store” (the first facility to use that name and concept in the United States), specializing in providing organically grown foods and the materials necessary for drugless cures; and founded the New York School of Massage (in 1896) and the American School of Chiropractic.
In 1902, when he purchased and began using the term naturopathy and calling himself a “naturopath,” Lust, in addition to operating his New York School of Massage and American School of Chiropractic, issuing his various publications, and running his Health Food Store, began to operate the American School of Naturopathy. All these activities were carried out at the same 59th Street address. By 1907, Lust’s enterprises had grown sufficiently large that he moved them to a 55-room building. It housed the Naturopathic Institute, Clinic, and Hospital; the American School of Naturopathy and American School of Chiropractic; the establishment now called the Original Health Food Store; Lust’s publishing enterprises; and the New York School of Massage. The operation remained in this four-story building, roughly twice the size of the original facility, from 1907 to 1915.
From 1912 through 1914, Lust took a sabbatical from his operations to further his own education. By this time he had founded his large estatelike sanitarium at Butler, New Jersey, known as Yungborn after the German sanitarium operation of Adoph Just. In 1912 he began attending the Homeopathic Medical College in New York, which granted him a degree in homeopathic medicine in 1913 and a degree in eclectic medicine in 1914. In early 1914, Lust traveled to Florida and obtained an MD’s license on the basis of his graduation from the Homeopathic Medical College.
From 1902, when he began to use the term naturopathy, until 1918, Lust replaced the Kneipp societies with the Naturopathic Society of America. Then in December 1919, the Naturopathic Society of America was formally dissolved because of insolvency, and Lust founded the American Naturopathic Association. Thereafter, the association was incorporated in some additional 18 states. Lust claimed at one time to have 40,000 practitioners practicing naturopathy. In 1918, as part of his effort to dissolve the Naturopathic Society of America (an operation into which he invested a great deal of his funds and resources in an attempt to organize a naturopathic profession) and replace it with the American Naturopathic Association, Lust published the first Yearbook of Drugless Therapy. Annual supplements were published in either The Naturopath and the Herald of Health or its companion publication, Nature’s Path (which began publication in 1925), with which The Naturopath at one time merged. The Naturopath and Herald of Health, sometimes printed with the two phrases reversed, was published from 1902 through 1927, and from 1934 until after Lust’s death in 1945.
Benedict Lust’s principles of health are found in the introduction to the first volume of the Universal Naturopathic Directory and Buyer’s Guide, a portion of which is reproduced in Box 21-1. Although the terminology is almost a century old, the concepts Lust proposed have provided a powerful foundation that has endured despite almost a century of active political suppression by the dominant school of medicine.
BOX 21-1 Principles, Aim, and Program of the Nature Cure System
From Lust B: Principles of health, vol 1, Universal naturopathic directory and buyer’s guide, Butler, NJ, 1918, Lust Publications.
Since the earliest ages, medical science has been of all sciences the most unscientific. Its professors, with few exceptions, have sought to cure disease by the magic of pills and potions and poisons that attacked the ailment with the idea of suppressing the symptoms instead of attacking the real cause of the ailment.
Medical science has always believed in the superstition that the use of chemical substances that are harmful and destructive to human life will prove an efficient substitute for the violation of laws, and in this way encourages the belief that a man may go the limit in self-indulgences that weaken and destroy his physical system, and then hope to be absolved from his physical ailments by swallowing a few pills, or submitting to an injection of a serum or vaccine, that are supposed to act as vicarious redeemers of the physical organism and counteract life-long practices that are poisonous and wholly destructive to the patient’s well-being.
The policy of expediency is at the basis of medical drug healing. It is along the lines of self-indulgence, indifference, ignorance and lack of self-control that drug medicine lives, moves and has its being.
The natural system for curing disease is based on a return to nature in regulating the diet, breathing, exercising, bathing and the employment of various forces to eliminate the poisonous products in the system, and so raise the vitality of the patient to a proper standard of health.
Official medicine has, in all ages, simply attacked the symptoms of disease without paying any attention to the causes thereof, but natural healing is concerned far more with removing the causes of disease, than merely curing its symptoms. This is the glory of this new school of medicine that it cures by removing the causes of the ailment, and is the only rational method of practicing medicine. It begins its cures by avoiding the uses of drugs and hence is styled the system of drugless healing.
The Program of Naturopathic Cure
Natural healing is the most desirable factor in the regeneration of the race. It is a return to nature in methods of living and treatment. It makes use of the elementary forces of nature, of chemical selection of foods that will constitute a correct medical dietary. The diet of civilized man is devitalized, is poor in essential organic salts. The fact that foods are cooked in so many ways and are salted, spiced, sweetened and otherwise made attractive to the palate, induces people to over-eat, and over eating does more harm than under feeding. High protein food and lazy habits are the cause of cancer, Bright’s disease, rheumatism and the poisons of autointoxication.
There is really but one healing force in existence and that is Nature herself, which means the inherent restorative power of the organism to overcome disease. Now the question is, can this power be appropriated and guided more readily by extrinsic or intrinsic methods? That is to say, is it more amenable to combat disease by irritating drugs, vaccines and serums employed by superstitious moderns, or by the bland intrinsic congenial forces of Natural Therapeutics, that are employed by this new school of medicine, that is Naturopathy, which is the only orthodox school of medicine? Are not these natural forces much more orthodox than the artificial resources of the druggist?
Schools of Thought That Formed the Philosophical Basis of Naturopathy
Because of the eclectic nature of naturopathic medicine, its history is by far the most complex of any healing art, which explains the unusually large portion of this chapter devoted to this subject. Although the following discussion is divided into distinct schools of thought, this is somewhat artificial, because those who founded and practiced these arts (especially the Americans) were often trained in, influenced by, and practiced several therapeutic systems or modalities. It was not until Benedict Lust, however, that the many threads were woven together into a unified professional practice, which makes naturopathic medicine the first Western system of full-scope integrative natural medicine based on the vis medicatrix naturae. Organized around this principle of the human capacity for healing, naturopathic medicine has been able to discriminately integrate diverse therapeutic systems and modalities into a cohesive framework, acknowledging the biomedical model of health and illness, but also supporting the whole person, including the psychological, social, and spiritual aspects of wellness. It has consistently promoted a patient-centered relationship, as well as collaboration with other health care professionals and disciplines, and today is poised as a model for integrative medicine. Although it draws from the eclectic tradition (see later), it does not do so randomly or indiscriminately. Rather, core principles, such as the vis medicatrix naturae, guide its flexible but solid structure, allowing it to navigate, perhaps uniquely, today’s medical world.
The following presents the formative schools of Western thought in natural healing and some of their leading adherents. Although the therapies differ, the philosophical thread of promoting health and supporting the body’s own healing processes runs through them all. These threads are derived from centuries of medical scholarship, both Western and non-Western, concerning the self-healing process.
After a brief overview of Hippocrates’ seminal contribution to the natural medicine way of thought, the basic themes are presented in the following order: healthful living; natural diet; detoxification; exercise, mechanotherapy, and physical therapy; mental, emotional, and spiritual healing; and natural therapeutic agents. Hippocrates and centuries of nature doctors’ writings remain empirically rich repositories of observations for future research.
Hippocrates
Prehistoric people believed that disease was caused by magic or supernatural forces, such as devils or angry gods. Hippocrates, breaking with this superstitious belief, became the first naturalistic doctor in recorded history. Hippocrates regarded the body as a “whole” and instructed his students to prescribe only beneficial treatments and refrain from causing harm or hurt.
Hippocratic practitioners assumed that everything in nature had a rational basis; therefore the physician’s role was to understand and follow the laws of the intelligible universe. They viewed disease as an effect and looked for its cause in natural phenomena: air, water, food, and so forth. They first used the term vis medicatrix naturae, the “healing power of nature,” to denote the body’s ability and drive to heal itself. One of the central tenets is that “there is an order to the process of healing which requires certain things to be done before other things to maximize the effectiveness of the therapeutics” (Zeff, 1997). The step order used by Tibetan medicine is also an example of the representation of this tenet in traditional world medicines.
Hydrotherapy
The earliest philosophical origins of naturopathy were clearly in the Germanic hydrotherapy movement: the use of hot and cold water for the maintenance of health and the treatment of disease. One of the oldest known therapies (water was used therapeutically by the Romans and Greeks), hydrotherapy began its modern history with the publication of The History of Cold Bathing in 1697 by Sir John Floyer. Probably the strongest impetus for its use came from Central Europe, where it was advocated by such well-known hydropaths as Priessnitz, Schroth, and Father Kneipp. They were able to popularize specific water treatments that quickly became the vogue in Europe during the nineteenth century. Vinzenz Priessnitz (1799-1851), of Graefenberg, Silesia, was a pioneer natural healer. Unfortunately, he was prosecuted by the medical authorities of his day and was actually convicted of using witchcraft because he cured his patients by the use of water, air, diet, and exercise. He took his patients back to nature—to the woods, the streams, the open fields—treated them with nature’s own forces, and fed them on natural foods. His cured patients numbered in the thousands, and his fame spread over Europe. Father Sebastian Kneipp (1821-1897) became the most famous of the hydropaths, with Pope Leo XIII and Ferdinand of Austria (whom he had walking barefoot in new-fallen snow for the purposes of hardening his constitution) among his many famous patients. He standardized the practice of hydrotherapy and organized it into a system of practice that was widely emulated through the establishment of health spas or “sanitariums.” The first sanitarium in this country, the Kneipp and Nature Cure Sanitarium, was opened in Newark, New Jersey, in 1891.
The best-known American hydropath was J.H. Kellogg, a medical doctor who approached hydrotherapy scientifically and performed many experiments trying to understand the physiological effects of hot and cold water. In 1900 he published Rational Hydrotherapy, which is still considered a definitive treatise on the physiological and therapeutic effects of water, along with an extensive discussion of hydrotherapeutic techniques. Drs. O.J. Carroll, Harold Dick, and John Bastyr, among others, brought the use of hydrotherapy techniques forward into modern naturopathic practice.
Nature Cure
Natural living, consumption of a vegetarian diet, and the use of light and air formed the basis of the nature cure movement founded by Dr. Arnold Rickli (1823-1926). In 1848 he established at Veldes Krain, Austria, the first institution of light and air cure or, as it was called in Europe, the atmospheric cure. He was an ardent disciple of the vegetarian diet and the founder, and for more than 50 years the president, of the National Austrian Vegetarian Association. In 1891, Louis Kuhne (ca. 1823-1907) wrote the New Science of Healing, which presented the basic principles of “drugless methods.” Dr. Henry Lahman (ca. 1823-1907), who founded the largest nature cure institution in the world at Weisser Hirsch, near Dresden, Saxony, constructed the first appliances for the administration of electric light treatment and baths. He was the author of several books on diet, nature cure, and heliotherapy. Professor F.E. Bilz (1823-1903) authored the first natural medicine encyclopedia, The Natural Method of Healing, which was translated into a dozen languages, and in German alone ran into 150 editions.
Nature cure became popular in America through the efforts of Henry Lindlahr, MD, ND, of Chicago, Illinois. Originally a rising businessman in Chicago with all the bad habits of those in the Gay Nineties era, he became chronically ill while only in his thirties. After receiving no relief from the orthodox practitioners of his day, he learned of nature cure, which improved his health. Subsequently, he went to Germany to stay in a sanitarium to be cured and to learn nature cure. He went back to Chicago and earned his degrees from the Homeopathic/Eclectic College of Illinois. In 1903 he opened a sanitarium in Elmhurst, Illinois; established Lindlahr’s Health Food Store; and shortly thereafter founded the Lindlahr College of Natural Therapeutics. In 1908 he began to publish Nature Cure Magazine and began publishing his six-volume series of Philosophy of Natural Therapeutics.
One of the chief advantages of training in the early 1900s was the marvelous inpatient facilities that flourished during this time. These facilities provided in-depth training in clinical nature cure and natural hygiene in inpatient settings. Nature cure and natural hygiene are still at the core of naturopathic medicine’s fundamental principles and approach to health care and disease prevention.
The Hygienic System
Another forerunner of American naturopathy, the “hygienic” school, amalgamated the hydrotherapy and nature cure movements with vegetarianism. It originated as a lay movement of the nineteenth century and had its genesis in the popular teachings of Sylvester Graham and William Alcott. Graham began preaching the doctrines of temperance and hygiene in 1830 and in 1839 published Lectures on the Science of Human Life, two hefty volumes that prescribed healthy dietary habits. He emphasized a moderate lifestyle, a flesh-free diet, and bran bread as an alternative to bolted or white bread. The earliest physician to have a significant impact on the hygienic movement and the later philosophical growth of naturopathy was Russell Trall, MD. According to Whorton (1982) in his Crusaders for Fitness,
The exemplar of the physical educator-hydropath was Russell Thatcher Trall. Still another physician who had lost his faith in regular therapy, Trall opened the second water cure establishment in America, in New York City in 1844. Immediately, he combined the full Priessnitzian armamentarium of baths with regulation of diet, air, exercise and sleep. He would eventually open and or direct any number of other hydropathic institutions around the country, as well as edit the Water-Cure Journal, the Hydropathic Review, and a temperance journal. He authored several books, including popular sex manuals which perpetuated Graham-like concepts into the 1890’s, sold Graham crackers and physiology texts at his New York office, was a charter member (and officer) of the American Vegetarian Society, presided over a short-lived World Health Association, and so on.
Trall established the first school of natural healing arts in this country to have a 4-year curriculum and the authorization to confer the degree of MD. It was founded in 1852 as a “Hydropathic and Physiological School” and was chartered by the New York State Legislature in 1857 under the name New York Hygio-Therapeutic College.
Trall eventually published more than 25 books on the subjects of physiology, hydropathy, hygiene, vegetarianism, and temperance, among many others. The most valuable and enduring of these was his 1851 Hydropathic Encyclopedia, a volume of nearly 1000 pages that covered the theory and practice of hydropathy and the philosophy and treatment of diseases advanced by older schools of medicine. The encyclopedia sold more than 40,000 copies.
Martin Luther Holbrook expanded on the work of Graham, Alcott, and Trall and, working with an awareness of the European concepts developed by Priessnitz and Kneipp, laid further groundwork for the concepts later advanced by Lust, Lindlahr, and others. According to Whorton (1982), Holbrook proposed the following:
For disease to result, the latter had to provide a suitable culture medium, had to be susceptible. As yet, most physicians were still so excited at having discovered the causative agents of infection that they were paying less than adequate notice to the host. Radical hygienists, however, were bent just as far in the other direction. They were inclined to see bacteria as merely impotent organisms that throve only in individuals whose hygienic carelessness had made their body compost heaps. Tuberculosis is contagious, Holbrook acknowledged, but “the degree of vital resistance is the real element of protection. When there is no preparation of the soil by heredity, predisposition or lowered health standard, the individual is amply guarded against the attack.” A theory favored by many others was that germs were the effect of disease rather than its cause; tissues corrupted by poor hygiene offered microbes, all harmless, an environment in which they could thrive.
The orthodox hygienists of the progressive years were equally enthused by the recent progress of nutrition, of course, and exploited it for their own naturopathic doctors, but their utilization of science hardly stopped with dietetics. Medical bacteriology was another area of remarkable discovery, bacteriologists having provided, in the short space of the last quarter of the nineteenth century, an understanding, at long last, of the nature of infection. This new science’s implications for hygienic ideology were profound—when Holbrook locked horns with female fashion, for example, he did not attack the bulky, ground-length skirts still in style with the crude Grahamite objection that the skirt was too heavy. Rather he forced a gasp from his readers with an account of watching a smartly dressed lady unwittingly drag her skirt “over some virulent, revolting looking sputum, which some unfortunate consumptive had expectorated.”
Trall and Holbrook both advanced the idea that physicians should teach the maintenance of health rather than simply provide a last resort in times of health crisis. Besides providing a strong editorial voice denouncing the evils of tobacco and drugs, they strongly advanced the value of vegetarianism, bathing and exercise, dietetics and nutrition along with personal hygiene.
John Harvey Kellogg, MD, another medically trained doctor who turned to more nutritionally based natural healing concepts, also greatly influenced Lust. Kellogg was renowned through his connection, beginning in 1876, with the Battle Creek Sanitarium, which was founded in the 1860s as a Seventh Day Adventist institution designed to perpetuate the Grahamite philosophies. Kellogg, born in 1852, was a “sickly child” who, at age 14, after reading the works of Graham, converted to vegetarianism. At the age of 20, he studied for a term at Trall’s Hygio-Therapeutic College and then earned a medical degree at New York’s Bellevue Medical School. He maintained an affiliation with the regular schools of medicine during his lifetime, more because of his practice of surgery than because of his beliefs in that area of health care (Figure 21-4)
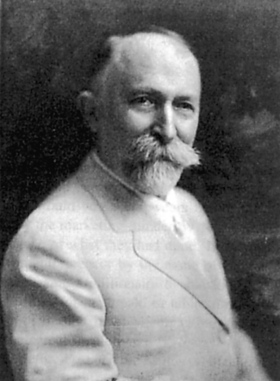
Figure 21-4 Dr. John Harvey Kellogg, brother to the Kellogg of breakfast cereal fame and a physical culture movement proponent.
(Courtesy Historical Society of Battle Creek, Battle Creek, Mich.)
Kellogg designated his concepts, which were basically the hygienic system of healthful living, as “biologic living.” Kellogg expounded vegetarianism, attacked sexual misconduct and the evils of alcohol, and was a prolific writer through the late nineteenth and early twentieth centuries. He produced a popular periodical, Good Health, which continued in existence until 1955. When Kellogg died in 1943 at age 91, he had had more than 300,000 patients through the Battle Creek Sanitarium, including many celebrities, and the “San” became nationally known.
Kellogg was also extremely interested in hydrotherapy. In the 1890s he established a laboratory at the San to study the clinical applications of hydrotherapy. This led to his writing of Rational Hydrotherapy in 1902. The preface espoused a philosophy of drugless healing that came to be one of the bases of the hydrotherapy school of medical thought in early-twentieth-century America.
Influence on Public Health
It is a little-known fact that most of our current and accepted public hygiene practices were brought into societal use by the early hygienic reformers. Before their efforts, neglect of these basic physiological safety measures was rampant. The hygienists had a great influence on decreasing morbidity and mortality and increasing life span, as well as on the adoption of public sanitation. Orthodox medicine is typically credited with these advances.
Currently, certified professional Natural Hygienists are advocates of the highest standards of training and supervised clinical fasting and participate in the training of naturopathic physicians. Naturopathic medicine uses the precepts of natural hygiene in reestablishing the basis of health, the first step in the therapeutic order.
Autotoxicity
Lust was also greatly influenced by the writings of John H. Tilden, MD (who published between 1915 and 1925). Tilden became disenchanted with orthodox medicine and began to rely heavily on dietetics and nutrition, formulating his theories of “autointoxication” (the effect of fecal matter’s remaining too long in the digestive process) and “toxemia.” He provided the natural health care literature with a 200-plus-page dissertation entitled Constipation, with a whole chapter devoted to the evils of not responding “when nature called.”
Elie Metchnikoff (director of the prestigious Pasteur Institute and winner of the 1908 Nobel Prize for his contribution to immunology) and Kellogg wrote prolifically on the theory of autointoxication. Kellogg, in particular, believed that humans, in the process of digesting meat, produced a variety of intestinal self-poisons that contributed to autointoxication. As a result, Kellogg widely advocated that people return to a more healthy natural state by allowing the naturally designed use of the colon. He believed that the average modern colon was devitalized by the combination of a low-fiber diet, sedentary living, the custom of sitting rather than squatting to defecate, and the modern civilized habit of ignoring “nature’s call” out of an undue concern for politeness.
Although the concept of toxemia is not a part of the body of knowledge taught in conventional medical schools, all naturopathic students are presented with this concept. Some of that presentation relies on outdated materials, such as the naturopathic texts of 75 and 100 years ago (e.g., Lindlahr, Tilden). However, modern research and textbooks are beginning to investigate this phenomenon. Drasar and Hill’s Human Intestinal Flora (1974) demonstrates some of the biochemical pathways involved in the generation of metabolic toxins in the gut through dysbiotic bacterial action on poorly digested food (Zeff, 1997). In the last 20 years, our understanding of the concept of toxemia has been significantly updated by practitioners in the newly emerging field of functional medicine, a health care approach that focuses attention on biochemical individuality, metabolic balance, ecological context, and unique personal experience in the dynamics of health. Maldigestion, malabsorption, and abnormal gut flora and ecology are often found to be primary contributing factors not only to gastrointestinal disorders but also to a wide variety of chronic, systemic illnesses. Laboratory assessment tools have been developed that are capable of evaluating the status of many organs, including the gastrointestinal tract. These cutting-edge diagnostic tools provide physicians with an analysis of numerous functional parameters of the individual’s digestion and absorption and precisely pinpoint what in the colonic environment is imbalanced, thus promoting dysbiosis.
Thomsonianism
In 1822, Samuel Thomson published his New Guide to Health, a compilation of his personal view of medical theory and American Indian herbal and medical botanical lore. Thomson espoused the belief that disease had one general cause—derangement of the vital fluids by “cold” influences on the human body—and that disease therefore had one general remedy—animal warmth or “heat.” The name of the complaint depended on the part of the body that was affected. Unlike the conventional American heroic medical tradition that advocated bloodletting, leeching, and the substantial use of mineral-based purgatives such as antimony and mercury, Thomson believed that minerals were sources of “cold” because they come from the ground and that vegetation, which grew toward the sun, represented “heat” (Figure 21-5).
Thomson’s view was that individuals could self-treat if they had an adequate understanding of his philosophy and a copy of New Guide to Health. The right to sell “family franchises” for use of the Thomsonian method of healing was the basis of a profound lay movement between 1822 and Thomson’s death in 1843. Thomson adamantly believed that no professional medical class should exist and that democratic medicine was best practiced by laypersons within a Thomsonian “family” unit. By 1839 Thomson claimed to have sold some 100,000 of these family franchises, called “friendly botanic societies.”
Despite his criticism of the early medical movement for its heroic tendencies, Thomson’s medical theories were heroic in their own fashion. Although he did not advocate bloodletting or heavy metal poisoning and leeching, botanical purgatives—particularly Lobelia inflata (Indian tobacco)—were a substantial part of the therapy.
Eclectic School of Medicine
Some of the doctors practicing the Thomsonian method, called botanics, decided to separate themselves from the lay movement and develop a more physiologically sound basis of therapy. They established a broader range of therapeutic applications of botanical medicines and founded a medical college in Cincinnati. These Thomsonian doctors were later absorbed into the “eclectic school,” which originated with Wooster Beach of New York.
Wooster Beach, from a well-established New England family, started his medical studies at an early age, apprenticing under an old German herbal doctor, Jacob Tidd, until Tidd died. Beach then enrolled in the Barclay Street Medical University in New York. After opening his own practice in New York, Beach set out to win over fellow members of the New York Medical Society (into which he had been warmly introduced by the screening committee) to his point of view that heroic medicine was inherently dangerous and should be reduced to the gentler theories of herbal medicine. He was summarily ostracized from the medical society. He soon founded his own school in New York, calling the clinic and educational facility the United States Infirmary. Because of political pressure from the medical society, however, he was unable to obtain charter authority to issue legitimate diplomas. He then located a financially ailing but legally chartered school, Worthington College, in Worthington, Ohio. There he opened a full-scale medical college, creating the eclectic school of medical theory based on the European, Native American, and American traditions. The most enduring eclectic herbal textbook is King’s American Dispensary by Harvey Wickes Felter and John Uri Lloyd. Published in 1898, this two-volume 2500-page treatise provided the definitive work describing the identification, preparation, pharmacognosy, history of use, and clinical application of more than 1000 botanical medicines. The eclectic herbal lore formed an integral core of the therapeutic armamentarium of the naturopathic doctor (ND).
Homeopathic Medicine
Homeopathy, the creation of an early German physician, Samuel Hahnemann (1755-1843), had four central doctrines: (1) that like cures like (the “law of similars”); (2) that the effect of a medication could be heightened by its administration in minute doses (the more diluted the dose, the greater the “dynamic” effect); (3) that nearly all diseases were the result of a suppressed itch, or “psora”; and (4) that healing proceeds from within outward, above downward, from more vital to less vital organs, and in the reverse order of the appearance of symptoms (pathobiography), known as Hering’s law.
Originally, most U.S. homeopaths were converted orthodox medical doctors, or allopaths (a term coined by Hahnemann). The high rate of conversion made this particular medical sect the archenemy of the rising orthodox medical profession. The first American homeopathic medical school was founded in 1848 in Philadelphia; the last purely homeopathic medical school, based in Philadelphia, survived into the early 1930s (see Chapter 24).
Manipulative Therapies: Osteopathy and Chiropractic
In Missouri, Andrew Taylor Still, originally trained as an orthodox practitioner, founded the school of medical thought known as osteopathy. He conceived a system of healing that emphasized the primary importance of the structural integrity of the body, especially as it affects the vascular system, in the maintenance of health. In 1892 he opened the American School of Osteopathy in Kirksville, Missouri.
In 1895, Daniel David Palmer, originally a magnetic healer from Davenport, Iowa, performed the first spinal manipulation, which gave rise to the school he termed chiropractic. His philosophy was similar to Still’s except for a greater emphasis on the importance of proper neurological function. He formally published his findings in 1910, after having founded a chiropractic school in Davenport (see Chapter 18).
Less well known is “zone therapy,” originated by Joe Shelby Riley, DC, a chiropractor based in Washington, D.C. Zone therapy was an early forerunner of acupressure. In zone therapy, pressure to and manipulation of the fingers and tongue and percussion of the spinal column were applied according to the relation of points on these structures to certain zones of the body.
Christian Science and the Role of Belief and Spirituality
Christian Science, formulated by Mary Baker Eddy in 1879, comprises a profound belief in the role of systematic religious study (which led to the widespread Christian Science Reading Rooms), spirituality, and prayer in the treatment of disease. In 1875 she published Science and Health with Key to the Scriptures, the definitive textbook for the study of Christian Science.
Lust was also influenced by the works of Sidney Weltmer, the founder of “suggestive therapeutics.” Weltmer’s work dealt specifically with the psychological process of desiring to be healthy. The theory behind Professor Weltmer’s work was that whether it was the mind or the body that first lost its grip on health, the two were inseparably related. When the problem originated in the body, the mind nonetheless lost its ability and desire to overcome the disease because the patient “felt sick” and consequently slid further into the diseased state. Alternatively, if the mind first lost its ability and desire to “be healthy” and some physical infirmity followed, the patient was susceptible to being overcome by disease (see Chapter 6).
Physical Culture
Bernarr Mcfadden, a close friend of Lust’s, founded the “physical culture” school of health and healing, also known as physcultopathy. This school of healing gave birth across the United States to gymnasiums where exercise programs were designed and taught to allow individual men and women to establish and maintain optimal physical health.
Although many theories exist to explain the rapid dissolution of these diverse healing arts (the practitioners of which at one time made up more than 25% of all U.S. health care practitioners) in the early part of the twentieth century, low ratings in the infamous Flexner Report (which rated all these schools of medical thought among the lowest), allopathic medicine’s anointing of itself with the blessing “scientific,” and the growing political sophistication of the AMA clearly played the most significant role.
All these healing systems and modalities were naturally unified in the field of naturopathic medicine because they shared one common tenet: respect for and inquiry into the self-healing process and what was necessary to establish health.
Halcyon Days of Naturopathy
In the early 1920s the “health fad” movement was reaching its peak in terms of public awareness and interest. Conventions were held throughout the United States, one of which was attended by several members of Congress, culminating in full legalization of naturopathy as a healing art in the District of Columbia. Not only were the conventions well attended by professionals, but the public also flocked to them, with more than 10,000 attending the 1924 convention in Los Angeles.
During the 1920s and up until 1937, naturopathy was in its most popular phase. Although the institutions of the orthodox school had gained ascendancy, before 1937 the medical profession had no real solutions to the problems of human disease.
During the 1920s, Gaylord Hauser, later to become the health food guru of the Hollywood set, came to Lust as a seriously ill young man. Lust, through application of the nature cure, removed Hauser’s afflictions and was rewarded by Hauser’s lifelong devotion. His regular columns in Nature’s Path became widely read among the Hollywood crowd.
The naturopathic journals of the 1920s and 1930s provide much valuable insight into the prevention of disease and the promotion of health. Much of the dietary advice focused on correcting poor eating habits, including the lack of fiber in the diet and an overreliance on red meat as a protein source. As in the 1990s, we now hear the pronouncements of the orthodox profession, the National Institutes of Health (NIH), and the National Cancer Institute that the early assertions of the naturopaths that such dietary habits would lead to degenerative diseases, including colon cancer and other cancers of the digestive tract, were true.
The December 1928 issue of Nature’s Path contained the first American publication of the work of Herman J. DeWolff, a Dutch epidemiologist. DeWolff was one of the first researchers to assert, on the basis of studies of the incidence of cancer in the Netherlands, that there was a correlation between exposure to petrochemicals and various types of cancerous conditions. He contended that the use of chemical fertilizers and their application in some soils (principally clay) led to their remaining in vegetables after they had arrived at the market and were purchased for consumption. It was almost 50 years before orthodox medicine began to see the wisdom of such assertions.
Suppression and Decline
In 1937 the popularity of naturopathy began to decline. The change came, as both Thomas and Campion note in their works, with the era of “miracle medicine.” Lust recognized this, and his editorializing became, if anything, even more strident. From the introduction of sulfa drugs in 1937 to the release of the Salk vaccine in 1955, the American public became used to annual developments of miracle vaccines and antibiotics. The naturopathic profession adhered to its vitalistic philosophy and a full range of practice but unfortunately was poorly unified at this time on other issues of standards. This made the profession vulnerable to interguild competition.
Lust died in September 1945 in residence at the Yungborn facility in Butler, New Jersey, preparing to attend the 49th Annual Congress of his American Naturopathic Association. Although a healthy, vigorous man, he had seriously damaged his lungs the previous year saving patients when a wing of his facility caught fire; he never fully recovered. On August 30, 1945, writing for the official program of that congress, held in October 1945 just after his death, he noted his concerns for the future. He was especially frustrated with the success of the medical profession in blocking the efforts of naturopaths to establish state licensing laws that would not only establish appropriate practice rights for NDs but also protect the public from the pretenders (i.e., those who chose to call themselves naturopaths without ever bothering to undergo formal training). As Lust (1945) stated:
Now let us see the type of men and women who are the Naturopaths of today. Many of them are fine, upstanding individuals, believing fully in the effectiveness of their chosen profession—willing to give their all for the sake of alleviating human suffering and ready to fight for their rights to the last ditch. More power to them! But there are others who claim to be Naturopaths who are woeful misfits. Yes, and there are outright fakers and cheats masking as Naturopaths. That is the fate of any science—any profession—which the unjust laws have placed beyond the pale. Where there is no official recognition and regulation, you will find the plotters, the thieves, the charlatans operating on the same basis as the conscientious practitioners. And these riff-raff opportunists bring the whole art into disrepute. Frankly, such conditions cannot be remedied until suitable safeguards are erected by law, or by the profession itself, around the practice of Naturopathy. That will come in time.
In the mid-1920s, Morris Fishbein came on the scene as editor of the Journal of the American Medical Association (JAMA). Fishbein took on a personal vendetta against what he characterized as “quackery.” Lust, among others, including Mcfadden, became Fishbein’s epitome of quackery. Unfortunately, he proved to be particularly effective politically and in the media.
The public infatuation with technology, the introduction of “miracle medicine,” World War II’s stimulation of the development of surgery, the Flexner Report, the growing political sophistication of the AMA under the leadership of Fishbein, intraprofession squabbles, and the death of Lust in 1945 all combined to cause the decline of naturopathic medicine and natural healing in the United States. In addition, these years, called the years of the great fear in David Caute’s book by the latter name, were the years during which to be unorthodox was to be un-American.
U.S. courts began to take the view that naturopaths were not truly doctors because they espoused doctrines from “the dark ages of medicine” (something American medicine had supposedly come out of in 1937) and that drugless healers were intended by law to operate without “drugs” (which came to be defined as anything a physician would prescribe for a patient to ingest or apply externally for any medical purpose). The persistent lack of uniform standards, lack of insurance coverage, lost court battles, a splintered profession, and a hostile legislative perspective progressively restricted practice until the core naturopathic therapies became essentially illegal and practices financially nonviable.
Although it was under considerable public pressure in those years, the American Naturopathic Association undertook some of its most scholarly work, coordinating all the systems of naturopathy under commission. This resulted in the publication of a formal textbook, Basic Naturopathy (Spitler, 1948) and a significant work compiling all the known theories of botanical medicine, Naturae Medicina (Kuts-Cheraux, 1953). Naturopathic medicine began splintering when Lust’s American Naturopathic Association was succeeded by six different organizations in the mid-1950s.
By the early 1970s, the profession’s educational institutions had dwindled to one: the National College of Naturopathic Medicine, with branches in Seattle and Portland, Oregon.
Naturopathic Medicine Reemerges
The combination of the counterculture years of the late 1960s, the public’s growing awareness of the importance of nutrition and the environment, and America’s disenchantment with organized institutional medicine (which began after the miracle era faded and it became apparent that orthodox medicine has its limitations and is prohibitively expensive) resulted in the emergence of new respect for alternative medicine in general and in the rejuvenation of naturopathic medicine. At this time, a new wave of students were attracted to the philosophical precepts of the profession. They brought with them an appreciation for the appropriate use of science, modern college education, and matching expectations for quality education.
Dr. John Bastyr (1912-1995) and his firm, efficient, professional leadership inspired science- and research-based training in natural medicine to begin to reach toward its full potential. Dr. Bastyr, whose vision was of “naturopathy’s empirical successes documented and proven by scientific methods,” was “himself a prototype for the modern naturopathic doctor, who culls the latest findings from the scientific literature, applies them in ways consistent with naturopathic principles, and verifies the results with appropriate studies.” Bastyr also saw “a tremendous expansion in both allopathic and naturopathic medical knowledge, and he played a major role in making sure the best of both were integrated into naturopathic medical education” (Kirchfield et al, 1994).
In response to the growth in public interest during the late 1970s, naturopathic colleges were established in Arizona (Arizona College of Naturopathic Medicine, 1977), Oregon (American College of Naturopathic Medicine, 1980), and California (Pacific College of Naturopathic Medicine, 1979). None of these three survived. In 1978 the John Bastyr College of Naturopathic Medicine (later renamed Bastyr University) was formed in Seattle by founding president Joseph E. Pizzorno, Jr., ND; Lester E. Griffith, ND; William Mitchell, ND; and Sheila Quinn to teach and develop science-based natural medicine. They believed that for the naturopathic profession to move back into the mainstream, it needed to establish accredited institutions, perform credible research, and establish itself as an integral part of the health care system. Bastyr University not only survived but thrived, and it became the first naturopathic college ever to become regionally accredited. In 1993, Michael Cronin, Kyle Cronin, and Konrad Kail, NDs, founded the Southwest College of Naturopathic Medicine and Health Science in Scottsdale, Arizona. In 1997 the University of Bridgeport, with the leadership of Jim Sensenig, ND, founded the University of Bridgeport College of Naturopathic Medicine.
With five credible colleges (including the Canadian College of Naturopathic Medicine in Ontario), active research, an appreciation of the appropriate application of science to natural medicine education, and clinical practice, naturopathic medicine is well on the road to recovery.
A sixth promising naturopathic college, the Boucher Institute of Naturopathic Medicine, was established in January 2000 in Vancouver, British Columbia. Boucher Institute graduated its first class in May 2004.
Recent Influences
A tremendous amount of research providing scientific support for the principles of naturopathic medicine has been conducted at mainstream research centers and increasingly at naturopathic medical schools. In fact, allopathy is turning more to the use of naturopathic methods in the search for effective prescriptions for diseases that are currently intractable and expensive to treat (Werbach, 1996). It is now well established that nutritional factors are of major importance in the pathogenesis of both atherosclerosis and cancer, the two leading causes of death in Western countries, and studies validating their importance in the pathogenesis of many other diseases continue to be published. Much of the research now documenting the scientific foundations of naturopathic medicine practices and principles can be found in A Textbook of Natural Medicine (Pizzorno et al, 1985-1995). This two-volume, 200-chapter work contains 7500 citations to the peer-reviewed scientific literature documenting the efficacy of many natural medicine therapies.
Although the naturopaths were astute clinical observers and a century ago recognized many of the concepts that are now gaining popularity and are being supported by scientific data, the scientific tools of the time were inadequate to assess the validity of their concepts. In addition, as a group they seemed to have little inclination for the application of laboratory research, especially because “science” was the bludgeon used by the AMA to suppress the profession. This has now changed. In the past few decades a considerable amount of research has now provided the scientific documentation of many of the concepts of naturopathic medicine, and the new breed of scientifically trained naturopaths is using this research to continue development of the profession. The following sections describe a few of the most important trends.
Therapeutic Nutrition
Since 1929, when Christiaan Eijkman and Sir Frederick Hopkins shared the Nobel Prize in medicine and physiology for the discovery of vitamins, the role of these trace substances in clinical nutrition has been a matter of scientific investigation. The discovery that enzyme systems depended on essential nutrients provided the naturopathic profession with great insights into why an organically grown, whole-foods diet is so important for health. Formulation of the concept of “biochemical individuality” by nutritional biochemist Roger Williams in 1955 further developed these ideas and provided great insights into the unique nutritional needs of each individual and the way to correct inborn errors of metabolism and even treat specific diseases through the use of nutrient-rich foods or large doses of specific nutrients. Linus Pauling, the two-time Nobel Prize winner, originated the concept of “orthomolecular medicine” and provided further theoretical substantiation for the use of nutrients as therapeutic agents.
Functional Medicine
In 1990, Jeff Bland, PhD, coined the term functional medicine to describe a putatively science-based development of therapeutic nutrition for the prevention of illness and promotion of health. Focusing on biochemical individuality, metabolic balance, and the ecological context, functional medicine practitioners avail themselves of recently developed laboratory tests to pinpoint perceived imbalances in an individual’s biochemistry that are thought to cause a cascade of biological triggers, paving the way to suboptimal function, chronic illness, and degenerative disease. A broad range of functional laboratory assessment tools in the areas of digestion (gastrointestinal system), nutrition, detoxification and oxidative stress, immunology and allergy, production and regulation of hormones (endocrinology), and the heart and blood vessels (cardiovascular system) provide physicians with a basis to recommend nutritional interventions specific to the individual’s needs and to monitor their efficacy.
Environmental Medicine and Clinical Ecology
Although recognition of the clinical impact of environmental toxicity and endogenous toxicity has existed since the earliest days of naturopathy, it was not until the environmental movement and the seminal work of Rachel Carson and others that the scientific basis was established. Clinical research and the development of laboratory methods for assessing toxic load have provided objective tools that have greatly increased the sophistication of clinical practice. Clinical and laboratory methods were developed for the assessment of idiosyncratic reactions to environmental factors and foods.
Spirituality, Health, and Medicine
Naturopathic medicine’s philosophy of treating the whole person and enhancing the individual’s inherent healing ability is closely aligned with its mission of integrating spirituality into the healing process. Scientific evidence is growing on the part spirituality can play in healing. René Descartes has been accused of separating mind from body back in the seventeenth century, and medical science has attempted to explain disease independently of mind, in terms of germs, environmental agents, or wayward genes. At present, however, the evidence on the link between mind and body is not just clinical observation but chemical fact. An explosion of research in the new and rapidly expanding field of psychoneuroimmunology is revealing physical evidence of the mind-body connection that is changing our understanding of disease (see Chapter 8). Scientists no longer question whether but rather how our minds have an impact on our health, and the implications of the connections uncovered in only the last 20 years are extraordinary.
In his book Healing Words (1993), Larry Dossey, MD, pulls together what he describes as “one of the best kept secrets in medical science”: the extensive experimental evidence for the beneficial effects of prayer. Dossey reviews studies that provide evidence for a positive effect of prayer on not only humans but mice, chicks, enzymes, fungi, yeast, bacteria, and cells of various sorts. He emphasizes, “We cannot dismiss these outcomes as being due to suggestion or placebo effects, since these so-called lower forms of life do not think in any conventional sense and are presumably not susceptible to suggestion” (Pizzorno, 1995).
“Cutting-Edge” Laboratory Methods
A final significant influence has been the development of laboratory methods for the objective assessment of nutritional status, metabolic dysfunction, digestive function, bowel flora, endogenous and exogenous toxic load, liver detoxification and other system functions, and genomics. Each of these has provided ever more effective tools for accurate assessment of patient health status and effective application of naturopathic principles.
Genomics
One of the most exciting recent advances is genomic testing, the ability to evaluate each individual’s template for making the enzymes of life. This technology is now providing a level of objective evaluation of biochemical individuality never before available, greatly strengthening the naturopathic doctor’s ability to practice personalized medicine. The ability to assess each individual’s unique nutrient needs as well as susceptibilities to environmental toxins promises to change fundamentally the practice of medicine (Pizzorno, 2003).
During the last several years, as America’s staggering health care debt accumulates because of the increase in chronic disease, these core, traditional naturopathic principles are surfacing widely as central to creating an effective health care system, as follows:
Current medical education inculcates many of the dominant values of modern medicine: reductionism, specialization, mechanistic models of disease, and faith in a definitive cure. . . . What is needed is a model of care that addresses the whole person and integrates care for the person’s entire constellation of comorbidities. . . . Nothing short of a fundamental redesign of primary care systems is required. (Grumbach, 2003)
PRINCIPLES
Although in many ways, modern medicine resembles a science, it continues to be criticized for its lack of unifying theories, and for this reason alone its claim to being a science has remained suspect.
What physicians think medicine is profoundly shapes what they do, how they behave in doing it, and the reasons they use to justify that behavior. . . . Whether conscious of it or not, every physician has an answer to what he thinks medicine is, with real consequences for all whom he attends. . . . The outcome is hardly trivial. . . . It dictates, after all, how we approach patients [and] how we make clinical judgments.
Medical philosophy comprises the underlying premises on which a healthcare system is based. Once a system is acknowledged, it is subject to debate. In naturopathic medicine, the philosophical debate is a valuable, ongoing process which helps the understanding that disease evolves in an orderly and truth-revealing fashion.
Naturopathic medicine is a distinct system of health-oriented medicine that, in contrast to the currently dominant disease-treatment system, stresses promotion of health, prevention of disease, patient education, and self-responsibility. However, naturopathic medicine symbolizes more than simply a health care system; it is a way of life. Unlike most other health care systems, naturopathy is not identified with any particular therapy but rather is a way of thinking about life, health, and disease. It is defined not by the therapies it uses but by the philosophical principles that guide the practitioner.
Seven powerful concepts provide the foundation that defines naturopathic medicine and create a unique group of professionals practicing a form of medicine that fundamentally changes the way we think of health care. In 1989 the American Association of Naturopathic Physicians unanimously approved the definition of naturopathic medicine, updating and reconfirming in modern terms its core principles as a professional consensus. “The definition and principles of practice provide a steady point of reference for this debate, for our evolving understanding of health and disease, and for all of our decision making processes as a profession” (Snider et al, 1988).
The seven core principles of naturopathic medicine are as follows, with “wellness and health promotion” emerging into the forefront of the scholarly discussion of naturopathic clinical theory:
The Healing Power of Nature (vis medicatrix naturae)
Belief in the ability of the body to heal itself—the vis medicatrix naturae (the healing power of nature)—if given the proper opportunity, and the importance of living within the laws of nature is the foundation of naturopathic medicine. Although the term naturopathy was coined in the late nineteenth century, its philosophical roots can be traced back to Hippocrates and derive from a common wellspring in traditional world medicines: belief in the healing power of nature.
Medicine has long grappled with the question of the existence of the vis medicatrix naturae. As Neuberger stated, “The problem of the healing power of nature is a great, perhaps the greatest of all problems which has occupied the physician for thousands of years. Indeed, the aims and limits of therapeutics are determined by its solution.” The fundamental reality of the vis medicatrix naturae was a basic tenet of the Hippocratic school of medicine, and “every important medical author since has had to take a position for or against it” (Neuberger, 1932).
When standard medicine soundly rejected the principle of the vis medicatrix naturae at the turn of the twentieth century, nature doctors, including naturopathic physicians in the United States from 1896 on, diverged from conventional medicine. Naturopathic physicians recognized the clinical importance of the inherent self-healing process; embraced it as their core academic and clinical principle; and developed an entire system of medical practice, training, and research based on it and on related principles of clinical medicine.
Naturopathic medicine is therefore “vitalistic” in its approach (i.e., life is viewed as more than just the sum of biochemical processes), and the body is believed to have an innate intelligence or process (the vis medicatrix naturae), which is always striving toward health. Vitalism maintains that the symptoms accompanying disease are not typically caused by the morbific agent (e.g., bacteria); rather, they are the result of the organism’s intrinsic response or reaction to the agent and the organism’s attempt to defend and heal itself (Lindlahr, 1914a; Neuberger, 1932). Symptoms are part of a constructive phenomenon that is the best “choice” the organism can make, given the circumstances. In this construct the physician’s role is to understand and aid the body’s efforts, not to take over or manipulate the functions of the body, unless the self-healing process has become weak or insufficient.
Although the context and life force of naturopathic medicine is its vitalistic core, both vitalistic and mechanistic approaches are applicable to modern naturopathic medicine. Vitalism has reemerged in current terms in the body-mind-spirit dialogue. Matter, mind, energy, and spirit are each part of nature and therefore are part of medicine that observes, respects, and works with nature. Much of modern biomedicine and related research is based on the application of the theory of mechanism (defined in Webster’s Dictionary as the “theory that everything in the universe is produced by matter in motion; materialism”) in a highly reductionistic, single-agent, pathology-based, disease care model. Applied in a vitalistic context, mechanistic and reductionistic interventions provide useful techniques and tools to naturopathic physicians. The unifying theory of naturopathic medicine, as discussed later, provides clinical guidance for integrating both approaches.
First Do No Harm (primum non nocere)
Naturopathic physicians prefer noninvasive treatments that minimize the risks of harmful side effects. They are trained to use the lowest-force and lowest-risk preventive, diagnostic, therapeutic, and co-management strategies. They are trained to know which patients they can safely treat and which ones they need to refer to other health care practitioners. Naturopathic physicians follow three precepts to avoid harming the patient:
Find the Cause (tolle causam)
Every illness has an underlying cause or causes, often in aspects of the lifestyle, diet, or habits of the individual. A naturopathic physician is trained to find and remove the underlying cause(s) of disease. The therapeutic order helps the physician remove them in the correct “healing order” for the body (see later discussion). As the new science of psychoneuroimmunology is explicitly demonstrating, the body is a seamless web with a multiplicity of brain–immune system–gut–liver connections (see Chapter 8). Not surprisingly, chronic disease typically involves a number of systems, with the most prominent or acute symptoms being those chronologically last in appearance. As the healing process progresses and these symptoms are alleviated, further symptoms then resurface that must then be addressed to restore health. To paraphrase David Jones, MD, on the “tack rules”: “If you’re sitting on a tack, it takes a lot of aspirin to feel better. If you’re sitting on two tacks, removing one does not necessarily lead to a 50% improvement or reduction in symptoms.”
Treat the Whole Person (Holism)
As noted previously, health or disease comes from a complex interaction of mental, emotional, spiritual, physical, dietary, genetic, environmental, lifestyle, and other factors. Naturopathic physicians treat the whole person, taking all these factors into account. Naturopathically, the body is viewed as a whole. Naturopathy is often called holistic medicine in reference to the term holism, coined by philosopher Jan Christian Smuts in 1926, to describe the gestalt of a system as greater than the sum of its parts. A change in one part causes a change in every part; therefore the study of one part must be integrated into the whole, including the community and biosphere.
Naturopathic medicine asserts that one cannot be healthy in an unhealthy environment, and it is committed to the creation of a world in which humanity may thrive. In contrast to the high degree of specialization in the present medical system, which reflects a mechanistic orientation to single organs, the holistic model relegates specialists to an ancillary role. Emphasis is placed on the physical, emotional, social, and spiritual integration of the whole person, including awareness of the impact of the environment on health.
Preventive Medicine
The naturopathic approach to health care helps prevent disease and keeps minor illnesses from developing into more serious or chronic degenerative diseases. Patients are taught the principles for living a healthful life, and by following these principles, they can prevent major illness. Health is viewed as more than just the absence of disease; it is considered a dynamic state that enables a person to thrive in, or adapt to, a wide range of environments and stresses. Health and disease are points on a continuum, with death at one end and optimal function at the other. The naturopathic physician believes that a person who goes through life living an unhealthful lifestyle will drift away from optimal function and move relentlessly toward progressively greater dysfunction. Genotype, constitution, maternal influences, and environmental factors all influence individual susceptibility to deterioration, and the organs and physiological systems affected. Box 21-2 lists these and other determinants of health addressed by the naturopathic physician in both treatment and prevention.
BOX 21-2 Determinants of Health and Other Factors in Naturopathic Preventive Medicine
The virulence of moribific agents or insults also plays a central role in disturbance, causing decreasing function and ultimately serious disease.
In our society, although our expected life span at birth has increased, our health span has not, nor has our health expectancy at age 65. We are living longer but as disabled individuals (Pizzorno, 1997). Although such deterioration is accepted by our society as the normal expectation of aging, it is not common in animals in the wild or among those fortunate peoples who live in an optimal environment (i.e., no pollution, low stress, regular exercise, and abundant natural, nutritious food).
In the naturopathic model, death is inevitable; progressive disability is not. This belief underscores a fundamental difference in philosophy and expectation between the conventional and naturopathic models of health and disease. In contrast to the disease treatment focus of allopathic medicine, the health promotion focus of naturopathic medicine emphasizes the means of maximizing health span.
Wellness and Health Promotion (emerging principle)
Establishing and maintaining optimal health and balance is a central clinical goal. Wellness and health promotion go beyond prevention. This principle refers to a proactive state of being healthy, characterized by positive emotion, thought, intention, and action. Wellness is inherent in everyone, no matter what disease is being experienced. The recognition, experience, and support of wellness through health promotion by the physician and patient will more quickly heal a given disease than treatment of the disease alone.
Doctor as Teacher (docere)
The original meaning of the word docere is “teacher.” A principle objective of naturopathic medicine is to educate the patient and emphasize self-responsibility for health. Naturopathic doctors also recognize the therapeutic potential of the physician-patient relationship. The patient is engaged and respected as an ally and a member of her or his own health care team. Adequate time is spent with patients to diagnose, treat, and educate them thoroughly (see Chapters 1 and 2).
Naturopathic Practice Today
Current naturopathic physicians are licensed primary care providers of integrative natural medicine and are also recognized for their clinical expertise and effectiveness in preventive medicine. NDs are trained as family physicians, regardless of elective postdoctoral training or clinical emphasis. This is intentional and consistent with naturopathic principles of practice. NDs are trained to assess causes and develop treatment plans from a systems perspective and with systems skills on the basis of naturopathic principles and, specifically, the principle of “treating the whole person,” as follows:
Naturopathy, in fact, is typically meta-systematic. . . . The organism [is] always seen in the context of its physical and social environment. . . . Beyond this, naturopathy ultimately might even be considered cross-paradigmatic, touching inevitably on the economics, politics, history, and sociology of the various healing alternatives, ultimately penetrating to the contrasting philosophies underlying naturopathy and allopathy. Naturopathy results from a guiding philosophy at odds with the dominant mechanistic philosophy undergirding Western industrialized society. Allopathy, in contrast, is clearly derived from these same premises. Or in Eisler’s terms, naturopathy embraces a partnership model of relationship, while allopathy falls within the dominator model. . . . [T]his partnership/dominator model extends not only to the treatment process but to the healer/patient relationship itself. (Funk, 1995)
NDs may also practice as specialists, after postdoctoral training in botanical medicine, homeopathy, nutritional medicine, physical medicine, acupuncture, Ayurvedic medicine, Oriental and Chinese herbal medicine, counseling and health psychology, spirituality and healing, applied behavioral sciences, or midwifery. Some NDs choose to focus their practice on population groups such as children, the elderly, or women, or in clinical areas such as cardiology, gastroenterology, immunology, or environmental medicine. These diverse practices are consistent with the eclectic origins of naturopathic medicine and are part of its strength.
In addition to NDs with these specialties, at one end of the spectrum are practitioners who adhere to the nature cure tradition and focus clinically only on diet, detoxification, lifestyle modification, hydrotherapy, and other self-healing modalities. At the other end are those whose practices appear to be similar to the average conventional medical practice, with the only apparent difference being the use of pharmaceutical-grade botanical medicines instead of synthetic drugs. However, fundamental to all styles of naturopathic practice is a common philosophy and principles of health and disease: the unifying theory in the hierarchy of therapeutics, or the therapeutic order described in the following section. The therapeutic order is derived from all of the principles and guides the ND’s choice of therapeutic interventions.
UNIFYING THEORY: THE HEALING POWER OF NATURE AND THE THERAPEUTIC ORDER
In facilitating the process of healing, the naturopathic physician seeks to use those therapies and strategies that are most efficient and that have the least potential to harm the patient. The concept of “harm” includes suppression or exhaustion of natural healing processes, including inflammation and fever. These precepts, coupled to an understanding of the process of healing, result in a therapeutic hierarchy. This hierarchy (or therapeutic order) is a natural consequence of how the organism heals. Therapeutic modalities are applied in a rational order, determined by the nature of the healing process. The natural order of appropriate therapeutic intervention is as follows:
This appropriate therapeutic order proceeds from least to most force. All modalities can be found at various steps, depending on their application. The spiritual aspect of the patient’s health is considered to begin with step 1 (Zeff, 1997; steps 5 through 7 added by Snider).
The concepts expressed in the therapeutic order are derived from the writings of Hippocrates and those of medical scholars since Hippocrates concerning the function and activation of the self-healing process. Dr. Jared Zeff (1997) expresses these concepts as the hierarchy of therapeutics in his article “The Process of Healing: A Unifying Theory of Naturopathic Medicine.” These concepts are further explored, refined, and developed in The Textbook of Natural Medicine, third edition (Pizzorno, 2006) in a chapter written by Zeff, Snider, and Myers entitled “A Hierarchy of Healing: The Therapeutic Order—the Unifying Theory of Naturopathic Medicine.”
The philosophy represented in the therapeutic order does not determine what modalities are good or bad. Rather, it provides a clinical framework for all approaches and modalities, used in an order consistent with that of the natural self-healing process. It respects the origins of disease and the applications of care and intervention necessary for health and healing with the least intervention.
The therapeutic order exemplifies the concept of using the least force, one of the key tenets of the naturopathic principle “Do no harm.” The therapeutic order schematically directs the ND’s therapeutic choices so that they are implemented in an efficient order rather than in a “shotgun” approach. This common philosophy and theory both distinguishes the field of naturopathic medicine and enables it to consider and incorporate new therapies.
Naturopathic medicine’s philosophical approach to health promotion and restoration requires that practitioners possess a broad range of diagnostic and therapeutic skills and accounts for the eclectic interests of the naturopathic profession. Obviously, at times the body needs more than just supportive help. The goal of the ND in such situations is first to use the lowest-force and lowest-risk clinical strategies (i.e., the least invasive intervention that will have the most effective therapeutic outcome) and, when necessary, to co-manage or refer to specialists and other health care professionals.
Because the goal of the ND is to restore normal body function rather than to apply a particular therapy, virtually every natural medicine therapy may be used. In addition, to fulfill their role as primary care family physicians, NDs may also administer vaccines and use therapies such as office surgery and prescription drugs when less invasive options have been exhausted or found inappropriate. In the restoration of health, prescription drugs and surgery are a last resort but are used when necessary. As Kirschner and Brinkman (1988) noted, “The use of petroleum by-products and the removal of body parts is a poor first line of defense against disease.”
Naturopathic medical school curricula are continually revised in light of these principles. Curriculum integration is built on the science-based educational structure already in place in these colleges. Basic science, ND, and non-ND physician faculty are trained in naturopathic philosophy and principles and the therapeutic order as core assumptions that invite scholarly inquiry. Discussion and inquiry concerning the philosophy and theory are stimulated and supported in interdisciplinary faculty teams. The fruits of these endeavors are brought into the classroom to enhance students’ critical thinking concerning clinical values and assumptions. Naturopathic research on these principles themselves is a widely embraced priority for the naturopathic profession. In 2004 the Naturopathic Medical Research Agenda, a 2-year research project sponsored by the NIH’s National Center for Complementary and Alternative Medicine, identified three key hypotheses as central to the future and the foundations of naturopathic medical research. The third hypothesis states: “The scientific exploration of naturopathic medical practices and principles will yield important insights into the nature of health and healing” (Standish et al, 2004).
DIAGNOSIS
In the naturopathic medicine program at Bastyr University, for example, the principles just discussed and the therapeutic order are translated into a series of questions that drive curriculum development and case analysis and provide guidance to students learning the art and science of naturopathic medicine. These Naturopathic Case Analysis and Management questions (see next section) are integrated with conventional SOAP (subjective, objective, assessment, plan) algorithms as the process of naturopathic case analysis and management, the clinical application of philosophy to patient care. For example, although a conventional pathological diagnosis is made through the use of physical, laboratory, and radiologic procedures, it is done in the context of understanding the underlying causes of the pathology and the obstacles to recovery.
NATUROPATHIC CASE ANALYSIS AND MANAGEMENT
I. The Healing Power of Nature (vis medicatrix naturae)
III. Find the Cause (tolle causam)
IV. Treat the Whole Person (Holism)
V. Preventive Medicine
VI. Wellness and Health Promotion (emerging principle)
THERAPEUTIC MODALITIES
Naturopathic medicine is a vitalistic system of health care that uses natural medicines and interventionist therapies as needed. Natural medicines and therapies, when properly used, generally have low invasiveness and rarely cause suppression or side effects. This is because, when used properly, they generally support the body’s healing mechanisms rather than taking over the body’s processes. The ND knows when, why, and with what patient more invasive therapies are needed based on the therapeutic order and appropriate diagnostic measures. The ND also recognizes that the use of natural, low-force therapies; lifestyle changes; and early functional diagnosis and treatment of nonspecific conditions is a form of preprimary prevention. This approach offers one viable solution for cost containment in primary health care.
Traditional health care disciplines such as traditional Chinese medicine (TCM), Unani medicine, and homeopathic medicine each have a philosophy, principles of practice, and clinical theory that form a system for diagnosis, treatment, and case management. A philosophy of medicine is, in essence, the rational investigation of the truth and principles of that medicine. The principles of practice form an outline of or guidelines to the main precepts or fundamental tenets of a system of medicine. Clinical theory provides a system of rules or principles explaining that medicine and applying that system to the patient by means of diagnosis, treatment, and management. The specific substances and techniques, as well as when, why, and to whom they are applied and for how long, depend on the system. Modalities (e.g., botanical medicine, physical medicine) are not systems but rather therapeutic approaches used within these systems. One modality may be used by many systems but in different ways.
The importance of systems is that the efficacy, safety, and efficiency of diagnostic and treatment approaches depend as much on the system as on the effects of the substance on physiology or biochemical pathways. This is exemplified by data in the TCM Work Force Survey conducted by the Department of Human Services in Victoria, New South Wales, and Queensland, Australia. In this study, Bensoussan and Myers (1996) assessed adverse events and length of TCM training for practitioners, as follows:
The number of adverse events reported were compared to the length of TCM training undertaken by the practitioner. It appears from these findings that shorter periods of training in TCM (less than one year) carry an adverse event rate double that of practitioners who have studied for four years or more. . . . These practitioners were asked to respond to two questions regarding the theoretical frameworks they used to guide their TCM practice. TCM philosophy is adopted more readily as the basis for practice by primary TCM practitioners than by allied health practitioners using TCM as part of their practice. In answer to the question, “Do you rely more predominantly on a TCM philosophy and theoretical framework for making your diagnosis and guiding your acupuncture or Chinese herbal medicine treatments?” 90% of primary TCM practitioners answered yes in contrast to 24% of non-primary practitioners.
Nonprimary practitioners were typically educated for less than 1 year and were medical doctors.
It is the system used by each of these disciplines that makes it a uniquely effective field of medicine rather than a vague compendium of complementary and alternative medicine (CAM) modalities. Techniques from many systems are used in naturopathic medicine because of its primary care integrative approach and strong philosophical orientation.
Clinical nutrition, or the use of diet as a therapy, serves as the therapeutic foundation of naturopathic medicine. A rapidly increasing body of knowledge supports the use of whole foods, fasting, natural hygiene, and nutritional supplements in the maintenance of health and treatment of disease. The recognition of unique nutritional requirements caused by biochemical individuality has provided a theoretical and practical basis for the appropriate use of megavitamin therapy. Controlled fasting is also used clinically.
Botanical medicines are also important. Plants have been used as medicines since antiquity. The technology now exists to understand the physiological activities of herbs, and a tremendous amount of research worldwide, especially in Europe, is demonstrating clinical efficacy. Botanical medicines are used for both vitalistic and pharmacological actions. Pharmacological effects and contraindications, as well as synergetic, energetic, and dilutional uses, are fundamental knowledge in naturopathic medicine (see Chapters 5 and 22).
Homeopathic medicine derives etymologically from the Greek words homeos, meaning “similar,” and pathos, meaning “disease.” Homeopathy is a system of medicine that treats a patient and his or her condition with a dilute, potentized agent, or drug, that will produce the same symptoms as the disease when given to a healthy individual, the fundamental principle being that like cures like. This principle was actually first recognized by Hippocrates, who noticed that herbs and other substances given in small doses tended to cure the same symptoms they produced when given in toxic doses. Prescriptions are based on the totality of all the patient’s symptoms and matched to “provings” of homeopathic medicines. Provings are symptoms produced in healthy people who are unaware of the specific remedy they have received. Large numbers of people are tested and these symptoms documented. The symptoms are then added to toxicology, symptomatology, and data from cured cases to form the homeopathic materia medica. Homeopathic medicines are derived from a variety of plant, mineral, and chemical substances and are prepared according to the specifications of the Homeopathic Pharmacopoeia of the United States. Approximately 100 clinical studies have demonstrated the clinical efficacy of homeopathic therapies (see Chapter 24).
Traditional Chinese medicine is analogous to naturopathic medicine to the extent that it is a system with principles corollary to working with the self-healing process. According to Bensoussan and Myers (1996),
TCM shares some common ideas with other forms of complementary medicine, including belief in a strong inter-relationship between the environment and bodily function and an understanding of illness as starting with an imbalance of energy. . . . The TCM diagnostic process is . . . particularly holistic in nature [again similar to that in naturopathic medicine] and is usually contrasted to a reductionistic approach in western medicine. Western medicine often defines disease at an organ level of dysfunction and is increasingly reliant on laboratory findings. In contrast, TCM defines disease as a whole person disturbance.
Quiang Cao, ND, LAc, Bastyr University, explains as follows:
TCM never treats just the symptom, but the individual’s whole constitution and environmental conditions; all are considered in a holistic context. The symptom signals constitutional excess or deficiency. The goal is not just to alleviate the symptom but to balance yin and yang, hot and cold, excess and deficiency, internally and externally.
Acupuncture is an ancient Chinese system of medicine involving the stimulation of certain specific points on the body to enhance the flow of vital energy (qi) along pathways called meridians. Acupuncture points can be stimulated by the insertion and withdrawing of needles, the application of heat (moxibustion), massage, laser, electrical means, or a combination of these methods. Traditional Chinese acupuncture implies use of a very specific acupuncture technique and knowledge of the Oriental system of medicine, including yin-yang, the five elements, acupuncture points and meridians, and a method of diagnosis and differentiation of syndromes quite different from that of Western medicine. Although most research in this country has focused on its use for the pain relief and the treatment of addictions, it is a complete system of medicine effective for management of many diseases (see Chapter 27).
Hydrotherapy is the use of water in any of its forms (e.g., hot, cold, ice, steam) and with any method of application (e.g., sitz bath, douche, spa and hot tub, whirlpool, sauna, shower, immersion bath, pack, poultice, foot bath, fomentation, wrap, colonic irrigation) in the maintenance of health or treatment of disease. It is one of the most ancient methods of treatment and has been part of naturopathic medicine since its inception. Nature doctors, before and since Sebastian Kneipp, have used hydrotherapy as a central part of clinical practice. Hydrotherapy has been used to treat disease and injury by many different cultures, including the Egyptians, Assyrians, Persians, Greeks, Hebrews, Hindus, and Chinese. Its most sophisticated applications were developed in eighteenth-century Germany. Naturopathic physicians today use hydrotherapy to stimulate and support healing, to detoxify, and to strengthen immune function in many chronic and acute conditions.
Physical medicine refers to the therapeutic use of touch, heat, cold, electricity, and sound. This includes the use of physical therapy equipment such as ultrasound, diathermy, and other electromagnetic energy devices; therapeutic exercise; massage; massage energy, joint mobilization (manipulative), and immobilization techniques; and hydrotherapy. In the therapeutic order, correction of deficiencies in structural integrity is a key factor; the hands-on approach of naturopathic physicians through physical medicine is unique in primary care.
Detoxification, the recognition and correction of endogenous and exogenous toxicity, is an important theme in naturopathic medicine. Liver and bowel detoxification, elimination of environmental toxins, correction of the metabolic dysfunction(s) that causes the buildup of non–end-product metabolites—all are important ways of decreasing toxic load. Spiritual and emotional toxicity are also recognized as important factors influencing health.
Spirituality and health measures are central to naturopathic practice and are based on the individual patient’s beliefs and spiritual orientation; put simply, what moves the patient toward life and a higher purpose than himself or herself. Because total health also includes spiritual health, naturopathic physicians encourage individuals to pursue their personal spiritual development. As a plethora of studies in the newly emerging field of psychoneuroimmunology have demonstrated, particularly those examining both the placebo and the nocebo effect, the body is not a mere collection of organs, but rather a body, mind, and spirit in which the mind-spirit part of the equation marshals tremendous forces promoting health or disease.
Counseling, health psychology, and lifestyle modification techniques are essential modalities for the naturopathic physician. An ND is a holistic physician formally trained in mental, emotional, and family counseling. Various treatment modalities include hypnosis and guided imagery, counseling techniques, correction of underlying organic factors, and family systems therapy.
THERAPEUTIC APPROACH
Respect Nature
We are natural organisms, with our genomes developed and expressed in the natural world. The patterns and processes inherent in nature are inherent in us. We exist as a part of complex patterns of matter, energy, and spirit. Nature doctors have observed the natural processes of these patterns in health and disease and have determined that there is an inherent drive toward health that lives within the patterns and processes of nature.
The drive is not perfect. At times, when unguided, unassisted, or unstopped, the drive goes astray, causing preventable harm or even death; the healing intention becomes pathology. The ND is trained to know, respect, and work with this drive and to know when to wait and do nothing, act preventively, assist, amplify, palliate, intervene, manipulate, control, or even suppress, using the principle of the least force. The challenge of twenty-first-century medicine is to support the beneficial effects of this drive and come to a sophisticated application of the least-force principle in mainstream health care. This will prevent the last 20 years of life from being those of debility from chronic, degenerative disease for the average American and extend the health span throughout the life span.
Because the total organism is involved in the healing attempt, the most effective approach to care must consider the whole person. In addition to physical and laboratory findings, important consideration is given to the patient’s mental, emotional, and spiritual attitude; lifestyle; diet; heredity; environment; and family and community life. Careful attention to each person’s unique individuality and susceptibility to disease is critical to the proper evaluation and treatment of any health problem.
Naturopathic physicians believe that most disease is the direct result of the ignorance and violation of “natural living laws.” These rules are summarized as consuming natural, unrefined, organically grown foods; ensuring adequate amounts of exercise and rest; living a moderately paced lifestyle; having constructive and creative thoughts and emotions; avoiding environmental toxins; and maintaining proper elimination. During illness, it is also important to control these areas to remove as many unnecessary stresses as possible and to optimize the chances that the organism’s healing attempt will be successful. Therefore, fundamental to naturopathic practice is patient education and responsibility, lifestyle modification, preventive medicine, and wellness promotion.
Naturopathic Approaches to Disease
The ND’s therapeutic approach is therefore basically twofold: to help patients heal themselves and to use the opportunity to guide and educate the patient in developing a more healthful lifestyle. Many supposedly incurable conditions respond very well to naturopathic approaches.
A typical first office visit to an ND takes 1 hour. The goal is to learn as much as possible about the patient using thorough history taking and review of systems, physical examination, laboratory tests, radiology, and other standard diagnostic procedures. Also, the patient’s diet, environment, toxic load, exercise, stress, and other aspects of lifestyle are evaluated, and laboratory tests are used to determine physiological function. Once a good understanding of the patient’s health and disease status is established (making a diagnosis of a disease is only one part of this process), the ND and patient work together to establish a treatment and health promotion program.
Although every effort is made to treat the whole person and not just his or her disease, the limits of a short description necessitate discussing typical naturopathic therapies for specific conditions in a simplified, disease-oriented manner. The following sections provide examples of how the person’s health can be improved through naturopathic approaches, resulting in alleviation of the disease.
Cervical Dysplasia
The only traditional medical approach to treating cervical dysplasia, a precancerous condition of the uterine cervix, is surgical resection. Nothing is done to treat the underlying causes. The typical naturopathic treatment would include the following:
The advantages of this approach are that (1) the causes of the cervical dysplasia have been identified and resolved, so the problem should not recur; (2) no surgery is used, thus no scar tissue is formed; and (3) the cost, particularly considering that many women with cervical dysplasia have recurrences when treated with standard surgery, is reasonable. More important, however, is that the woman’s health has been improved, and other conditions that could have been caused by the identified nutritional deficiencies have now been prevented.
Migraine Headache
The standard medical treatment for migraine heachache is primarily to use drugs to relieve symptoms, a costly and recurrent practice. Nothing is done to address the underlying causes. In contrast, the naturopath recognizes that most migraine headaches are due to food allergies, and abnormal prostaglandin metabolism caused by nutritional abnormalities results in excessive platelet aggregation. The approach is straightforward, as follows:
Hypertension
Patients with so-called idiopathic, or essential, hypertension can be treated very effectively if they are willing to make the necessary lifestyle changes, as follows:
The causes of high blood pressure are not unknown, but they are generally unheeded.
Lifestyle modification is crucial to the successful implementation of naturopathic techniques—health does not come from a doctor, pills, or surgery but rather from patients’ own efforts to take proper care of themselves. Unfortunately, our society expends considerable resources to induce disease-promoting habits. Although it is relatively easy to tell a patient to stop smoking, get more exercise, and reduce his or her stress, such lifestyle changes are difficult in the context of peer, habit, and commercial pressure. The ND is specifically trained to assist the patient in making the needed changes. This involves many aspects: helping the patient acknowledge the need; setting realistic, progressive goals; identifying and working through barriers; establishing a support group of family and friends or of others with similar problems; identifying the stimuli that reinforce the unhealthy behavior; and giving the patient positive reinforcement for his or her gains.
ACCOUNTABILITY IN NATUROPATHIC MEDICINE
Acceptance of a profession typically is seen to derive from sanctions associated with educational institutions, professional associations and licensing boards.
It is extremely important to realize that the establishment of standards and especially credentialling standards is critical for the public to know . . . whatever the discipline is.
Although naturopathic medicine in the early part of the twentieth century was unique, clinically effective, and powerfully vitalistic, it suffered because it had not reached maturity in terms of professional unification, scientific research, and other recognizable standards of public accountability. These goals have finally been achieved during the two decades of 1978 to 2000.
Naturopathic medicine has responded to the need not only to integrate the best that conventional and natural medicine have to offer, but also to address the issues of public safety, efficacy, and affordability through the following mechanisms:
These are well-accepted mechanisms for public accountability in all forms of licensed health care. Naturopathic medicine’s credibility has resulted in part from these important achievements by a unified profession.
SCOPE OF PRACTICE, LICENSING, AND PROFESSIONAL ORGANIZATIONS
NDs practice as primary care providers. They see patients of all ages, from all walks of life, with every known disease. They make a conventional Western diagnosis using standard diagnostic procedures, such as physical examination, laboratory tests, and radiological examination. However, they also make a pathophysiological diagnosis using physical and laboratory procedures to assess nutritional status, metabolic function, and toxic load. In addition, considerable time is spent assessing the patient’s mental, emotional, social, and spiritual status.
Therapeutically, NDs use virtually every known natural therapy: dietetics, therapeutic nutrition, botanical medicine (primarily European, Native American, Chinese, and Ayurvedic), physical therapy, spinal manipulation, lifestyle counseling, exercise therapy, homeopathic medicine, acupuncture, psychological and family counseling, hydrotherapy, and clinical fasting and detoxification. In addition, according to state law, NDs may perform office surgery, administer vaccinations, and prescribe a limited range of drugs. Because NDs consider themselves an integral part of the health care system, they meet public health requirements and work within a referral network of specialists in much the same way as a family practice medical (allopathic) doctor. This network includes the range of conventional and nonconventional providers.
NDs (or NMDs) are licensed in 13 states (Alaska, Arizona, California, Connecticut, Hawaii, Kansas, Maine, Montana, New Hampshire, Oregon, Utah, Vermont, and Washington), the District of Columbia, and the two U.S. territories of Puerto Rico and the Virgin Islands. NDs have a legal right to practice in Idaho and Minnesota. Because no licensing standards exist in these two states and NDs also practice in other states without government approval, individuals with little or no formal education are still able to proclaim themselves NDs, to the significant detriment of the public and the profession. The American Association of Naturopathic Physicians (AANP, Washington, DC) assists consumers in identifying qualified NDs (http://www.naturopathic.org).
The scope of naturopathic practice is stipulated by state law. Legislation typically allows standard diagnostic privileges. Therapeutic scope is more varied, ranging from only natural therapies to vaccinations, limited prescriptive rights, and office surgery. In addition, some states allow the practice of natural childbirth. Many states identify NDs as primary caregivers in their statutes.
In addition to the Council on Naturopathic Medical Education (CNME), two key organizations provide leadership and standardization for the naturopathic profession. The AANP, founded in 1985 by James Sensenig, ND, and others, was established to provide consistent educational and practice standards for the profession and a unified voice for public relations and political activity. Most licensed NDs in the United States are AANP members. The Naturopathic Physicians Licensing Examination (NPLEx) was founded under the auspices of the AANP in 1986 by Ed Hoffman-Smith, PhD, ND, to establish a nationally recognized standardized test for licensing. NPLEx is recognized by all states licensing NDs. All states licensing NDs and all states in the process of attaining licensure have state professional naturopathic associations. The Alliance for State Licensing is an ongoing state licensure effort.
INTEGRATION INTO THE MAINSTREAM
The American public has increasingly turned to alternative practitioners in search of healing for a variety of conditions not ameliorated by conventional medical practices. Such conditions include otitis media, cardiovascular disease, depression, chronic fatigue syndrome, gastrointestinal disorders, chemical sensitivities, recurrent infectious diseases, rheumatoid arthritis, general loss of vitality and wellness, and many other chronic and acute conditions.
Unquestionably, the health care system is undergoing profound change. . . . Many . . . current aspects of health care have resulted from a period of rapid change in the early part of this century. We are returning to a period of rapid change. . . . What is less certain is exactly where that change will lead. The task . . . is to identify and understand the forces of change and describe these forces so that [we] can make [our] decisions more wisely. (Bezold, 1986)
Examples of Integrative Steps
Naturopathic medicine has accomplished important steps in integrating into mainstream delivery systems.
Reimbursement: “Every Category of Provider” Law
In 1993, during health care reform in Washington State, the “every category of provider” law was passed. This law mandated that insurance companies include access to every category of licensed provider in all types of plans in insurance systems for the treatment of all conditions covered in the basic health plan. Washington State Insurance Commissioner Deborah Senn, who vigorously enforced this law, formed the Clinician Working Group on the Integration of Complementary and Alternative Medicine, bringing together medical directors, plan representatives, and conventional and CAM providers to identify issues and solutions to integration barriers in insurance systems. This step has been important in increasing consumers’ access to the health care providers of their choice, including licensed CAM professionals, as well as providing a solution focus to valid integration challenges.
Other reimbursement initiatives have also been successful. NDs throughout the United States are being integrated as primary care providers and specialists in traditional and managed care systems. The Pacific Northwest has emerged as a testing ground or model for integration because of the legislative and regulatory environment in the region.
Health Professional Loan Repayment and Scholarship Program
In 1995, Washington State’s Department of Health made naturopathic physicians eligible for student loan repayment in the state’s Health Professional Loan Repayment and Scholarship Program. Grants are awarded for student scholarships and student loan reimbursement to health care providers qualified and willing to provide health care in underserved areas or to underserved populations. The first and second naturopathic physician grants for loan repayment were awarded in 1998 and 2000.
King County Natural Medicine Clinic
No conventional model or infrastructure now exists in mainstream medicine for the systematic delivery of care that integrates natural and conventional providers. This integrative model is fundamental to naturopathic medicine. The King County Natural Medicine Clinic in Kent, Washington, is the first publicly funded integrative care clinic in the United States and has been a collaboration between Bastyr University and Community Health Centers of King County with funding provided by the Seattle King County Department of Public Health. This project forms an unprecedented union between three health forms: conventional medicine, natural medicine, and public health. The clinic has successfully applied a co-management model by using an interdisciplinary health care team co-led by naturopathic physicians and medical doctors, including nurse practitioners, acupuncturists, and dietitians. The clinic serves the medically underserved.
The Centers for Disease Control and Prevention and independent investigators have conducted research to study the provider-to-provider interactions and their effect on health care, patient satisfaction, and cost effectiveness. Other studies have compared results from natural and conventional therapies on specific conditions treated using this model.
Co-management
In The Emerging Integrative Care Model, Milliman and Donovan (1996) describe co-management as follows:
Naturopathic medical [co-management] is the practice of medicine by a naturopathic physician (N.D.) in concert with other care givers (N.D., M.D., D.O., L.Ac., D.C., etc.) wherein each care giver operates:
Co-management presents an opportunity to educate other providers to naturopathic medicine as well as a chance to learn from them and expand one’s information base and diagnostic and therapeutic potential. Most importantly, however, it greatly increases the therapeutic choices and quality of care to patients, often resulting in more supportive and less invasive therapies (minimizing iatrogenic diseases), while promoting healthier lifestyles and overall reduction in health-care dollars spent.
Continuous Quality Improvement
In 1996 the Washington Association of Naturopathic Physicians developed a quality assurance program consistent with national accreditation standards. This plan, known as Continuous Quality Improvement (CoQI), was completed and adopted by the Washington State Department of Health and was the first naturopathic CoQI plan approved in the United States. This process is used by all health care professions and enables the profession to define and continuously update its own standards of care. Jennifer Booker and Bruce Milliman, NDs, led this effort.
Residencies
Utah is the first state to require a 1-year residency for naturopathic licensure. Residency opportunities for NDs are growing rapidly through sites established by the naturopathic colleges. Cancer Treatment Centers of America offers a growing number of residencies and staff positions to naturopathic physicians. The National College of Naturopathic Medicine and Bastyr University offer a growing number of residencies throughout the United States. All naturopathic colleges also offer on-site residencies.
Hospitals and Hospital Networks
A number of hospitals across the United States continue to employ NDs as part of their physician staff in both inpatient and outpatient settings. Examples of the types of treatment centers established over the last 10 years are the following:
When health systems, insurers, and health maintenance organizations decide to cover alternative medicine, NDs are sought out in states with licensure. Even in states without naturopathic licensure, health systems and managed care organizations exploring integration have come to understand and value the depth of training of naturopathic physicians (Weeks, 1998).
EDUCATION
The trend of modern medical research and practice in our great colleges and endowed research institutes is almost entirely along combative lines, while the individual, progressive physician learns to work more and more along preventive lines.
The education of the ND is extensive and incorporates much of the diversity that typifies the natural health care movement. The training program has important similarities to conventional medical education (science based, identical basic sciences, intensive clinical diagnostic sciences), with the primary differences being in the therapeutic sciences, enhanced clinical sciences, clinical theory, and integrative case management. Naturopathic training places the pathology-based training of conventional physicians into the context of the broader naturopathic assessment and management model inclusive of nature, mind, body, and spirit in health care. To be eligible to enroll, prospective students must first successfully complete a conventional premedicine program that typically requires a college degree in a biological science. The naturopathic curriculum then takes an additional 4 years to complete. Residency opportunities are increasing rapidly throughout the United States, at the National College of Naturopathic Medicine, Bastyr University, and Southwest College of Naturopathic Medicine and Health Sciences. As noted previously, residency is now required for licensure in the state of Utah.
The first 2 years concentrate on the standard human biological sciences, basic diagnostic sciences, and introduction to the various treatment modalities. The conventional basic medical sciences include anatomy, human dissection, histology, physiology, biochemistry, pathology, microbiology, immunology and infectious diseases, public health, pharmacology, and biostatistics. The development of diagnostic skills is initiated with courses in physical diagnosis, laboratory diagnosis, and clinical assessment. The program also covers natural medicine subjects such as environmental health, pharmacognosy (pharmacology of herbal medicines), botanical medicine, naturopathic philosophy and case management, Chinese medicine, Ayurvedic medicine, homeopathic medicine, spinal manipulation, nutrition, physiotherapy, hydrotherapy, physician well-being, counseling and health psychology, and spirituality and health.
The second 2 years are oriented toward the clinical sciences of diagnosis and treatment while natural medicine subjects continue. Not only are the standard diagnostic techniques of physical, laboratory, and radiological examination taught, but what makes the diagnostic training unique is its emphasis on preventive diagnosis, such as diet analysis, recognition of the early physical signs of nutritional deficiencies, laboratory methods for assessing physiological dysfunction before it progresses to cellular pathology and end-stage disease, assessment and treatment of lifestyle and spiritual factors, and methods of assessing toxic load and liver detoxification efficacy. The natural therapies, such as nutrition, botanical medicines, homeopathy, acupuncture, natural childbirth, hydrotherapy, fasting, physical therapy, exercise therapy, counseling, and lifestyle modification, are studied extensively. Courses in naturopathic case analysis and management integrate naturopathic philosophy into conventional algorithms using the therapeutic order.
During the last 2 years, students also work in outpatient clinics, where they see patients first as observers and later as primary caregivers under the supervision of licensed NDs.
As previously mentioned, four schools currently exist in the United States and two in Canada: Bastyr University, National College of Naturopathic Medicine (NCNM), the Southwest College of Naturopathic Medicine and Health Sciences (SCNM), the University of Bridgeport College of Naturopathic Medicine (UBCNM), and, in Canada, the Canadian College of Naturopathic Medicine (CCNM) and the Boucher Institute of Naturopathic Medicine. The oldest institution is NCNM, which was established in 1965 in Portland, Oregon. The largest institution and first to receive accreditation is Bastyr, established in Seattle, Washington, in 1978. Over the years Bastyr has broadened its mission also to include accredited degree and certificate programs in nutrition, acupuncture and Chinese medicine, midwifery, applied behavioral sciences, health psychology, exercise, and spirituality and health. SCNM, established in 1993, has developed an active research department. The UBCNM, established in 1997, is the most recent addition. Like its counterparts in the United States, CCNM in Toronto, Ontario, has a rapidly increasing enrollment. Naturopathic education is accredited by the CNME, recognized by the U.S. Department of Education. The CNME has granted accreditation to the naturopathic medicine programs at NCNM, Bastyr, SCNM, and UBCNM. Bastyr and NCNM also have institutional accreditation by the Northwest Commission on Colleges and Universities, SCNM has institutional accreditation by the Higher Learning Commission of the North Central Association of Colleges and Schools, and UBCNM has institutional accreditation by the New England Association of Schools and Colleges. All states licensing naturopathic physicians recognize the CNME as the official accrediting agency for naturopathic medicine. The offices of the CNME are located in Portland, Oregon.
RESEARCH
However, clinical decisions cannot be solely dependent on science, when, with the best of efforts and with billions of public and private dollars spent, medical research has yielded twenty percent (and in some narrow areas up to fifty percent) of medical procedures and practices as scientifically proven and efficacious.
There is a paucity of theories of medicine. . . . The theory of medicine has lagged seriously behind theories of other sciences . . . any unitary theory of medicine which identifies it exclusively with science is doomed to failure.
The primary intellectual problem facing medicine today is that the information base of medicine is so poor. For a profession with a 2,000 year history which is responsible in the United States for 250 million lives and spends over $600 billion a year, we are astonishingly ignorant. We simply do not know the consequences of a large proportion of medical activities. The . . . task is to change our mind set about what constitutes an acceptable source of knowledge in medicine.
The relationship between scientific research and the study of the healing power of nature, a traditionally vitalistic principle, is important. The scientific method is a well-accepted approach to communicating what we learn about medicine’s mysteries to others; however, it has been limited in its development by conventional medicine’s approach to research. Orthodox research appears to turn on the premise that the universe functions without telos or purpose. Connections are mechanistic. Clinical investigation is directed toward pharmaceutical disease management based on a single-agent, placebo-controlled, double-blind crossover trial.
What distinguishes naturopathic medicine’s clinical research from that of biomedicine (a term coined to refer to the currently dominant school of medicine) is not the presence or lack of science. It is a collective confidence in the perception of a vital force or life force. The arguments then follow. What is it? What exactly does it do and how? As Dr. John Bastyr noted in an interview in August 1989, “We all have an innate ability to understand that there is a moving force in us, that doesn’t necessarily need to be understood mechanistically.” Future scientific work and naturopathic medical research on this principle is bound by the shared perception that (1) there is a pattern in health and disease, (2) there is order in the healing process, and (3) order is based on the life force, which is self-organized, intelligent, and intelligible. Within this paradigm, we can research the life force.
Confirming and challenging clinical perceptions and even disproving core assumptions is fundamental to naturopathic medicine’s core values. Scientific methods must be challenged to find new approaches to test large quantities and types of clinical data, outcomes, and systems from naturopathic practices. So far, the reality of the healing power of nature (vis medicatrix naturae) has not been proved or disproved by the single-agent double-blind study. New models (e.g., outcomes research, field- and practice-based research, multifactorial models) provide fruitful methods for researching the validity of nonconventional medicine and offer new opportunities for research on conventional practices.
Until recently, original research at naturopathic institutions has been quite limited. The profession has relied on its clinical traditions and the worldwide published scientific research, as follows:
Research in whole practices [is] only recently gaining interest with the development of methodologies in practice-based and outcomes research. There is a lack of research in whole practices like naturopathy, Oriental medicine, or Ayurveda compared to conventional practice whether in a particular disease or in overall health outcomes. Biomedical research methods which are considered gold-standard by the scientific community have been typically developed to provide reliable data on a single therapeutic intervention for a specific Western disease entity. The requirements of these research methods distort naturopathic practice and may render it apparently less effective than it may actually be. The measures may not take account of residual benefits in a patient’s other health problems nor on future health and health care utilization.
Compounding the methodological difficulties of research in this medical variant, there are structural obstacles as well. Distinct from the situation in conventional medicine, there is only the beginning of a research infrastructure at the profession’s academic centers. Practitioners expert in naturopathic medicine and the individualization of treatment are typically not trained in rigorous comparative trials. Even if the infrastructure and training were in place, sources of funding remain few and small, and most funding agencies make their decisions on the basis of biomedical theories which naturopathy may directly challenge. When research is done on aspects of naturopathic treatment, more studies are done on substances rather than procedures or lifestyle changes. Without the economic incentives which favor the in-depth study of patentable drugs, trials in naturopathic therapeutics, often derived from a long history of human use, are smaller and with fewer replications. Many practices present special methodological or ethical problems for control, randomization, blinding, etc., perhaps making it impossible to perform a study as rigorous as some might wish. Nevertheless, there are numerous studies which yield indications of the effectiveness of individual treatments. (Calabrese et al, 1997)
As mentioned earlier, a comprehensive compilation of the scientific documentation of naturopathic philosophy and therapies can be found in A Textbook of Natural Medicine, coauthored and edited by Joseph Pizzorno, ND, and Michael Murray, ND. First published in 1985, the textbook was, until 1998, in a loose-leaf, two-volume set, published by Bastyr University Publications and updated regularly. The third edition (2006, Churchill Livingstone) consists of more than 200 chapters and references more than 7500 citations from the peer-reviewed scientific literature.
In the past 20 years, Bastyr University, NCNM, SCNM, and CCNM have developed active research departments, which has resulted in expanding publication of original research in peer-reviewed journals, both alternative and mainstream. In 1994, Bastyr University was awarded a 3-year, $840,000 grant by the NIH Office of Alternative and Complementary Medicine to establish a research center to study alternative therapies for human immunodeficiency virus infection and acquired immunodeficiency syndrome (HIV/AIDS). Of particular importance has been the approval and funding by the federal government’s National Center for Complementary and Alternative Medicine of numerous research studies as well as fellowships and postdoctoral study positions at the naturopathic institutions. The result has been a growing number of naturopathic physicians with strong research training and credentials.
THE FUTURE
We could have a significant and immediate impact on costly health care problems if the complementary and alternative medicine disciplines and interventions were widely available.
Naturopathic medicine is enabling patients to regain their health as NDs effectively co-manage and integrate care with pertinent providers, to their patients’ and the public’s benefit. Today’s ND, an extensively trained and state-licensed family physician, is equipped with a broad range of conventional and unconventional diagnostic and therapeutic skills. This modern ND considers himself or herself an integral part of the health care system and takes a full share of responsibility for common public health issues. NDs are healers and scientists, policy makers, and teachers and are active in industry and environmental issues.
The scientific tools now exist to assess and appreciate many aspects of naturopathy’s approach to health and healing. Conventional medical organizations that spoke out strongly against naturopathic medicine in the past now often endorse techniques such as lifestyle modification, stress reduction, exercise, consumption of a high-fiber diet rich in whole foods, other dietary measures, supplemental nutrients, and toxin reduction.
These changes in perspective signal the paradigm shift that is occurring in medicine. Emerging knowledge, high health care costs, and unmet health care needs continue to force this shift in perspective into changes in our current health care system. What was once rejected is now becoming generally accepted as effective. In many situations, it is now recognized that naturopathic alternatives offer benefit over certain orthodox practices. In the future, more concepts and practices of naturopathic medicine will undoubtedly be assessed and integrated into mainstream health care.
Historically, emerging bodies of knowledge in health care have formed into schools of thought and professions (with standards) as the public’s need for their services increased. Naturopathic medicine’s reemergence is no accident or anomaly. Naturopathic medicine has followed the developmental stages that health care professions typically undergo while becoming accountable to the public. Access has increased with increasing research, conceptual unity, and standards.
These models and standards in emerging CAM fields, including naturopathic medicine, hold answers to issues in health care, its delivery, and the health care system that are as significant as the interventions. With accreditation, licensure, reimbursement, ongoing research, and widespread public acceptance, the naturopathic clinical model is reaching professional maturity today.
 Chapter References can be found on the Evolve website at http://evolve.elsevier.com/Micozzi/complementary/
Chapter References can be found on the Evolve website at http://evolve.elsevier.com/Micozzi/complementary/