CHAPTER 4
Tooth Development and Disturbances in Number and Shape of Teeth
Göran Koch, Irma Thesleff, and Sven Kreiborg
Mechanisms of normal and abnormal tooth development
Teeth develop as epithelial appendages from the ectoderm covering the oral cavity. The morphologic aspects of tooth development at the microscopic level have been described in great detail long ago, and more recent research has started to uncover the molecular details underlying the morphogenesis of teeth, dental cell differentiation and extracellular matrix formation, and mineralization. The genetic regulation of normal tooth development has been elucidated by experimental studies mainly using mouse teeth as models, and studies in human molecular genetics have led to the identification of gene defects causing dental aberrations.
Principles of tooth development
Tooth development starts from placodes, local thickenings of the dental lamina forming as a stripe of oral epithelium at the sites of future dental arches. The placodes bud to the underlying mesenchyme which condenses around the bud. Rapid growth and folding morphogenesis of the epithelium leads to the cap stage of development. The shape of the tooth crown becomes established during the bell stage when the locations and heights of tooth cusps are set by additional foldings and growth of the epithelium. The odontoblasts and ameloblasts differentiate during the bell stage, and deposit the extracellular matrices of dentin and enamel, respectively. Differentiation, matrix deposition, and mineralization start from the tips of the cusps and proceed cervically, and after they reach the future cemento‐enamel junction, root development starts (Box 4.1).
Permanent (secondary) teeth develop from the successional dental lamina associated with the primary (deciduous) tooth germs, and their budding starts during the cap stage of primary tooth development. Also posterior molars form in succession from the dental lamina at the distal aspect of the previous molar. Both the primary and successional dental laminae contain stem cells which have the capacity to form teeth. Sox2, a known marker gene of stem cells, is expressed in the primary as well as successional dental lamina [1].
Bone formation is initiated in the maxilla and mandible only after the initiation and budding of primary teeth, but the subsequent development of alveolar bone from the mesenchyme surrounding the tooth germs is tightly coordinated with tooth morphogenesis. At the time of eruption, the teeth are surrounded by bone, and their eruption depends on precisely regulated bone remodeling, i.e., bone resorption between crown and the oral cavity and bone apposition at the base of the roots.
The most important mechanism regulating tooth development is the interaction between the epithelial and mesenchymal cells. During the initiation of tooth development, the epithelium has an instructive role and determines the type of the tooth to be formed as well as the odontogenic fate of the mesenchymal cells. The capacity to regulate tooth development shifts to the mesenchyme during budding and, subsequently, mesenchymal signals regulate the morphogenesis of the epithelium and the shape of the tooth. The differentiation of the odontoblasts, ameloblasts, and cementoblasts, as well as their matrix deposition, is also regulated by interactions between the different tissues. Hence, tooth development is controlled by a series of reciprocal tissue interactions. It is noteworthy that similar sequential and reciprocal cell interactions govern the development of all organs in the embryo.
Molecules regulating tooth development
The most important molecules regulating tooth development are those that participate in the signaling networks mediating epithelial–mesenchymal interactions. The actual signals are small peptides which are secreted by one cell and exert their influence on nearby cells through binding to specific receptors (Figure 4.1). This leads to changes in gene expression in the responding cell and subsequent changes in cell behavior. Extensive studies on the signaling molecules in teeth and other organs and in different animals have shown that they have been conserved to an astonishing extent during evolution. It is now known that the same signals regulate the development of practically all organs in the embryos of all species, but depending on the organ and stage of development, the signals elicit different responses.

Figure 4.1 Cells communicate via soluble signal molecules regulating gene expression (transcription).
The actual signals belong to a few families, of which four have been mostly studied and they also, importantly, regulate tooth development. These are the Hedgehog, FGF (fibroblast growth factor), BMP (bone morphogenetic protein) and Wnt families. These signals are already expressed in the very early dental epithelium and regulate the initiation of tooth development. They also signal back from mesenchyme to epithelium and initiate epithelial folding and thereby shape development. During advancing development several signals are locally expressed in the dental epithelium in small clusters of cells, the dental placodes and the enamel knots, which are signaling centers regulating tooth initiation and crown shape. The placodes form at sites where the dental epithelium buds to mesenchyme. The primary enamel knot forms at the tip of the bud and induces the folding of the epithelium and onset of cap formation. In molars, secondary enamel knots appear at the sites of new cusps and produce signals, which stimulate the growth of the cusps (Figure 4.2). The signals regulate a great number of different transcription factors which determine the identities of cells and the ways in which the cells respond to signals. The central roles of several transcription factors in tooth development have been demonstrated by transgenic mouse experiments in which inhibition of their function has resulted in arrested tooth development. The chain of reciprocal interactions between the dental epithelium and mesenchyme, and the mediating signals and transcription factors, can be considered the “program of tooth development.”

Figure 4.2 Reciprocal interactions between the epithelial and mesenchymal tissues are mediated by conserved signaling molecules (BMP = bone morphogenetic protein; FGF = fibroblast growth factor; Shh = sonic hedgehog; Wnt). Numerous transcription factors are associated with signaling, and only those in which mutations cause dental abnormalities are indicated in the boxes (PITX2, MSX1, PAX9, RUNX2).
Disturbances in tooth development
Disturbances in tooth development are seen as:
- numerical variations (missing or supernumerary teeth)
- variations in size and shape of teeth
- defects in the mineralized tissues, enamel, dentin, and cementum, which may result from defects in the composition of the respective extracellular matrices and/or their mineralization (see Chapter 20)
- problems in eruption (see Chapter 5).
It is obvious that tooth development may be disturbed at different stages of morphogenesis, and that the end result depends on the timing and the type of insult. Variations in the number, shape, and size of teeth are commonly linked. In particular, hypodontia together with small and peg‐shaped teeth are often seen in the same patient. In these cases it is apparent that there is an inhibition of the early morphogenesis, and that it leads either to a complete arrest of development or to small teeth depending on the tooth type and extent of disruption. The most commonly missing teeth are the third molars, second premolars, and maxillary lateral incisors. It is believed that they are affected because they are the last teeth to develop from the respective dental placode. It is possible that the development of some of the teeth ultimately missing is actually initiated and may even have proceeded to early stages but that their development has been arrested because the tooth germs did not reach a threshold size.
Clinical aspects
Chronology of dental development
Data on the chronology of tooth development are usually given as mean values from series of observations. Even if the chronology in tooth development has a documented stability, deviations may occur. The timing of onset to completion of mineralization/development of the primary and permanent dentition is presented in Box 4.2 and Figures 4.3 and 4.4. The mineralization of the primary teeth starts during 14–18 weeks in utero. The root formation of the primary teeth is completed between 1.5 and 3 years. The crowns are halfway mineralized at birth and become fully formed during the first year of life (Figure 4.3). Mineralization of the permanent teeth starts at birth with the first molars. The incisors and canines start their mineralization during the first year of life, the premolars and second molars between the second and third years of life, and the third molar between the eighth and eleventh years of life. However, the normal range is wide. The crowns of the permanent teeth (except third molars) are generally completed between 5 and 7 years of age. Root development takes about 6–7 years. In general, the mandibular teeth develop earlier than the maxillary teeth (Figure 4.4). A marked sex difference has been observed in tooth formation, girls being on average half a year ahead of boys.

Figure 4.3 The chronology of mineralization of primary teeth.

Figure 4.4 The chronology of mineralization of permanent teeth.
Dental age estimation
The reasonable stability of the chronology of tooth development has been helpful in the evaluation of general growth and developmental disturbances and also in estimation of the chronologic age of children with unknown birth date. Dental age may be evaluated from assessments of pre‐eruptive tooth formation as judged from orthopantomograms. Several systems have been developed (see Chapter 2) where various stages of tooth development are given numerical values (scores).
Terminology and definitions
The terminology used to describe congenitally missing teeth has been confusing, as terms such as agenesis, anodontia, aplasia, hypodontia, and oligodontia have been used interchangeably. More recently, Schalk van der Weide [2] proposed definitions to overcome this (Box 4.3).
Numerical variations in the primary dentition
Epidemiologic investigations report a prevalence of hypodontia between 0.1 and 0.7%. The mandibular central incisors are almost exclusively affected and then mainly the laterals. Oligodontia or anodontia is rare but may be found in connection with ectodermal dysplasia. There is a rather strong correlation between hypodontia in the primary and permanent dentition. The prevalence of supernumerary teeth varies between 0.3 and 0.6%. Ninety percent of all supernumerary teeth are located in the maxillary anterior region.
Numerical variations in the permanent dentition
Hypodontia is more frequent in the permanent than in the primary dentition, with a prevalence reported between 6 and 10% excluding the third molar. The most affected teeth are, in decreasing order, the mandibular second premolar (around 40%), the maxillary lateral incisor (around 20%), the maxillary second premolar (around 20%), and the mandibular central incisor (around 4%). Hypodontia in the permanent dentition usually affects two or more teeth in 50% of cases (Figure 4.5). Oligodontia and anodontia are rare. Symmetrical hypodontia often occurs for maxillary lateral incisors and second premolars. There is a particular relation between hypodontia and microdontia in the maxillary laterals and strong evidence that this form of hypodontia is inherited as an autosomal dominant trait.
Figure 4.5 Distribution of children according to number of missing teeth. The horizontal axis shows the number of missing teeth per child. The vertical axis is logarithmic and shows the absolute number of children. The proportion of children is given above each column.
Source: Rølling 1980 [4], figure 1. Reproduced with permission of John Wiley & Sons.
Hyperdontia, or supernumerary teeth, are found with a frequency of 0.1–3.6%. The most frequent supernumerary tooth is the mesiodens in the midline of the maxilla (Figure 4.6) or a supernumerary lateral incisor in the maxilla. Supernumerary teeth are common in children with clefts and in several syndromes, e.g., cleidocranial dysplasia, Kreiborg–Pakistani syndrome, familial adenomatous polyposis (FAP), and tricho‐rhino‐phalangeal syndrome.

Figure 4.6 Mesiodens in an inverted position in the midline of the maxilla.
Syndromes involving congenitally missing teeth
There are a great number of syndromes with reported congenitally missing teeth. When any of the recently developed computer‐aided syndrome diagnosis systems, e.g., OMIM (Online Mendelian Inheritance in Man), POSSUM (Pictures of Standardized Syndromes and Undiagnosed Malformations), or LDDB (London Dysmorphology Database), are consulted more than 100 syndromes with missing teeth as a trait are presented. The most common syndromes with missing teeth are listed in Box 4.4.
Treatment of children with missing teeth or hyperdontia
In the primary dentition there is often no need for treatment unless there is a very severe oligodontia or anodontia. In such cases, uncomplicated prostheses are prepared to facilitate speech and also to be a psychological support. Such treatment can also be necessary in situations where a large number of teeth have been lost due to trauma or caries.
Congenitally missing teeth in the permanent dentition need thorough treatment planning and a serious consideration of different therapies in order to save tooth substance and to optimize the outcome in a life‐long perspective. In the premolar region, the treatment is mostly aimed at spontaneous closure of the space supported by timing of extraction of primary molars. In the frontal region, orthodontic treatment should always be considered before prosthodontic therapy. The hypodontia often concerns the lateral incisors in the maxilla. The morphology of the canines is important if they are expected to erupt in the place of a missing lateral incisor. However, slight grinding and morphologic rebuild with composites can achieve good aesthetics. Composite‐retained onlay bridges are also used to replace missing laterals (Figure 4.7a,b). Hypodontia of permanent mandibular incisors may result in a frontal collapse with a deep overbite (Figure 4.8). Early prosthetic treatment in the mandible is therefore indicated, e.g., an onlay bridge. In cases with extensive lack of teeth a multidisciplinary team approach is strongly recommended [3]. In this team, specialists in pediatric dentistry, orthodontics, oral surgery, prosthodontics, radiology, and a consulting psychologist should be represented. The treatment will often cover a 10–20‐year period and may involve orthodontics, tooth transplantations (auto), implants, and fixed and removable prosthodontics. This team should follow the child from the time when the diagnosis of oligodontia or anodontia has been settled and continuously plan and supervise the treatment to adulthood [1–3]. In Figure 4.9a to 4.9h, the treatment of a boy with ectodermal dysplasia is presented, following a team approach model.
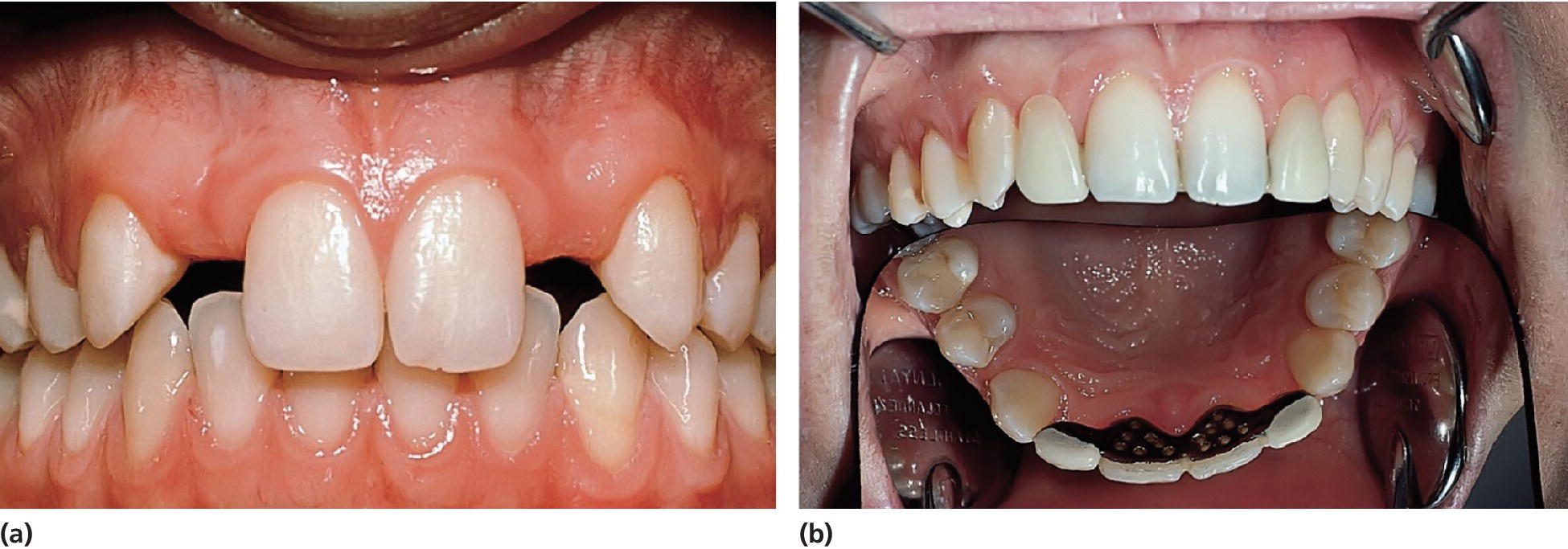
Figure 4.7 (a) Hypodontia of the permanent maxillary lateral incisors in a 15‐year‐old boy. (b) The same boy with the laterals replaced with a composite‐retained onlay bridge. The material in the Rochette bridge is stainless steel and fused porcelain.

Figure 4.8 Hypodontia of permanent mandibular incisors in an 18‐year‐old boy resulting in elongation of the maxillary central incisors and a deep bite.
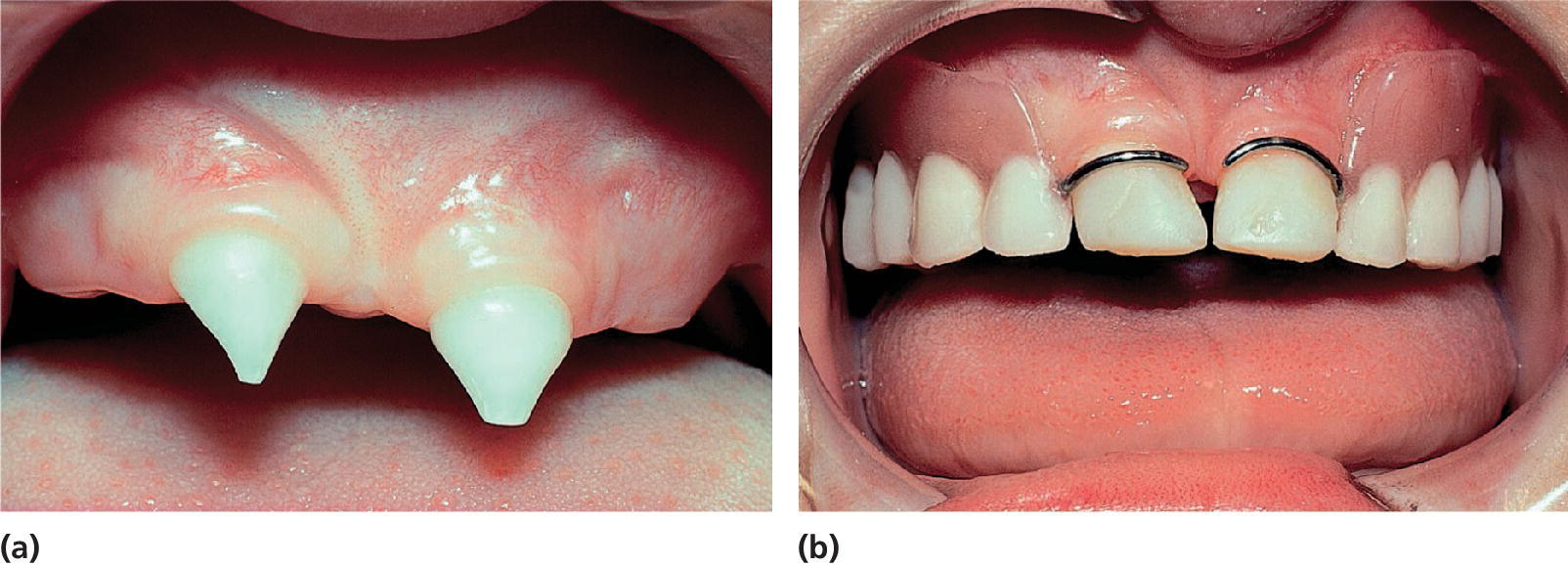



Figure 4.9 A boy with ectodermal dysplasia. (a) Intraoral view at the age of 2 years. Conically shaped primary incisors 51 and 61. (b) Teeth 51 and 61 rebuilt with composite resin and a removable partial denture in the maxilla at the age of 3 years. (c) Radiographic examination at the age of 4 years. No teeth in the mandible. In the maxilla 16, 11, 21, 26 and 53, 51, 61, 63 are present. (d) Two fixtures installed in the mandible at the age of 6 years. (e) Removable partial denture in the maxilla and implant retained over denture in the mandible at the age of 7 years. Note small, “primary” acrylic teeth. (f) Eruption of malformed permanent maxillary central incisors at the age of 8 years. (g) Temporary crowns 11 and 21 and rebuilt maxillary and mandibular denture at 18 years of age. (h) At 20 years of age, two fixed bridges were placed in the maxilla (53 and 63 were used in the bridges as they were stable and showed no root resorption) and two more implants were placed in the mandible, enabling the construction of a bridge in the mandible as well.
The treatment of hyperdontia is usually extraction or surgical removal of the supernumerary tooth, especially if there is a disturbance of the eruption of surrounding teeth.
Morphologic abnormalities
A variety of tooth morphology abnormalities can occur. As already discussed, tooth morphology is predominantly determined by genetic factors. Consequently, many aberrations are better understood in an anthropological context. However, there are also a number of external influencing factors, e.g., effect of cytotoxic medication, trauma, radiation, or pulpal complications to the teeth during their development.
Variation in tooth size
Generally men have larger teeth than women. Racial differences have also been seen. Tooth size is defined as abnormal when dimensions deviate two standard deviations from average. The deviation may be general or local and may involve the whole tooth or only parts of it.
Microdontia is defined as teeth smaller than normal. General microdontia is a rare condition occurring in connection with congenital hypopituitarism, ectodermal dysplasia, and Down syndrome. Local microdontia, involving single teeth, is more common and often associated with hypodontia. Microdontia mostly concerns maxillary laterals and third molars. The frequency of microdontia in maxillary laterals is slightly less than 1%. Radiation to the jaws during tooth development may cause microdontia in the area involved. Macrodontia is defined as teeth larger than normal. General macrodontia is extremely rare but can be seen in cases with gigantism. Double formations might sometimes be misinterpreted as macrodontia (Figure 4.10a,b). In congenital hemifacial hypertrophy, macrodontia may be seen unilaterally in the affected side in combination with a difference in developmental stage (Figure 4.11a,b).

Figure 4.10 Double formation in (a) primary and (b) permanent teeth in the maxillary frontal region.
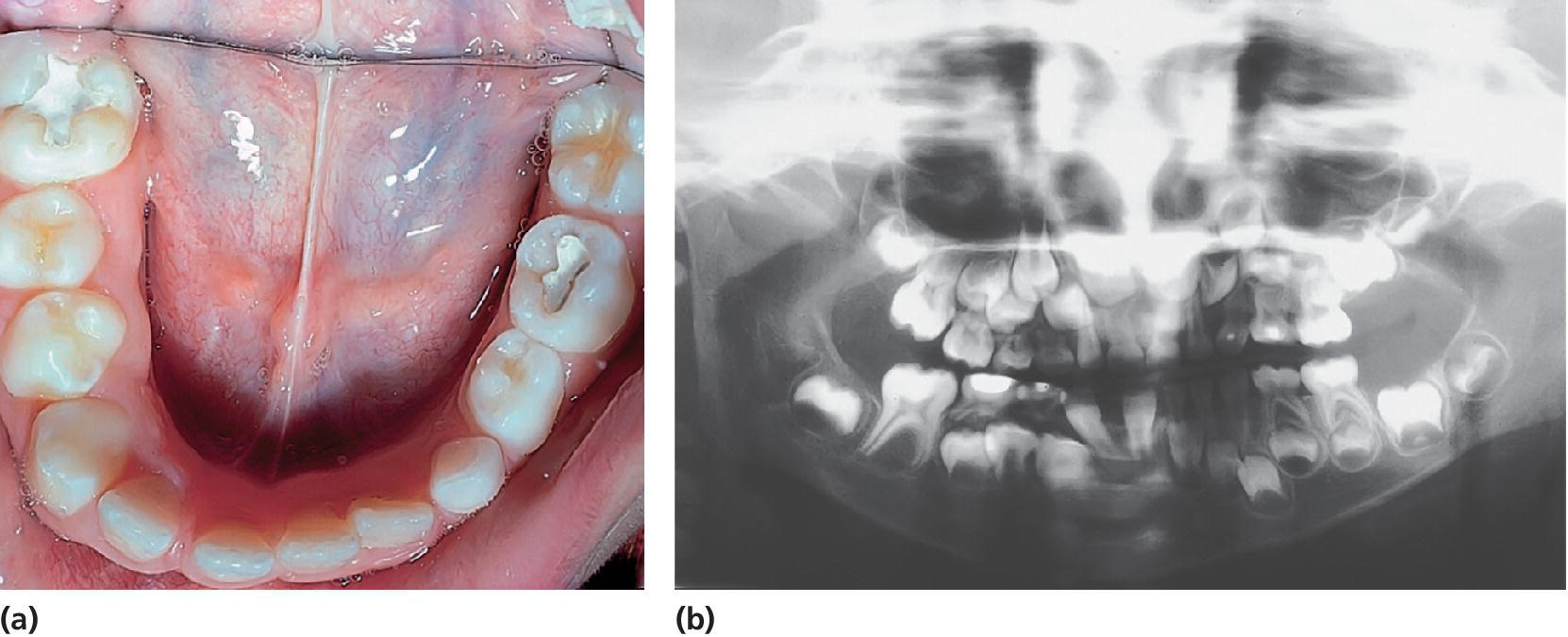
Figure 4.11 (a) A 6‐year‐old girl with hemifacial hypertrophy on the right side. Observe the difference in size and developmental stage between the left and the right sides. (b) Orthopantomogram of the same girl taken at 4 years of age. Compare the developmental differences between the permanent first molars in the left and right sides.
Rhizomicry means that the length of the root is shorter than the height of the crown. This is seen in osteoporosis and in dentinal dysplasia.
Local rhizomicry may be acquired as a result of trauma, pulpal infections, and radiation during root development and later due to root resorption. A familiar pattern of rhizomicry has been reported, predominantly affecting maxillary incisors and premolars. In cases of established heredity this aberration is designated SR anomaly (short root). Abnormally large roots, rhizomegaly, is an unusual anomaly mainly affecting maxillary canines.
Variation in tooth morphology
The maxillary lateral incisor frequently exhibits variation in the form of the crowns. Conical peg‐shaped form and accentuated cingulum often connected to the incisal edge are the most common aberrations. The “cusp‐shaped” cingulum of maxillary anterior teeth, talon cusp, can interfere with normal occlusion (Figure 4.12). The same abnormality may also be seen in premolars or molars and is called evagination. The two conditions usually contain an extension of the pulp. The treatment is therefore careful, successive grindings to avoid pulp involvement or, if this is not possible, to perform a partial pulpotomy (see Chapters 17, 18, and 20).

Figure 4.12 “Cusp‐shaped” cingulum of permanent central incisor interfering with occlusion.
The permanent maxillary first molar and also the primary maxillary second molar may appear with an extra tuberculum, Carabelli’s cusp, which is located on the palatinal side of the mesiopalatal cusp. The third molar exhibits the greatest variation of size and morphology of all teeth. The shovel‐shaped incisor is seen more frequently among Eskimos, Mongolians, and American Indians.
Dens invaginatus (Figure 4.13) is a common malformation due to an invagination of enamel epithelium resulting in a channel or lumen surrounded by hard tissues within the tooth. The anomaly occurs most frequently in the palatinal surface of maxillary laterals but can be found in other teeth. A frequency of 3% has been reported in a Swedish population. The defect varies in severity and a classification into three types has been described (Box 4.5).

Figure 4.13 Some examples of invaginations. Note enamel lining inside the lumen.
Invagination can be suspected at clinical examination if the tooth has a marked cingulum or palatal cusp. The entrance to the invagination can be extremely narrow, thus X‐ray examination is necessary.
Taurodontism (Latin taurus = bull) is a rare anomaly found in multirooted teeth in both dentitions and is characterized by elongated root‐stem with the furcation more apical than normally. The anomaly is genetically determined and the degree of taurodontism increases from the first to the third molar.
Double formation of teeth
In contrast to other dental anomalies, double formations appear more frequently in the primary dentition than in the permanent dentition. Double formations are mostly found in the front teeth area and are rare in the premolar and molar area (Box 4.6, Figure 4.10). The prevalence of double formations in the primary dentition is approximately 0.5–0.8%. In general, fusions are more common than gemination. Double formations in the primary dentition are often followed by aplasia of the permanent successor (20–75%). The anomaly is often observed in connection with Down syndrome, thalidomide embryopathy, and cleft palate.
Treatment of teeth with morphologic aberrations
Most of the teeth with morphologic abnormalities are easily reshaped and built up with composite resins by using the acid‐etch technique. Small peg‐shaped teeth, for example, can be transformed to normal size and appearance by such treatment (Figure 4.14a to 4.14d).

Figure 4.14 (a) A 4‐year‐old girl with incontinentia pigmenti. Observe the peg‐shaped primary incisors. (b) Orthopantomogram at the age of 8 years. Observe the missing premolars and molars. (c) At the age of 9 years, thin peg‐shaped permanent incisors are erupting in the mandible. (d) The same girl after rebuilding the mandibular incisors with composite resin.
The invagination requires special treatment attention because of the risk of poor quality and permeability of the dental hard tissues in the bottom of the invagination. Thus, the risk of pulpal involvement is obvious after eruption of the tooth.
Due to retention of food and plaque in the fossa, caries may attack the tooth before complete eruption. Therefore, sealing of all lingual pits in incisors should be undertaken as soon as possible after eruption. True invaginations should be treated as deep carious lesions. Softened or carious tissues should be removed. The risk of accidental pulp exposure of the buccal side during excavation due to improper inclination of the drill is obvious. Extra‐long drills should thus be used to avoid guidance of the incisal edge of the tooth (Figure 4.15). If the dentin at the bottom is hard and the tooth is without any pulpal symptoms, it is not necessary to extend the excavation into the frequently occurring canal seen as a small black spot at the bottom of the cavity. The bottom should be covered with a calcium hydroxide base and then filled with a composite resin material. If the pulp is exposed or if there are pulpal complications further treatment is dependent on root development, morphology, and accessibility of the canal.
Figure 4.15 The treatment of dens invaginatus. The lumen is reamed out with an elongated round drill. The bottom and buccal walls of the lumen are covered with calcium hydroxide compound.
Odontomas
Odontomas may develop from disturbances in dental organogenesis varying from malformation of a tooth to odontogenic hamartomous tumors. Odontomas are the most common odontogenic “tumor.” They occur mostly in the permanent dentition and can vary in size from some millimeters up to several centimeters. They are often revealed in radiographic examination with late tooth eruption or retentions. The odontomas can occur in compound or complex form. The compound odontoma consists of a varying number of tooth‐like formations where the different dental hard tissues can be clearly distinguished (Figure 4.16). The pathogenesis of compound odontomas may involve activation of the Wnt signal pathway since they are frequent in familial adenomatosis coli patients (caused by mutations in the Wnt inhibitor APC) and since structures resembling compound odontomas formed in transgenic mice as a result of Wnt signal activation [5]. The complex odontoma is a more or less hazardous arrangement of dental hard tissue (Figure 4.17). Odontomas are often well encapsulated and surgical removal is uncomplicated.

Figure 4.16 Radiographic examination of a compound odontoma.

Figure 4.17 Radiographic examination of a complex odontoma in a 2‐year‐old girl as a result of trauma.
Background literature
- AlQahtani SJ, Hector MP, Liversidge HM. Brief communication: The London atlas of human tooth development and eruption. Am J Phys Anthropol 2010;142:481–90.
- Gene expression in teeth: http://bite‐it.helsinki.fi/
- Jussila, M., Thesleff, I. Signaling networks regulating tooth organogenesis and regeneration, and the specification of dental mesenchymal and epithelial cell lineages. In: Signals, switches and networks in mammalian development. J Rossant, PPL Tam, WJ Nelson (eds), Cold Spring Harb Perspect Biol. Published online March 13, 2012.
- Nanci A. Ten Cate’s Oral Histology: Development, Structure, and Function, 7th edn. St Louis, MO: Mosby Elsevier, 2008.
- Nieminen P. Dental Anomalies: Genetics. John Wiley & Sons Ltd, 2001. DOI: 10.1002/9780470015902.a0006088.pub2
- Thesleff, I. Current understanding of the process of tooth formation; transfer from the laboratory to the clinic. Aust Dent J 2014;59 Suppl 1:48–54.
References
- 1. Juuri E, Jussila M, Seidel K, Holmes S, Wu P, Richman J, Heikinheimo K, Chuong CM, Arnold K, Hochedlinger K, Klein O, Michon F, Thesleff I. Sox2 marks epithelial competence to generate teeth in mammals and reptiles. Development 2013;140:1424–32.
- 2. Schalk van der Weide Y. Oligodontia: A clinical, radiographic and genetic evaluation. Thesis. University of Utrecht, 1992.
- 3. Bergendal B, Bergendal T, Hallonsten A‐L, Koch G, Kurol J, Kvint S. A multidisciplinary approach to oral rehabilitation with osseo‐integrated implants in children and adolescents with multiple aplasia. Eur J Orthod 1996;18:119–29.
- 4. Rølling S. Hypodontia of permanent teeth in Danish school‐children. Scand J Dent Res 1980;88:365–9.
- 5. Järvinen E, Salazaar‐Ciudad I, Birchmeier W, Taketo MM, Jernvall J, Thesleff I. Continuous tooth generation in mouse is induced by activated epithelial Wnt/β‐catenin signaling. Proc Natl Acad Sci USA 2006;103:18627–32.