| True or False | |
| Testosterone replacement is a cure for erectile dysfunction. | ____ |
| Aging causes a 50 percent decrease in testosterone levels. | ____ |
| Healthy males can make sperm into their eighties. | ____ |
| All men go through a midlife crisis by the time they are 50. | ____ |
| (Answers at end of chapter) | |
Have you been moody lately? Or maybe you’ve lost interest in sex? Do you feel weak and tired a lot?
You might be thinking these questions are geared toward women, but if you are a male and experiencing these symptoms, you might be going through “male menopause.”
In recent years, we’ve started to learn that many men experience some of the same types of symptoms women do as they reach their forties and fifties. In men, it may be due to low testosterone.
I realize that a lot of men and even some doctors don’t like the term male menopause. I agree, as it doesn’t describe the problem very well and probably discourages men from discussing their symptoms. After all, what male would want to talk about having “menopause”? That doesn’t seem normal.
Even though “menopause” includes the word “men,” it means permanent cessation of the menses. So no matter how catchy the phrase “male menopause” might be, if you’re not a woman, you can’t experience menopause. There’s another reason why “male menopause” isn’t a very useful term, and that’s because it’s misleading. The hormonal changes that are associated with menopause in women happen fairly quickly. Once the processes surrounding a woman’s menopause are complete, she no longer menstruates and her hormone levels are significantly and permanently changed. In men, the decrease in testosterone happens much more gradually, over the course of decades. There usually isn’t one particular period of time when a man can say, “I’m going through ‘the change’”—or a time when he can say, “Okay, that was it, my testosterone has now decreased.”
Many doctors use the term andropause to describe the decrease in testosterone in a more medically appropriate way. You’ll also see age-associated decreases in testosterone described as partial androgen deficiency in aging men (PADAM) or late-onset hypogonadism (LOH). For men who seem to have symptoms, you’ll see terms including androgen deficiency syndrome of the aging male and symptomatic androgen deficiency (SAD).
After the age of 60, 20 percent of men have low testosterone. After the age of 70, that number jumps to about 30 percent. Once men are 80, they have a 50 percent chance of experiencing a testosterone deficiency.
But what does it mean to have low testosterone? You might have heard that when your testosterone level drops, so does your sex drive, your vitality, your muscle strength, your joie de vivre.
It’s normal for a man’s testosterone level to decline as he ages. When you’re 60 or 70 or 80, you just don’t have as much testosterone as you did when you were 20 or 30. But this doesn’t have to mean an end to life as you know it. It also doesn’t mean that you should expect to go through the same things that your wife or female friends may have experienced when their estrogen levels dropped during menopause. You probably don’t have to brace yourself for mood swings or hot flashes. But you will experience some changes.
Before I explain the effects of low testosterone, I want to tell you a little bit about how your body makes testosterone and what it does. Then we’ll look more closely at the changes in testosterone that happen as you age, the signs and symptoms that can be associated with low testosterone, and what’s normally expected as we age, and what you can do if you think you have a problem.
Culturally speaking, testosterone is the hormone that represents masculinity. When men try to one-up each other by bragging about their accomplishments in sports or at work, we say, “That’s the testosterone talking.” When a man has to have the fastest car or the biggest TV, we blame that on testosterone, too.
The medical reality is a little different. When a male baby is developing in the womb, testosterone and hormones made from it are essential for his body to develop male genitalia. When a boy reaches puberty, it is androgens, including testosterone, that cause him to grow pubic hair and make his testicles and penis develop into their adult shape and size. Androgens are also what make a boy’s voice change and his face start to look like a man’s. In adult men, testosterone is important to keep the sexual organs working properly. Within the testes, it is essential for making sperm.
So it sort of makes sense to think that if you have lots of testosterone, you’re somehow more “manly” than a guy with a lower level, right? Well, it turns out that, within a pretty wide range of normal, guys have all kinds of testosterone levels. There might be some connections between testosterone levels and certain behaviors, like thrill seeking in young men, but for the most part, as long as your development during puberty was normal and you’re healthy today, your testosterone levels probably don’t have much to do with how much of a man you are. Your high school and college buddies simply were wrong!
Testosterone does a lot of other things in the body, beyond the development and maintenance of male physical characteristics. Various studies have found connections between testosterone levels and bone strength, muscle mass, metabolism, risk of diabetes, and even general quality of life. Testosterone may even have an influence on brain function.
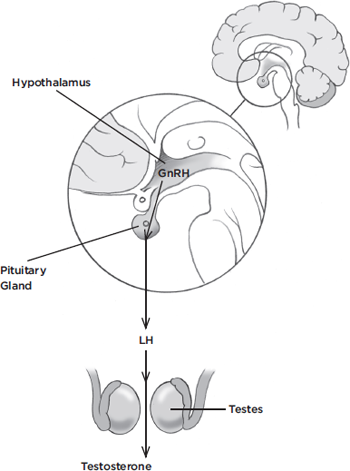
Most of the testosterone in a man’s body comes from the testes, from specific cells called Leydig cells. (A much smaller amount comes from the adrenal glands, which lie just above the kidneys.) The Leydig cells are regulated by hormones made in the pituitary gland, which sits way up in your skull at the base of your brain. And the pituitary gland itself gets messages from a part of the brain called the hypothalamus. The hypothalamus puts out a substance called gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to start releasing luteinizing hormone (LH), which travels through your body and tells the testes to get going and make some testosterone. When there is plenty of testosterone, the pituitary and hypothalamus reduce their signals. There are lots of other hormones, proteins, and other substances helping to regulate testosterone production, but this basic explanation should be enough to help you understand the changes that occur with aging and the idea of “male menopause.” You can follow the hypothalamic-pituitary-testicular axis in the diagram below.
As a man gets older, it’s normal for his testosterone levels to decline. Starting around age 40, most men will experience a decline of about 1 percent per year in total testosterone. Just as with other conditions, individual men have their own unique patterns. Some might see their levels decline more quickly, others more slowly. Some men’s levels never drop below what is considered “normal.” Others become testosterone deficient, at least according to their laboratory reports, with no associated symptoms.
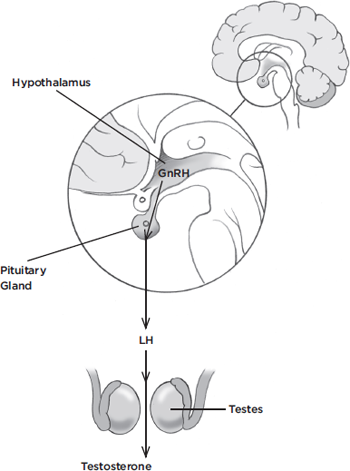
Hypothalamic-Pituitary-Testicular Axis—The hypothalamus receives signals from the brain to produce sperm and/or testosterone, causing it to signal the pituitary gland, which sends a unique signal to the testes and other glands involved in these processes.
Medical researchers are trying to determine exactly why testosterone levels drop as men age. It could be a decline in testicular function, a change in the regulation by the pituitary gland and hypothalamus, or a combination of the two. Some recent research has tried to separate out the decline in testosterone due to aging from declines due to other medical problems that often occur as we get older, such as gaining excess weight. This research suggests that the age-related decline is more likely to be due to something changing in the testes, while an obesity-related decline is more likely due to a change in the body’s regulation of testosterone. This sort of information might be useful in the future, because it could help us decide how to treat someone with signs or symptoms of low testosterone.
Many of my male patients have asked me if wearing tight underwear could have a negative impact on their testosterone levels. The answer is: absolutely not. Wearing tight underwear or pants may decrease sperm count, but sperm count and testosterone levels are two completely different issues. Your choice of underwear does not in any way impact your levels of testosterone.
Even as your testosterone levels decline over the years, you may not notice any adverse effects. And while there are symptoms associated with low testosterone, sometimes there can be other medical causes for these symptoms.
One symptom of low testosterone is erectile dysfunction (ED). It’s estimated that as many as 20 percent of men with ED have a testosterone deficiency. In these cases, ED medications such as Viagra and Levitra don’t work effectively; so if you’re taking one of these drugs and not seeing any results, it could be because you have low testosterone.
The following lists are adapted from guidelines created by the Endocrine Society, an organization dedicated to research on hormones and to the medical practice of endocrinology.1 If you experience these symptoms, it’s a good idea to go to your doctor and have your testosterone levels checked, as well as additional health screenings to rule out other possible causes.
• Reduced libido
• Decreased spontaneous erections
• Development of breast tissue
• Decreased body hair or the need to shave less often
• Small or shrinking testes
• Low sperm count (as measured by your doctor)
• A broken bone from mild injury, loss of height, or low bone density
• Hot flashes
The organization also suggests that your doctor consider checking your testosterone if you have some less specific signs and symptoms, too. Again, there are many possible causes for these signs and symptoms, so make sure to discuss them fully with your doctor.
• Decreased energy, loss of motivation, low initiative, or low self-confidence
• Depressed or “blue” mood
• Poor concentration or problems with memory
• Problems with sleep
• Anemia (low red blood cell count)
• A decrease in muscle strength or bulk
• An increase in body fat
• A decrease in performance at work or in physical tasks
If your doctor does think that your symptoms could be due to low testosterone, there are several different ways he or she may check your level. Bear in mind that many doctors aren’t in agreement that low testosterone can be the cause of these symptoms, so you might need to speak up and ask for the test.
There are a few things you should know about the test. Much of the testosterone in your body is strongly bound to a protein called sex hormone binding globulin (SHBG). About 2 percent is unbound, or “free,” and about 60 percent is weakly bound to other proteins, including a common one called albumin. Together, the free and albumin-bound portions are known as bioavailable testosterone, meaning that the testosterone is available for the body to use.
One common test, “total testosterone,” measures both the bound and free testosterone to give a single snapshot of the testosterone in your body. Sometimes, this test is all you need to make sure that your testosterone levels are within the range of normal. But it’s important for you and your doctor to understand that it can also be misleading.
The problem is that a test for total testosterone doesn’t really tell you how much testosterone is actually usable, or “free,” within your body. If your total testosterone level is low-normal, and your level of SHBG is higher than usual, your free testosterone might actually be low. Then again, with a low-normal total testosterone level and a normal or low level of SHBG, your body might have access to all the testosterone it needs. Levels of SHBG increase with age and also change with certain medical conditions, so if your total testosterone is on the low side, it may be worth checking your free or bioavailable testosterone, too.
You should also talk with your doctor about the time of day the test is performed. Testosterone levels change over the course of the day, so experts often recommend checking testosterone in the morning to get the most consistent and appropriate measurement.
Andropause is not the only reason a man’s testosterone level might be low. Low testosterone has also been associated with obesity and other health problems, certain medications, and radiation and chemotherapy for cancer. It can also be caused by a tumor in the pituitary gland. If you’re having problems due to low testosterone, don’t just assume it’s because you’re getting older. Make sure to talk with your doctor about all the possibilities.
If you and your doctor decide that you could benefit from testosterone supplementation, you have several options. There are testosterone patches; there are gels you rub into your skin; there are injections; and there is even a sort of pill that you tuck up against your gums. Your doctor can help you decide which one is the best choice for your medical needs and your lifestyle.
The safety of long-term testosterone supplementation isn’t known, and it’s too complex a topic to cover in this book. So just like with hormone replacement for women, we aim for the smallest dose for the shortest period of time. When I treat patients for symptoms that could be due to low testosterone, I monitor their testosterone levels, red blood cell count, and prostate-specific antigen (PSA); turn to page 198 for PSA information.
There are also a few drawbacks and side effects to testosterone supplementation. It is not a good choice for men who plan to start or expand a family in the near future, as supplemental testosterone will actually make you less able to conceive a child. Also, if a patient has prostate cancer, I don’t recommend supplemental testosterone, as it may worsen prostate cancer. Anytime I prescribe testosterone for a patient, I check in regularly to make sure that the treatment is actually working. If it doesn’t alleviate my patient’s symptoms, I stop the testosterone and look for other solutions.
Fred is 67 years old. He was widowed in his forties and remarried at age 58. He says his wife is the best thing that ever happened to him—”And she’s gorgeous, too!” Fred worked in construction most of his life until he retired 2 years ago. He has always been the upbeat one among his friends. He loves a good practical joke, and he and his friends like to play elaborate tricks on one another. When he retired, he knew he would have to make an effort to stay in shape, so he and his wife go to the gym together three times a week.
So when Fred came into my office complaining that he wasn’t feeling right, I knew to pay attention. “I’ve been feeling out of sorts lately, doc,” he said. “It’s nothing really major, but I just don’t have the energy I used to.” He said he can still think up good practical jokes, but he doesn’t have the oomph to put them together. At the gym, he felt frustrated. He was used to his workouts gradually getting easier over time, but lately, he just felt stuck. But the worst part, he confided, was that his marriage wasn’t what it used to be. He seemed embarrassed to talk about it, but he finally admitted that he was talking about intimacy. “I’m not even sure if the parts are still working,” he said, because he just didn’t feel much desire anymore. He couldn’t say for sure when all this started. “Maybe in the last year or so?” he speculated.
There are a lot of things that could be going on with Fred. First, I screened him for depression and other illnesses. Maybe retirement wasn’t agreeing with him. Anemia can cause low energy. All sorts of illnesses could be throwing him off his stride. As for the intimacy issues, I asked if anything had changed on an emotional level. Maybe he and his wife were having marital problems as they adjusted to their new lifestyle? I made sure I knew about any medicines he was taking. But I didn’t discover anything that would cause his symptoms.
While I was ruling out the other possibilities, I went ahead and checked Fred’s testosterone levels. It turns out that his free testosterone was low. I recommended a testosterone gel, and he agreed to give it a try. At his follow-up appointment, we rechecked his testosterone level, and it was back in the normal range. He said that the intimacy had returned to his marriage, and that he was feeling more energetic, both at the gym and in everyday life.
If a man develops prostate cancer, the treatment may include androgen deprivation therapy. Keeping levels of androgens, including testosterone, very low can slow the growth of a tumor or even cause it to shrink, at least for a while. Androgen deprivation therapy usually involves the use of drugs that shut down most of the body’s production of testosterone; low testosterone levels can also be accomplished by surgically removing the testes. When it comes to testosterone supplementation, many people worry that giving a man extra testosterone could cause a tiny, as-yet-undetected tumor to start growing out of control. There has also been concern that testosterone supplementation could cause a new cancer to develop.
If your doctor diagnoses you with low testosterone and you want to try testosterone replacement therapy, how much should you worry about prostate cancer? No one knows for sure, but you need to be aware of the latest recommendations and you should ask questions. Some doctors believe that there isn’t any risk, and that even men who have been treated for prostate cancer can use testosterone as long as the cancer seems to have been eradicated and the patients are carefully monitored. Other doctors hesitate to prescribe testosterone supplementation at all.
We’re still waiting for a definitive answer. A few years ago, researchers examined 19 different studies of testosterone replacement therapy.2 They looked at events such as prostate biopsies; elevated prostate-specific antigen (PSA), which can be a sign of prostate cancer; and prostate cancer diagnoses. (I’ll explain more about PSA in the next section.) Taken all together, these events were more common in men who took testosterone. But when the researchers looked at prostate cancer by itself, the difference was small enough that, statistically speaking, it may have been just a coincidence.
One argument for safety is that testosterone supplementation isn’t meant to raise your levels above what would be considered “normal,” so it shouldn’t be any riskier than having a normal testosterone level in the first place. A number of studies have looked for a connection between natural testosterone levels and prostate cancer, and the results have been mixed. They must have concluded that the data didn’t show any link between testosterone levels and prostate cancer risk. However, research is ongoing. A very recent study suggests that there could be a connection between higher natural levels of free testosterone and more aggressive forms of prostate cancer, at least in men over age 65.3 It remains to be seen what future studies will tell us.
The Endocrine Society’s guidelines advise against giving testosterone replacement therapy to men with certain abnormalities of the prostate, such as nodules (bumps) that can be felt on a physical exam. A lump or bump on the prostate could be an undiagnosed cancer. An elevated PSA level would be a reason to hold off on prescribing testosterone, too.
Before trying testosterone supplementation, ask your doctor about the possible risks and side effects, and follow your doctor’s instructions regarding follow-up tests and checkups.
I said I’d explain more about PSA, and since we’re on the topic of prostate cancer, this seems like a good place to do it. Prostate-specific antigen is a protein that’s produced by the prostate gland, and it can be measured with a blood test. Certain prostate problems, including infection and an enlarged prostate, can cause your PSA level to rise. So can prostate cancer.
1 Hit the heavy weights. Numerous studies have shown that lifting heavy weights can increase testosterone levels for several days after an intense workout.
2 Consider eating foods rich in vitamin A, vitamin E, zinc, and carnitine. These vitamins and minerals have been shown to increase testosterone levels. Good sources include chicken, fish, avocados, pumpkin seeds, peanuts, almonds, and sweet potatoes.
3 Limit alcohol consumption to no more than two beers or glasses of wine daily. Drinking large amounts of alcohol does not make you manlier; in fact, it will decrease testosterone levels.
For many years, PSA testing has been used as a screening method to check for prostate cancer. Many doctors do this test routinely as part of an annual physical. We all know that catching cancer early can be lifesaving, so this sounds like a great idea, right?
Actually, it’s a lot more complicated. Prostate cancer is pretty common, and in fact the American Cancer Society estimates that a man’s lifetime risk of being diagnosed with prostate cancer is about one in six.4 This cancer can be a killer. About 30,000 men die of it each year, and more than 90 percent of these men are middle-aged and older. But prostate cancer can also grow very, very slowly. Autopsy studies have shown that it is not uncommon for men to have prostate cancer and never even know it or be affected by it. We are starting to figure out which prostate cancers are likely to be dangerous and which ones are likely to be less harmful.
If the treatment for prostate cancer were more straightforward, then it would make sense to screen every man and automatically treat every cancer that was diagnosed. In fact, the treatments that are usually recommended have important side effects, including a risk of causing impotence. Depending on the treatment, other potential complications include urinary incontinence and bowel problems. If the cancer appears to carry a very low risk of spreading, one option is to hold off on treatment and just keep an eye on things, with regular tests to be sure the cancer isn’t growing. We used to call this watchful waiting, but that sounded too much like we weren’t doing anything, so now we call it active surveillance. For a lot of men, though, “low risk” prostate cancer is just as scary as any other cancer. They want it out of their bodies, no matter what. And that means some men are undergoing surgery, chemotherapy, or radiation treatment when, if they hadn’t had a screening test, they likely would have been just fine.
Another concern about using PSA testing to screen for prostate cancer is the fact that cancer isn’t the only thing that causes elevated levels. Many men will end up with a lot of worry, not to mention the discomfort of a prostate biopsy, only to find out that they’re just fine. Then again, when a PSA test catches a dangerous, high-risk cancer, screening seems like a very good idea indeed.
Because of this balance between the potential for saving lives and the risk of unnecessary biopsies and treatments, many expert organizations now recommend that men talk it over with their doctors before undergoing a PSA test. Once you have a better understanding of the potential risks and benefits, you can make the decision that’s right for you.
The American Cancer Society has some recommendations for screening that I think make a lot of sense. The following advice is based on their screening guidelines:5
• First, talk with your doctor. Make sure you understand what screening can and can’t accomplish and what will happen if your test is positive.
• Most men should have this discussion starting at age 50. Men at high risk should start earlier, at age 45; this includes African Americans and men whose fathers or brothers had prostate cancer before age 65. If you have a strong family history of prostate cancer, such as several close relatives who were diagnosed before age 65, start at age 40.
• If you choose screening, it should involve a PSA test and may also include a digital rectal exam (DRE). For a DRE, your doctor will insert a gloved finger into your rectum and feel the surface of your prostate to check for any lumps or other abnormalities.
• The schedule for future screening tests will depend on your PSA level.
• Over the years, continue to talk with your doctor about the pros and cons of prostate cancer screening. It’s likely that new information will become available, and you’ll want to know if anything important has changed.
If it’s true that testosterone can make men feel stronger, livelier, and sexier—and even help with erectile dysfunction—wouldn’t it make sense to give all older men the option of supplementing their decreasing testosterone?
It might, if we knew for sure that it would make a difference, and that there weren’t better, safer ways to achieve the same results. But we just don’t have that evidence yet. We also don’t know what risks might be involved in giving testosterone to otherwise healthy men. For now, though, I don’t know about you, but I’d prefer to avoid testosterone supplements if I’m not 100 percent sure I need them.
| Male Menopause: What’s Normal and Not Normal As We Age | |
| Normal | Not Normal |
| Having a little extra fat on your body, relative to muscle | Developing breast tissue |
| Sympathizing with a female spouse or partner who’s having hot flashes | Having hot flashes yourself |
| Losing some strength or muscle bulk if you haven’t been exercising lately | Losing strength or muscle bulk without a good reason |
| Recognizing that you don’t have the energy you did when you were 21 | Feeling like you don’t have any energy at all |
Answers to true/false statements: False, True, True, False