Chapter 17
Clinical applications
In selecting pulse sequences and measurement parameters for a specific application, MRI allows the user tremendous flexibility to produce variations in contrast between normal and diseased tissue. This flexibility is available when imaging both stationary tissue as well as flowing blood. For example, the use of both bright blood and dark blood MRA techniques described in Chapter 12 permits more accurate assessment of vascular patency and intravascular mass lesions. A typical patient examination acquires multiple series of images with different types of contrast (proton density, T1, T2) and different slice orientations (transverse, sagittal, coronal, oblique), providing the clinician with more complete information on the nature of the tissue under observation and increasing the likelihood of lesion detection and correct characterization. It is critical that the scan protocols be appropriate for the disease process under investigation, the organ or organs being imaged, and the individual patient. For example, breath-hold scans may not be possible for some patients. Also, an incorrect choice of scan parameters may render the diseased tissue to be isointense with the normal tissue. The MR physician may choose to provide detailed measurement parameters for each examination or have a predetermined regimen of scans that are to be performed by a technologist. Establishing fixed measurement protocols ensures the efficient operation of the MR scanner and that reliable, reproducible imaging examinations are performed. We advocate the second approach for clinical scanning.
17.1 General principles of clinical MR imaging
There are three fundamental principles that should guide the development of MRI scan protocols:
- Accurate and reproducible image quality.
- Good visualization of disease processes.
- Comprehensive imaging information for the area under observation.
Because ideal achievement of all three goals may not be practical, pulse sequences and/or scan parameters should be chosen that will provide adequate results within a clinically acceptable scan time. However, careful consideration should be made in prescribing scan protocols as the ability to visualize disease relative to normal tissue can be dramatically affected by improper scan protocols. One common approach to enhance the contrast between abnormal and background tissue is to make the signal of one of the tissues significantly different from the other one. For example, variation of the signal of fat through the use of unsuppressed and fat-suppressed techniques aids in the detection of lymph nodes. On T1-weighted images, lymph nodes have a low signal and therefore are conspicuous in a background of high signal fat, while on T2-weighted images, lymph nodes are relatively bright and their conspicuity is improved by decreasing the signal of background fat using fat suppression techniques. Following administration of a gadolinium-chelated contrast agent, lymph nodes have significantly shorter T1 values and produce a moderately high signal on T1-weighted images. The use of fat suppression is helpful to reduce the competing high signal of fat. The combined use of gadolinium-chelated contrast agents and fat suppression to increase the signal of diseased tissue and to decrease the signal from background fat, respectively, is widely used in various organ systems including the orbits, the bony skeleton, soft tissue of the extremities, and the breast.
An additional consideration is in the choice of pulse sequence, in that there may be differences in signal from flowing tissue or dramatic differences in image quality. For example, fat-suppressed spoiled gradient echo may be preferable to fat-suppressed spin echo when a concomitant evaluation of patency of vessels is desired, as in assessing vascular grafts for patency or infection, or for imaging extremities to determine soft tissue infection or vascular thrombosis. This is because spoiled gradient echo images display high signal intensity for patent vessels and low signal intensity for occluded vessels when acquired within a time window of 2–5 minutes following administration of gadolinium-chelated contrast media. In comparison, spin echo images may have a signal void from both patent and thrombosed vessels. Flowing tissue is commonly seen as a signal void on spin echo images due to the dephasing of moving spins during the gradient pulses, while blood clots produce a low signal due to the presence of fibrinous clot and increased T2* effects from blood breakdown products.
It is important when defining protocols for MRI studies to obtain a sufficient variety of sequences to provide comprehensive information, while at the same time not to be too redundant and generate excessively long exams. For example, our approach for imaging of the abdomen has been to employ a variety of short-duration T1- and T2-weighted sequences with the majority of them performed in the transverse plane, but also obtain at least one set of images in a plane orthogonal to the transverse plane. The particular choice of image orientation and number of slices for a measurement is dictated by the area of anatomy under observation.
17.2 Examination design considerations
The initial studies of MRI used primarily transverse T1- and T2-weighted spin echo techniques. As the modality has matured, it has become clear that imaging strategies must be modified beyond this elementary approach. There are several reasons for this:
- Imaging of organs in the plane of the best anatomical display. Imaging of the spine or the female pelvis requires the use of both sagittal and transverse images to best demonstrate the anatomical structures. Similarly, the evaluation of large masses in the region of the upper poles of the kidneys is facilitated by sagittal as well as transverse images. On the other hand, coronal images are useful for visualization of the left lobe of the liver. Some organs, such as cardiac MRI, have organ-specific planes that are particularly useful but are oblique to the standard planes mentioned above.
- Compensation for the most severe artifacts generated by various organ systems. Abdominal imaging is severely compromised by artifacts from respiratory motion. Imaging protocols that employ breath-hold spoiled gradient echo sequences (e.g., FLASH, spoiled GRASS), as described in Chapter 10, can produce images with substantial T1-weighting while minimizing respiratory artifacts. Cardiac gating is useful when imaging the thorax in order to minimize phase artifacts from cardiac motion. Three-dimensional volume gradient echo techniques are superior to 2D techniques for T1-weighted imaging of lungs, because the 3D techniques exhibit fewer phase artifacts from flowing blood and cardiac motion.
- Increased spatial resolution and/or signal-to-noise. Imaging of small anatomical regions such as extremities (e.g., ankles, wrists, knees) or the breast require specialized surface coils to maximize both signal-to-noise and spatial resolution.
- The use of contrast agents. Imaging of nonorgan-deforming focal lesions in the liver, spleen, and pancreas using intravenous gadolinium-based contrast agents requires rapid, breath-hold imaging techniques to capture the capillary phase of lesion enhancement. This approach necessitates the use of spoiled gradient echo techniques (e.g., FLASH or spoiled GRASS, either 2D or 3D versions) with temporal resolution of less than 20 seconds. In many instances, the visualization of contrast enhancement in T1-weighted images may be improved through the use of fat suppression to remove the competing high signals from fat.
17.3 Protocol considerations for anatomical regions
The following considerations and recommendations are offered for imaging various organ systems. They are intended to indicate general guidelines for use in developing imaging examinations. Exact sequence protocols are not provided because different manufacturers have different imaging capabilities and functions.
17.3.1 Brain
17.3.2 Neck
The use of a surface coil for neck imaging is essential due to the small volume of tissue under examination. High resolution T1- and T2-weighted sequences are useful for visualizing soft tissue. The use of gadolinium-based contrast agents may be helpful for tumor and lymph node detection, and for thyroid and parathyroid studies. The addition of fat suppression to postcontrast studies is helpful to delineate tissue. Uniform fat suppression may be difficult to achieve due to magnetic field distortions from the large magnetic susceptibility differences between the neck and the upper thorax.
17.3.3 Spine
A combination of T1- and T2-weighted images is important. Both sagittal and transverse images are valuable for examining the spinal cord and structural deformations such as disk herniations (Figures 17.4, 17.5, and 17.6). Transverse images allow excellent visualization of nerve roots and possible disk fragments. Use of spatial presaturation pulses is recommended to reduce artifacts from jaw, tongue, or esophageal motion in cervical studies or abdominal motion in lumbar studies. Administration of gadolinium-based contrast media and fat suppression are recommended in circumstances in which bony metastases are suspected.

Figure 17.4 Sagittal echo train spin echo T1-weighted lumbar spine image. TR,  ; effective TE,
; effective TE,  ; echo train length, 3. Anterior spatial presaturation pulse is used to suppress peristalsis and respiration artifacts.
; echo train length, 3. Anterior spatial presaturation pulse is used to suppress peristalsis and respiration artifacts.
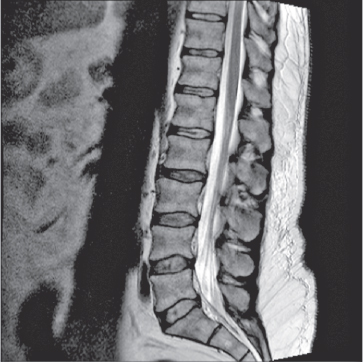
Figure 17.5 Sagittal echo train T2-weighted lumbar spine image. TR,  ; effective TE,
; effective TE,  ; echo train length, 17. Anterior spatial presaturation pulse is used to suppress peristalsis and respiration artifacts.
; echo train length, 17. Anterior spatial presaturation pulse is used to suppress peristalsis and respiration artifacts.
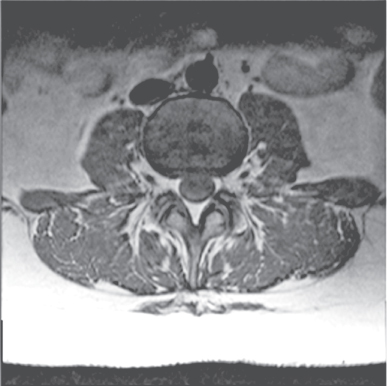
Figure 17.6 Transverse echo train spin echo T1-weighted lumbar spine image. TR,  ; effective TE,
; effective TE,  ; echo train length, 3.
; echo train length, 3.
17.3.4 Musculoskeletal
A combination of T1- and T2-weighted images is routinely used in musculoskeletal imaging. Images should be acquired in at least two orthogonal planes with high spatial resolution to ensure proper anatomical visualization (Figures 17.7, 17.8, and 17.9). Fat suppressed images are frequently valuable for detection of tumor, inflammation, or avascular necrosis and may replace T2-weighted images in some settings (Figure 17.10). T2*-weighted images are often used for visualizing fluid and bony detail. Use of gadolinium-based contrast agents is important for the evaluation of inflammatory and neoplastic disease, often in combination with fat suppression. When imaging small anatomical regions away from the magnet isocenter, field homogeneity may limit the usefulness of fat suppression (Figures 17.11 and 17.12).
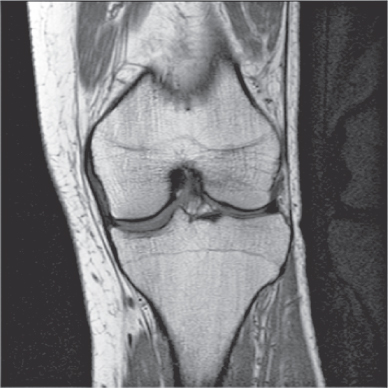
Figure 17.7 Coronal spin echo T1-weighted knee image. TR,  ; TE,
; TE,  .
.

Figure 17.8 Sagittal echo train spin echo proton density–weighted knee image. TR, 3000 ms; effective TE,  ; echo train length, 6.
; echo train length, 6.
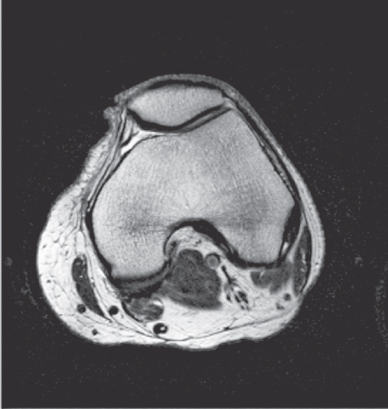
Figure 17.9 Transverse echo train spin echo proton density–weighted knee image. TR,  ; effective TE,
; effective TE,  ; echo train length, 11.
; echo train length, 11.
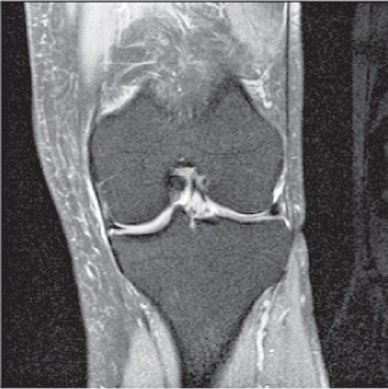
Figure 17.10 Coronal echo train spin echo proton density–weighted knee image with fat saturation. TR, 3000 ms; effective TE,  ; echo train length, 6.
; echo train length, 6.

Figure 17.11 Oblique sagittal spin echo T1-weighted shoulder image. TR,  ; TE,
; TE,  .
.
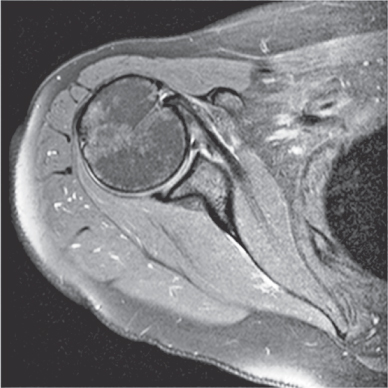
Figure 17.12 Transverse echo train spin echo proton density–weighted shoulder image with fat saturation. TR,  ; effective TE,
; effective TE,  ; echo train length, 7.
; echo train length, 7.
17.3.5 Thorax
Cardiac triggering may be of value to minimize motion artifacts from the heart. Transverse T1-weighted images provide good anatomical evaluation of the mediastinum and chest wall. T2-weighted transverse images are helpful, particularly in the evaluation of chest wall or mediastinal involvement with cancer. T1-weighted images acquired following administration of gadolinium-based contrast media provide similar and complementary information. Fat suppression is a useful adjunct when gadolinium-based contrast agents are employed. The lowered signal from fat improves the visualization of abnormal tissue enhancement, which is helpful for delineating the presence of chest wall invasion by malignant or infectious processes. Lesions in the lung apex and occasionally in the lung base require additional coronal or sagittal views. Breath-hold imaging following administration of gadolinium-based contrast media improves visualization of small peripheral lung lesions; metastases can be reliably seen at a diameter of  at
at  and at
and at  at
at  using this approach. A 3D gradient echo sequence is preferred for imaging lung parenchyma because the technique minimizes phase artifacts from cardiac motion. For most examinations, imaging between 2 and 5 minutes following contrast administration provides a good balance between contrast enhancement of lung masses with diminished enhancement of the blood pool. The prolonged retention of contrast in the vascular space in MR, compared to CT using iodinated contrast media, is advantageous for visualization of patent pulmonary arteries.
using this approach. A 3D gradient echo sequence is preferred for imaging lung parenchyma because the technique minimizes phase artifacts from cardiac motion. For most examinations, imaging between 2 and 5 minutes following contrast administration provides a good balance between contrast enhancement of lung masses with diminished enhancement of the blood pool. The prolonged retention of contrast in the vascular space in MR, compared to CT using iodinated contrast media, is advantageous for visualization of patent pulmonary arteries.
17.3.6 Breast
Optimal breast MR examination requires a dedicated multichannel breast coil to maximize spatial resolution. T1-weighted imaging using thin-slice 3D volume techniques are routinely used incorporating fat suppression. Lesion detection is achieved using serial, dynamic imaging following gadolinium-based contrast media administration and provides useful information on lesion characterization (see Figure 12.5). Many carcinomas exhibit intense early enhancement while most benign disease processes enhance in a delayed, less intense fashion. Further information regarding lesion morphology may be provided using high-resolution T2-weighted ETSE sequences. Morphology of lesions on gadolinium-enhanced T1-weighted images has become the primary method for lesion evaluation.
17.3.7 Heart and great vessels
Transverse cardiac-triggered T1-weighted segmented gradient echo sequences are essential in the evaluation of cardiac anatomy. When possible, breath-hold scanning, real-time imaging, or use of navigator echoes is preferred to minimize artifacts from respiratory motion. High spatial resolution is frequently needed, particularly in assessing congenital heart disease; therefore, a slice thickness of less than  is recommended. Coronal and sagittal triggered T1-weighted images may provide additional information in many instances. They are essential in the evaluation of congenital heart disease by providing anatomical information regarding vessels, airways, and cardiac chambers. The left anterior oblique sagittal plane is an important view for the evaluation of the thoracic aorta.
is recommended. Coronal and sagittal triggered T1-weighted images may provide additional information in many instances. They are essential in the evaluation of congenital heart disease by providing anatomical information regarding vessels, airways, and cardiac chambers. The left anterior oblique sagittal plane is an important view for the evaluation of the thoracic aorta.
The signal from flowing blood within the cardiac chambers is often heterogeneous as a result of changes in flow direction and velocity. For T1-weighted sequences, it is helpful to minimize the blood signal, both to reduce flow artifacts and to delineate vessels using dark blood techniques (Figure 17.10). Application of superior and inferior presaturation pulses or gradient dephasing may be required. Flow compensation should be avoided because it results in an increased signal from flowing blood. Alternately, refocused gradient echo techniques that produce a high signal from flowing blood (bright blood techniques) are used for the evaluation of chamber dynamics. Multiphasic techniques (cine MR) are particularly useful in the evaluation of wall motion and thickening, valvular disease, and shunts.
Useful image orientations in cardiac MR differ from the standard imaging planes used elsewhere and are tailored to the cardiac anatomy, which is usually in a double-oblique orientation with respect to the standard planes and varies from person to person. The short-axis view is useful for evaluating the pulmonary valve and for performing volumetric measurements (Figure 17.13). The four-chamber view is useful for evaluating septal defects, chamber size, the lateral walls and apex of the left ventricle, and the free wall of the right ventricle (Figure 17.14). Other views can be tailored to examine the major vessels and valves (Figure 17.15), the coronary vessels, or the left ventricle long axis. Single-shot echo train spin echo techniques can minimize cardiac motion artifacts and are useful as bright or dark blood techniques. For the evaluation of the aorta and major branches, a widely used technique is MR angiography employing a dynamic 3D gradient echo sequence following gadolinium-based contrast media administration.
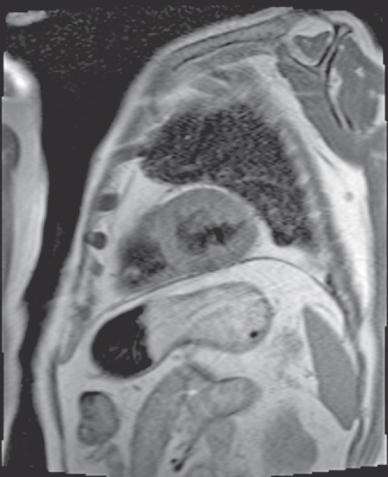
Figure 17.13 Short axis echo train spin echo dark-blood cardiac image. TR, 1142 ms; effective TE, 32 ms; echo train length, 21.
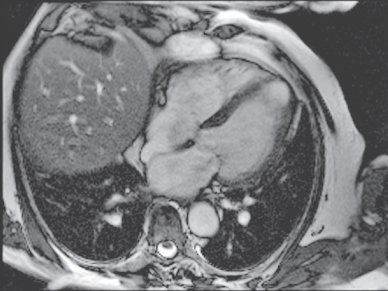
Figure 17.14 Four-chamber steady-state gradient echo bright-blood cardiac image. TR, 36.1 ms; TE, 1.8 ms.
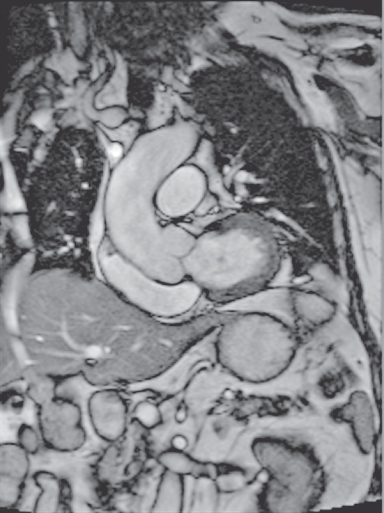
Figure 17.15 Oblique coronal steady-state gradient echo bright-blood heart image. TR,  ; TE,
; TE,  .
.
17.3.8 Liver
Both T1- and T2-weighted transverse images are important for evaluating the liver. Combining breath-hold and nonbreath-hold sequences is often useful since some patients can suspend respiration but cannot breathe regularly, while other patients breathe regularly but cannot hold their breath well. Most current protocols combine breath-hold T1- and T2-weighted sequences with breathing independent T2-weighted sequences. A spoiled gradient echo sequence is most often used for T1-weighted imaging, either 2D or 3D, assuming that very short TE are used; however, T1-weighted spin echo with respiratory compensation may be considered for some patients. When the image quality is acceptable, 3D techniques are preferred. For T2-weighted images, breathing averaged ETSE with fat suppression is a useful technique. The addition of fat suppression diminishes respiratory ghosts, removes chemical shift artifacts, and diminishes the signal of a fatty infiltrated liver, which permits good visualization of the liver capsular surface and facilitates lesion detection. In many cases, T2-weighted single-shot ETSE techniques acquired with and without fat suppression may be sufficient (Figures 17.16–17.18, and 17.19).
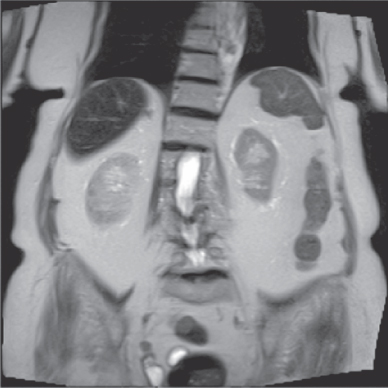
Figure 17.16 Coronal single-shot echo train T2-weighted image of liver and kidneys. Effective TE,  .
.
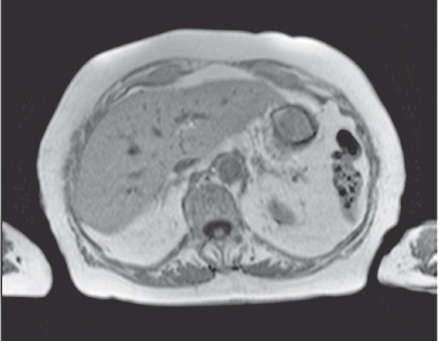
Figure 17.17 Transverse spoiled gradient echo T1-weighted liver image. TR,  ; TE,
; TE,  ; excitation angle, 70°.
; excitation angle, 70°.
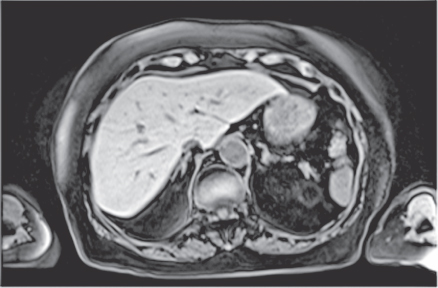
Figure 17.18 Transverse three-dimensional volume T1-weighted spoiled gradient echo liver image with fat suppression. TR,  ; TE,
; TE,  ; excitation angle, 10°.
; excitation angle, 10°.
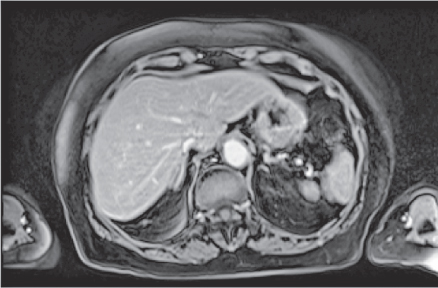
Figure 17.19 Transverse three-dimensional volume spoiled gradient echo T1-weighted liver image with fat suppression, following gadolinium – chelate contrast administration. TR,  ; TE,
; TE,  ; excitation angle, 10°.
; excitation angle, 10°.
The use of intravenous contrast agents significantly improves lesion detection over nonenhanced imaging techniques. Currently available contrast agents include various gadolinium-based complexes for T1 enhancement and ferumoxides for T2 enhancement. When using gadolinium-based contrast agents, it is important to image early after contrast (∼30 seconds) to maximize the specific enhancement features of various focal hepatic lesions (Figure 17.19). Spoiled gradient echo techniques (2D or 3D) are extremely useful to accomplish this goal. In addition, serial sequence repetition with additional acquisitions at approximately 1 and 2 minutes postcontrast may be routinely useful to visualize the temporal behavior of contrast uptake.
While contrast agents are used primarily to assess early perfusion of the liver, there are agents that also provide good contrast for hepatocyte phase imaging. Eovist is a gadolinium-chelate agent with hepatocyte phase imaging available 20 minutes following injection, facilitating both early perfusion and late hepatocyte phase imaging in one 20 minute study. Multihance also possesses a hepatocyte phase, but its slower biliary elimination causes this phase to occur one hour following contrast administration, requiring careful time management of the scanner and patient. Currently, the advantages of Eovist include the shorter hepatocyte phase development time and better visualization of the biliary tree compared to Multihance. Significant disadvantages include increased cost and lesser hepatic arterial enhancement when using approved dosages.
While not yet established as routine practice at all centers, the use of diffusion-weighted imaging is drawing increasing attention for hepatic applications. The motion sensitivity of diffusion poses challenges in the abdomen, as does the off-resonance sensitivity of the EPI readout. As a result, both shimming and respiratory techniques are important, with some centers using a breath-hold approach, others using a free-breathing approach, and still others using a respiratory navigator approach. All three approaches have drawbacks and limitations that can render them undiagnostic, but, when successful, abdominal DWI generates a high image contrast between normal liver parenchyma and malignant lesions.
17.3.9 Abdominal organs
T1-weighted breath-hold spoiled gradient echo techniques, either 2D or 3D, are useful for controlling respiratory artifacts in the abdomen. When the image quality is acceptable, 3D techniques are preferred. As with the liver, combining breath-hold with breathing independent sequences are advantageous. Single-shot ETSE T2-weighted sequences are particularly effective at demonstrating bowel and for distinguishing bowel from other entities. Transverse fat-suppressed and conventional spoiled gradient echo images are useful in combination both prior to and following administration of intravenous gadolinium-based contrast agents. Following contrast administration, the unsuppressed technique is useful to visualize capillary phase enhancement, while the subsequent acquisition of the fat-suppressed technique provides interstitial phase information. For the kidneys and pancreas, dynamic acquisition of fat-suppressed 3D gradient echo images enables excellent organ visualization. Imaging of the adrenal glands require noncontrast out-of-phase gradient echo images (Figures 17.20, 17.21, and 17.22).
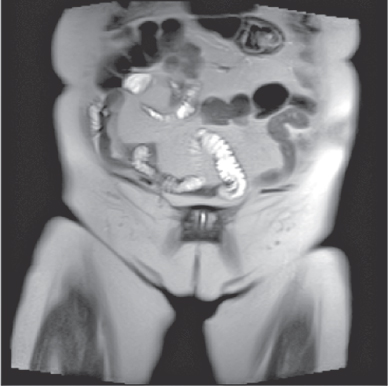
Figure 17.20 Coronal single-shot echo train T2-weighted image of bowel. Effective TE,  .
.

Figure 17.21 Coronal three-dimensional volume spoiled gradient echo T1-weighted image of kidneys with fat suppression, following gadolinium – chelate contrast administration. TR,  ; TE,
; TE,  ; excitation angle, 10°.
; excitation angle, 10°.

Figure 17.22 Coronal single-shot echo train spin echo T2-weighted image of common bile duct, following fat suppression. TR,  ; effective TE,
; effective TE,  ; TI,
; TI,  .
.
17.3.10 Pelvis
Transverse images are routinely used, while sagittal images provide a useful adjunct. T1-weighted images are frequently best performed as conventional spin echo or spoiled gradient echo (either 2D or 3D), whereas T2-weighted images may be acquired as breathing-averaged ETSE or single-shot ETSE. Thin slices (5 mm thickness) in the sagittal plane are necessary to optimally visualize the uterus and ovaries in the female and the seminal vesicles in the male (Figures 17.23, 17.24, and 17.25). Detailed imaging of the pelvis also requires high in-plane spatial resolution (512 × 512 matrices, ETSE, small FOV). T2-weghted scans, acquired as thin-slice 3D acquisitions, are useful for mulitplanar reconstruction. Gadolinium-based contrast administration is important in the evaluation of uterine and adnexal masses as well as in the evaluation and characterization of other pelvic masses such as rectal tumors. Fat suppression is an important adjunct to contrast administration when ovarian cancer is clinically suspected. Diffusion-weighted imaging is gaining acceptance for management of prostate cancer (Figure 17.26).
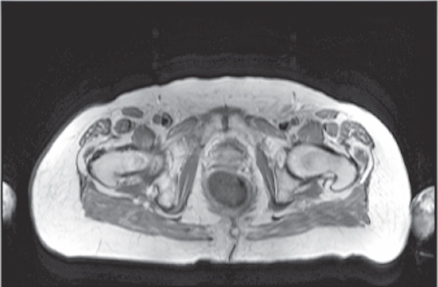
Figure 17.23 Transverse echo train spin echo proton density–weighted image of pelvis. TR, 4500 ms; effective TE,  ; echo train length, 7.
; echo train length, 7.
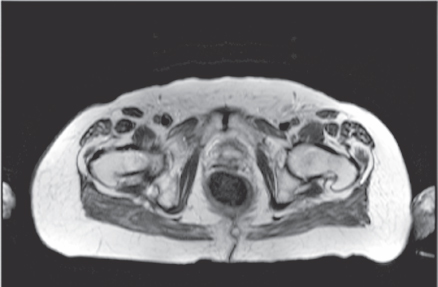
Figure 17.24 Transverse echo train spin echo proton density–weighted image of pelvis. TR,  ; effective TE,
; effective TE,  ; echo train length, 7.
; echo train length, 7.
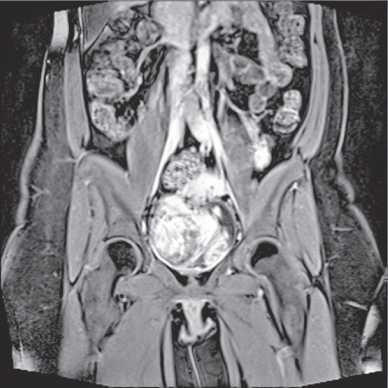
Figure 17.25 Coronal three-dimensional volume spoiled gradient echo image, following gadolinium–chelate contrast administration. TR, 4.9 ms; TE,  ; excitation angle, 10°.
; excitation angle, 10°.
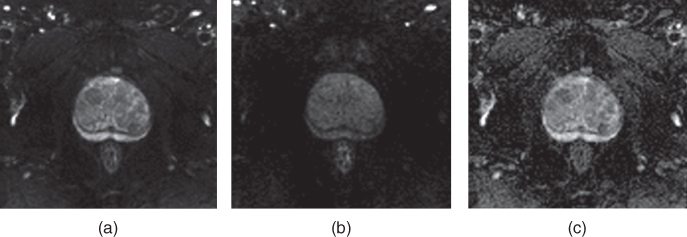
Figure 17.26 Diffusion-weighted imaging of the prostate at 3 T: (a) b-value, 50 s mm−2; (b) b-value, 800 s mm−2; (c) apparent diffusion coefficient map. Courtesy of Siemens AG, in cooperation with Dr. Engelhardt, Hospital Martha-Maria, Nuernberg, Germany.
17.4 Recommendations for specific sequences and clinical situations
17.4.1 T1-weighted techniques
Single echo spin echo
For routine T1-weighted imaging, a moderate TR is recommended (400–700 ms at 1.0 and 1.5 T) with a short TE (20 ms or less). This combination allows acquisition of a sufficient number of slices yet provides acceptable contrast between most tissues. The slice thickness and in-plane spatial resolution can be tailored to the particular anatomical region under examination. Spin echo sequences are typically not used at 3 T due to increased limitations from SAR.
Spoiled gradient echo
Imaging parameters include a relatively long TR (∼140 ms) and the shortest in-phase echo time  for unsuppressed or an opposed-phase echo time for fat suppressed imaging, one signal average, and an excitation angle of
for unsuppressed or an opposed-phase echo time for fat suppressed imaging, one signal average, and an excitation angle of  . These parameters maximize the number of slices, SNR, and T1-weighting, yet minimize artifacts and the measurement time. This spoiled gradient echo sequence is ideal for T1-weighted imaging in the abdomen, for imaging in multiple planes, and for imaging following administration of intravenous gadolinium-based contrast media. It is also a standard method for obtaining T1-weighted images at 3 T or higher. In general, 3D techniques are preferred over 2D techniques on current generation MR scanners, as the complete imaging volume can be scanned and thinner slices can be obtained. These require a minimal TR and a reduced flip angle. The use of parallel imaging techniques allows an image of high spatial resolution to be acquired.
. These parameters maximize the number of slices, SNR, and T1-weighting, yet minimize artifacts and the measurement time. This spoiled gradient echo sequence is ideal for T1-weighted imaging in the abdomen, for imaging in multiple planes, and for imaging following administration of intravenous gadolinium-based contrast media. It is also a standard method for obtaining T1-weighted images at 3 T or higher. In general, 3D techniques are preferred over 2D techniques on current generation MR scanners, as the complete imaging volume can be scanned and thinner slices can be obtained. These require a minimal TR and a reduced flip angle. The use of parallel imaging techniques allows an image of high spatial resolution to be acquired.
Out-of-phase gradient echo
Imaging parameters should include the shortest possible opposed-phase  , which must be shorter than the in-phase TE used. This technique allows easy detection of fat and water in similar proportions within a tissue volume through signal cancellation. For clinical use, the most important applications for this technique are the examination for fatty infiltration of liver and for benign adrenal adenoma. In both cases, the observation of signal drop observed on out-of-phase images compared to in-phase images permits the diagnosis of fatty infiltration. For adrenal glands, this technique is virtually pathognomonic for benign disease when the signal loss is uniform.
, which must be shorter than the in-phase TE used. This technique allows easy detection of fat and water in similar proportions within a tissue volume through signal cancellation. For clinical use, the most important applications for this technique are the examination for fatty infiltration of liver and for benign adrenal adenoma. In both cases, the observation of signal drop observed on out-of-phase images compared to in-phase images permits the diagnosis of fatty infiltration. For adrenal glands, this technique is virtually pathognomonic for benign disease when the signal loss is uniform.
Fat saturation
This technique is ideal when an expanded range of soft tissue signal intensities and decreased phase artifact from moving tissues containing fat is desired. Improved demonstration of tissue with a high protein content (e.g., normal pancreas) or detection of subacute blood are important uses for T1-weighted fat saturation techniques. When used following administration of gadolinium-based contrast media, the removal of the high signal intensity of fat results in easier discrimination of diseased tissue (e.g., diseased bowel or peritoneum, breast cancer, musculoskeletal neoplasms or inflammation). Fat-suppressed spin echo or spoiled gradient echo imaging is also useful in assessing the fat composition in certain masses such as adrenal myelolipoma, colonic lipoma, or ovarian dermoid cyst. Unlike out-of-phase gradient echo techniques, in which the maximal signal loss occurs in tissues where the fat and water are of equal proportions, fat suppression is maximal when the fat content in the tissue approaches 100%.
STIR
Musculoskeletal imaging benefits from the use of STIR imaging because of the relatively high signal from diseased tissue. Images resemble those obtained using fat-suppressed T2-weighted spin echo techniques. STIR is not as sensitive to magnetic field homogeneity as fat saturation and therefore is well suited for imaging small anatomical regions, regions away from the magnet isocenter, or for regions where there are large differences in magnetic susceptibility, such as the cervical spine. STIR sequences acquired using TI times for fat and for silicon suppression are useful for the investigation of breast implant rupture. Because long TR times are necessary, most implementations of STIR incorporate an echo train in order to dramatically shorten acquisition time. Performed as a breath-hold scan, this technique has achieved clinical utility in liver imaging.
17.4.2 T2-weighted techniques
Standard multiecho spin echo
Standard multiecho spin echo techniques are used when subtle differences in T2 between normal and diseased tissue are expected. A long TR (greater than  at
at  and
and  ) is used to minimize T1 saturation of most tissues, though CSF and other fluids are significantly suppressed in signal due to saturation. A short TE (less than 20 ms) is used to produce proton-density-weighted images while a long TE (80 ms or greater) generates T2-weighted images. Gradient motion rephasing is normally used on the long TE image in brain and spine imaging to minimize flow artifacts from bright CSF.
) is used to minimize T1 saturation of most tissues, though CSF and other fluids are significantly suppressed in signal due to saturation. A short TE (less than 20 ms) is used to produce proton-density-weighted images while a long TE (80 ms or greater) generates T2-weighted images. Gradient motion rephasing is normally used on the long TE image in brain and spine imaging to minimize flow artifacts from bright CSF.
Echo train spin echo
ETSE techniques are useful when high spatial resolution or decreased imaging time is desired for T2-weighted images (e.g., brain, spine, or pelvic imaging). These sequences are best used when T2 differences between normal and diseased tissues are significant since they result in an averaging of T2 information. Use of very long TR (greater than 3500 ms) allow coverage of anatomical regions and reduce the amount of signal loss from CSF saturation. Caution should be employed when using ETSE techniques for imaging the liver, particularly in the investigation for hepatocellular carcinoma, because the T2 difference between the tumor and background liver may be slight. This is normally not a problem if this technique is used in conjunction with spoiled gradient echo, either 2D or 3D, immediately following administration of gadolinium-based contrast media, as the latter technique is the most effective method for lesion detection.
Fat saturation
Fat-suppressed T2-weighted spin echo is useful for liver or musculoskeletal imaging. It results in a decreased phase artifact from respiratory motion of the abdominal wall and provides an expanded dynamic range of tissue signal intensities and increased conspicuity for focal lesions. It is an excellent technique for imaging capsular-based disease (e.g., hepatosplenic candidiasis or metastases spread through peritoneal seeding) since competing high signal from fat is removed and chemical shift artifacts are absent. Fat saturation can also be applied to echo train and single-shot echo train sequences. It is essential to use fat saturation when performing T2-weighted ETSE sequences of the liver to attenuate the signal of fat in the setting of fatty liver, because the high signal of fatty liver on nonsuppressed ETSE sequences can mask the presence of liver lesions. The use of fat suppression on T2-weighted sequences also facilitates the detection of lymph nodes, which appear relatively bright against a background of low fat signal. For single-shot ETSE sequences incorporating fat suppression, a more uniform suppression is obtained using inversion recovery combined with excitation spoiling.
17.4.3 Sedated or agitated patients
Optimal MR imaging results require cooperation from patients to minimize motion artifacts. For brain, spine, or musculoskeletal imaging, pads or restraints may be used to restrict patient movement. For abdominal imaging, patients who are unable to hold their breath because of sedation or decreased consciousness cannot be imaged with breath-hold imaging. Spin echo sequences may produce images of good quality in sedated patients, but poor image quality may result in agitated patients. Use of reordered phase encoding or navigator echoes may prove advantageous. For dynamic scanning following administration of gadolinium-based contrast media, images can be obtained using slice-selective 180° inversion pulse prepared snapshot gradient echo sequences (e.g., slice selective TurboFLASH, IR-prepared GRASS) followed by either regular or fat-suppressed T1-weighted spin echo techniques.
Patients who are unable to hold their breath or who are slightly agitated require imaging using rapid techniques that are motion insensitive. These include snapshot inversion pulse prepared gradient echo sequences for T1-weighted images and snapshot ETSE for T2-weighted images. These techniques are less sensitive to respiratory motion and acceptable image quality may be obtained. Imaging studies of sedated patients can produce results of good quality when combining breathing-averaged spin echo or navigator echo-based techniques with single-shot approaches.