YOU MAY WELL have had an operation before, but if it’s the first time you’ve had one this basic introduction may be helpful. Having an operation is the same as having surgery. Your surgeon will make an incision (a cut) in your skin, use instruments to remove your breast cancer or lymph nodes, and will then stitch the skin closed.
Surgery is the main treatment for breast cancer. It also allows your doctors to get more information about what type of breast cancer you have and whether your lymph nodes are involved so they can plan what further treatment you might need.
Your surgery is done in an operating theatre, which is a specially designed room that has all the equipment that your surgeon and anaesthetist need, and is kept spotlessly clean. It is in a separate part of the hospital from the wards and the clinics, with a recovery area next to it where you will wake up. As well as your surgeon, anaesthetist and their trainees, there are also surgical nurses and healthcare practitioners in the theatre who help with your operation.
In the NHS, your consultant surgeon (a surgeon who has finished their training) works with junior doctors who are training to become a consultant. These trainees may do some or all of your operation, under the supervision of your consultant, depending on how close they are to finishing their training. If you want to guarantee that your consultant will perform all of your operation, you may need to have surgery privately.
You might meet your consultant when you are first assessed in the breast clinic. Alternatively, if you were seen by a nurse or junior doctor, you might meet your consultant when you get your results. Finally, some patients do not meet their consultant surgeon until the day of their operation.
Most patients feel confident with the surgeon looking after them. They have an open and trusting relationship with them and feel they can ask them anything, no matter how small or stupid it may seem. Occasionally, however, patients don’t get on with their surgeon, normally because they don’t like their bedside manner, and find that they are too direct. Sometimes patients can also feel that they are not being listened to.
If you aren’t happy, you could ask your breast care nurse whether you could see a different consultant. Alternatively, you could ask your GP to refer you to another hospital, although this will delay your cancer treatment by a couple of weeks.
Before you can have your operation, your surgeon needs to make sure that you are fit enough to have an anaesthetic. Anaesthetics have several complications which can be serious (though these are rare – see here). Before your operation, you will be seen in a pre-assessment clinic by a doctor or a nurse to make sure that you can cope with the anaesthetic and the surgery. You may have a blood test, as well as a chest X-ray or a tracing of your heart rhythm (ECG).
The pre-assessment clinic will give you information about what to bring into hospital, where to go and when, whether you should take your normal medicines in the morning, and when to stop eating and drinking. If you are having a day-case operation you will need someone to take you home and stay with you overnight. If you live alone and have nobody to help you, you will probably be advised to stay in hospital for one night.
If you aren’t fit enough to have a general anaesthetic (for example, you have serious heart, lung or kidney problems), your surgeon might be able to do your surgery using only local anaesthetic. This numbs your skin and tissues, so although you may feel pushing and pulling while your surgeon removes your cancer, it shouldn’t hurt. You may also have a medicine to make you feel a little sleepy, so you won’t really be aware of what is happening.
WHAT TO PACK FOR YOUR OPERATION
With many operations, patients go home on the same day, but you may stay longer, depending on what operation you are having. This checklist will help you pack:
ESSENTIALS
● Purse with a little money (hospitals aren’t secure and things do get stolen).
● Mobile phone/tablet and charger.
● Books/magazines, etc. to keep you entertained.
TOILETRIES
● What you’d take for a weekend away – toothbrush and toothpaste as a bare minimum (hospital bathrooms just have hand soap).
CLOTHES
● Dressing gown to put over your hospital gown to keep you warm.
● A couple of spare pairs of knickers.
● Soft, non-wired bra for after the operation – front-fastening if you can find one (see here).
● Comfy clothes to go home in – ideally shirts and cardigans that you don’t need to pull over your head.
● Sleepwear – pyjamas are easier than a nightdress for your doctor to examine you.
● Slippers or non-slip footwear.
MEDICATION
● All your normal tablets along with a written list of when you take them and what dose (the ‘repeat prescription’ printout from your GP is a good source of this).
Anaesthesia means ‘without sensation’. There are two forms of anaesthetic – general and local. Most breast cancer operations are done using a general anaesthetic. This is a combination of drugs given by an anaesthetist (a doctor trained in giving anaesthetics) which make sure you are deeply asleep, unable to move and unable to feel pain during your operation (i.e. unconscious). Because an anaesthetic relaxes all your muscles, it means that the normal reflexes that stop food going into your windpipe don’t work. If you were sick during the surgery, food could travel into your lungs and cause pneumonia. Therefore you need to have empty stomach when you have a general anaesthetic to stop this happening. Your surgeon will also use a local anaesthetic drug to numb the wound and reduce the pain afterwards.
One of the main side effects of anaesthetic is feeling sick or being sick. This doesn’t happen to everyone, and you will be given medicine to prevent this. If you’ve been sick after an anaesthetic before, tell your anaesthetist. There is also a very small chance that you might be allergic to one of the drugs being used.
You might have a sore throat when you wake up because your anaesthetist will put a tube down your throat to help you breathe when you are asleep. If you have wobbly or loose teeth, there is also a risk that your teeth might be damaged or even fall out when the tube is put into your throat, though this is rare.
There are several complications that can happen with a general anaesthetic, and these include clots in the veins in your legs which can travel to your lungs, as well as heart and lung problems that can be very serious, especially if you have a relevant medical condition, such as emphysema or heart failure. These and other conditions might mean that the risks from a general anaesthetic are higher for you. Your nurse or doctor will talk to you about this when you go to the pre-assessment clinic.
You may be told to go to a main ward or to a waiting area next to the operating theatre. You will be taken to a bed where someone will get you ready for your operation, including giving you a hospital gown to put on and some compression socks to reduce the chance of getting a clot in your leg veins. If you are having simple breast surgery, you will be able to keep your own knickers on. If you are having a reconstruction involving your tummy, thighs or bottom, you will have to take your knickers off and may be given a sterile paper pair to put on. If you wear glasses, a wig or have dentures, you can keep these on/in until you are in the operating theatre. They should be at your bedside when you wake up.
Your anaesthetist will see you to explain what they are going to do, check your teeth and answer your questions. You will also meet either your consultant surgeon or one of their trainees who will check that you understand what operation you are going to have, answer any final questions, and mark your skin to show what side you are having surgery on (normally with a large arrow). They may also draw some additional guidelines to help guide them while you are asleep.
If someone has come with you to the hospital, they can wait with you while you are getting ready, but they can’t go with you to the operating theatre. Some hospitals have a waiting room, but it might be nicer for your relative or friend to wait in a coffee shop, or even go home. One of the ward staff will call them when you are back on the ward.
You may either walk to theatre or be pushed in a wheelchair, bed or trolley, depending on where you are waiting. You will either have your anaesthetic in a small anteroom or in the operating theatre itself. After your operation, you will wake up in a special recovery area where there are nurses and doctors to monitor you. Your surgeon will come to see you, but you might not remember seeing them due to the effects of the anaesthetic. When you are properly awake (which can take up to an hour), you will be taken back to the ward to have something to eat and drink.
Most patients now go home on the same day. If you are staying in overnight, you should be seen by a doctor every day, but it might be someone you haven’t met before, especially if you have your operation on a Friday.
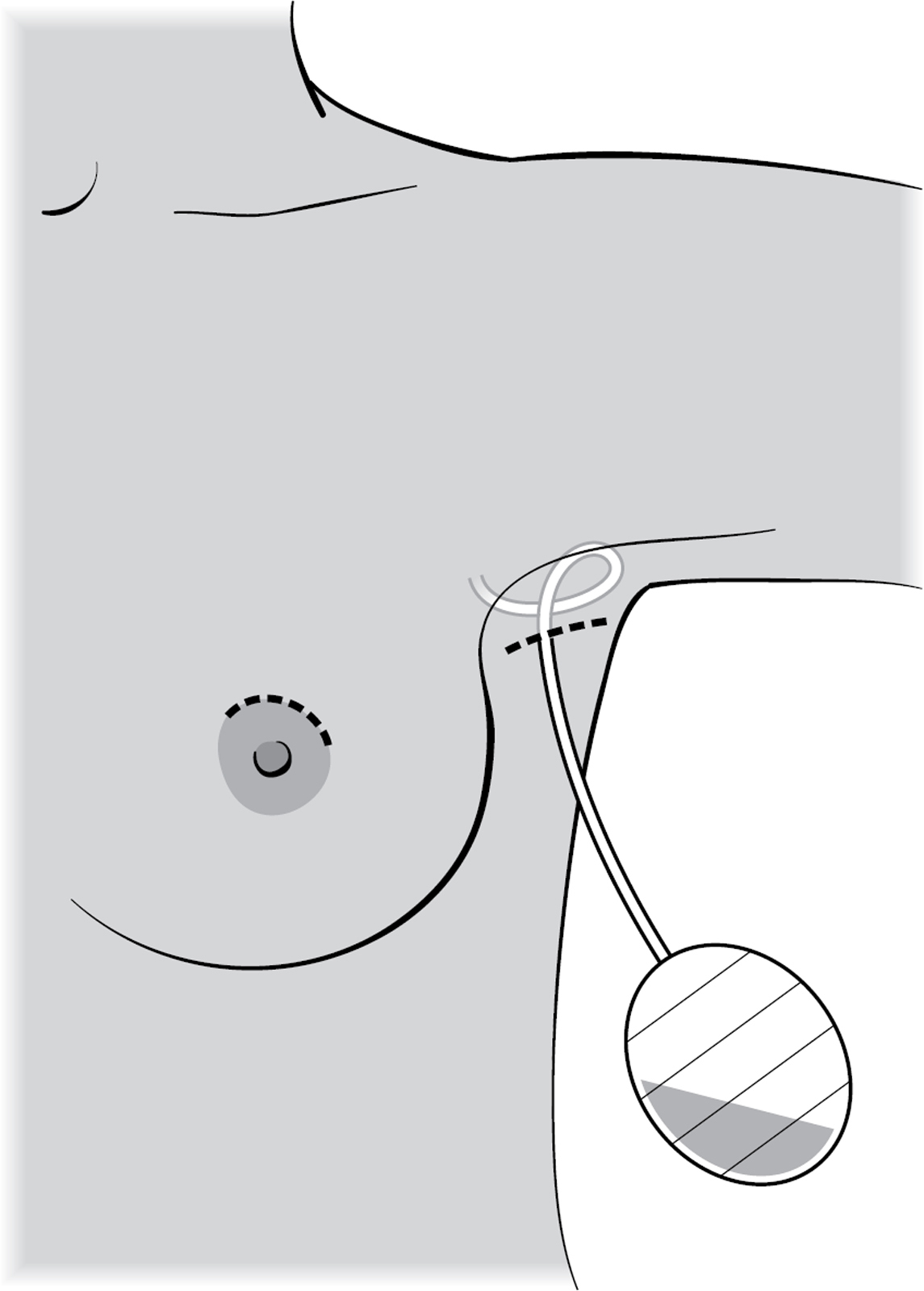
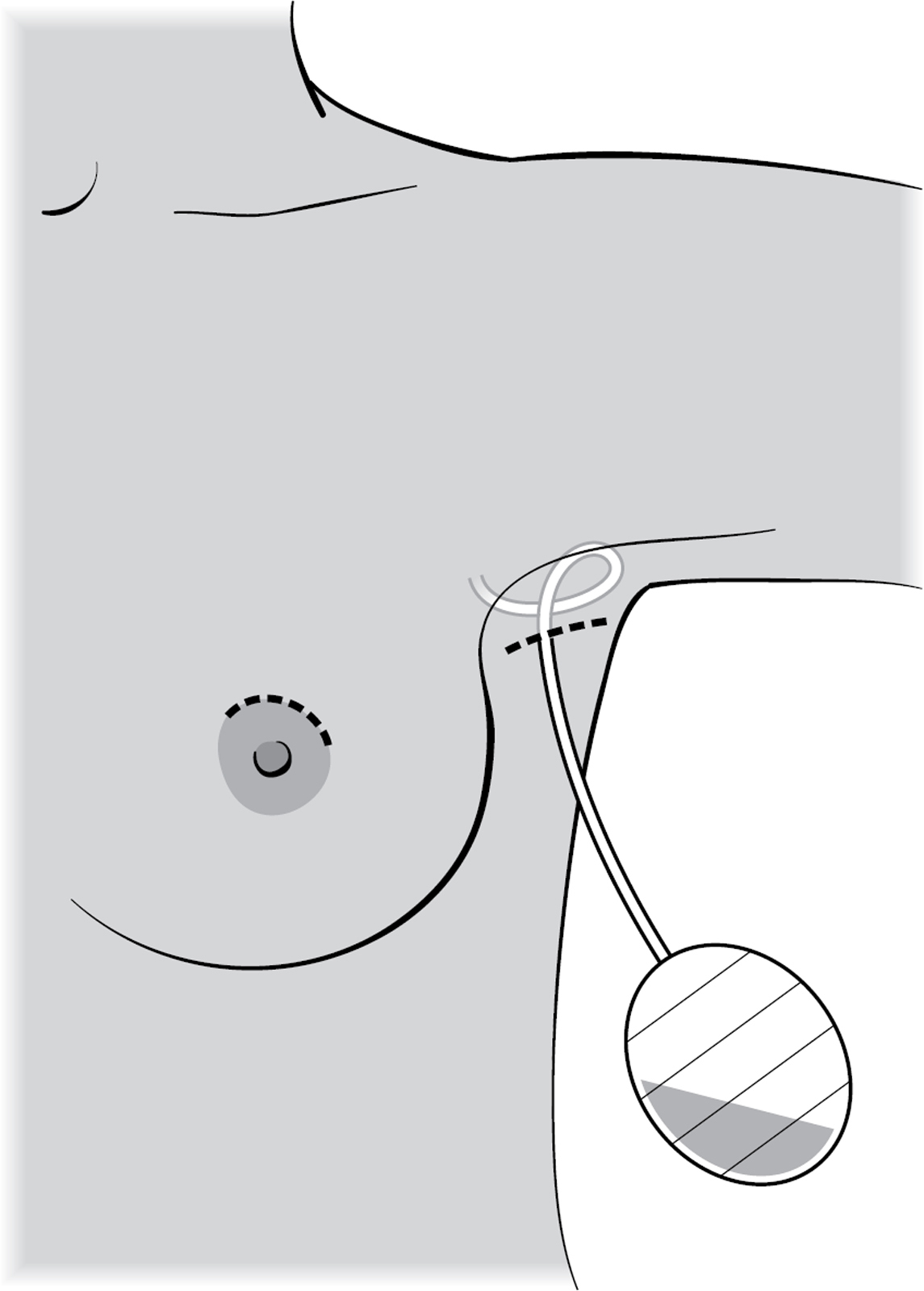
A drain is a long plastic tube, stitched to your skin, which is connected to a bottle. It uses suction to drain any fluid that collects in your wound. Some surgeons use very small drains to infuse local anaesthetic into your wound; these are removed before you go home. If you have had a more complex breast operation or have had a lot of lymph nodes removed from your armpit, you may be sent home with your drains. In this case, you will be given detailed instructions about how to look after them. The tubing on a drain is deliberately long so you can (for example) put the drain bottle on the floor and stand up without it pulling. If you have a drain, you will probably be given a short course of antibiotics to reduce the chance of a wound infection. Your drain may be removed at home by a district nurse, or you may have it removed in the breast clinic. Drains typically stay in for 3–5 days.
You should see a breast care nurse before you go home. They will tell you how to look after your wounds, give you advice about wearing bras and staying active when you are at home. You will be shown some shoulder exercises (see here) and will be given an appointment to come back for your results. They will also make sure that you know who to call if you have a problem at home. If you’ve had a mastectomy, you might be given a heart-shaped mastectomy pillow to use under your arm when you go to sleep, and if you have a drain, you should also be given a bag to keep the drain in (you will need to give it back when you next see your surgeon). Drain bags and mastectomy pillows can also be bought online.
Trish woke up from her mastectomy attached to various monitors recording her pulse, blood oxygen level and blood pressure. She wasn’t in any pain, but she felt a bit sick. She vomited once and felt much better. Her surgeon came to see her, but she doesn’t remember it. An hour after returning to the ward, she had a sandwich and a cup of tea. The next morning, the nurses removed her drain and let her go home. She was well enough to go out for a meal with her family that same evening.
Liz can’t remember being in recovery at all, and only remembers waking up on the ward. However, her lovely husband videoed Liz declaring her undying love for him under the influence of morphine. She didn’t believe it until she saw the video. She had very little pain and went home the next day with her drains still in place.
You will probably be a little sore after your operation. It is normally your armpit wound that hurts the most because you move your arms all the time, whereas your breast just sits in a bra. You will hopefully have been advised to buy some simple painkillers to take at home, and it is important to take them regularly. You can have 1g of paracetamol up to four times a day, and 400mg of ibuprofen (if it’s safe for you to take it) up to three times a day. Keeping active after your surgery (gentle walking) and doing your shoulder exercises will also help ease the pain. If you have had a large operation, like a reconstruction, it will be more painful. In this case, your doctor will prescribe some stronger painkillers, such as liquid morphine, to take as well.
After your operation, you will need to spend a minimum of one to two weeks recovering at home. If you are working, you can write yourself a sick note for the first week, but your surgeon or GP will need to give you one for the rest of your time away from work. If you have had a reconstruction (see Chapter 8), you might need several months off.
Take it easy for the first few days, but don’t spend hours on end lying on the sofa as this can increase the risk of you developing a blood clot in your leg. You should be able to do basic activities like getting washed and dressed without too much discomfort, and you should aim to walk regularly. It isn’t safe to drive until you can safely do an emergency stop without pausing to think whether it might hurt, and can easily turn to look behind you when reversing. This normally takes two weeks, so you might need to plan ahead and get help with things like food shopping and school runs. It is normal to feel tired after an operation, and you may feel that you need an afternoon nap for the first week or two until your energy levels pick up. You may also still be dealing with the emotional aftermath of a breast cancer diagnosis, so be kind to yourself and don’t stress too much if the laundry isn’t done and the house isn’t spotless.
You should see your doctor after two weeks to have your wound checked. If you have had a reduction or a reconstruction, you may have your wound looked at after a week. If your wound has healed and your surgeon is happy, they will give you the okay to go back to work and to exercise properly. They will also tell you when you can start wearing an underwired bra again.
Your doctor will also give you your results and discuss with you what other treatments you might need. The one treatment that most people are scared of is chemotherapy, and we both needed it. In the next chapter, we’re going to explain what chemotherapy is, what happens when you have it and, more importantly, tell you all our tips to help you cope with the symptoms.