A BREAST RECONSTRUCTION is an operation to recreate a breast shape after a mastectomy. Your surgeon will try to match your opposite breast size and shape. There are two ways to do this. The first uses a breast implant, and the second uses your own fat and muscle (called a ‘flap’ or ‘autologous’ reconstruction). Your reconstruction may be done at the same time as your mastectomy, or many months or years later.
When you hear that you need a mastectomy, your initial reaction may be shock, fear or even horror. This is completely normal. Most of us rarely think about what our breasts mean to us, and it’s even harder to think about them with regards to sexuality and body image when your judgement is clouded by the fact that you’ve been told that you have breast cancer. You might think that having a mastectomy means you’ll lose your confidence, femininity and sexuality but this isn’t necessarily true, and many women choose to stay flat-chested after surgery. However, having a breast reconstruction can boost your self-esteem and help you feel feminine and confident, especially if your breasts are important to you. There is nothing wrong with being concerned about your appearance, and having a reconstruction does not mean you are being vain.
If you do need to have a mastectomy, your surgeon should discuss breast reconstruction with you when they are planning that first operation. Not every breast surgeon is trained to do every type of reconstruction, but they should talk to you about all of the available options, even if it means another surgeon does your reconstruction at another hospital. It is important to discuss your thoughts and feelings, especially with your partner (if you have one), but ultimately it is your body and your decision to make. There are patients who decide to have a reconstruction to keep their partner, or even their surgeon, happy, and live to regret it, especially if they end up having a complication that needs further operations to fix it. We urge you not to do something just to make other people happy.
Every surgeon wants to give you a great result but they can’t promise perfection. It helps if you can decide whether your priority is to look good in your clothes, in your bra or naked. This will guide your surgeon and they can then be realistic about what is achievable. If you have an implant, your reconstructed breast won’t age like your natural breast (which changes in size and shape and starts to droop as you get older). The great result you have in the first year after your surgery may not look quite as good in the future. Radiotherapy can also affect the shape of a reconstruction, especially if you have an implant (see here for more information), and your surgeon will talk to you about this in more detail.
Your new breast won’t feel like your healthy breast when someone touches it. This is because the nerves in your skin and nipple are cut when your breast tissue is removed. You may only feel a pins and needles sensation when your breast is touched, or you might not feel anything at all. You won’t get a sexual response when your breast or nipple is stimulated.
There are several reasons why your surgeon may not be able to give you your ideal reconstruction:
If you want to use your own tissue, you need to have enough of it to recreate a breast. If you are very thin, you are unlikely to have enough body fat and muscle for a flap-based reconstruction. It is also impossible to recreate a large, droopy breast using an implant unless you have a breast reduction on the other side.
Both Trish and Liz were advised to have implants because they didn’t have enough tissue for a flap-based reconstruction.
If you have other medical conditions, such as very high blood pressure, it might not be medically safe for you to have the longer general anaesthetic that a reconstruction needs (the operation can take up to six to eight hours). Although age per se should not be a barrier to reconstruction surgery, your surgeon does need to be frank with you about how the operation might affect you. It takes much longer to recover from a major operation if you are in your sixties and seventies, and you may never fully ‘bounce back’ to the person you were before.
The nicotine in cigarettes narrows the blood vessels in the body. When you have a mastectomy, the blood supply to the breast skin is reduced because your breast tissue has been removed. Smoking reduces the blood supply to the skin even more, and there is a high chance that your scars won’t heal. To fix this, your surgeon would probably need to remove the reconstruction (leaving you with a flat chest). Some animal studies have shown that vaping and e-cigarettes also cause problems with wound healing. Many surgeons won’t take that risk and will recommend that you have a mastectomy to treat your cancer, followed by a delayed reconstruction after you have stopped smoking.
It takes a couple of months to recover from implant surgery, and up to six months to recover from flap surgery, compared to a couple of weeks following a simple mastectomy. If you can’t (or don’t want to) put your life on hold to recover from surgery – for example, if you have young children to look after or elderly relatives to care for – you may need to compromise on the look and feel of your new breast (choosing an implant with a shorter recovery time), or delay your reconstruction until you’re ready for it.
When your surgeon first talks to you about reconstruction, you will be given information about the different options. This may be a lot to take on board, especially when you’re still dealing with a new breast cancer diagnosis. It can help to talk to other women who have had a reconstruction, and your breast care nurse will know if there is a local support group where you can meet patient volunteers. You can also talk to other patients in forums on websites such as Breast Cancer Care and Macmillan. Breast Cancer Care has an animated guide on their website. The Touch Surgery app may also be useful. It is designed for trainee surgeons and shows surgical details of the operations, so is quite graphic. (See the Resources section here for more details.)
If you have secondary breast cancer when you are diagnosed, or have had a mastectomy and developed metastases before your delayed reconstruction, you may still be able to have a breast reconstruction. Most surgeons will want to make sure that your cancer has been stable for a minimum of three months, i.e. your scans haven’t shown any new deposits, and your current metastases haven’t increased in size. You also need to be strong enough to cope with, and recover from, a big operation, and it will need to fit around your ongoing cancer treatment.
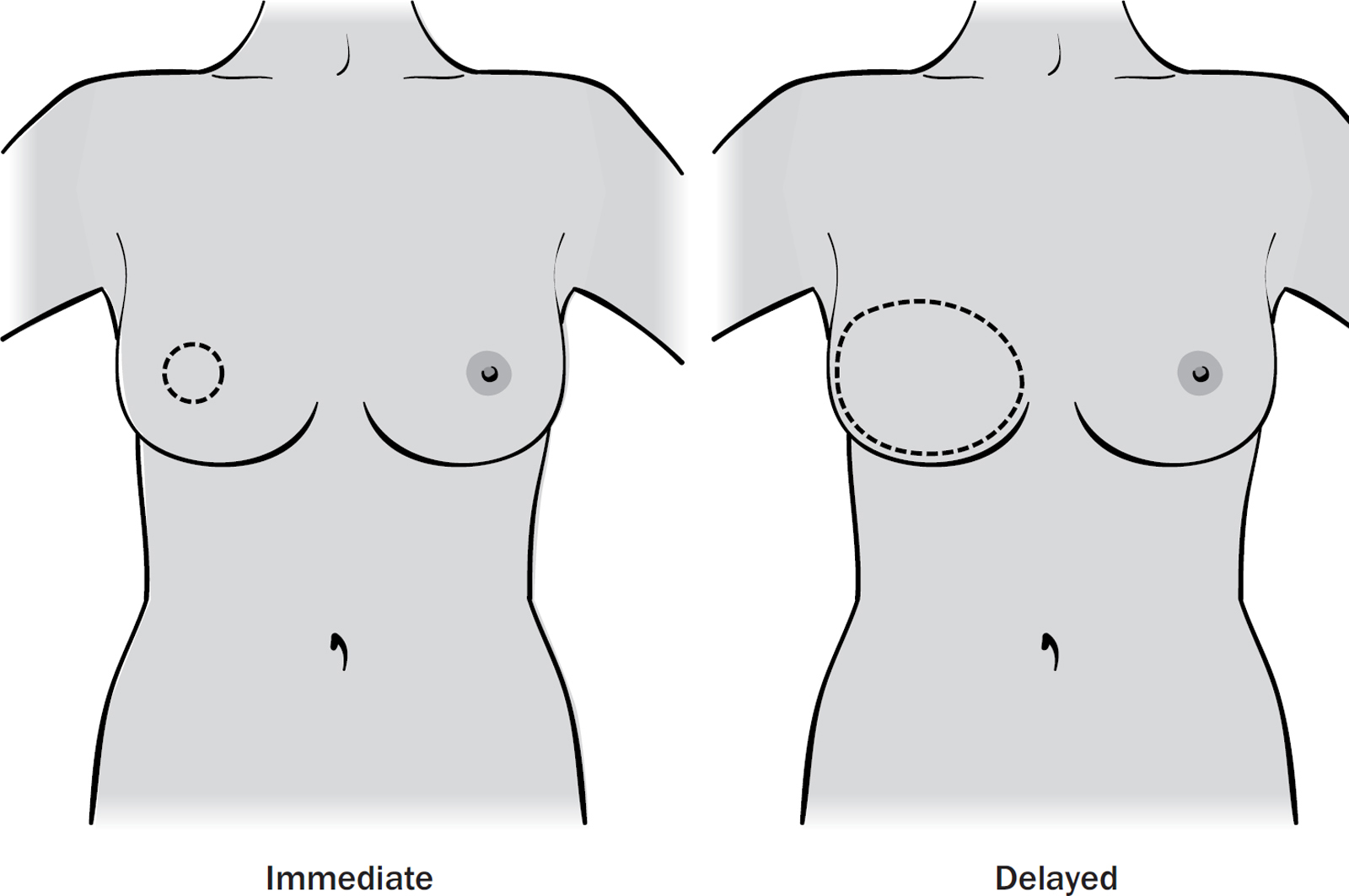
Your surgeon will help you decide when to have your reconstruction. There are two options:
1. Immediate reconstruction happens at the same time as your mastectomy. It gives the best cosmetic results because the surgeon can put the implant or flap inside your natural breast skin. There is also the psychological boost of never having a flat chest or having to wear a false breast (prosthesis) in your bra.
2. Delayed reconstruction happens months to years after your mastectomy. This could be due to personal preference, being pregnant when you are diagnosed or your doctors advising you to wait until after you’ve finished other treatments, such as chemotherapy and radiotherapy. The cosmetic result from a delayed reconstruction is often not as good as an immediate reconstruction. Because your breast skin has been removed, your surgeon needs to stretch the remaining skin with an expander implant (if you haven’t had radiotherapy) or use skin from your flap to help recreate a breast shape. If they use skin from your flap, you will have a scar that goes all the way around your new breast, instead of a small scar in the middle or at the side.
The first difference is the feel of the new breast. An implant feels like a soft, firm bag of jelly. It doesn’t move when you run or jump. It will always look ‘perky’ while your natural breast will change shape with time. Implants are best suited for women with small A–D cup breasts that aren’t droopy. A flap-based reconstruction uses your own tissue and it looks, feels and moves like your other breast. This is a good option if you have small breasts and want to avoid an implant, or have large or droopy breasts and don’t want to make your breasts smaller (provided you have enough tissue to use).
The second major difference is the surgery and recovery time. Implant surgery is relatively quick (2–4 hours), involves a short stay in hospital (usually 1–3 nights) and a 1–2-month recovery period. There is only one scar (the mastectomy scar on the breast). The natural lifespan of an implant is 10–15 years, and you may want or need to have further surgery in the future to revise the shape and feel of the implant (especially if you have radiotherapy), or to reshape the other breast to maintain symmetry.
Flap-based surgery, on the other hand, involves a much longer operation (5–10 hours), a 3–7-night stay in hospital and a 3–6-month recovery period. You have at least two scars, which means double the risk of a wound complication. You may want or need a second shorter operation to tidy up the scars, boost the shape with lipofilling (see here) and create a new nipple to get the best cosmetic outcome.
Most consultant breast surgeons are trained to do implant reconstructions, and some do back- and tummy-based flap-based reconstructions as well. Plastic surgeons are trained to do all the flap-based reconstructions. If your breast surgeon isn’t trained to do the reconstruction that you prefer, they will refer you to see a plastic surgeon who will do your operation. The plastic surgeon may work in a different hospital. Your breast surgeon would then travel to that hospital to do your mastectomy while the plastic surgeon does the flap.
Being examined by a plastic surgeon can feel quite impersonal. This is because they have to look at your body for muscle and fat that could be used to recreate a breast, and this means examining your tummy, thigh, bottom and lower back fat. It can feel embarrassing to stand there in your knickers while the surgeon grabs a handful of tummy fat, but it is the only way to work out whether you have enough tissue to recreate a breast.
If you have very large breasts, it may be possible to make both breasts smaller at the same time by doing a breast reduction (see here). If you used to have large breasts that have now ‘deflated’ a bit (perhaps after pregnancy), your surgeon may be able to give you fuller breasts. However, if you are naturally small-breasted, it is difficult for your surgeon to make your breasts larger. This is because your breast skin has to be able to stretch to accommodate the implant or tissue being used. If the skin is stretched too much, like an elastic band about to snap, it may start to die in places. This can leave holes in the skin or a scar that won’t heal. If this happens, your surgeon will have to remove the reconstruction and leave you with a flat chest while everything heals, and this could delay chemotherapy or radiotherapy.
Whether you can keep your nipple depends on the position of the cancer in your breast and the size of your breast. If the cancer involves or lies directly behind your nipple, your surgeon must remove the nipple when they do the mastectomy.
If the cancer isn’t close to the nipple, you may be able to keep your nipple. This does slightly increase the risk of getting a recurrence in the breast, but the overall risk of recurrence after a mastectomy is still very low. Your surgeon may want to take a biopsy from behind your nipple first to make sure that the nipple doesn’t contain cancer cells.
In order to keep your nipple, your surgeon has to make sure it will get enough blood from your breast skin to survive. If it doesn’t get enough blood, it may start to die and even fall off, leaving you with a flat stump. The larger your breasts, the further the blood has to travel to reach the nipple and the more likely it is to die. As a general rule, if your breasts are larger than a D cup, your nipple is less likely to survive.
If you can’t keep your nipple, you may be able to have a nipple reconstruction later. The nipple is normally made using a flap of skin from the middle of your reconstruction using a local anaesthetic and takes about 20 minutes. Many women have it tattooed (often by breast care nurses) to make it look more realistic. If you don’t want another operation, you can either have a nipple tattoo without a nipple reconstruction, or use a stick-on silicone nipple.
Liz’s cancer was in the top half of her breast, and she chose to have a nipple-sparing mastectomy. The nipple looked a bit battered and bruised for a few weeks, and then the tip became scabby and fell off (a bit like when a baby’s umbilical cord falls off). This didn’t hurt, but it was a bit ‘gross’! She was left with a flat nipple stump.
Trish’s cancer involved her nipple, so she couldn’t keep it. Six months after her initial implant surgery, she had a new nipple (which sticks up like her normal nipple) made using the skin of her reconstructed breast. This took about 20 minutes, using a local anaesthetic. She decided not to have a nipple tattoo to make it look more realistic, but knows she can have it done in the future.
Most surgeons will ask you to wear a bra day and night for the first 2–4 weeks after your reconstruction. This helps support the new breast and can ease discomfort. Ideally you want a post-mastectomy bra, with a front fastening, so it is easy to get on and off, and a range of fastenings to allow for post-op swelling. You can buy a post-mastectomy bra from most high street stores and even supermarkets, although they may not cater for women with a very small or large bra size. You could also try online specialist mastectomy bra retailers such as Amoena and Nicola Jane, and companies like Recoheart and Macom that only sell post-surgery bras (see here for details). Your breast care nurse will also be able to advise you.
QUESTIONS TO ASK YOUR SURGEON
Breast reconstruction is complicated and there are many things to take into account. The following questions may help you as you plan your discussion with your surgeon:
● Can I have a reconstruction?
● What’s the difference between an implant and a flap-based reconstruction? Are both these options available for me?
● What kind of reconstruction would give me the best shape?
● Should I have my reconstruction at the same time as my mastectomy or wait until after I’ve finished treatment?
● If I want to go flat now, can I have a reconstruction in the future?
● Can you make my breasts bigger (or smaller) while you are doing the reconstruction?
● Can I keep my nipple?
● Where will the scars be?
● Where will I have the operation?
● How long will the surgery take?
● How long will I be in hospital for?
● Do I need to wear a special bra afterwards?
● How long will it take me to recover and get back to my normal activities?
● What are the complications?
● What happens if it goes wrong?
● What will it look and feel like in the months and years ahead?
● What experience do you have in this operation?
● Can I see photos of your patients who have had this reconstruction? (All medical photos are anonymous and don’t show patients’ heads.)
● Can I talk to a patient who has had this operation?
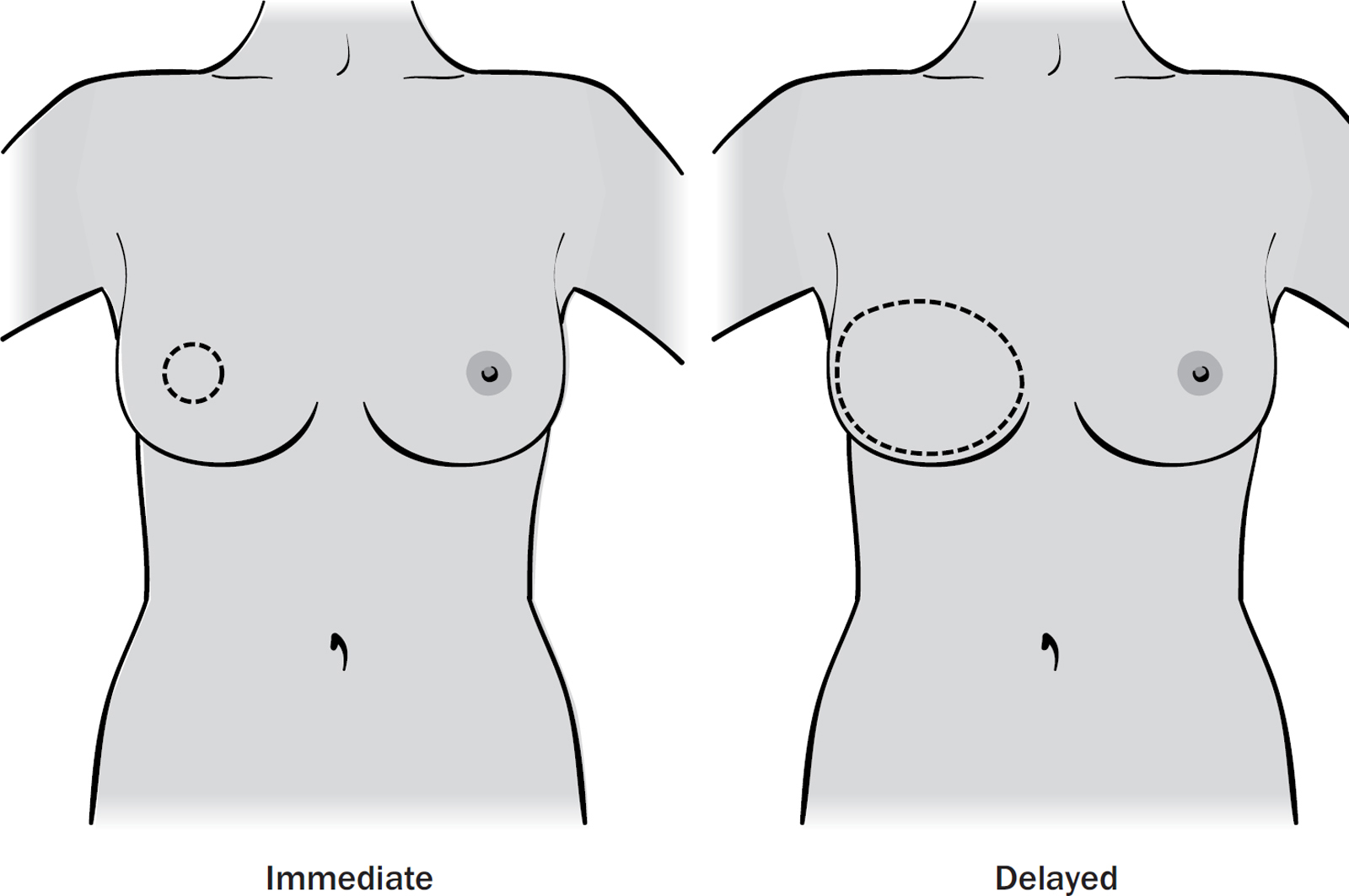
A permanent breast implant is a strong silicone shell filled with silicone that comes in a wide variety of shapes and sizes so the surgeon can match your opposite breast volume, height and width. Implants undergo rigorous laboratory testing and have to be approved by the Medicines & Healthcare products Regulatory Agency (MRHA) which ensures that they are safe and fit for use. It is almost impossible to damage an implant. If you have an implant in the UK, you will be asked if your details can be stored in the NHS Breast and Cosmetic Implant Registry. This means that any problems with your implant can be carefully followed up, and it is easier for research to be done looking at implant complications in the future.
A temporary implant is also called a ‘tissue expander’. This is an empty silicone shell that can be filled with sterile water. Some tissue expanders have a small amount of silicone inside them as well. They are filled up using a port, which is located either in the middle of the implant or connected via a small plastic tube which sits at your bra line.
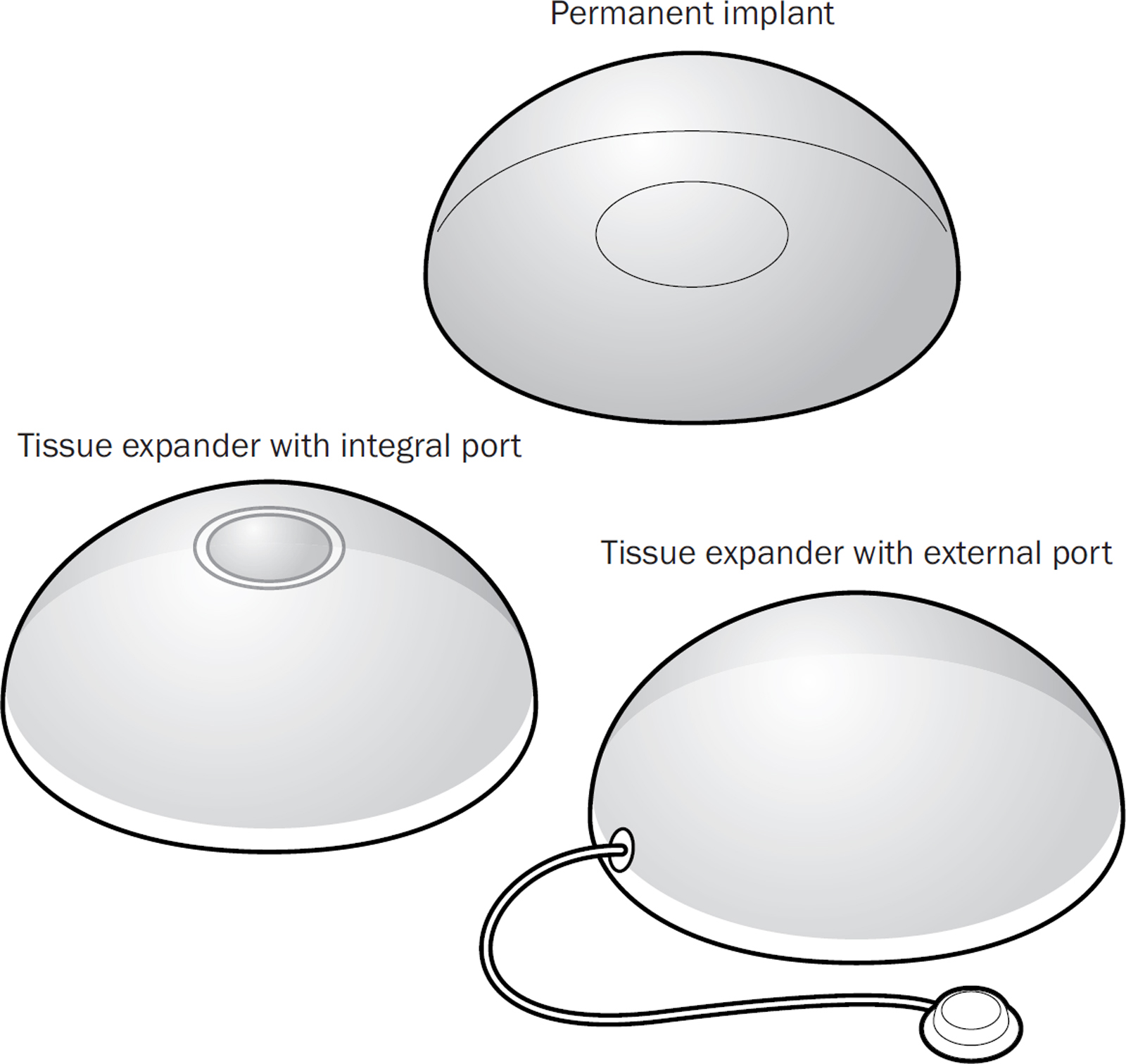
There are several different ways to reconstruct a breast using an implant, and they can all give good results. Every surgeon has their preferred technique. A one-stage operation means that your surgeon puts in a permanent implant at the same time as the reconstruction. A two-stage operation means that your surgeon first uses a tissue expander, which is slowly expanded every couple of weeks in clinic. Once the expander has reached the right size for you, your surgeon will swap it for a permanent implant at a second operation, normally three to six months later. This is often done if you need to have radiotherapy.
The implant has to be completely covered by tissue, and this can be done in one of two ways. The first uses your chest muscle (pectoralis major) to cover the implant. Because the muscle lies flat on your chest, it has to be stretched using a tissue expander. The expander is slowly filled with sterile water in the outpatient clinic. This gradually stretches the muscle until the right breast size is reached. At a second operation, your surgeon will either remove the port and leave the expander implant in place, or swap it for a permanent silicone implant.
The second technique uses a special mesh called an acellular dermal matrix (ADM) to cover some or all of the silicone implant, and this often gives your reconstruction a more natural shape. There are two ways to use the mesh. The first way (sub-pectoral) involves lifting the chest muscle, putting the top half of the implant underneath it and then sewing a mesh from the bottom of the muscle to your chest wall at the bra line to create a sling for the lower half of the implant.
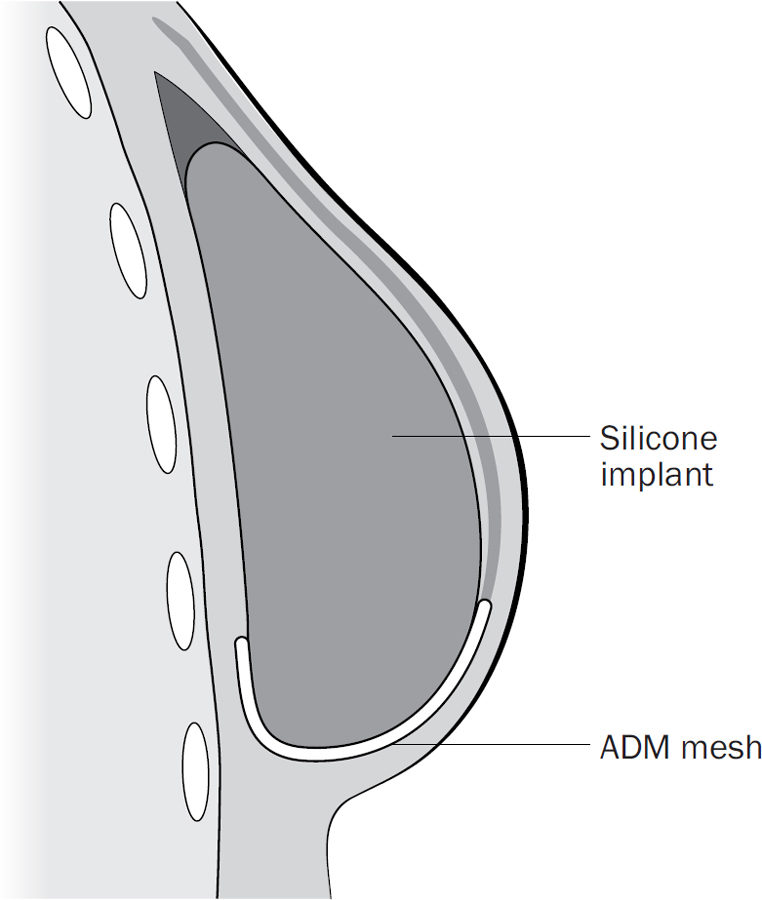
The second way (pre-pectoral) involves covering the implant completely in mesh and stitching this mesh on top of the muscle.
Your surgeon will tell you which method will give you the best result. If you have an implant, you will probably have one or two drains (see here) which are left in for several days to stop fluid building up around the implant which can delay healing.

On top of the complications from a simple mastectomy (see here), there are complications specific to implant surgery. There is a greater risk of a wound infection because your surgeon is putting a foreign object inside you, and you will probably be given antibiotics to take at home to prevent this. If you do develop a wound infection, you may need to have the implant removed, let everything settle and try again later.
If your chest muscle was lifted during surgery, you may notice that the implant appears to jump up when you flex that muscle. This can be hard to fix, and is more noticeable in slim women.
Your body forms a shell around the implant called a ‘capsule’ which is normally thin and can’t be seen or felt. Over time (months or years), the capsule can thicken and cause visible ripples or folds underneath the skin. It can also contract and change the shape of the implant, or cause pain. Radiotherapy increases the likelihood of this happening. If this happens to you, your surgeon may recommend an operation to release or remove the capsule and replace the implant together with lipofilling (see here) to smooth out any visible ripples.
A very rare but serious complication of implant surgery is the development of a rare cancer called Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL). This is a form of non-Hodgkin Lymphoma, a cancer of white blood cells. The risk of developing this is less than 1 in 6,000 women, and may be linked to implants with a textured surface. It typically develops several years after your surgery, and the main symptom is a swollen breast. If caught early, it is treated with surgery and has a very good prognosis.
A flap is some of your own tissue (fat, muscle or fat and muscle) that is used to reconstruct your breast. The area it is taken from is called the ‘donor site’. There are two types of flaps:
1. Pedicled flaps stay attached to the donor site (e.g. upper back and tummy) and are rotated to reach your chest wall and create a breast shape.
2. Free flaps are disconnected from the donor site (e.g. tummy, lower back, thigh and bottom) and their blood vessels are carefully plumbed into blood vessels on your chest wall using a microscope.
Sometimes your surgeon needs to use a small implant to match the volume of your opposite breast. You will have at least two scars: one on the breast and one or more at the donor site. Your surgeon will probably leave a plastic tube called a drain at the donor site to remove any fluid that collects there (see here).
The flap or donor tissue can come from your upper or lower back, tummy, thigh or bottom.
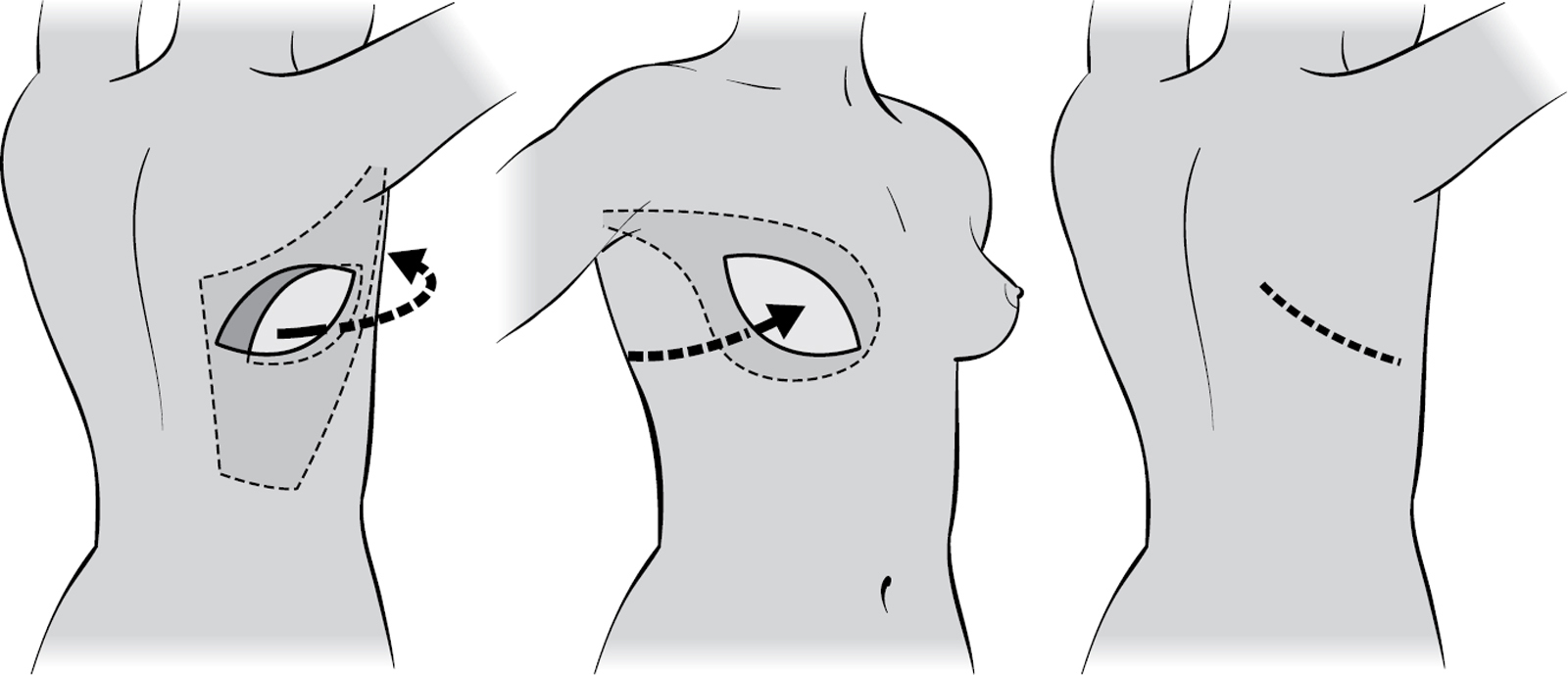
This is a pedicle flap that uses a large back muscle called latissimus dorsi with fat from your upper back. You have a scar on your back where your bra sits. You may have some back and shoulder weakness which should improve in time as other muscles learn to make up for the missing muscle. If you play a lot of sport, this might not be the best choice for you.
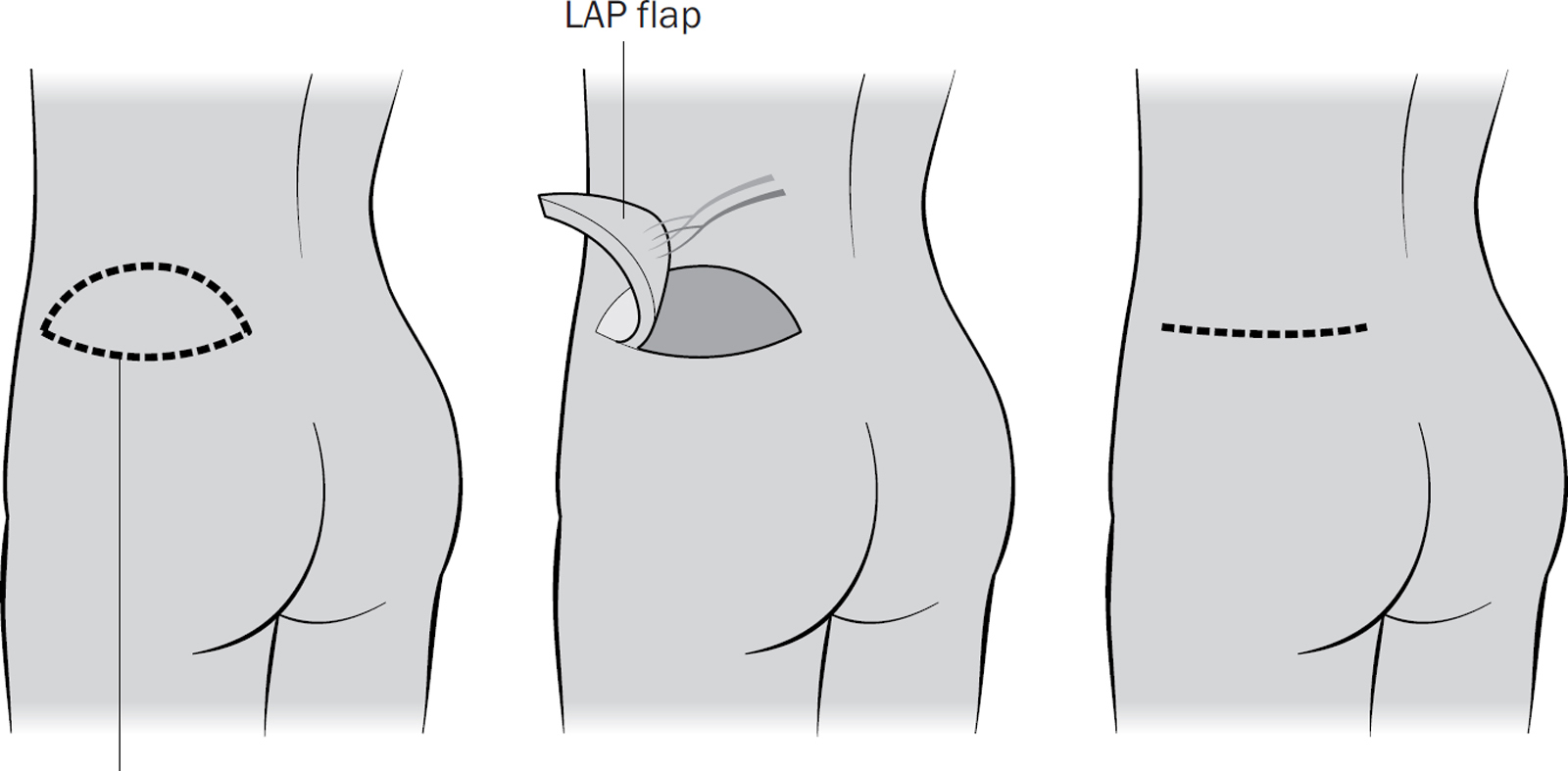
This is a free flap that uses your ‘love handles’. You will have a scar on your lower back, normally below your waistline.
This is either a pedicle or a free flap that uses a muscle from your tummy called the rectus abdominus muscle together with some overlying fat. You have a low scar on your tummy that goes from hip to hip. You will have a weak core because you have lost one of the muscles that helps you pull your tummy in.
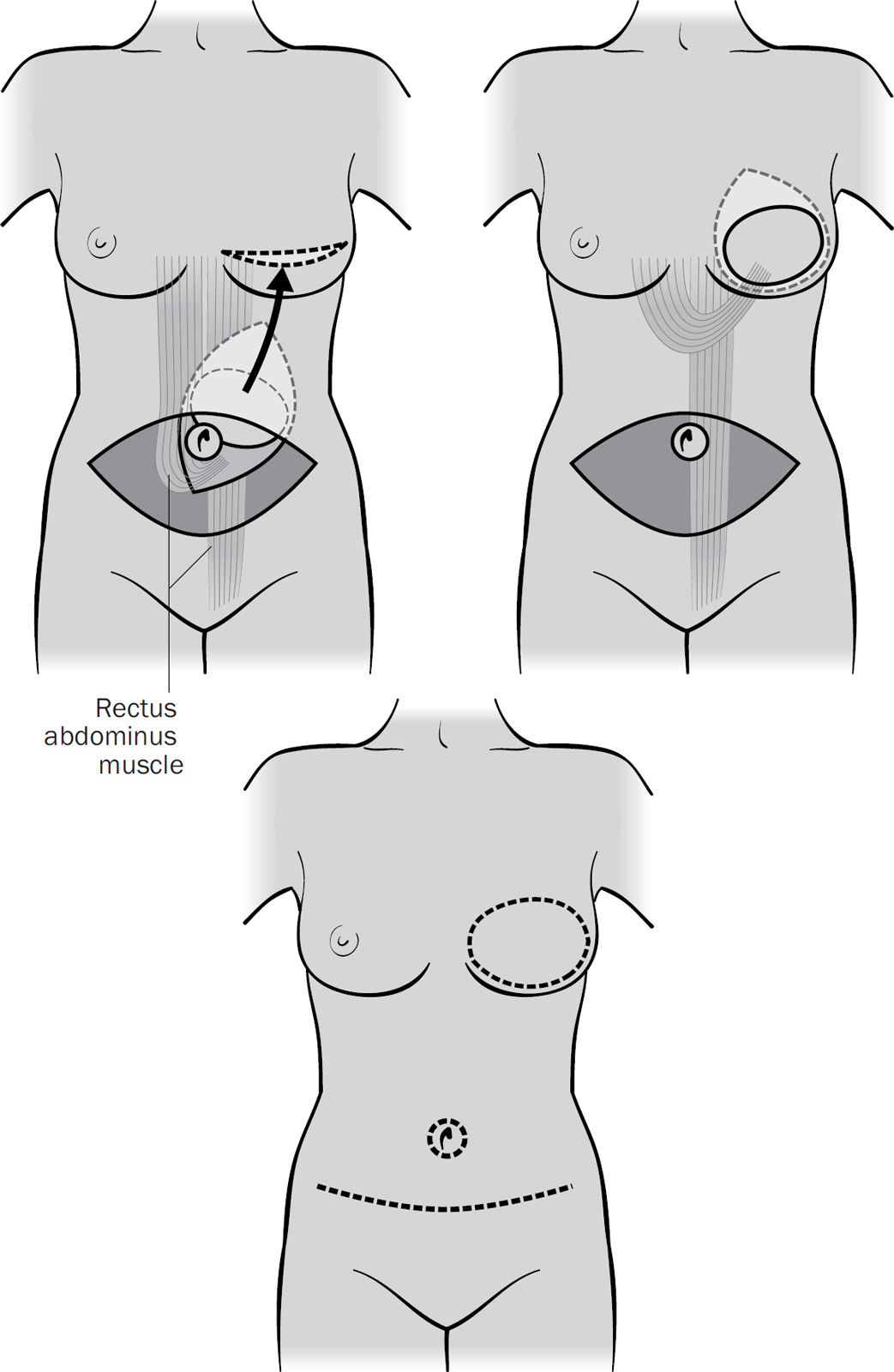
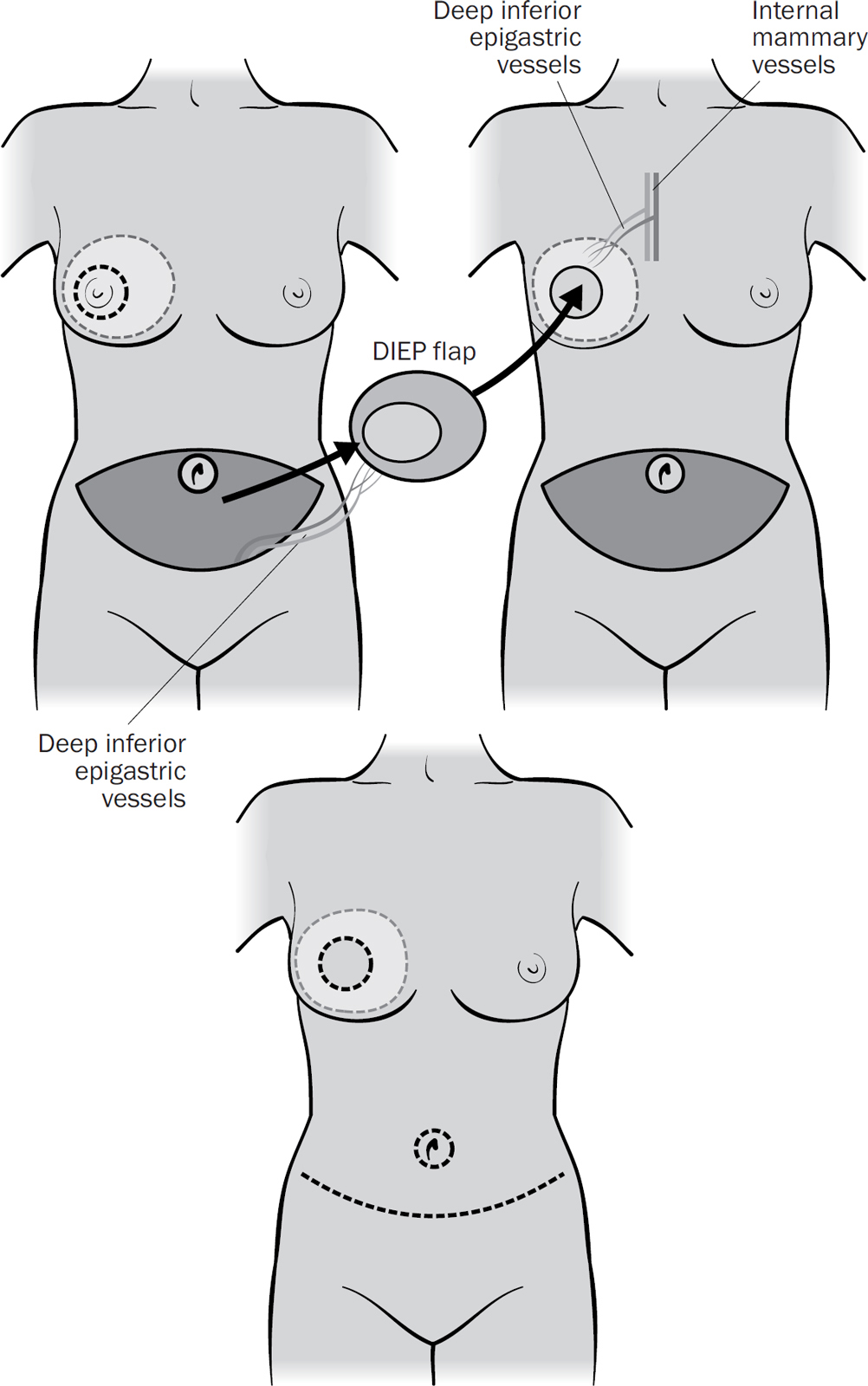
This is a free flap that uses your tummy fat below your belly button. It gets its blood supply from a vessel called the deep inferior epigastric perforator. It is essentially a ‘tummy tuck’ but instead of being thrown away, the fat is used to make a breast. You are left with a long, low scar going from hip to hip.
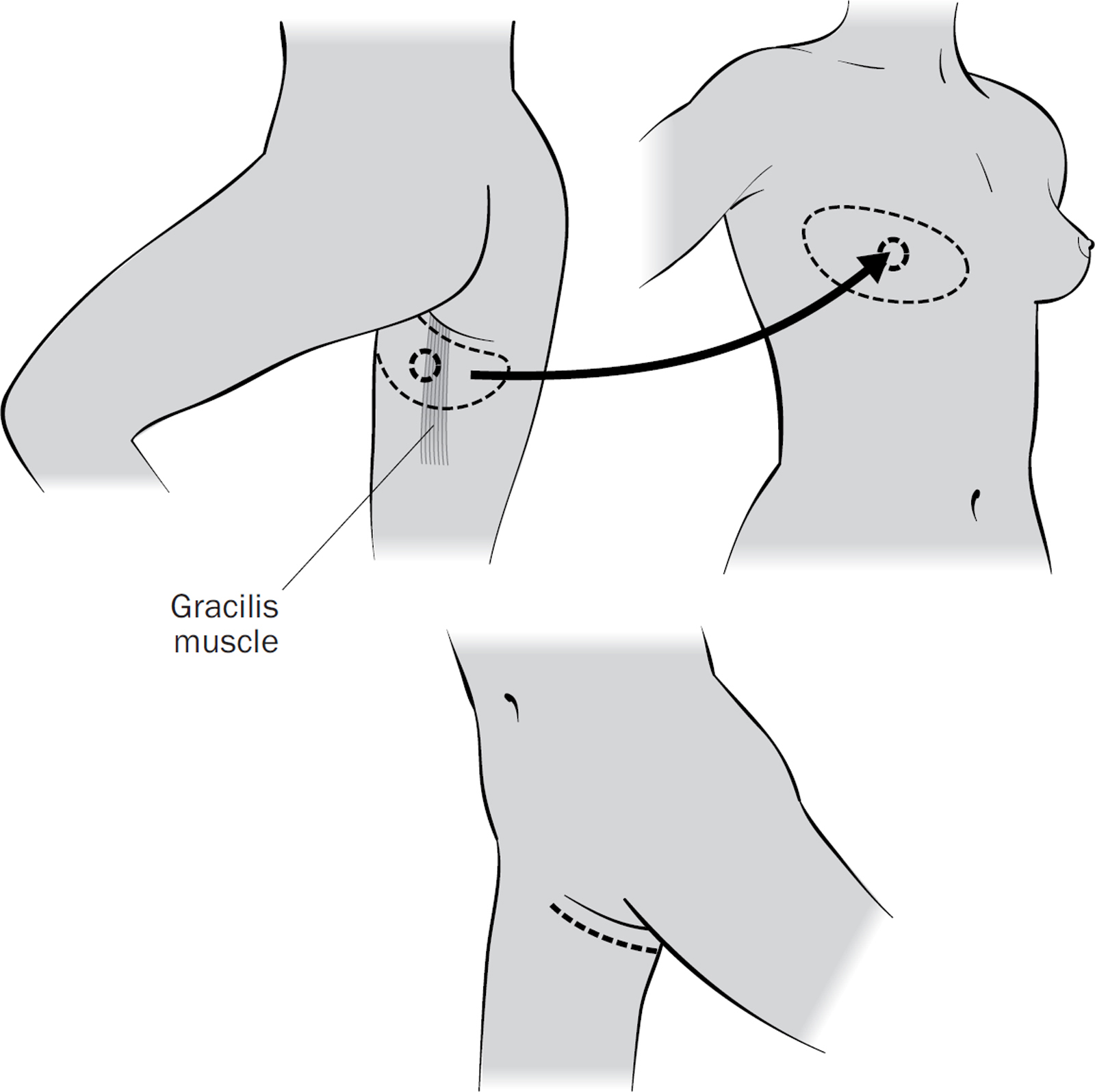
This is a free flap that uses the gracilis muscle in your inner thigh and your inner thigh fat ‘roll’. The other muscles in your leg make up for the one that is used in the reconstruction. The scar runs all the way around your inner upper thigh at the groin, from front to back. If you are slender, you may need the muscles from both thighs to get the necessary volume.
This is very similar to the TUG flap, but only uses fat from the back of your upper thigh, just underneath your buttock.
This is a free flap that uses the fat ‘roll’ on your outer thigh, with a scar on the outside of your thigh, below your hip.
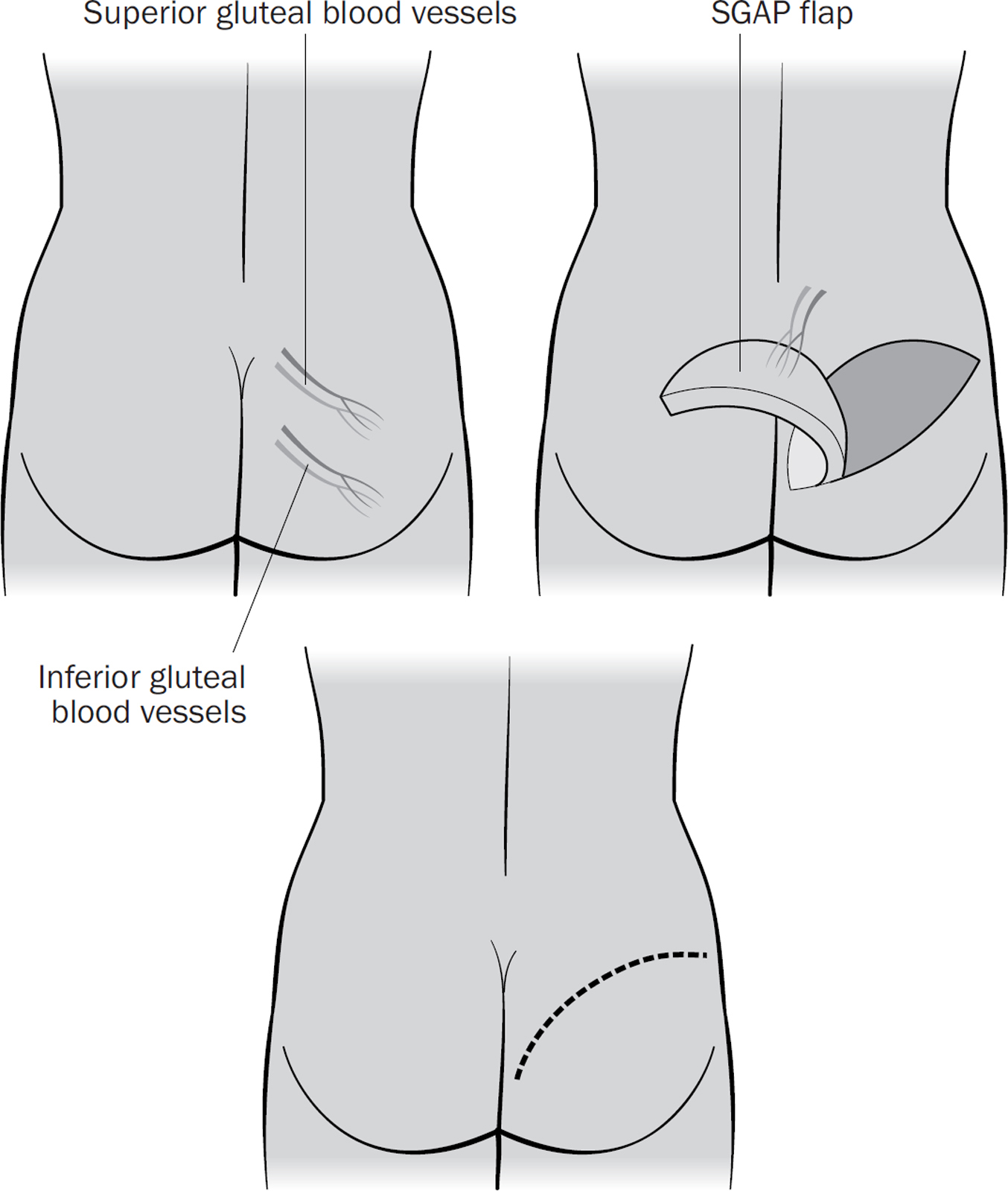
This is a free flap using fat from your upper or lower buttock to recreate the breast. One of the downsides is that you end up with a flatter bottom on that side.
As well as complications from your mastectomy (see here), you could have any of those complications at your donor site. These include problems with wound healing, fluid collection (seroma), bleeding and infection. You may also notice weakness at your donor site, especially if a muscle was used to reconstruct your breast.
It is normal for some of the fat at the edges of your reconstructed breast to die away because it isn’t getting enough blood. This may cause a hard, lumpy area, or you may notice a dimple or a dent in your new breast. The fat can be replaced with lipofilling at a second operation (see here).
Finally, there is a very small chance that your flap doesn’t work. This is normally because it isn’t getting enough blood, possibly because of a blood clot in one of the blood vessels. Your surgeon may be able to fix this at a second operation, but a very small number of women may end up flat-chested.
As you can see, deciding whether to have a breast reconstruction involves a lot of careful thinking and planning by both you and your surgeon, so you get the best possible outcome. However, the operation itself can be daunting, and in the next chapter we’re going to walk you through what happens on the day of your operation, what you need to take with you, and share our tips to help you recover afterwards.