Viruses recognize no international borders or time zones. They have no obligations to country, race, social status, or gender. Rich and poor alike are victims of viral infections. If given the opportunity, viruses do not stay in any one place and may travel over extraordinarily long distances. In 1983, the Asian tiger mosquito, Ades albopictus, a relative of A. aegypti, the mosquito that transmits dengue fever virus, was found in the United States for the first time. The mosquito larvae, stowaways in accumulated rainwater inside automobile tires, were transported on a cargo ship from Southeast Asia.
In our modern world, viruses and other infectious microbes can easily hitch rides on international flights to and from any major city. A European tourist visiting Thailand can bring home a strain of immunodeficiency virus from a sexual encounter in Bangkok; a Cantonese grandmother visiting her family in San Francisco can harbor a potent influenza virus in her lungs and carry it all the way from China and pass it to her grandchildren who transmit it to other children in preschool.
Viruses do not leave fossil remains or other archeological clues. They leave only what we have found, for example, in frozen tissue samples of their victims, such as from the remains of Eskimos in the Arctic tundra, or victims of the influenza epidemic of 1918. Though there are a variety of theories, there is no way of completely knowing the origin, natural history, or evolution of viruses. Yet what we do know is fascinating.
For one, we know that viruses have been with us a long time. Archeological evidence indicates that smallpox developed along with civilization in the river basin agricultural settlements of Asia and the Middle East as early as 10,000 years ago. We also know that viral epidemic diseases were unheard of in the New World before the arrival of the Spanish. Viruses are not only the cause of many infectious diseases, ranging from the common cold to slow death of AIDS and the frightening hemorrhagic fevers, but they have dramatically influenced history as well.
As agents of change, they have toppled dynasties, changed the outcomes of wars, and altered populations. In the twentieth century, smallpox alone killed an estimated 300 million people. In the sixteenth and seventeenth centuries, smallpox killed the emperors of Japan and Burma, as well as kings and queens of Europe. Queen Mary of England died of smallpox in 1694; Louis XV of France, Joseph I of Germany, and Peter II of Russia also died from the same disease.
The Aztec emperor and many in his immediate household were killed by smallpox. It is a matter of historical record that the successful conquest of the Aztec empire in Mexico by Hernando Cortez and the Incan empire by Francisco Pizarro in Peru were ultimately achieved more by the enormous deaths from fatal epidemics of smallpox and measles than by superior military strategy or overwhelming firepower.
The 1918–19 epidemic of Spanish influenza killed 20–40 million people in less than a year, causing more deaths than all the massive military casualties of World War I. In the spring of 1918, the German Army's assault on Paris was halted by this flu. It not only affected Europeans, but an unbelievable 80 percent of the United States Army's death toll was from the Spanish flu that killed 43,000 American soldiers between 1917 and 1919—nearly as many as died in combat in the Korean War some thirty years later.
Viruses not only infect humans but all living things including plants, animals, birds, and sea creatures. In 1988, seal plague virus killed 2,800 seals in the United Kingdom; a similar disease had already devastated the rare freshwater seals of Lake Baikal in Siberia in 1987. Canine distemper and other common animal viruses kill our pets as well as livestock. Rinderpest, or cattle plague, killed an estimated 2 million cattle annually in South Africa during the 1920s. The virus responsible was introduced into South Africa in 1889, and within the first ten years there it spread northward, killing an estimated 90 percent of the wild buffalo population in Kenya.
Viruses are everywhere, and due to their microscopic size they also infect the invisible world, including bacteria, fungi, and protozoa. If viruses are ubiquitous in nature and have intimately accompanied us in the human evolutionary journey, why have viral infections become so devastating in recent years?
This question is as yet unanswered even by the experts. My hypothesis, which I develop throughout this book, is that it is because of widespread immunological breakdown caused by the stress of modern living, environmental destruction, and toxic chemical pollution—nature out of balance. The experts are starting to catch up with this possibility.
The most frequently quoted popular definition of a virus belongs to Sir Peter Medawar (1983): “A virus is a piece of bad news wrapped up in protein.” However succinct and graphic this definition is, it does not describe a virus in sufficient detail, nor does it answer any of the evolutionary and ecological questions concerning the nature of viruses. The word “virus,” coming from the Latin meaning “poisonous fluid,” also does not reveal what a virus is. Here are three things that a virus is: small, parasitic, and genetically lean.
Viruses Are Very Small: Viruses are referred to as subcellular organisms, meaning they are smaller than cells, smaller than bacteria, and certainly smaller than most human host cells. Bacteria are measured in micrometers (10−6 meters) and viruses in nanometers (10−9), which is a thousand times smaller. Viruses are so minute they can maintain their ability to infect even after passing through filters small enough to strain out all bacteria. In fact, they are so small that they can only be seen by the most powerful of electron microscopes.
Viruses were long thought of as the smallest infectious agent, yet we now know of two other pathogens that are even smaller: prions, the suspected cause of Mad Cow Disease, discovered only recently by the 1997 Nobel Laureate in medicine, Stanely Prusiner; and viroids, organisms that only affect plants.
Viruses Are Parasites: Viruses are intracellular molecular parasites. They enter the body silently, and in the case of HIV and hepatitis C viruses, they often do so without notice. Then they use our cells to manufacture substances needed for their own replication and life cycle. They have no metabolic life of their own outside a host cell, which makes them dependent on living cells for their existence. Viruses have a receptor binding protein that allows them to attach to other cells and convert them into virus-producing mini-factories. They do not make their own energy or proteins for survival and cannot reproduce without the assistance of cellular material from other living cells. Viruses grow and multiply only within other living cells—human, animal, plant, bacteria. Outside the host cell, a virus is not alive and exists in a world between the living and nonliving.
Viruses Are Genetically Lean: The basic viral particle or single virus is called a virion. It consists of a nucleic acid genome, in which the virus's hereditary information is stored, surrounded by a shell of protein. Unlike most living cells, viruses do not have cell walls composed of a plasma membrane. Instead, a protein coat called a capsid, which may also contain lipids and sugars, protects the viral genome.
All living cells contain both known types of genetic material, RNA and DNA, but viruses possess only one type, either RNA or DNA. They also have a very small number of genes compared to other cells. For comparison: the human immunodeficiency virus (HIV) has fewer than ten genes; a larger virus like smallpox contains between 200 and 400 genes, but even the smallest bacteria contains 5,000 to 10,000 genes, and a human cell has 80,000 to 100,000 genes (see figure 1-1).
While at first it seems like a reproductive disadvantage compared to other life forms, minuteness and limited genetic material become an advantage for the virus. These characteristics make it easier for a virus to jump from one host to another, and at times from one species to another, rearranging and reengineering the host's genetic material to suit its needs. Dorothy Crawford, Ph.D., in The Invisible Energy (2000) describes viruses as “rogue pieces of genetic material,” as if they were accidents waiting to happen.
Nothing could be further from the truth. Viruses exhibit a remarkable intelligence and a superb ability to survive and adapt to new environments, but Western science has only recently focused its attention on the viral world.
Advances in microbiology and bacteriology were at least a century ahead of those in virology, which is a relatively new science with its beginnings only in the twentieth century. Though there were many microbe hunters in the early 1800s, the first virus discovered is credited to the Russian scientist, Dimitri Ivanowsky. In 1892, while studying tobacco mosaic disease, he found that the agent that caused the disease was small enough to pass through a filter known to trap all bacteria.
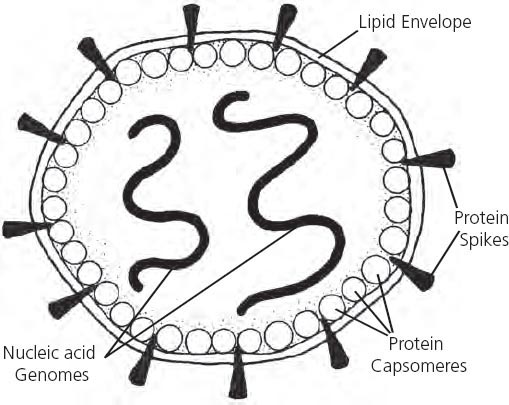
Figure 1-1: Representation of a Basic Viral Unit
The virion is a subcellular particle with a shell or envelope of protein and lipids called a capsid. The capsid may contain protein spikes or round capsomeres that serve to help penetration of a host cell. Inside the shell is the functional portion containing the virus's genetic material, referred to as the nucleic acid genome, which directs the activity and function of the virus.
Yellow fever was the first human virus identified. One of the most devastating plagues of past centuries, and a re-emerging infectious disease of the twenty-first century, yellow fever has been responsible for tens of millions of deaths. Although Carlos Juan Finlay, a Cuban physician practicing in Havana in 1880, proposed that yellow fever, then epidemic in Cuba, was a mosquito-borne infection, it was not until 1901 that Walter Reed, a physician and colonel in the United States Army, identified the causative source as a virus. Once mosquitoes were identified as the disease vector (the method of how the virus is carried from human to human), the introduction of aggressive mosquito control dramatically reduced the incidence of yellow fever within a few years.
Antibiotic drugs were developed far in advance of drugs to treat viruses. Penicillin, the first antibiotic, was discovered in 1928 by Alexander Fleming and introduced for clinical use in 1941. However, no antiviral drugs were developed until the late 1950s and were not available for general clinical use until two decades later.
Since there were no drugs until recently that treated infectious viral disease, the focus of medical research for viruses was on the development of vaccines. The first vaccine developed in the West was by Edward Jenner in 17961 against smallpox. Though controversy and different opinions plague it, vaccination continues to be one of the cornerstones for the treatment of viruses in modern medicine. (The use and risks of vaccinations are discussed in appendix D at the end of this book.)
However, it was not until 1930 that the first virus was actually seen. The tobacco mosaic virus had the honors here (as pictured on the cover); the electron microscope brought the vague viral symmetry into view. Detailed characterization of viruses only began in the later part of the twentieth century with the advent of better techniques for studying viruses, including more advanced electron microscopy, cell culture, high-speed centrifugation, electrophoresis of RNA and DNA genomes, and nucleotide sequencing.
Before discussing viruses and the diseases they cause, let's establish a point of view that suggests a relationship between the co-evolution of viruses and other species. The conventional, current model looks at a virus as a unique entity separate from the host, with a linear relationship between them: the virus infects the host, the host gets sick and develops symptoms; gets well, dies, or carries the virus which eventually infects others to continue its life cycle. This linear model is useful in analyzing basic viral characteristics and in quickly assessing and treating symptoms. However, it does not penetrate deep enough into the viral world and is not solving the problem of the current viral disease paradigm.
The evolutionary model questions this hypothesis and suggests that it may be more of a two-way street with virus and host exchanging genetic material. This idea presents more of an interdependent picture than is currently postulated, and allows for an understanding of how humans and viruses coexist and have done so for hundreds of thousands of years.
Though simple compared to the complexity of a human being, viruses are elegantly constructed organisms exhibiting remarkable bioarchitecture, beautiful design, and precision functioning. They play a significant role in the life cycles of all living organisms and are rightfully imbedded in the ecological infrastructure. From this evolutionary and ecological point of view, viruses have a place in assisting human evolution by assuring the survival of the species through natural selection. By exchanging genetic material from host to host, they influence the heredity of cells. As evolutionary messengers, viruses have effectively colonized nearly every living thing on this planet, from bacteria to humans. That is why viral disease will remain among us and why it can never eliminate the human race: we depend on each other.
The evolutionary model presents more of an interdependent picture than is currently postulated, and allows for an understanding of how humans and viruses coexist and have done so for hundreds of thousands of years.
There is an ancient Chinese saying, “Pure water has no fish” (Zhang 2000). For some things to live, other things must die, and nothing lives in a completely purified environment. Ultimately it may be a great mistake of modern medicine to attempt to sterilize the planet of viruses.
Interdependence among all living things is a rule of nature. We live in a biological world populated by billions of microscopic organisms that are friendly, neutral, and lethal. Biological life is a continuum, and there is less separation between independent organisms than previously thought. In fact, there may be no separation at all; viruses are not “us,” yet their DNA has been worked into our genes, and therefore is a part of what we are as biological beings.
There are 4,000 known types of viruses, but less than 4 percent are well characterized, and new viruses are discovered regularly. Indeed, at least fifty have been identified since 1988. Classification of viruses is based on several criteria, mainly by the type of nucleic acid (DNA or RNA) and by whether the genome contains a single strand (ss) or double strand (ds) of genetic material.
For example, smallpox is a dsDNA virus and HIV has an ssRNA genome. Among the DNA type are viruses that cause hepatitis B infections, herpes simplex blisters, and warts. In the RNA family, there are viruses that cause yellow fever, measles, polio, bronchitis, AIDS, and hepatitis C (see table 1).
Besides being based on the type of genetic material, classification of viruses is also made on structural characteristics that include: size (ranging from 20 to 450 nanometers in diameter); symmetry (helical, icosahedral, or complex); and presence of an envelope membrane.
Classification of Viruses: Viruses are classified into seventy-one families (distinct groups) with names ending in “-viridae,” and 164 genera (subgroups that share similar characteristics) with endings of “virus.” Further classification into individual species is not used for viruses.2
The specific identification of virally produced illnesses is based on clinical or immunological means, such as the symptoms and clinical signs presented by the patient. For example, in measles, the patient develops Koplik spots, small spots that resemble white grains of sand on the inside of the mouth opposite the first and second upper molar teeth. They also develop the characteristic measles rash that starts on the neck and spreads to the trunk, arms, and legs. For hepatitis C virus, diagnosis is made by a positive test for antibodies to the virus and for an elevated alanine aminotransferase (ALT) level, which is a test for liver function.
Naming new viruses is an interesting exercise. Some are named after the type of disease they cause, such as poxviruses (i.e., smallpox). Others are named for the location where they were first isolated, such as the Spanish flu from Spain, or the Marburg virus from a town in Germany. Others are given numerical designations like HHV-4 for Epstein-Barr virus, which, as it was originally named after its discoverers, has two names. Some viruses are named after their structure or morphological features, such as corona viruses for the halo of spikes projecting from the virion.
Viral Carriers and Natural Hosts: To understand how viruses cause disease, it is important to discuss a few additional concepts and define some commonly used terms. Although the specific origin of viruses is unknown, it is accepted that they usually descend from a parent source that already exists in nature and then spread from animal to animal and then from animals to humans. The infected animal or person is referred to as the host.
Since viral infections are often transmitted by an intermediary, such as a mosquito or tick bite, the mode of disease transmission is referred to as a vector. Viruses can inhabit as well as infect virtually any living organism, so relationships often develop between the virus and living host allowing both to coexist. The host acts as a carrier, such as occurs with herpes or hepatitis viruses, assuring the survival of the virus by spreading it from one person to another.
Viruses have a high mutation rate and produce great diversity among the different possible types or subtypes. This adaptive characteristic not only assures survival for viruses but also makes it easier for them to avoid a potential host's defenses. It also makes them a difficult foe to treat successfully. Viruses mutate readily when exposed to antiviral drugs; however, they have a difficult time adapting to the broad spectrum of active components in botanical medicines. This is one of the reasons why herbal antivirals are effective in treating viral illnesses and why working with natural processes works better than artificial chemical drugs.
Still, the role that viral mutation plays in disease is poorly understood. However, evolution occurs in three forms, independently or in combination, creating new or emerging viruses: (1) they evolve as a newly appearing variant; (2) they are introduced from another species; and (3) they disseminate from a smaller population and spread into a larger population, changing form as they do so. Mutation, as a form of rapid environmental adaptation, benefits the evolutionary needs of the virus but makes it difficult to understand and treat effectively. That is why it is important to work with the natural processes of your body by enhancing health and immunity.
Although the individual person is understandably concerned only with his own ailment, what many people are unaware of is that even the most common of viral diseases originate in animal hosts. For example, though influenza virus causes common respiratory infections worldwide, most strains of it originate in China where the natural hosts are livestock, especially pigs, chickens, and ducks. Other animal hosts that carry viruses infecting humans are migratory water-fowl, birds, rodents, and monkeys.
Humans can also carry viral disease, and certain human groups are more likely to carry viruses than others. Interestingly, children are the most common hosts and carriers for many viruses such as the common cold and measles. Due to their high exposure to sickness, healthcare workers are also frequent carriers for viruses. The most seriously affected, and the groups in which the most mortality are seen are the very young and the very old; this is why public health measures concentrate on vaccinations for children and flu shots for seniors. Since healthcare workers like doctors and nurses are particularly at risk due to their daily exposure to sick people, they are also encouraged to be vaccinated against influenza virus.
Viruses have a unique way of promoting their own life cycle. First they infect the host, often causing sickness in the process, and then they pass out of the host, usually in body fluids. For example, rotaviruses that cause traveler's diarrhea (or more serious and even lethal illnesses) pass from the body of the host in the feces. In every gram of infected feces reside about one billion rotaviruses. If sanitation measures are not in place, these active viruses readily enter the water or food supply to infect many others. People spread influenza by coughing and sneezing virus-laden particles of saliva and mucus into the air, which are then inhaled by every person in the vicinity.
How Viruses Enter the Body: There are three locations where viruses typically enter the human body: the respiratory tract (nose, throat, and lungs); the gastrointestinal tract (mouth, stomach, and intestines); and the genitourinary tract (the sex organs and urinary area). Viruses gain entry into the body via the respiratory tract by inhaled air that people sick with a virus have coughed or sneezed into, such as with the flu; or via the gastrointestinal tract through contaminated food, as in hepatitis A. Sexual intercourse can also cause the passing of viruses, as with HIV and herpes through the genitourinary tract.
Though these three routes are the main ways viruses enter the body, the skin is another way in which viruses can infect us (such as through warts), by kissing (mononucleosis), or hand contact. From a simple handshake, one can rub a virus into one's eyes or nose or mouth. One of my acupuncture colleagues developed a serious herpes infection in his eye after inadvertently rubbing an itch in his eye immediately after treating a patient for herpes simplex virus.
Perhaps appropriately, in Asia, hand-shaking is not the custom as it is in the West, and intimate touching of people in public is discouraged—perhaps for good health reasons. A polite or formal bow is preferred. If one has had the experience of traveling in Asia, the dense congestion of people and tightly packed crowds can be overwhelming. It is no wonder that such a custom developed: it is a practical way of reducing the passing of germs. Perhaps in our modern, population-dense world with our ever-increasing viral concerns, some thought should be given to alternative public ways of showing affection.
Viruses also have been quick to exploit modern medical practices. The normal portals of entry now include direct blood-to-blood transmission, such as found in blood transfusions. Though unintentionally, blood transfusions greatly contributed to the spread of HIV and hepatitis B and C. Shared hypodermic needle use in the case of hepatitis C also caused widespread viral transmission among drug users. When viruses are introduced directly into the blood stream, they bypass natural immune defenses (the respiratory mucosa or hydrochloric acid in the stomach) that might have screened them out.
In effect, the immune system receives a surprise attack and its response must be appropriately strong enough to eliminate the virus. Often, as in HIV and HCV, there is no immediate immune response, as the virus has stealth mechanisms to outsmart the body's natural defenses. Only after the virus is well-established in the liver or nervous system does the immune system react, and even then it may be in a manner that is more destructive to the host than to the virus. Something very strange is occurring with the spread of these diseases, and it may take generations for the human immune system to adapt to them.
Some viruses, like German measles and HIV, can spread from mother to child, passing through the placenta during pregnancy. In the case of herpes simplex virus, a baby can be infected from the mother's blood when passing through the birth canal. Some viruses can also be passed along in breast milk, such as cytomegalovirus (CMV) and HIV.
The Mechanics of Viral Infection: Viral infection can lead to a variety of effects. However, first the virus must invade the host, travel in the blood or other body fluids, identify an organ or tissue that it has affinity with, attach itself to a target cell, and then get inside the susceptible cell. To enter an individual target cell the virus must cross the cell membrane and enter its cytoplasm. Sometimes the cell invites the virus in by a process of translocation across the cell membrane. Why this happens is still unknown. Other types of viruses fuse with the target cell's outer membrane and inject their own protein directly into the cytoplasm of the target cell.
Once the viral protein is within the target cell it places its genes into that cell's nucleus (where the genetic material is) and begins to make substances to create the next generation of itself. This process is not happening to only one or two cells at a time, but to millions of cells concurrently.
The virus then replicates itself quickly enough to overcome the body's local defenses, and it does this at an alarming rate. A complete viral cycle takes an average of only six to eight hours, and in the course of that time each single infected cell can release an additional 10,000 copies of the virus. Once this bridgehead has been breeched, the viral infection can spread from the site of inoculation to other areas, called secondary sites, via the bloodstream or lymph. Once reaching its target area, such as the liver in hepatitis or the spinal nerves in herpes zoster (shingles), it replicates further, and eventually the specific symptoms of infection appear, such as jaundice in hepatitis or pain and blistering with shingles.
These events establish the beginning of the infectious stage. After the virus has infected the host's cells, cell death usually follows with the bursting of the infected cell. Finally, the virus exits its former host, usually in body fluids, to directly infect others through this same process. Some viruses are very tough and can survive outside the host almost indefinitely. Many can endure temperature extremes, strong acids or alkalis, and drying, while others are more sensitive and die with exposure to air.
Clinical Manifestations of Viral Infection: Doctors are trained that viral infections follow characteristic stages. An incubation period of several days to a few weeks occurs before symptoms of the initial infection begin to appear. In chronic viral infections, like HCV or CMV, the incubation period is extended and the virus can remain dormant or silent for years before symptoms appear.
In acute viral infections, the first set of symptoms are called prodromal and manifest as fever, fatigue, and malaise, followed by the specific characteristics of the disease like the red rash from chickenpox. For acute viral illnesses like measles, there is also a peak when the illness reaches its worst stage during which time the patient is the sickest. Several days later, the symptoms begin to diminish and the patient recovers, thanks to their immune system's ability to control the viral invader.
Types of Viral Infections: The list of diseases caused by viruses is immense and ranges from the common cold to cancer. Viruses not only cause specific diseases with clear diagnostic symptoms, but they can also cause a constellation of symptoms that can defy diagnosis. Some viral diseases mimic other illnesses, like the fatigue caused by anemia, or cause secondary inflammation, like the joint pain associated with arthritis. Certain viruses have specific affinity for only one type of tissue, such as the liver or skin, while others range among many body organs and systems. Viruses can cause localized infections such as warts or a sore throat, or a generalized infection such as in influenza, in which your whole body feels sick.
The patterns of disease caused by viruses are classified into several groups. Acute infections were originally thought to be the only manner in which viruses caused illnesses: you got sick and then you either got better or died. However, it is now well known that acute infections come in many forms. Therefore, viral illnesses are now classified as acute, chronic, latent, reactivated, and transforming (see figure 1-2).
Figure 1-2: Patterns of Viral Disease
After initial infection, the virus can cause an active acute infection or a latent infection. Reactivation of a latent infection can return to latency, cause an acute response, or cause chronic illness, as in the case of Epstein-Barr virus and chronic fatigue.
The advantage of acute infections is that they cause rapid cell death, which results in active and aggressive management by the immune system. On the other hand, a chronic or low-grade infection kills a smaller number of cells than in an acute infection. In this type of infection, the person may feel constantly or episodically ill, as in chronic Epstein-Barr virus (EBV), or they may have no symptoms at all, as in the early stages of HCV. The immune response develops a tolerance to the virus, and the host lives on, but with reduced energy and wellness.
Some viruses can become completely latent or exist in a dormant state, such as herpes simplex virus (HVS), only maintaining sufficient activity to sustain themselves. When circumstances are right, the virus can reactivate itself, causing symptoms. Viruses can also transform the infected cell in such a way as to cause cancer in a process called oncogenesis. Both herpes and hepatitis viruses are associated with the transformation of normal cells to cancerous ones (see discussion to follow).
Clinical Classification of Viral Infections: Viral infections are also further classified as persistent or non-persistent. Acute nonpersistent infections are generally short-lived and have no other consequences than the immediate symptoms during the infection. You get sick, your immune system goes to work, and you get better within a week or two. Examples include the common cold or a mild flu. Persistent infections with acute onset are often due to a latent infection, or a virus that persists in the cell host, and may activate or reactivate on more than one occasion, causing episodes of illness. Examples include herpes simplex and cytomegalovirus.
In the case of recurring illness, you feel repeatedly sick. Often, just when you start to feel better, you get sick again, as is the case with repetitive colds. Chronic, persistent infections are those in which the viral agent is being continually produced to cause a viral load sufficient to produce ongoing symptoms, such as in some types of Epstein-Barr virus (EBV) and the retroviruses, like HIV.
Additionally, viral co-infections can occur such as when AIDS and HCV appear together; or a satellite virus may assist another virus, each using the other to replicate. Opportunistic bacterial infections are also commonly seen with viral infections, such as in cases of influenza co-infected by staphylococcus or streptococcus, causing a bacterial bronchitis, or when a viral rhinitis or common cold turns into bacterial sinusitis.
Stealth Infections: Those viruses associated with long incubation periods during which time there may be no symptoms or signs of infection at all are often referred to as slow viruses. Examples of insidious viral infections include the “slow” or “stealth” viruses that often cause no apparent acute or chronic symptoms until the organism is well invaded and the tissue cells are compromised by a fully entrenched virus, as in the cases of HCV and HHV-6.
The slow virus concept first appeared in 1957 with the work of a National Institute of Health scientist, Carleton Gajdusek, who was in New Guinea investigating kuru, a fatal type of spongiform encephalopathy that attacked the victim's brain, leading to paralysis and death. Upon uncovering the grizzly details, which suggested that a virus was responsible, and was transmitted when New Guinea tribes-men cannibalized their victims and ate the brain, Gajdusek proceeded to infect lab monkeys with brain tissue from kuru victims. In time, the monkeys developed neurological symptoms and eventually died. When the government of New Guinea enforced sanctions against cannibalism, kuru was eliminated.
The term “stealth infection” was coined by Paul W. Ewald, Ph.D., an evolutionary biologist at Amherst College in Massachusetts, to refer to microbial infections that cause other seemingly unrelated illnesses. The stealth concept has been expanded to include difficult-to-diagnose neurological conditions like some forms of multiple sclerosis (MS), in which a virus is suspected.
The terminology is not very specific and sometimes the concepts of a slow virus and a stealth infection are combined and referred to as stealth virus. This term seems appropriate, since not only do they seem to invade the host tissues slowly, causing no symptoms, but they sneak up on the infected individual and only give warning when it is too late, like the stealth fighter bomber or the cloaking devices used by alien vessels in the Star Trek science fiction series.
The most notorious stealth virus is human immunodeficiency virus (HIV), the currently accepted cause of AIDS. HIV belongs to a family of viruses called lentivirus that mostly produce diseases in domestic livestock, though some affect primates. Two other stealth viruses are hepatitis C and HHV-6. For the virus, this is an ideal situation: a nearly symptomless infection, with the host's immune system unable to clearly detect or destroy the virus so it lives for decades within the host, which provides it comfortable and safe accommodations and then transmits it to others through reproductive activity.
The Virus and Cancer Connection: Cancer remains one of the leading causes of death in the developed countries. One out of every three (and it's rapidly approaching one out of two) individuals will develop some form of cancer. Despite efforts made in conventional medicine and science, and even alternative therapies, most people who develop cancer will die from it. Contrary to previous opinion, cancer is not merely a localized disease with a single cause, but it derives from a multitude of factors. Immune suppression by drugs used to control the rejection of transplanted organs, many commonly used pharmaceutical drugs, environmental toxins, tobacco smoking, diets high in fat, family genetics, stress, and others conditions all work as cofactors in contributing to cancer risk.
Oncogenesis, the term used to describe the development of cancer, has long been associated with viruses. Since viruses directly interact with genetic material, and due to their small size can potentially gain access to any site and cell in the body, it is no surprise that they can also cause cancer.
The first proven human cancer caused by a virus, human T-cell leukemia virus-1 (HTLV1), was identified in 1981. Though rare in North America and Europe, Burkitt's lymphoma, another virally induced cancer, caused by Epstein-Barr virus (EBV) is the most common cancer in children in tropical Africa. Anthony Epstein, the primary researcher (after whom the virus is named), was later to find several other tumors induced by EBV, including nasopharyngeal carcinoma and cancers of the lymph glands.
Other virally induced cancers include cervical cancer, one of the most common cancers in women, caused by the papillomavirus, a member of the same viral family that causes warts; hepatocellular carcinoma caused by hepatitis B and C; and Kaposi's sarcoma, caused by a newly discovered herpes virus, HHV-8, which occurs in AIDS.
Though the idea that viruses cause cancer seems to go in and out of favor, finding specific viral causes of cancer is a relatively new field of research, and an extremely important one. Before the 1970s, a considerable amount of research effort was directed towards finding a viral cause of cancer. Failing that, scientists abandoned the theory and moved on to genetic causes. Current statistics show that around 15 percent of all cancers worldwide are linked to viral infections.
One of the unanswered questions about virally induced cancers is why more cancers are developing from common viruses that have coexisted with humans for thousands of years. Why does the immune system let the virus get in at all and, once there, why does it let it get away with inducing cancerous changes in the infected cells?
No one yet has the answers to these questions, but it is known that there is a long interval between the original infection and the onset of cancer; in the case of hepatitis C, it may take thirty years or longer to induce cellular changes in the liver that cause cancer. Since the incidence of cancer is so high, and viruses are becoming more accepted as potential causative factors, it is important for each of us to prevent viral infections, effectively treat existing or suspected infections, and improve immune function. (I discuss how to accomplish this in part 2.)
Looking for a Viral Cause to Syndromes: It has become all too common for a medical doctor to blame the cause of a patient's complaints on a nonspecific virus when he does not know what the cause is. We used to call this type of diagnosis a “wastebasket diagnosis,” one that the physician just throws out. Though it may be the current trend to blame things on a virus, there may be some truth behind it. Many of the new illnesses are poorly defined and take on the characteristics of other diseases. They also display a constellation of symptoms, often unrelated, and situated in different parts of the body. This type of condition is called a syndrome, and many may have a viral cause, such as chronic fatigue syndrome, which has been blamed on EBV, chronic influenza A, and other viruses.
Even some forms of heart disease are linked to common viruses. Evidence that cytomegalovirus (CMV), found in nearly half of all American men over the age of 40, may be involved in atherosclerosis was only discovered in 1999. CMV and other chronic sub-clinical infections like the bacteria chlamydia can stimulate an immune response that causes inflammation in the heart and coronary blood vessels, and can even lead to fatal heart attacks.
Viral illnesses can also cause damage to the nervous system leading to paralysis, as is the case in transverse myelitis, a neurological syndrome caused by inflammation of the spinal cord and characterized by progressive demyelination (loss of the fatty tissue around the nerves). Its cause is often attributed to herpes simplex virus or Epstein-Barr virus. Both Parkinson's and Alzheimer's have been theoretically linked to a viral trigger or viral causative component.
Emerging Viruses: The AIDS pandemic is viewed as the paradigm for the emergence of new viral diseases. Though still hotly debated by some scientists (notably Donald Carrigan of the Wisconsin Viral Research Group and Peter Duesberg of the University of California in Berkeley, both discussed in more detail in chapter 2), by 1983 the cause of AIDS was identified as HIV, now divided into two types: HIV-1 and HIV-2. The source of the AIDS pandemic appears to have been Africa, with the first identified cases simultaneously occurring in the United States and Africa in 1981, though doctors were treating strange fatal infections in homosexual men in the late 1970s without knowing the cause of these deaths.
HIV is a retrovirus closely related to a virus that infects chimpanzees, and it appears to have first originated from a primate pool and then spread to humans. Among the many unanswered questions of the AIDS epidemic is why did a virus in monkeys spread to humans in the middle of the twentieth century when primates and humans have lived in close proximity in the same geographical regions for more than a hundred thousand years?
AIDS is a severe chronic viral infection. Statistics indicate that 50 million people worldwide are HIV-positive or have AIDS, and many of them—24.5 million—live in Africa. AIDS, like other viral diseases, spreads by infection, causing severe illness and eventual death in nearly all cases. Since it weakens the immune system by infecting and depleting CD4 helper T-lymphocytes (a type of white blood cell), AIDS patients can develop life-threatening co-infections such as pneumonia and fungal conditions.
There is no doubt that we are experiencing illnesses caused by viral infections that were either once rare or unheard of, or are new infections that were not involved in human illness in the past. The alarming rate at which they are occurring is of considerable concern.
However, new fatal infections or previously unrecognized diseases are familiar to human history. After all, smallpox was new to the Aztecs and Incas, but not to the Spanish. Another example is HHV-6, a recently identified herpes virus, which was first identified in 1988 by Japanese scientists as the cause of roseola, a common childhood disease. Though first scientifically discovered in 1920, roseola has been with us for a long time; therefore HHV-6 is also likely to have been around for at least as long. It is only our identification of it as the specific cause of roseola that is new. More importantly, why have some children in recent times who have contracted roseola developed severe neurological disease, damage to their kidneys and liver, and even died from it?
There is no doubt that we are experiencing illnesses caused by viral infections that were either once rare or unheard of, or are new infections that were not involved in human illness in the past. The alarming rate at which they are occurring is of considerable concern.
Linked to the increasing incidence of emerging infections is a mutation in the microbe and / or a change in the immune status of the host. A number of environmental and ecological factors are implicated here, such as changes in agriculture and wildlife habitats, new dams and irrigation systems, large-scale cutting of tropical rain forests, increasing human population density, rapid mass-transport systems (such as airplanes) allowing for infected humans to move from one location to another, the large number of wars in the twentieth century, and medical technology (transfusions, drug resistance, and immune suppressing drugs).
Other new viral infections include hepatitis C virus and the feared hemorrhagic fevers. Viral hemorrhagic fevers include yellow fever, dengue, hanta, Junin, Machupo, Lassa, Marburg, and the alarming Ebola viruses. In addition, known viruses like West Nile Fever are appearing in parts of the world where they were unheard of before. This mosquito-borne virus, a member of the viral family that causes encephalitis, was first isolated in Uganda in 1937. It has since appeared throughout Africa, India, China, and parts of Europe. However, West Nile virus (WNV) was never seen in the Western Hemisphere until late 1999 when its appearance in New York City caused eight deaths.
It seems there is no end to new and dangerous viruses. Among the most recent is TT virus (TTV). Like HCV, this new mystery virus was first discovered by the Japanese. It was at first thought a hepatitis virus since it produces a similar symptom presentation. But, according to Isa Mushahwar, the main researcher on the TTV trail, sufficient evidence shows that it is not related to the hepatitis virus families, and is structurally distinct enough to have a family of its own, the Circinoviridae.
Mushahwar speculates that TTV is present in 33–92 percent of the healthy population, and questions what these viruses are doing in humans and why they are not causing disease. However, immune dysfunction and mutation of a TTV subspecies can still cause disease in humans, as is the case with TTV-caused hepatitis.
Other new infections not caused by viruses are also appearing, including Lyme disease, the re-emergence of bubonic plague, and drug-resistant strains of tuberculosis (TB), all caused by bacteria. One third of the world's population is infected with TB, and there are 16 million active cases, 95 percent in developing nations—an astonishing figure.
Complications surrounding TB are frightening. The AIDS virus can activate dormant TB, leading to a lethal combination of a bacterial and viral infection. Unbeknownst to most people, TB is still the greatest single infectious cause of death worldwide, killing two million people each year. The re-emergence of malaria, compounded by drug resistance, is another serious concern with 300–500 million cases worldwide and one to two million deaths each year.
A New Viral Plague? Historically, it appears that diseases go into latent or dormant phases and then re-emerge when conditions are favorable for their spread—just as they do in our bodies. What is of concern now is the increasing variety of new viruses and other infectious diseases, the weakening of natural immunity from toxic pollutants and stress, and the spread of potent viruses into areas of dense human population. Every element is in place for a new plague.
In the past, when population density was considerably smaller and the balanced laws of nature still ruled the plains, savannas, forests, and mountains, human viral diseases were rare and appeared primarily in the overcrowded and filthy cities. After the great smallpox epidemics that occurred during the clash of cultures when Europeans colonized the rest of the planet, viral diseases were relatively quiescent. The new viral diseases described in this chapter (discussed in more detail in subsequent chapters) are a phenomenon of the late twentieth century, and they will be of great concern to us in the twenty-first century.
Since the linear scientific paradigm is having considerable difficulty in understanding and effectively managing these new diseases, especially viruses, it is important that we explore and try to understand other ways of viewing and treating disease. The evolutionary model is a good step, but it is still bound up with logical Western thinking. Not that logical thinking is the problem. The problem is that this one way of thinking occupies all our time and resources; if it is not working, repeating it endlessly will not work and will waste time. One option is to explore alternative models of disease causation and to develop a deeper insight into how we interact with viral illnesses.
Our world and the universe are complex. In order to advance civilization and understand the changing nature of disease, we must acknowledge that our contribution to modern disease has been the polluting of the environment with toxins and destroying the ecological balance that nature created. Alternative ways of conceptualizing medical care are therefore required.
To accomplish this we could usefully explore the ancient systems of energy medicine of the Chinese and Ayurvedic medicine from India. In these, we will find a way of thinking that fulfills the basic requirements to complement Western thinking. They are less linear, balance logic with intuition, work with the changing nature of biology rather than attempt to dominate it, and emphasize the health of the individual rather than concentrating excessively on disease. Today, as a culture, we are also beginning to re-examine our view of the beliefs of indigenous peoples, like shamanic practices and their attunement with natural forces. Evolutionary biology and quantum physics are only the beginning of this new way of thinking.
My own background demonstrates this new way of thinking in medicine which is supported by an increasing volume of research data and the conversion of many medical doctors to the practice of alternative therapies. A brief review of this background will make my point clear.
During my undergraduate studies in biology and anthropology, I became involved in native cultures, and in 1968 was “adopted” by a Siberian Eskimo family on St. Lawrence Island in the Bering Sea. After that I made numerous excursions, learning from indigenous cultures in North America, Mexico, and South America. Those experiences developed into my interest in enthomedical practices and ethnobotany, the study of medical plants used for healing by native peoples. I also extensively explored Chinese culture, philosophy, and health practices like qi gong and tai chi. In 1974, I started the study of acupuncture and Chinese medicine, receiving my first diploma in acupuncture in 1983 from the California Acupuncture College in San Diego and my doctor of Oriental medicine (O.M.D.) in 1985 from Sino-American University of Oriental Medicine in Los Angeles.
I completed my hospital rotations at the Shanghai College of Chinese Medicine in China. Study in naturopathic medicine followed my course of oriental medicine, and I received national board certification as a naturopathic physician (N.D.) in 1997 from the American Naturopathic Medicine Certification and Accreditation Board in Washington, D.C. Among my other credentials include a fellowship with the American Association of Integrative Medicine, and a diplomate certified in Integrative Medicine, and diplomate in Chinese Herbology.
I have sat at the feet of Chinese Taoist and Buddhist masters, and studied under Chinese, Ayurvedic, naturopathic, and medical doctors. I have hunted seal and walrus with Eskimo hunters, lived in remote jungle areas in Central and South America, and participated in indigenous healing ceremonies. These experiences, along with an open scientific mind, equipped me to explore other areas of consciousness; prompted me to think outside the conventional medical box, and to reconceptualize the causes of disease and how we heal.
Among these causes are the individual's inherent and created immune status, and the susceptibility to not only infectious disease but chronic disease and age-related disease as well. Subtle energy and balance between organ function, body chemistry, and the body's relationship to the immediate and greater environment play significant roles in health and disease, and I explain these ideas in more detail in chapter 5 and step 10.
So far in this chapter I have discussed viruses based on Western models of modern allopathic medicine and I have introduced current evolutionary theory, as rooted in Western thought. However, traditional forms of medicine, notably what is called Traditional Chinese Medicine, the source of acupuncture, has a different and, I contend, a viable alternative model for understanding and treating illness. That model is based not so much on biochemistry and physiology, but on the energy underlying both.
The Organization of Energy: The Chinese model of health is based upon balance and harmony within the individual and between the individual, society, and nature. According to Chinese medicine, there are four essential substances that rule this balance: qi (pronounced “chee”), blood, yin, and yang. Chinese scholars debate to this day about the nature of these substances, so it is not surprising if the concepts are difficult for a Westerner to understand. Let me try to explain them in a way that will help make further reading of the book much easier.
The force called qi is the vital intrinsic energy of all living things. Qi has five attributes: defense mechanisms, constant movement, transformation, warmth and the maintenance of body temperature, and holding things in place by resisting gravity. If the qi is strong, the body can defend itself against pestilence and disease. Emotional states also affect the qi. If the emotions are harmonious, then qi flows effortlessly and its defense mechanisms work well to guard one against infection.
In Chinese medicine, the blood is thought to be more than a fluid that carries oxygen, cells, and nutrients. It is one of the major media for the concentration of the life force, the qi. The other media for qi are the sexual secretions (semen), spinal fluid, and most importantly, the acupuncture meridians, which are conduits or channels where refined qi flows. If the blood is abundant, vital, and healthy, the qi is also strong and vital. The qi and blood are two sides of the same coin: the qi is invisible energy and the blood is energy made visible.
The Chinese insist, and I agree, that if you improve the quality of your blood through correct diet, herbal medicines, and acupuncture, the blood will purify itself and become vital and healthy. The same is true for the qi: you can enhance your body's qi by practicing slow moving exercises like tai chi (pronounced “tie chee”) and breathing exercises called qi gong (pronounced “chee gung”), by receiving acupuncture, and by doing meditation practices.
In addition, the constitution of the person is important. Some people have an innately stronger immunity than others; they require less attention to strengthening their system and may only need to prevent illness. Others who are weaker need to actively cultivate balance and inner strength through qi gong, the use of tonic herbs, and a balanced lifestyle. Herbs for cultivating qi and blood are discussed in part 2.
Qi and blood are among the most important aspects of the body but are governed by a yet deeper principle of mutually dependent opposites. According to Chinese cosmology, yin and yang are the underlying universal principles that make up the structure and character of all things on this planet. Yang is the male force and is aggressive, quick-acting, fiery, and symbolized by the sun. Yin is the feminine principle and is passive, more patient, cooler, and symbolized by the moon. Since one cannot exist without the other, the variety of relationships between yin and yang is endless. In the body yin and yang forces are called yin qi and yang qi, and when these are harmonious and in a balanced relationship, the individual is healthy. You might call this interplay “the dance of health.” However, when the yin qi and yang qi fall into conflict, the dance is disharmonious, the individual is more susceptible to infection, and illness arises.
In modern society, stress, overwork, the fast pace of living, and overuse of prescription drugs, especially antibiotics, causes a gradual reduction in the amount of yin qi, which predisposes the body to chronic viral diseases like AIDS and HCV.3 This concept will be discussed in more detail in chapter 5 and step 8. As you will see in the next section, the Chinese knew the concepts and clinical presentations of both acute and chronic viral diseases long before the West discovered viruses.
The Chinese have an unbroken history of keeping detailed medical records. As early as several thousand years ago, Chinese doctors were well aware of epidemic diseases and categorized them as “pestilent” factors. Based upon a complex codex of the nature and treatment of disease, they developed a comprehensive system of medicine that encompassed all types of illnesses, as well as health and preventive medicine. They were also adept at treating what we now know are viral diseases. According to the Chinese, pestilent factors were associated with the wind and changed from season to season.
In the The Yellow Emperor's Classic on Internal Medicine, a translation of Huang Ti Nei Ching (Veth 1949), the Yellow Emperor mused: “I should like to hear why it is that in certain years everyone is struck by a similar illness.” Shao-shih, a physician-sage of the second century B.C., answered: “This is the result of a manifestation of the winds of the eight seasonal turning points.”7
In traditional Chinese medicine, “wind” meant both the physical wind and a subtle wind that was similar to qi, invisible and active in the body. The Chinese concept of wind also carried the connotation of “bad air” or “evil wind” as a carrier of disease. One was “attached by wind” or became ill from the influence of an unfavorable circumstance carried upon the wind. This is not as simplistic as it might seem.
It is well known that viral particles of influenza spread through the atmosphere. The Chinese also believed that people were susceptible to seasonal differences in illnesses. The most vulnerable time was when one season transitioned to the next, like when summer is turning to fall, and at each of the solstices and equinoxes—making a total of eight turning points.
Though the ancient Chinese did not identify or name “viruses” as the direct cause of specific infectious diseases, they developed extraordinarily detailed empirical knowledge about the occurrence and treatment of what we now call viral diseases, including yellow fever, hepatitis, and influenza. In fact, since China is the homeland for many of these viruses, it is not surprising to find that Chinese practitioners have an extensive materia medica of antiviral herbal medications, many which are discussed in detail in part 2 of this book.
Modern doctors of Chinese medicine recognize viruses and viral diseases, while retaining the traditional knowledge of how the body's energy systems function and respond to viral infections. In fact, since the 1980s, intense research has been carried out on the identification of herbs with the most potential as antivirals. Both Chinese and Western scientists are investigating a new class of substances called immune modulators which enhance and normalize immune activity.
The Energy Model, Ecology, and Evolutionary Medicine: The energy model looks closely at the relationships of the outer environments, such as the workplace and home, and inner environments, such as the health of the large intestine and liver, and works towards improving their relationships and functions. It does not focus exclusively on pathology and the symptoms of disease.
The energy model is comprehensive and provides a holistic understanding of disease, supports health and focuses on prevention, including immune-enhancing medications, and it teaches exercises and lifestyle recommendations that improve immune function.
Therefore, the energy model is comprehensive and provides a holistic understanding of disease, supports health and focuses on prevention, including immuneenhancing medications, and it teaches exercises and lifestyle recommendations that improve immune function. It offers functional support for organs, such as the liver, that are critical in the process of removing viruses from our bodies, and prescribes potent antiviral herbs that reduce the overall viral load (discussed in later chapters).
The Chinese model of energy medicine dovetails with evolutionary medicine. Both look at a broader picture of disease placing it within ecological contexts and taking into consideration the specific individual's symptoms and condition. More importantly, though Chinese medicine may take longer to have a symptomatic effect, it poses little environmental impact by using low-tech methods and non-toxic medicines, and leaves the patient with few or no side effects. Often Chinese medical therapies strengthen the individual, leaving one in better condition than before the disease occurred, and they provide a curative effect unavailable with the use of chemical drugs.