Key points
- Normal blood glucose levels rarely go above 4–6 mmol/l, except for a short time after a meal.
- Diabetes is diagnosed when fasting glucose levels are 7.0 mmol/l or above, or more than 11.1 when there are obvious symptoms of high glucose – for example, excessive thirst or weight loss.
- Most people don’t have symptoms when they are diagnosed on a blood test.
- In many people, high glucose levels have been present but undetected for years before diagnosis.
- Occasionally, diabetes presents with a serious complication, such as a heart attack or stroke.
Chapter 1 described an up-to-date view of the origins of diabetes, and we saw that Type 2 is caused by a combination of a strong genetic susceptibility to diabetes and overnutrition that stresses the liver and pancreas, which then no longer work together in harmony to maintain stable low blood glucose levels. Dysfunctional insulin produced by the pancreas leads to glucose escaping from the liver overnight, and to blood glucose levels remaining high after a carbohydrate-rich meal. Abnormal insulin also leads to high blood pressure and abnormal cholesterol balance, and to a host of other important problems that are often overlooked while we focus too much on blood glucose levels (these problems are covered in Chapter 3). However, we can’t get away from the fact that although Type 2 diabetes is much, much more than ‘just’ a high blood glucose level, diagnosing it has always been based on the precise measurement of blood glucose.
Blood glucose tests in context
It’s worthwhile knowing a little about the history of why blood glucose has been the standard way to diagnose diabetes, and will remain so. As we saw in Chapter 1, it’s only over the past 30 years or so that we have been able to make a reliable distinction between Type 1 and Type 2 diabetes.
In Type 1 diabetes, the kind of diabetes that usually affects children and adolescents, the condition develops suddenly and the only organ to misbehave is the pancreas, where insulin is produced; therefore in this type of diabetes the only problem appeared to be high blood glucose levels. High blood pressure and blood vessel disorders – for example, in the heart and kidneys – certainly occur after many years with Type 1, but until recently they were still thought to be caused by persisting high glucose levels resulting from imperfect insulin treatment (since the pancreas fails almost completely in Type 1 diabetes, insulin is needed immediately and permanently). So it’s easy to understand why diabetes starting later in life was considered to be more or less the same condition as Type 1, though usually with a less scary onset. (The distinction was further blurred by the fact that between 1921 when insulin was first used in humans and the 1950s, the only treatments for any type of diabetes were diet and insulin.)
At this early stage of research into diabetes, epidemiologists (scientists who study disease in populations rather than individuals) measured blood glucose levels in large numbers of people so they could establish a ‘number’ that could be used to diagnose diabetes. They focused exclusively on blood glucose levels, and did not take account of, for example, blood pressure and lipids such as HDL cholesterol and triglycerides that we now know are as important as blood glucose in determining the long-term outcomes of Type 2. But since all diabetes at the time was considered to be a condition of high blood glucose levels, and because blood glucose can be measured reliably, easily and cheaply, that’s what they focused on. The unintended result of all this blood glucose-measuring activity is that Type 2 diabetes is still considered by many professionals and patients to be predominantly a problem of high blood glucose levels. Nevertheless, we have to accept that blood glucose will remain the diagnostic test for Type 2 diabetes, and we therefore need to understand the numbers that have been agreed, while always bearing in mind that high glucose is only the easily measurable tip of a large iceberg of other problems.
Key point: Although Type 2 diabetes usually includes high blood pressure and abnormal cholesterol levels as well as high blood glucose levels, historically we’ve always used blood glucose values to diagnose it.
What are ‘normal’ blood glucose levels?
Before discussing the blood glucose levels we use to diagnose diabetes, we need to get an idea of what are normal glucose levels in people who don’t have diabetes. We’ll defer the prickly problem of ‘pre-diabetes’ (the grey zone between strictly normal blood glucose levels and definite diabetes) until Chapter 3.
Figure 2.1 shows glucose levels monitored continuously over 24 hours in a thin young person – that is, someone at zero risk of having undiagnosed diabetes. Clock time runs along the bottom, from midnight to midnight. The test was run over four days, so there are four different lines (the average measurement is shown with a dotted line).
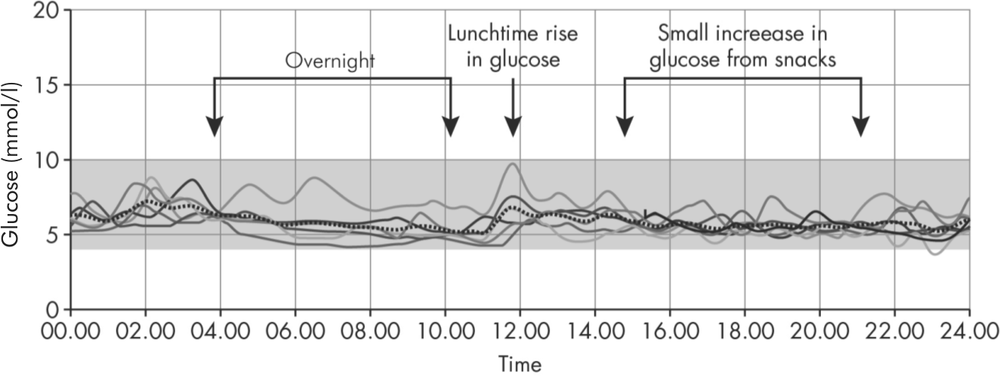
Figure 2.1: Glucose measurements taken continuously in a young, non-diabetic person of normal weight over four consecutive days.
I always find tracings like Figure 2.1 remarkable: glucose levels nearly always lie between 4 and 6 mmol/l. As you might expect, the graph looks even flatter and lower during the night (on the left), while during the day there are small blips caused by eating, especially around midday, when the subject seems to have eaten her highest-carbohydrate meal of the day. One day, the lunchtime blip is higher, reaching nearly 10 mmol/l. (This is an important point for Type 2s. Many would be disturbed to find a peak blood glucose of 10 shortly after a meal, but you can see that this is common in people without diabetes; the key point is how quickly the values return to normal – within about an hour in a non-diabetic individual, but up to three or even five hours in someone with Type 2.) Because blood glucose levels rise briefly after meals even in non-diabetic individuals, fasting glucose levels (eight hours or more after food) are used for diagnosis, as they are at their lowest and most stable in the fasting state.
Key point: In someone without diabetes, blood glucose levels are usually in the range 4–6 mmol/l, though they can rise to 10 or even perhaps higher for a very short time after a large meal, particularly if it contained lots of carbohydrates.
Another (very important) key point: Although non-diabetic glucose levels are usually 4–6 mmol/l, there is no advantage (and possibly some harm) in aiming for these low levels if you have diabetes, especially if you are taking insulin. In general, values between 6 and 10 mmol/l are near-ideal for all people taking medication or insulin (or both).
The time frame over which Type 2 diabetes develops
Type 1 diabetes develops very rapidly, usually over a few weeks, because the pancreas fails suddenly and permanently. The young people affected usually lose weight dramatically, often have raging thirst and can pass urine every few minutes, and feel weak and dreadful. This is what happens when blood glucose levels suddenly surge and stay there for a few weeks – most people with newly diagnosed Type 1 have glucose levels of 20 mmol/l or higher. This dramatic onset of symptoms is unusual in Type 2 diabetes, where the process is played out over a much longer time frame – years rather than weeks. However, we’ll see that this still occurs in Type 2 when the blood glucose levels rise sufficiently high and stay there.
The characteristic slow progression of Type 2, which causes no symptoms for a long time, was documented in what is called the ‘Whitehall study’ of British civil servants (see Reference section page 209). Blood glucose levels were measured every year until the expected small proportion of them developed diabetes (see Figure 2.2). Over the course of 10 years, the average fasting glucose levels rose only slightly, from 5.5 to 5.8 mmol/l, but a year before diagnosis it increased from 5.8 to 6.3, and then to 7.0 (which, as we will see, is the level at which Type 2 is diagnosed). The slow rise in the previous 10 years explains why an occasional blood glucose taken over this period will usually be normal, while the rapid rise in the two years preceding diagnosis explains why some people with Type 2 can have symptoms of high blood glucose for several months before diagnosis. The slow-then-fast trajectory accounts for the different ways Type 2 is diagnosed, and that’s what we will discuss next.
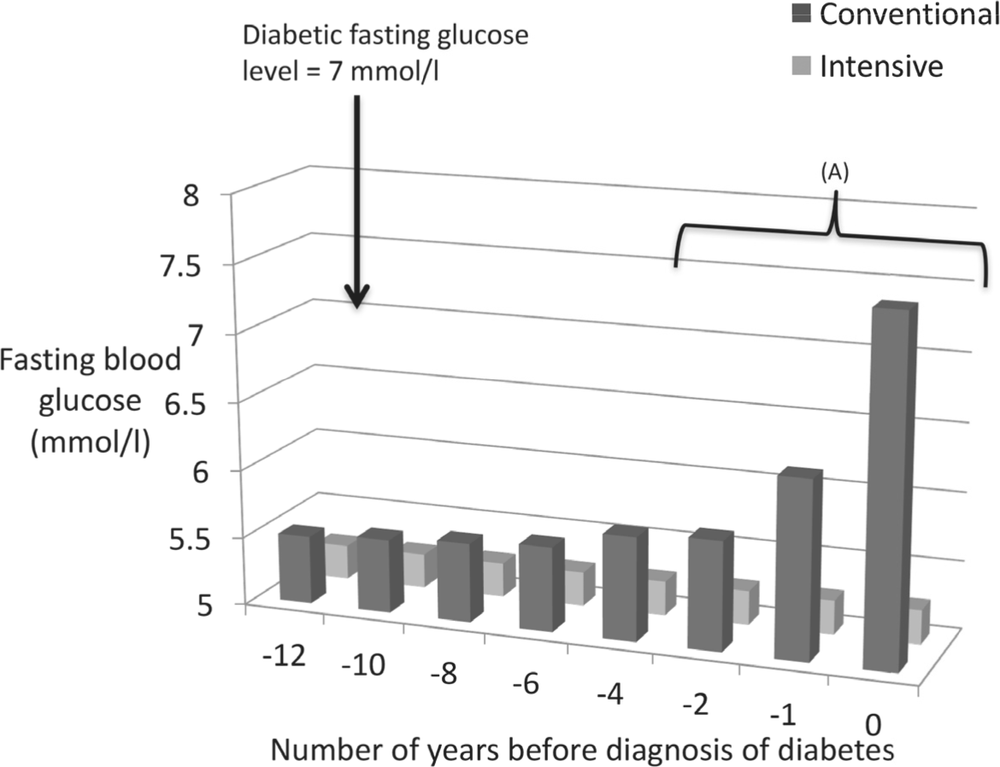
Figure 2.2: Blood glucose levels in the Whitehall study of civil servants. In people who go on to develop Type 2 diabetes, blood glucose levels rise very slowly for many years until about two years before diagnosis, when they increase from just under 6 mmol/l to 7 (A). Although this is the diagnostic value for diabetes, nobody has symptoms at this level. Follow-up stopped at this point, but you can see that if blood glucose levels continue to rise at the same fast rate, many people will start developing symptoms over the next year or two when they reach 12–13 or higher – this happens frequently in real life, in contrast to research studies where blood glucose levels are measured every year.
Diabetes diagnosed on a blood test without any symptoms of diabetes
These days most people are unaware they have diabetes until they have a routine blood test requested for other reasons (for example, many people with high blood pressure have a blood glucose test with their annual tests of kidney and liver function; a good idea, as hypertension is itself a risk factor for developing Type 2). Increasingly, people are self-diagnosing by doing a finger-prick blood glucose test using someone else’s meter. There’s one practical point: a high blood glucose won’t come up on a routine blood test because glucose needs a separate sample taken into a different blood tube, usually colour-coded yellow. If you’re concerned about your risk of developing Type 2, ask specifically for a blood glucose test.
What blood glucose level defines diabetes?
We now have to grasp the nettle, and mention the values needed to diagnose Type 2 diabetes. Amazingly, the whole world agrees that a fasting glucose level of 7.0 mmol/l or above is the diagnostic level. (It used to be 7.8, but relatively recently it has been revised downwards and it is unlikely to change again.) The reason the world agreed on 7.0 and above is that complications specifically due to diabetes – for example, those involving the retina of the eye (see Chapter 11) – almost never occur in people with values under 7.0.
Key point: Diabetes is diagnosed when a fasting glucose level is 7.0 mmol/l or higher. This measurement needs to be made in a laboratory – finger-prick blood tests using home glucose meters may give a broad indication, but aren’t accurate enough to make such an important diagnosis.
We can make an interesting observation from the non-diabetic glucose tracing in Figure 2.1. Glucose in a non-diabetic person runs between 4 and 6 mmol/l, yet diabetes is diagnosed when the value is only apparently slightly higher – that is, 7 or above. So it’s no surprise that most people diagnosed with diabetes have no symptoms.
The HbA1c test for diagnosis of Type 2
More recently most, but in this case not all, of the world has agreed that a specialised blood test known as the glycated haemoglobin (HbA1c) test can be used to diagnose diabetes. HbA1c indicates how high average blood glucose levels have been over the previous six to eight weeks. All people with diabetes are familiar with HbA1c, which has been used from the early 1980s to monitor diabetes annually or more frequently. We are less familiar using the test to diagnose diabetes, but you can see why it might be helpful. It could indicate whether someone has intermittently slightly high blood glucose measurements that wouldn’t be apparent on an occasional blood glucose test, and it would be particularly valuable in those Type 2s who have almost normal fasting glucose levels but who develop high values after meals. Because it looks backwards at the general blood glucose level, HbA1c gives the same result whatever time of day it’s measured, so unlike a diagnostic blood glucose test, it doesn’t have to be taken when fasting. HbA1c, like glucose, requires a separate blood tube, so it won’t be measured on a ‘routine’ blood test, and the result will take a few days to come back, compared with the glucose level which will return within a day (even quicker if the laboratory finds it is very high). HbA1c isn’t accepted worldwide as a test for diabetes, but it’s still useful.
The accuracy of blood glucose and HbA1c measurements made the ‘oral glucose tolerance test’ obsolete, except in pregnancy. The aim of this test was to measure how well the body coped with a large (very large) dose of glucose. Blood glucose tests were taken fasting and two hours after the glucose drink. Although this test should have hit the history books about 10 years ago, it still surfaces occasionally, as it is still available in hospitals for diagnosing diabetes during pregnancy.
Key point: An HbA1c of 6.5% or more (45 mmol/mol in the units introduced in 2011) can be used to diagnose diabetes.
Symptoms of diabetes caused by high blood glucose levels
Urinary symptoms
In non-diabetic people, the body has a remarkable ability to hang on to glucose. This shouldn’t be a surprise: when humans didn’t have access to regular food, which was the case for nearly all of us until very recently, it was imperative to retain as much glucose as possible so that the body – and especially the brain – could continue functioning. This responsibility for preciously guarding glucose fell to the kidneys: they filter thousands of litres of blood every day. Kidneys have a very effective mechanism for reabsorbing glucose from the urine back into the circulation. The result is that people without diabetes (and many with well-controlled diabetes) almost never have detectable glucose in the urine.
However, when blood glucose levels rise above about 10 mmol/l, the kidney’s glucose-retaining mechanism finds it difficult to cope, and glucose starts leaking into the urine. The higher the blood glucose level, the more finds its way into the urine. This has several consequences. First, when glucose passes into the urine, it takes extra salt and water along with it. The result: excessive urine, so that sometimes people with high blood glucose levels end up peeing very frequently, day and night. Excessive loss of glucose, salt and water in the urine leads to thirst, and many people start drinking water during the night as well as visiting the loo, and carrying large bottles of water around with them. Second, because glucose is the body’s major source of energy, if it is lost in the urine then it isn’t available to be used by the muscles. Result: unintentional weight loss. At first, losing some weight is often welcomed, but if it continues, it’s clear something’s not right.
Throughout this book I’m doing my best not to focus on specific drug treatments, as I think they get quite sufficient publicity, but it’s worth noting that scientists have exploited this kidney mechanism to develop a new class of diabetes drugs. These are the ‘flozin’ drugs, also called ‘SGLT2 inhibitors’ – for example, dapagliflozin, canagliflozin and empagliflozin. They prevent the kidney reabsorbing glucose from the urine, so deliberately encourage loss of glucose – in a gentle and controlled way, of course. More urinary glucose means lower blood glucose levels, and with the energy lost, some weight reduction. The downside is that some people tend to pee excessively when they take these newer medications, and there is a risk of the fungal infection thrush.
Infections and blurred vision
Like humans, bugs (bacteria and fungi) love glucose and thrive on it. So, genital irritation due to thrush (the candida fungus) is common when glucose levels are high. Also, although not so common these days, bacterial skin infections, such as boils, can occur when blood glucose levels have been high for a long time. Finally, if glucose levels remain high for weeks, the lens of the eye becomes dehydrated, and intermittent blurred vision is a well-known symptom. It often prompts a visit to the optometrist, who is likely to recognise the symptom and confirm it with an eye examination. (Because this symptom takes a long time to develop, blurred vision doesn’t settle until a few weeks after blood glucose levels fall.)
Many people developing these reversible symptoms of diabetes have blood glucose levels in the range 15–20 mmol/l. The rules allow a diagnosis of Type 2 diabetes if someone has these symptoms and a blood glucose level measured at any time of day, not necessarily fasting, is 11.1 mmol/l or higher. Because the diagnosis of diabetes has significant consequences for people and their families, a repeat test – after fasting – is sometimes needed, but if the blood test was done in a laboratory and is very high, then there’s no need for a repeat (an HbA1c measurement would confirm the diabetes, and give an indication of how high the average blood glucose had been over the past few weeks).
Symptoms of the complications of diabetes
Most people, like the civil servants in the Whitehall study mentioned earlier, slide very gently into diabetes. But there is another, fortunately much smaller, group who seem to have had glucose levels well into the diabetes range for years before they are diagnosed. I have encountered several people who clearly describe periods where they have had symptoms of diabetes that have then settled, perhaps of their own accord, or with weight loss or increased exercise, only for the symptoms to return and then to have the diagnosis confirmed. They often have detectable diabetes complications affecting the blood vessels, and sometimes symptoms of nerve damage in the feet – for example, numbness, or pins and needles, and in men often accompanied by erectile dysfunction. Using information on the most specific of these complications (retinopathy affecting the eye), the epidemiologists calculate that diabetic blood glucose levels have been present for an average of seven years, but we will see in Chapter 3 that other factors that stress the blood vessels tend to cluster with high glucose levels – the metabolic syndrome. So over the seven years that blood glucose levels were high, there is likely to be high blood pressure, abnormal cholesterol levels and an increased tendency for the blood to clot. All these are likely to have gone undetected (and may have been made worse by smoking), and it’s not surprising that some people are first diagnosed with diabetes when they are admitted to hospital with one of its most serious complications – a heart attack.
In the early 2000s it was found that up to one third of patients admitted to hospital with a heart attack had diabetes that had not been diagnosed before their admission. This still occurs frequently: a double and terrible shock – newly diagnosed diabetes and a heart attack. The first inkling some patients have of their diabetes is a stroke or mini-stroke (transient ischaemic attack or TIA).
This highlights two themes we’ll discuss further: first, mild but persistent elevations in blood glucose levels that do not cause symptoms, but nevertheless contribute to the long-term complications of diabetes. The sudden rise around the time of diagnosis (or, indeed, after an occasional blow-out meal) comes as a shock, but except in very rare cases does not cause serious problems. Second, Type 2 diabetes can cause undetected damage to blood vessels throughout the body. This leads to the question, still unresolved, whether people at risk of diabetes should be screened every so often. The discussion would occupy books much larger than this one, but there are simple questionnaires that can indicate your risk of diabetes – for example, the one promoted by Diabetes UK. If you are at risk, don’t forget to nudge other members of your family to estimate their risk, as Type 2 runs so strongly within families.
Summary
Although Type 2 diabetes is not just a condition of high blood glucose levels, measuring glucose goes back a long way and is cheap and reliable. Diabetes is diagnosed when fasting glucose levels are 7.0 mmol/l or higher, compared with 4–6 in people without diabetes. Most people don’t have symptoms at blood glucose levels of 7–10 (and these may have been present undetected and without symptoms for many years), but higher values result in glucose leaking into the urine, causing thirst, frequent toilet visits and occasionally weight loss, blurred vision and an increased risk of fungal and bacterial infections. A few people first find out about their Type 2 diabetes when they have a major illness, usually involving blockages to blood vessels, especially heart attacks and strokes.