41
Sports Medicine & Outpatient Orthopedics
Anthony Luke, MD, MPH
C. Benjamin Ma, MD
Musculoskeletal problems account for about 10–20% of outpatient primary care clinical visits. Orthopedic problems can be classified as traumatic (ie, injury-related) or atraumatic (ie, degenerative or overuse syndromes) as well as acute or chronic. The history and physical examination are sufficient in most cases to establish the working diagnosis; the mechanism of injury is usually the most helpful part of the history in determining the diagnosis.
SHOULDER
1. Subacromial Impingement Syndrome
ESSENTIALS OF DIAGNOSIS

 Shoulder pain with overhead motion.
Shoulder pain with overhead motion.
 Night pain with sleeping on shoulder.
Night pain with sleeping on shoulder.
 Numbness and pain radiation below the elbow are usually due to cervical spine disease.
Numbness and pain radiation below the elbow are usually due to cervical spine disease.
 General Considerations
General Considerations
The shoulder is a ball and socket joint. The socket is very shallow, however, which enables this joint to have the most motion of any joint. The shoulder, therefore, relies heavily on the surrounding muscles and ligaments to provide stability. The subacromial impingement syndrome describes a collection of diagnoses that cause mechanical inflammation in the subacromial space. Causes of impingement syndrome can be related to muscle strength imbalances, poor scapula control, rotator cuff tears, subacromial bursitis, and bone spurs.
With any shoulder problem, it is important to establish the patient’s hand dominance, occupation, and recreational activities because shoulder injuries may present differently depending on the demands placed on the shoulder joint. For example, baseball pitchers with impingement syndrome may complain of pain while throwing. Alternatively, older adults with even full-thickness rotator cuff tears may not complain of any pain because the demands on the joint are low.
 Clinical Findings
Clinical Findings
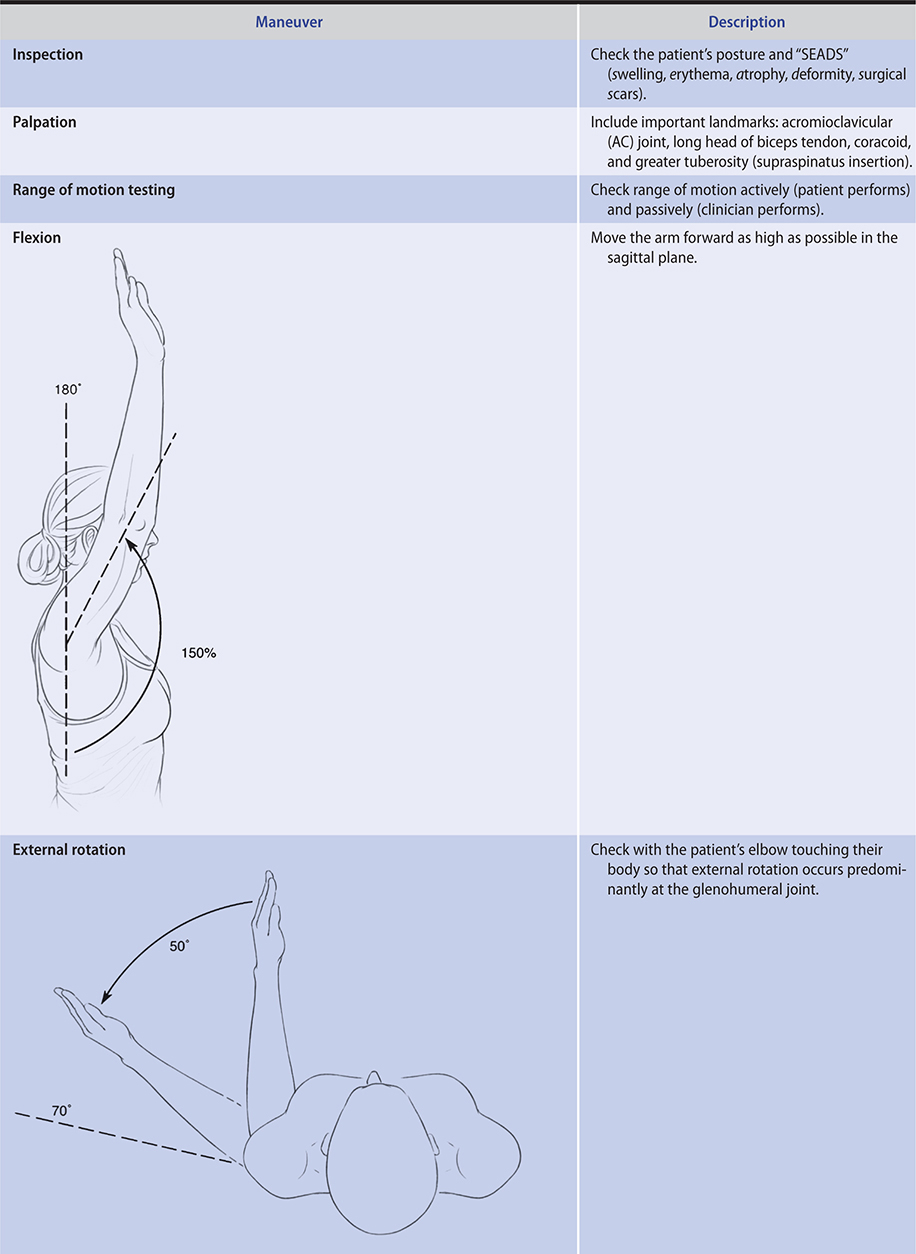
A. Symptoms and Signs
Subacromial impingement syndrome classically presents with one or more of the following: pain with overhead activities, nocturnal pain with sleeping on the shoulder, or pain on internal rotation (eg, putting on a jacket or bra). On inspection, there may be appreciable atrophy in the supraspinatus or infraspinatus fossa. The patient with impingement syndrome can have mild scapula winging or “dyskinesis.” The patient often has a rolled-forward shoulder posture or head-forward posture. On palpation, the patient can have tenderness over the anterolateral shoulder at the edge of the greater tuberosity. The patient may lack full active range of motion (Table 41–1) but should have preserved passive range of motion. Impingement symptoms can be elicited with the Neer and Hawkins impingement signs (Table 41–1).
Table 41–1. Shoulder examination.


B. Imaging
The following four radiographic views should be ordered to evaluate subacromial impingement syndrome: the anteroposterior (AP) scapula, the AP acromioclavicular joint, the lateral scapula (scapular Y), and the axillary lateral. The AP scapula view can rule out glenohumeral joint arthritis. The AP acromioclavicular view evaluates the acromioclavicular joint for inferior spurs. The scapula Y view evaluates the acromial shape, and the axillary lateral view visualizes the glenohumeral joint as well and for the presence of os acromiale.
MRI of the shoulder may demonstrate full- or partial-thickness tears or tendinosis. Ultrasound evaluation may demonstrate thickening of the rotator cuff tendons and tendinosis. Tears may also be visualized on ultrasound, although it is more difficult to identify partial tears from small full-thickness tears than on MRI.
 Treatment
Treatment
A. Conservative
The first-line treatment for impingement syndrome is usually a conservative approach with education, activity modification, and physical therapy exercises. Impingement syndrome can be caused by muscle weakness or tear. Rotator cuff muscle strengthening can alleviate weakness or pain, unless the tendons are seriously compromised, in which case exercises may cause more symptoms. Physical therapy is directed at rotator cuff muscle strengthening, scapula stabilization, and postural exercises. There is no strong evidence supporting the effectiveness of ice and NSAIDs as a prolonged therapy. In a Cochrane review, corticosteroid injections produced slightly better relief of symptoms in the short term when compared with placebo. Most patients respond well to conservative treatment.
B. Surgical
Procedures include arthroscopic acromioplasty with coracoacromial ligament release, bursectomy, or debridement or repair of rotator cuff tears. However, the value of acromioplasty alone for rotator cuff problems is not supported by evidence.
 When to Refer
When to Refer
• Failure of conservative treatment over 3 months.
• Young and active patients with impingement due to full-thickness rotator cuff tears.
Consigliere P et al. Subacromial impingement syndrome: management challenges. Orthop Res Rev. 2018 Oct 23;10:83–91. [PMID: 30774463]
Lai CC et al. Effectiveness of stretching exercise versus kinesiotaping in improving length of the pectoralis minor: a systematic review and network meta-analysis. Phys Ther Sport. 2019 Nov;40:19–26. [PMID: 31442850]
McFarland EG et al. Clinical faceoff: what is the role of acromioplasty in the treatment of rotator cuff disease? Clin Orthop Relat Res. 2018 Sep;476(9):1707–12. [PMID: 30001291]
Saracoglu I et al. Does taping in addition to physiotherapy improve the outcomes in subacromial impingement syndrome? A systematic review. Physiother Theory Pract. 2018 Apr;34(4):251–63. [PMID: 29111849]
2. Rotator Cuff Tears
ESSENTIALS OF DIAGNOSIS

 A common cause of shoulder impingement syndrome after age 40.
A common cause of shoulder impingement syndrome after age 40.
 Difficulty lifting the arm with limited active range of motion.
Difficulty lifting the arm with limited active range of motion.
 Weakness with resisted strength testing suggests full-thickness tears.
Weakness with resisted strength testing suggests full-thickness tears.
 Tears can occur following trauma or can be more degenerative.
Tears can occur following trauma or can be more degenerative.
 General Considerations
General Considerations
Rotator cuff tears can be caused by acute injuries related to falls on an outstretched arm or to pulling on the shoulder. It can also be related to chronic repetitive injuries with overhead movement and lifting. Partial rotator cuff tears are one of the most common reasons for impingement syndrome. Full-thickness rotator cuff tears are usually more symptomatic and may require surgical treatment. The most commonly torn tendon is the supraspinatus.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Most patients complain of weakness or pain with overhead movement. Night pain is also a common complaint. The clinical findings with rotator cuff tears include those of the impingement syndrome except that with full-thickness rotator cuff tears there may be more obvious weakness noted with light resistance testing of specific rotator cuff muscles. Supraspinatus tendon strength is tested with resisted shoulder abduction at 90 degrees with slight forward flexion to around 45 degrees (“open can” test). Infraspinatus/teres minor strength is tested with resisted shoulder external rotation with shoulder at 0 degrees of abduction and elbow by side. Subscapularis strength is tested with the “lift-off” or “belly-press” tests. The affected patient usually also has positive Neer and Hawkins impingement tests (Table 41–1).
B. Imaging
Recommended radiographs are similar to impingement syndrome: AP scapula (glenohumeral), axillary lateral, supraspinatus outlet, and AP acromioclavicular joint views. The AP scapula view is useful in visualizing rotator cuff tears because degenerative changes can appear between the acromion and greater tuberosity of the shoulder. Axillary lateral views show superior elevation of the humeral head in relation to the center of the glenoid. Supraspinatus outlet views allow evaluation of the shape of the acromion. High-grade acromial spurs are associated with a higher incidence of rotator cuff tears. The AP acromioclavicular joint view evaluates for the presence of acromioclavicular joint arthritis, which can mimic rotator cuff tears, and for spurs that can cause rotator cuff injuries.
MRI is the best method for visualizing rotator cuff tears. The MR arthrogram can show partial or small (less than 1 cm) rotator cuff tears. For patients who cannot undergo MRI testing or when postoperative artifacts limit MRI evaluations, ultrasonography can be helpful.
 Treatment
Treatment
Partial rotator cuff tears may heal with scarring. Most partial rotator cuff tears can be treated with physical therapy and scapular and rotator cuff muscle strengthening. However, research suggests that 40% of the partial-thickness tears progress to full-thickness tears in 2 years. Physical therapy can strengthen the remaining muscles to compensate for loss of strength and can have high rate of success for chronic tears. Physical therapy is also an option for older sedentary patients. On the contrary, full-thickness rotator cuff tears do not heal well and also have a tendency to increase in size with time. Forty-nine percent of the full-thickness tears get bigger over an average of 2.8 years. When tears get larger, they are also associated with worsening pain. Fatty infiltration is a degenerative process where muscle is being replaced by fat following injury to the rotator cuff tendons. Fatty infiltration progresses in full-thickness rotator cuff tears and it is a negative prognostic factor for successful surgical treatment. Fatty infiltration is an irreversible process so operative interventions are usually performed when the degree of infiltration is low. Most young active patients with acute, full-thickness tears should be treated with operative fixation. Full-thickness subscapularis tendon tears should undergo surgical repair since untreated tears usually lead to premature osteoarthritis (OA) of the shoulder. Nonetheless, physical therapy is indicated for atraumatic degenerative rotator cuff tears and success can be as high as 70%. That said, long-term (10-year) outcome studies show that surgical repair of rotator cuff tears can result in better outcomes than physical therapy alone.
 When to Refer
When to Refer
• Young and active patients with full-thickness rotator cuff tears.
• Partial tears with greater than 50% involvement and with significant pain.
• Acute rotator cuff tears and loss of function.
• Older and sedentary patients with full-thickness rotator cuff tears who have not responded to nonoperative treatment.
• Full-thickness subscapularis tears.
Allen H et al. Overuse injuries of the shoulder. Radiol Clin North Am. 2019 Sep;57(5):897–909. [PMID: 31351540]
Amoo-Achampong K et al. Evaluating strategies and outcomes following rotator cuff tears. Shoulder Elbow. 2019 May;11(1 Suppl):4–18. [PMID: 31019557]
Katthagen JC et al. Improved outcomes with arthroscopic repair of partial-thickness rotator cuff tears: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018 Jan;26(1):113–24. [PMID: 28526996]
Mannava S et al. Options for failed rotator cuff repair. Sports Med Arthrosc Rev. 2018 Sep;26(3):134–8. [PMID: 30059448]
Moosmayer S et al. At a 10-year follow-up, tendon repair is superior to physical therapy in the treatment of small and medium-sized rotator cuff tears. J Bone Joint Surg Am. 2019 Jun19;101(12):1050–60. [PMID: 31220021]
Novi M et al. Irreparable rotator cuff tears: challenges and solutions. Orthop Res Rev. 2018 Dec 5;10:93–103. [PMID: 30774464]
Piper CC et al. Operative versus nonoperative treatment for the management of full-thickness rotator cuff tears: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2018 Mar;27(3):572–6. [PMID: 29169957]
Sochacki KR et al. Superior capsular reconstruction for massive rotator cuff tear leads to significant improvement in range of motion and clinical outcomes: a systematic review. Arthroscopy. 2019 Apr;35(4):1269–77. [PMID: 30878330]
Stoll LE et al. Lower trapezius tendon transfer for massive irreparable rotator cuff tears. Orthop Clin North Am. 2019 Jul;50(3):375–82. [PMID: 31084840]
3. Shoulder Dislocation & Instability
ESSENTIALS OF DIAGNOSIS

 Most dislocations (95%) are in the anterior direction.
Most dislocations (95%) are in the anterior direction.
 Pain and apprehension with an unstable shoulder that is abducted and externally rotated.
Pain and apprehension with an unstable shoulder that is abducted and externally rotated.
 Acute shoulder dislocations should be reduced as quickly as possible, using manual relocation techniques if necessary.
Acute shoulder dislocations should be reduced as quickly as possible, using manual relocation techniques if necessary.
 General Considerations
General Considerations
The shoulder is a ball and socket joint, similar to the hip. However, the bony contours of the shoulder bones are much different than the hip. Overall, the joint has much less stability than the hip, allowing greater movement and action. Stabilizing the shoulder joint relies heavily on rotator cuff muscle strength and also scapular control. If patients have poor scapular control or weak rotator cuff tendons or tears, their shoulders are more likely to have instability. Ninety-five percent of the shoulder dislocations/instability occur in the anterior direction. Dislocations usually are caused by a fall on an outstretched and abducted arm. Patients complain of pain and feeling of instability when the arm is in the abducted and externally rotated position. Posterior dislocations are usually caused by falls from a height, epileptic seizures, or electric shocks. Traumatic shoulder dislocation can lead to instability. The rate of repeated dislocation is directly related to the patient’s age: patients aged 21 years or younger have a 70–90% risk of redislocation, whereas patients aged 40 years or older have a much lower rate (20–30%). Other risks include male gender and patients with hyperlaxity. Ninety percent of young active individuals who had traumatic shoulder dislocation have labral injuries often described as Bankart lesions when the anterior inferior labrum is torn, which can lead to continued instability. Older patients (over age 55 years) are more likely to have rotator cuff tears or fractures following dislocation. Atraumatic shoulder dislocations are usually caused by intrinsic ligament laxity or repetitive microtrauma leading to joint instability. This is often seen in swimmers, gymnasts, and pitchers as well as other athletes involved in overhead and throwing sports.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
For acute traumatic dislocations, patients usually have an obvious deformity with the humeral head dislocated anteriorly. The patient holds the shoulder and arm in an externally rotated position. The patient complains of acute pain and deformity that are improved with manual relocation of the shoulder. Reductions are usually performed in the emergency department. Even after reduction, the patient will continue to have limited range of motion and pain for 4–6 weeks, especially following a first-time shoulder dislocation.
Patients with recurrent dislocations can have less pain with subsequent dislocations. Posterior dislocations can be easily missed because the patient usually holds the shoulder and arm in an internally rotated position, which makes the shoulder deformity less obvious. Patients complain of difficulty pushing open a door.
Atraumatic shoulder instability is usually well tolerated with activities of daily living. Patients usually complain of a “sliding” sensation during exercises or strenuous activities such as throwing. Such dislocations may be less symptomatic and can often undergo spontaneous reduction of the shoulder with pain resolving within days after onset. The clinical examination for shoulder instability includes the apprehension test, the load and shift test, and the O’Brien test (Table 41–1). Most patients with persistent shoulder instability have preserved range of motion.
B. Imaging
Radiographs for acute dislocations should include a standard trauma series of AP and axillary lateral scapula (glenohumeral) views to determine the relationship of the humerus and the glenoid and to rule out fractures. Orthogonal views are used to identify a posterior shoulder dislocation, which can be missed easily with one AP view of the shoulder. An axillary lateral view of the shoulder can be safely performed even in the acute setting of a patient with a painful shoulder dislocation. A scapula Y view in the acute setting is insufficient to diagnose dislocation. For chronic injuries or symptomatic instability, these recommended radiographic views are helpful to identify bony injuries and Hill-Sachs lesions (indented compression fractures at the posterior-superior part of the humeral head associated with anterior shoulder dislocation). MRI is commonly used to show soft tissue injuries to the labrum and to visualize associated rotator cuff tears. MRI arthrograms better identify labral tears and ligamentous structures. Three-dimensional CT scans are used to determine the significance of bone loss.
 Treatment
Treatment
For acute dislocations, the shoulder should be reduced as soon as possible. The Stimson procedure is the least traumatic method and is quite effective. The patient lies prone with the dislocated arm hanging off the examination table with a weight applied to the wrist to provide traction for 20–30 minutes. Afterward, gentle medial mobilization can be applied manually to assist the reduction. The shoulder can also be reduced with axial “traction” on the arm with “counter-traction” along the trunk. The patient should be sedated and relaxed. The shoulder can then be gently internally and externally rotated to guide it back into the socket.
Initial treatment of acute shoulder dislocations should include sling immobilization for 2–4 weeks along with pendulum exercises. Early physical therapy can be used to maintain range of motion and strengthening of rotator cuff muscles. Patients can also modify their activities to avoid active and risky sports. For patients with a traumatic incident and unilateral shoulder dislocation, a Bankart lesion is commonly present. The risk of recurrence is dependent on the age of first shoulder dislocation. Up to 70% of young patients (age less than 27 years) can have a recurrence whereas only 10% of patients older than age 40 have recurrences. However, once the patient has a second dislocation, the recurrence rate is extremely high, up to 95%, regardless of age. Operative intervention is the only treatment that has been shown to decrease recurrence. Open and arthroscopic stabilization have very similar outcomes. Repeated dislocations have been shown to increase the risk of arthritis and further bony deterioration.
The treatment of atraumatic shoulder instability is different than that of traumatic shoulder instability. Patients with chronic, recurrent shoulder dislocations should be managed with physical therapy and a regular maintenance program, consisting of scapular stabilization and postural and rotator cuff strengthening exercises. Activities may need to be modified. Surgical reconstructions are less successful for atraumatic shoulder instability than for traumatic shoulder instability. However, patients with recurrent dislocations have much higher incidence of bone loss or biceps pathology when compared to patients with first-time dislocations. They are also more likely to require open surgery with bone augmentation rather than arthroscopic stabilization.
 When to Refer
When to Refer
• Patients who are at risk for second dislocation, such as young patients and certain job holders (eg, police officers, firefighters, and rock climbers), to avoid recurrent dislocation or dislocation while at work.
• Patients who have not responded to a conservative approach or who have chronic instability.
Barlow JD et al. Surgical treatment outcomes after primary vs recurrent anterior shoulder instability. J Clin Orthop Trauma. 2019 Mar–Apr;10(2):222–30. [PMID: 30828182]
Borbas P et al. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. J Shoulder Elbow Surg. 2019 Oct;28(10):2031–8. [PMID: 31350107]
Garcia JC Jr et al. Comparative systematic review of fixation methods of the coracoid and conjoined tendon in the anterior glenoid to treat anterior shoulder instability. Orthop J Sports Med. 2019 Jan 25;7(1):2325967118820539. [PMID: 30719477]
Gottlieb M et al. Point-of-care ultrasound for the diagnosis of shoulder dislocation: a systematic review and meta-analysis. Am J Emerg Med. 2019 Apr;37(4):757–61. [PMID: 30797607]
Hasebroock AW et al. Management of primary anterior shoulder dislocations: a narrative review. Sports Med Open. 2019 Jul 11;5(1):31. [PMID: 31297678]
Rugg CM et al. Surgical stabilization for the first-time shoulder dislocators: a multicenter analysis. J Shoulder Elbow Surg. 2018 Apr;27(4):674–85. [PMID: 29321108]
Tamaoki MJ et al. Surgical versus conservative interventions for treating acromioclavicular dislocation of the shoulder in adults. Cochrane Database Syst Rev. 2019 Oct 11;10:CD007429. [PMID: 31604007]
4. Adhesive Capsulitis (“Frozen Shoulder”)
ESSENTIALS OF DIAGNOSIS

 Very painful shoulder triggered by minimal or no trauma.
Very painful shoulder triggered by minimal or no trauma.
 Pain out of proportion to clinical findings during the inflammatory phase.
Pain out of proportion to clinical findings during the inflammatory phase.
 Stiffness during the “freezing” phase and resolution during the “thawing” phase.
Stiffness during the “freezing” phase and resolution during the “thawing” phase.
 General Considerations
General Considerations
Adhesive capsulitis (“frozen shoulder”) is seen commonly in patients 40 to 65 years old. It is more commonly seen in women than men, especially in perimenopausal women or in patients with endocrine disorders, such as diabetes mellitus or thyroid disease. There is higher incidence following breast cancer care (such as mastectomy). Adhesive capsulitis is a self-limiting but very debilitating disease.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Patients usually present with a painful shoulder that has a limited range of motion with both passive and active movements. A useful clinical sign is limitation of movement of external rotation with the elbow by the side of the trunk (Table 41–1). Strength is usually normal but it can appear diminished when the patient is in pain.
There are three phases: the inflammatory phase, the freezing phase, and the thawing phase. During the inflammatory phase, which usually lasts 4–6 months, patients complain of a very painful shoulder without obvious clinical findings to suggest trauma, fracture, or rotator cuff tear. During the “freezing” phase, which also usually lasts 4–6 months, the shoulder becomes stiffer and stiffer even though the pain is improving. The “thawing” phase can take up to a year as the shoulder slowly regains its motion. The total duration of an idiopathic frozen shoulder is usually about 24 months; it can be much longer for patients who have trauma or an endocrinopathy.
B. Imaging
Standard AP, axillary, and lateral glenohumeral radiographs are useful to rule out glenohumeral arthritis, which can also present with limited active and passive range of motion. Imaging can also rule out calcific tendinitis, which is an acute inflammatory process in which calcifications are visible in the soft tissue. However, adhesive capsulitis is usually a clinical diagnosis, and it does not need an extensive diagnostic workup.
 Treatment
Treatment
Adhesive capsulitis is caused by acute inflammation of the capsule followed by scarring and remodeling. During the acute “freezing” phase, NSAIDs and physical therapy are recommended to maintain motion. There is also evidence of short-term benefit from intra-articular corticosteroid injection or oral prednisone. A randomized control trial showed that intra-articular corticosteroid injection provided better pain relief than NSAIDs in the first 8 weeks. However, no difference was seen in range of motion or pain after 12 weeks, which is similar to other noncontrolled studies. One study demonstrated improvement at 6 weeks but not 12 weeks following 30 mg of daily prednisone for 3 weeks. During the “freezing” phase, the shoulder is less painful but remains stiff. Anti-inflammatory medication is not as helpful during the “thawing” phase as it is during the “freezing” phase, and the shoulder symptoms usually resolve with time. Surgical treatments, which are rarely indicated, include manipulation under anesthesia and arthroscopic release.
 When to Refer
When to Refer
• When the patient does not respond after more than 6 months of conservative treatment.
• When there is no progress in or worsening of range of motion over 3 months.
Alsubheen SA et al. Effectiveness of nonsurgical interventions for managing adhesive capsulitis in patients with diabetes: a systematic review. Arch Phys Med Rehabil. 2019 Feb;100(2):350–65. [PMID: 30268804]
Boutefnouchet T et al. Comparison of outcomes following arthroscopic capsular release for idiopathic, diabetic and secondary shoulder adhesive capsulitis: a systematic review. Orthop Traumatol Surg Res. 2019 Sep;105(5):839–46. [PMID: 31202716]
Cho CH et al. Treatment strategy for frozen shoulder. Clin Orthop Surg. 2019 Sep;11(3):249–57. [PMID: 31475043]
Fields BKK et al. Adhesive capsulitis: review of imaging findings, pathophysiology, clinical presentation, and treatment options. Skeletal Radiol. 2019 Aug;48(8):1171–84. [PMID: 30607455]
Wang W et al. Effectiveness of corticosteroid injections in adhesive capsulitis of shoulder: a meta-analysis. Medicine (Baltimore). 2017 Jul;96(28):e7529. [PMID: 28700506]
Xiao RC et al. Evaluating nonoperative treatments for adhesive capsulitis. J Surg Orthop Adv. 2017 Winter;26(4):193–9. [PMID: 29461189]
SPINE PROBLEMS
1. Low Back Pain
ESSENTIALS OF DIAGNOSIS

 Nerve root impingement is suspected when pain is leg-dominant rather than back-dominant.
Nerve root impingement is suspected when pain is leg-dominant rather than back-dominant.
 Alarming symptoms include unexplained weight loss, failure to improve with treatment, severe pain for more than 6 weeks, and night or rest pain.
Alarming symptoms include unexplained weight loss, failure to improve with treatment, severe pain for more than 6 weeks, and night or rest pain.
 Cauda equina syndrome is an emergency; often presents with bowel or bladder symptoms (or both).
Cauda equina syndrome is an emergency; often presents with bowel or bladder symptoms (or both).
 General Considerations
General Considerations
Low back pain remains the number one cause of disability globally and is the second most common cause for primary care visits. The annual prevalence of low back pain is 15–45%. Annual health care spending for low back and neck pain is estimated to be $87.6 billion. Low back pain is the condition associated with the highest years lived with disability. Approximately 80% of episodes of low back pain resolve within 2 weeks and 90% resolve within 6 weeks. The exact cause of the low back pain is often difficult to diagnose; its cause is often multifactorial. There are usually degenerative changes in the lumbar spine involving the disks, facet joints, and vertebral endplates (Modic changes).
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Aggravating factors of flexion and prolonged sitting commonly suggest anterior spine disk problems, while extension pain suggests facet joint, stenosis, or sacroiliac joint problems. Alarming symptoms for back pain caused by cancer include unexplained weight loss, failure to improve with treatment, pain for more than 6 weeks, and pain at night or rest. History of cancer and age older than 50 years are other risk factors for malignancy. Alarming symptoms for infection include fever, rest pain, recent infection (urinary tract infection, cellulitis, pneumonia), or history of immunocompromise or injection drug use. The cauda equina syndrome is suggested by urinary retention or incontinence, saddle anesthesia, decreased anal sphincter tone or fecal incontinence, bilateral lower extremity weakness, and progressive neurologic deficits. Risk factors for back pain due to vertebral fracture include use of corticosteroids, age over 70 years, history of osteoporosis, severe trauma, and presence of a contusion or abrasion. Back pain may also be the presenting symptom in other serious medical problems, including abdominal aortic aneurysm, peptic ulcer disease, kidney stones, or pancreatitis. The patient’s previous response to treatments and the results of risk prediction tools can help guide management.
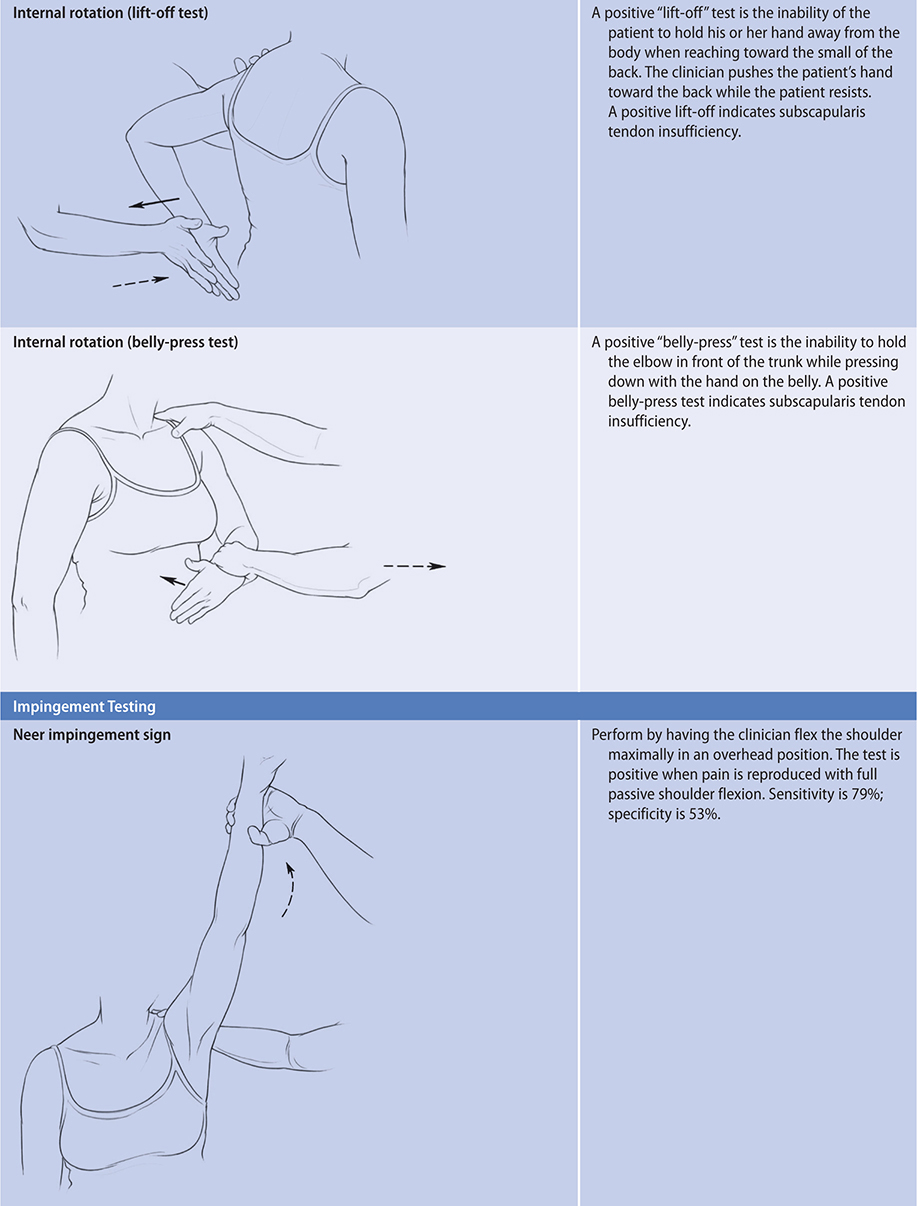
The physical examination can be conducted with the patient in the standing, sitting, supine, and finally prone positions to avoid frequent repositioning of the patient. In the standing position, the patient’s posture can be observed. Commonly encountered spinal asymmetries include scoliosis, thoracic kyphosis, and lumbar hyperlordosis. The active range of motion of the lumbar spine can be assessed while standing. The common directions include flexion, extension, rotation, and lateral bending. The one-leg standing extension test assesses for pain as the patient stands on one leg while extending the spine. A positive test can be caused by pars interarticularis fractures (spondylolysis or spondylolisthesis) or facet joint arthritis.
With the patient sitting, motor strength, reflexes, and sensation can be tested (Table 41–2). The major muscles in the lower extremities are assessed for weakness by eliciting a resisted isometric contraction for about 5 seconds. Comparing the strength bilaterally to detect subtle muscle weakness is important. Similarly, sensory testing to light touch can be checked in specific dermatomes for corresponding nerve root function. Knee (femoral nerve L2–4), ankle (deep peroneal nerve L4–L5), and Babinski (sciatic nerve L5–S1) reflexes can be checked with the patient sitting.
Table 41–2. Neurologic testing of lumbosacral nerve disorders.
In the supine position, the hip should be evaluated for range of motion, particularly internal rotation. The straight leg raise test puts traction and compression forces on the lower lumbar nerve roots.
Finally, in the prone position, the clinician can carefully palpate each vertebral level of the spine and sacroiliac joints for tenderness. A rectal examination is required if the cauda equina syndrome is suspected. Superficial skin tenderness to a light touch over the lumbar spine, overreaction to maneuvers in the regular back examination, low back pain on axial loading of spine in standing, and inconsistency in the straight leg raise test or on the neurologic examination suggest nonorthopedic causes for the pain or malingering.
B. Imaging
In the absence of alarming “red flag” symptoms suggesting infection, malignancy, or cauda equina syndrome, most patients do not need diagnostic imaging, including radiographs, in the first 6 weeks. The Agency for Healthcare Research and Quality guidelines for obtaining lumbar radiographs are summarized in Table 41–3. Most clinicians obtain radiographs for new back pain in patients older than 50 years. If done, radiographs of the lumbar spine should include AP and lateral views. Oblique views can be useful if the neuroforamina or bone lesions need to be visualized. MRI is the method of choice in the evaluation of symptoms not responding to conservative treatment or in the presence of red flags of serious conditions.
Table 41–3. AHRQ criteria for lumbar radiographs in patients with acute low back pain.
Possible fracture
Major trauma
Minor trauma in patients > 50 years of age
Long-term corticosteroid use
Osteoporosis
> 70 years of age
Possible tumor or infection
> 50 years of age
< 20 years of age
History of cancer
Constitutional symptoms
Recent bacterial infection
Injection drug use
Immunosuppression
Supine pain
Nocturnal pain
AHRQ, Agency for Healthcare Research and Quality.
Adapted from Bigos S, Bowyer O, Braen G, et al. Acute Low Back Problems in Adults. Clinical Practice Guideline Quick Reference Guide No. 14. AHCPR Publication No. 95-0643. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services. December 1994.
C. Special Tests
Electromyography or nerve conduction studies may be useful in assessing patients with possible nerve root symptoms lasting longer than 6 weeks; back pain may or may not also be present. These tests are usually not necessary if the diagnosis of radiculopathy is clear.
 Treatment
Treatment
A. Conservative
Nonpharmacologic treatments are key in the management of low back pain. Education alone improves patient satisfaction with recovery and recurrence. Patients require information and reassurance, especially when serious pathology is absent. Discussion must include reviewing safe and effective methods of symptom control as well as how to decrease the risk of recurrence with proper lifting techniques, abdominal wall/core strengthening, weight loss, and smoking cessation. Exercise, psychological therapies (eg, cognitive behavioral therapy), and multidisciplinary rehabilitation have been shown to be modestly effective for acute low back pain (strength of evidence, low). Complementary therapies, such as Tai chi, mindfulness-based stress reduction, and yoga, have shown benefit for chronic low back pain patients.
Physical therapy exercise programs can be tailored to the patient’s symptoms and pathology. A randomized controlled trial demonstrated that individualized physical therapy was clinically more beneficial than advice alone with sustained improvements at 6 months and 12 months. Strengthening and stabilization exercises effectively reduce pain and functional limitation compared with usual care. Heat and cold treatments have not shown any long-term benefits but may be used for symptomatic treatment. The efficacy of transcutaneous electrical nerve stimulation (TENS), back braces, and physical agents is unproven. Spinal manipulation, massage, and acupuncture have limited, low-strength evidence for chronic low back pain. Improvements in posture including chair ergonomics or standing desks, core stability strengthening, physical conditioning, and modifications of activities to decrease physical strain are keys for ongoing management. Radiofrequency denervation of facet joints, sacroiliac joints, or intervertebral disks did not result in clinically important improvement in chronic low back even when combined with a standardized exercise program in randomized controlled trials. A multidisciplinary approach to back pain care is beneficial to address the physical, psychological, and social aspects of low back pain, especially when pain is chronic, avoiding medication if possible.
If medications are needed, NSAIDs are effective in the early treatment of low back pain (see Chapter 20). Acetaminophen and oral corticosteroids are relatively ineffective for chronic low back. There is limited evidence that muscle relaxants provide short-term relief; since these medications have addictive potential, they should be used with care. Muscle relaxants are best used if there is true muscle spasm that is painful rather than simply a protective response. Opioids alleviate pain in the short term, but have the usual side effects and concerns of long-term opioid use (Chapter 5). Treatment of more chronic neuropathic pain with alpha-2-delta ligands (eg, gabapentin), serotonin-norepinephrine reuptake inhibitors (eg, duloxetine), or tricyclic antidepressants (eg, nortriptyline) may be helpful (Chapter 5). Epidural injections may reduce pain in the short term and reduce the need for surgery in some patients within a 1-year period but not longer. Therefore, spinal injections are not recommended for initial care of patients with low back pain without radiculopathy.
B. Surgical
Indications for back surgery include cauda equina syndrome, ongoing morbidity with no response to more than 6 months of conservative treatment, cancer, infection, or severe spinal deformity. Prognosis is improved when there is an anatomic lesion that can be corrected and symptoms are neurologic. Spinal surgery has limitations. Patient selection is very important and the specific surgery recommended should have very clear indications. Patients should understand that surgery can improve their pain but is unlikely to cure it. Surgery is not generally indicated for radiographic abnormalities alone when the patient is relatively asymptomatic. Depending on the surgery performed, possible complications include persistent pain; surgical site pain, especially if bone grafting is needed; infection; neurologic damage; non-union; cutaneous nerve damage; implant failure; deep venous thrombosis; and death.
 When to Refer
When to Refer
• Patients with the cauda equina syndrome.
• Patients with cancer, infection, fracture, or severe spinal deformity.
• Patients who have not responded to conservative treatment.
Barrey CY et al; French Society for Spine Surgery. Chronic low back pain: relevance of a new classification based on the injury pattern. Orthop Traumatol Surg Res. 2019 Apr;105(2):339–46. [PMID: 30792166]
Bydon M et al. Degenerative lumbar spondylolisthesis: definition, natural history, conservative management, and surgical treatment. Neurosurg Clin N Am. 2019 Jul;30(3):299–304. [PMID: 31078230]
Chan AK et al. Summary of guidelines for the treatment of lumbar spondylolisthesis. Neurosurg Clin N Am. 2019 Jul;30(3):353–64. [PMID: 31078236]
Galliker G et al. Low back pain in the emergency department: prevalence of serious spinal pathologies and diagnostic accuracy of red flags—a systematic review. Am J Med. 2020 Jan;133(1):60–72. [PMID: 31278933]
Johnson SM et al. Imaging of acute low back pain. Radiol Clin North Am. 2019 Mar;57(2):397–413. [PMID: 30709477]
Karsy M et al. Surgical versus nonsurgical treatment of lumbar spondylolisthesis. Neurosurg Clin N Am. 2019 Jul;30(3):333–40. [PMID: 31078234]
Tucker HR et al. Harms and benefits of opioids for management of non-surgical acute and chronic low back pain: a systematic review. Br J Sports Med. 2020 Jun;54(11):664. [PMID: 30902816]
Urits I et al. Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Curr Pain Headache Rep. 2019 Mar 11;23(3):23. [PMID: 30854609]
2. Spinal Stenosis
ESSENTIALS OF DIAGNOSIS

 Pain is usually worse with back extension and relieved by sitting.
Pain is usually worse with back extension and relieved by sitting.
 Occurs in older patients.
Occurs in older patients.
 May present with neurogenic claudication symptoms with walking.
May present with neurogenic claudication symptoms with walking.
 General Considerations
General Considerations
OA in the lumbar spine can cause narrowing of the spinal canal. A large disk herniation can also cause stenosis and compression of neural structures or the spinal artery resulting in “claudication” symptoms with ambulation. The condition usually affects patients aged 50 years or older.
 Clinical Findings
Clinical Findings
Patients report pain that worsens with extension. They describe reproducible single or bilateral leg symptoms that are worse after walking several minutes and that are relieved by sitting (“neurogenic claudication”). On examination, patients often exhibit limited extension of the lumbar spine, which may reproduce the symptoms radiating down the legs. A thorough neurovascular examination is recommended (Table 41–2).
 Treatment
Treatment
Exercises, usually flexion-based as demonstrated by a physical therapist, can help relieve symptoms. Physical therapy showed similar results as surgical decompression in a randomized trial, though there was a 57% crossover rate from physical therapy to surgery. Facet joint corticosteroid injections can also reduce pain symptoms. While epidural corticosteroid injections have been shown to provide immediate improvements in pain and function for patients with radiculopathy, the benefits are small and only short term. Consequently, there is limited evidence to recommend epidural corticosteroids for spinal stenosis.
Surgical treatments for spinal stenosis include spinal decompression (widening the spinal canal or laminectomy), nerve root decompression (freeing a single nerve), and spinal fusion (joining the vertebra to eliminate motion and diminish pain from the arthritic joints). However, a Cochrane review showed surgery was not clearly better than nonsurgical treatment and had complication rates of 10–24% compared to 0% for nonoperative treatments. Thus, the role of surgery for spinal stenosis is limited. In one multicenter randomized trial, subgroups initially improved significantly more with surgery than with nonoperative treatment. Variables associated with greater treatment effects included lower baseline disability scores, not smoking, neuroforaminal stenosis, predominant leg pain rather than back pain, not lifting at work, and the presence of a neurologic deficit. However, long-term follow-up of the patients with symptomatic spinal stenosis who received surgery in the multicenter randomized trial showed less benefit of surgery between 4 and 8 years, suggesting that the advantage of surgery for spinal stenosis diminishes over time. A Cochrane review of 24 randomized controlled trials of treatments for lumbar spinal stenosis showed that various surgeries including decompression plus fusion and interspinous process spacers were not superior to conventional spinal decompression surgery alone.
 When to Refer
When to Refer
• If a patient exhibits radicular or claudication symptoms for longer than 12 weeks.
• MRI or CT confirmation of significant, symptomatic spinal stenosis.
• However, surgery has not been shown to have clear benefit over nonsurgical treatment for lumbar spinal stenosis.
Bagley C et al. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res. 2019 Jan 31;8:137. [PMID: 30774933]
Cook CJ et al. Systematic review of diagnostic accuracy of patient history, clinical findings, and physical tests in the diagnosis of lumbar spinal stenosis. Eur Spine J. 2020 Jan;29(1):93–112. [PMID: 31312914]
3. Lumbar Disk Herniation
ESSENTIALS OF DIAGNOSIS

 Pain with back flexion or prolonged sitting.
Pain with back flexion or prolonged sitting.
 Radicular pain into the leg due to compression of neural structures.
Radicular pain into the leg due to compression of neural structures.
 Lower extremity numbness and weakness.
Lower extremity numbness and weakness.
 General Considerations
General Considerations
Lumbar disk herniation is usually due to bending or heavy loading (eg, lifting) with the back in flexion, causing herniation or extrusion of disk contents (nucleus pulposus) into the spinal cord area. However, there may not be an inciting incident. Disk herniations usually occur from degenerative disk disease (dessication of the annulus fibrosis) in patients between 30 and 50 years old. The L5–S1 disk is affected in 90% of cases. Compression of neural structures, such as the sciatic nerve, causes radicular pain. Severe compression of the spinal cord can cause the cauda equina syndrome, a surgical emergency.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Discogenic pain typically is localized in the low back at the level of the affected disk and is worse with activity. “Sciatica” causes electric shock-like pain radiating down the posterior aspect of the leg often to below the knee. Symptoms usually worsen with back flexion such as bending or sitting for long periods (eg, driving). A significant disk herniation can cause numbness and weakness, including weakness of plantar flexion of the foot (L5/S1) or dorsiflexion of the toes (L4/L5). The cauda equina syndrome should be ruled out if the patient complains of perianal numbness or bowel or bladder incontinence.
B. Imaging
Plain radiographs are helpful to assess spinal alignment (scoliosis, lordosis), disk space narrowing, and OA changes. MRI is the best method to assess the level and morphology of the herniation and is recommended if surgery is planned.
 Treatment
Treatment
For an acute exacerbation of pain symptoms, bed rest is appropriate for up to 48 hours. Otherwise, first-line treatments include modified activities; NSAIDs and other analgesics; and physical therapy, including core stabilization and McKenzie back exercises. Following nonsurgical treatment for a lumbar disk for over 1 year, the incidence of low back pain recurrence is at least 40% and is predicted by longer time to initial resolution of pain. In a randomized trial, oral prednisone caused a modest improvement in function at 3 weeks, but there was no significant improvement in pain in patients with acute radiculopathy who were monitored for 1 year. The initial dose for oral prednisone is approximately 1 mg/kg once daily with tapering doses over 10–15 days. Analgesics for neuropathic pain, such as the calcium channel alpha-2-delta ligands (ie, gabapentin, pregabalin) or tricyclic antidepressants, may be helpful (see Chapter 5). Epidural and transforaminal corticosteroid injections can be beneficial. A systematic review demonstrated strong evidence that fluoroscopic-guided epidural injections gave short-term benefit (less than 6 months) in acute radicular pain for individuals. However, epidural injections have not shown any change in long-term surgery rates for disk herniations.
The severity of pain and disability as well as failure of conservative therapy were the most important reasons for surgery. A large trial has shown that patients who underwent surgery for a lumbar disk herniation achieved greater improvement than conservatively treated patients in all primary and secondary outcomes except return to work status after 4-year follow-up. Patients with sequestered fragments, symptom duration greater than 6 months, higher levels of low back pain, or who were neither working nor disabled at baseline showed greater surgical treatment effects. Microdiskectomy is the standard method of treatment with a low rate of complications and satisfactory results in over 90% in the largest series. Minimally invasive percutaneous endoscopic spine surgery uses an endoscope to remove fragments of disk herniation (interlaminar or transforaminal approaches) under local anesthesia for the treatment of primary and recurrent disk disease. The most commonly reported complications of endoscopic lumbar surgery include dural tear, infection, and epidural hematoma. Percutaneous endoscopic diskectomy has promise, though there is lack of randomized controlled trials comparing it with open microdiskectomy. Recurrent disk herniations are treated with decompression surgeries and spinal fusion surgeries. Disk replacement surgery has shown benefits in short-term pain relief, disability, and quality of life compared with spine fusion surgery.
 When to Refer
When to Refer
• Cauda equina syndrome.
• Progressive worsening of neurologic symptoms.
• Loss of motor function (sensory losses can be followed in the outpatient clinic).
Butler AJ et al. Endoscopic lumbar surgery: the state of the art in 2019. Neurospine. 2019 Mar;16(1):15–23. [PMID: 30943703]
Gadjradj PS et al. Management of symptomatic lumbar disk herniation: an international perspective. Spine (Phila Pa 1976). 2017 Dec 1;42(23):1826–34. [PMID: 28632645]
Lee JS et al. Comparison of percutaneous endoscopic lumbar diskectomy and open lumbar microdiskectomy for recurrent lumbar disk herniation. J Neurol Surg A Cent Eur Neurosurg. 2018 Nov;79(6):447–52. [PMID: 29241269]
4. Neck Pain
ESSENTIALS OF DIAGNOSIS

 Chronic neck pain is mostly caused by degenerative joint disease; whiplash often follows a traumatic neck injury.
Chronic neck pain is mostly caused by degenerative joint disease; whiplash often follows a traumatic neck injury.
 Poor posture is often a factor for persistent neck pain.
Poor posture is often a factor for persistent neck pain.
 General Considerations
General Considerations
Most neck pain, especially in older patients, is due to mechanical degeneration involving the cervical disks, facet joints, and ligamentous structures and may occur in the setting of degenerative changes at other sites. Pain can also come from the supporting neck musculature, which often acts to protect the underlying neck structures. Posture is a very important factor, especially in younger patients. Many work-related neck symptoms are due to poor posture and repetitive motions over time. Acute injuries can also occur secondary to trauma. Whiplash occurs from rapid flexion and extension of the neck and affects 15–40% of people in motor vehicle accidents; chronic pain develops in 5–7%. Neck fractures are serious traumatic injuries acutely and can lead to OA in the long term. Ultimately, many degenerative conditions of the neck result in cervical canal stenosis or neural foraminal stenosis, sometimes affecting underlying neural structures.
Cervical radiculopathy can cause neurologic symptoms in the upper extremities usually involving the C5–C7 disks. Patients with neck pain may report associated headaches and shoulder pain. Both peripheral nerve entrapment and cervical radiculopathy, known as a “double crush” injury, may develop. Thoracic outlet syndrome, in which there is mechanical compression of the brachial plexus and neurovascular structures with overhead positioning of the arm, should be considered in the differential diagnosis of neck pain. Other causes of neck pain include rheumatoid arthritis, fibromyalgia, osteomyelitis, neoplasms, polymyalgia rheumatica, compression fractures, pain referred from visceral structures (eg, angina), and functional disorders. Amyotrophic lateral sclerosis, multiple sclerosis, syringomyelia, spinal cord tumors, and Parsonage-Turner syndrome can mimic myelopathy from cervical arthritis.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
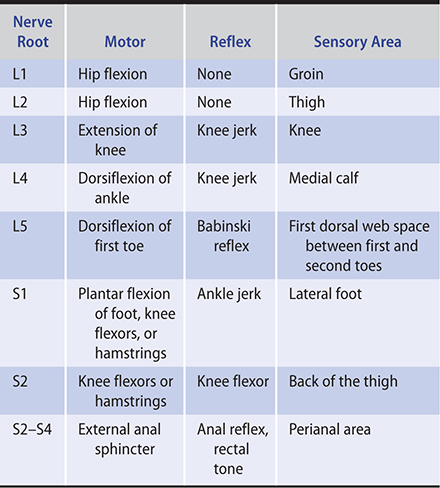
Neck pain may be limited to the posterior region or, depending on the level of the symptomatic joint, may radiate segmentally to the occiput, anterior chest, shoulder girdle, arm, forearm, and hand. It may be intensified by active or passive neck motions. The general distribution of pain and paresthesias corresponds roughly to the involved dermatome in the upper extremity.
The patient’s posture should be assessed, checking for shoulder rolled forward or head forward posture as well as scoliosis in the thoracolumbar spine. Patients with discogenic neck pain often complain of pain with flexion, which causes cervical disks to herniate posteriorly. Extension of the neck usually affects the neural foraminal and facet joints of the neck. Rotation and lateral flexion of the cervical spine should be measured both to the left and the right. Limitation of cervical movements is the most common objective finding.
A detailed neurovascular examination of the upper extremities should be performed, including sensory input to light touch and temperature; motor strength testing, especially the hand intrinsic muscles (thumb extension strength [C6], opponens strength [thumb to pinky] [C7], and finger abductors and adductors strength [C8–T1]); and upper extremity reflexes (biceps, triceps, brachioradialis). True cervical radiculopathy symptoms should match an expected dermatomal or myotomal distribution. The Spurling test involves asking the patient to rotate and extend the neck to one side (Table 41–4). The clinician can apply a gentle axial load to the neck. Reproduction of the cervical radiculopathy symptoms is a positive sign of nerve root compression. Palpation of the neck is best performed with the patient in the supine position where the clinician can palpate each level of the cervical spine with the muscles of the neck relaxed.
Table 41–4. Spine: neck examination.
B. Imaging and Special Tests
Radiographs of the cervical spine include the AP and lateral view of the cervical spine. The odontoid view is usually added to rule out traumatic fractures and congenital abnormalities. Oblique views of the cervical spine can provide further information about arthritis changes and assess the neural foramina for narrowing. Plain radiographs can be completely normal in patients who have suffered an acute cervical strain. Comparative reduction in height of the involved disk space and osteophytes are frequent findings when there are degenerative changes in the cervical spine. Loss of cervical lordosis is commonly seen but is nonspecific.
MRI is the best method to assess the cervical spine since the soft tissue structures (such as the disks, spinal cord, and nerve roots) can be evaluated. If the patient has signs of cervical radiculopathy with motor weakness, these more sensitive imaging modalities should be obtained urgently. CT scanning is the most useful method if bony abnormalities, such as fractures, are suspected.
EMG is useful in order to differentiate peripheral nerve entrapment syndromes from cervical radiculopathy. However, sensitivity of electrodiagnostic testing for cervical radiculopathy ranges from only 50% to 71%, so a negative test does not rule out nerve root problems.
 Treatment
Treatment
In the absence of trauma or evidence of infection, malignancy, neurologic findings, or systemic inflammation, the patient can be treated conservatively. More frequent observation of individuals in whom very severe symptoms are present early on after an injury is recommended because high pain-related disability is a predictor of poor outcome at 1 year even if individuals decline care. Ergonomics should be assessed at work and home. A course of neck stretching, strengthening, and postural exercises in physical therapy have demonstrated benefit in relieving symptoms. A soft cervical collar can be useful for short-term use (up to 1–2 weeks) in acute neck injuries. Chiropractic manual manipulation and mobilization can provide short-term benefit for mechanical neck pain. Although the rate of complications is low (5–10/million manipulations), care should be taken whenever there are neurologic symptoms present. Specific patients may respond to use of home cervical traction. NSAIDs are commonly used and opioids may be needed in cases of severe neck pain. Muscle relaxants (eg, cyclobenzaprine 5–10 mg orally three times daily) can be used short term if there is muscle spasm or as a sedative to aid in sleeping. Acute radicular symptoms can be treated with neuropathic medications (eg, gabapentin 300–1200 mg orally three times daily), and a short course of oral prednisone (5–10 days) can be considered (starting at 1 mg/kg). Cervical foraminal or facet joint injections can also reduce symptoms. Surgeries are successful in reducing neurologic symptoms in 80–90% of cases, but are still considered as treatments of last resort. Common surgeries for cervical degenerative disk disease include anterior cervical diskectomy with fusion and cervical disk arthroplasty. A meta-analysis of 18 randomized controlled trials showed that cervical disk arthroplasty was superior to anterior diskectomy and fusion for the treatment of symptomatic cervical disk disease, with better success and less reoperation rates.
 When to Refer
When to Refer
• Patients with severe symptoms with motor weakness.
• Surgical decompression surgery if the symptoms are severe and there is identifiable, correctable pathology.
Cohen SP et al. Advances in the diagnosis and management of neck pain. BMJ. 2017 Aug 14;358:j3221. [PMID: 28807894]
Martel JW et al. Evaluation and management of neck and back pain. Semin Neurol. 2019 Feb;39(1):41–52. [PMID: 30743291]
Peng B et al. Cervical discs as a source of neck pain. An analysis of the evidence. Pain Med. 2019 Mar 1;20(3):446–55. [PMID: 30520967]
Sterling M. Best evidence rehabilitation for chronic pain part 4: neck pain. J Clin Med. 2019 Aug 15;8(8):E1219. [PMID: 31443149]
Strudwick K et al. Review article: best practice management of neck pain in the emergency department (part 6 of the musculoskeletal injuries rapid review series). Emerg Med Australas. 2018 Dec;30(6):754–72. [PMID: 30168261]
UPPER EXTREMITY
1. Lateral & Medial Epicondylosis
ESSENTIALS OF DIAGNOSIS

 Tenderness over the lateral or medial epicondyle.
Tenderness over the lateral or medial epicondyle.
 Diagnosis of tendinopathy is confirmed by pain with resisted strength testing and passive stretching of the affected tendon and muscle unit.
Diagnosis of tendinopathy is confirmed by pain with resisted strength testing and passive stretching of the affected tendon and muscle unit.
 Physical therapy and activity modification are more successful than anti-inflammatory treatments.
Physical therapy and activity modification are more successful than anti-inflammatory treatments.
 General Considerations
General Considerations
Tendinopathies involving the wrist extensors, flexors, and pronators are very common complaints. The underlying mechanism is chronic repetitive overuse causing microtrauma at the tendon insertion, although acute injuries can occur as well if the tendon is strained due to excessive loading. The traditional term “epicondylitis” is a misnomer because histologically tendinosis or degeneration in the tendon is seen rather than acute inflammation. Therefore, these entities should be referred to as “tendinopathy” or “tendinosis.” Lateral epicondylosis involves the wrist extensors, especially the extensor carpi radialis brevis. This is usually caused be lifting with the wrist and the elbow extended. Medial epicondylosis involves the wrist flexors and most commonly the pronator teres tendon. Ulnar neuropathy and cervical radiculopathy should be considered in the differential diagnosis.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
For lateral epicondylosis, the patient describes pain with the arm and wrist extended. For example, common complaints include pain while shaking hands, lifting objects, using a computer mouse, or hitting a backhand in tennis (“tennis elbow”). Medial epicondylosis presents with pain during motions in which the arm is repetitively pronated or the wrist is flexed. This is also known as “golfer’s elbow” due to the motion of turning the hands over during the golf swing. For either, tenderness directly over the epicondyle is present, especially over the posterior aspect where the tendon insertion occurs. The proximal tendon and musculotendinous junction can also be sore. To confirm that the pain is due to tendinopathy, pain can be reproduced over the epicondyle with resisted wrist extension and third digit extension for lateral epicondylosis and resisted wrist pronation and wrist flexion for medial epicondylosis. The pain is also often reproduced with passive stretching of the affected muscle groups, which can be performed with the arm in extension. It is useful to check the ulnar nerve (located in a groove at the posteromedial elbow) for tenderness as well as to perform a Spurling test for cervical radiculopathy.
B. Imaging
Radiographs are often normal, although a small traction spur may be present in chronic cases (enthesopathy). Diagnostic investigations are usually unnecessary, unless the patient does not improve after up to 3 months of conservative treatment. At that point, a patient who demonstrates significant disability due to the pain should be assessed with an MRI or ultrasound. Ultrasound and MRI can visualize the tendon and confirm tendinosis or tears.
 Treatment
Treatment
Treatment is usually conservative, including patient education regarding activity modification and management of symptoms. Ice and NSAIDs can help with pain. The mainstay of treatment is physical therapy exercises. The most important steps are to begin a good stretching program followed by strengthening exercises, particularly eccentric ones. Counterforce elbow braces might provide some symptomatic relief, although there is no published evidence to support their use. If the patient has severe or long-standing symptoms, injections can be considered. A randomized trial showed improvement with corticosteroid injection at 1 month as well as evidence of decreased tendon thickness and Doppler changes but no improvement at 3 months. Percutaneous needle tenotomy showed some positive results as an alternative to surgery but lacks demonstrated efficacy in a randomized control study. Evidence on platelet-rich plasma (PRP) injections continues to accumulate and it is becoming more commonly used in practice. Reviews suggest that PRP and autologous blood injections both have positive benefits in lateral epicondylitis. In a randomized controlled trial comparing PRP injection to controls (n = 119), the PRP-treated patients reported 55.1% improvement in their pain scores at 12 weeks compared to 47.4% in the control patients (P = 0.163). More significant improvement was seen at 24 weeks; 71.5% improvement in the pain scores in the PRP-treated patients compared to 56.1% in the control patients (P = 0.019). (A 25% improvement of pain symptoms was considered to be clinically significant.) However, the varied methods of PRP preparations and varied post-injection recommendations for rest and physiotherapy make interpretation of various study results difficult to summarize. Compared to ultrasound therapy, extracorporeal shock wave therapy has shown better efficacy for pain relief (as measured with visual analog scales) and better grip strength. However, it is used less commonly than injection treatments and is still considered second-line therapy.
 When to Refer
When to Refer
Patients not responding to 6 months of conservative treatment should be referred for an injection procedure (PRP or tenotomy), surgical debridement, or repair of the tendon.
Lai WC et al. Chronic lateral epicondylitis: challenges and solutions. Open Access J Sports Med. 2018 Oct 30;9:243–51. [PMID: 30464656]
Lenoir H et al. Management of lateral epicondylitis. Orthop Traumatol Surg Res. 2019 Dec;105(8S):S241–6. [PMID: 31543413]
Moradi A et al. Clinical outcomes of open versus arthroscopic surgery for lateral epicondylitis, evidence from a systematic review. Arch Bone Jt Surg. 2019 Mar;7(2):91–104. [PMID: 31211187]
Shergill R et al. Ultrasound-guided interventions in lateral epicondylitis. J Clin Rheumatol. 2019 Apr;25(3):e27–34. [PMID: 30074911]
Yan C et al. A comparative study of the efficacy of ultrasonics and extracorporeal shock wave in the treatment of tennis elbow: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2019 Aug 6;14(1):248. [PMID: 31387611]
2. Carpal Tunnel Syndrome
ESSENTIALS OF DIAGNOSIS

 Pain, burning, and tingling in the distribution of the median nerve.
Pain, burning, and tingling in the distribution of the median nerve.
 Initially, most bothersome during sleep.
Initially, most bothersome during sleep.
 Late weakness or atrophy of the thenar eminence.
Late weakness or atrophy of the thenar eminence.
 Can be caused by repetitive wrist activities.
Can be caused by repetitive wrist activities.
 Commonly seen during pregnancy and in patients with diabetes mellitus or rheumatoid arthritis.
Commonly seen during pregnancy and in patients with diabetes mellitus or rheumatoid arthritis.
 General Considerations
General Considerations
An entrapment neuropathy, carpal tunnel syndrome is a painful disorder caused by compression of the median nerve between the carpal ligament and other structures within the carpal tunnel. The contents of the tunnel can be compressed by synovitis of the tendon sheaths or carpal joints, recent or malhealed fractures, tumors, tissue infiltration, and occasionally congenital syndromes (eg, mucopolysaccharidoses). The disorder may occur in fluid retention of pregnancy, in individuals with a history of repetitive use of the hands, or following injuries of the wrists. Carpal tunnel syndrome can also be a feature of many systemic diseases, such as rheumatoid arthritis and other rheumatic disorders (inflammatory tenosynovitis), myxedema, amyloidosis, sarcoidosis, leukemia, acromegaly, and hyperparathyroidism. There is a familial type of carpal tunnel syndrome in which no etiologic factor can be identified.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The initial symptoms are pain, burning, and tingling in the distribution of the median nerve (the palmar surfaces of the thumb, the index and long fingers, and the radial half of the ring finger). Aching pain may radiate proximally into the forearm and occasionally proximally to the shoulder and over the neck and chest. Pain is exacerbated by manual activity, particularly by extremes of volar flexion or dorsiflexion of the wrist. It is most bothersome at night. Impairment of sensation in the median nerve distribution may or may not be demonstrable. Subtle disparity between the affected and opposite sides can be shown by testing for two-point discrimination or by requiring the patient to identify different textures of cloth by rubbing them between the tips of the thumb and the index finger. A Tinel or Phalen sign may be positive. A Tinel sign is tingling or shock-like pain on volar wrist percussion. The Phalen sign is pain or paresthesia in the distribution of the median nerve when the patient flexes both wrists to 90 degrees for 60 seconds. The carpal compression test, in which numbness and tingling are induced by the direct application of pressure over the carpal tunnel, may be more sensitive and specific than the Tinel and Phalen tests. Muscle weakness or atrophy, especially of the thenar eminence, can appear later than sensory disturbances as compression of the nerve worsens.
B. Imaging
Ultrasound can demonstrate flattening of the median nerve beneath the flexor retinaculum. Sensitivity of ultrasound for carpal tunnel syndrome is variable but estimated between 54% and 98%.
C. Special Tests
Electromyography and nerve conduction studies show evidence of sensory conduction delay before motor delay, which can occur in severe cases. Electrodiagnosis can provide information on focal median mononeuropathy at the wrist and can classify carpal tunnel syndrome from mild to severe.
 Treatment
Treatment
Treatment is directed toward relief of pressure on the median nerve. When a causative lesion is discovered, it should be treated appropriately. Otherwise, patients in whom carpal tunnel syndrome is suspected should modify their hand activities. The affected wrist can be splinted in the neutral position for up to 3 months, but a series of Cochrane reviews show limited evidence for splinting, exercises, and ergonomic positioning. Moderate evidence supported benefit from several physical therapy and electrophysical modalities (eg, ultrasound therapy and radial extracorporeal shockwave therapy). These modalities provided short-term and mid-term relief of carpal tunnel syndrome symptoms in different studies. Oral corticosteroids or NSAIDs have also shown benefit for carpal tunnel syndrome. Methylprednisolone injections were found to have more effect at 10 weeks than placebo, but the benefits diminished by 1 year.
Compared to trigger finger management, which usually includes injections, as many as 71% of patients with carpal tunnel directly undergo surgery without first getting injections. There is strong evidence that a steroid injection to the carpal tunnel is more effective in the short term than surgery. A randomized, controlled trial showed both corticosteroid injection and surgery resolved symptoms but only decompressive surgery led to resolution of neurophysiologic changes. Carpal tunnel release surgery can be beneficial if the patient has a positive electrodiagnostic test, at least moderate symptoms, high clinical probability, unsuccessful nonoperative treatment, and symptoms lasting longer than 12 months. Surgery can be done with an open approach or endoscopically, both yielding similar good improvements.
 When to Refer
When to Refer
• If symptoms persist more than 3 months despite conservative treatment, including the use of a wrist splint.
• If thenar muscle (eg, abductor pollicis brevis) weakness or atrophy develops.
Huisstede BM et al. Carpal tunnel syndrome: effectiveness of physical therapy and electrophysical modalities. An updated systematic review of randomized controlled trials. Arch Phys Med Rehabil. 2018 Aug;99(8):1623–34. [PMID: 28942118]
Huisstede BM et al. Effectiveness of surgical and postsurgical interventions for carpal tunnel syndrome—a systematic review. Arch Phys Med Rehabil. 2018 Aug;99(8):1660–80. [PMID: 28577858]
Petrover D et al. Ultrasound-guided surgery for carpal tunnel syndrome: a new interventional procedure. Semin Intervent Radiol. 2018 Oct;35(4):248–54. [PMID: 30402007]
Urits I et al. Recent advances in the understanding and management of carpal tunnel syndrome: a comprehensive review. Curr Pain Headache Rep. 2019 Aug 1;23(10):70. [PMID: 31372847]
Wang L. Guiding treatment for carpal tunnel syndrome. Phys Med Rehabil Clin N Am. 2018 Nov;29(4):751–60. [PMID: 30293628]
3. Dupuytren Contracture
ESSENTIALS OF DIAGNOSIS

 Benign fibrosing disorder of the palmar fascia.
Benign fibrosing disorder of the palmar fascia.
 Contracture of one or more fingers can lead to limited hand function.
Contracture of one or more fingers can lead to limited hand function.
 General Considerations
General Considerations
This relatively common disorder is characterized by hyperplasia of the palmar fascia and related structures, with nodule formation and contracture of the palmar fascia. The cause is unknown, but the condition has a genetic predisposition and occurs primarily in white men over 50 years of age, particularly in those of Celtic descent. The incidence is higher among alcoholic patients and those with chronic systemic disorders (especially cirrhosis). It is also associated with systemic fibrosing syndrome, which includes plantar fibromatosis (10% of patients), Peyronie disease (1–2%), mediastinal and retroperitoneal fibrosis, and Riedel struma. The onset may be acute, but slowly progressive chronic disease is more common.
 Clinical Findings
Clinical Findings
Dupuytren contracture manifests itself by nodular or cord-like thickening of one or both hands, with the fourth and fifth fingers most commonly affected. The patient may complain of tightness of the involved digits, with inability to satisfactorily extend the fingers, and on occasion there is tenderness. The resulting cosmetic problems may be unappealing, but in general the contracture is well tolerated since it exaggerates the normal position of function of the hand.
 Treatment
Treatment
The literature is still limited to direct the best option for Dupuytren contracture. Corticosteroid injection with a percutaneous needle aponeurotomy, collagenase Clostridium histolyticum injections, and open fasciectomy are common treatment options. If the palmar nodule is growing rapidly, injections of triamcinolone or collagenase into the nodule may be of benefit; the injection of collagenase C histolyticum lyses collagen, thereby disrupting the contracted cords. Surgical options include open fasciectomy, partial fasciectomy, or percutaneous needle aponeurotomy and are indicated in patients with significant flexion contractures. A multicenter study showed that collagenase injection and limited fasciectomy had similar improvements with contractures at the metacarpophalangeal joints, while surgery had better results for contractures involving the proximal interphalangeal joints. Splinting after surgery is beneficial. Recurrence is possible after surgery with more adverse events compared to nonoperative treatments. Compared to placebo, tamoxifen therapy produced moderate evidence of improvement before or after a fasciectomy.
 When to Refer
When to Refer
Referral can be considered when one or more digits are affected by severe contractures, which interfere with everyday activities and result in functional limitations.
Huisstede BM et al. Effectiveness of conservative, surgical, and postsurgical interventions for trigger finger, Dupuytren disease, and De Quervain disease: a systematic review. Arch Phys Med Rehabil. 2018 Aug;99(8):1635–49. [PMID: 28860097]
Sanjuan-Cervero R. Current role of the collagenase Clostridium histolyticum in Dupuytren’s disease treatment. Ir J Med Sci. 2020 May;189(2):529–34. [PMID: 31713028]
Soreide E et al. Treatment of Dupuytren’s contracture: a systematic review. Bone Joint J. 2018 Sep;100-B(9):1138–45. [PMID: 30168768]
4. Bursitis
ESSENTIALS OF DIAGNOSIS

 Often occurs around bony prominences where it is important to reduce friction.
Often occurs around bony prominences where it is important to reduce friction.
 Typically presents with local swelling that is painful acutely.
Typically presents with local swelling that is painful acutely.
 Septic bursitis can present without fever or systemic signs.
Septic bursitis can present without fever or systemic signs.
 General Considerations
General Considerations
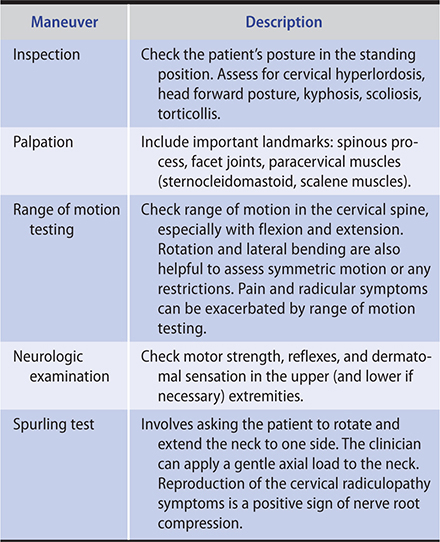
Inflammation of bursae—the synovium-like cellular membranes overlying bony prominences—may be secondary to trauma, infection, or arthritic conditions such as gout, rheumatoid arthritis, or OA. Bursitis can result from infection. The two common sites are the olecranon (Figure 41–1) and prepatellar bursae; however, others include subdeltoid, ischial, trochanteric, and semimembranosus-gastrocnemius (Baker cyst) bursae. The bursitis can be septic. Aseptic bursitis is usually afebrile.

Figure 41–1. Chronic aseptic olecranon bursitis without erythema or tenderness. (Used, with permission, from Richard P. Usatine, MD, in Usatine RP, Smith MA, Mayeaux EJ Jr, Chumley H. The Color Atlas of Family Medicine, 2nd ed. McGraw-Hill, 2013.)
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Bursitis presents with focal tenderness and swelling and is less likely to affect range of motion of the adjacent joint. Olecranon or prepatellar bursitis, for example, causes an oval (or, if chronic, bulbous) swelling at the tip of the elbow or knee and does not affect joint motion. Tenderness, erythema and warmth, cellulitis, a report of trauma, and evidence of a skin lesion are more common in septic bursitis but can be present in aseptic bursitis as well. Patients with septic bursitis can be febrile but the absence of fever does not exclude infection; one-third of those with septic olecranon bursitis are afebrile. A bursa can also become symptomatic when it ruptures. This is particularly true for Baker cyst, the rupture of which can cause calf pain and swelling that mimic thrombophlebitis.
B. Imaging
Imaging is unnecessary unless there is concern for osteomyelitis, trauma, or other underlying pathology. Ruptured Baker cysts are imaged easily by sonography or MRI. It may be important to exclude a deep venous thrombosis, which can be mimicked by a ruptured Baker cyst.
C. Special Tests
Acute swelling and redness at a bursal site call for aspiration to rule out infection especially if the patient is either febrile (temperature more than 37.8°C) or has prebursal warmth (temperature difference greater than 2.2°C) or both. A bursal fluid white blood cell count of greater than 1000/mcL indicates inflammation from infection, rheumatoid arthritis, or gout. The bursal fluid of septic bursitis characteristically contains a purulent aspirate, fluid-to-serum glucose ratio less than 50%, white blood cell count more than 3000 cells/mcL, polymorphonuclear cells more than 50%, and a positive Gram stain for bacteria. Most cases are caused by Staphylococcus aureus; the Gram stain is positive in two-thirds.
 Treatment
Treatment
In general, aspiration and corticosteroid injections in mild, nonseptic bursitis should be avoided to reduce complications of iatrogenic infection and skin atrophy. Bursitis caused by trauma responds to local heat, rest, NSAIDs, and local corticosteroid injections. Repetitive minor trauma to the olecranon bursa should be eliminated by avoiding resting the elbow on a hard surface or by wearing an elbow pad. For chronic aseptic bursitis or when there are athletic or occupational demands, aspiration with intrabursal steroid injection can be performed. Ultrasound-guided aspiration and injection can improve the accuracy of the procedures. Treatment of a ruptured Baker cyst includes rest, leg elevation, and possibly injection of triamcinolone, 20–40 mg into the knee anteriorly (the knee compartment communicates with the cyst).
Treatment for septic bursitis involves incision and drainage and antibiotics usually delivered intravenously, especially against S aureus.
 When to Refer
When to Refer
• Surgical removal of the bursa is indicated only for cases in which infections occur.
• Elective surgical removal can be considered for persistent symptoms affecting activities of daily living.
Khodaee M. Common superficial bursitis. Am Fam Physician. 2017 Feb 15;95(4):224–31. [PMID: 28290630]
Raas C et al. Treatment and outcome with traumatic lesions of the olecranon and prepatellar bursa: a literature review apropos a retrospective analysis including 552 cases. Arch Orthop Trauma Surg. 2017 Jun;137(6):823–7. [PMID: 28447166]
HIP
1. Hip Fractures
ESSENTIALS OF DIAGNOSIS

 Internal rotation of the hip is the best provocative diagnostic maneuver.
Internal rotation of the hip is the best provocative diagnostic maneuver.
 Hip fractures should be surgically repaired as soon as possible (within 24 hours).
Hip fractures should be surgically repaired as soon as possible (within 24 hours).
 Delayed treatment of hip fractures in older adults leads to increased complications and mortality.
Delayed treatment of hip fractures in older adults leads to increased complications and mortality.
 General Considerations
General Considerations
Approximately 4% of the 7.9 million fractures that occur each year in the United States are hip fractures. There is a high mortality rate among older adult patients following hip fracture, with death occurring in 8–9% within 30 days and in approximately 25–30% within 1 year. Osteoporosis, female sex, height greater than 5-feet 8-inches, and age over 50 years are risk factors for hip fracture. Hip fractures usually occur after a fall. High-velocity trauma is needed in younger patients. Stress fractures can occur in athletes or individuals with poor bone mineral density following repetitive loading activities.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Patients typically report pain in the groin, though pain radiating to the lateral hip, buttock, or knee can also commonly occur. If a displaced fracture is present, the patient will not be able to bear weight and the leg may be externally rotated. Gentle logrolling of the leg with the patient supine helps rule out a fracture. Examination of the hip demonstrates pain with deep palpation in the area of the femoral triangle (similar to palpating the femoral artery). Provided the patient can tolerate it, the clinician can, with the patient supine, flex the hip to 90 degrees with the knee flexed to 90 degrees. The leg can then be internally and externally rotated to assess the range of motion on both sides. Pain with internal rotation of the hip is the most sensitive test to identify intra-articular hip pathology. Hip flexion, extension, abduction, and adduction strength can be tested.
Patients with hip stress fractures have less pain on physical examination than described previously but typically have pain with weight bearing. The Trendelenburg test can be performed to examine for weakness or instability of the hip abductors, primarily the gluteus medius muscle; the patient balances first on one leg, raising the non-standing knee toward the chest. The clinician can stand behind the patient and observe for dropping of the pelvis and buttock on the non-stance side. Another functional test is asking the patient to hop or jump during the examination. If the patient has a compatible clinical history of pain and is unable or unwilling to hop, then a stress fracture should be ruled out. The back should be carefully examined in patients with hip complaints, including examining for signs of sciatica.
Following displaced hip fractures, delay of operative intervention leads to an increased risk of perioperative morbidity and mortality. A thorough medical evaluation and treatment should be done to maximize the patient’s ability to undergo operative intervention. A patient who was unable to get up after a fall may have been immobile for hours or even days. Her clinician must exclude rhabdomyolysis, hypothermia, deep venous thrombosis, pulmonary embolism, and other possible sequelae of prolonged immobilization.
B. Imaging
Useful radiographic imaging of the hip includes AP views of the pelvis and bilateral hips and frog-leg-lateral views of the painful hip. A CT scan or MRI may be necessary to identify the hip fracture pattern or to exclude non-displaced fractures. Hip fractures are generally described by location, including femoral neck, intertrochanteric, or subtrochanteric.
 Treatment
Treatment
Almost all patients with a hip fracture will require surgery and may need to be admitted to the hospital for pain control while they await surgery. Surgery is recommended within the first 24 hours because studies have shown that delaying surgery 48 hours results in at least twice the rate of major and minor medical complications, including pneumonia, pressure injuries (formerly pressure ulcers), and deep venous thrombosis. High-volume centers have multidisciplinary teams (including orthopedic surgeons, internists, social workers, and specialized physical therapists) to comanage these patients, which improves perioperative medical care and expedites preoperative evaluation leading to reduced costs.
Stress fractures in active patients require a period of protected weight bearing and a gradual return to activities, although it may take 4–6 months before a return to normal activities. Femoral neck fractures are commonly treated with hemiarthroplasty or total hip replacement. This allows the patient to begin weight bearing immediately postoperatively. Peritrochanteric hip fractures are treated with open reduction internal fixation, where plate and screw construct or intramedullary devices are used. The choice of implant will depend on the fracture pattern. Since fracture fixation requires the fracture to proceed to union, the patient may need to have protected weight bearing during the early postoperative period. Dislocation, periprosthetic fracture, and avascular necrosis of the hip are common complications after surgery. Patients should be mobilized as soon as possible postoperatively to avoid pulmonary complications and pressure injuries. Supervised physical therapy and rehabilitation are important for the patient to regain as much function as possible. Unfortunately, most patients following hip fractures will lose some degree of independence. Patients with hip fracture surgery when compared with elective total hip replacement have been shown to have higher risk of in-hospital mortality.
 Prevention
Prevention
Bone density screening can identify patients at risk for osteopenia or osteoporosis, and treatment can be planned accordingly. There is strong evidence that bisphosphonates, denosumab, and teriparatide reduce fractures compared with placebo, with relative risk reductions of 0.60–0.80 for nonvertebral fractures. There is an increase in atypical femoral fractures with bisphosphonate use (relative risk 1.7), especially in patients of an Asian race in North America, patients with femoral bowing, and patients who had used glucocorticoids. Consensus is that there is benefit in using bisphosphonates, particularly during years 3–5 of therapy, with considerations for drug holidays. Nutrition and bone health (bone densitometry, serum calcium and 25-OH vitamin D levels) should be reviewed with the patient (see Chapter 26). However, there is no evidence that increasing calcium intake prevents hip fractures. For patients with decreased mobility, systemic anticoagulation should be considered to avoid deep venous thrombosis (see Table 14–14). Fall prevention exercise programs are available for older adult patients at risk for falls and hip fractures. Hip protectors are uncomfortable and have less use in preventing fractures.
Table 41–5. Differential diagnosis of knee pain.
Mechanical dysfunction or disruption
Internal derangement of the knee: injury to the menisci or ligaments
Degenerative changes caused by osteoarthritis
Dynamic dysfunction or misalignment of the patella
Fracture as a result of trauma
Intra-articular inflammation or increased pressure
Internal derangement of the knee: injury to the menisci or ligaments
Inflammation or infection of the knee joint
Ruptured popliteal (Baker) cyst
Peri-articular inflammation
Internal derangement of the knee: injury to the menisci or ligaments
Prepatellar or anserine bursitis
Ligamentous sprain
 When to Refer
When to Refer
• All patients in whom hip fracture is suspected.
• All patients with hip fracture or in whom the diagnosis is uncertain after radiographs.
Black DM et al. Atypical femur fractures: review of epidemiology, relationship to bisphosphonates, prevention, and clinical management. Endocr Rev. 2019 Apr 1;40(2):333–68. [PMID: 30169557]
Dreizin D et al. Imaging acetabular fractures. Radiol Clin North Am. 2019 Jul;57(4):823–41. [PMID: 31076035]
Guyen O. Hemiarthroplasty or total hip arthroplasty in recent femoral neck fractures? Orthop Traumatol Surg Res. 2019 Feb;105(1S):S95–101. [PMID: 30449680]
Sobolev B et al; Canadian Collaborative Study of Hip Fractures. Mortality effects of timing alternatives for hip fracture surgery. CMAJ. 2018 Aug 7;190(31):E923–32. [PMID: 30087128]
Stirton JB et al. Total hip arthroplasty for the management of hip fracture: a review of the literature. J Orthop. 2019 Feb 26;16(2):141–4. [PMID: 30886461]
2. Hip Osteoarthritis
ESSENTIALS OF DIAGNOSIS

 Pain deep in the groin on the affected side.
Pain deep in the groin on the affected side.
 Swelling.
Swelling.
 Degeneration of joint cartilage.
Degeneration of joint cartilage.
 Loss of active and passive range of motion in severe OA.
Loss of active and passive range of motion in severe OA.
 General Considerations
General Considerations
In the United States, the prevalence of OA will grow as the number of persons over age 65 years doubles to more than 70 million by 2030. Cartilage loss and OA symptoms are preceded by damage to the collagen-proteoglycan matrix. The etiology of OA is often multifactorial, including previous trauma, prior high-impact activities, genetic factors, obesity, and rheumatologic or metabolic conditions. Femoroacetabular impingement, which affects younger active patients, is considered an early development of hip OA.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
OA usually causes pain in the affected joint with loading of the joint or at the extremes of motion. Mechanical symptoms—such as swelling, grinding, catching, and locking—suggest internal derangement, which is indicated by damaged cartilage or bone fragments that affect the smooth range of motion expected at an articular joint. Pain can also produce the sensation of “buckling” or “giving way” due to muscle inhibition. As the joint degeneration becomes more advanced, the patient loses active range of motion and may lose passive range of motion as well.
Patients complain of pain deep in the groin on the affected side and have problems with weight-bearing activities such as walking, climbing stairs, and getting up from a chair. They may limp and develop a lurch during their gait, leaning toward the unaffected side as they walk to reduce pressure on the arthritic hip. The most specific findings to identify hip osteoarthritis were squat causing posterior pain, groin pain on passive abduction or adduction, abductor weakness, and decreased passive hip adduction or less passive internal rotation compared with the contralateral leg. The presence of normal passive hip adduction was most useful for suggesting the absence of OA (LR–, 0.25 [95% CI, 0.11–0.54]).
B. Imaging
An anterior-posterior weight-bearing radiograph of the pelvis with a lateral view of the symptomatic hip are preferred views for evaluation of hip OA. Joint space narrowing and sclerosis suggest early OA. Findings of femoroacetabular impingement are commonly reported on radiograph reports with arthritic changes and anatomic variations involving the acetabulum and femoral head neck junction. After age 35, MRI of the hips already show labral changes in almost 70% of asymptomatic patients. Osteophytes near the femoral head or acetabulum and subchondral bone cysts (advanced Kellgren and Lawrence grade), superior or (supero) lateral femoral head migration, and subchondral sclerosis suggest the patient will more likely progress to total hip replacement. However, not all patients with radiographic hip OA have hip or groin pain; the converse is also true.
 Treatment
Treatment
A. Conservative
Changes in the articular cartilage are irreversible. Therefore, a cure for the diseased joint is not possible, although symptoms or structural issues can be managed to try to maintain activity level. Conservative treatment for patients with OA includes activity modification, proper footwear, therapeutic exercises, weight loss, and use of assistive devices (such as a cane). A 2014 randomized study found that physical therapy did not lead to greater improvement in pain or function compared with sham treatment in patients with hip OA. Analgesics may be effective in some cases. Corticosteroid injections can be considered for short-term relief of pain; however, hip injections are best performed under fluoroscopic, ultrasound, or CT guidance to ensure accurate injection in the joint.
B. Surgical
Joint replacement surgeries are effective and cost-effective for patients with significant symptoms and functional limitations, providing improvements in pain, function, and quality of life. Various surgical techniques and computer-assisted navigation during operation continue to be investigated. A review of nine randomized controlled trials concluded that a direct anterior approach for hip replacement was associated with a shorter incision, lower blood loss, lower pain scores, and earlier functional recovery. However, there was no significant difference in complication rates between groups for the direct anterior or posterior approaches. There has not been clear clinical benefit of minimally invasive surgery compared to the standard invasive surgery, except for less total blood loss, shorter duration of surgery, and a shorter length of hospital stay.
Hip resurfacing surgery is a newer joint replacement technique. Rather than use a traditional artificial joint implant of the whole neck and femur, only the femoral head is removed and replaced. Evidence to date suggests that hip resurfacing is comparable to total hip replacement and is a viable alternative for younger patients. The cumulative survival rate of this implant at 10 years is estimated to be 94%. Concerns following resurfacing surgery include the risk of femoral neck fracture and collapse of the head. In a systematic review of national databases, the average time to revision was 3.0 years for metal-on-metal hip resurfacing versus 7.8 years for total hip arthroplasty. Dislocations were more frequent with total hip arthroplasty than metal-on-metal hip resurfacing: 4.4 vs 0.9 per 1000 person-years, respectively.
Guidelines recommend prophylaxis for venous thromboembolic disease for a minimum of 14 days after arthroplasty of the hip or knee using warfarin, low-molecular-weight heparin, fondaparinux, aspirin, rivaroxaban, dabigatran, apixaban, or portable mechanical compression (see Table 14–14).
 When to Refer
When to Refer
Patients with sufficient disability, limited benefit from conservative therapy, and evidence of severe OA on imaging can be referred for joint replacement surgery.
Hunter DJ et al. Osteoarthritis. Lancet. 2019 Apr 27;393(10182):1745–59. [PMID: 31034380]
Metcalfe D et al. Does this patient have hip osteoarthritis? The Rational Clinical Examination Systematic Review. JAMA. 2019 Dec 17;322(23):2323–33. [PMID: 31846019]
Migliorini F et al. Total hip arthroplasty: minimally invasive surgery or not? Meta-analysis of clinical trials. Int Orthop. 2019 Jul;43(7):1573–82. [PMID: 30171273]
Teirlinck CH et al. Prognostic factors for progression of osteoarthritis of the hip: a systematic review. Arthritis Res Ther. 2019 Aug 23;21(1):192. [PMID: 31443685]
Wang Z et al. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg Res. 2018 Sep 6;13(1):229. [PMID: 30189881]
KNEE
1. Knee Pain
ESSENTIALS OF DIAGNOSIS

 Effusion can occur with intra-articular pathology (eg, OA, meniscus and cruciate ligament tears).
Effusion can occur with intra-articular pathology (eg, OA, meniscus and cruciate ligament tears).
 Acute knee swelling (due to hemarthrosis) within 2 hours may indicate ligament injuries or patellar dislocation or fracture.
Acute knee swelling (due to hemarthrosis) within 2 hours may indicate ligament injuries or patellar dislocation or fracture.
 General Considerations
General Considerations
The knee is the largest joint in the body and is susceptible to injury from trauma, inflammation, infection, and degenerative changes. The knee is a hinge joint. The joint line exists between the femoral condyles and tibial plateaus. Separating and cushioning these bony surfaces is the lateral and medial meniscal cartilage, which functions as a shock absorber during weight bearing, protecting the articular cartilage. The patella is a large sesamoid bone anterior to the joint. It is embedded in the quadriceps tendon, and it articulates with the trochlear groove of the femur. Poor patellar tracking in the trochlear groove is a common source of knee pain especially when the cause is atraumatic in nature. The knee is stabilized by the collateral ligaments against varus (lateral collateral ligament) and valgus (medial collateral ligament) stresses. The tibia is limited in its anterior movement by the anterior cruciate ligament (ACL) and in its posterior movement by the posterior cruciate ligament (PCL). The bursae of the knee are located between the skin and bony prominences. They act to decrease friction of tendons and muscles as they move over adjacent bony structures. Excessive external pressure or friction can lead to swelling and pain of the bursae. The prepatellar bursae (located between the skin and patella) and the pes anserine bursa (which is medial and inferior to the patella, just below the tibial plateau) are most commonly affected. Joint fluid, when excessive due to synovitis or trauma, can track posteriorly through a potential space, resulting in a popliteal cyst (also called a Baker cyst). Other structures that are susceptible to overuse injury and may cause knee pain following repetitive activity include the patellofemoral joint and the iliotibial band. OA of the knees is common after 50 years of age and can develop due to previous trauma, aging, activities, alignment issues, and genetic predisposition.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Evaluation of knee pain should begin with general questions regarding duration and rapidity of symptom onset and the mechanism of injury or aggravating symptoms. Overuse or degenerative problems can occur with stress or compression from sports, hobbies, or occupation. A history of trauma, previous orthopedic problems with, or surgery to, the affected knee should also be specifically queried. Symptoms of infection (fever, recent bacterial infections, risk factors for sexually transmitted infections [such as gonorrhea] or other bacterial infections [such as staphylococcal infection]) should always be elicited.
Common symptom complaints include the following:
1. Presence of grinding, clicking, or popping with bending may be indicative of OA or the patellofemoral syndrome.
2. “Locking” or “catching” when walking suggests an internal derangement, such as meniscal injury or a loose body in the knee.
3. Intra-articular swelling of the knee or an effusion indicates an internal derangement or a synovial pathology. Large swelling may cause a popliteal (Baker) cyst. Acute swelling within minutes to hours suggests a hemarthrosis, most likely due to an ACL injury, fracture, or patellar dislocation, especially if trauma is involved.
4. Lateral “snapping” with flexion and extension of the knee may indicate inflammation of the iliotibial band.
5. Pain that is worsened with bending and walking downstairs suggests issues with the patellofemoral joint, usually degenerative such as chondromalacia of the patella or OA.
6. Pain that occurs when rising after prolonged sitting suggests a problem with tracking of the patella.
A careful history coupled with a physical examination that includes observation, palpation, and range of motion testing, as well as specific tests for particular anatomic structures is frequently sufficient to establish a diagnosis. When there is a knee joint effusion caused by increased fluid in the intra-articular space, physical examination will demonstrate swelling in the hollow or dimple around the patella and distention of the suprapatellar space.
Table 41–5 shows the differential diagnosis of knee pain, and Table 41–6 outlines possible diagnoses based on the location of pain.
Table 41–6. Location of common causes of knee pain.
Medial knee pain
Medial compartment osteoarthritis
Medial collateral ligament strain
Medial meniscal injury
Anserine bursitis (pain over the proximal medial tibial plateau)
Anterior knee pain
Patellofemoral syndrome (often bilateral)
Osteoarthritis
Prepatellar bursitis (associated with swelling anterior to the patella)
“Jumper’s knee” (pain at the inferior pole of the patella)
Septic arthritis
Gout or other inflammatory disorder
Lateral knee pain
Lateral meniscal injury
Iliotibial band syndrome (pain superficially along the distal iliotibial band near lateral femoral condyle or lateral tibial insertion)
Lateral collateral ligament sprain (rare)
Posterior knee pain
Popliteal (Baker) cyst
Osteoarthritis
Meniscal tears
Hamstring or calf tendinopathy
B. Laboratory Findings
Laboratory testing of aspirated joint fluid, when indicated, can lead to a definitive diagnosis in most patients (see Tables 20–2 and 20–3).
C. Imaging
Knee pain is evaluated with plain (weight-bearing) radiographs and MRI most commonly, but CT and ultrasound are sometimes useful.
An acute hemarthrosis represents bloody swelling that usually occurs within the first 1–2 hours following trauma. In situations where the trauma may be activity-related and not a result of a fall or collision, the differential diagnosis most commonly includes ACL tear (responsible for more than 70% in adults), fracture (patella, tibial plateau, femoral supracondylar, growth plate [physeal]), and patellar dislocation. Meniscal tears are unlikely to cause large hemarthrosis.
Bunt CW et al. Knee pain in adults and adolescents: the initial evaluation. Am Fam Physician. 2018 Nov 1;98(9):576–85. [PMID: 30325638]
Dadabo J et al. Noninterventional therapies for the management of knee osteoarthritis. J Knee Surg. 2019 Jan;32(1):46–54. [PMID: 30477045]
Lee B et al. Injection alternatives for the management of knee osteoarthritis pain. Surg Technol Int. 2019 May 15;34:513–9. [PMID: 30888679]
Mora JC et al. Knee osteoarthritis: pathophysiology and current treatment modalities. J Pain Res. 2018 Oct 5;11:2189–96. [PMID: 30323653]
Price AJ et al. Knee replacement. Lancet. 2018 Nov 3;392(10158):1672–82. [PMID: 30496082]
Ramlall Y et al. Examining pain before and after primary total knee replacement (TKR): a retrospective chart review. Int J Orthop Trauma Nurs. 2019 Aug;34:43–7. [PMID: 31272918]
Richardson C et al. Intra-articular hyaluronan therapy for symptomatic knee osteoarthritis. Rheum Dis Clin North Am. 2019 Aug;45(3):439–51. [PMID: 31277754]
Urits I et al. Minimally invasive interventional management of osteoarthritic chronic knee pain. J Knee Surg. 2019 Jan;32(1):72–9. [PMID: 30500975]
2. Anterior Cruciate Ligament Injury
ESSENTIALS OF DIAGNOSIS

 An injury involving an audible pop when the knee buckles.
An injury involving an audible pop when the knee buckles.
 Acute swelling immediately (or within 2 hours).
Acute swelling immediately (or within 2 hours).
 Instability occurs with lateral movement activities and going down stairs.
Instability occurs with lateral movement activities and going down stairs.
 General Considerations
General Considerations
The anterior cruciate ligament (ACL) connects the posterior aspect of the lateral femoral condyle to the anterior aspect of the tibia. Its main function is to control anterior translation of the tibia on the femur. It also provides rotational stability of the tibia on the femur. ACL tears are common with sporting injuries. They can result from both contact (valgus blow to the knee) and non-contact (jumping, pivoting, and deceleration) activities. The patient usually falls down following the injury, has acute swelling and difficulty with weight bearing and complains of instability. ACL injuries are common in skiing, soccer, football, and basketball among young adolescents and middle-aged patients. Prepubertal and older patients usually sustain fractures instead of ligamentous injuries.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Acute ACL injuries usually lead to acute swelling of the knee, causing difficulty with motion. After the swelling has resolved, the patient can walk with a “stiff-knee” gait or quadriceps avoidance gait because of the instability. Patients describe symptoms of instability while performing side-to-side maneuvers or descending stairs. Stability tests assess the amount of laxity of the knee while performing these maneuvers. The Lachman test (84–87% sensitivity and 93% specificity) is performed with the patient lying supine and the knee flexed to 20–30 degrees (Table 41–7). The clinician grasps the distal femur from the lateral side and the proximal tibia with the other hand on the medial side. With the knee in neutral position, stabilize the femur, and pull the tibia anteriorly using a similar force to lifting a 10- to 15-pound weight. Excessive anterior translation of the tibia compared with the other side indicates injury to the ACL. The anterior drawer test (48% sensitivity and 87% specificity) is performed with the patient lying supine and the knee flexed to 90 degrees (Table 41–7). The clinician stabilizes the patient’s foot by sitting on it and grasps the proximal tibia with both hands around the calf and pulls anteriorly. A positive test finds ACL laxity compared with the unaffected side. The pivot shift test is used to determine the amount of rotational laxity of the knee (Table 41–7). The patient is examined while lying supine with the knee in full extension. It is then slowly flexed while applying internal rotation and a valgus stress. The clinician feels for a subluxation at 20–40 degrees of knee flexion. The patient must remain very relaxed to have a positive test.

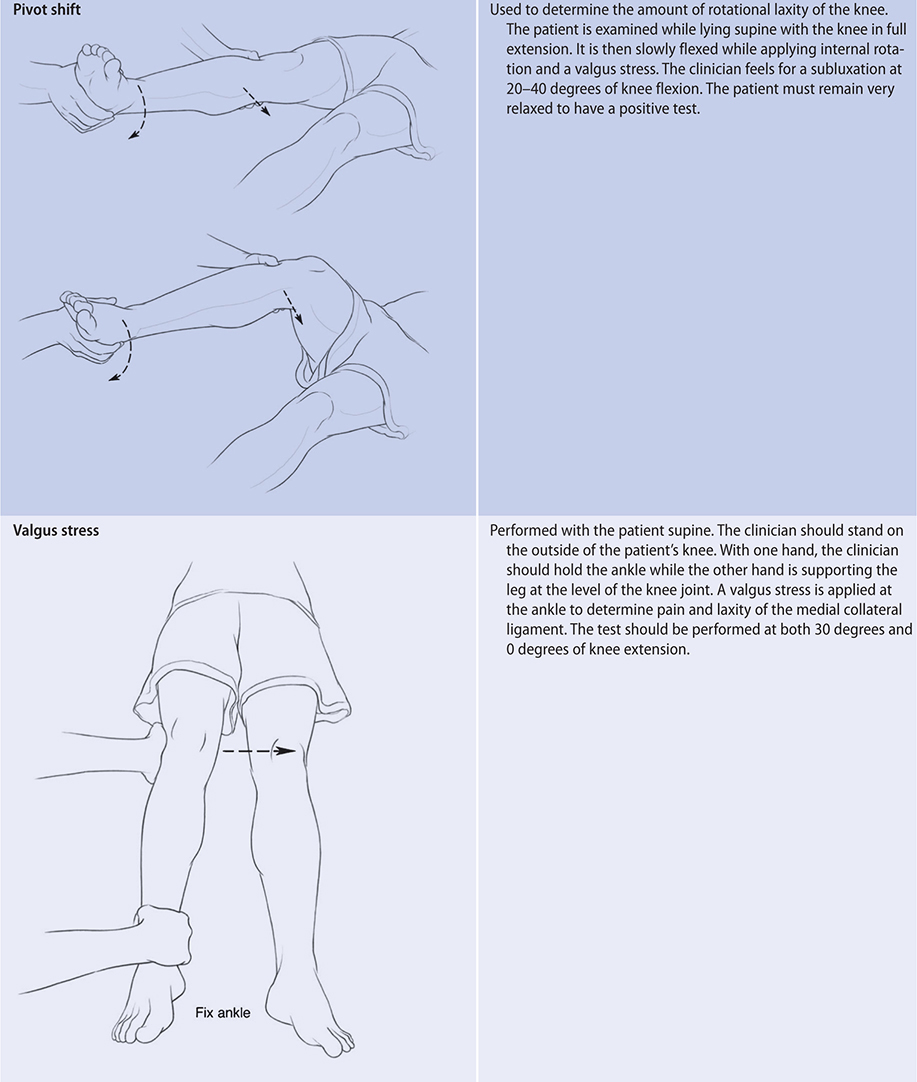
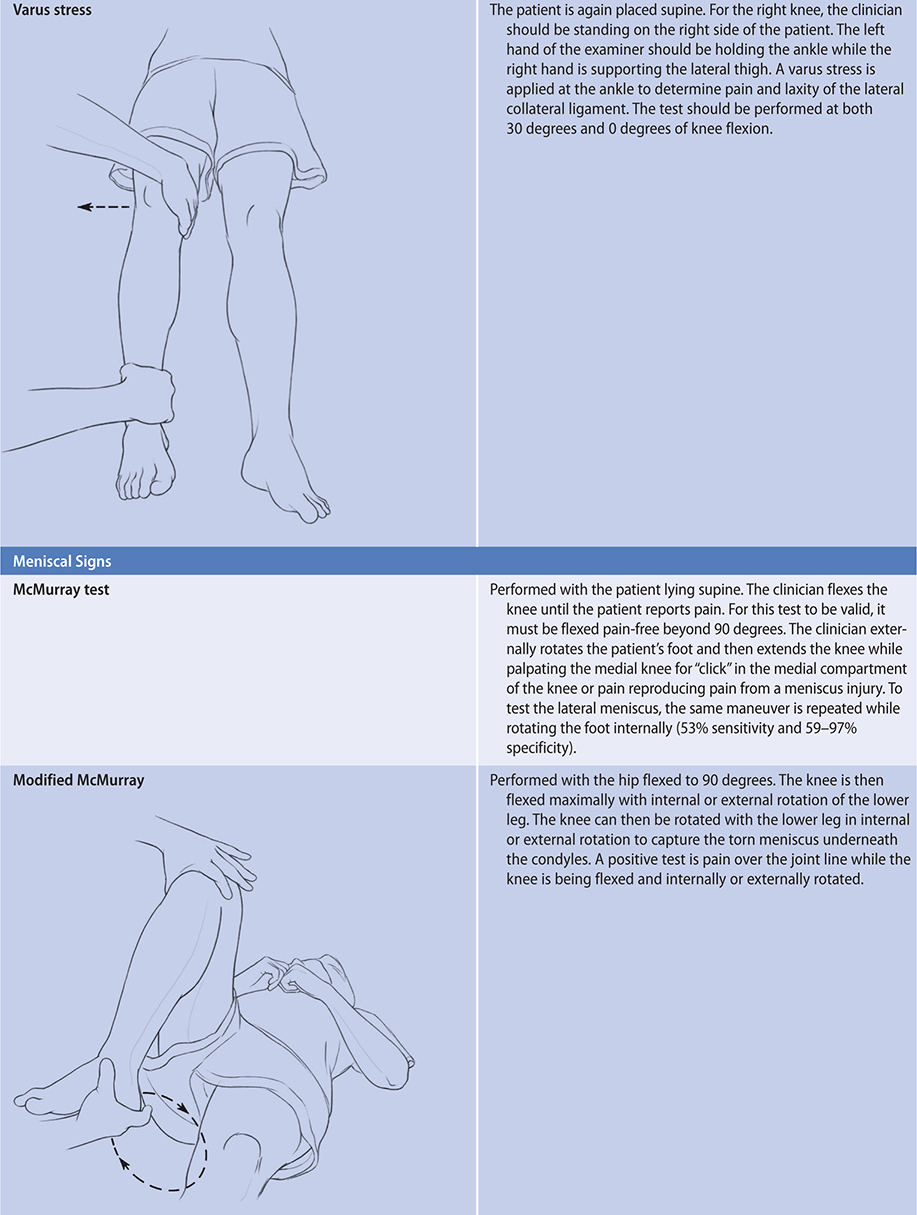
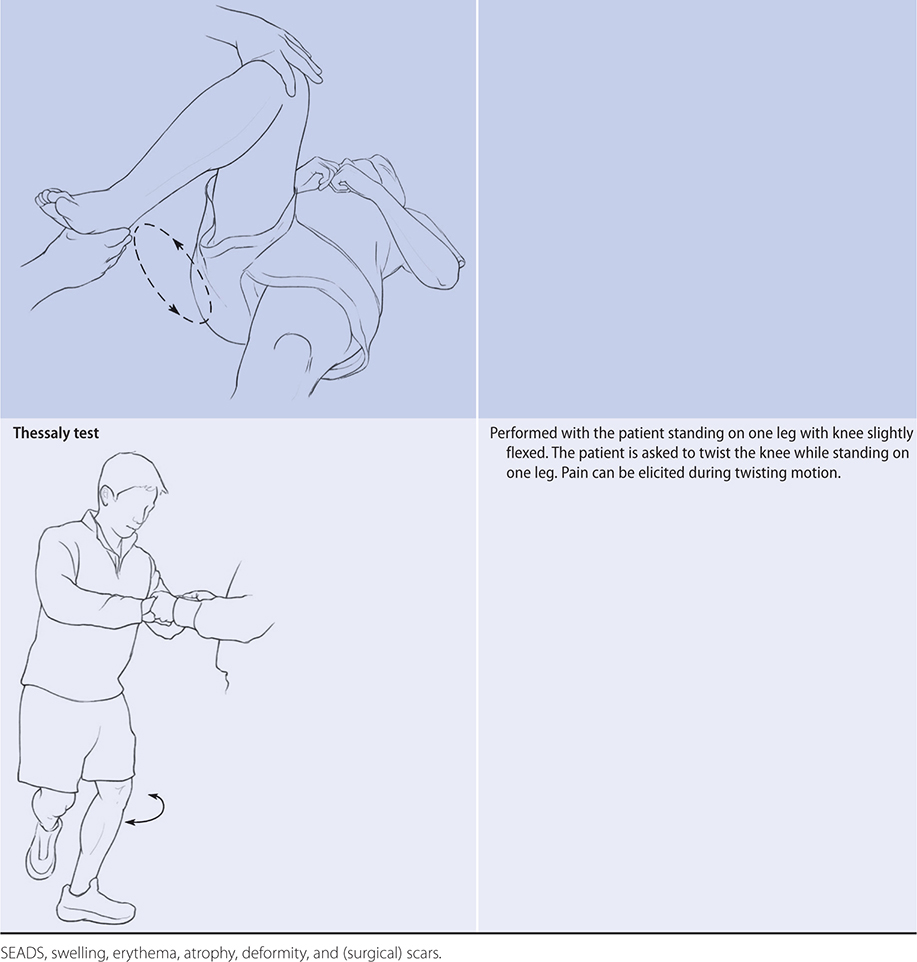
B. Imaging
Plain radiographs are usually negative in ACL tears but are useful to rule out fractures. A small avulsion injury can sometimes be seen over the lateral compartment of the knee (“Segond” fracture) and is pathognomonic of an ACL injury. An ACL injury that avulsed the tibial spine can be seen in radiographs. MRI is the best tool to diagnose ACL tears and associated articular and meniscal cartilage issues. It has greater than 95% sensitivity and specificity for ACL tears.
 Treatment
Treatment
Most young and active patients will require surgical reconstruction of the ACL. Some data suggest that reconstruction within 5 months of the tear has better outcomes. However, a small randomized trial suggested that acute ACL injuries can be treated nonoperatively and delayed ACL reconstruction had similar outcomes to acute ACL reconstructions. But patients for whom the reconstruction is delayed have more cartilage or meniscus problems at the time of surgery. Common surgical techniques use the patient’s own tissue, usually the patellar or hamstring tendons (autograft), or use a cadaver graft (allograft) to arthroscopically reconstruct the torn ACL. Different patient groups experienced improved results with specific surgical graft choices. However, allografts do have a higher failure rate when compared with autografts. Recovery from surgery usually requires 6 months.
Nonoperative treatments are usually reserved for older patients or those with a very sedentary lifestyle. Physical therapy can focus on hamstring strengthening and core stability. An ACL brace can help stability. Longitudinal studies have demonstrated that nonoperative management of an ACL tear can lead to a higher incidence of meniscus tears. Cost-analysis studies have shown that early ACL reconstruction can be more beneficial than nonoperative treatment and delayed subsequent surgeries.
 When to Refer
When to Refer
• Almost all ACL tears should be referred to an orthopedic surgeon for evaluation.
• Individuals with instability in the setting of a chronic ACL tear (greater than 6 months) should be considered for surgical reconstruction.
• Patients with an ACL tear and associated meniscus or articular injuries may benefit from surgery to address the other injuries.
Filbay SR et al. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. 2019 Feb;33(1):33–47. [PMID: 31431274]
Horvath A et al. Outcome after anterior cruciate ligament revision. Curr Rev Musculoskelet Med. 2019 Jul 8:397–405. [PMID: 31286413]
Kaplan Y et al. When is it safe to return to sport after ACL reconstruction? Reviewing the criteria. Sports Health. 2019 Jul/Aug;11(4):301–5. [PMID: 31136725]
Richmond JC. Anterior cruciate ligament reconstruction. Sports Med Arthrosc Rev. 2018 Dec;26(4):165–7. [PMID: 30395059]
Webster KE et al. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med. 2019 Jun;49(6):917–29. [PMID: 30905035]
3. Collateral Ligament Injury
ESSENTIALS OF DIAGNOSIS

 Caused by a valgus or varus blow or stress to the knee.
Caused by a valgus or varus blow or stress to the knee.
 Pain and instability in the affected area.
Pain and instability in the affected area.
 Limited range of motion.
Limited range of motion.
 General Considerations
General Considerations
The medial collateral ligament (MCL) is the most commonly injured ligament in the knee. It is usually injured with a valgus stress to the partially flexed knee. It can also occur with a blow to the lateral leg. The MCL is commonly injured with acute ACL injuries. The lateral collateral ligament (LCL) is less commonly injured, but this can occur with a medial blow to the knee. Since both collateral ligaments are extra-articular, injuries to these ligaments may not lead to any intra-articular effusion. Affected patients may have difficulty walking initially, but this can improve when the swelling decreases.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The main clinical findings for patients with collateral ligament injuries are pain along the course of the ligaments. The patient may have limited range of motion due to pain, especially during the first 2 weeks following the injury. The best tests to assess the collateral ligaments are the varus and valgus stress tests. The sensitivity of the tests is as high as 86–96%.
The valgus stress test is performed with the patient supine (Table 41–7). The clinician should stand on the outside of the patient’s knee. With one hand, the clinician should hold the ankle while the other hand is supporting the leg at the level of the knee joint. A valgus stress is applied at the ankle to determine pain and laxity of the MCL. The test should be performed at both 30 degrees and at 0 degrees of knee extension.
For the varus stress test, the patient is again placed supine (Table 41–7). For the right knee, the clinician should be standing on the right side of the patient. The clinician’s left hand should be holding the ankle while the right hand is supporting the lateral thigh. A varus stress is applied at the ankle to determine pain and laxity of the LCL. The test should be performed at both 30 degrees and at 0 degrees of knee flexion.
The test results can be graded from 1 to 3. Grade 1 is when the patient has pain with varus/valgus stress test but no instability. With grade 2 injuries, the patient has pain, and the knee shows instability at 30 degrees of knee flexion. In grade 3 injuries, the patient has marked instability but not much pain. The knee is often unstable at both 30 degrees and 0 degrees of knee flexion.
B. Imaging
Radiographs are usually nondiagnostic except for avulsion injuries. However, radiographs should be used to rule out fractures that can occur with collateral ligament injuries. Isolated MCL injuries usually do not require evaluation by MRI, but MRI should be used to evaluate possible associated cruciate ligament injuries. LCL or posterolateral corner injuries should have MRI evaluation to exclude associated injuries and to determine their significance.
 Treatment
Treatment
The majority of MCL injuries can be treated with protected weight bearing and physical therapy. For grade 1 and 2 injuries, the patient can usually bear weight as tolerated with full range of motion. A hinged knee brace can be given to patients with grade 2 MCL tears to provide stability. Early physical therapy is recommended to protect range of motion and muscle strength. Grade 3 MCL injuries require long leg braces to provide stability. Patients can weight-bear, but only with the knee locked in extension with a brace. The motion can then be increased with the brace unlocked. Grade 3 injuries can take up to 6–8 weeks to heal. MCL injuries rarely need surgery. LCL injuries are less common but are usually associated with other ligament injuries (such as ACL and PCL). LCL injuries do not recover well with nonoperative treatment and usually require urgent surgical repair or reconstruction.
 When to Refer
When to Refer
• Symptomatic instability with chronic MCL tears or acute MCL tears with other ligamentous injuries.
• LCL or posterolateral corner injuries require urgent surgical repair or reconstruction (within 1 week).
Elkin JL et al. Combined anterior cruciate ligament and medial collateral ligament knee injuries: anatomy, diagnosis, management recommendations, and return to sport. Curr Rev Musculoskelet Med. 2019 Jun;12(2):239–44. [PMID: 30929138]
Grawe B et al. Lateral collateral ligament injury about the knee: anatomy, evaluation, and management. J Am Acad Orthop Surg. 2018 Mar 15;26(6):e120–7. [PMID: 29443704]
Porrino J et al. An update and comprehensive review of the posterolateral corner of the knee. Radiol Clin North Am. 2018 Nov;56(6):935–51. [PMID: 30322491]
Shon OJ et al. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017 Dec 1;29(4):256–68. [PMID: 29172386]
4. Posterior Cruciate Ligament Injury
ESSENTIALS OF DIAGNOSIS

 Usually follows an anterior trauma to the tibia, such as a dashboard injury during a motor vehicle accident.
Usually follows an anterior trauma to the tibia, such as a dashboard injury during a motor vehicle accident.
 The knee may freely dislocate and reduce.
The knee may freely dislocate and reduce.
 One-third of multi-ligament injuries involving the PCL have neurovascular injuries.
One-third of multi-ligament injuries involving the PCL have neurovascular injuries.
 General Considerations
General Considerations
The posterior cruciate ligament (PCL) is the strongest ligament in the knee. PCL injuries usually represent significant trauma and are highly associated with multi-ligament injuries and knee dislocations. More than 70–90% of PCL injuries have associated injuries to the posterolateral corner, MCL, and ACL. Neurovascular injuries occur in up to one-third of all knee dislocations or PCL injuries. There should be high suspicion for neurovascular injuries and a thorough neurovascular examination of the limb should be performed.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Most patients with acute injuries have difficulty with ambulation. Patients with chronic PCL injuries can ambulate without gross instability but may complain of subjective “looseness” and often report pain and dysfunction, especially with bending. Clinical examinations of PCL injuries include the “sag sign”; the patient is placed supine and both hips and knees are flexed to 90 degrees. Because of gravity, the posterior cruciate ligament-injured knee will have an obvious set-off at the anterior tibia that is “sagging” posteriorly. The PCL ligament can also be examined using the posterior drawer test; the patient is placed supine with the knee flexed to 90 degrees. In a normal knee, the anterior tibia should be positioned about 10 mm anterior to the femoral condyle. The clinician can grasp the proximal tibia with both hands and push the tibia posteriorly. The movement, indicating laxity and possible tear of the PCL, is compared with the uninjured knee (90% sensitivity and 99% specificity). A PCL injury is sometimes mistaken for an ACL injury during the anterior drawer test since the tibia is subluxed posteriorly in a sagged position and can be abnormally translated forward, yielding a false-positive test for an ACL injury. Pain, swelling, pallor, and numbness in the affected extremity may suggest a knee dislocation with possible injury to the popliteal artery.
B. Imaging
Radiographs are often nondiagnostic but are required to diagnose any fractures. MRI is used to diagnose PCL and other associated injuries.
 Treatment
Treatment
Isolated PCL injuries can be treated nonoperatively. Acute injuries are usually immobilized using a knee brace with the knee extension; the patient uses crutches for ambulation. Physical therapy can help achieve increased range of motion and improved ambulation. Many PCL injuries are associated with other injuries and may require operative reconstruction.
 When to Refer
When to Refer
• The patient should be seen urgently within 1–2 weeks.
• If the lateral knee is also unstable with varus stress testing, the patient should be assessed for a posterolateral corner injury, which may require an urgent surgical reconstruction.
• Isolated PCL tears may require surgery if the tear is complete (grade 3) and the patient is symptomatic.
Badri A et al. Clinical and radiologic evaluation of the posterior cruciate ligament-injured knee. Curr Rev Musculoskelet Med. 2018 Sep;11(3):515–20. [PMID: 29987531]
Devitt BM et al. Isolated posterior cruciate reconstruction results in improved functional outcome but low rates of return to preinjury level of sport: a systematic review and meta-analysis. Orthop J Sports Med. 2018 Oct 26;6(10):2325967118804478. [PMID: 30386804]
Strauss MJ et al. The use of allograft tissue in posterior cruciate, collateral and multi-ligament knee reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019 Jun;27(6):1791–809. [PMID: 30824979]
5. Meniscus Injuries
ESSENTIALS OF DIAGNOSIS

 Patient may or may not report an injury.
Patient may or may not report an injury.
 Joint line pain and pain with deep squatting are the most sensitive signs.
Joint line pain and pain with deep squatting are the most sensitive signs.
 Difficulty with knee extension suggests an internal derangement that should be evaluated urgently with MRI.
Difficulty with knee extension suggests an internal derangement that should be evaluated urgently with MRI.
 General Considerations
General Considerations
The menisci act as shock absorbers within the knee. Injuries to a meniscus can lead to pain, clicking, and locking sensation. Most meniscus injuries occur with acute injuries (usually in younger patients) or repeated microtrauma, such as squatting or twisting (usually in older patients).
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The patient may have an antalgic (painful) gait and difficulty with squatting. He or she may complain of catching or locking of the meniscal fragment. Physical findings can include effusion or joint line tenderness. Patients can usually point out the area of maximal tenderness along the joint line. Swelling usually occurs during the first 24 hours after the injury or later. Meniscus tears rarely lead to the immediate swelling that is commonly seen with fractures and ligament tears. Meniscus tears are commonly seen in arthritic knees. However, it is often unclear whether the pain is coming from the meniscus tear or the arthritis.
Provocative tests, including the McMurray test, the modified McMurray test, and the Thessaly test, can be performed to confirm the diagnosis (Table 41–7). Most symptomatic meniscus tears cause pain with deep squatting and when waddling (performing a “duck walk”).
B. Imaging
Radiographs are usually normal but may show joint space narrowing, early OA changes, or loose bodies. MRI of the knee is the best diagnostic tool for meniscal injuries (93% sensitivity and 95% specificity). High signal through the meniscus (bright on T2 images) represents a meniscal tear.
 Treatment
Treatment
Conservative treatment can be used for degenerative tears in older patients. The treatment is similar for patients with mild knee OA, including analgesics and physical therapy for strengthening and core stability. A randomized controlled trial showed that physical therapy compared to arthroscopic partial meniscectomy had similar outcomes at 6 months. However, 30% of the patients who were assigned to physical therapy alone underwent surgery within 6 months.
Randomized studies have shown that arthroscopic surgery has no benefit over sham operations in patients who have degenerative meniscal tears, especially with imaging showing signs of osteoarthritis. Another randomized controlled trial found that patients with degenerative meniscus tears but no signs of arthritis on imaging treated conservatively with supervised exercise therapy had similar outcomes to those treated with arthroscopy at 2-year follow-up. There is crossover between the groups; patients can be treated with supervised exercise therapy first, and if they do not respond to nonoperative treatment, they can undergo meniscus surgeries. Acute tears in young and active patients with clinical signs of internal derangement (catching and swelling) and without signs of arthritis on imaging or patients with acute mechanical locking with a displaced meniscus can be best treated arthroscopically with meniscus repair or debridement. There is also growing evidence that untreated meniscus root tears can lead to accelerated osteoarthritic changes. Surgical treatment before cartilage breakdown is recommended for acute meniscus root injuries.
 When to Refer
When to Refer
• If the patient has symptoms of internal derangement suspected as meniscus injury. The patient should receive an MRI to confirm the injury.
• If the patient cannot extend the knee due to a mechanical block, the patient should be evaluated as soon as possible. Certain shaped tears on MRI, such as bucket handle tears, meniscus root injuries, are amenable to meniscal repair surgery.
• If the patient has not responded to physical therapy and nonoperative treatment and continues to have symptoms related to the torn meniscus.
• If the patient has MRI confirmation of acute meniscus root injuries.
Donohue MA et al. Meniscus injuries in the military athlete. J Knee Surg. 2019 Feb;32(2):123–6. [PMID: 30630210]
Driban JB et al. Accelerated knee osteoarthritis is characterized by destabilizing meniscal tears and pre-radiographic structural disease burden. Arthr Rheumatol. 2019 Jul;71(7):1089–100. [PMID: 30592385]
Karia M et al. Current concepts in the techniques, indications and outcomes of meniscal repairs. Eur J Orthop Surg Traumatol. 2019 Apr;29(3):509–20. [PMID: 30374643]
Kurzweil PR et al. Meniscus repair and replacement. Sports Med Arthrosc Rev. 2018 Dec;26(4):160–4. [PMID: 30395058]
Pache S et al. Meniscal root tears: current concepts review. Arch Bone Jt Surg. 2018 Jul;6(4):250–9. [PMID: 30175171]
6. Patellofemoral Pain
ESSENTIALS OF DIAGNOSIS

 Pain experienced with bending activities (kneeling, squatting, climbing stairs).
Pain experienced with bending activities (kneeling, squatting, climbing stairs).
 Lateral deviation or tilting of the patella in relation to the femoral groove.
Lateral deviation or tilting of the patella in relation to the femoral groove.
 General Considerations
General Considerations
Patellofemoral pain, also known as anterior knee pain, chondromalacia, or “runner’s knee,” describes any pain involving the patellofemoral joint. The pain affects any or all of the anterior knee structures, including the medial and lateral aspects of the patella as well as the quadriceps and patellar tendon insertions. The patella engages the femoral trochlear groove with approximately 30 degrees of knee flexion. Forces on the patellofemoral joint increase up to three times body weight as the knee flexes to 90 degrees (eg, climbing stairs), and five times body weight when going into full knee flexion (eg, squatting). Abnormal patellar tracking during flexion can lead to abnormal articular cartilage wear and pain. When the patient has ligamentous hyperlaxity, the patella can sublux out of the groove, usually laterally. Patellofemoral pain is also associated with muscle strength and flexibility imbalances as well as altered hip and ankle biomechanics.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Patients usually complain of pain in the anterior knee with bending movements and less commonly in full extension. Pain from this condition is localized under the kneecap but can sometimes be referred to the posterior knee or over the medial or lateral inferior patella. Symptoms may begin after a trauma or after repetitive physical activity, such as running and jumping. When maltracking, palpable and sometimes audible crepitus can occur.
Intra-articular swelling usually does not occur unless there are articular cartilage defects or if OA changes develop. On physical examination, it is important to palpate the articular surfaces of the patella. For example, the clinician can use one hand to move the patella laterally, and use the fingertips of the other hand to palpate the lateral undersurface of the patella. Patellar mobility can be assessed by medially and laterally deviating the patella (deviation by one-quarter of the diameter of the kneecap is consider normal; greater than one-half the diameter suggests excessive mobility). The apprehension sign suggests instability of the patellofemoral joint and is positive when the patient becomes apprehensive when the patella is deviated laterally. The patellar grind test is performed by grasping the knee superior to the patella and pushing it downward with the patient supine and the knee extended, pushing the patella inferiorly. The patient is asked to contract the quadriceps muscle to oppose this downward translation, with reproduction of pain or grinding being the positive sign for chondromalacia of the patella. There are two common presentations: (1) patients whose ligaments and patella are too loose (hypermobility); and (2) patients who have soft tissues that are too tight, leading to excessive pressure on the joint.
Evaluation of the quadriceps strength and hip stabilizers can be accomplished by having the patient perform a one-leg squat without support. Normally, with a one-leg squat, the knee should align over the second metatarsal ray of the foot. Patients who are weak may display poor balance, with dropping of the pelvis (similar to a positive hip Trendelenburg sign) or excessive internal rotation of the knee medially.
B. Imaging
Diagnostic imaging has limited use in younger patients and is more helpful in older patients to assess for OA or to evaluate patients who do not respond to conservative treatment. Radiographs may show lateral deviation or tilting of the patella in relation to the femoral groove. MRI may show thinning of the articular cartilage but is not clinically necessary, except prior to surgery or to exclude other pathology.
 Treatment
Treatment
A. Conservative
For symptomatic relief, use of local modalities such as ice and anti-inflammatory medications can be beneficial. If the patient has signs of patellar hypermobility, physical therapy exercises are useful to strengthen the quadriceps (especially the vastus medialis obliquus muscle) to help stabilize the patella and improve tracking. There is consistent evidence that exercise therapy for patellofemoral pain syndrome may result in clinically important reduction in pain and improvement in functional ability. Lower quality research supports that hip and knee exercises are better than knee exercises alone. Strengthening the quadriceps and the posterolateral hip muscles such as the hip abductors that control rotation at the knee should be recommended. Support for the patellofemoral joint can be provided by use of a patellar stabilizer brace or special taping techniques (McConnell taping). Correcting lower extremity alignment (with appropriate footwear or over-the-counter orthotics) can help improve symptoms, especially if the patient has pronation or high-arched feet. If the patient demonstrates tight peripatellar soft tissues, special focus should be put on stretching the hamstrings, iliotibial band, quadriceps, calves, and hip flexors.
B. Surgical
Surgery is rarely needed and is considered a last resort for patellofemoral pain. Procedures performed include lateral release or patellar realignment surgery.
 When to Refer
When to Refer
Patients with persistent symptoms despite a course of conservative therapy.
Bolgla LA et al. National Athletic Trainers’ Association Position Statement: management of individuals with patellofemoral pain. J Athl Train. 2018 Sep;53(9):820–36. [PMID: 30372640]
Crossley KM et al. Rethinking patellofemoral pain: prevention, management and long-term consequences. Best Pract Res Clin Rheumatol. 2019 Feb;33(1):48–65. [PMID: 31431275]
Neal BS et al. Risk factors for patellofemoral pain: a systematic review and meta-analysis. Br J Sports Med. 2019 Mar;53(5):270–81. [PMID: 30242107]
Saltychev M et al. Effectiveness of conservative treatment for patellofemoral pain syndrome: a systematic review and meta-analysis. J Rehabil Med. 2018 May 8;50(5):393–401. [PMID: 29392329]
7. Knee Osteoarthritis
ESSENTIALS OF DIAGNOSIS

 Degeneration of joint cartilage.
Degeneration of joint cartilage.
 Pain with bending or twisting activities.
Pain with bending or twisting activities.
 Swelling.
Swelling.
 Loss of active and passive range of motion in severe OA.
Loss of active and passive range of motion in severe OA.
 General Considerations
General Considerations
In the United States, the prevalence of OA will grow if, as some predict, the number of persons over age 65 years doubles to more than 70 million by 2030. The incidence of knee OA in the United States is 240 per 100,000 person-years.
Cartilage loss and OA symptoms are preceded by damage to the collagen-proteoglycan matrix. The etiology of OA is often multifactorial including previous trauma, prior high-impact activities, genetic factors, obesity, and rheumatologic or metabolic conditions.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
OA usually causes pain in the affected joint with loading of the joint or at the extremes of motion. Mechanical symptoms—such as swelling, grinding, catching, and locking—suggest internal derangement, which is indicated by damaged cartilage or bone fragments that affect the smooth range of motion expected at an articular joint. Pain can also produce the sensation of “buckling” or “giving way” due to muscle inhibition. As the joint degeneration becomes more advanced, the patient loses active range of motion and may lose passive range of motion as well.
As the condition worsens, patients with knee OA have an increasingly limited ability to walk. Symptoms include pain with bending or twisting activities, and going up and down stairs. Swelling, limping, and pain while sleeping are common complaints with OA, especially as it progresses.
B. Imaging
The most commonly recommended radiographs include bilateral weight-bearing 45-degree bent knee posteroanterior, lateral, and patellofemoral joint views (Merchant view). Radiographic findings include diminished width of the articular cartilage causing joint space narrowing, subchondral sclerosis, presence of osteophytes, and cystic changes in the subchondral bone. MRI of the knee is most likely unnecessary unless other pathology is suspected, such as ischemic osteonecrosis of the knee.
 Treatment
Treatment
A. Conservative
Changes in the articular cartilage are irreversible. Therefore, a cure for the diseased joint is not possible, although symptoms or structural issues can be addressed to try to maintain activity level. Conservative treatment for all patients with OA includes activity modification, therapeutic exercises, and weight loss. Lifestyle modifications also include proper footwear and avoidance of high-impact activities. Optimal exercise programs for knee OA should focus on improving aerobic capacity, quadriceps muscle strength, or lower extremity performance. Ideally, the program should be supervised and carried out three times a week.
Use of a cane in the hand opposite to the affected side is mechanically advantageous. Knee sleeves or braces provide some improvement in subjective pain symptoms most likely due to improvements in neuromuscular function. If patients have unicompartmental OA in the medial or lateral compartment, joint unloader braces are available to offload the degenerative compartment. Cushioning footwear and appropriate orthotics or shoe adjustments are useful for reducing impact to the lower extremities.
There are several oral and intra-articular pharmacologic options. Treatments that have been studied include oral acetaminophen, diclofenac, ibuprofen, naproxen, celecoxib, and intra-articular corticosteroids and hyaluronic acid. All treatments except acetaminophen showed clinically significant improvement in pain. If a traditional NSAID is indicated, the choice should be based on cost, side-effect profile, and adherence. The cyclooxygenase (COX)-2 inhibitor celecoxib is no more effective than traditional NSAIDs; it may offer short-term, but probably not long-term, advantage in preventing gastrointestinal complications. Due to its cost and potential cardiovascular risk, celecoxib should be reserved for carefully selected patients. Topical NSAIDs or capsaicin can be effective in the treatment of OA, since they avoid many of the traditional NSAID complications. Opioids can be used appropriately in patients with severe OA (see Chapter 5). Glucosamine and chondroitin sulfate are supplements that have been widely used and marketed for OA. Despite some initial promise, the best-controlled studies indicate these supplements are ineffective as analgesics in OA. However, they have minimal side effects and may be appropriate if the patient experiences subjective benefit.
Knee joint corticosteroid injections are options to help reduce pain and inflammation and can provide short-term pain relief, usually lasting about 6–12 weeks. While intra-articular triamcinolone is still commonly used in knee arthritis, a randomized controlled trial showed that 2 years of intra-articular triamcinolone every 3 months, compared with intra-articular saline, resulted in significantly greater quantitative cartilage volume loss by MRI and no significant difference in knee pain. This finding suggests that regular use of corticosteroid injections for long-term treatment of knee osteoarthritis should be avoided.
Viscosupplementation using injections of hyaluronic acid–based products is controversial. Because reviews suggested that viscosupplementation has a questionably clinically relevant effect size and an increased risk of non-threatening adverse events, the American Academy of Orthopedic Surgeons recommended that viscosupplementation should not be used in the treatment of knee OA. However, the American College of Rheumatology’s 2012 OA guidelines still recommend the use of intra-articular hyaluronic acid injection for the treatment of OA of the knee in adults.
Platelet-rich plasma injections contain high concentration of platelet-derived growth factors, which regulate some biologic processes in tissue repair. A meta-analysis of 10 studies demonstrated that platelet-rich plasma injections reduced pain in patients with knee OA more efficiently than placebo and hyaluronic acid injections. However, 9 of the 10 studies had a high risk of bias, and the underlying mechanism of biologic healing is unknown. An FDA safety and efficacy study showed that leukocyte-poor PRP autologous conditioned plasma improved overall Western Ontario and McMaster Universities Arthritis Index scores by 78% from the baseline score after 12 months, compared to 7% for the placebo group, though the sample size was small (30 patients).
B. Surgical
Two randomized trials demonstrated that arthroscopy does not improve outcomes at 1 year over placebo or routine conservative treatment of OA. Joint replacement surgeries are effective and cost-effective for patients with significant symptoms or functional limitations, providing improvements in pain, function, and quality of life. The number of total knee arthroplasty procedures jumped 162% from 1991 to 2010, along with an increase in complications and hospital readmissions. Minimally invasive surgeries and computer-assisted navigation during operation are being investigated as methods to improve techniques (eg, accurate placement of the hardware implant) and to reduce complication rates; however, major improvements have yet to be demonstrated.
Knee realignment surgery, such as high tibial osteotomy or partial knee replacement surgery, is indicated in patients younger than age 60 with unicompartmental OA, who would benefit from delaying total knee replacement. Knee joint replacement surgery has been very successful in improving outcomes for patient with end-stage OA. Long-term series describe more than 95% survival rate of the implant at 15 years.
 When to Refer
When to Refer
Patients with sufficient disability, limited benefit from conservative therapy, and evidence of severe OA can be referred for joint replacement surgery.
Honvo G et al. Update on the role of pharmaceutical-grade chondroitin sulfate in the symptomatic management of knee osteoarthritis. Aging Clin Exp Res. 2019 Aug;31(8):1163–7. [PMID: 31243744]
Paik J et al. Triamcinolone acetonide extended-release: a review in osteoarthritis pain of the knee. Drugs. 2019 Mar;79(4):455–62. Erratum in: Drugs. 2019 Apr;79(5):587. [PMID: 30847805]
Richardson C et al. Intra-articular hyaluronan therapy for symptomatic knee osteoarthritis. Rheum Dis Clin North Am. 2019 Aug;45(3):439–51. [PMID: 31277754]
Skou ST et al. Physical therapy for patients with knee and hip osteoarthritis: supervised, active treatment is current best practice. Clin Exp Rheumatol. 2019 Sep–Oct;37(Suppl 120):112–7. [PMID: 31621559]
Vincent P. Intra-articular hyaluronic acid in the symptomatic treatment of knee osteoarthritis: a meta-analysis of single-injection products. Curr Ther Res Clin Exp. 2019 Mar 7;90:39–51. [PMID: 31289603]
ANKLE INJURIES
1. Inversion Ankle Sprains
ESSENTIALS OF DIAGNOSIS

 Localized pain and swelling.
Localized pain and swelling.
 The majority of ankle injuries involve inversion injuries affecting the lateral ligaments.
The majority of ankle injuries involve inversion injuries affecting the lateral ligaments.
 Consider chronic ankle instability or associated injuries if pain persists for longer than 3 months following an ankle sprain.
Consider chronic ankle instability or associated injuries if pain persists for longer than 3 months following an ankle sprain.
 General Considerations
General Considerations
Ankle sprains are the most common sports injuries seen in outpatient clinics. Patients usually report “turning the ankle” during a fall or after landing on an irregular surface such as a hole or an opponent’s foot. The most common mechanism of injury is an inversion and plantar flexion sprain, which injures the anterior talofibular (ATF) ligament rather than the calcaneofibular (CF) ligament. Other injuries that can occur with inversion ankle injuries are listed in Table 41–8. Women appear to sustain an inversion injury more frequently than men. Chronic ankle instability is defined as persistent complaints of pain, swelling, and “giving way” in combination with recurrent sprains for at least 12 months after the initial ankle sprain. Chronic ankle instability can occur in up to 43% of ankle sprains despite physical therapy, which makes appropriate attention to acute ankle sprains important.
Table 41–8. Injuries associated with ankle sprains.
Ligaments
Subtalar joint sprain
Sinus tarsi syndrome (ongoing anterolateral post-traumatic ankle pain)
Syndesmotic (distal tibiofibular ligamentous) sprain
Deltoid sprain
Lisfranc (tarsometatarsal bony or ligamentous) injury
Tendons
Posterior tibial tendon strain
Peroneal tendon subluxation
Bones
Osteochondral talus injury
Lateral talar process fracture
Posterior impingement (os trigonum)
Fracture at the base of the fifth metatarsal
Jones fracture (between base and middle of fifth metatarsal)
Salter (growth plate) fracture (fibula)
Ankle fractures
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
The usual symptoms following a sprain include localized pain and swelling over the lateral aspect of the ankle, difficulty weight bearing, and limping. The patient’s ankle may feel unstable. On examination, there may be swelling or bruising over the lateral aspect of the ankle. The anterior, inferior aspect below the lateral malleolus is most often the point of maximal tenderness consistent with ATF and CF ligament injuries. The swelling may limit motion of the ankle.
Special stress tests for the ankle include the anterior drawer test; the clinician keeps the foot and ankle in the neutral position with the patient sitting, then uses one hand to fix the tibia and the other to hold the patient’s heel and draw the ankle forward. Normally, there may be approximately 3 mm of translation until an endpoint is felt. A positive test includes increased translation of one foot compared to the other with loss of the endpoint of the ATF ligament.
Another stress test is the subtalar tilt test, which is performed with the foot in the neutral position with the patient sitting. The clinician uses one hand to fix the tibia and the other to hold and invert the calcaneus. Normal inversion at the subtalar joint is approximately 30 degrees. A positive test consists of increased subtalar joint inversion by greater than 10 degrees on the affected side with loss of endpoint for the CF ligament. In order to grade the severity of ankle sprains, no laxity on stress tests is considered a grade 1 injury, laxity of the ATF ligament on anterior drawer testing but a negative tilt test is a grade 2 injury, and both positive drawer and tilt tests signify a grade 3 injury. Difficulty jumping and landing within 2 weeks from the acute ankle sprain, abnormal postural or hip muscle control, or ligamentous laxity noted 8 weeks after injury are poor prognostic signs.
B. Imaging
Routine ankle radiographic views include the AP, lateral, and oblique (mortise) views. Less common views requested include the calcaneal view and subtalar view. The Ottawa Ankle Rules remain the best clinical prediction rules to guide the need for radiographs and have an 86–99% sensitivity and a 97–99% negative predictive value. If the patient is unable to bear weight immediately in the office setting or emergency department for four steps, then the clinician should check for (1) bony tenderness at the posterior edge of the medial or lateral malleolus and (2) bony tenderness over the navicular (medial midfoot) or at the base of the fifth metatarsal. If either malleolus demonstrates pain or deformity, then ankle radiographs should be obtained. If the foot has bony tenderness, obtain foot radiographs. An MRI is helpful when considering the associated injuries.
 Treatment
Treatment
Immediate treatment of an ankle sprain follows the MICE mnemonic: modified activities, ice, compression, and elevation. NSAIDs are useful in reducing pain and swelling in the first 72 hours following the ankle sprain. Subsequent treatment involves protected weight bearing with crutches and use of an ankle stabilizer brace, especially for grade 2 and 3 injuries. Early motion is essential, and patients should be encouraged to do a program of exercises or physical therapy. Proprioception and balance exercises (eg, “wobble board”) are useful to restore function to the ankle and prevent future ankle sprains. There is strong evidence for bracing and moderate evidence for neuromuscular training in preventing recurrence of an ankle sprain. Chronic instability can develop after acute ankle sprain in 10–20% of people and may require surgical stabilization with ligament reconstruction surgery.
 When to Refer
When to Refer
• Ankle fractures.
• Recurrent ankle sprains or signs of chronic ligamentous ankle instability.
• No response after more than 3 months of conservative treatment.
• Suspicion of associated injuries.
Delahunt E et al. Risk factors for lateral ankle sprains and chronic ankle instability. J Athl Train. 2019 Jun;54(6):611–6. [PMID: 31161942]
Doherty C et al. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017 Jan;51(2):113–25. [PMID: 28053200]
Kaminski TW et al. Prevention of lateral ankle sprains. J Athl Train. 2019 Jun;54(6):650–61. [PMID: 31116041]
Mandegaran R et al. Beyond the bones and joints: a review of ligamentous injuries of the foot and ankle on (99m)Tc-MDP-SPECT/CT. Br J Radiol. 2019 Dec;92(1104):20190506. [PMID: 31365277]
Medina McKeon JM et al. The ankle-joint complex: a kinesiologic approach to lateral ankle sprains. J Athl Train. 2019 Jun;54(6):589–602. [PMID: 31184957]
Vuurberg G et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018 Aug;52(15):956. [PMID: 29514819]
2. Eversion (“High”) Ankle Sprains
ESSENTIALS OF DIAGNOSIS

 Severe and prolonged pain.
Severe and prolonged pain.
 Limited range of motion.
Limited range of motion.
 Mild swelling.
Mild swelling.
 Difficulty with weight bearing.
Difficulty with weight bearing.
 General Considerations
General Considerations
A syndesmotic injury or “high ankle” sprain involves the anterior tibiofibular ligament in the anterolateral aspect of the ankle, superior to the anterior talofibular (ATF) ligament. The injury mechanism often involves the foot being turned out or externally rotated and everted (eg, when being tackled). This injury is commonly missed or misdiagnosed as an ATF ligament sprain on initial visit.
 Clinical Findings
Clinical Findings
A. Symptoms and Signs
Symptoms of a high ankle sprain include severe and prolonged pain over the anterior ankle at the anterior tibiofibular ligament, worse with weight bearing. This is often more painful than the typical ankle sprain. The point of maximal tenderness involves the anterior tibiofibular ligament, which is higher than the ATF ligament. It is also important to palpate the proximal fibula to rule out any proximal syndesmotic ligament injury and associated fracture known as a “maisonneuve fracture.” There is often some mild swelling in this area, and the patient may or may not have an ankle effusion. The patient usually has limited range of motion in all directions. To perform the external rotation stress test, the clinician fixes the tibia with one hand and grasps the foot in the other with the ankle in the neutral position. The ankle is then dorsiflexed and externally rotated, reproducing the patient’s pain. (Note: The patient’s foot should have an intact neurovascular examination before undertaking this test.)
B. Imaging
Radiographs of the ankle should include the AP, mortise, and lateral views. The mortise view may demonstrate loss of the normal overlap between the tibia and fibula, which should be at least 1–2 mm. Asymmetry in the joint space around the tibiotalar joint suggests disruption of the syndesmotic ligaments. If there is proximal tenderness in the lower leg especially around the fibula, an AP and lateral view of the tibia and fibula should be obtained to rule out a proximal fibula fracture. Radiographs during an external rotation stress test may visualize instability at the distal tibiofibular joint. MRI is the best method to visualize injury to the tibiofibular ligament and to assess status of the other ligaments and the articular cartilage.
 Treatment
Treatment
Whereas most ankle sprains are treated with early motion and weight bearing, treatment for a high ankle sprain should be conservative with a cast or walking boot for 4–6 weeks. Thereafter, protected weight bearing with crutches is recommended until the patient can walk pain-free. Physical therapy can start early to regain range of motion and maintain strength with limited weight bearing initially.
 When to Refer
When to Refer
If there is widening of the joint space and asymmetry at the tibiotalar joint, the patient should be referred urgently to a foot and ankle surgeon. Severe or prolonged persistent cases that do not heal may require internal fixation to avoid chronic instability at the tibiofibular joint. Screw fixation remains the gold standard, although newer techniques with bioabsorbable constructs are emerging.
Chen ET et al. Ankle sprains: evaluation, rehabilitation, and prevention. Curr Sports Med Rep. 2019 Jun;18(6):217–23. [PMID: 31385837]
Nickless JT et al. High ankle sprains: easy to miss, so follow these tips. J Fam Pract. 2019 Apr;68(3):E5–13. [PMID: 31039220]