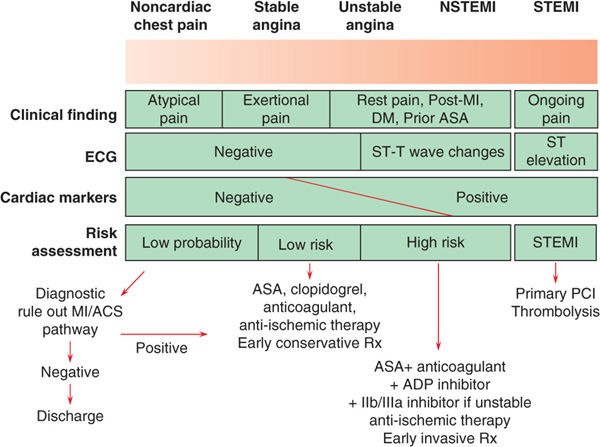
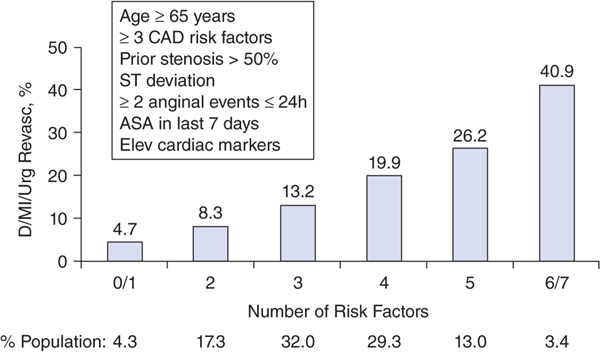
First step is appropriate triage based on likelihood of coronary artery disease (CAD) and acute coronary syndrome (Fig. 129-1) as well as identification of higher-risk pts (Fig. 129-2). Pts with low likelihood of active ischemia are initially monitored by serial ECGs and serum cardiac biomarkers, and for recurrent chest discomfort; if these are negative, stress testing (or CT angiography if probability of CAD is low) can be used for further therapeutic planning.
FIGURE 129-1 Algorithm for risk stratification and treatment of pts with suspected coronary artery disease. ACS, acute coronary syndrome; ASA, aspirin; DM, diabetes mellitus; ECG, electrocardiogram; LMWH, low-molecular-weight heparin; MI, myocardial infarction; PCI, percutaneous coronary intervention; Rx, treatment; STEMI, ST-segment elevation myocardial infarction. [Adapted from CP Cannon, E Braunwald, in Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 8th ed, P Libby et al (eds). Philadelphia, Saunders, 2008.]
FIGURE 129-2 The TIMI Risk Score for UA/NSTEMI. The quantity of listed attributes correlates with risk of death, MI, or need for urgent revascularization over 14 days. (Modified from E Antman et al: JAMA 284:835, 2000.)
Therapy of UA/NSTEMI is directed (1) against the inciting intracoro-nary thrombus, and (2) toward restoration of balance between myocardial oxygen supply and demand. Pts with the highest risk scores (Fig. 129-2) benefit the most from aggressive interventions.
ANTITHROMBOTIC THERAPIES
• Aspirin (325 mg initially, then 75–325 mg/d).
• Platelet ADP receptor antagonist: Clopidogrel (300–600 mg PO load, then 75 mg/d) unless excessive risk of bleeding or immediate coronary artery bypass grafting (CABG) likely; alternatives include ticagrelor [180 mg PO, then 90 mg PO bid (chronic aspirin dose should not exceed 100 mg daily)] or prasugrel (60 mg PO, then 10 mg daily) if PCI is planned.
• Anticoagulant: Unfractionated heparin (UFH) [60 U/kg then 12 (U/kg)/h (maximum 1000 U/h)] to achieve aPTT 1.5–2.5 × control, or low-molecular-weight heparin (e.g., enoxaparin 1 mg/kg SC q12h), which is superior to UFH in reduction of future cardiac events. Alternatives include (1) the factor Xa inhibitor fondaparinux (2.5 mg SC daily), which is associated with lower bleeding risk, or (2) the direct thrombin inhibitor bivalirudin [0.1 mg/kg, then 0.25 (mg/kg)/h], which causes less bleeding in pts undergoing catheterization compared with UFH plus a GP IIb/IIIa inhibitor.
• For high-risk unstable pts who undergo PCI, consider an IV GP IIb/IIIa antagonist [e.g., tirofiban, 0.4 (μg/kg)/min × 30 min, then 0.1 (μg/kg)/min for 48–96 h; or eptifibatide, 180-μg/kg bolus, then 2.0 (μg/kg)/min for 72–96 h].
ANTI-ISCHEMIC THERAPIES
• Nitroglycerin 0.3–0.6 mg sublingually or by buccal spray. If chest discomfort persists after three doses given 5 min apart, consider IV nitroglycerin (5–10 μg/min, then increase by 10 μg/min every 3–5 min until symptoms relieved or systolic bp <100 mmHg). Do not use nitrates in pts with recent use of phosphodiesterase-5 inhibitors for erectile dysfunction (e.g., not within 24 h of sildenafil or within 48 h of tadalafil).
• Beta blockers (e.g., metoprolol 25–50 mg PO q6h) targeted to a heart rate of 50–60 beats/min. In pts with contraindications to beta blockers (e.g., bronchospasm), consider long-acting verapamil or diltiazem (Table 126-1).
ADDITIONAL RECOMMENDATIONS
• Admit to unit with continuous ECG monitoring, initially with bed rest.
• Consider morphine sulfate 2–5 mg IV q5–30min for refractory chest discomfort.
• Add HMG-CoA reductase inhibitor (initially at high dose, e.g., atorvastatin 80 mg daily) and consider ACE inhibitor (Chap. 128).
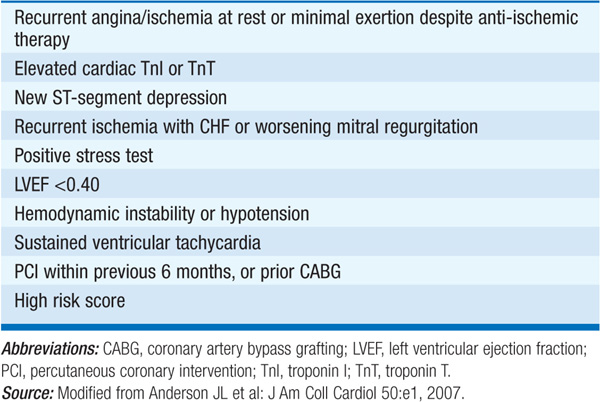
INVASIVE VS CONSERVATIVE STRATEGY In highest-risk pts (Table 129-1), an early invasive strategy (coronary arteriography within ~48 h followed by percutaneous intervention or CABG) improves outcomes. In lower-risk pts, angiography can be deferred but should be pursued if myocardial ischemia recurs spontaneously (angina or ST deviations at rest or with minimal activity) or is provoked by stress testing.
TABLE 129-1 CLASS I RECOMMENDATIONS FOR USE OF AN EARLY INVASIVE STRATEGY
LONG-TERM MANAGEMENT
• Stress importance of smoking cessation, achieving optimal weight, diet low in saturated and trans fats, regular exercise; these principles can be reinforced by encouraging pt to enter cardiac rehabilitation program.
• Continue aspirin, clopidogrel (or prasugrel or ticagrelor), beta blocker, statin, and ACE inhibitor or angiotensin receptor blocker (especially if hypertensive, or diabetic, or LV ejection fraction is reduced).