Cirrhosis is defined histopathologically and has a variety of causes, clinical features, and complications. In cirrhosis, there is the development of liver fibrosis to the point that there is architectural distortion with the formation of regenerative nodules, which results in decreased liver function.
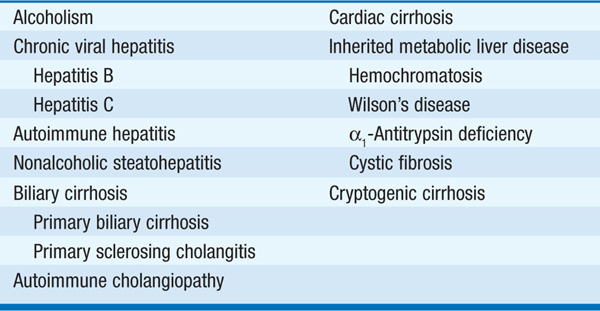
TABLE 165-1 CAUSES OF CIRRHOSIS
May be absent, with cirrhosis being incidentally found at surgery.
Anorexia, nausea, vomiting, diarrhea, vague RUQ pain, fatigue, weakness, fever, jaundice, amenorrhea, impotence, infertility.
Spider telangiectases, palmar erythema, jaundice, scleral icterus, parotid and lacrimal gland enlargement, clubbing, Dupuytren’s contracture, gynecomastia, testicular atrophy, hepatosplenomegaly, ascites, gastrointestinal bleeding (e.g., varices), hepatic encephalopathy.
Anemia (microcytic due to blood loss, macrocytic due to folate deficiency; hemolytic called Zieve’s syndrome), pancytopenia (hypersplenism), prolonged PT, rarely overt DIC; hyponatremia, hypokalemic alkalosis, glucose disturbances, hypoalbuminemia.
Depend on clinical setting. Serum: HBsAg, anti-HBc, anti-HBs, anti-HCV, anti-HDV, Fe, total iron-binding capacity, ferritin, antimitochondrial antibody (AMA), smooth-muscle antibody (SMA), anti-liver/kidney micro-somal (anti-LKM) antibody, ANA, ceruloplasmin, α1 antitrypsin (and phenotyping); abdominal ultrasound with Doppler study, CT or MRI (may show cirrhotic liver, splenomegaly, collaterals, venous thrombosis). Definitive diagnosis often depends on liver biopsy (percutaneous, transjugular, or open).
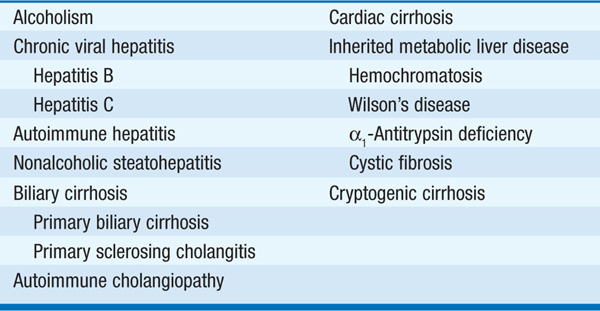
TABLE 165-2 COMPLICATIONS OF CIRRHOSIS
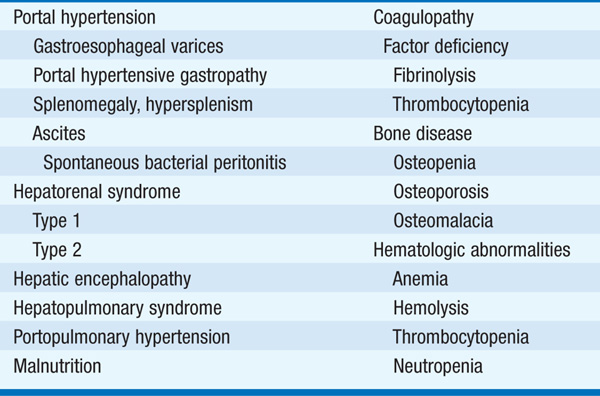
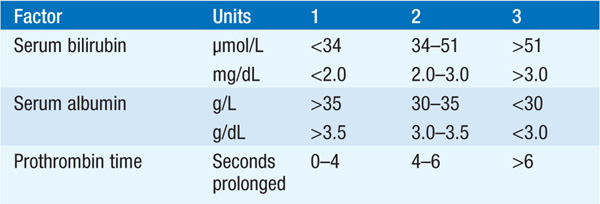
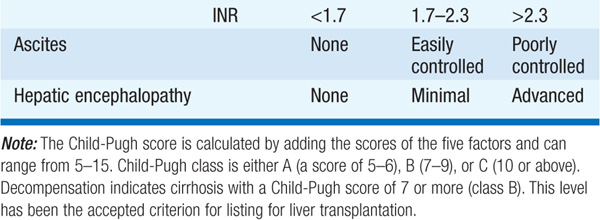
The Child-Pugh scoring system has been used to predict the severity of cirrhosis and the risk of complications (Table 165-3).
TABLE 165-3 CHILD-PUGH CLASSIFICATION OF CIRRHOSIS
Excessive alcohol use can cause fatty liver, alcoholic hepatitis, cirrhosis. Alcoholic cirrhosis accounts for about 40% of the deaths due to cirrhosis. History of excessive alcohol use often denied. Severe forms (hepatitis, cirrhosis) associated with ingestion of 160 g/d for 10–20 years; women more susceptible than men and develop advanced liver disease with less alcohol intake. Hepatitis B and C may be cofactors in the development of liver disease. Malnutrition may contribute to development of cirrhosis.
Often presents as asymptomatic hepatomegaly and mild elevations in biochemical liver tests. Reverses on withdrawal of ethanol; does not lead to cirrhosis.
Clinical presentation ranges from asymptomatic to severe liver failure with jaundice, ascites, GI bleeding, and encephalopathy. Typically anorexia, nausea, vomiting, fever, jaundice, tender hepatomegaly. Occasional cholestatic picture mimicking biliary obstruction. Aspartate aminotransferase (AST) usually <400 U/L and more than twofold higher than alanine aminotransferase (ALT). Bilirubin and WBC may be elevated. Diagnosis defined by liver biopsy findings: hepatocyte swelling, alcoholic hyaline (Mallory bodies), infiltration of PMNs, necrosis of hepatocytes, pericentral venular fibrosis.
Increased NADH/NAD ratio leads to lactic acidemia, ketoacidosis, hyper-uricemia, hypoglycemia, hypomagnesemia, hypophosphatemia. Also mitochondrial dysfunction, induction of microsomal enzymes resulting in altered drug metabolism, lipid peroxidation leading to membrane damage, hypermetabolic state; many features of alcoholic hepatitis are attributable to toxic effects of acetaldehyde and cytokines (interleukins 1 and 6, and TNF, released because of impaired detoxification of endotoxin).
Critically ill pts with alcoholic hepatitis have 30-day mortality rates >50%. Severe alcoholic hepatitis characterized by PT >5 × above control, bilirubin >137 μmol/L (>8 mg/dL), hypoalbuminemia, azotemia. A discriminant function can be calculated as 4.6 × (pt’s PT in seconds) (control PT in seconds) + serum bilirubin (mg/dL). Values ≥32 are associated with poor prognosis. Ascites, variceal hemorrhage, encephalopathy, hepatorenal syndrome predict a poor prognosis.
TREATMENT Alcoholic Liver Disease
Abstinence is essential; 8500- to 12,500-kJ (2000- to 3000-kcal) diet with 1 g/kg protein (less if encephalopathy). Daily multivitamin, thiamine 100 mg, folic acid 1 mg. Correct potassium, magnesium, and phosphate deficiencies. Transfusions of packed red cells, plasma as necessary. Monitor glucose (hypoglycemia in severe liver disease). Prednisone 40 mg/d or prednisolone 32 mg/d PO for 1 month may be beneficial in severe alcoholic hepatitis with encephalopathy (in absence of GI bleeding, renal failure, infection). Pentoxifylline demonstrated improved survival and led to the inclusion of this agent as an alternative to glucocorticoids in the treatment of severe alcoholic hepatitis. Liver transplantation may be an option in carefully selected cirrhotic pts who have been abstinent >6 months.
PBC is a progressive nonsuppurative destructive intrahepatic cholangitis. Strong female predominance, median age of 50 years. Presents as asymptomatic elevation in alkaline phosphatase (better prognosis) or with pruritus, progressive jaundice, consequences of impaired bile excretion, and ultimately cirrhosis and liver failure.
Pruritus, fatigue, jaundice, xanthelasma, xanthomata, osteoporosis, steator-rhea, skin pigmentation, hepatosplenomegaly, portal hypertension; elevations in serum alkaline phosphatase, bilirubin, cholesterol, and IgM levels.
Sjögren’s syndrome, collagen vascular diseases, thyroiditis, glomerulonephritis, pernicious anemia, renal tubular acidosis.
Antimitochondrial antibodies (AMA) in 90% (directed against enzymes of the pyruvate dehydrogenase complex and other 2-oxo-acid dehydrogenase mitochondrial enzymes). Liver biopsy most important in AMA-negative PBC. Biopsies identify 4 stages: stage 1—destruction of interlobular bile ducts, granulomas; stage 2—ductular proliferation; stage 3—fibrosis; stage 4—cirrhosis.
Correlates with age, serum bilirubin, serum albumin, prothrombin time, edema.
TREATMENT Primary Biliary Cirrhosis
Ursodeoxycholic acid 13–15 mg/kg per day has been shown to improve the biochemical and histologic features of disease. Response is greatest when given early. Cholestyramine 4 g PO with meals for pruritus; in refractory cases consider rifampin, naltrexone, plasmapheresis. Calcium, vitamin D, and bisphosphonates are given for osteoporosis. Liver transplantation for end-stage disease.
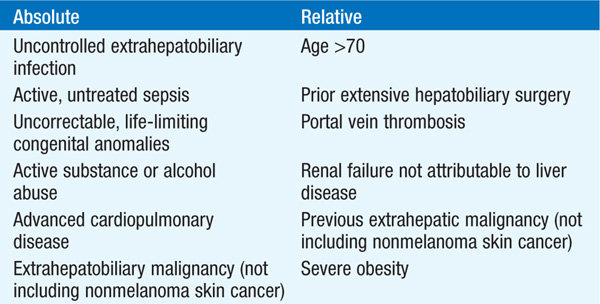
Consider in the absence of contraindications for chronic, irreversible, progressive liver disease or fulminant hepatic failure when no alternative therapy is available (Table 165-4).
TABLE 165-4 INDICATIONS FOR LIVER TRANSPLANTATION
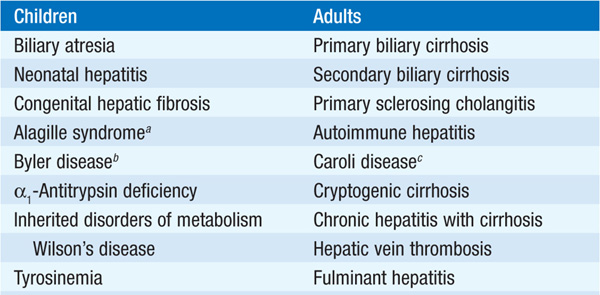
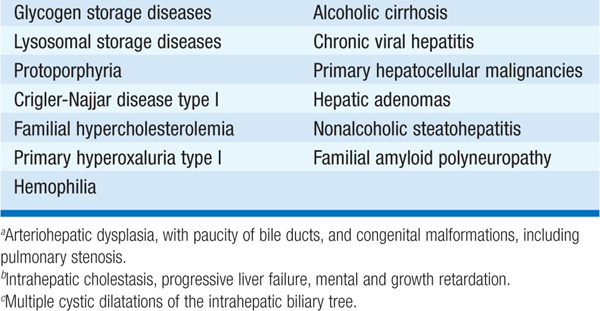
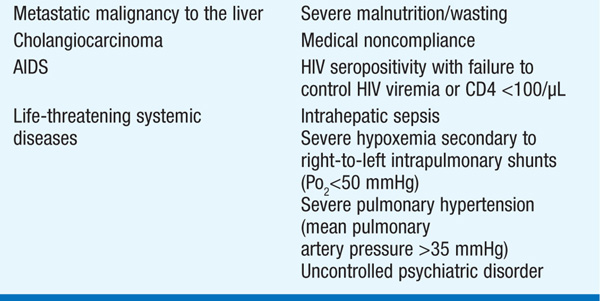
TABLE 165-5 CONTRAINDICATIONS TO LIVER TRANSPLANTATION
Matched for ABO blood group compatibility and liver size (reduced-size grafts may be used, esp. in children). Should be negative for HIV, HBV, and HCV. Living-donor transplant has gained increased popularity with transplantation of the right hepatic lobe from a healthy adult donor to an adult. Living-donor transplant of the left lobe accounts for one-third of all liver transplants in children.
Various combinations of tacrolimus or cyclosporine and glucocorticoids, sirolimus, mycophenolate mofetil, or OKT3 (monoclonal antithymocyte globulin).
Liver graft dysfunction (primary nonfunction, acute or chronic rejection, ischemia, hepatic artery thrombosis, biliary obstruction or leak, recurrence of primary disease); infections (bacterial, viral, fungal, opportunistic); renal dysfunction; neuropsychiatric disorders, cardiovascular instability, pulmonary compromise.
Currently, 5-year survival rates exceed 60%; less for certain conditions (e.g., chronic hepatitis B, hepatocellular carcinoma).